Abstract
In the past few decades, extensive research has been conducted on atrial conduction disorders and their clinical relevance. An association between interatrial block (IAB) and supraventricular arrhythmias [most commonly atrial fibrillation (AF)] has been discovered and extensively investigated. We coined the term “Bayés Syndrome” to describe this association, and the medical community has accepted the eponym in recognition to the scientist who discovered most of the aspects associated with it. In this non-systematic review, we will focus on the association between IAB and AF, with special emphasis on the value of the surface 12-lead ECG as a valid tool to predict AF.
Keywords: Atrial fibrillation, bayes syndrome, interatrial block
Interatrial block (IAB) is a distinct electrocardiographic pattern that has been studied with growing interest since it was first described in 1979 by Bayés de Luna [1]. The conduction delay seen in IAB is thought to be mediated by the Bachmann region, which is the largest and most common anatomical route for interatrial conduction during a normal sinus rhythm [2–6]. IAB results from a conduction delay between the atria, and like other blocks can be classified into degrees [6]. Partial (first degree) IAB (pIAB), which is much more common, manifests as a prolongation of the P-wave (P-wave duration ≥120 ms) (measured in the inferior leads: II, III, and aVF) without any other significant abnormality [6, 7]. This prolongation is thought to occur when the electrical impulses from the right atrium continue to conduct via a partially blocked Bachmann region [7]. Advanced (third degree) IAB (aIAB) is less frequent and is represented on ECG as a biphasic (±) P-wave in the inferior leads in addition to the elongated P-wave described above (Fig. 1). aIAB is thought to occur when the sinus impulses can no longer pass via the Bachmann region or other preferential conduction tracts. Instead, the net electrical vector goes toward the AV node as the right atrium depolarizes through the internodal pathways, following which the left atrium is depolarized in a caudocranial direction starting at a crossing point at the inferior aspect of the left atrium near the atrioventricular node (most frequently the coronary sinus, and in small proportion, the fossa ovalis) [7]. This superior-inferior-superior activation pattern is what is thought to result in the biphasic (±) P-wave seen on the inferior leads [6] (Fig. 2). Although few studies have examined the histological and pathophysiological changes that accompany partial or complete blockade of this interatrial conduction pathway, it is reasonable to believe the same underlying structural remodeling process may be responsible for both partial and advanced IAB. There is emerging evidence that atrial remodeling resulting from progressive fibrosis of the interatrial conduction system or from changes in the electrical properties of the atrial myocytes play a role [8, 9] (Fig. 3). If IAB is truly a progressive process, temporal modification of the P-wave would be expected to occur, a phenomenon which has been documented in several studies and case reports. Interestingly, there is recent evidence that in certain conditions, the changes to the atria that result in IAB may be reversed with specific therapies. A reduction in the P-wave duration has been noted in several studies, indicating that the pathological process leading to IAB may be dynamic. This reverse atrial remodeling supports the idea that the development and progression of IAB depends on insults to the atrium in a time-dependent manner and is not a single permanent event. The recent demonstration of the atrial fibrotic process using cardiac magnetic resonance reconfirms the ECG/VCG observations [10, 11].
Figure 1.
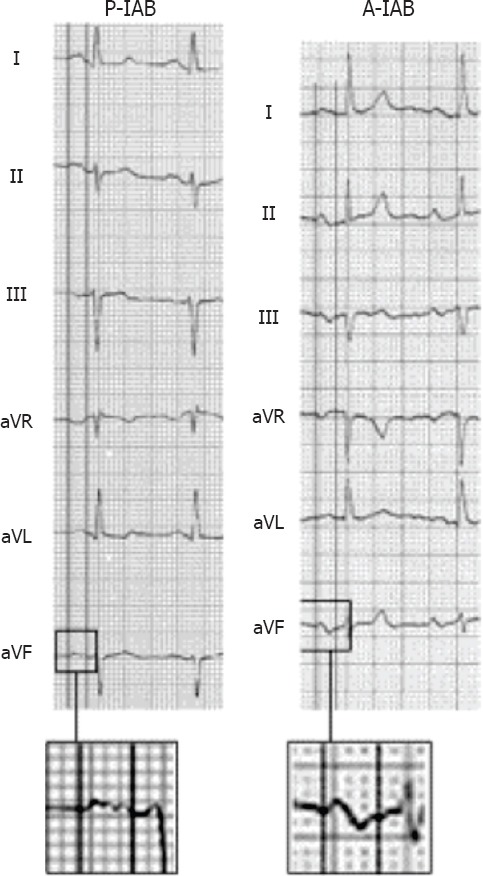
The most common types of IAB are partial (P-IAB) and advanced (A-IAB). Note the calipers simultaneously measuring the P-wave onset and P-wave offset in all lead limbs
Figure 2.
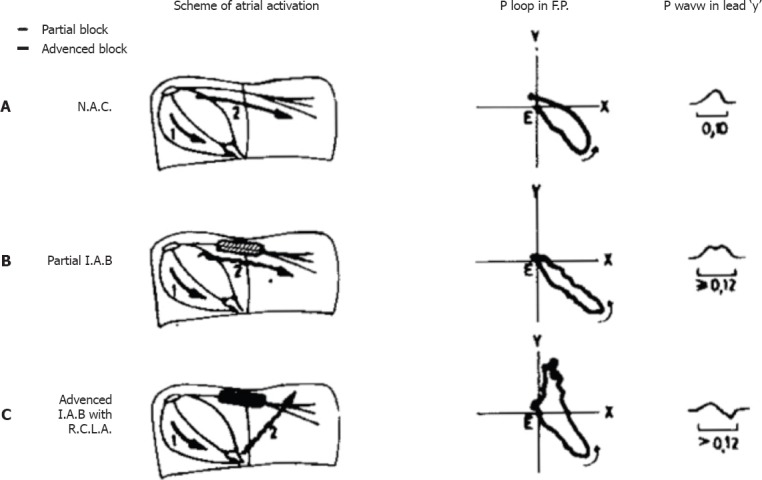
Traditional diagram from the original papers of Bayés de Luna to explain the delay of conduction in the Bachmann region and the retrograde activation of the left atrium.
