Abstract
Background:
The purpose of this study was to determine a correlation between surgical case order and the length of operative time, total length of time in the operating room, time until discharge from the hospital, and the incidence of intraoperative complications for primary total shoulder arthroplasty cases.
Methods:
A retrospective review was conducted of records for all individual primary total shoulder arthroplasty and reverse total shoulder arthroplasty at a single hospital. In order to compare true parameters and minimize variables, only the cases performed by one senior author were analyzed. Operative and hospital records were reviewed.
Results:
There were 162 primary TSA and with the following order: 55 first order cases, 46 second order cases, 34 third order cases, 21 fourth order cases, and six fifth order cases. There were 71 primary rTSA patients included (27: 27:10:6:1). Length of stay was statistically increased for both female gender (8.3%; 95% confidence interval (CI)= 0.5-16.7%; p=0.0386) and fourth case order compared to first case (13.3%; 95% CI = 0.6%; 27.6%) p=0.041). For reverse TSA, there was no analyzed predictor that was significant.
Conclusion:
Even between anatomic TSA and reverse TSA patients, there was variability in what factors played a part in case inpatient length of stay. As such, we believe that this study highlights that case order can have an effect on operating room parameters for shoulder arthroplasty patients. The need for larger studies remains to better define that effect.
Key Words: Length of stay, Operative time, Reverse total shoulder arthroplasty, Shoulder complications, Surgical case order, Total shoulder arthroplasty
Introduction
The volume of total shoulder arthroplasty (TSA) in the United States has been steadily increasing over recent years (1). One analysis of the Nationwide Inpatient Sample (NIS) showed a 369% increase in the number of primary TSA surgeries performed from 1993 to 2007 (1). A later, independent analysis of the updated NIS showed that the demand for shoulder arthroplasty in patients younger than 55 years of age is projected to increase by 333% between 2011 and 2030 (2). In order to meet increased demand, surgeons and their respective hospital personnel are required to maintain larger operating schedules without compromising the safety and efficiency of the surgical care they provide. This combination of necessary growth and continued quality has led many to look at various factors that may influence care such as surgical case order.
Surgical case order has been associated with increased medical complications, infection rates, operative time, blood loss, intraoperative complications, and readmission rates (3-5). Up to 30% of hospital-acquired infections are due to the infection of surgical sites, which lead to higher costs in hospital charges as well as increased length of stay (3). Schimmel et al found that longer exposure time leads to a higher risk of surgical site infection (SSI) (4). In regard to shoulder arthroplasty, Schairer et al found that 18% of readmissions were attributed to surgical complications with infection being the most common of those surgical complications at 4.2% (5). Some have postulated that physician and operating room staff fatigue along with the possible shift changes with employees who are less adept at the procedures required during shoulder arthroplasty may place patients scheduled later in the day at increased risk of these complications.
To date, no study has investigated the relationship between case order and the length of operative time, length of hospital stay, and the incidence of intraoperative complications for shoulder arthroplasty patients. The purpose of this study was to determine whether there was a correlation between surgical case order and the length of operative time, total length of time in the operating room, time until discharge from the hospital, and the incidence of intraoperative complications. Our hypothesis is that cases scheduled later in the operative schedule would have a higher association with increased times and a higher incidence of intraoperative complications.
Materials and Methods
After approval by our institutional review board, a retrospective review was conducted of the inpatient and outpatient records for all primary total shoulder arthroplasties and reverse total shoulder arthroplasties at a single hospital from May 2013 to September 2014. After all procedures were tabulated, the case order was recorded based on the closing time. In order to compare true parameters, only cases performed by one senior author (GRW) were analyzed. Patient demographics including age, gender, body mass index (BMI), and Charlson co-morbidity index (CCI) scores were recorded. Operative and hospital records were reviewed with regard to operative time (described as time from incision to closure), total time in the operating room, length of stay (LOS), and intraoperative complications. All surgical cases included in this study were only followed up until the point of hospital discharge.
Statistical analysis was performed using linear regression models for each of these outcomes as a function of case order, controlling for the effect of gender, BMI, and Charlson co-morbidity index (prior to regression, LOS was log-transformed to satisfy the assumptions of linear regression, so the regression parameters returned percentages changes). For intraoperative complications, a similar logistic regression analysis was performed. Spearman’s rank correlation coefficient was utilized to check for any monotonic relationships between BMI and outcome variables. All statistical analysis was performed for anatomic total shoulder arthroplasty, reverse total shoulder arthroplasty, and all arthroplasty combined.
