Abstract
A large proportion of the public health costs of alcohol use disorder (AUD) can be accounted for by a small percentage of severe cases with a chronic course starting in adolescence and persisting into adulthood. However, chronicity may be a less effective marker of AUD severity in women than men due to a gender risk-severity paradox wherein comparable levels of risk exposure yield more co-occurring problems for women than men with AUD. To model this paradox, we compared trajectories of alcohol and drug use problems, depression symptoms, and antisocial behavior from ages 17 to 29 in men and women with a persistent, desistent, or no history of AUD. Problems followed a quadratic trajectory (i.e., increases followed by decreases), with gender and AUD chronicity moderating age-related change. Specifically, persistent and desistent courses differentiated the severity of problems more effectively in men while chronicity had less utility for differentiating AUD severity in women.
Keywords: alcohol use disorder, gender, adolescent problems, emerging adulthood, development
Alcohol use disorder (AUD) confers exorbitant financial and human costs worldwide (Rehm et al., 2009; WHO, 2004). AUD has a high lifetime prevalence (overall, 29.1%; men, 36.0; women, 22.7%; Grant et al., 2015), with early onset cases emerging in late adolescence, followed by an escalation through young adulthood, and a steady decline thereafter. A large proportion of the public health costs and service utilization can be accounted for by a small percentage of severe cases (Dickey & Azeni, 1996) with chronic AUD in emerging adulthood (Babor et al., 1992; Culverhouse et al., 2005; Hicks, Iacono, & Mcgue, 2010; Leggio, Kenna, Fenton, Bonenfant, & Swift, 2009; Moss, Chen, & Yi, 2007; Windle & Scheidt, 2004). Person-centered studies of AUD chronicity in men have identified that chronic cases are frequently accompanied by early and persisting psychiatric problems while developmentally-limited AUD cases remitting by the late 20’s exhibit ostensible recovery across these domains of functioning (i.e., AUD subtypes; e.g., Zucker, 1994). AUD chronicity subtypes have unclear utility for women due to a gender risk-severity paradox wherein the relatively lower levels of AUD risk in women as compared to men appear to confer more severe outcomes (Foster, Hicks, Iacono & McGue, 2015). To adequately test this paradox, more research is needed to determine if a chronic course of AUD differentiates its developmental severity (i.e., the accumulation of psychiatric problems through emerging adulthood) equally in men and women or if women are more vulnerable to the accumulation of problems co-morbid with AUD, irrespective of its chronicity.
AUD Symptom Chronicity and Psychosocial Development in Men and Women
Age-related trends in AUD prevalence involve early onset in late adolescence, a rise to peak prevalence in the early to mid-20’s (Chassin, Flora, & King, 2004; Chen & Kandel, 1995; Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2015), followed by a substantial decline through the late 20’s (Chassin et al., 2004; Chen & Kandel, 1995; Johnstone, Leino, Ager, Ferrer, & Fillmore, 1996). To understand the network of processes that underlie AUD severity in emerging adulthood, it is necessary to consider developmental variation in the temporal stability and acceleration (or deceleration) of co-occurring problems across individuals who express the target trait (e.g., AUD) along distinct trajectories.
Developmental theorists have consistently discouraged a priori assumptions of within-group homogeneity (Granic & Hollenstein, 2017) as change over time in co-developing processes necessarily contributes to between-person heterogeneity in their trajectory. This is particularly important during emerging adulthood when increasing levels of independence – marked specifically by matriculation to college and/or entry into the workforce – lead to a notable diversification of life trajectories thereafter (Arnett, 2000; Schulenberg & Maggs, 2002; Schulenberg, O’Malley, Bachman, & Johnston, 2000; Sherrod, Haggerty, & Featherman, 1993). An individual’s existing characteristics at the beginning of this period are further shaped by engagement across multiple contexts in a dynamic process of mutual selection that progressively shapes the individuals context and the persistence/desistence of specific characteristics like AUD (Granic & Patterson, 2006; Nurmi, 1993; Plomin, DeFries, & Loehlin, 1977; Scarr & McCartney, 1983).
As emerging adulthood is both the period of peak prevalence for AUD and the period when co-developing processes grow increasingly diverse, it will be important to understand how features of this multidimensional network of co-developing processes potentiate a severe trajectory of AUD. One approach that has been particularly advantageous for this is the identification of person-centered profiles or typologies of AUD through the period of emerging adulthood (Babor et al., 1992; Clark, Kirisci, & Tarter, 1998; Cloninger, 1987; Zucker, 1994). The numerous typologies identified consistently deploy two key features of AUD to account for its heterogeneity: the chronicity of AUD symptoms (i.e., persisting vs. developmentally-limited types, Zucker, 1994) and individual differences in psychosocial functioning (i.e., behavioral disinhibition, affective dysregulation and a problematic social context) that develop alongside them (Babor et al., 1992). The most well replicated aspects of this research suggest that men with AUD symptoms that persist past the period of peak prevalence (i.e., through to adulthood) exhibit a consistent trajectory of persisting psychosocial impairment, with the poorest outcomes observed among men with the longest course of AUD (i.e., adolescence onset, persistent course; Clark, 2004; Hicks et al., 2010). In contrast, a “maturing out” of symptoms frequently coincides with a reduction of concomitant psychosocial problems (e.g., Littlefield & Winograd, 2013), with the negative consequences largely remediated by adulthood in men with the shortest courses of the disorder (i.e., young adult onset, adult desistence). Consequently, AUD chronicity effectively differentiates the risks and long-term consequences for AUD in men.
Extending the Study of AUD Chronicity to Women
Despite its utility in men, AUD chronicity may be less useful for differentiating co-occurring problems for women with AUD. That is, men and women may experience differing consequences of heavy alcohol use during emerging adulthood along with mean-level and structural gender differences in the association between co-morbid problems and AUD. Compared to men, women are likely to experience a broader and more severe set of consequences following alcohol use, ranging from greater risk of physical victimization and medical harm to more punitive social sanctions (Acker, 1986a; Erol & Karpyak, 2015; Grant, LaBrie, Hummer, & Lac, 2012; Greenfield, 2002; Hommer, Momenan, Kaiser, & Rawlings, 2001; Mann et al., 2005; Niaura, Nathan, Frankenstein, Shapiro, & Brick, 1987; Nolen-Hoeksema, 2004; Stockwell et al., 2002; Wilsnack, Wilsnack, & Kantor, 2013). By extension, women not only develop AUD in the context of disproportionately punitive biological consequences for heavy alcohol use but may also are simultaneously subjected to systematic sexism and gender role identification that both prescribe limited patterns of alcohol use (Gomberg, 1981, 1988; Grant, 2006; Greenfield, 2002). Heavy drinking females with AUD may then experience significantly more social costs and negative experiences like isolation, shame, and stigma in conjunction with the disorder than men for whom heavy alcohol use may be more socially permissible (Beckman & Amaro, 1986; Gomberg, 1981, 1988; Huselid & Cooper, 1992). Additionally, mean-levels of risk factors known to contribute to AUD persistence in men (i.e., heavy alcohol use, drug use, antisocial behavior, and deviant peer affiliation) occur at normatively higher levels in men than women throughout development (Nolen-Hoeksema, 2004), suggesting that being female may be considered a protective factor for an AUD outcome. Psychosocial problems also appear to have different structural relationships with AUD in women wherein the same amount of risk exposure in both genders yields larger increases in the odds of developing AUD for women than men (e.g., equivalent exposure to depression at age 17 produces greater odds of developing AUD by age 29 for women than men; Foster et al., 2015). Consequently, women are generally not likely to incur AUD risk levels comparable to men but also appear to require less of this risk than men to develop AUD and concomitant problems.