Evaluate ECG-VCG diagnostic criteria; To study the prevalence; Relationship with LAE; Relationship with P.T.
Figure 3.
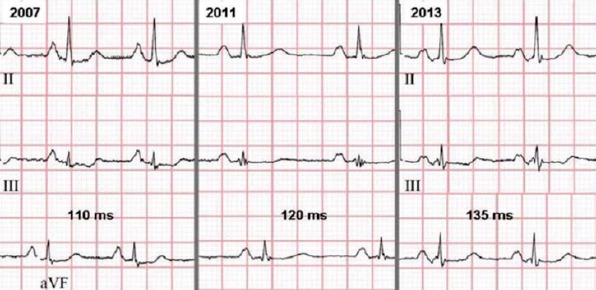
Progressive IAB. Note the prolongation of the P-wave and the appearance of the final negative component over time
More recently, sophisticated echocardiographic studies using “speckle tracking” have also demonstrated the activation pattern and physiopathological mechanisms described above [12].
Pathophysiology
Atrial conduction
The Bachmann Bundle (BB), first described in 1916, is the most common anatomical route for interatrial conduction during sinus rhythm [2–5]. BB (although we consider that the proper term should be “Bachmann region”) is a broad, muscular band that originates from the anterior internodal pathway as it emerges from the anterior lip of the sinoatrial node. It is composed of a trapezoid, band-like bundle of parallel fibers that follow the superior segment of the interatrial sulcus [13]. The role of this bundle is to allow for rapid conduction between the atria, allowing for synchronously timed atrial contraction [8]. Additional interatrial conduction routes have also been described at the level of the fossa ovalis [14, 15] and coronary sinus [16–18], which may also play a role in electrical impulse propagation between the atria [19]. BB is thought to mediate IAB because the experimental interruptions of BB in a canine model reproduced the classic wide P-waves with±morphology of aIAB [20]. Among other evidence, a study by Cosio et al. [4] showed that in two human cases with ECG evidence of advanced atrial block, the timing of activation over the left atrial roof was consistent with a block of the Bachmann region. While the macro scale conduction disturbances of IAB have been well correlated with a disruption of the Bachmann region, few studies have observed the mechanism through which this disruption occurs.
Structural atrial remodeling
Reduced atrial contractility, fibrosis development, and atrial enlargement are the main components of atrial structural remodeling [21]. The ability of atrial fibrosis to delay cardiac electrical conduction has been well documented [22–24]. It has been demonstrated in humans that reactive fibrosis accompanying the reparative fibrosis of degenerating myocytes can cause interstitial expansion, which in turn can cause a separation of surviving myocytes and a deterioration of intermyocyte coupling, creating a barrier to impulse propagation [22–24]. Atrial fibrosis is the common end pathway for various cardiac insults, which share common molecular fibrotic pathways [22]. The cellular mechanisms underlying atrial fibrosis are not entirely clear; however, there is emerging evidence that a multifactorial process involving complex interactions between neurohormonal and cellular mediators is responsible [24].
It has been hypothesized that IAB results from fibrotic atrial remodeling due to reduction of the blood supply (ischemia) to the Bachmann region [8, 25]. Supporting this hypothesis, coronary artery disease and hypertension have been described as leading risk factors for IAB [25]. The sinoatrial nodal (SAN) artery and its branches provide the main arterial blood supply to this region [26]. The SAN artery may arise from the proximal or mid portions of the right coronary or left circumflex arteries [8]; however, the majority of the time the origin is the right coronary artery [26]. Ariyarajah et al. [26] demonstrated in 2007 that in patients with significant coronary artery disease (>70% stenosis) and IAB, RCA (compared with LCx) was the artery affected in the majority of cases. Since this correlates with a blockage of the most common blood supply of the Bachmann region, the authors postulated that ischemia of the Bachmann region and resulting fibrosis predispose the development of IAB.
In 2008, Saremi et al. performed a retrospective trial using computed tomographic angiography [8, 27]. They found that patients with severe coronary artery disease and IAB or atrial fibrillation (AF) had higher structural changes and a less well-visualized Bachmann region8. Although the role of atrial fibrosis in the development of interatrial block is still unproven, it is a leading candidate among possible structural etiologic agents.
How to measure the P-wave?
In the surface ECG, the measurement of the P-wave and the diagnosis of IAB can be done at the first glance if the ECG recording and morphology in leads II, III, and aVF is clear and free of artifacts or pacing spikes. The diagnosis of aIAB may be done after the consensus paper published in 20126 following the criteria established by Bayés de Luna already in 19891. To be sure about the measurement of the P-wave in difficult cases (and for research purposes), consistency in the measurements is key. Analyzing digitalized ECG images using amplification as well as using ECG systems that allow at least three simultaneous channels (six or 12 channels are ideal) is paramount (Fig. 1). Particular attention should be given to the six leads of the frontal plane simultaneously because it is where we will better identify the changes to the P-wave duration and morphology produced by IAB. However, the horizontal plane leads, particularly lead V1, are also important (Morris index and P-terminal force in lead V1) and should be checked for the possible diagnosis of associated LA enlargement. To perform a good measurement of the P-wave duration, it is important to check and define the interval between the earliest detection of the P-wave (onset) in any lead of the frontal plane and the latest one (offset). Once these two points are defined with lines, the P-wave duration can be measured using calipers or semi-automatic calipers [28].