Procedural Protocol
Preoperatively, all patients undergoing TSA and reverse TSA (rTSA) received an interscalene nerve block for postoperative pain control. All patients were placed in the beach chair position for surgery with the use of a McConnell arm positioner. All surgeries were done utilizing the deltopectoral approach. All times were recorded in the operating rooms as per our institutional time out and time keeping policies.
Results
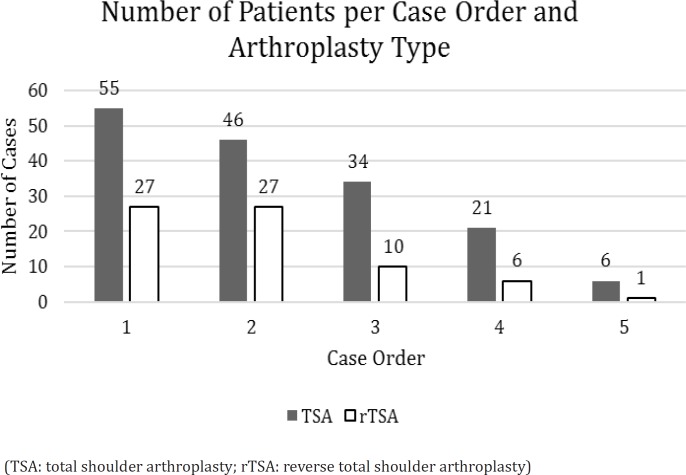
A total of 232 primary shoulder arthroplasty cases were considered for analysis [Table 1]. There were 162 primary TSA patients included in this study. Eighty-four (51.8%) of the TSA patients were male with an average age of 70 years old [range, 40-90 years] with an average BMI of 29.81 kg/m2 [range, 18.79-48.54 kg/m2]. The breakdown of case order for the TSA patients was the following: 55 first order cases, 46 second order cases, 34 third order cases, 21 fourth order cases, and six fifth order cases. There were 71 primary rTSA patients included in this study. Seventeen (23.9%) of the rTSA patients were male with an average age of 76 years old [range, 54-90 years] and an average BMI of 29.77 kg/m2 [range, 19-59 kg/m2]. The breakdown of case order for the rTSA patients was the following: 27 first order cases, 27 second order cases, 10 third order cases, six fourth order cases, and one fifth order case [Figure 1].
Table 1.
Patient Demographics per Case Order and Arthroplasty Type
| Demographics | Case Order | Anatomic TSA (162) | Reverse TSA (71) |
|---|---|---|---|
| Gender (M:F) | First | 30:25 | 5:22 |
| Second | 18:28 | 11:16 | |
| Third | 21:13 | 0:10 | |
| Fourth | 10:11 | 1:5 | |
| Fifth | 5:1 | 0:1 | |
| Overall | 84:78 | 17:54 | |
| Mean Age (Years) [Range] | First | 68 [40-83] | 76 [54-90] |
| Second | 73 [57-85] | 74 [60-90] | |
| Third | 72 [57-90] | 74 [63-85] | |
| Fourth | 66 [50-76] | 80 [72-87] | |
| Fifth | 67 [51-81] | 85 [NR] | |
| Overall | 70 [40-90] | 76 [54-90] | |
| Mean BMI [Range] | First | 29.77 [18.79-48.54] | 32.06 [19.31-58.55] |
| Second | 30.01 [19.13-42.93] | 27.94 [20.84-39.87] | |
| Third | 29.55 [19.23-41.71] | 29.39 [18.95-47.57] | |
| Fourth | 29.59 [20.81-40.7] | 28.65 [23.18-36.82] | |
| Fifth | 30.15 [27.19-36.18] | 27.54 [NR] | |
| Overall | 29.81 [18.79-48.54] | 29.77 [19.31-58.55] |
(TSA: total shoulder arthroplasty; M: male; F: female; BMI: body mass index)
Figure 1.
