Abstract
The objective of this study was to understand outcomes of patients treated with ALK inhibitors, especially when ALK inhibitors are followed by other ALK inhibitors. A systematic literature review was conducted in PubMed, Embase, and Cochrane through July 17, 2017. Conference abstracts (three meetings in past 2 years) also were searched. Of 504 unique publications, 80 met inclusion criteria (47 clinical trials, 33 observational studies). Observational studies have the potential to provide information for ALK inhibitors used sequentially. Ten observational studies reported median overall survival of crizotinib-led sequences ranging from 30.3 to 63.75 months from initiation of crizotinib; 49.4–89.6 months from metastatic non-small-cell lung cancer diagnosis; and 15.5–22.0 months from initiation of the second-generation ALK inhibitor after initial crizotinib. Sequencing of ALK inhibitors may benefit patients progressing on initial ALK inhibitors.
Keywords: ALK, non-small-cell lung cancer, NSCLC, carcinoma, non-small-cell lung
Introduction
ALK is a member of the insulin receptor superfamily,1 and oncogenic EML4-ALK fusion variants represent molecular targets in non-small-cell lung cancer (NSCLC). ALK fusions have been identified in both squamous and adenocarcinoma histologic subtypes, with a higher frequency observed in adenocarcinoma.2,3 Overall, ALK fusions occur in 3%–5% of patients with metastatic NSCLC.4
Prior to 2011, when the first ALK tyrosine kinase inhibitor was approved, the standard of care for patients with ALK-positive NSCLC was chemotherapy, and outcomes were poor, with median overall survival (OS) of ~12 months.5,6 Crizotinib was approved by the United States Food and Drug Administration (FDA) under accelerated approval in 2011 and was the first ALK inhibitor approved for patients with ALK-positive advanced NSCLC.7
Although patients with ALK-positive advanced NSCLC initially respond to ALK inhibitors, resistance eventually often develops in these patients.8 One of the mechanisms of acquired resistance is a mutation in the kinase domain of ALK, although other resistance mechanisms have also been reported, such as activation of alternative pathways (EGFR, KIT, and IGF-IR), ALK amplification, and epithelial–mesenchymal transition.9 In some patients, the mechanism of acquired resistance remains unknown.9
To address resistance, additional ALK inhibitors have been introduced. Ceritinib was approved by the FDA in April 201410 for the treatment of patients with ALK-positive metastatic NSCLC who have progressed on or are intolerant to crizotinib, and in May 2017 it received approval for expanded use to include first-line treatment.11 Subsequently, alectinib received FDA approval in December 2015 for the treatment of patients with ALK-positive metastatic NSCLC who have progressed on or are intolerant to crizotinib12,13 and in November 2017 for first-line treatment.14 Brigatinib received FDA approval in April 2017 for the treatment of patients with ALK-positive metastatic NSCLC who have progressed on or are intolerant to crizotinib.15
The current standard of care for treating ALK-positive NSCLC is the use of ALK inhibitors. Multiple available ALK inhibitors allow the possibility of sequencing these agents to extend patient benefit and improve outcomes. The available ALK inhibitors have different potencies, differential penetration into the central nervous system, unique safety profiles, and different “spectrums” of activity against particular acquired resistance mutations.
Outcomes of ALK inhibitors are well documented in controlled clinical trials; however, less is known about the outcomes associated with sequencing. We hypothesized that sequencing of ALK inhibitors will benefit survival outcomes of patients. Herein, we report the first systematic literature review with an aim to understand the outcomes of patients treated with ALK inhibitors, especially when an ALK inhibitor is followed by another ALK inhibitor.
Material and methods
Electronic literature searches were conducted in PubMed, Embase, and the Cochrane Library databases through July 17, 2017 for real-world and clinical trial evidence for drug sequencing/treatment patterns and the related outcomes associated with the use of ALK inhibitors. Additional studies not published in the peer-reviewed literature were identified by searching online conference abstracts of three professional societies for the previous 2 calendar years: the American Society of Clinical Oncology (2016 and 2017), the European Society of Medical Oncology (2015 and 2016), and the International Association for the Study of Lung Cancer World Conference on Lung Cancer (2015 and 2016). The electronic database searches were also supplemented by a review of the bibliographic reference lists of relevant literature review articles.
The search terms for the medical library databases included Medical Subject Heading, Emtree, and free-text terms, including disease terms (carcinoma, non-small-cell lung; non-small-cell lung cancer; non-small-cell lung carcinoma; non-small-cell lung cancer), terms to identify drug sequencing/treatment patterns (practice pattern, prescribing pattern, treatment pattern), terms to identify the agents of interest (crizotinib, Xalkori, PF-02341066, ceritinib, Zykadia, LDK378, alectinib, Alecensa, CH5424802, brigatinib, AP26113, ALK inhibitor), various terms to identify study types and outcomes of interest, and terms to identify observational studies and clinical trials (Table S1). The search was limited to English-language studies of humans and had no date limit.
Two independent reviewers screened the titles and abstracts according to predefined inclusion and exclusion criteria (Table S2). Full-text articles of selected records were obtained, and the two independent reviewers further screened each article according to the same predefined inclusion and exclusion criteria. Data extraction by a single researcher included study design, patient characteristics, line/sequence of therapy, and outcomes, including treatment duration, response rates, median OS, and median progression-free survival (PFS). A separate researcher conducted quality control of data extraction.
Results
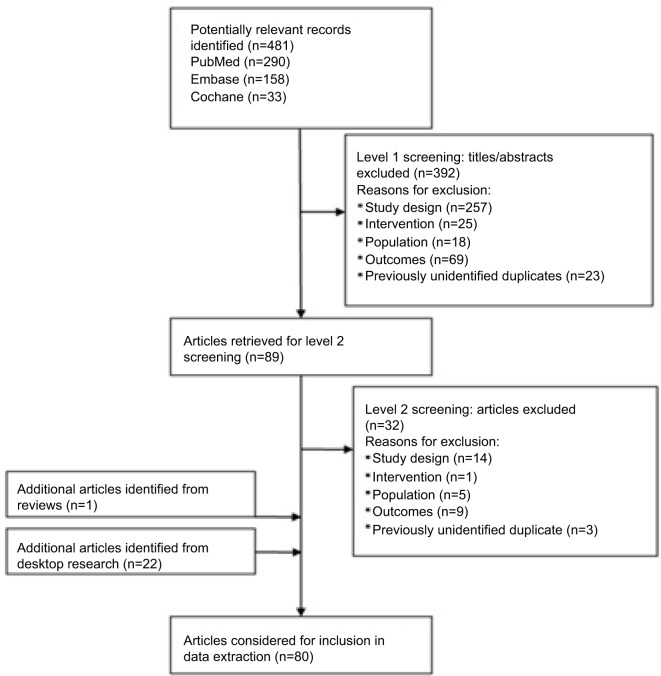
The electronic literature database search identified 481 unique records. One additional article was identified following a review of the bibliographic reference lists of relevant literature review articles. Twenty-two additional abstracts were identified from the search of professional societies and associated conferences. Of the 504 unique articles/abstracts identified, 80 publications met the inclusion criteria (Figure 1). Of the 80 publications, 47 were from clinical trials and 33 were from observational studies. Studies were heterogeneous regarding study design, data source, sample size, timeframe of observation, and outcomes collected, including PFS and OS. A detailed overview of the PFS and OS outcomes in the observational studies of ALK inhibitors used after an initial ALK inhibitor is shown in Tables 1 and 2, respectively. The online supplement provides a list of the 80 publications included (Table S3).
