Abstract
The numbers of multiple drug-resistant Gram-negative bacterial infections are rising worldwide. The threat is increased by the lack of new antibiotics, so clinicians are turning to older drugs previously abandoned due to their recognized toxicity, such as colistin. However, the need to avoid kidney toxicity from colistin has led to its topical use. We present the case of a patient with type I cardiorenal syndrome with cystitis due to multiple drug-resistant Pseudomonas aeruginosa who was successfully treated with intravesical instillation of colistin.
LEARNING POINTS
The case report is one of the few in the literature on the intravesical instillation of colistin to address lower urinary tract infection.
Isolated intravesical colistin instillation was effective in a patient with anuria.
Keywords: Colistin, Pseudomonas, multiple drug resistance
INTRODUCTION
Pseudomonas aeruginosa is a Gram-negative bacterium frequently associated with hospital-acquired infections and is one of the most frequent multiple-drug-resistant Gram-negative bacteria (MDR-GNB) encountered. It is often the agent behind ventilator-associated pneumonia and other hospital-acquired infections[1,2].
The emergence of MDR-GNB is posing a threat as they cause significant morbidity and mortality worldwide in the form of hospital-acquired infections and, increasingly, community-acquired infections in immunocompromised patients or patients with severe pulmonary or cardiovascular comorbidities[3]. However, few new antibiotics are available to combat these organisms, so clinicians are turning to older antibiotics such as colistin.
Colistin is an antibiotic belonging to the polymyxin group which was discovered in 1949 by Koyama et al and made available in the form of a less toxic prodrug, colistimethate sodium. It was later largely abandoned due to its nephrotoxicity[4]. This toxicity together with the need to tackle MDR-GNB has led to topical routes of administration, such as intrathecal and intraventricular, as well as by inhalation. Instillation in the bladder for urinary tract infections (UTI) caused by Acinetobacter baumani has been reported to be effective[5,6]. However, there are few reports in the literature of its use against UTI due to P. aeruginosa[7].
This article describes the case of a patient with type I cardiorenal syndrome with anuria who developed cystitis due to MDR P. aeruginosa and was treated successfully with bladder instillation of colistin.
CASE PRESENTATION
A 78-year-old male patient with a history of heart failure due to ischaemic heart disease, atrial flutter, essential hypertension, chronic kidney disease (with base serum creatinine of 1.9 mg/dl and an estimated glomerular filtration rate of 33 ml/min/1.73 m2) and peripheral artery disease presented to the emergency department with severe peripheral oedema, shortness of breath and low urinary output for the previous 4 days.
He was admitted to the Intermediate Care Unit having been diagnosed with acute on chronic heart failure due to poor therapeutic compliance. During his stay, he had an unfavourable evolution, developing increasing dyspnoea, peripheral oedema, and AKIN stage 3 acute on chronic kidney injury (with serum creatinine of 5.2 mg/dl, BUN of 25.63 mmol/l, and low urine output of 200 ml/day). On the 4th day after admission, the patient developed fever and lower abdominal pain. His laboratory results revealed elevated C-reactive protein (CRP) (10 mg/dl) and leucocytosis (14.11×109/l), and arterial blood gas evaluation demonstrated metabolic acidosis with 3.1 mmol/dl lactate. Urinalysis showed the presence of leucocyturia, and bacteriuria was present in the urine sediment. Kidney ultrasound and abdominal CT excluded obstructive causes of oliguria as well as upper UTI or other abdominal infections. Blood and urine cultures were obtained, and the patient started empiric antibiotic treatment with piperacillin/tazobactam.
Due to the multiple organ failure, the patient required invasive mechanical ventilation, vasopressor and inotropic support and continuous renal replacement therapy (CRRT), which were administered in the Intensive Care Unit (ICU).
On the 6th day after hospital admission, urine culture revealed the growth of an MDR P. aeruginosa sensible only to colistin. The blood cultures were negative. As the patient still had acute kidney failure with anuria, the administration of colistin through bladder instillation was considered the best option.
Continuous bladder instillation was initiated with 3 million IU for a total of 7 days as previously proposed by Garcés-Jimeno et al. [7]. The colistin was diluted in normal saline (1 million IU in 500 ml of normal saline). Initially requiring vasopressor and inotropic support with norepinephrine and dobutamine, the patient started to slowly recover, allowing for weaning from vasopressor, inotropic and ventilatory support. Recovery from acute kidney injury followed the same pattern, with the patient eventually resuming effective diuresis, allowing for suspension of the CRRT on the 13th day after admission. During the period of antibiotic treatment with colistin, blood analysis showed progressive reduction of leucocytosis and CRP.
The patient was later discharged from the ICU without requiring any organ support device, including haemodialysis. Urine cultures obtained after treatment with colistin showed no bacterial growth.