Number of patients per case order and arthroplasty type
(TSA: total shoulder arthroplasty; rTSA: reverse total shoulder arthroplasty)
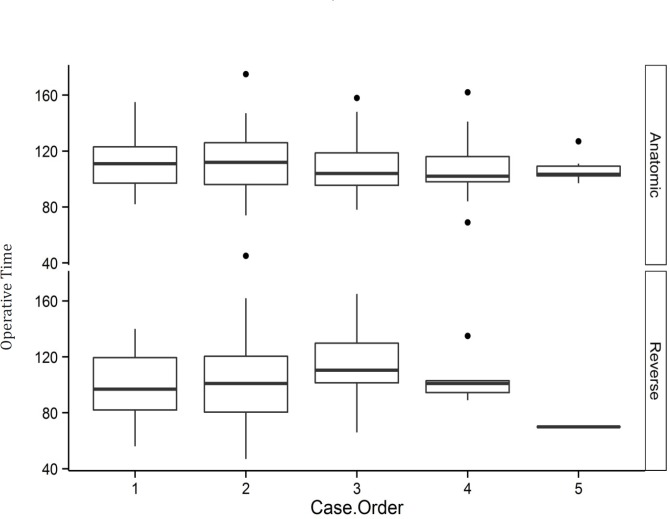
For anatomic TSA, the regression model estimated that operative time was significantly increased for males compared to females [7.8 minutes +/- 3.2 minutes, mean +/- SE; P=0.0157] and was also increased with each point of the CCI [3.9 minutes +/- 1.8 minutes, mean +/- SE; P=0.0338], but there was no association with case order (P=0.67717). Within each case order (1-5), the average operative time was 103.5-111 minutes, and the standard deviation was 11 to 23 minutes. There was no statistical difference for case order, gender, BMI, or CCI in regards to total time spent in the operating room. Length of stay was slightly increased for both female gender [mean 8.3%; 95% confidence interval = 0.5-16.7%; P=0.0386] and fourth case order compared to first case [mean 13.3%; 95% CI = 0.6%; 27.6%) P=0.041]. Lastly, only an increased CCI was correlated with an increased risk of intraoperative complication [Odds Ratio 2.2; 95% CI =1.2 4.0; P<0.01]. For reverse TSA, there was no analyzed predictor that correlated with an increased operative time, time to discharge from the hospital, or intraoperative complication. The third order cases had a significantly longer total time in the operating room [23.2+/- 10.2 minutes; P=0.0272] than the first case. The visible tendency was for the total time in the operating to increase and then decrease for reverse TSA [Figure 2].
Figure 2.
Operative Time (in Minutes) per Case Order for Anatomic TSA and Reverse TSA Individually
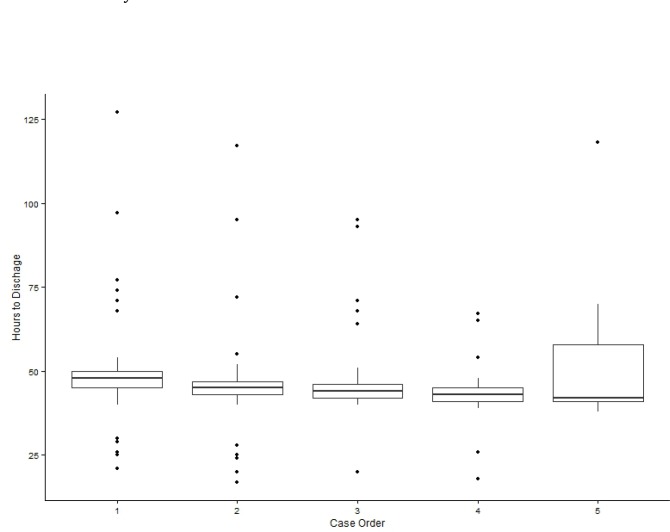
Lastly, when the two cohorts of reverse TSA and anatomic TSA cases were combined, cases performed later in the day showed a significant trend towards longer time until discharge from the hospital (P<0.05) [Figure 3].
Figure 3.