Figure 1.
PRISMA diagram.
Table 1.
Results of observational studies of an ALK inhibitor after initial ALK inhibitor – median PFS
| Reference | Median PFS of first ALK inhibitor, months | Median PFS of second ALK inhibitor, months | Median combined PFS, monthsa |
|---|---|---|---|
| Ceritinib after initial crizotinib | |||
| Bendaly et al81 | NR | NR | NR |
| Bendaly et al80 | NR | 12.9 | NR |
| Gainor et al82 | 8.2 | 7.8 | 17.4 17.0 for patients with no interval between CRZ and CERT |
| Kayaniyil et al48 | NR | 9.6 for patients who received CERT immediately after CRZ 4.6 for patients who received CERT at any time after CRZ | NR |
| Alectinib after initial crizotinib | |||
| Ito et al44 | 7.0 | 24.7b | NR |
| Watanabe et al84 | 6.1 | 15.2c | 18.2 |
| Asao et al46 | 10.7 | 16.6d | 35.2 |
| Yoshida et al57 | NR | NR | NR |
| Any second-generation ALK inhibitor after crizotinib | |||
| Chiari et al45 | 10 | 7 | 17 |
| Roeper et al83 | NR | NR | NR |
| Nosaki et al47 | NR | NR | NR |
| Cadranel et al50 | NR | NR | NR |
| Duruisseaux et al54 | NR | NR | NR |
| Second-generation ALK inhibitor after second generation | |||
| Nosaki et al47 | NR | NR | NR |
Notes:
Summarized as reported in the publication, ie, the authors of this review did not calculate the results.
Retrospective study of 28 patients in whom 15 received alectinib alone and 13 received alectinib after initial crizotinib.
Retrospective study of 11 patients; all patients received crizotinib followed by alectinib but 6 of the 11 also received ≥1 cytotoxic chemotherapy regimen prior to crizotinib. Range of median PFS on alectinib was 1.0–28.3.
Retrospective study of 13 patients who received crizotinib followed by alectinib.
Abbreviations: CERT, ceritinib; CRZ, crizotinib; NR, not reported; PFS, progression-free survival.
Table 2.
Results of observational studies of an ALK inhibitor after initial ALK inhibitor – median OS
| Reference | Median OS from initiation of second ALK inhibitor, months | Median OS from initiation of first ALK inhibitor (ie, OS of ALK sequence), months | Median OS from diagnosis of metastatic disease, months |
|---|---|---|---|
| Ceritinib after initial crizotinib | |||
| Bendaly et al81 | NR | NR | NR |
| Bendaly et al80 | 15.5 | NR | NR |
| Gainor et al82 | NR | 30.3a | 49.4 |
| Kayaniyil et al48 | 20.4 | NR | 51.0 |
| Alectinib after initial crizotinib | |||
| Ito et al44 | NR | Not reachedb | NR |
| Watanabe et al84 | NR | 48.6 | 51.1 |
| Asao et al46 | NR | NR | NR |
| Yoshida et al57 | NR | NR | NR |
| Any second-generation ALK inhibitor after crizotinib | |||
| Chiari et al45 | 22 | 40 | NR |
| Roeper et al83 | NR | Not reachedc | NR |
| Nosaki et al47 | NR | 63.75 | NR |
| Cadranel et al50 | NR | Not reachedd | NR |
| Duruisseaux et al54 | NR | Not reachede | 89.6 |
| Second-generation ALK inhibitor after second generation | |||
| Nosaki et al47 | NR | Not reachedf | NR |
Notes:
From initiation of crizotinib in subset of patients previously treated with chemotherapy.
Median duration of follow-up: 21.3 months.
Median duration of follow-up: not reported.
Median duration of follow-up: 21.4 months.
Median duration of follow-up: 44.4 months.
Median duration of follow-up: not reported.
Abbreviations: NR, not reported; OS, overall survival.
Evidence base of first use of an ALK inhibitor with or without prior chemotherapy (ALK inhibitor naïve)
A total of 45 publications assessed outcomes of first use of an ALK inhibitor with or without prior chemotherapy in patients who were ALK inhibitor naïve. Of the 45 publications, 27 were from clinical trials16–42 and 18 were from observational studies.43–60 In clinical trials, median PFS ranged from 7.7 months30 to 25.9 months,19 median OS ranged from 20.3 months30 to 39.1 months,20 and objective response rate (ORR) ranged from 46%27 to 100%.36 In the observational studies, median PFS ranged from ~7 months (reported as 28 weeks)51 to 17.7 months (from diagnosis of advanced NSCLC)58 and median OS ranged from 11.2 months54 to ~104 months (reported as 416 weeks);47 note that data from Nosaki et al47 were presented in a conference abstract and thus not all data may have been included.