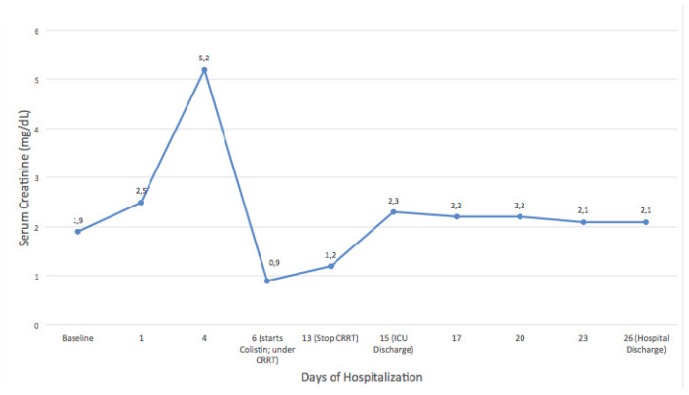
During CRRT, creatinine levels remained relatively stable due to the technique itself and rose to 2.3 mg/dl on the 15th day of hospitalization, followed by a progressive return to basal values (Fig. 1). After CRRT suspension until hospital discharge on the 26th day of hospitalization, the patient maintained adequate diuresis (1,200–1,800 ml/day under diuretic therapy with furosemide 40 mg/day) with no need for haemodialysis.
Figure 1.
Serum creatinine (mg/dL) evolution through hospitalization (including baseline and hospital discharge values).
DISCUSSION
In the present case, bladder instillation was the only effective method for addressing the patient’s UTI. The option of intravenous colistin was deferred due to its nephrotoxicity and presumable low drug concentration that would be delivered to the urinary epithelia due to anuria, below the minimal inhibitory concentration. This could potentially lead to the selection of new, colistin-resistant, P. aeruginosa. Our strategy was successful as urine culture after antibiotic treatment was negative and the patient’s kidney function remained stable during and after treatment (Fig. 1) allowing for hospital discharge without additional need for haemodialysis.
Although an off-label use, colistin can be administered effectively through bladder instillation. This case report demonstrates that bladder instillation of colistin can be a safe and effective way of combating lower UTIs due to MDR-GNB, allowing for controlled exposure of patients to this drug’s toxicity.
Footnotes
Conflicts of Interests: The Authors declare that there are no competing interests.
REFERENCES
- 1.Ruiz-Garbajosa P, Cantón R. Epidemiology of antibiotic resistance in Pseudomonas aeruginosa. Implications for empiric and definitive therapy. Rev Esp Quimioter. 2017;30(Suppl 1):8–12. [PubMed] [Google Scholar]
- 2.Kollef M, Chastre J, Fagon J, François B, Niederman M, Rello J, et al. Global prospective epidemiologic and surveillance study of ventilator-associated pneumonia due to Pseudomonas aeruginosa. Crit Care Med. 2014;42:2178–2187. doi: 10.1097/CCM.0000000000000510. [DOI] [PubMed] [Google Scholar]
- 3.Cillóniz C, Gabarrús A, Ferrer M, Puig de la Bellacasa J, Rinaudo M, Mensa J, et al. Community-acquired pneumonia due to multidrug- and non-multidrug-resistant Pseudomonas aeruginosa. Chest. 2016;150:415–425. doi: 10.1016/j.chest.2016.03.042. [DOI] [PubMed] [Google Scholar]
- 4.Grégoire N, Aranzana-Climent V, Magréault S, Marchand S, Couet W. Clinical pharmacokinetics and pharmacodynamics of colistin. Clin Pharmacokinet. 2017;56:1441–1460. doi: 10.1007/s40262-017-0561-1. [DOI] [PubMed] [Google Scholar]
- 5.Giua R, Pedone C, Cortese L, Antonelli Incalzi R. Colistin bladder instillation, an alternative way of treating multi-resistant Acinetobacter urinary tract infection: a case series and review of literature. Infection. 2014;42:199–202. doi: 10.1007/s15010-013-0507-y. [DOI] [PubMed] [Google Scholar]
- 6.Pietropaolo A, Jones P, Moors M, Birch B, Somani BK. Use and effectiveness of antimicrobial intravesical treatment for prophylaxis and treatment of recurrent urinary tract infections (UTIs): a systematic review. Curr Urol Rep. 2018;19:78. doi: 10.1007/s11934-018-0834-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcés-Jimeno B, Tomasa-Irriguible TM, Moreno-Molina JA. Intravesical instillations of colistin in urine infections with multiresistant pathogens. Med Intensiva. 2014;39:125–126. doi: 10.1016/j.medin.2014.07.004. [DOI] [PubMed] [Google Scholar]