Abstract
Background:
Tibial tuberosity-trochlear groove distance (TT-TGD) measurements play a decisive role in evaluating patellofemoral joint disorders. However, the prevalence of pathological TT-TGD among patients with patellofemoral pain remains unclear. The purpose of this study was to compare the size of TT-TGD among patients with patellofemoral pain syndrome (PFPS) and those with no history of patellofemoral pain.
Methods:
A total of 100 cases participated in this case-control study, among whom 53 individuals were in the case group and 47 individuals were in the control group. TT-TGD was measured by magnetic resonance imaging.
Results:
The mean TT-TGD was 12.3±3.3 in patients and 9.3±2.4 in controls (P<0.001). Among patients, we had totally 34 patients with TT-TG equal or lower than 13 (64.2%) and in 18 patients, it was higher than 13 (34%).
Conclusion:
The mean TT-TGD in patients with PFPS was greater than that in the control group (P=0.001). An increase in TT-TGD can be considered one of the factors behind the development of PFPS.
Key Words: Chondromalacia patellae, MRI, Patellofemoral pain, Tibial tuberosity-trochlear groove distance
Introduction
Patellofemoral pain syndrome (PFPS) is one of the most common diseases in musculoskeletal system. The patient often complains of pain in the anterior knee region, which is aggravated by ascending and descending the stairs or keeping the knee bent for a long time. Various names have been proposed to describe this disorder, most notably chondromalacia patella and anterior knee pain syndrome. A significant number of these patients experience frequent episodes of recurrence. Some patients also experience chronic and resistant pain in case of conservative therapy, which can interfere with daily activities (1).
There are several theories about the multifactorial causes of PFPS. Malalignment in the lower extremity is one of the most commonly believed etiologies for this disorder. Abnormal patellar tracking increases the pressure in the area of subchondral bone and causes pain. In addition, quadriceps muscle weakness, especially vastus medialis obliqus, can be effective in creating PFPS through applying dynamic imbalance in knee extensor mechanism. Unfortunately, the underlying factors in the development of this disorder have not yet been well known (2).
Tibial tuberosity-trochlear groove distance (TT-TGD) measurements play a decisive role in evaluating patellofemoral joint disorders. The increase in the distance indirectly indicates lateral pull increase in the knee extensor mechanism (3). The exact measurement of this parameter is possible through both CT scan and MRI. However, MRI is superior to CT scan in the examination of articular cartilage and soft tissue component (4). The normal values defined for the TT-TGD vary considerably (3, 5). A TT-TGD of more than 20 mm in CT scan is considered pathological and tibial tuberosity osteotomy (TTO) has been suggested for these cases by some studies (5-7). It has been shown that the TT-TGD value is 3 to 4 mm less in MRI measurements compared to CT scan. Hence, TT-TGD values of more than 15 mm in MRI are suggested to be regarded as pathological (8, 9).
Several studies have shown that TT-TGD has increased in patients with recurrent patellar dislocation without a history of trauma. Accordingly, in case of patellar instability, TTO is performed routinely to correct the tibial tuberosity malposition. Although TTO has been proposed to relieve pain in patients with PFPS, factors affecting the disease are not well known yet (10-17).
The purpose of this study was to compare the size of TT-TGD among patients with PFPS and those with no history of patellofemoral pain. We assumed that the mean TT-TGD in patients with PFPS was higher compared to the painless control group.
Materials and Methods
This prospective case-control study measured TT-TGD in patients with isolated patellofemoral pain syndrome referring to radiology and orthopedic departments of Shariati Hospital (affiliated to Tehran University of Medical Sciences). A total of 100 cases participated were divided into case (n=53) and control (n=47) groups.
The participants in case group were selected from those with bone maturity (growth plate closure) and complain of pain in patellofemoral region for at least 6 months. However, patients were excluded from the study in cases of a history of major knee injury within the last six months, clinical or radiological diagnosis of osteoarthritis, inflammation of the patellar tendon, bursitis or fat pad syndrome, fracture, history of knee surgery or arthroscopy, obvious ligament or meniscus injury, cartilage injury, fluid accumulation in the joint and arthritis.
Patients in the control group were selected from those who experienced knee trauma and were referred due to knee pain; however, there was no evidence of obvious instability of patella or knee in any of the anteroposterior, axial, and coronal plans in their clinical examination and a knee surgeon has recommended MRI in order to diagnose their clinical complaints. MRI was mostly performed on the patients with suspicion of minor meniscal tear or other minor knee injuries assuming that such minor injuries do not result in the changes in TT-TGD. Moreover, there should be no significant issue on the patients’ MRI.