Hours to Discharge from Hospital per Case Order for Combined Anatomic and Reverse TSA
Discussion
The results of this study demonstrate that although case order in the operative schedule does have an effect on durations of operative time and length of time until discharge, this impact is not consistent. For our anatomic TSA patients, those scheduled as a fourth case for the day had significantly longer stays until discharge than those scheduled as a first case (P=0.041). The most statistically significant finding was that when all arthroplasty patients were considered, there was strong correlation between later case order and longer time to discharge from the hospital (P<0.05). The effect of length of stay on patient outcome is an important area of research as it drives hospital costs. Jain et al found that surgeons who performed high-volume number of shoulder arthroplasties (more than four per year) had patients with shorter length of stays when compared to low-volume surgeons (6). These findings paralleled with those of Kreder et al who demonstrated similar differences among hip arthroplasty patients (6, 7). This is intuitive as a surgeon who performs shoulder arthroplasty routinely is likely more familiar with the nuances of the surgical technique and likely has a supportive operating room team and nursing/ancillary staff who are better suited to treat patients in the immediate postoperative period. However, our data shows that even patients of a facile high-volume surgeon can vary in their duration of hospital stay. Patients who are placed later in the surgical case order can often be susceptible to the late-day shift change in the operating room and the care of the “on-call” or “cross-covering” floor provider who may not be as well-versed in caring for a patient undergoing shoulder arthroplasty. As the surgeon’s operative schedule continues through the day, the ancillary staff that helps to coordinate postoperative lab draws, physical therapy sessions, and disposition planning will often finish their shift regardless of the state of operating room. The result is that patients who undergo their operation later in the day will not have these coordinated efforts started until the following morning, whereas those patients scheduled for the earlier cases will often have their postoperative care organized by that afternoon. We, unfortunately, were unable to map out the “clock-in” and “clock-out” times of such ancillary personnel, but would strongly consider doing so in future studies.
Surprisingly, operative time did not appear to be significantly affected by the order of the case in the schedule. In fact, the only variable measured that affected any operative time for any of the arthroplasty patients was male gender in regards to anatomic total shoulder arthroplasty. Operative time was significantly increased for males compared to females undergoing TSA (P=0.0157) which is consistent with findings in other areas of joint replacement. Kosashvili et al evaluated the influence of gender on surgical time for primary total knee arthroplasty and found that more time was required for surgery on men than on women (8). The authors concluded that this time discrepancy is largely due to the anatomic and physiologic differences between males and females. Males, on average, tend to have a higher percentage of lean muscle mass (8, 9). This can result in larger deltoid and pectoralis major muscles which inhibit surgical exposure. Similarly, studies of the lower extremities have shown that women possess increased joint and ligamentous laxity (8, 10, 11), which aids in extremity manipulation for surgical exposure. With its extensive capsular and ligamentous attachments, the shoulder joint is also easily affected by such physiology. This results in potentially easier dislocation and exposure of the glenohumeral joint which, in turn, leads to shorter operative time. It has been the experience of the authors of this study that male patients also tend to have increased stiffness in the setting of their osteoarthritis which would also account for this increased exposure difficulty.
The other impact of gender on anatomic TSA was the longer hospital stays required for females when compared to males. This finding is similar to much of the data previously published. Menendez et al sought to find preoperative and postoperative factors that predicted increased length of stay in TSA and rTSA patients and found that female patients were more than twice as likely to have longer stays compared to their male counterparts (12). Matsen et al also found longer stays amongst female patients with male patients averaging stays that were 14% shorter (13). Similar findings have been published with regards to gender influence on hip and knee arthroplasty patients (13, 14). There is uncertainty for causes of this trend. We found no influence of gender on the operative time or length of stay in the reverse total shoulder arthroplasty patient population.