Evidence base of use of second or subsequent ALK inhibitor (ALK inhibitor followed by another ALK inhibitor)
A total of 38 publications assessed outcomes of use of an ALK inhibitor after an initial ALK inhibitor. Of the 38 publications, 25 were from clinical trials35–37,40–42,61–79 and 13 were from observational studies.44–48,50,54,57,80–84 All 38 publications reported on use of a second-generation ALK inhibitor after initial crizotinib therapy; one publication of an observational study also included a population that used a second-generation ALK inhibitor after an initial second-generation ALK inhibitor (ceritinib after initial alectinib),47 and one publication of an observational study mentioned two patients who received crizotinib after alectinib.84 The efficacy data reported in clinical trials are from initiation of the second-generation ALK inhibitor only; as noted, all sequences were of a second-generation ALK inhibitor after initial crizotinib therapy. In the 25 publications from clinical trials, median PFS from initiation of the second-generation ALK inhibitor ranged from 5.4 months77 to 15.6 months,70 median OS ranged from 14.9 months75 to 26.0 months,61,65 and ORR ranged from 33.0%42 to 80.0%;36 estimated 12-month survival rates ranged from 63.8%75 to 83.0%.36 Only seven clinical trial publications reported treatment duration of the second-generation ALK inhibitor, which ranged from 8.1 weeks76 to 38.6 weeks.37
Of the 13 publications from observational studies, there was a heterogeneous makeup in study design, population, and the method in which results were reported. Combined PFS of a crizotinib-led sequence was reported in four publications45,46,82,84 and ranged from 17.0 months45,82 to 35.2 months.46 In general, median combined PFS was defined as the sum of PFS of the two ALK inhibitors and did not include the interval from discontinuation of crizotinib to initiation of the second-generation ALK inhibitor or postprogression use of crizotinib. In some instances, patients may have been allowed to receive chemotherapy in the interval between use of the two ALK inhibitors. Five observational study publications44–46,82,84 of crizotinib-led sequences reported PFS of crizotinib ranging from 6.1 months84 to 10.7 months.46 Seven publications44–46,48,80,82,84 reported PFS from initiation of the second-generation ALK inhibitor ranging from 4.6 months48 to 24.7 months.44
Ten publications from observational studies44,45,47,48, 50,54,80,82–84 of crizotinib-led sequences reported median OS. Of these ten publications, four reported median OS for the sequence as not reached.44,50,54,83 Median follow-up for the sequence was reported as follows: not reported,83 21.3 months,44 21.4 months,50 and 44.4 months.54 Four publications45,47,82,84 reported median OS from initiation of crizotinib (ie, for the full ALK sequence) ranging from 30.3 months82 to ~64 months (reported as 255 weeks).47 The 64 months reported by Nosaki et al47 was in patients receiving alectinib or ceritinib after initial crizotinib; however, this publication was a conference abstract and thus limited data are reported. Four publications48,54,82,84 reported median OS from diagnosis of metastatic disease ranging from 49.4 months82 to 89.6 months.54 The 89.6 months reported by Duruisseaux et al54 were in 84 patients who received a second-generation ALK inhibitor at some point after progressing on initial crizotinib. Three publications45,48,80 reported median OS of the second-generation ALK inhibitor after crizotinib ranging from 15.5 months80 to 22.0 months.45 One publication of a second-generation ALK inhibitor after an initial second-generation ALK inhibitor (ceritinib after initial alectinib) reported median OS for the sequence as not reached; median duration of follow-up was not reported.47
Survival rates were reported in five publications from observational studies.46,48,50,54,80 Twelve-month survival rates in crizotinib-led sequences were reported as 59.9%50 and 92.9%54 from first dose of crizotinib.
Specific sequences
Ceritinib after initial crizotinib
When reviewing specific sequences, 12 publications described results of ceritinib after initial crizotinib; 8 were from clinical trials,37,40–42,75–77,79 and 4 were from observational studies.48,80–82 The clinical trials reported results for only the ceritinib portion of the sequence. Median PFS ranged from 5.4 months77 to 6.9 months,37,41 median OS ranged from 14.9 months75 to 20.0 months,79 and ORR ranged from 33% to 63%.42
In the four observational study publications, combined median PFS was reported in only one publication and was reported as 17.4 months.82 Combined PFS for sequential treatment with crizotinib and ceritinib did not include postprogression use of crizotinib or the interval between crizotinib discontinuation and start of ceritinib, in which patients could have received cytotoxic chemotherapy.82 In patients in which crizotinib was discontinued and ceritinib immediately initiated (ie, no intervening treatment), median combined PFS was 17.0 months.82 Median PFS while patients were on ceritinib ranged from 7.8 months82 to 12.9 months.80 Only one study reported median PFS while patients were on crizotinib, which was reported as 8.2 months.82
Finally, median OS was reported as 30.3 months from initiation of crizotinib,82 15.5 months80 and 20.4 months48 from initiation of ceritinib, and 49.4 months82 and 51.0 months48 from diagnosis of metastatic disease.
Alectinib after initial crizotinib
A total of 15 publications described results of alectinib after initial crizotinib; 11 were from clinical trials,35,61–69,78 and 4 were from observational studies.44,46,57,84 The clinical trials reported results for just the alectinib portion of the sequence. Median PFS ranged from 8.0 months64 to 13.9 months,78 median OS was reported as 22.7 months64 and 26.0 months,61,65 and ORR ranged from 44.0%62 to 72.2%.35 The estimated 12-month survival rate was 71.0%.63
Of the four observational studies, two publications reported combined median PFS as 18.2 months84 and 35.2 months.46 Asao et al46 defined combined PFS as the sum of the PFS of the two ALK inhibitors without the interval between the ALK inhibitors, ie, treatment duration with cytotoxic chemotherapy between the two ALK inhibitors was excluded. In Watanabe et al,84 combined PFS did not include postprogression use of crizotinib or the interval from discontinuation of crizotinib to initiation of alectinib. Median PFS from initiation of alectinib ranged from 15.2 months84 to 24.7 months.44 Median PFS while patients received crizotinib ranged from 6.1 months84 to 10 months.45
Median OS was reported to be not reached44 (median follow-up of 21.3 months) and 48.6 months84 from initiation of crizotinib and 51.1 months84 from diagnosis of metastatic disease. Estimated 12-month survival was reported to be 38.6% in patients on crizotinib and 60.0% in those on ceritinib;46 the estimated 5-year survival for the sequence was 77.8%.46
Brigatinib after initial crizotinib
Six publications described results of brigatinib after initial crizotinib, all of them clinical trials.36,70–74 There were no observational studies found in the literature that assessed brigatinib after initial crizotinib. Median PFS from initiation of brigatinib ranged from 8.8 months70 to 15.6 months,70 and ORR ranged from 45%70,73 to 80%.36 Median OS was not reported in any of the six publications. Estimated 12-month survival rates ranged from 71%73 to 83%.36
Any second-generation ALK inhibitor after initial crizotinib
Five publications from observational studies described outcomes of a second-generation ALK inhibitor after initial crizotinib.45,47,50,54,83 In these publications, either the second-generation ALK inhibitor was not specified or the results were combined for more than one ALK inhibitor. All five publications were from observational studies. Median PFS was reported in only one publication and was 17 months combined for the sequence, 10 months for crizotinib, and 7 months from initiation of the second ALK inhibitor (alectinib or ceritinib).45 Median OS was 40.0 months45 and ~64 months47 for the sequence, 22 months from initiation of the second ALK inhibitor,45 and 89.6 months from diagnosis of metastatic disease.54 Two publications reported median OS as not reached for the specific sequence being studied54,83 (median follow-up not reported in Roeper et al83 and 44.4 months in Duruisseaux et al54). Estimated 12-month survival was reported to be 59.9% from the start of a sequence of ceritinib, alectinib, or brigatinib after initial crizotinib50 and 92.9% from the start of a sequence of ceritinib or alectinib after initial crizotinib.54
Ceritinib after initial alectinib
Nosaki et al47 reported median OS as not being reached in patients who received ceritinib after initial alectinib; median follow-up time was not reported. Note these data were reported from a conference abstract with limited information.