PFPS diagnosis in the patient group was confirmed based on the clinical history and examination by a knee surgeon. After obtaining the participant’s consent, information on age, gender, weight, height, and body mass index (BMI) were recorded. In addition, a visual analogue scale (VAS) was used to determine pain severity during the day.
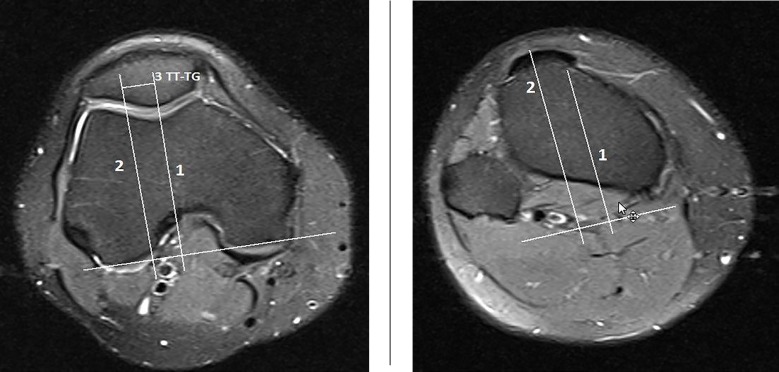
MRI was performed in both control and case groups using a Siemens 1.5-T Avanto with a knee coil. The MRI protocol included sagittal, coronal, and axial PD fat sat, as well as T1WI coronal and axial and T2WI sagittal images. The images were examined by a professional radiologist in terms of the presence or absence of knee and ligament injuries and arthritis. TT-TGD was measured according to the standard methodology. A vertical line was first drawn from the trochlear groove depth to the posterior condylar line at the axial cross section on the femoral condyles (which passed through in parallel and tangent to the posterior of femoral condyles) in order to measure TT-TGD [Figure 1, line 1]. Then, another vertical line, transferring to the lower axial sections of the above-mentioned lines, was drawn from the anterior-most and most prominent point of the tibial tuberosity at the middle region of the joint of patella tendon, [Figure 1, line 2], and the distance between the two lines perpendicular to the tibial tuberosity and trochlear groove was measured [Figure 1, line 3]. This line indicates the TT-TGD.
Figure 1.
axial image of knee joint at distal femur.note to posterior line was drawn at posterior border of condyles of femur. there is a vertical line at trochlear groove and the other parallel line along the tibial tuberosity that transfered to this level and distance between two lines indicate TT-TG
Data was analyzed using SPSS 22 (Chicago, IL, USA). The Kolmogorov-Smirnov test was used to examine the normality of the values. The student t-test and U-Mann-Whitney were used to compare the two groups accordingly. Pearson’s and Spearman’s correlation coefficients were also used to examine the relationship between variables.
Regression analysis was used to provide a linear model. In addition, TT-TGD was randomly re-measured in 20 cases for intraobserver variability. However, they did not differ significantly from those measured earlier.
Results
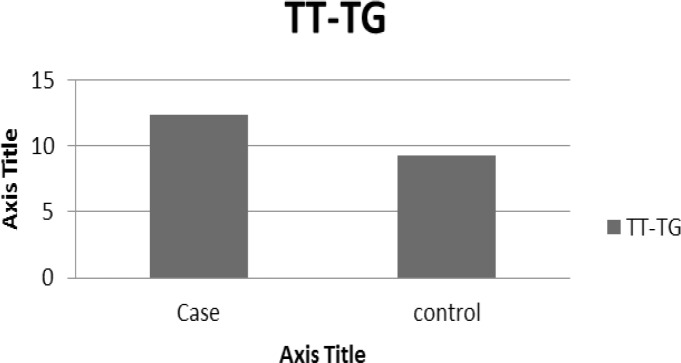
A total of 100 subjects (53 cases and 47 controls were) enrolled in the study. The mean age among patients and controls were 35.2±7 and 31.9±8.1 years, respectively (P=0.035). The mean weight was 73.2±14.2 Kg in patients and 73.7±11.1 Kg in controls (P=0.84). The mean BMI was 25.4±4.8 in patients and 24.1±4.1 in controls (P=0.14) [Table 1]. The mean TT-TGD was 12.3±3.3 mm (range: 3-20) in patients and 9.3±2.4 mm (range: 3-13) in controls (P<0.001) [Chart 1].
Table 1.