Bayés Syndrome: IAB as a predictor of AF general considerations
The association between IAB and supraventricular arrhythmias (mostly AF) has been initially described by Bayés de Luna and subsequently demonstrated in many different clinical scenarios. This association, recently termed as “Bayés Syndrome,” has important clinical implications [28–32]. The early identification of the ECG pattern would prompt more extensive cardiac monitoring searching for AF. This would allow early initiation of oral anticoagulation to prevent stroke. An interesting hypothesis has been advanced to consider early full oral anticoagulation in patients with aIAB but non-documented AF (NDAF). In this section, we will review the relationship between IAB and AF in different clinical scenarios.
IAB as a predictor of post-cardioversion AF recurrence
In 2014, Enriquez et al. [33] conducted a study to determine whether IAB predicted AF recurrence following pharmacological cardioversion. They included 61 patients with recent-onset AF and no structural heart disease who recently underwent cardioversion with one of the two antiarrhythmic drugs. Thirty-one patients received a single oral dose of propafenone, whereas 30 patients received IV vernakalant. A 12-lead ECG following conversion was evaluated for the presence of partial or advanced IAB. Clinical follow-up and electrocardiographic recordings were performed for a 12-month period. aIAB was present in 18% of the population and partial IAB in 16.4% of the population. Overall AF recurrence was 36%, with a 90.9% recurrence in patients with aIAB versus 70% in those with partial IAB. In patients without IAB, there was a 12.5% recurrence rate (p=0.001) [33]. A multivariate analysis found IAB to be independently associated with AF recurrence (odds ratio, 18.4) [33]. The study confirms that aIAB is strongly associated with a higher risk of AF recurrence 1 year following pharmacological cardioversion, independent of the antiarrhythmic drug used.
IAB as a predictor of post-pulmonary vein isolation AF recurrence
Pulmonary vein isolation is only successful in 70%–80% of cases and often requires a repeat procedure, indicating that electrical abnormalities outside of the pulmonary veins may be involved in the pathogenesis of recurrent paroxysmal AF in this population. Caldwell et al. [34] studied a cohort of 114 patients who underwent pulmonary vein isolation to test the hypothesis that patients with IAB have a higher rate of paroxysmal AF recurrence than those without IAB. They analyzed 12-lead ECGs for all patients for the presence of IAB as well as P-wave dispersion and followed patients for paroxysmal AF recurrence. They found that patients with aIAB had a higher rate of paroxysmal AF recurrence than those without IAB (66.6% vs. 40.3%; p=<0.05), indicating that IAB is a predictor of AF in the post-pulmonary vein isolation population [34].
IAB as a predictor of post-atrial flutter ablation AF recurrence
Cavotricuspid isthmus ablation is the first-line curative therapy for typical atrial flutter and has a success rate of >90%. Enriquez et al. [35] hypothesized that aIAB is associated with an elevated risk of AF in patients who underwent catheter ablation for typical atrial flutter. They studied a cohort of 187 patients with typical atrial flutter and no AF history. Patients with repeat ablations or no evidence of bidirectional block were excluded from the study. The mean age of the population was 67 years. Over a mean follow-up period of 24.2 months, they found that patients with aIAB had a higher rate of recurrence of new-onset AF than those without aIAB (64.7% vs. 29.4%; p=<0.001)[35]. After a comprehensive multivariate analysis, aIAB was determined to be the strongest predictor of AF (odds ratio, 4.2; 95% confidence interval, 1.9–9.3; p=<0.001). Therefore, this study indicates that IAB is a predictor of new-onset AF in the post-cavotricuspid isthmus ablation population [35].
IAB as a predictor of new-onset AF in patients with chagas disease
Chagas cardiomyopathy is an endemic disease in Latin America. Patients with Chagas cardiomyopathy usually present with a low ejection fraction, and some patients have an ICD device implanted for primary or secondary prevention. A significant proportion of these patients develop AF, which may result in stroke, embolism, and inappropriate ICD shock. This is associated with increased morbidity and/or mortality. For this reason, Enriquez et al. investigated IAB as a possible predictor for AF in this population [36]. They conducted a retrospective study of patients with Chagas cardiomyopathy and ICDs from 14 centers in Latin America. The presence of advanced or partial IAB was identified, and the patients were followed up over a 33-month period for evaluating new-onset AF36. The mean age was 54.6 years, the mean ejection fraction was 49%, and the presence of IAB was 18.8% (10% advanced, 8.8% partial). During the follow-up period, AF occurred in 13.8% of the patients and was significantly greater in the group with IAB (advanced and partial) than in the group without IAB (73.3% vs. 0%; p<0.0001). The number of inappropriate ICD shocks was significantly higher in the group with IAB (p=0.014). In conclusion, IAB predicts new-onset AF in patients with Chagas’ cardiomyopathy and ICDs [36].
IAB as a predictor of new-onset AF in patients with NSTEMI
IAB is thought to occur via partial or complete blockade of BB, the largest and most common anatomical route for conduction between the atria. It has been suggested that fibrotic remodeling of the atria may lead to IAB. Alexander et al. [25] hypothesized that a higher burden of coronary artery disease is associated with a higher prevalence of IAB in patients who present with NSTEMI due to fibrotic ischemic atrial remodelling. As a secondary outcome, they hypothesized that IAB is associated with new-onset AF in this population. They analyzed 322 consecutive patients who presented with NSTEMI and underwent both coronary angiography and a baseline ECG at a single center. The mean age of the population was 65.4 years. They found that the presence of diffuse coronary artery disease defined as >1 significant coronary artery lesion (≥70% occlusion) was associated with the presence of IAB (69.8% vs. 48.1%; p=0.026). In addition, they found that patients with IAB had a higher incidence of new-onset AF within 1 year than those without IAB (55.9% vs 36.1%; p=0.021) [25]. This study shows that in the general NSTEMI population, IAB is associated with the development of new-onset AF [25].