The extent to which chronic AUD alters the course of co-occurring problems among women is not well known. One possibility is that a gender-specific disruption in the trajectory of normative development may occur following the period of peak prevalence for alcohol problems. Greater consequences of alcohol use and AUD for women than men during this period may include reduced engagement, achievement, and identity development across multiple personal and professional contexts. Disruption in these processes could subsequently have a gender-specific cascading effect on development thereafter (e.g., Hankin & Abramson, 2001), as they are known to independently increase psychiatric problems that may prolong AUD. Broadly, these gender differences suggest that the trajectory of AUD in women may be generally more severe – with greater consequences for long-term development – among women than men.
To date, the few studies of AUD chronicity that include women highlight gender-specific associations of some factors (i.e., “negative affect alcoholism”; Zucker, 1994) and indicate that, even after AUD remission, women with either desistent or persistent AUD exhibit similarly high levels of psychosocial problems compared to women with no history of AUD (Foster, Hicks, Iacono & McGue, 2014). However, these studies have either conducted gender analyses in women separately from men (e.g., “negative affect alcoholism”; Zucker, 1994) or modeled effects as if they were equivalent in men and women, thereby ignoring known gender differences in these phenomena (Babor et al., 1992). Overall, these approaches model effects in women as either qualitatively different or equivalent to men rather than explicitly modeling the degree to which AUD chronicity is associated with atypical development within each gender. A more comprehensive longitudinal approach that simultaneously models between- and within-gender variation is needed to determine gender differences in the clinical and prognostic utility of AUD chronicity.
The Gender Risk-Severity Paradox of AUD
The joint observations that women have a lower prevalence of AUD (Keyes, Grant, & Hasin, 2008), lower mean-levels of risk exposure, greater vulnerability to comparable risk exposure, and a faster accumulation of consequences from alcohol use than men suggest that a gender risk-severity paradox is present. While women are generally thought to be resilient to AUD onset, they simultaneously appear more vulnerable to the deleterious effects of alcohol that may have gender-specific consequences for long-term development, especially for those with a long course of AUD. By contrast, typologies of AUD in men differentiate unique profiles of problems via the persistence/desistence of AUD symptoms – wherein a large contingent of men are known to ostensibly recover from the debilitating effects of AUD. Therefore, AUD chronicity likely accounts for significant, prolonged developmental variation in co-occurring problems among men while its utility remains less clear for women. Studies estimating gender moderation of the link between AUD chronicity and psychosocial problems are needed to test this gender risk-severity paradox.
To address this, we estimated how AUD chronicity moderates developmental change in the trajectory of frequently co-occurring problems (i.e., alcohol and drug use problems, depression symptoms, and antisocial behavior) in a large sample of men and women assessed prospectively from ages 17 to 29. Specifically, we compared the trajectories of problems across groups of men and women with desistent, persistent, and no history of AUD. Prior cross-sectional and longitudinal investigations have confirmed robust associations between these factors and AUD (Cranford, Nolen-Hoeksema, & Zucker, 2011; Granic & Patterson, 2006; Hawkins, Catalano, & Miller, 1992; Iacono, Malone, & McGue, 2008; Kendler, Prescott, Myers, & Neale, 2003; Krueger et al., 2002; Moffitt & Caspi, 2001; Patterson & Yoerger, 1997; Rutledge & Sher, 2001). Functioning in these domains is also commonly modulated by gender, age, and AUD severity and covers key liabilities in behavior and affective dysregulation previously implicated in AUD typologies. Our 12-year longitudinal design was opportune for mapping different courses of AUD (i.e., desistent vs. persistent) in conjunction with normative development (i.e., no history of AUD) from adolescence (to capture problems preceding AUD chronicity) through to young adulthood (to capture the accumulation of consequences over the course of the disorder).
AUD chronicity differences in co-occurring problems were hypothesized to be greater for men than women, with four critical implications for understanding AUD severity: 1) proportionally more women than men with AUD would endorse a trajectory of problems in a severe range relative to same-gender controls without a history of AUD, 2) adolescent risk would have less prognostic utility for AUD course and severity in women than men, 3) even after AUD symptoms desist, women would not ostensibly recover to the same degree as men and 4) prominence of a particular problem in one gender more than the other would mark gender-specific risk for AUD.
Method
Sample
Participants were male (n=578) and female (n=674) twins of the Minnesota Twin Family Study (MTFS), a prospective, community-based study designed to examine the etiology of substance use disorders (for extensive details on study design see Iacono, Carlson, Taylor, Elkins, & McGue, 1999). Twin pairs born between the years of 1972 and 1979 were recruited from Minnesota public birth records at age 17. Of the 90% of families located, 83% were assessed in-person at the University of Minnesota. Families recruited initially were typically employed in skilled jobs (i.e. “blue collar” employment) and had an average of slightly higher than high school education (i.e., average rating of 4 on the Hollingshead Index; Hollingshead, 1957). By Age 24, the average participant had completed some college. Levels of education were consistent across gender and AUD groups. Participants were predominately European American (96%; Iacono et al., 1999) and were similar to non-participating families in terms of parental occupation, education, and history of mental health treatment.
Longitudinal Assessment
At age 17, participants were assessed for lifetime alcohol and other drug use disorders along with several other psychiatric, psychosocial, and environmental variables. Follow-up assessments were conducted every 3–5 years at the target ages of 20 (n = 1110, 89% retention rate, 83% of men and 93% of women), 24 (n = 1159, 92% retention rate, 94% of men and 91% of women) and 29 years (n = 1164, 93% retention rate, 91% of men and 94% of women) and covered the period since the last assessment. Attrition did not significantly predict variation in focal variables. Analogous measures at each time point were used to chart age-related change in psychiatric variables. A more comprehensive description of the assessment battery included in the MTFS is provided elsewhere (Hicks et al., 2010).
AUD Diagnosis and Course
Using DSM-III-R and later DSM-IV criteria, AUD status was assessed with the Substance Abuse Module (SAM; Cottler, Robins, & Helzer, 1989) of the Composite International Diagnostic Interview (CIDI; Robins et al., 1988) at ages 17, 20, 24 and 29 (diagnostic reliability κ = 0.91, and re-test reliability, α = 0.80). To be consistent with the DSM-5 diagnostic threshold for AUD, 2 or more symptoms of alcohol abuse or dependence (no information was available for the DSM-5 craving symptom) were coded as a positive AUD diagnosis for each assessment through age 29 (lifetime AUD: males, n=316; females, n=155). Numerous studies using the MTFS sample have demonstrated the validity of this approach (Elkins, King, McGue, & Iacono, 2006; Elkins, McGue, & Iacono, 2007; Elkins, McGue, Malone, & Iacono, 2004; McGue & Iacono, 2005). A persisting course was defined by 2 symptoms of AUD at age 29 and at one prior assessment. A desisting course was defined as 0 symptoms of AUD at age 29 following a period of 2 or more symptoms at a prior assessment (Foster et al., 2014; Hicks et al., 2010). In the MTFS sample, 58.0% of participants with a lifetime AUD who met these inclusion criteria exhibited a desisting course (males, n=106; females, n=76) while 42.0% had a persistent course (males, n=93; females, n=41). Compared to overall rates within-gender (i.e., number of persistent AUD women vs. number of AUD women overall), a higher proportion of women (65.0%) than men (53.3%) with AUD desisted while persistence was more common in men (46.7%) than women (35.0%). Both the persisting and desisting groups of men and women were compared to a same-sex control group (males, n=226; females, n=449) who reported no more than 1 symptom of AUD at each assessment.
