Patients with resuscitated out-of-hospital cardiac arrest (OHCA) in the setting of myocardial infarction (MI) continue to have high rates of in-hospital mortality.1 However, limited data are available regarding outcomes of OHCA in young adults, particularly in the setting of MI. We sought to determine the prevalence and outcomes of OHCA in individuals with their first MI at ≤ age 50.
We retrospectively analyzed records of patients with or without OHCA presenting with Type 1 MI and age ≤50 years at two academic hospitals from 2000-2016. The design of the Partners YOUNG-MI registry has been previously described.2 The Third Universal Definition of MI was used to adjudicate all events. In-hospital and long-term mortality were determined by review of medical records and via the Social Security Administration’s Death Master File and the National Death Index. Cause of death was adjudicated by two cardiologists. The study was approved by an institutional review board; subjects did not provide informed consent as this was a retrospective analysis.
Cox proportional hazards models were constructed for survival free from all-cause death and cardiovascular death. Multivariable risk adjustment was performed using variables with significant univariable association with either all-cause mortality or cardiovascular death. Landmark analysis was performed for patients who survived to hospital discharge.
Of 2097 patients with Type 1 MI (mean age 44±5.1 years, 19.3% female, 73% white), 100 (4.8%) presented with OHCA. Patients with OHCA were significantly more likely to present with an ST-elevation MI (77,77.0% versus 1044,52.3%, p<0.001), higher creatinine (1.3 versus 1.0, p<0.001), and higher troponin levels (p<0.001). In addition, patients with OHCA had a significantly lower ejection fraction (45% versus 55%, p<0.001).
Patients with OHCA were less likely to have diabetes (9, 9.0% versus 401, 20.3%, p=0.004), and had lower median ASCVD scores (3.5 versus 4.7, p=0.005). However, patients with OHCA were significantly more likely to use tobacco (62, 62.0% versus 1004, 50.8%, p=0.03) as well as cocaine or marijuana (25,25.0% versus 296,14.8%, p=0.01).3 Median length of stay was significantly longer in the OHCA group (8.0 versus 3.0 days, p<0.001). Eighty-nine patients (89.0%) had a shockable rhythm.
Patients with OHCA were significantly less likely to undergo coronary angiography (89.9% versus 96.4%, p=0.004); however, among patients who survived to discharge, there was no significant difference (96.6% versus 96.2%, p=0.75). There was no difference in revascularization between those who underwent angiography in the two groups (92.1% versus 90.5%, p=0.85).
Among patients who survived to hospital discharge, there was no difference in the number of patients prescribed aspirin, beta-blocker, antiplatelet, and statin therapy between the OHCA and non-OHCA groups. Fourteen patients (17.7%) received an ICD prior to discharge.
Over a median follow-up of 11.2 years, 26 deaths (26%) occurred in the OHCA group compared with 228(11.4%) in those without OCHA (logrank p<0.001); Figure 1A). The adjusted hazard ratio of OCHA for all-cause death was 2.72 (95% CI 1.75 to 4.22, p < 0.001). In-hospital death occurred in 21 (21.0%) of the OHCA group compared with 23 (1.2%) in the non-OHCA group (p<0.001). Among patients who survived to discharge, there was no difference in all-cause mortality [5 deaths (6.3%) in OHCA group versus 204 deaths (10.3%) in non-arrest group, p=0.34] or cardiovascular mortality [2 cardiovascular deaths (2.5%) vs 204 deaths (10.3%) in non-arrest group, p=0.77] (Figure 1B). For those patients who survived to discharge, the adjusted hazard ratio of OHCA for all-cause death was 0.70 (95% CI 0.29 to 1.71, p = 0.436).