IAB as a predictor of post-transcatheter aortic valve replacement new-onset AF
The transcatheter aortic valve replacement (TAVR) procedure was first performed in 2002 and has since become an increasingly popular procedure for those deemed to be at a high risk for TAVR. Alexander et al. [37] conducted a retrospective study of one hospital in Canada and one hospital in Spain to examine the association of aIAB and new-onset AF in the TAVR population. ECGs were analyzed for the presence of IAB. Patients were followed up for a minimum of 1 year to determine the incidence of new-onset AF. The population had a mean age of 83 years. New-onset AF occurred more frequently in patients with aIAB at baseline than those without aIAB (42.9% vs. 22.9%; p=0.14) [37]. This study indicates that aIAB is associated with new-onset AF in the post-TAVR population [37].
IAB as a predictor of new-onset AF in patients with severe heart failure
Sadiq Ali et al. [38] further evaluated IAB in patients with advanced heart failure (HF) requiring cardiac resynchronization therapy (CRT). They sought to determine whether IAB could predict new-onset AF in this population. The study included 112 patients with severe HF receiving an implanted cardiac resynchronization device. These patients had no AF history and 65% of HF was due to ischemic heart disease. The mean age was 67 years, and 37.2% of patients had aIAB. After 30 months of follow-up, new-onset AF occurred in 29% of the patients. The prevalence of AF was significantly higher in the group with aIAB than in the group without aIAB (50% vs. 17% respectively; p<0.001) [38]. In a multivariate analysis, older age (OR, 1.06; 95% CI, 1.002–1.130; p=0.04) and aIAB (OR, 4.91; 95% CI, 2.06–11.69; (p<0.001) were independent predictors of AF occurrence. In summary, IAB was detected in more than one third of this population. It was an independent predictor of AF in patients with severe HF undergoing cardiac resynchronization device implantation with no AF history [38].
IAB as a predictor of atrial high-rate episodes in patients with cardiac devices
Recent studies suggest that asymptomatic paroxysmal atrial fibrillation (PAF) episodes occur more frequently than symptomatic PAF [39]. Technological advances in long-term ECG monitoring particularly in patients with cardiac implantable electronic devices enabled clinicians to diagnose asymptomatic PAF episodes, namely atrial high-rate episodes (AHRE) (Fig. 4). Subsequent studies established the predictive role of AHRE as a harbinger of future symptomatic AF and ischemic stroke [39–41]. Tekkesin et al. [42] evaluated the predictive value of IAB on the occurrence of AHRE in 367 patients with dual-chamber pacemakers implanted due to sinus node dysfunction. Standard 12-lead surface ECG was performed to patients before device implantation to diagnose IAB. AHRE was detected in 107 patients (30.1%) during device interrogation 6 months after the implantation. Study patients were divided into two groups according to the presence of AHRE in their device interrogation. Sixty-seven (27%) patients in AHRE (−) group had IAB, whereas 48 (44.9%) patients had in AHRE (+) group (p<0.01) [42]. This initial experience suggested that IAB was a predictor of future symptomatic as well as asymptomatic AF.
Figure 4.
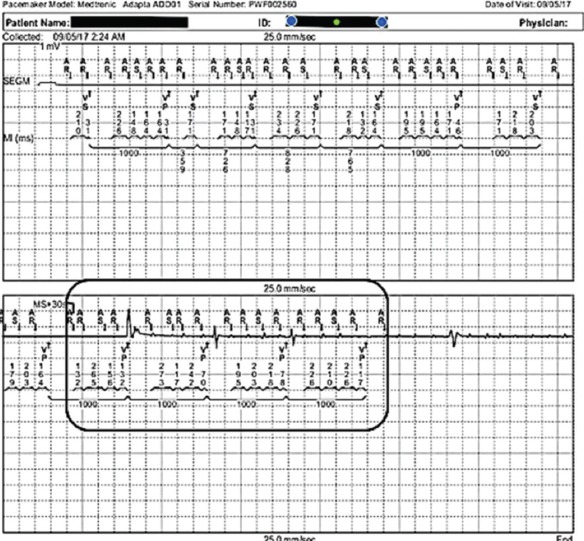
AHRE episode detected by a dual-chamber pacemaker. Note AF in the electrogram recorded and stored by the device.
AR: atrial refractory; AS: atrial sensing; VP: ventricular pacing; VS: ventricular sensing
IAB as a predictor of AF in the general population
P-wave prolongation has shown a strong association with the development of AF in the general population. The two epidemiological studies that more clearly showed the relation of IAB with the risk of AF are the Atherosclerosis Risk in Communities (ARIC) study [43] and the Copenhagen ECG Study [44]. In both cases, it was shown that IAB, particularly aIAB, is associated with an increased risk of AF. Also, in the ARIC cohort, the risk factors for developing aIAB were similar to those for developing AF.
Aging with IAB
Aging gradually modifies the specialized cardiac conducting system, creating a milieu that facilitates the appearance of IAB [45]. IAB is related to atrial fibrosis, which produces a slowing of electrical transmission and atrial activation. The progressive degree of atrial fibrosis probably plays a central role in the increase of IAB prevalence with age [7]; moreover, fibrosis is associated with age and is per se a risk factor for stroke [46]. The P-wave duration is positively correlated to age, even in infancy [47]. IAB, practically inexistent in healthy children, is rare in younger adults (except in the case of cryptogenic stroke and patent foramen ovale), with a prevalence of only 16% in a control group with a mean age of 37 years. However, the prevalence of IAB increases with age [48, 49]. In septuagenarians, the prevalence is almost 40%50 and is >50% in those aged >80 years [48]. In the case of aIAB, the relation with age is even clearer. In the ARIC study [43], performed in a global population with mean age of 54 years, only 0.5% had aIAB at baseline; however, age had a strong effect as 1.3% developed aIAB during the mean 6-year follow-up. These authors found an incidence of 2.3 per 1.000 person-years for aIAB. This association with age is probably related to the fact that aging increases not only the rate of elderly population but also the prevalence of cardiovascular disease, a strong predictor of IAB. Moreover, the recent advances in the management of cardiac conditions are increasing the survival of patients with heart disease, particularly those who already have IAB or will acquire it during the course of their disease.