In regards to reverse total shoulder arthroplasty, there was very little influence from any of the measured predictors on outcome variables. There appeared to be an increase in operative time as one compared the second and third reverse TSA cases of the day to the first reverse TSA case. However, this increase in time ended up declining again as the schedule progressed on to the fourth and fifth reverse TSA cases. This is appreciated in Figure 2 with a rise and fall in the operative times as one moves along from first to fifth scheduled cases. It is difficult to ascertain why this trend occurred. One possible explanation is that the first cases of the day tend to begin with the usual operative ancillary staff that work with the surgeon routinely and then as the day continues, certain members of that team are relieved for scheduled breaks throughout the day. With this change in staff, comes the possibility of certain substituting members of the team being less familiar with the operative procedure and there is increased requirement in the time to perform the case. As the day continues on, those usual members of the operative staff return from their breaks and are able to complete the later cases at a faster pace. The more likely explanation for this rise and fall in operative time is likely a product of the amount of cases analyzed at each order in our study. As seen in Figure 1, the amount of reverse TSA cases analyzed at first, second, and third case order were greater than (First Case: n=27, Second Case: n=27, Third Case: n=10) than the fourth and fifth reverse TSA cases (Fourth Case: 6, Fifth Case: 1). The reason for these smaller population sizes for the fourth and fifth case orders is because of the rarity of having four or five cases performed in one operating room on any given day of the surgeon’s schedule. Clearly, performing one to three cases in one room per day is a much more likely event than performing four or more. This gives these later case orders less power for analysis. That being said, we would likely expect the operative times for those respective cases to be increased and show an overall trend of increased time in Figure 2. It is also possible that larger numbers in the reverse TSA population would have yielded results similar to the anatomic TSA cohort, which showed no real difference at all.
Lastly, one of the goals for this study was to evaluate the influence of case order on intraoperative complications. Case order as it relates to perioperative complications has been studied in various other surgical fields. Our study noted a trend for shoulder arthroplasty patients with no influence of case order on perioperative complication incidence. This is encouraging as there have been reports in the spine surgery literature which have shown higher risk of infection for decompression cases performed later in the day which can lead to longer hospital stays, higher readmission rates, and increased patient morbidity and mortality (15). The authors of that study noted that other factors not measured in their study such as shift-changes and OR traffic contamination may be to blame for the later cases having higher infection rates. In the case of our study, only increased Charlson Co-morbidity Index scores were associated with higher increased risk of intraoperative complication and increased operative times for TSA. This is not surprising as multiple studies have shown the effect of CCI on complications in various orthopaedic surgical procedures including shoulder arthroplasty (16-18).
This study has several limitations. The first limitation is inherent to a retrospective study design in which there are uncontrolled biases that can exist. Once such example inherent to this retrospective design is the recording of operative times, which are dependent on the electronic records of the hospital and not our own timekeeping. Secondly, our study only examined the patients of one high-volume surgeon. Although this could be considered a strength by providing homogeneity in the analysis, using only one surgeon’s standardized technique could negatively influence generalizability. In the case of this particular surgeon, case order is not chosen by the surgeon himself which decreases any influence case complexity or variability in surgical technique (e.g. bone grafting of the glenoid). Given that this study only looked at primary arthroplasty cases also decreased the chance of increased complexity that can often be seen in revision cases. For many surgeons, these factors are often considered in selecting case order and often will influence surgical times as well as selected case order. This, again, makes generalizability difficult. Additionally, we did not examine any patient outcomes (radiographs, physical examination, functional outcomes scores) to see if the order of their scheduled cases and their time spent in the operating room had any effect. Although, we found it important to measure the influence of case order on surgical and discharge times, it is ultimately important to understand the effects on patient outcomes. We did not address this and would certainly recommend that future studies measure these parameters long term. Finally, even though we evaluated cases done by a high volume shoulder arthroplasty surgeon, our study was underpowered to draw conclusions about rare events, such as intra- and post-operative complications.
In conclusion, the effect of surgical case order on patient time spent in the operating room and in the hospital seems to vary widely. One would likely expect that cases scheduled later in the day would result in longer operative times and longer times until discharge as staff fatigue, processing of implants, and late transfers from the post-operative care unit to the inpatient floor would negatively impact the speed and efficiency by which patients are treated. This, however, was not found in our experience. Even between anatomic TSA and reverse TSA patients, there was variability in what factors played a role in inpatient duration of admission. As such, we believe that this study highlights that case order can have an effect on operating room parameters for shoulder arthroplasty patients, but larger prospective studies are required to better define this effect.
Patient Consent: This was a retrospective study that did not require patient consent as it did not affect the standard of care. All collected data was de-identified. This was approved by our IRB. No new drugs or devices were used in this study.
Disclosure: The authors report no conflict of interest concerning the materials or methods used in this study of the findings specified in this paper.
Acknowledgements
We would like to acknowledge Mitchell Maltenfort, PhD for his expertise in statistical analysis.