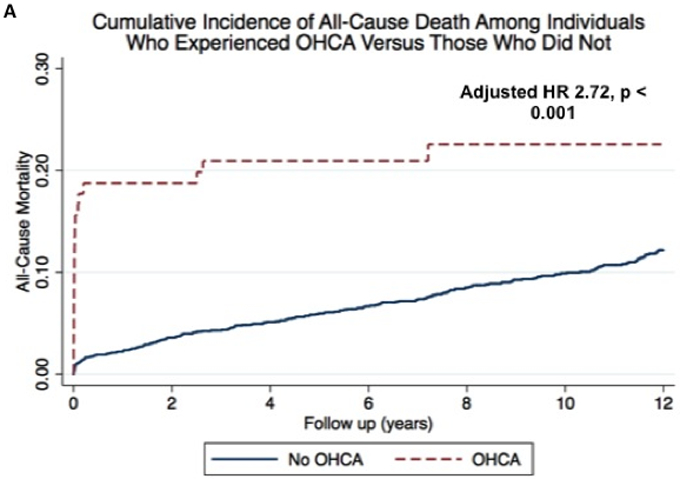
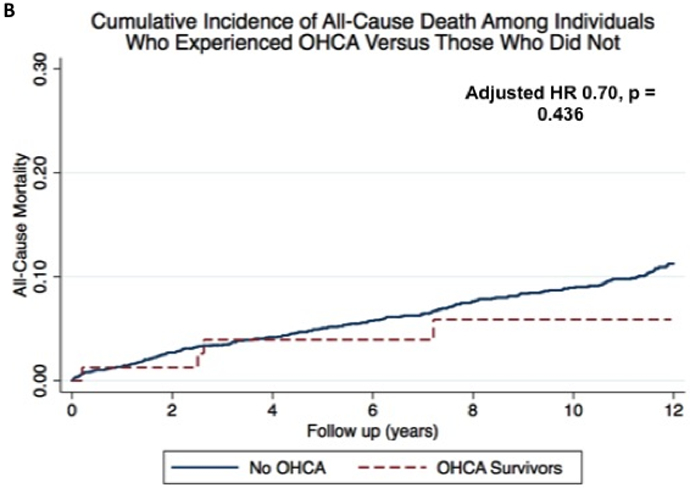
Cumulative incidence curves illustrating cumulative all-cause mortality in patients with out-of-hospital cardiac arrest compared with those without out-of-hospital cardiac arrest (Panel A) and landmark analysis of those with out-of-hospital cardiac arrest who survived past hospital discharge compared with those without out-of-hospital cardiac arrest (Panel B).
Our study examined the prevalence and outcomes of OHCA in young patients with MI. Approximately 1 in 20 patients presenting with a first MI at age ≤50 had an OHCA. Patients with OHCA were more likely to die in-hospital compared with patients without OHCA. However, among OHCA patients who survived to hospital discharge, there was no significant difference in long term all-cause or cardiovascular mortality when compared to those without OHCA. Supporting the favorable outcomes observed in young adults who experience an OHCA, data from the MONICA registry evaluated trends in outcomes of OHCA in younger (25-64 years) and older (65-74 years) populations and found that survival beyond 28 days was better in the younger age group.4 Our data are unique in that they specifically focus on young patients with OHCA with MI and compare them to a similar group of young individuals with MI who did not experience OHCA.
OHCA in young adults in the setting of myocardial infarction is infrequent but associated with significant in-hospital mortality. However, over a median follow-up of 11.2 years, we found no significant difference in all-cause and cardiovascular mortality among the OHCA patients who survived to hospital discharge and those patients without OHCA. Our results support the need for further research for prompt treatment of sudden cardiac death in this population.
Footnotes
Disclosures: Dr. Deepak L. Bhatt discloses the following relationships - Advisory Board: Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute), Cleveland Clinic, Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine, Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Vice-Chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), HMP Global (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Population Health Research Institute (clinical trial steering committee), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Abbott, Amarin, Amgen, AstraZeneca, Bristol-Myers Squibb, Chiesi, Eisai, Ethicon, Forest Laboratories, Idorsia, Ironwood, Ischemix, Lilly, Medtronic, PhaseBio, Pfizer, Regeneron, Roche, Sanofi Aventis, Synaptic, The Medicines Company; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); Site Co-Investigator: Biotronik, Boston Scientific, St. Jude Medical (now Abbott), Svelte; Trustee: American College of Cardiology; Unfunded Research: FlowCo, Merck, PLx Pharma, Takeda. Dr. Blankstein has served on the advisory board of Amgen; and has received research support from Amgen Inc., Sanofi Inc, and Astellas Inc. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Data Sharing: The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
References
- 1.Alahmar AE, Nelson CP, Snell KIE, Yuyun MF, Musameh MD, Timmis A, Birkhead JS, Chugh SS, Thompson JR, Squire IB, Samani NJ. Resuscitated cardiac arrest and prognosis following myocardial infarction. Heart Br Card Soc. 2014;100:1125–1132. [DOI] [PubMed] [Google Scholar]
- 2.Singh A, Collins B, Qamar A, Gupta A, Fatima A, Divakaran S, Klein J, Hainer J, Jarolim P, Shah RV, Nasir K, Di Carli MF, Bhatt DL, Blankstein R. Study of young patients with myocardial infarction: Design and rationale of the YOUNG-MI Registry. Clin Cardiol. 2017;40:955–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeFilippis EM, Singh A, Divakaran S, Gupta A, Collins BL, Biery D, Qamar A, Fatima A, Ramsis M, Pipilas D, Rajabi R, Eng M, Hainer J, Klein J, Januzzi JL, Nasir K, Di Carli MF, Bhatt DL, Blankstein R. Cocaine and Marijuana Use Among Young Adults With Myocardial Infarction. J Am Coll Cardiol. 2018;71:2540–2551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Forslund A-S, Söderberg S, Jansson J-H, Lundblad D. Trends in incidence and outcome of out-of-hospital cardiac arrest among people with validated myocardial infarction. Eur J Prev Cardiol. 2013;20:260–267. [DOI] [PubMed] [Google Scholar]