IAB and stroke
The relevance of IAB is mainly related to its association with stroke, an association particularly strong in patients with aIAB [50, 51]. This association could be related, at least in part, to supraventricular arrhythmias and poor left atrium contractility. Conversely, IAB could just be a marker for the overall burden of cardiovascular disease. In the Cardiac and Clinical Characterization of Centenarians (4C) registry [49], the incidence of previous stroke in centenarians with IAB was high (reaching almost 30% in patients with aIAB). In the 4C registry, the relatively low incidence of stroke in centenarians with AF was probably related to the fact that patients with AF frequently benefit from anticoagulation therapy, whereas this is not the case in those with aIAB. Centenarians with IAB also presented a higher rate of dementia than those with a normal P-wave, a possible consequence of cerebral microinfarcts.
The BAYES registry
An International Registry has been launched in October 2016 with almost 40 centers from all around the world looking after almost 700 patients, the BAYES (Interatrial Block and Yearly Events) registry [52]. This work will provide further insight into the ability of IAB to predict AF (in elderly populations with structural heart disease) using a simple and economical method such as the 12-lead ECG. Patients are enrolled in three groups: normal P-wave, pIAB, or aIAB. More than 450 patients had been enrolled by September 2017, and we are collecting outcomes on new-onset AF, stroke, and dementia (using the Pfeiffer Score). We hope the registry’s results will contribute with data to support a randomized control trial of full oral anticoagulation vs. placebo in this population.
Is it time to consider oral anticoagulation in patients with IAB and NDAF?
This is an attractive hypothesis [53]. The rationale relies in a series of observations that could lead us to believe that a randomized control trial for elderly patients with aIAB may be suitable:
Recently, implantable devices have demonstrated a lack of a clear temporal relationship between cryptogenic stroke and paroxysmal AF [54–56]. Therefore, AF may not necessarily be the cause of stroke but rather another clinical risk factor.
-
There are many clinical and physiopathological similarities between AF and aIAB:
- a) Both processes increase with age
- b) Both processes present the same anatomical substrate: fibrotic atrial cardiomyopathy (CM) [57]
- c) Fibrotic atrial CM and atrial remodeling induce blood stasis, hypercoagulation, and more atrial fibrosis (Fig. 5)
- d) Finally, both AF and aIAB are risk factor for stroke [58]
Figure 5.
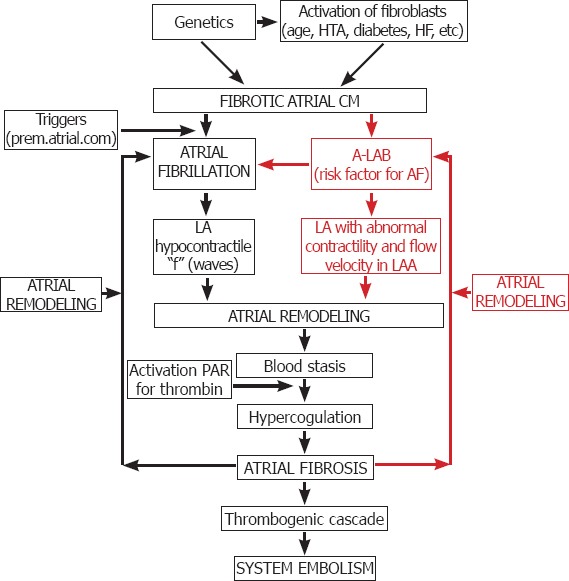
Diagram integrating IAB, atrial fibrosis, and the activation of pro-coagulation states and AF.
CM: Cardiomyopathy; HF: Heart failure; AF: Atrial fibrillation
Before advancing a new recommendation for oral anticoagulation, a randomized controlled clinical trial comparing the efficacy of NOACs in preventing stroke in patients with NDAF and aIAB is needed. If the results of this study are positive, a global strategy for anticoagulation to prevent stroke in patients with NDAF should be considered.
CONCLUSIONS
Bayés syndrome is a clinical electrocardiographic entity that encompasses the presence of IAB in the surface ECG and the detection of clinical or asymptomatic AF. IAB is a strong predictor of AF and stroke in many different clinical scenarios. Its proper identification may help prevent stroke in several patients, if early anticoagulation is considered. This hypothesis should be tested with a randomized control trial.
Footnotes
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
Authorship contributions: Concept – A.B., G.C., A.B.L., M.M.S.; Design – A.B., B.A., A.I.T.; Supervision – R.E., A.B., A.B.L.; Materials – A.B., G.C.; Data collection &/or processing – A.B., B.A.; Analysis and/or interpretation – G.C., A.I.T.; Writing – A.B.; Critical review – A.B., A.B.L.