Discussion
In this systematic literature review, we aimed to understand the outcomes of patients treated with ALK inhibitors, especially when an ALK inhibitor is followed by another ALK inhibitor.
The identified clinical trials of patients who were ALK inhibitor naïve reported median PFS ranging from 7.7 to 25.9 months and median OS ranging from 20.3 to 39.1 months. Observational studies reported median PFS ranging from 7 to 17.7 months and median OS ranging from 11.2 to 104 months.
In clinical trials of a second-generation ALK inhibitor used after initial crizotinib, median PFS from initiation of the second-generation ALK inhibitor ranged from 5.4 to 15.6 months and median OS ranged from 14.9 to 26.0 months. In observational studies of an ALK inhibitor followed by another ALK inhibitor, median PFS ranged from 4.6 to 35.2 months and median OS ranged from 15.5 to 89.6 months.
In sequencing observational studies of an ALK inhibitor used after an initial ALK inhibitor, median OS from initiation of the first ALK inhibitor, ie, for the ALK sequence, has varied and has been reported as 30.3 months,82 40 months,45 48.6 months,84 and ~64 months.47 Median OS has been consistently reported to be ~50 months from time of diagnosis of metastatic disease in several observational studies of ALK inhibitors used in sequence,48,82,84 indicating that sequential use of ALK inhibitors may be clinically beneficial to patients. There are currently several examples of median OS being reported as “not reached” in studies of the full sequence of an ALK inhibitor after an initial ALK inhibitor. This is not surprising given that only relatively recently multiple ALK inhibitors became available. As sequential ALK inhibitors are utilized and survival data mature, we expect that additional outcomes data will become available to help inform treatment decisions for improved outcomes of patients with ALK-positive NSCLC. Important to note is that lorlatinib, a third generation ALK inhibitor, recently became available in the USA. Lorlatinib is indicated for the treatment of patients with ALK-positive metastatic NSCLC whose disease has progressed on crizotinib and at least one other ALK inhibitor; or alectinib or ceritinib as the first ALK inhibitor therapy for metastatic disease,85 which further supports the sequencing of ALK inhibitors. Approval was based on a phase 2 study in which lorlatinib demonstrated substantial overall and intracranial response both in treatment-naive patients with ALK-positive NSCLC, and in those who had progressed on crizotinib, second-generation ALK inhibitors, or after up to three previous ALK inhibitors.86
The evidence base is broader and more mature for crizotinib-led sequences than for second-generation-led sequences. The amount of research of crizotinib-led sequences is not unexpected given that crizotinib was the first ALK inhibitor on the market. Additional research is needed to understand the survival outcomes of second-generation ALK inhibitors as initial therapy.
This study adds to the current literature in that it is the first systematic review of sequencing of ALK inhibitors. A robust methodology was used that included a study protocol, multiple broad electronic databases searching for both clinical trials and observational studies, and that did not limit by date. In addition, two reviewers independently screened all titles, abstracts, and full-text articles using predefined inclusion and exclusion criteria. This robust methodology enables the reproducibility of the review.
It is important to note in the interpretation of retrospective studies reporting median OS or “combined” PFS for a sequence that immortal time bias must be considered. In studies of sequential therapy conducted retrospectively, patients who do not survive to receive the second treatment are not included in the analysis. Patients who received both ALK inhibitors are selected for having lived long enough and for having stable enough disease (in some instances related in part to chemotherapy after the first ALK inhibitor) that they were able to receive both ALK inhibitors in sequence. Therefore, the observed value for combined PFS and OS reported in these studies is likely to be biased upward from what may be expected at the outset for patients treated according to such a sequential treatment plan; however, as no prospectively designed studies have evaluated this question to date, retrospective studies are currently the best available evidence.
Another important consideration in interpreting the findings from this systematic review is that the cutoff date of July 17, 2017 did not allow for inclusion of the final OS data from PROFILE 1014, which is the first long-term study with mature OS data for an ALK-positive NSCLC population. Results showed that median OS was not reached for crizotinib and was 47.5 months for chemotherapy (median follow-up was ~46 months in each treatment arm).87 Most patients (84.2%) receiving chemotherapy crossed over to crizotinib; therefore, a crossover-adjusted analysis was conducted demonstrating OS in the crizotinib arm to be significantly longer than the chemotherapy arm (HR, 0.346; 95% CI, 0.081–0.718).87 At 4 years, 56.6% of crizotinib patients and 49.1% of chemotherapy patients were still alive.87 Interestingly, these results were consistent with the OS data of around 50 months from observational studies of ALK inhibitors that we identified in this systematic literature review.
Owing to the data immaturity and currently available trial designs, it is not currently possible to determine which sequence confers the best long-term outcomes.
Conclusion
Subsequent use of ALK inhibitors may clinically benefit patients progressing on an initial ALK inhibitor. Crizotinib-led sequences have a broader evidence base and more mature clinical outcomes than second-generation-led sequences. No evidence was found directly comparing different ALK inhibitor sequences. Further research is warranted to directly compare ALK inhibitor sequences and to understand the outcomes of second-generation ALK inhibitors as initial ALK inhibitor therapy.
Supplementary Materials
Acknowledgments
This work was funded by Pfizer, Inc. The abstract of this paper was presented at the International Society for Phar-macoeconomics and Outcomes Research (ISPOR) 23rd Annual International Meeting; May 19–23, 2018, as a poster presentation with interim findings. The poster’s abstract is published online at https://tools.ispor.org/ScientificPresen-tationsDatabase/Presentation/81967?pdfid=54840. In addition, the ISPOR abstract was published in Value in Health 2018;21(S1):S49–S50.