Comparison of Age, Anthropometric Data and TT-TG between Patients and Controls
| GROUP | MEAN | P-VALUE |
|---|---|---|
| AGE | ||
| CASE CONTROL | 35.2+-7 31.9+-8.1 |
0.035 |
| HEIGHT | ||
| CASE CONTROL | 170.1+-9.1 175.4+-7.3 |
0.007 |
| WEIGHT | ||
| CASE CONTROL | 73.2+-14.2 73.7+-11.1 |
0.84 |
| BMI | ||
| CASE CONTROL | 25.4+-4.8 24.1+-4.1 |
0.14 |
| TT-TGD | ||
| CASE CONTROL | 12.3+-3.3 9.3+-2.4 |
<0.001 |
Chart 1.
TT-TG:Tibial tuberosity trochlear groove distance
The TT-TGD was ≤13 mm in 34 patients (64.2%) and >13 mm in 18 patients (34%) (the TT-TGD value in one patient was missing). Among 18 patients with TT-TGD>13 mm, the TT-TGD was ≤18 mm in 16 patients (30.2%) and two patients showed TT-TGD=20 mm (3.8%). Also, the TT-TGD was ≤10 mm in 35 controls and between 11-13 mm in 12 others (25.5%). The TT-TGD was 13 mm in 5 patients (10.6%) (P<0.001).
The correlation coefficients between BMI and TT-TGD in patients and controls were -0.14 and -0.10, respectively (both Ps>0.32). In addition, the correlation coefficients between TT-TGD and height as well as weight and BMI were not significant between the patient and control groups.
The regression coefficient for linear model considering the TT-TGD and age and BMI was < 0.1 and non-significant. The mean VAS in patients was 8.7±1.1 (7-10). Correlation coefficient of VAS with TT-TGD was 0.18 (P=0.18).
Discussion
Several anatomical risk factor may play role in development of PFPS.an increased TT-TGD is known as a risk factor for patellofemoral instability (3, 4, 7, 10, 12). Displacement of the tibial tuberosity toward the lateral side increase contact pressure in patellofemoral joint and causes pain (2, 18). on this basis we think that the increase of TT-TGD can be considered one of the factor causing PFPS. our study showed that the mean TT-TGD in the group of patients is more than that of the healthy group (18).
One of the weaknesses of this study was that the control group was not composed of healthy people. another limitation of our study was that our mri unit didn’t have three dimensional software and capability to overlap the selected image from distal femur at trochlear groove on proximal tibial tuberosity .therefor ,its better to use three dimensional mri to measure TT-TGD more precisely.
In a study recently conducted by Carlson et al, TT-TGD was measured in patients with PFPS by MRI. In this study, the mean TT-TGD was higher in the patients group than in the control group. Also, 30% of the patient group had TT-TGD higher than 15 mm (19).
In another study conducted by Wittstein et al with the aid of MRI, it was shown that TT-TGD in the PFPS group was higher than that of the healthy group. The findings were consistent with our study results. However, the main problem of the study was that it was done with a small sample size (20).
In an older study by Jones et al, TT-TGD was measured in patients with PFPS by CT scan. In this study, TT-TGD was significantly higher in the patients group than in the control group (21). Although the study was performed using CT scan, the mean TT-TGD in the healthy control group was 9.29 mm, which was similar to our study. The main problem with the previous study was that patients with patellar instability were not excluded from the study. In other studies by MRI, the mean TT-TGD in healthy subjects and adults was reported 10±1, which is slightly higher than the mean TT-TGD in our study (8, 9).
Conservative treatment often improves patellar tracking and reduces pain by balancing knee posture. However, some patients do not respond to the treatment. According to the findings of this study and previous studies an increase in TT-TGD might justify part of the PFPS-resistant cases (19-21). TTO is one of the most commonly used treatments for patellar instability; however, its effectiveness in the treatment of PFPS is unclear yet. Some studies have reported excellent results after TTOs in PFPS (14, 15). However, several other studies have reported that the results of the TTO of PFPS are not satisfactory (22-24). Based on the studies conducted using MRI, a TT-TGD higher than 15 mm can be considered a threshold to perform TTO (7, 19, 25, 26). TTO may help in improving the pain in these patients by creating a balance in the extensor mechanism of the knee although there is currently a lack of evidence to perform TTO in all patients with increased TT-TGD. In addition, in case of overcorrection towards medial side during surgery, an increased pain can be expected (18). Therefore, the presence of TT-TGD of more than 15 in MRI for performing TTO in all cases of PFPS is not sufficient (8, 9, 19). According to the findings of this study, we cannot offer optimal cut-off value to perform TTO on patients with resistant PFPS.