REFERENCES
- 1.Bayés de Luna A, Cladellas M, Oter R, Torner P, Guindo J, Martí V, et al. Interatrial conduction block and retrograde activation of the left atrium and paroxysmal supraventricular tachyarrhythmia. Eur Heart J. 1988;9:1112–8. doi: 10.1093/oxfordjournals.eurheartj.a062407. [DOI] [PubMed] [Google Scholar]
- 2.Leier CV, Jewell GM, Magorien RD, Wepsic RA, Schaal SF. Interatrial conduction (activation) times. Am J Cardiol. 1979;44:442–6. doi: 10.1016/0002-9149(79)90394-1. [DOI] [PubMed] [Google Scholar]
- 3.Josephson ME, Scharf DL, Kastor JA, Kitchen JG. Atrial endocardial activation in man. Electrode catheter technique of endocardial mapping. Am J Cardiol. 1977;39:972–81. doi: 10.1016/s0002-9149(77)80210-5. [DOI] [PubMed] [Google Scholar]
- 4.Cosio FG, Martin-Penato A, Pastor A, Núñez A, Montero MA, Cantale CP, et al. Atrial activation mapping in sinus rhythm in the clinical electrophysiology laboratory: observations during Bachmann's bundle block. J Cardiovasc Electrophysiol. 2004;15:524–31. doi: 10.1046/j.1540-8167.2004.03403.x. [DOI] [PubMed] [Google Scholar]
- 5.Dolber PC, Spach MS. Structure of canine Bachmann's bundle related to propagation of excitation. Am J Physiol. 1989;257:H1446–57. doi: 10.1152/ajpheart.1989.257.5.H1446. [DOI] [PubMed] [Google Scholar]
- 6.Bayes de Luna A, Platonov P, Cosio FG, Cygankiewicz I, Pastore C, Baranowski R, et al. Interatrial blocks. A separate entity from left atrial enlargement: a consensus report. J Electrocardiol. 2012;45:445–51. doi: 10.1016/j.jelectrocard.2012.06.029. [DOI] [PubMed] [Google Scholar]
- 7.Ariyarajah V, Kranis M, Apiyasawat S, Spodick DH. Potential factors that affect electrocardiographic progression of interatrial block. Ann Noninvasive Electrocardiol. 2007;12:21–6. doi: 10.1111/j.1542-474X.2007.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saremi F, Channual S, Krishnan S, Gurudevan SV, Narula J, Abolhoda A. Bachmann Bundle and its arterial supply: imaging with multidetector CT-implications for interatrial conduction abnormalities and arrhythmias. Radiology. 2008;248:447–57. doi: 10.1148/radiol.2482071908. [DOI] [PubMed] [Google Scholar]
- 9.Enriquez A, Conde D, Redfearn DP, Baranchuk A. Progressive interatrial block and supraventricular arrhythmias. Ann Noninvasive Electrocardiol. 2015;20:394–6. doi: 10.1111/anec.12208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benito E, Bayes de Luna A, Baranchuk A, Mont L. Extensive Atrial Fibrosis Assessed by Late Gadolinium Enhancement Cardiovascular Magnetic Resonance Associated with Advanced Interatrial Block Electrocardiogram Pattern. Europace. 2017;19:377. doi: 10.1093/europace/euw294. [DOI] [PubMed] [Google Scholar]
- 11.Pontecorboli G, Figueras I, Ventura RM, Carlosena A, Benito E, Prat-Gonzales S, et al. Use of delayed-enhancement magnetic resonance imaging for fibrosis detection in the atria: a review. Europace. 2017;19:180–9. doi: 10.1093/europace/euw053. [DOI] [PubMed] [Google Scholar]
- 12.Lacalzada-Almeida J, García-Niebla J, Bayés-de Luna A. Speckle-Tracking Echocardiography and Advanced Interatrial Block. Rev Esp Cardiol. 2017;70:591. doi: 10.1016/j.rec.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 13.Ariyarajah V, Spodick DH. The Bachmann Bundle and interatrial conduction. Cardiol Rev. 2006;14:194–9. doi: 10.1097/01.crd.0000195221.26979.2b. [DOI] [PubMed] [Google Scholar]
- 14.Antz M, Otomo K, Arruda M, Scherlag BJ, Pitha J, Tondo C, et al. Electrical conduction between the right atrium and the left atrium via the musculature of the coronary sinus. Circulation. 1998;98:1790–5. doi: 10.1161/01.cir.98.17.1790. [DOI] [PubMed] [Google Scholar]
- 15.Ho SY, Anderson RH, Sanchez-Quintana D. Atrial structure and fibres: morphologic bases of atrial conduction. Cardiovasc Res. 2002;54:325–36. doi: 10.1016/s0008-6363(02)00226-2. [DOI] [PubMed] [Google Scholar]
- 16.Chauvin M, Shah DC, Haissaguerre M, Marcellin L, Brechenmacher C. The anatomic basis of connections between the coronary sinus musculature and the left atrium in humans. Circulation. 2000;101:647–52. doi: 10.1161/01.cir.101.6.647. [DOI] [PubMed] [Google Scholar]
- 17.Mitrofanova L, Ivanov V, Platonov PG. Anatomy of the inferior interatrial route in humans. Europace. 2005;7(Suppl 2):49–55. doi: 10.1016/j.eupc.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 18.Platonov PG, Mitrofanova LB, Chireikin LV, Olsson SB. Morphology of inter-atrial conduction routes in patients with atrial fibrillation. Europace. 2002;4:183–92. doi: 10.1053/eupc.2002.0221. [DOI] [PubMed] [Google Scholar]
- 19.Holmqvist F, Husser D, Tapanainen JM, Carlson J, Jurkko R, Xia Y, et al. Interatrial conduction can be accurately determined using standard 12-lead electrocardiography: validation of P-wave morphology using electroanatomic mapping in man. Heart Rhythm. 2008;5:413–8. doi: 10.1016/j.hrthm.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 20.Waldo AL, Bush HL, Jr, Gelband H, Zorn GL, Jr, Vitikainen KJ, Hoffman BF. Effects on the canine P wave of discrete lesions in the specialized atrial tracts. Circ Res. 1971;29:452–67. doi: 10.1161/01.res.29.5.452. [DOI] [PubMed] [Google Scholar]
- 21.Pang H, Ronderos R, Perez-Riera AR, Femenia F, Baranchuk A. Reverse atrial electrical remodeling: a systematic review. Cardiol J. 2011;18:625–31. doi: 10.5603/cj.2011.0025. [DOI] [PubMed] [Google Scholar]