Footnotes
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Elizabeth T Masters, Marc Chioda, Robin Wiltshire, and Knut Martin Torgersen are employees of Pfizer, Inc. RTI Health Solutions received funding from Pfizer to conduct this research and for manuscript development; Stephanie M Barrows, Kelly Wright, Catherine Copley-Merriman, and James A Kaye are employees of RTI Health Solutions. The authors report no other conflicts of interest in this work.
References
- 1.Morris SW, Naeve C, Mathew P, et al. ALK, the chromosome 2 gene locus altered by the t(2;5) in non-Hodgkin’s lymphoma, encodes a novel neural receptor tyrosine kinase that is highly related to leukocyte tyrosine kinase (LTK) Oncogene. 1997;14(18):2175–2188. doi: 10.1038/sj.onc.1201062. [DOI] [PubMed] [Google Scholar]
- 2.Inamura K, Takeuchi K, Togashi Y, et al. EML4-ALK lung cancers are characterized by rare other mutations, a TTF-1 cell lineage, an acinar histology, and young onset. Mod Pathol. 2009;22(4):508–515. doi: 10.1038/modpathol.2009.2. [DOI] [PubMed] [Google Scholar]
- 3.Wong DW, Leung EL, So KK, et al. The EML4-ALK fusion gene is involved in various histologic types of lung cancers from nonsmokers with wild-type EGFR and KRAS. Cancer. 2009;115(8):1723–1733. doi: 10.1002/cncr.24181. [DOI] [PubMed] [Google Scholar]
- 4.Gerber DE, Minna JD. ALK inhibition for non-small cell lung cancer: from discovery to therapy in record time. Cancer Cell. 2010;18(6):548–551. doi: 10.1016/j.ccr.2010.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee JK, Park HS, Kim DW, et al. Comparative analyses of overall survival in patients with anaplastic lymphoma kinase-positive and matched wild-type advanced nonsmall cell lung cancer. Cancer. 2012;118(14):3579–3586. doi: 10.1002/cncr.26668. [DOI] [PubMed] [Google Scholar]
- 6.Shaw AT, Yeap BY, Solomon BJ, et al. Impact of crizotinib on survival in patients with advanced, ALK-positive NSCLC compared with Historical controls. J Clin Oncol. 2011;29(15_suppl):7507. [Google Scholar]
- 7.FDA . NDA 202570 Accelerated Approval. US Food and Drug Administration; 2011. [Accessed November 16, 2017]. Available from: https://www.accessdata.fda.gov/drug-satfda_docs/appletter/2011/202570s000ltr.pdf. [Google Scholar]
- 8.Katayama R, Shaw AT, Khan TM, et al. Mechanisms of acquired crizotinib resistance in ALK-rearranged lung cancers. Sci Transl Med. 2012;4(120):120ra17. doi: 10.1126/scitranslmed.3003316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liao BC, Lin CC, Shih JY, Yang JC. Treating patients with ALK-positive non-small cell lung cancer: latest evidence and management strategy. Ther Adv Med Oncol. 2015;7(5):274–290. doi: 10.1177/1758834015590593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.FDA . NDA 205755 Approval Letter. US Food and Drug Administration; 2014. [Accessed December 22, 2017]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2014/205755Orig1s000ltr.pdf. [Google Scholar]
- 11.FDA . NDA 205755/S-09 Supplement Approval Fulfillment of Postmarketing Requirement. US Food and Drug Administration; 2017. [Accessed March 7, 2018]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2017/205755Orig1s009ltr.pdf. [Google Scholar]
- 12.CDER . Approval Package for Application Number 208434Orig1s000. Center for Drug Evaluation and Research; 2015. [Accessed March 7, 2018]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/208434Orig1s000Approv.pdf. [Google Scholar]
- 13.EMA . Alecensa (Alectinib) Authorization Details. European Medicines Agency; 2017. [Accessed March 7, 2018]. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/004164/human_med_002068.jsp&mid=WC0b01ac058001d124. [Google Scholar]
- 14.FDA . NDA 208434/S-03 Supplement Approval Fulfillment of Postmarketing Requirement. US Food and Drug Administration; 2017. [Accessed March 7, 2018]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2017/208434Orig1s003ltr.pdf. [Google Scholar]
- 15.Brigatinib Prescribing Information (United States) Cambridge, MA: ARIAD Pharmaceuticals, Inc.; Apr, 2017. [Accessed December 19, 2017]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/208772lbl.pdf. [Google Scholar]
- 16.Tamura T, Kiura K, Seto T, et al. Three-year follow-up of an alectinib phase I/II study in ALK-positive non-small-cell lung cancer: AF-001JP. J Clin Oncol. 2017;35(14):1515–1521. doi: 10.1200/JCO.2016.70.5749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hida T, Nokihara H, Kondo M, et al. Alectinib versus crizotinib in patients with ALK-positive non-small-cell lung cancer (J-ALEX): an open-label, randomised phase 3 trial. Lancet. 2017;390(10089):29–39. doi: 10.1016/S0140-6736(17)30565-2. [DOI] [PubMed] [Google Scholar]
- 18.Peters S, Camidge DR, Shaw AT, et al. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N Engl J Med. 2017;377(9):829–838. doi: 10.1056/NEJMoa1704795. [DOI] [PubMed] [Google Scholar]
- 19.Takiguchi Y, Hida T, Nokihara H. Updated efficacy and safety of the J-ALEX study comparing alectinib (ALC) with crizotinib (CRZ) in ALK-inhibitor naïve ALK fusion positive non-small cell lung cancer (ALK+ NSCLC). Paper presented at: Annual Meeting of the American Society of Clinical Oncology; 2017; Chicago, IL. [Google Scholar]
- 20.Tan D, Felip E, Chow LQ. Ceritinib as first-line therapy in patients with ALK-rearranged non-small cell lung cancer: ASCEND-1 subgroup analysis. 17th World Conference on Lung Cancer; Vienna, Austria. 2016. [Google Scholar]
- 21.Felip E, Orlov S, Park K, et al. Phase 2 study of ceritinib in ALKi-naïve patients (PTS) with ALK-rearranged (ALK+) non-small cell lung cancer (NSCLC): whole body responses in the overall Pt group and in PTS with baseline brain metastases (BM) Ann Oncol. 2016;27(suppl_6):12080. [Google Scholar]