Psychiatric Variables
The current study focused on psychiatric variables prominently linked to AUD across numerous studies and replicated in the MTFS sample (Foster et al., 2014; Hicks et al., 2010). All variables were assessed using the same measures at ages 17, 20, 24, and 29. Age 17 variables reflect lifetime problem exposure up to that assessment while all subsequent assessments reflect time since last assessment.
Alcohol Use Composite
An alcohol use composite was calculated using the mean z-score of the average quantity and the maximum number of drinks consumed in 24 hours in the past year. These two variables were used because a prior study with the MTFS sample showed that they loaded best onto a single alcohol use factor (Hicks, Schalet, Malone, Iacono & McGue, 2011), have a robust relationship with the AUD diagnosis, and are dimensional measures sensitive to individual differences across a wide range of variation in alcohol use. Alternative metrics like drinking frequency had a demonstrably weaker relationship with AUD given that frequency can be high in the absence of the type of heavy drinking characteristic of alcohol problems (e.g., 30 days of drinking in one month with one drink per occasion). The final alcohol use composite was converted to a T-score to aid interpretability and repeated measures were standardized to the age 17 mean and standard deviation.
Drug Use Problems Composite
To index broad liability for using drugs other than alcohol across members of our community sample, a drug use problems composite was calculated using the mean z-score across symptoms of nicotine dependence, symptoms of abuse/dependence for illicit drugs across the drug classes of amphetamines, cannabis, cocaine, hallucinogens, inhalants, opioids, PCP, and sedatives as operationalized in the DSM-III-R and -IV criteria for other substance use disorders. These symptoms were assessed using the CIDI-SAM (diagnostic reliabilities for each substance use disorder diagnosis, κ > 0.91 and re-test reliability for symptom count, α > 0.86). The symptom count for the illicit drug class with the highest number of symptoms endorsed was used to quantify each participant’s abuse/dependence status for illicit drugs. Additional variables included frequency of marijuana use and the number of different drug classes tried. The final drug use composite was converted to a T-score to aid interpretability and repeated measures were standardized to the age 17 mean and standard deviation. Results from the composite are presented following verification that results were consistent across each drug group included (i.e., nicotine, marijuana, and illicit drugs).
Psychiatric Symptom Counts
A count of symptoms of major depression was obtained from the Structured Clinical Interview for DSM–IV (diagnostic reliability, κ = 0.79, and re-test reliability, α =0.61). A count of symptoms of adult antisocial behavior was also obtained via structured interview similar to the Structured Clinical Interview for the DSM-IV Axis II module for antisocial personality disorder (diagnostic reliability, κ = 0.95, and re-test reliability, α =0.80). The original symptom metric was retained to aid in interpretability.
Statistical Analysis
Multilevel modeling (MLM) was used to estimate age-related change for each mental health variable separately. Residuals for alcohol and drug use composites were normally distributed, permitting use of a maximum likelihood approach. Count data for depression and antisocial behavior symptoms was modeled using a multilevel Poisson distribution. Robust standard error estimates are reported for each of the four variables.
Gender, AUD course group, and their interaction were included as predictors to account for variability in developmental change in each variable from age 17 to age 29. MLM has been identified as particularly useful for analyzing nested data (Hox, 2010; Raudenbush and Bryk, 2002). A three-level equation was used to nest repeated observations over time within individuals who were also nested within families. Nesting data allowed for adjustment of robust standard errors and p-values for the non-independence of the family-level data and within-person longitudinal observations. Time effects were modeled using actual age to account for variation in age across people at each assessment. Age was centered at 17 (i.e., intercept reflected age 17 value of the dependent variable) and the Age and Age2 effects modeled the shape of change thereafter. Inclusion of a random intercept controlled for between-family variation in the level of the dependent variable at the initial measurement (i.e., age 17).
Using HLM 7.0 software, models were fit for each variable in two steps. First, an unconditional model that included only Level-1 parameters (i.e., intercept, Age, Age2) was fit to determine if the inclusion of a quadratic parameter was appropriate (i.e., if quadratic age effects account for significant variation in the variable). We then added orthogonal contrasts for gender and AUD groups to fit a full model including all additive and multiplicative effects. Explanatory variables were entered as level-2 predictors of the level-1 parameters (Intercept, Age, and Age2). Additive, main effects of gender (coded as 1 for males and −1 for females) and AUD group were represented as orthogonal contrasts comparing control versus desistent groups (coded as 0 for those in the persistent group, −1 for control, + 1 for desist) and the persistent versus desistent groups (coded as 0 for the control group, −1 for desist, and +1 for persist). Interactions between the contrasts for gender and AUD group were also included to test whether 1) AUD group differences in the problem were moderated by gender and 2) AUD group differences in the Age and Age2 effects were also moderated by gender. Orthogonal coding was used to allow for simultaneous testing of the planned, focal contrasts. Use of an orthogonal coding scheme testing focal group contrasts in a single model was optimal for reducing unnecessary inflation of Type I error that would result from using other coding schemes (e.g., effects coding) that would require many more models be run to obtain group-specific interaction estimates.
To aid in interpretability of results (particularly interaction effects), model estimates (presented in Table 1) were used to calculate and plot model-predicted growth by age, gender, and AUD group for each psychiatric variable in Figures 1–4. On the left side of Table 1, the growth parameters are presented as “Level-1 estimates”. On the right side of Table 1, main effects and interactions of Gender and AUD course groups (across rows) are reported under the three “Level-2 estimates” columns corresponding to the intercept (i.e., direct effects of level-2 parameters on the variable), the linear age effect (i.e., group differences in the age-related increase/decrease in the variable), and the quadratic age effect (i.e., group differences in age-related acceleration/deceleration in the variable). Importantly, the Gender x AUD group interaction effects predicting the linear and quadratic effects of age tested for gender moderation of differences in the age-related change in the problem between the two AUD groups specified. For example, a significant Gender x AUD (Persistent vs. Desistent) in the “Predicting Age2” column would indicate that AUD group differences in age-related acceleration (i.e., positive values) or deceleration (i.e., negative values) in the problem are moderated by gender.
Table 1.