- 22.Akoum N, Fernandez G, Wilson B, McGann C, Kholmovski E, Marrouche N. Association of atrial fibrosis quantified using LGE-MRI with atrial appendage thrombus and spontaneous contrast on transesophageal echocardiography in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2013;24:1104–9. doi: 10.1111/jce.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marrouche NF, Wilber D, Hindricks G, Jais P, Akoum N, Marchlinski F, et al. Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA. 2014;311:498–506. doi: 10.1001/jama.2014.3. [DOI] [PubMed] [Google Scholar]
- 24.Guichard JB, Nattel S. Atrial Cardiomyopathy: A Useful Notion in Cardiac Disease Management or a Passing Fad? J Am Coll Cardiol. 2017;70:756–65. doi: 10.1016/j.jacc.2017.06.033. [DOI] [PubMed] [Google Scholar]
- 25.Alexander B, MacHaalany J, Lam B, van Rooy H, Haseeb S, Kuchtaruk A, et al. Comparison of the Extent of Coronary Artery Disease in Patients With Versus Without Interatrial Block and Implications for New-Onset Atrial Fibrillation. Am J Cardiol. 2017;119:1162–5. doi: 10.1016/j.amjcard.2016.12.032. [DOI] [PubMed] [Google Scholar]
- 26.Ariyarajah V, Fernandes J, Apiyasawat S, Spodick DH. Angiographic localization of potential culprit coronary arteries in patients with interatrial block following a positive exercise tolerance test. Am J Cardiol. 2007;99:58–61. doi: 10.1016/j.amjcard.2006.07.065. [DOI] [PubMed] [Google Scholar]
- 27.Saremi F, Abolhoda A, Ashikyan O, Milliken JC, Narula J, Gurudevan SV, et al. Arterial supply to sinuatrial and atrioventricular nodes: imaging with multidetector CT. Radiology. 2008;246:99–107. doi: 10.1148/radiol.2461070030. [DOI] [PubMed] [Google Scholar]
- 28.Baranchuk A, Bayés de Luna A. The P-wave morphology: what does it tell us? Herzschrittmacherther Elektrophysiol. 2015;26:192–9. doi: 10.1007/s00399-015-0385-3. [DOI] [PubMed] [Google Scholar]
- 29.Conde D, Baranchuk A. Interatrial block as anatomical-electrical substrate for supraventricular arrhythmias: Bayés syndrome. [Article in Spanish] Arch Cardiol Mex. 2014;84:32–40. doi: 10.1016/j.acmx.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 30.Conde D, Baranchuk A. Bayes'syndrome: what every cardiologist should know. Rev Argent Cardiol. 2014;82:237–9. [Google Scholar]
- 31.Bacharova L, Wagner GS. The time for naming the Interatrial Block Syndrome: Bayes Syndrome. J Electrocardiol. 2015;48:133–4. doi: 10.1016/j.jelectrocard.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 32.Conde D, Seoane L, Gysel M, Mitrione S, Bayes de Luna A, et al. Bayés'Syndrome: The Association Between Interatrial Block and Supraventricular Arrhythmias. Expert Rev Cardiovasc Ther. 2015;13:541–50. doi: 10.1586/14779072.2015.1037283. [DOI] [PubMed] [Google Scholar]
- 33.Enriquez A, Conde D, Hopman W, Mondragon I, Chiale P, Bayes de Luna A, et al. Advanced interatrial block is associated with recurrence of atrial fibrillation post pharmacological cardioversion. Cardiovas Ther. 2014;32:52–6. doi: 10.1111/1755-5922.12063. [DOI] [PubMed] [Google Scholar]
- 34.Caldwell JC, Koppikar S, Barake W, Redfearn D, Michael K, Simpson C, et al. Advanced interatrial block is associated with atrial fibrillation recurrence after successful pulmonary vein isolation for paroxysmal atrial fibrillation. Journal of Electrocardiology. 2013;46:e1. doi: 10.1007/s10840-013-9851-1. [DOI] [PubMed] [Google Scholar]
- 35.Enriquez A, Sarrias A, Villuendas R, Sadiq Ali F, Conde D, Hopman W, et al. New-onset atrial fibrillation after cavotricuspid isthmus ablation: Identification of advanced interatrial block is key. Europace. 2015;17:1289–93. doi: 10.1093/europace/euu379. [DOI] [PubMed] [Google Scholar]
- 36.Enriquez A, Conde D, Femenia F, Bayes de Luna A, Ribeiro A, Muratore C, et al. Relation of Interatrial Block to New-Onset Atrial Fibrillation in Patients with Chagas Cardiomyopathy and Implantable Cardioverter-Defibrillators. Am J Cardiol. 2014;113:1740–43. doi: 10.1016/j.amjcard.2014.02.036. [DOI] [PubMed] [Google Scholar]
- 37.Alexander B, Rodriguez C, de la Isla LP, Islas F, Quevedo PJ, Nombela-Franco L, et al. The impact of advanced Interatrial block on new-onset atrial fibrillation following TAVR procedure. Int J Cardiol. 2016;223:672–3. doi: 10.1016/j.ijcard.2016.08.083. [DOI] [PubMed] [Google Scholar]
- 38.Sadiq Ali F, Enriquez A, Conde D, Redfearn D, Michael K, Simpson C, et al. Advanced interatrial block is a predictor of new onset atrial fibrillation in patients with severe heart failure and cardiac resynchronization therapy. Ann Noninv Electrophysiol. 2015;20:586–91. doi: 10.1111/anec.12258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Page RL, Wilkinson WE, Clair WK, McCarthy EA, Pritchett ELC. Asymptomatic arrhythmias in patients with symptomatic paroxysmal atrial fibrillation and paroxysmal supraventricular tachycardia. Circulation. 1994;89:224–7. doi: 10.1161/01.cir.89.1.224. [DOI] [PubMed] [Google Scholar]
- 40.Glotzer TV, Hellkamp AS, Zimmerman J, Sweeney MO, Yee R, Marinchak R, et al. Atrial high rate episodes detected by pacemaker diagnostics predict death and stroke: Report of the atrial diagnostics ancillary study of the mode selection trial (MOST) Circulation. 2003;107:1614–9. doi: 10.1161/01.CIR.0000057981.70380.45. [DOI] [PubMed] [Google Scholar]