We propose that increased TT-TGD should be considered as one of the factors influencing the development of PFPS. To the best of our knowledge, there are few studies comparing TT-TGD between healthy people and those with PFPS, thus more studies are needed to determine the prevalence of tibial tuberosity lateralization among people with PFPS. Considering the advantages of MRI in detecting cartilage lesions and soft tissue, the use of this diagnostic modality instead of CT scan to measure TT-TGD is recommended.
Another issue that needs to be addressed is that TT-TGD is not a definite parameter and its values change in the knee range of motion. Previous studies have shown that the TT-TGD value changes during knee flexion (27, 28). Therefore, there is a need for future studies to measure TT-TGD in varying degrees of knee flexion, among patients with PFPS.
The mean TT-TGD in patients with PFPS was greater than that in the control group. An increase in TT-TGD can be considered as one of the factors behind the development of PFPS; therefore, TT-TGD measurement using MRI should be performed as part of the evaluation of PFPS-resistant cases.
Acknowledgements
The authors thank Dr. Majid Shakiba from the diagnostic and interventional research center (Tehran University of Medical Sciences) for data analysis.
References
- 1.Crossley KM, Stefanik JJ, Selfe J, Collins NJ, Davis IS, Powers CM, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med. 2016;50(14):839–43. doi: 10.1136/bjsports-2016-096384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Powers CM, Bolgla LA, Callaghan MJ, Collins N, Sheehan FT. Patellofemoral pain: proximal, distal, and local factors, 2nd International Research Retreat. J Orthop Sports Phys Ther. 2012;42(6):A1–54. doi: 10.2519/jospt.2012.0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dietrich TJ, Fucentese SF, Pfirrmann CW. Imaging of individual anatomical risk factors for patellar instability. Semin Musculoskelet Radiol. 2016;20(1):65–73. doi: 10.1055/s-0036-1579675. [DOI] [PubMed] [Google Scholar]
- 4.Berruto M, Ferrua P, Carimati G, Uboldi F, Gala L. Patellofemoral instability: classification and imaging. Joints. 2013;1(2):7–14. [PMC free article] [PubMed] [Google Scholar]
- 5.Alemparte J, Ekdahl M, Burnier L, Hernández R, Cardemil A, Cielo R, et al. Patellofemoral evaluation with radiographs and computed tomography scans in 60 knees of asymptomatic subjects. Arthroscopy. 2007;23(2):170–7. doi: 10.1016/j.arthro.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 6.Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2007;15(1):39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 7.Balcarek P, Jung K, Frosch KH, Sturmer KM. Value of the tibial tuberosity- trochlear groove distance in patellar instability in the young athlete. Am J Sports Med. 2011;39(8):1756–61. doi: 10.1177/0363546511404883. [DOI] [PubMed] [Google Scholar]
- 8.Pandit S, Frampton C, Stoddart J, Lynskey T. Magnetic resonance imaging assessment of tibial tuberosity-trochlear groove distance: normal values for males and females. Int Orthop. 35(12):1799–803. doi: 10.1007/s00264-011-1240-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ho CP, James EW, Surowiec RK, Gatlin CC, Ellman MB, Cram TR, et al. Technique-dependent differences in CT versus MRI measurement of the tibial tubercletrochlear groove distance. Am J Sports Med. 2015;43(3):675–82. doi: 10.1177/0363546514563690. [DOI] [PubMed] [Google Scholar]
- 10.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 11.Steensen RN, Bentley JC, Trinh TQ, Backes JR, Wiltfong RE. The prevalence and combined prevalences of anatomic factors associated with recurrent patellar dislocation: a magnetic resonance imaging study. Am J Sports Med. 2015;43(4):921–7. doi: 10.1177/0363546514563904. [DOI] [PubMed] [Google Scholar]
- 12.Tse MS, Lie CW, Pan NY, Chan CH, Chow HL, Chan WL. Tibial tuberosity-trochlear groove distance in Chinese patients with or without recurrent patellar dislocation. J Orthop Surg (Hong Kong) 2015;23(2):180–1. doi: 10.1177/230949901502300212. [DOI] [PubMed] [Google Scholar]