Multilevel Model Analyses for Psychosocial Factors
| Factor | Level-1 Parameters | Level-2 Parameters | |||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Intercept | Age | Age2 | Predicting Intercept | Predicting Age | Predicting Age2 | ||
| Alcohol Use | 52.18 (0.53)*** | 2.73 (0.17)*** | −0.18 (0.01)*** | Gender | 0.45 (0.53) | 1.28 (0.17)*** | −0.09 (0.01)*** |
| Desist (vs. Control) | 5.69 (0.54)*** | 0.21 (0.18) | −0.02 (0.01)* | ||||
| Persist (vs. Desist) | 3.49 (0.83)*** | 0.06 (0.25) | 0.02 (0.02) | ||||
| Gender x Desist (vs. Control) | 0.33 (0.54) | 0.63 (0.18)*** | −0.05 (0.01)*** | ||||
| Gender x Persist (vs. Desist) | 1.69 (0.83)* | 0.18 (0.25) | −0.02 (0.02) | ||||
| Drug Use Problems | 50.85 (0.73)*** | 3.13 (0.35)*** | −0.22 (0.02)*** | Gender | −2.19 (0.73)*** | 1.08 (0.18)*** | −0.06 (0.02)*** |
| Desist (vs. Control) | 2.71 (0.72)*** | 2.22 (0.36)*** | −0.16 (0.02)*** | ||||
| Persist (vs. Desist) | 2.06 (1.21)* | 1.98 (0.57)*** | −0.13 (0.04)*** | ||||
| Gender x Desist (vs. Control) | −1.99 (0.72)** | 1.03 (0.36)** | −0.06 (0.01)*** | ||||
| Gender x Persist (vs. Desist) | −0.79 (1.21) | 0.89 (0.30)** | −0.06 (0.02)** | ||||
| Depression Symptoms | −0.48 (0.10)*** | −0.03 (0.03) | 0.00 (0.00) | Gender | −0.28 (0.10)** | −0.02 (0.03) | 0.00 (0.00) |
| Desist (vs. Control) | −0.05 (0.11) | 0.10 (0.04)** | −0.01 (0.003)** | ||||
| Persist (vs. Desist) | 0.16 (0.14) | 0.01 (0.05) | 0.00 (0.00) | ||||
| Gender x Desist (vs. Control) | −0.17 (0.11) | 0.02 (0.04) | 0.00 (0.00) | ||||
| Gender x Persist (vs. Desist) | −0.05 (0.14) | −0.01 (0.05) | 0.00 (0.00) | ||||
| Antisocial Behavior | −0.49 (0.07)*** | 0.18 (0.02)*** | −0.01 (0.001)*** | Gender | 0.16 (0.07)* | 0.02 (0.02) | −0.001 (0.001) |
| Desist (vs. Control) | 0.78 (0.08)*** | −0.07 (0.02)** | 0.003 (0.001)* | ||||
| Persist (vs. Desist) | 0.54 (0.09)*** | −0.05 (0.02)* | 0.004 (0.001)** | ||||
| Gender x Desist (vs. Control) | −0.21 (0.08)* | 0.06 (0.02)** | −0.003 (0.001)** | ||||
| Gender x Persist (vs. Desist) | 0.06 (0.09) | 0.00 (0.00) | 0.00 (0.00) | ||||
p<.001;
p<.01;
p<.05;
no adjustments for multiple tests and robust standard errors are reported for all estimates. Intercept values reflect age 17 scores. Random effects are estimated for the intercept; all other parameters were fixed.
Figure 1.
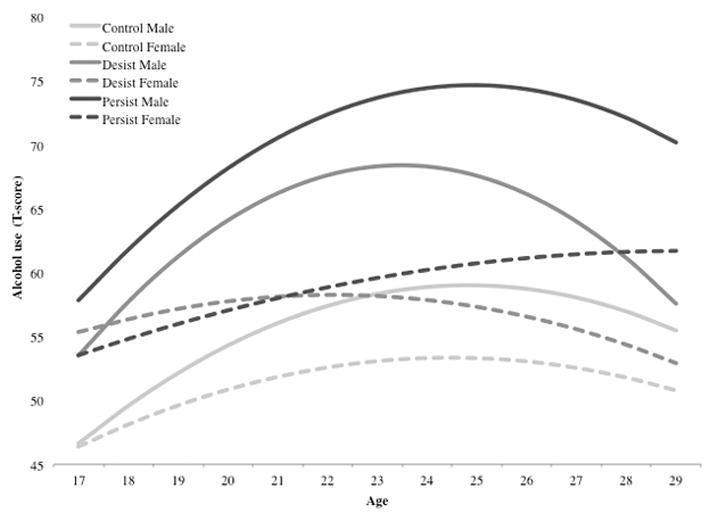
Model Predicted Alcohol Use by Gender and AUD Course Group
Figure 4.
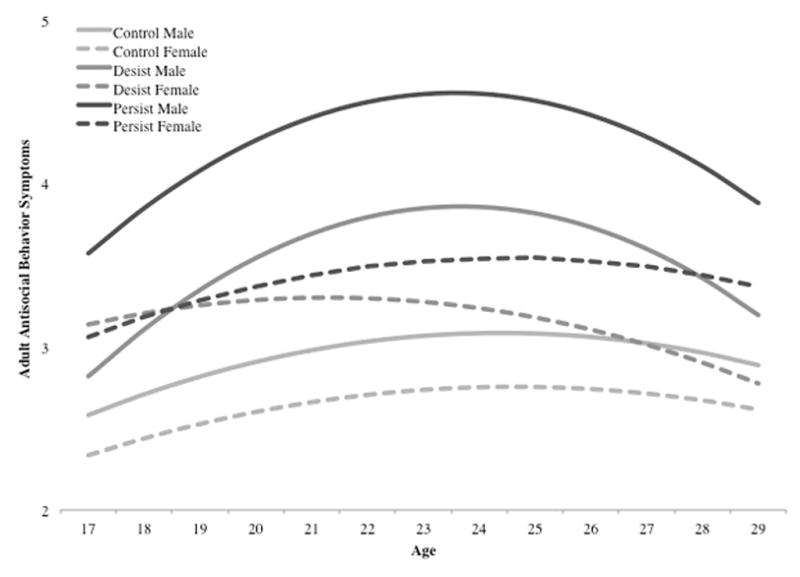
Model Predicted Antisocial Behavior by Gender and AUD Course Group
Results
Alcohol use
Results for the MLM predicting alcohol use are presented in Table 1 along with model-estimated growth plots for mean-level alcohol use from age 17 to age 29 in Figure 1. For the alcohol use composite, the linear effect of age was positive (β = 2.73, p < 0.001) while the quadratic effect of age was negative (β = −0.18, p < 0.001), indicating significant increases followed by significant deceleration in alcohol use from ages 17 to 29. Gender did not predict differences in the alcohol use intercept at age 17 (i.e., intercept, β = 0.45, p > 0.05), but did predict significant linear increases (β = 1.28, p < 0.001) and quadratic deceleration (β = −0.09, p < 0.001) in alcohol use such that men both increased and then decelerated alcohol use at a faster rate than women. AUD chronicity predicted differences in alcohol use at the age 17 intercept, with higher alcohol use detected in the persistent group than the desistent group (β = 3.49, p < 0.001) and in the desistent group relative to the control group (β = 5.69, p < 0.001). The desistent group decelerated alcohol use significantly faster than controls (i.e. negative quadratic age effect; β = −0.02, p < 0.05) but deceleration of alcohol use was similar between the AUD groups (β = 0.02, p > 0.05).