- 22.de Castro G, Tan DS-W, Crinò L, et al. PL03.07: first-line ceritinib versus chemotherapy in patients with ALK-rearranged (ALK+) NSCLC: a randomized, phase 3 study (ASCEND-4) J Thorac Oncol. 2017;12(1):S7. [Google Scholar]
- 23.Soria JC, Tan DSW, Chiari R, et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet. 2017;389(10072):917–929. doi: 10.1016/S0140-6736(17)30123-X. [DOI] [PubMed] [Google Scholar]
- 24.Camidge DR, Bang YJ, Kwak EL, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol. 2012;13(10):1011–1019. doi: 10.1016/S1470-2045(12)70344-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim DW, Ahn MJ, Shi Y. Results of a global phase II study with crizotinib in advanced ALK-positive non-small cell lung cancer (NSCLC) J Clin Oncol. 2012;30(Suppl) Abstract 7533. [Google Scholar]
- 26.Shaw AT, Janne PA, Besse B, et al. Crizotinib vs chemotherapy in ALK + advanced non-small cell lung cancer (NSCLC): final survival results from PROFILE 1007. J Clin Oncol. 2016;34(15_suppl):9066. [Google Scholar]
- 27.Costa DB, Shaw AT, Ou SH, et al. Clinical experience with crizotinib in patients with advanced ALK-rearranged non-small-cell lung cancer and brain metastases. J Clin Oncol. 2015;33(17):1881–1888. doi: 10.1200/JCO.2014.59.0539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nishio M, Kim DW, Wu YL, et al. Crizotinib versus chemotherapy in Asian patients with ALK-positive advanced non-small cell lung cancer. Cancer Res Treat. 2018;50(3):691–700. doi: 10.4143/crt.2017.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lei YY, Yang JJ, Zhong WZ, et al. Clinical efficacy of crizotinib in Chinese patients with ALK-positive non-small-cell lung cancer with brain metastases. J Thorac Dis. 2015;7(7):1181–1188. doi: 10.3978/j.issn.2072-1439.2015.06.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shaw AT, Kim DW, Nakagawa K, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368(25):2385–2394. doi: 10.1056/NEJMoa1214886. [DOI] [PubMed] [Google Scholar]
- 31.Solomon BJ, Cappuzzo F, Felip E, et al. Intracranial efficacy of crizotinib versus chemotherapy in patients with advanced ALK-positive non-small-cell lung cancer: results from PROFILE 1014. J Clin Oncol. 2016;34(24):2858–2865. doi: 10.1200/JCO.2015.63.5888. [DOI] [PubMed] [Google Scholar]
- 32.Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371(23):2167–2177. doi: 10.1056/NEJMoa1408440. [DOI] [PubMed] [Google Scholar]
- 33.Shaw AT, Yeap BY, Solomon BJ, et al. Effect of crizotinib on overall survival in patients with advanced non-small-cell lung cancer harbouring ALK gene rearrangement: a retrospective analysis. Lancet Oncol. 2011;12(11):1004–1012. doi: 10.1016/S1470-2045(11)70232-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010;363(18):1693–1703. doi: 10.1056/NEJMoa1006448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Iwama E, Goto Y, Murakami H, et al. Alectinib for patients with ALK rearrangement-positive non-small cell lung cancer and a poor performance status (Lung Oncology Group in Kyushu 1401) J Thorac Oncol. 2017;12(7):1161–1166. doi: 10.1016/j.jtho.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 36.Gettinger SN, Bazhenova LA, Langer CJ, et al. Activity and safety of brigatinib in ALK-rearranged non-small-cell lung cancer and other malignancies: a single-arm, open-label, phase 1/2 trial. Lancet Oncol. 2016;17(12):1683–1696. doi: 10.1016/S1470-2045(16)30392-8. [DOI] [PubMed] [Google Scholar]
- 37.Kim DW, Mehra R, Tan DSW, et al. Activity and safety of ceritinib in patients with ALK-rearranged non-small-cell lung cancer (ASCEND-1): updated results from the multicentre, open-label, phase 1 trial. Lancet Oncol. 2016;17(4):452–463. doi: 10.1016/S1470-2045(15)00614-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Felip E, Tan DS-W, Kim D-W, et al. Whole body and intracranial efficacy of ceritinib in ALK-inhibitor (ALKi)-naive patients (pts) with ALK-rearranged (ALK+) NSCLC and baseline (BL) brain metastases (BM): Results from ASCEND-1 and -3. J Clin Oncol. 2016;34(15_suppl):e20520. [Google Scholar]
- 39.Tan DS, Araújo A, Zhang J, et al. Comparative efficacy of ceritinib and crizotinib as initial ALK-Targeted therapies in previously treated advanced NSCLC: an adjusted comparison with external controls. J Thorac Oncol. 2016;11(9):1550–1557. doi: 10.1016/j.jtho.2016.05.029. [DOI] [PubMed] [Google Scholar]
- 40.Nishio M, Murakami H, Horiike A, et al. Phase I study of ceritinib (LDK378) in Japanese patients with advanced, anaplastic lymphoma kinase-rearranged non-small-cell lung cancer or other tumors. J Thorac Oncol. 2015;10(7):1058–1066. doi: 10.1097/JTO.0000000000000566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shaw AT, Kim DW, Mehra R, et al. Ceritinib in ALK-rearranged non-small-cell lung cancer. N Engl J Med. 2014;370(13):1189–1197. doi: 10.1056/NEJMoa1311107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Felip E, de Braud FG, Maur M. Ceritinib plus nivolumab (NIVO) in patients (pts) with anaplastic lymphoma kinase positive (ALK+) advanced non-small cell lung cancer (NSCLC). Paper Presented at: Annual Meeting of the American Society of Clinical Oncology; 2017; Chicago, IL. [Google Scholar]
- 43.Murakami H, Ono A, Nakashima K, et al. Long-term clinical outcomes of ALK inhibitors in patients with ALK-positive advanced non-small cell lung cancer. J Clin Oncol. 2017;35(15_suppl):e20542. [Google Scholar]
- 44.Ito K, Hataji O, Kobayashi H, et al. Sequential therapy with crizotinib and alectinib in ALK-rearranged non-small cell lung cancer – a multi-center retrospective study. J Thorac Oncol. 2017;12(2):390–396. doi: 10.1016/j.jtho.2016.07.022. [DOI] [PubMed] [Google Scholar]