- 13.Fulkerson JP. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res. 1983;177(1):176–81. [PubMed] [Google Scholar]
- 14.Tigchelaar S, van Essen P, Benard M, Koeter S, Wymenga A. A self-centring osteotomy of the tibial tubercle for patellar maltracking or instability: results with ten-years’ follow-up. Bone Joint J. 2015;97(3):329–36. doi: 10.1302/0301-620X.97B3.34515. [DOI] [PubMed] [Google Scholar]
- 15.Rillmann P, Oswald A, Holzach P, Ryf C. Fulkerson’s modified Elmslie-Trillat procedure for objective patellar instability and patellofemoral pain syndrome. Swiss Surg. 2000;6(6):328–34. doi: 10.1024/1023-9332.6.6.328. [DOI] [PubMed] [Google Scholar]
- 16.Bellemans J, Cauwenberghs F, Witvrouw E, Brys P, Victor J. Anteromedial tibial tubercle transfer in patients with chronic anterior knee pain and a subluxation-type patellar malalignment. Am J Sports Med. 1997;25(3):375–81. doi: 10.1177/036354659702500318. [DOI] [PubMed] [Google Scholar]
- 17.Lund F, Nilsson BE. Anterior displacement of the tibial tuberosity in chondromalacia patellae. Acta Orthop Scand. 1980;51(4):679–88. doi: 10.3109/17453678008990861. [DOI] [PubMed] [Google Scholar]
- 18.Stephen JM, Lumpaopong P, Dodds AL, Williams A, Amis AA. The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am J Sports Med. 2015;43(1):186–94. doi: 10.1177/0363546514554553. [DOI] [PubMed] [Google Scholar]
- 19.Carlson VR, Boden BP, Shen A, Jackson JN, Yao L, Sheehan FT. The tibial tubercle-trochlear groove distance is greater in patients with patellofemoral pain: implications for the origin of pain and clinical interventions. Am J Sports Med. 2017;45(5):1110–6. doi: 10.1177/0363546516681002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wittstein JR, Bartlett EC, Easterbrook J, Byrd JC. Magnetic resonance imaging evaluation of patellofemoral malalignment. Arthroscopy. 2006;22(6):643–9. doi: 10.1016/j.arthro.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 21.Jones RB, Bartlett EC, Vainright JR, Carroll RG. CT determination of tibial tubercle lateralization in patients presenting with anterior knee pain. Skeletal Radiol. 1995;24(7):505–9. doi: 10.1007/BF00202146. [DOI] [PubMed] [Google Scholar]
- 22.Kumar A, Jones S, Bickerstaff DR, Smith TW. Functional evaluation of the modified Elmslie-Trillat procedure for patello-femoral dysfunction. Knee. 2001;8(4):287–92. doi: 10.1016/s0968-0160(01)00105-3. [DOI] [PubMed] [Google Scholar]
- 23.Palmer SH, Servant CT, Maguire J, Machan S, Parish EN, Cross MJ. Surgical reconstruction of severe patellofemoral maltracking. Clin Orthop Relat Res. 2004;419(1):144–8. doi: 10.1097/00003086-200402000-00023. [DOI] [PubMed] [Google Scholar]
- 24.Gul S, Lee PY, Davies A. Clinical outcomes of tibial tubercle transfer for anterior knee pain and patello-femoral instability. J Arthritis. 2016; 5(3):204–9. [Google Scholar]
- 25.Camp CL, Stuart MJ, Krych AJ, Levy BA, Bond JR, Collins MS, et al. CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 2013;41(8):1835–40. doi: 10.1177/0363546513484895. [DOI] [PubMed] [Google Scholar]
- 26.Thakkar RS, Del Grande F, Wadhwa V, Chalian M, Andreisek G, Carrino JA, et al. Patellar instability: CT and MRI measurements and their correlation with internal derangement findings. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):3021–8. doi: 10.1007/s00167-015-3614-8. [DOI] [PubMed] [Google Scholar]
- 27.Camathias C, Pagenstert G, Stutz U, Barg A, Müller-Gerbl M, Nowakowski AM. The effect of knee flexion and rotation on the tibial tuberosity-trochlear groove distance. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2811–7. doi: 10.1007/s00167-015-3508-9. [DOI] [PubMed] [Google Scholar]
- 28.Izadpanah K, Weitzel E, Vicari M, Hennig J, Weigel M, Südkamp NP, et al. Influence of knee flexion angle and weight bearing on the Tibial Tuberosity-Trochlear Groove (TTTG) distance for evaluation of patellofemoral alignment. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2655–61. doi: 10.1007/s00167-013-2537-5. [DOI] [PubMed] [Google Scholar]