Three significant Gender x AUD chronicity group interactions predicted alcohol use. Persistent-desistent group differences in the intercept were moderated by gender such that persistence produced significantly larger effects on alcohol use for men than women at the age 17 intercept (β = 1.69, p < 0.001). However, desistent-control group differences were similar in men and women at age 17 (β = 0.33, p > 0.05). Subsequent to this initial similarity between desistent and control groups of men and women at age 17, differences in age-related change for these groups were moderated by gender such that men in the desistent group increased (β = 0.63, p < 0.001) and decelerated (β = −0.05, p < 0.001) alcohol use faster than women in the desistent group. By contrast, persistent-desistent differences in age-related increases (β = 0.18, p > 0.05) and deceleration (β = −0.02, p > 0.05) were similar for men and women.
Drug use problems
Results for the MLM model predicting drug use problems are presented in Table 1. The model-estimated growth plots for drug use problems from age 17 to age 29 are presented in Figure 2. Similar to alcohol use, drug use problems initially increased (i.e., positive linear effect) followed by a decrease (i.e., negative quadratic effect) from ages 17 to 29. While no gender differences in the intercept were present for alcohol use, higher levels of drug use problems were observed in women than men at age 17 (β = −2.19, p < 0.001). Despite this initial elevation in drug use problems among women, men went on to exhibit faster age-related increases (β = 1.08, p < 0.001) and deceleration (β = −0.06, p < 0.001) in drug use problems than women. Similar to alcohol use, AUD chronicity differentiated levels of drug use problems at age 17 with more problems reported for the persistent than desistent group (β = 2.06, p < 0.05) as well as more drug use problems among the desistent group relative to the control group (β = 2.71, p < 0.001). Different from alcohol use, drug use problems increased from age 17 to age 29 at a significantly faster rate for the desistent group than the control group (β = 2.22, p < 0.001) and for the persistent group relative to the desistent group (β = 1.98, p < 0.001). Age-related decreases in drug use problems were also faster in the desistent group compared to the control group (β = −0.16, p < 0.001) and also in the persistent group relative to the desistent group (β = −0.13, p < 0.001).
Figure 2.
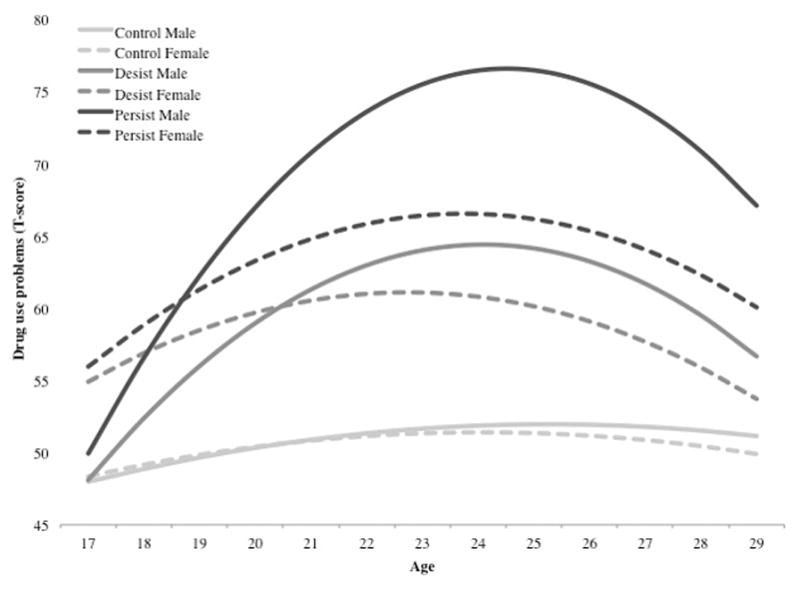
Model Predicted Drug Use Problems by Gender and AUD Course Group
Five significant interactions between gender and AUD chronicity groups predicted drug use problems. First, gender moderated desistent-control group differences in drug use problems at age 17, with larger differences evident for women than men (β = −1.99, p < 0.01). That is, women with a desistent AUD course were uniquely elevated on drug use problems at age 17 while men with a desistent AUD course reported problems at similar rates to their male counterparts without a history of AUD. Despite these initial differences in drug use problems at age 17, desistent-control differences in age-related change were moderated by gender such that the desistent group increased (β = 1.03, p < 0.01) and decelerated (β = −0.06, p < 0.001) in drug use problems faster than desistent women. Additionally, gender moderated persistent-desistent group differences in age-related change, wherein persistent men increased (β = 0.89, p < 0.01) and decelerated (β = −0.06, p < 0.01) drug use problems faster than persistent women.
Symptoms of major depression
Results for the MLM predicting depression symptoms are presented in Table 1 along with model-estimated growth plots for depression symptoms from age 17 to age 29 in Figure 3. In contrast to age effects present in alcohol use and drug use problems, linear and quadratic age effects in depression symptoms were not significant (linear, β = −0.03, p > 0.05; quadratic, β = 0.00, p > 0.05), suggesting that symptoms of depression generally remained stable across the sample from age 17 to age 29. Despite the lack of age-related effects on depression, women reported significantly more symptoms at the age 17 intercept than men (β = −0.28, p < 0.01). Initial similarity between desistent and control groups was followed by faster increases (β = 0.10, p < 0.01) and deceleration (β = −0.01, p < 0.01) in depression for those in the desistent group as compared to controls. While model-predicted increases in depression appeared to accelerate at the fastest rate for persistent women, this increase was not significant.
Figure 3.
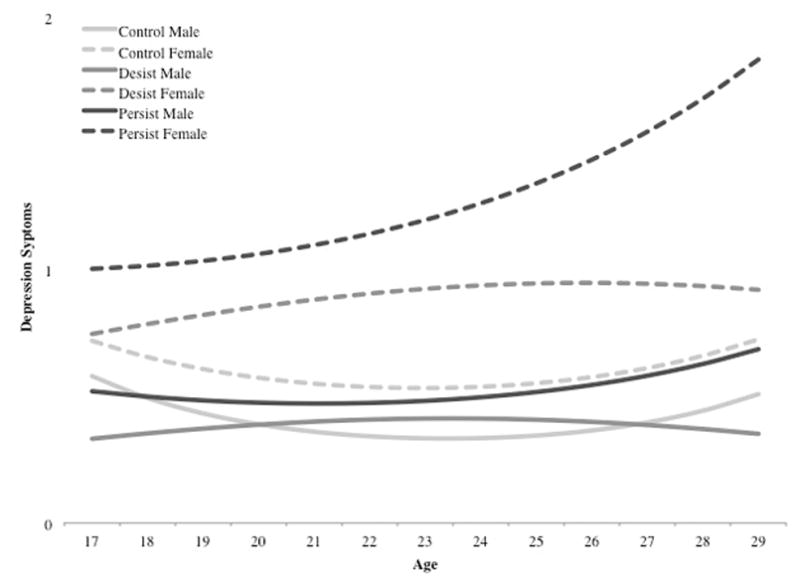
Model Predicted Depression Symptoms by Gender and AUD Course Group
Adult antisocial behavior
Results for the MLM model predicting antisocial behavior are presented in Table 1 along with model-estimated growth plots for antisocial behavior from age 17 to age 29 in Figure 4. As with alcohol use and drug use problems, the linear effect of age on antisocial behavior was positive (β = 0.18, p < 0.001) while the quadratic effect of age was negative (β = −0.01, p < 0.001), indicating an increase followed by a decrease in antisocial behavior from ages 17 to 29. Gender predicted a significant difference in the intercept with more antisocial behavior at age 17 in men than women (β = 0.16, p < 0.05). Despite these initial differences, linear growth and quadratic deceleration in antisocial behavior was similar between genders. Both AUD group contrasts were significant predictors of the intercept, with more antisocial behavior at age 17 detected in the desistent than control group (β = 0.78, p < 0.001) and in the persistent than desistent group (β = 0.54, p < 0.001). A similar pattern was observed for age-related change, with linear increases and quadratic deceleration faster in the desistent (vs. control: linear, β = −0.07, p < 0.01; quadratic, β = 0.003, p < 0.05) and persistent (vs. desistent: linear, β = −0.05, p < 0.01; quadratic, β = 0.004, p < 0.001) groups.