- 45.Chiari R, Metro G, Iacono D, et al. Clinical impact of sequential treatment with ALK-TKIs in patients with advanced ALK-positive non-small cell lung cancer: results of a multicenter analysis. Lung Cancer. 2015;90(2):255–260. doi: 10.1016/j.lungcan.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 46.Asao T, Fujiwara Y, Itahashi K, et al. Sequential use of anaplastic lymphoma kinase inhibitors in Japanese patients with ALK-rearranged non-small-cell lung cancer: a retrospective analysis. Clin Lung Cancer. 2017;18(4):e251–e258. doi: 10.1016/j.cllc.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 47.Nosaki K, Toyozawa R, Taguchi K, et al. Real-world data on treatment patterns and survival among ALK+ NSCLC patients in Japan. J Clin Oncol. 2017;35(15_suppl):e20505. [Google Scholar]
- 48.Kayaniyil S, Hurry M, Wilson J, et al. Treatment patterns and survival in patients with ALK-positive non-small-cell lung cancer: a Canadian retrospective study. Curr Oncol. 2016;23(6):589–e597. doi: 10.3747/co.23.3273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Berge EM, Lu X, Maxson D, et al. Clinical benefit from pemetrexed before and after crizotinib exposure and from crizotinib before and after pemetrexed exposure in patients with anaplastic lymphoma kinase-positive non-small-cell lung cancer. Clin Lung Cancer. 2013;14(6):636–643. doi: 10.1016/j.cllc.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cadranel J, Park K, Arrieta O, et al. Characteristics, treatment patterns, and survival among ALK+ non-small cell lung cancer (NSCLC) patients treated with crizotinib: a chart review study. Lung Cancer. 2016;98:9–14. doi: 10.1016/j.lungcan.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 51.Cao Y, Xiao G, Qiu X, Ye S, Lin T. Efficacy and safety of crizotinib among Chinese EML4-ALK-positive, advanced-stage non-small cell lung cancer patients. PLoS One. 2014;9(12):e114008. doi: 10.1371/journal.pone.0114008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cui S, Zhao Y, Dong L, et al. Is there a progression-free survival benefit of first-line crizotinib versus standard chemotherapy and second-line crizotinib in ALK-positive advanced lung adenocarcinoma? A retrospective study of Chinese patients. Cancer Med. 2016;5(6):1013–1021. doi: 10.1002/cam4.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cui S, Zhao Y, Gu A, et al. Efficacy and tolerability of crizotinib in the treatment of ALK-positive, advanced non-small cell lung cancer in Chinese patients. Med Oncol. 2015;32(6):626. doi: 10.1007/s12032-015-0626-7. [DOI] [PubMed] [Google Scholar]
- 54.Duruisseaux M, Besse B, Cadranel J, et al. Overall survival with crizotinib and next-generation ALK inhibitors in ALK-positive non-small-cell lung cancer (IFCT-1302 CLINALK): a French nationwide cohort retrospective study. Oncotarget. 2017;8(13):21903–21917. doi: 10.18632/oncotarget.15746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lim SH, Yoh KA, Lee JS. Characteristics and outcomes of ALK+ non-small cell lung cancer patients in Korea. Asia Pac J Clin Oncol. 2017 doi: 10.1111/ajco.12645. [DOI] [PubMed] [Google Scholar]
- 56.Noronha V, Ramaswamy A, Patil VM, et al. ALK positive lung cancer: clinical profile, practice and outcomes in a developing country. PLoS One. 2016;11(9):e0160752. doi: 10.1371/journal.pone.0160752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yoshida T, Oya Y, Tanaka K, et al. Clinical impact of crizotinib on central nervous system progression in ALK-positive non-small lung cancer. Lung Cancer. 2016;97:43–47. doi: 10.1016/j.lungcan.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 58.Xing P, Wang S, Hao X, Zhang T, Li J. Clinical data from the real world: efficacy of crizotinib in Chinese patients with advanced ALK-rearranged non-small cell lung cancer and brain metastases. Oncotarget. 2016;7(51):84666–84674. doi: 10.18632/oncotarget.13179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang Q, Qin N, Wang J, et al. Crizotinib versus platinum-based double-agent chemotherapy as the first line treatment in advanced anaplastic lymphoma kinase-positive lung adenocarcinoma. Thorac Cancer. 2016;7(1):3–8. doi: 10.1111/1759-7714.12264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Guérin A, Sasane M, Wakelee H, et al. Treatment, overall survival, and costs in patients with ALK-positive non-small-cell lung cancer after crizotinib monotherapy. Curr Med Res Opin. 2015;31(8):1587–1597. doi: 10.1185/03007995.2015.1057115. [DOI] [PubMed] [Google Scholar]
- 61.Barlesi F, Dingemans A-MC, Yang JC-H, et al. Updated efficacy and safety from the global phase II NP28673 study of alectinib in patients (PTS) with previously treated ALK+ non-small-cell lung cancer (NSCLC) Ann Oncol. 2016;27(suppl_6) [Google Scholar]
- 62.Ou SH, Ahn JS, de Petris L, et al. Alectinib in Crizotinib-Refractory ALK-rearranged non-small-cell lung cancer: a phase II global study. J Clin Oncol. 2016;34(7):661–668. doi: 10.1200/jco.2015.63.9443. [DOI] [PubMed] [Google Scholar]
- 63.Shaw AT, Gandhi L, Gadgeel S, et al. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: a single-group, multi-centre, phase 2 trial. Lancet Oncol. 2016;17(2):234–242. doi: 10.1016/S1470-2045(15)00488-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Camidge DR, Sm G, Ou S. Updated efficacy and safety data from the phase 2 NP28761 study of alectinib in ALK-positive non-small-cell lung cancer (now available). 17th World Conference on Lung Cancer; Vienna, Austria. 2016. [Google Scholar]