- 41.Kaufman ES, Israel CW, Nair GM, Armaganijan L, Divakaramenon S, Mairesse GH, et al. ASSERT Steering Committee and Investigators. Positive predictive value of device-detected atrial high-rate episodes at different rates and durations: An analysis from ASSERT. Heart Rhythm. 2012;9:1241–6. doi: 10.1016/j.hrthm.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 42.Tekkesin AI, Çinier G, Cakilli Y, Hayıroğlu Mİ, Alper AT. Interatrial block predicts atrial high rate episodes detected by cardiac implantable electronic devices. J Electrocardiol. 2017;50:234–7. doi: 10.1016/j.jelectrocard.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 43.O'Neal WT, Zhang ZM, Loehr LR, Chen LY, Alonso A, Soliman EZ. Electrocardiographic Advanced interatrial block and atrial fibrillation risk in the general population. Am J Cardiol. 2016;117:1755–9. doi: 10.1016/j.amjcard.2016.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nielsen JB, Kühl JT, Pietersen A, Graff C, Lind B, Struijk JJ, et al. P-wave duration and the risk of atrial fibrillation: Results from the Copenhagen ECG Study. Heart Rhythm. 2015;12:1887–95. doi: 10.1016/j.hrthm.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 45.Vicent L, Martínez-Sellés M. Electrocardiogeriatrics: ECG in advanced age. J Electrocardiol. 2017;50:698–700. doi: 10.1016/j.jelectrocard.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 46.King JB, Azadani PN, Suksaranjit P, Bress AP, Witt DM, Han FT, et al. Left atrial fibrosis and risk of cerebrovascular and cardiovascular events in patients with atrial fibrillation. J Am Coll Cardiol. 2017;70:1311–21. doi: 10.1016/j.jacc.2017.07.758. [DOI] [PubMed] [Google Scholar]
- 47.Dilaveris P, Raftopoulos L, Giannopoulos G, Katinakis S, Maragiannis D, Roussos D, et al. Prevalence of interatrial block in healthy school-aged children: definition by P-wave duration or morphological analysis. Ann Noninvasive Electrocardiol. 2010;15:17–25. doi: 10.1111/j.1542-474X.2009.00335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martínez-Sellés M. Prevalence and incidence of interatrial block in global population and in different clinical situations. J Geriatr Cardiol. 2017;14:158–60. doi: 10.11909/j.issn.1671-5411.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martínez-Sellés M, Massó-van Roessel A, Álvarez-García J, García de la Villa B, Cruz-Jentoft AJ, Vidán MT, et al. Investigators of the Cardiac and Clinical Characterization of Centenarians (4C) registry. Interatrial block and atrial arrhythmias in centenarians: Prevalence, associations, and clinical implications. Heart Rhythm. 2016;13:645–51. doi: 10.1016/j.hrthm.2015.10.034. [DOI] [PubMed] [Google Scholar]
- 50.O'Neal WT, Kamel H, Zhang ZM, Chen LY, Alonso A, Soliman EZ. Advanced interatrial block and ischemic stroke: The Atherosclerosis Risk in Communities Study. Neurology. 2016;87:352–6. doi: 10.1212/WNL.0000000000002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu JT, Wang SL, Chu YJ, Long DY, Dong JZ, Fan XW, et al. CHADS2 and CHA2DS2-VASc Scores Predict the Risk of Ischemic Stroke Outcome in Patients with Interatrial Block without Atrial Fibrillation. J Atheroscler Thromb. 2017;24:176–84. doi: 10.5551/jat.34900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martinez-Selles M, Baranchuk A, Elousa R, de Luna AB. Rationale and Design of the BAYES (interatrial Block And Yearly EventS) Registry. Clin Cardiol. 2017;40:196–9. doi: 10.1002/clc.22647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bayés de Luna A, Martínez-Sellés M, Bayés-Genís A, Elosua R, Baranchuk A. Surface ECG interatrial block-guided treatment for stroke prevention: rationale for an attractive hypothesis. BMC Cardiovascular Disorders. 2017;17:211. doi: 10.1186/s12872-017-0650-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Glotzer TV, Daoud EG, Wyse DG, Singer DE, Ezekowitz Hilker C, et al. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythmia Electrophysiol. 2009;2:74–80. doi: 10.1161/CIRCEP.109.849638. [DOI] [PubMed] [Google Scholar]
- 55.Hohnloser SH, Capucci A, Fain E, Gold MR, van Gelder IC, Healey J, et al. ASSERT Investigators and Committees. Asymptomatic atrial fibrillation and stroke evaluation in pacemaker patients and the atrial fibrillation reduction atrial pacing Trial (ASSERT) Am Heart J. 2006;152:442–7. doi: 10.1016/j.ahj.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 56.Martin DT, Bersohn MM, Waldo AL, Wathen MS, Choucair WK, Lip GY, et al. IMPACT Investigators. Randomized trial of atrial arrhythmia monitoring to guide anticoagulation in patients with implanted defibrillator and cardiac resynchronization devices. Eur Heart J. 2015;36:1660–8. doi: 10.1093/eurheartj/ehv115. [DOI] [PubMed] [Google Scholar]
- 57.Hirsh BJ, Copeland-Halperin RS, Halperin JL. Fibrotic Atrial Cardiomyopathy, Atrial Fibrillation, and thromboembolism: Mechanistic Links and Clinical Inferences. J Am Coll Cardiol. 2015;65:2239–51. doi: 10.1016/j.jacc.2015.03.557. [DOI] [PubMed] [Google Scholar]
- 58.Martínez-Sellés M, Fernandez Lozano I, Baranchuk A, Bayés-Genís A, Bayés de Luna A. Should we anticoagulate patients at high risk of atrial fibrillation? Rev Esp Card. 2016;69:374–6. doi: 10.1016/j.rec.2016.01.008. [DOI] [PubMed] [Google Scholar]