Three significant Gender x AUD chronicity group interactions predicted antisocial behavior. Desistent-control group differences on the intercept and age-related change were moderated by gender with initially more antisocial behavior in men (β = −0.21, p < 0.05), followed by faster linear increases (β = 0.06, p < 0.01) and deceleration (β = −0.003, p < 0.01) in the antisocial behavior of men than women. Gender did not moderate initial differences or age related change in the desistent-persistent contrast, indicating that antisocial behavior between these groups was similar for men and women.
Discussion
The proposed gender risk-severity paradox hypothesized that the developmental consequences of AUD during emerging adulthood would be more profound for women than for men despite typically lower initial levels of alcohol use and AUD risk exposure in women. The present study supported this hypothesis by confirming four key observations. First, proportionally more women than men with AUD exhibited a trajectory of problems in a severe range relative to same-gender controls without a history of AUD. Specifically, persistent AUD in men conferred the fastest increases in absolute levels of problems (except for depression symptoms) of any group tested while persistent and desistent AUD conferred similar levels of psychiatric problems in women. Second, adolescent risk levels were more distinct between persistent and desistent AUD groups of men than women, suggesting that early risk levels may be less clinically informative of subsequent AUD chronicity and severity for women than men. Third, age-related recovery from co-occurring problems was less prominent in women. Consistent with prior research, men with AUD generally recovered their mental health leading up to age 29. Women with AUD, however, did not ostensibly recover their mental health to the same degree as men, even when their AUD symptoms desisted. Moreover, rates of recovery for persistent and desistent groups of women were nearly indistinguishable, suggesting that women may not benefit from desistence to the same degree as men. Fourth, some gender-specific features of AUD group trajectories were evident. Compared to AUD groups of men, AUD groups of women showed significant elevation in drug use problems in adolescence and depression symptoms during the entire developmental period. In particular, women with a persistent course of AUD were notably elevated on depression symptoms relative to controls at each age while men with either AUD course had similarly low levels of depression to male controls. The disruption in normative development linked with AUD for women may confer additional risk for increasing levels of depression through adulthood, especially in cases when AUD persists through this period. While this finding supports prior characterizations of a negative affective typology for AUD in women (Zucker, 1994) and studies of a gender-specific structure of risk for AUD in young adulthood (Foster et al., 2015), it also illustrates that depression may be a unique feature of a chronic course of AUD in women.
Higher rates of AUD prevalence and risk exposure in men than women understandably attract more attention from researchers. Yet, these results provide evidence that mean-levels of risk are an insufficient predictor of the degree of developmental disruption associated with a disorder. In fact, we provided further support for the idea that important clinical differences are occluded by focusing only on the age period or group (i.e., gender) with the highest prevalence (Clark 2004, Clark et al., 1998) or the mean-level of a problem (Foster et al., 2015) without further examination of the degree of deviation from normative development it may represent (e.g., mean-level problem in a target group compared to a matched control).
From a developmental-contextual perspective (Nurmi, 1993; Plomin et al., 1977; Scarr & McCartney, 1983), the stability, acceleration, and/or desistence of psychiatric problems during the transition to adulthood likely reflects the dynamic interaction between a person’s existing attributes (e.g., AUD) and the broader context that promotes or constrains specific determinants of these problems (e.g., biological and social variation in alcohol consequences by sex and gender). For women in the present study, AUD not only began with risks for alcohol problems already apparent by adolescence (i.e., cross-domain differences between women in the non-AUD control group and women in either of the AUD groups) but also occurred in the broader context where these levels constitute a more profound violation of their gender role norm (Beckman & Amaro, 1986; Gomberg, 1981, 1988). By contrast, AUD for men in the present study was associated with early heavy alcohol use but relatively few early deviations from the non-AUD control group in other domains and occurred in the broader context of more permissive social attitudes toward deviant behavior in men. Consequently, women may be less predisposed to drink at the level of men but those with uniquely high levels of problems may be subjected to a gender-specific context with its own problematic effects on the trajectory of their mental health.
An apparent homogeneity in women with these early risks obscured differentiation between women who would later develop a chronic course of AUD and those who would remit by adulthood. Subsequent deviation from the normative trajectory of same-sex peers may follow from a diverse array of consequences of heavy alcohol use during adolescence and cascade into producing longer term effects across a broader set of functional domains (Erol & Karpyak, 2015; Grant, LaBrie, Hummer, & Lac, 2012; Hommer, Momenan, Kaiser, & Rawlings, 2001; Mann et al., 2005; Niaura, Nathan, Frankenstein, Shapiro, & Brick, 1987; Nolen-Hoeksema, 2004; Stockwell et al., 2002). For instance, early elevation in antisocial behavior is known to have a more potent effect on the AUD outcome in women compared to men (Foster et al., 2015) and may also pose gender-specific consequences for women’s engagement and perceived success in her broader developmental context (e.g., increasing alienation and punitive social sanctions from peers in college and/or the workforce and decreasing the likelihood of securing a marital relationship or having children) that may have a lasting influence on AUD symptoms and their remission in addition to well-being more generally.
Despite the higher absolute levels of alcohol use among men during emerging adulthood, proportionally more women with AUD exhibited atypical problems for their gender while problems varied significantly more in men based on the chronicity of their AUD. Our results further illustrate that key features of the extant typologies for AUD do not have uniform utility across men and women, necessitating future work that develops gender-specific typologies for AUD in women. Though women exhibit lower levels of alcohol use, develop AUD less often, and are less likely to have high levels of initial risks for AUD like antisocial behavior, our results suggest that they AUD may lead to a greater accrual of problems through young adulthood for women than men when compared to age and gender-matched controls.
Despite the numerous strengths of our approach, several limitations are evident. Given the person-centered framework used, it is important to caution that these results are not intended to measure AUD course effects on the problems measured (or vice versa). Chronic AUD symptoms could interfere with the development of vital competencies that undergird adult mental health, early and persistent psychiatric problems could drive AUD chronicity, or these problems may aggregate within individuals as a result of an unmeasured factor determined earlier in development. Despite these challenges common to longitudinal AUD research, we contribute to knowledge of how developmental change in the network of co-occurring phenomena may be moderated by gender and the course AUD takes during emerging adulthood. Second, while our predominately European-American sample was representative of the broader Minnesota region at the time of sample ascertainment, replication of these effects in more diverse populations is necessary to determine if results generalize beyond this ancestry group. Third, the small size of the female persistent group somewhat reduced power to detect significant differences between this group and others. Finally, multiple statistical comparisons were used to test our hypothesis. While this is not ideal, effects were interpreted both within and across domains rather than relying on single tests of significance.