- 65.Yang JC, Si O, de Petris L. Pooled systemic efficacy and safety data from the pivotal phase II studies (NP28673 and NP28761) of alectinib in ALK-positive non-small cell lung cancer. J Thorac Oncol. 2017 doi: 10.1016/j.jtho.2017.06.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gandhi L, Ou SI, Shaw AT, et al. Efficacy of alectinib in central nervous system metastases in crizotinib-resistant ALK-positive non-small-cell lung cancer: comparison of RECIST 1.1 and RANO-HGG criteria. Eur J Cancer. 2017;82:27–33. doi: 10.1016/j.ejca.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 67.Gandhi L, Gadgeel S, Shaw A, et al. Time to response in patients with ALK+ NSCLC receiving alectinib in the phase II NP28673 and NP28761 studies. Ann Oncol. 2016;27(suppl_6):1209PD. doi: 10.2147/LCTT.S209231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gadgeel SM, Shaw AT, Govindan R, et al. Pooled analysis of CNS response to alectinib in two studies of pretreated patients with ALK-positive non-small-cell lung cancer. J Clin Oncol. 2016;34(34):4079–4085. doi: 10.1200/JCO.2016.68.4639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gadgeel SM, Gandhi L, Riely GJ, et al. Safety and activity of alectinib against systemic disease and brain metastases in patients with crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF-002JG): results from the dose-finding portion of a phase 1/2 study. Lancet Oncol. 2014;15(10):1119–1128. doi: 10.1016/S1470-2045(14)70362-6. [DOI] [PubMed] [Google Scholar]
- 70.Ahn M-J, Camidge DR, Tiseo M.Brigatinib (BRG) in crizotinib (CRZ)-refractory ALK+ non-small cell lung cancer (NSCLC): updates from ALTA, a pivotal randomized phase 2 trial Paper presented at: Annual Meeting of the American Society of Clinical Oncology;2017Chicago, IL [Google Scholar]
- 71.Camidge DR, Bazhenova LA, Salgia R. Assessment of brigatinib (AP26113) CNS activity in patients (Pts) with ALK+ NSCLC and intracranial metastases in a phase 1/2 study. 18th European Cancer Congress; Vienna, Austria. 2015. [Google Scholar]
- 72.Gettinger SN, Kim D, Tiseo M. Brigatinib activity in patients with ALK+ NSCLC and intracranial CNS metastases in two clinical trials. 17th World Conference on Lung Cancer; Vienna, Austria. 2016. [Google Scholar]
- 73.Kim D-W, Tiseo M, Ahn M-J, et al. Brigatinib in patients with crizotinib-refractory anaplastic lymphoma kinase-positive non-small-cell lung cancer: a randomized, multicenter phase II trial. J Clin Oncol. 2017;35(22):2490–2498. doi: 10.1200/JCO.2016.71.5904. [DOI] [PubMed] [Google Scholar]
- 74.Ou SH, Tiseo M, Camidge DR. Brigatinib (BRG) in patients (pts) with crizotinib (CRZ)-refractory ALK+ non-small cell lung cancer (NSCLC) and brain metastases in the pivotal randomized phase 2 ALTA trial. Paper presented at: Annual Meeting of the American Society of Clinical Oncology; 2017; Chicago, IL. [Google Scholar]
- 75.Crinò L, Ahn MJ, de Marinis F, et al. Multicenter phase II study of whole-body and intracranial activity with ceritinib in patients with ALK-rearranged non-small-cell lung cancer previously treated with chemotherapy and crizotinib: results from ASCEND-2. J Clin Oncol. 2016;34(24):2866–2873. doi: 10.1200/JCO.2015.65.5936. [DOI] [PubMed] [Google Scholar]
- 76.Hida T, Satouchi M, Nakagawa K. Ceritinib in patients with advanced, crizotinib-treated, anaplastic lymphoma kinase-rearranged NSCLC: Japanese subset. Jpn J Clin Oncol. 2017:1–7. doi: 10.1093/jjco/hyx045. [DOI] [PubMed] [Google Scholar]
- 77.Shaw AT, Kim TM, Crinò L, et al. Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2017;18(7):874–886. doi: 10.1016/S1470-2045(17)30339-X. [DOI] [PubMed] [Google Scholar]
- 78.Hida T, Nakagawa K, Seto T, et al. Pharmacologic study (JP28927) of alectinib in Japanese patients with ALK+ non-small-cell lung cancer with or without prior crizotinib therapy. Cancer Sci. 2016;107(11):1642–1646. doi: 10.1111/cas.13066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liu G, Zhang J, Zhou ZY, Li J, Cai X, Signorovitch J. Association between time to progression and subsequent survival in ceritinib-treated patients with advanced ALK-positive non-small-cell lung cancer. Curr Med Res Opin. 2016;32(11):1911–1918. doi: 10.1080/03007995.2016.1220934. [DOI] [PubMed] [Google Scholar]
- 80.Bendaly E, Dalal AA, Culver K, et al. Treatment patterns and early outcomes of ALK-positive non-small cell lung cancer patients receiving ceritinib: a chart review study. Adv Ther. 2017;34(5):1145–1156. doi: 10.1007/s12325-017-0527-6. [DOI] [PubMed] [Google Scholar]
- 81.Bendaly E, Dalal AA, Culver K, et al. Monitoring for and characterizing crizotinib progression: a chart review of ALK-positive non-small cell lung cancer patients. Adv Ther. 2017;34(7):1673–1685. doi: 10.1007/s12325-017-0551-6. [DOI] [PubMed] [Google Scholar]
- 82.Gainor JF, Tan DS, de Pas T, et al. Progression-free and overall survival in ALK-positive NSCLC patients treated with sequential crizotinib and ceritinib. Clin Cancer Res. 2015;21(12):2745–2752. doi: 10.1158/1078-0432.CCR-14-3009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Roeper J, Netchaeva M, Lueers AC, et al. Impact on OS of 2nd and 3rd generation TKI in EGFR mt+ and ALK+ patients: Results of the NOWEL network. J Clin Oncol. 2017;35(15_suppl):e20560. [Google Scholar]
- 84.Watanabe S, Hayashi H, Okamoto K, et al. Progression-free and overall survival of patients with ALK rearrangement-positive non-small cell lung cancer treated sequentially with crizotinib and alectinib. Clin Lung Cancer. 2016;17(6):528–534. doi: 10.1016/j.cllc.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 85.LORBRENA (lorlatinib) U.S. Prescribing Information. New York, NY: Pfizer Inc; 2018. [Google Scholar]
- 86.Solomon BJ, Besse B, Bauer TM, et al. Lorlatinib in patients with ALK-positive non-small-cell lung cancer: results from a global phase 2 study. Lancet Oncol. 2018;19(12):1654–1667. doi: 10.1016/S1470-2045(18)30649-1. [DOI] [PubMed] [Google Scholar]
- 87.Mok TSK, Kim D-W, Wu Y-L, et al. Overall survival (OS) for first-line crizotinib versus chemotherapy in ALK+ lung cancer: updated results from PROFILE 1014. Paper presented at: Annual Meeting of the European Society for Medical Oncology; 2017; Madrid, Spain. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.