Despite its limitations, this study uniquely evaluated the extent to which AUD chronicity differentiated the trajectories of problems in women and men during emerging adulthood. Notable strengths are the full coverage of the emerging adult period characterized by significant change in AUD and co-morbid problems, the consideration of both between- and within-gender effects (i.e., comparison to a same-gender control group), tests of the hypothesis across multiple domains to evaluate converging evidence, and the use of a developmental framework and an analytic model designed to estimate effects at multiple levels of the nested data (i.e., in prediction of mean-differences and age-effects). Use of this approach provided new insights regarding unique clinical features of AUD severity in men and women transitioning to adulthood. These findings have direct utility for effectively tailoring treatment plans to key developmental and gender-specific inflection points in co-morbid problems associated with AUD and for understanding gender differences in co-developing processes in emerging adulthood. Specifically, women are generally more likely to desist from problem alcohol use but the remission of AUD and its co-occurring problems may be slower than for men, even after AUD symptoms ostensibly remit. Though heavy alcohol use may be less prevalent and more stigmatized in women than men, AUD may be paradoxically overlooked as less severe in women than men. Unless clinicians and researchers take this gender-specific paradox for AUD into account carefully, it is likely that the accessibility and quality of AUD care for women and the generalizability of AUD research for women will be profoundly diminished. Future work in this area should continue to utilize a person-centered framework to determine how developmental-contextual factors related to biological maturation and environmental selection modulate the severity of AUD.
Acknowledgments
This research was supported by United States Public Health Service grants F31 AA023121 (Foster) and R01 AA009367 (McGue) from the National Institute on Alcohol Abuse and Alcoholism and R37 DA005147 (Iacono), R01 DA034606 (Hicks), and R01 DA039112 (Durbin) from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors have no conflicts of interest to report
References
- Acker C. Neuropsychological Deficits in Alcoholics: the relative contributions of gender and drinking history. Addiction. 1986a;81(3):395–403. doi: 10.1111/j.1360-0443.1986.tb00346.x. [DOI] [PubMed] [Google Scholar]
- Acker C. Neuropsychological deficits in alcoholics: The relative contributions of gender and drinking history. British Journal of Addiction. 1986b;81:395–403. doi: 10.1111/j.1360-0443.1986.tb00346.x. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55(5):469–480. doi: 10.1037//0003-066X.55.5.469. [DOI] [PubMed] [Google Scholar]
- Babor T, Hofmann M, Delboca F, Hesselbrock V, Meyer R, Dolinksky Z, Rounsaville B. Types of Alcoholoics. 1. Evidence for an empirically derived typology base on indicators of vulnerability and severity. Archives of General Psychiatry. 1992;49(8):599–608. doi: 10.1001/archpsyc.1992.01820080007002. [DOI] [PubMed] [Google Scholar]
- Beckman LJ, Amaro H. Personal and social difficulties faced by women and men entering alcoholism treatment. Journal of Studies on Alcohol. 1986;47(2):135–145. doi: 10.15288/jsa.1986.47.135. [DOI] [PubMed] [Google Scholar]
- Chassin L, Flora D, King K. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: the effect of familial alcoholism and personality. Journal of Abnormal Psychology. 2004;113:483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Chen K, Kandel DB. The natural history of drug use from adolescence to the mid-thirties in a general population sample. American Journal of Public Health. 1995;85(1):41–47. doi: 10.2105/AJPH.85.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DB. The natural history of adolescent alcohol use disorders. Addiction. 2004;99:5–22. doi: 10.1111/j.1360-0443.2004.00851.x. [DOI] [PubMed] [Google Scholar]
- Clark DB, Kirisci L, Tarter RE. Adolescent versus adult onset and the development of substance use disorders in males. Drug and Alcohol Dependence. 1998;49(2):115–121. doi: 10.1016/S0376-8716(97)00154-3. [DOI] [PubMed] [Google Scholar]
- Cloninger CR. Neurogenetic adaptive mechanisms in alcoholism. Science. 1987;236(4800):410–416. doi: 10.1126/science.2882604. [DOI] [PubMed] [Google Scholar]
- Cottler L, Robins L, Helzer J. The Reliability of the CIDI-SAM: a comprehensive substance abuse interview. Addiction. 1989;84(7):801–814. doi: 10.1111/j.1360-0443.1989.tb03060.x. [DOI] [PubMed] [Google Scholar]
- Cranford JA, Nolen-hoeksema S, Zucker RA. Alcohol involvement as a function of co-occurring alcohol use disorders and major depressive episode: Evidence from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2011;117(2–3):145–151. doi: 10.1016/j.drugalcdep.2011.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JI, Porjesz B, Schuckit MA, Reich T, Bierut LJ. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: an evaluation after 5 years. Archives of General Psychiatry. 2005;62(7):753–760. doi: 10.1001/archpsyc.62.7.753. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, King SM, McGue M, Iacono WG. Personality traits and the development of nicotine, alcohol, and illicit drug disorders: Prospective links from adolescence to young adulthood. Journal of Abnormal Psychology. 2006;115(1):26–39. doi: 10.1037/0021-843X.115.1.26. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Archives of General Psychiatry. 2007;64(10):1145–52. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Malone S, Iacono WG. The effect of parental alcohol and drug disorders on adolescent personality. The American Journal of Psychiatry. 2004;161(4):670–6. doi: 10.1176/appi.ajp.161.4.670. [DOI] [PubMed] [Google Scholar]
- Erol A, Karpyak VM. Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug and Alcohol Dependence. 2015 doi: 10.1016/j.drugalcdep.2015.08.023. [DOI] [PubMed]
- Foster KT, Hicks BM, Iacono W, McGue M. Alcohol Use Disorder in Women: Risks and Consequences of an Adolescent Onset and Persistent Course. Psychology of Addictive Behaviors. 2014;28(1) doi: 10.1037/a0035488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster KT, Hicks B, Iacono W, McGue M. Gender differences in the structure of risk for alcohol use disorder in adolescence and young adulthood. Psychological Medicine. 2015:1–12. doi: 10.1017/S0033291715001014. [DOI] [PMC free article] [PubMed]
- Gomberg E. Women, sex roles, and alcohol problems. Professional Psychology. 1981 doi: 10.1037/0735-7028.12.1.146. [DOI]
- Gomberg E. Alcoholic women in treatment: the question of stigma and age. Alcohol and Alcoholism. 1988;23(6):507–14. doi: 10.1093/oxfordjournals.alcalc.a044852. [DOI] [PubMed] [Google Scholar]
- Granic I, Hollenstein T. Dynamic systems methods for models of developmental psychopathology. Development and Psychopathology. 2017;15:641–669. doi: 10.1017/s0954579403000324. http://doi.org/10.1017.S0954579403000324. [DOI] [PubMed] [Google Scholar]
- Granic I, Patterson GR. Toward a comprehensive model of antisocial development: a dynamic systems approach. Psychological Review. 2006;113(1):101–31. doi: 10.1037/0033-295X.113.1.101. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS. Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72(8):757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant J. Women and drugs: A feminist perspective. Advancing critical criminology: Theory and application. 2006:179–198. [Google Scholar]
- Grant S, LaBrie JW, Hummer JF, Lac A. How drunk am I? Misperceiving one’s level of intoxication in the college drinking environment. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors. 2012;26(1):51–8. doi: 10.1037/a0023942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF. Women and alcohol use disorders. Harvard Review of Psychiatry. 2002;10(2):76–85. doi: 10.1080/10673220216212. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability–transactional stress theory. Psychological Bulletin. 2001;127(6):773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychological Bulletin. 1992;112(1):64–105. doi: 10.1037/0033-2909.112.1.64. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/1529040. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Iacono WG, Mcgue M. Consequences of an Adolescent Onset and Persistent Course of Alcohol Dependence in Men: Adolescent Risk Factors and Adult Outcomes. Alcoholism: Clinical & Experimental Research. 2010;34(5):819–833. doi: 10.1111/j.1530-0277.2010.01154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hommer D, Momenan R, Kaiser E, Rawlings R. Evidence for a gender-related effect of alcoholism on brain volumes. The American Journal of Psychiatry. 2001;158(2):198–204. doi: 10.1176/appi.ajp.158.2.198. [DOI] [PubMed] [Google Scholar]
- Huselid RF, Cooper ML. Gender roles as mediators of sex differences in adolescent alcohol use and abuse. Journal of Health and Social Behavior. 1992;33(4):348. doi: 10.2307/2137313. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-use disorders: findings from the Minnesota Twin Family Study. Development and Psychopathology. 1999;11(4):869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Malone S, McGue M. Behavioral disinhibition and the development of early-onset addiction: common and specific influences. Annual Review of Clinical Psychology. 2008;4:325–48. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG. National Survey Results on Drug Use from the Monitoring the Future Study, 1975–2001, I. Secondary School Students. Rockville, MD: National Institute on Drug Abuse; 2001. [Google Scholar]
- Johnstone B, Leino E, Ager C, Ferrer H, Fillmore K. Determinants of life-course variation in the frequency of alcohol consumption: meta-analysis of studies from the Collaborative Alcohol-Related Longitudinal Project. Journal of Studies on Alcohol. 1996;57:494–506. doi: 10.15288/jsa.1996.57.494. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60(9):929–37. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Grant BF, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug and Alcohol Dependence. 2008;93(1–2):21–9. doi: 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111(3):411–424. doi: 10.1037//0021-843X.111.3.411. [DOI] [PubMed] [Google Scholar]
- Leggio L, Kenna GA, Fenton M, Bonenfant E, Swift RM. Typologies of alcohol dependence. From Jellinek to genetics and beyond. Neuropsychology Review. 2009;19(1):115–29. doi: 10.1007/s11065-008-9080-z. [DOI] [PubMed] [Google Scholar]
- Mann K, Ackermann K, Croissant B, Mundle G, Nakovics H, Diehl A. Neuroimaging of Gender Differences in Alcohol Dependence: Are Women More Vulnerable? Alcoholism: Clinical & Experimental Research. 2005;29(5):896–901. doi: 10.1097/01.ALC.0000164376.69978.6B. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Development and Psychopathology. 2001;13(2):355–75. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Moss HB, Chen CM, Yi H. Subtypes of alcohol dependence in a nationally representative sample. Drug and Alcohol Dependence. 2007;91(2–3):149–58. doi: 10.1016/j.drugalcdep.2007.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niaura RS, Nathan PE, Frankenstein W, Shapiro AP, Brick J. Gender differences in acute psychomotor, cognitive, and pharmacokinetic response to alcohol. Addictive Behaviors. 1987;12(4):345–56. doi: 10.1016/0306-4603(87)90048-7. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Nurmi JE. Adolescent Development in an Age-graded Context: The Role of Personal Beliefs, Goals, and Strategies in the Tackling of Developmental Tasks and Standards. International Journal of Behavioral Development. 1993;16(2):169–189. doi: 10.1177/016502549301600205. [DOI] [Google Scholar]
- Patterson GR, Yoerger K. A developmental model for late-onset delinquency. In: Osgood DW, editor. Motivation and delinquency. Lincoln, NE: University of Nebraska Press; 1997. [PubMed] [Google Scholar]
- Plomin R, DeFries JC, Loehlin JC. Genotype-environment interaction and correlation in the analysis of human behavior. Psychological Bulletin. 1977;84(2):309–322. [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–33. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Robins L, Wing J, Wittchen H, Helzer J, Babor T, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA, Sartorius N, Towle L. The Composite International Diagnostic Interview - An Epidemiologic Instrument Suitable for Use in Conjunction with Different Diagnostic Systems and in Different Cultures. Archives of General Psychiatry. 1988;45(12):1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Rutledge P, Sher K. Heavy drinking from the freshman year into early young adulthood: The roles of stress, tension-reduction drinking motives, gender and personality. Journal of Studies on Alcohol. 2001;62(4):457–466. doi: 10.15288/jsa.2001.62.457. [DOI] [PubMed] [Google Scholar]
- Scarr S, McCartney K. How people make their own environments: A theory of genotype (leading to) environment effects. Child Development. 1983;54(2):424–435. doi: 10.2307/1129703. [DOI] [PubMed] [Google Scholar]
- Schulenberg J, Maggs JL. A Developmental Perspective on Alcohol Use and Heavy Drinking during Adolescence and the Transition to Young Adulthood. Journal of Studies on Alcohol and Drugs. 2002;14(14 Supp):54–70. doi: 10.15288/jsas.2002.s14.54. Retrieved from http://www.jsad.com.proxy.lib.umich.edu/doi/pdf/10.15288/jsas.2002.s14.54. [DOI] [PubMed] [Google Scholar]
- Schulenberg J, O’Malley PM, Bachman JG, Johnston LD. “Spread Your Wings and Fly”: The Course of Well-Being and Substance Use During the Transition to Young Adulthood. In: Crockett Lisa J, Silbereisen Rainer K., editors. Negotiating Adolescence in Times of Social Change. New York: Cambridge Univ Press; 2000. pp. 224–255. [Google Scholar]
- Sherrod LR, Haggerty RJ, Featherman DL. Introduction: Late Adolescence and the Transition to Adulthood. Journal of Research on Adolescence. 1993:217–226. doi: 10.1111/1532-7795.ep11301463. [DOI]
- Stockwell T, McLeod R, Stevens M, Phillips M, Webb M, Jelinek G. Alcohol consumption, setting, gender and activity as predictors of injury: a population-based case-control study. Journal of Studies on Alcohol. 2002;63(3):372–9. doi: 10.15288/jsa.2002.63.372. [DOI] [PubMed] [Google Scholar]
- Wilsnack SC, Wilsnack RW, Kantor LW. Focus on: women and the costs of alcohol use. Alcohol Research: Current Reviews. 2013;35(2):219–28. doi: 10.1016/j.drugalcdep.2014.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M, Scheidt DM. Alcoholic subtypes: are two sufficient? Addiction. 2004;99(12):1508–19. doi: 10.1111/j.1360-0443.2004.00878.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Dept. of Substance. Global Status Report on Alcohol. 2004 Retrieved from http://www.who.int/iris/handle/10665/42971.
- Zucker RA. Pathways to alcohol problems and alcoholism: A developmental account of the evidence for multiple alcoholisms and for contextual contributions to risk. In: Zucker RA, Boyd GM, Howard J, editors. The Developmental of Alcohol Problems: Exploring the Biopsychosocial Matrix of Risk. Department of Health and Human Services; 1994. pp. 255–289. NIAAA Research Monograph 26. [Google Scholar]