References
- 1.Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010;19(8):1115–20. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Padegimas EM, Maltenfort M, Lazarus MD, Ramsey ML, Williams GR, Namdari S. Future patient demand for shoulder arthroplasty by younger patients: national projections. Clin Orthop Relat Res. 2015;473(6):1860–7. doi: 10.1007/s11999-015-4231-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poultsides LA, Ma Y, Della Valle AG, Chiu YL, Sculco TP, Memtsoudis SG. In-hospital surgical site infections after primary hip and knee arthroplasty--incidence and risk factors. J Arthroplasty. 2013;28(3):385–9. doi: 10.1016/j.arth.2012.06.027. [DOI] [PubMed] [Google Scholar]
- 4.Schimmel JJ, Horsting PP, de Kleuver M, Wonders G, van Limbeek J. Risk factors for deep surgical site infections after spinal fusion. Eur Spine J. 2010;19(10):1711–9. doi: 10.1007/s00586-010-1421-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schairer WW, Zhang AL, Feeley BT. Hospital readmissions after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(9):1349–55. doi: 10.1016/j.jse.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Jain N, Pietrobon R, Hocker S, Guller U, Shankar A, Higgins LD. The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg Am. 2004;86-A(3):496–505. doi: 10.2106/00004623-200403000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Kreder HJ, Williams JI, Jaglal S, Hu R, Axcell T, Stephen D. Are complication rates for elective primary total hip arthroplasty in Ontario related to surgeon and hospital volumes? A preliminary investigation. Can J Surg. 1998;41(6):431–7. [PMC free article] [PubMed] [Google Scholar]
- 8.Kosashvili Y, Mayne IP, Trajkovski T, Lackstein D, Safir O, Backstein D. Influence of sex on surgical time in primary total knee arthroplasty. Can J Surg. 2010;53(4):256–60. [PMC free article] [PubMed] [Google Scholar]
- 9.Neder JA, Nery LE, Silva AC, Andreoni S, Whipp BJ. Maximal aerobic power and leg muscle mass and strength related to age in non-athlethic males and females. Eur J Appl Physiol Occup Physiol. 1999;79(6):522–30. doi: 10.1007/s004210050547. [DOI] [PubMed] [Google Scholar]
- 10.van der Esch M, Steultjens MP, Lems WF, Dekker J. Gender difference in varus-valgus laxity in osteoarthritis of the knee. Scand J Rheumatol. 2007;36(2):157–9. doi: 10.1080/03009740600905372. [DOI] [PubMed] [Google Scholar]
- 11.Felson DT, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum. 1998;41(8):1343–55. doi: 10.1002/1529-0131(199808)41:8<1343::AID-ART3>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 12.Menendez ME, Baker DK, Fryberger CT, Ponce BA. Predictors of extended length of stay after elective shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(10):1527–33. doi: 10.1016/j.jse.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 13.Matsen FA 3rd, Li N, Gao H, Yuan S, Russ SM, Sampson PD. Factors affecting length of stay, readmission, and revision after shoulder arthroplasty: a population-based study. J Bone Joint Surg Am. 2015;97(15):1255–63. doi: 10.2106/JBJS.N.01107. [DOI] [PubMed] [Google Scholar]
- 14.Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008;79(2):168–73. doi: 10.1080/17453670710014941. [DOI] [PubMed] [Google Scholar]
- 15.Gruskay J, Kepler C, Smith J, Radcliff K, Vaccaro A. Is surgical case order associated with increased infection rate after spine surgery? Spine. 2012;37(13):1170–4. doi: 10.1097/BRS.0b013e3182407859. [DOI] [PubMed] [Google Scholar]
- 16.Petrigliano FA, Bezrukov N, Gamradt SC, SooHoo NF. Factors predicting complication and reoperation rates following surgical fixation of proximal humeral fractures. J Bone Joint Surg Am. 2014;96(18):1544–51. doi: 10.2106/JBJS.M.01039. [DOI] [PubMed] [Google Scholar]
- 17.Singh JA, Sperling JW, Cofield RH. Ninety day mortality and its predictors after primary shoulder arthroplasty: an analysis of 4,019 patients from 1976-2008. BMC Musculoskelet Disord. 2011;12(12):231. doi: 10.1186/1471-2474-12-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Voskuijl T, Hageman M, Ring D. Higher Carlson comorbidity index scores are associated with readmission after orthopaedic surgery. Clin Orthop Relat Res. 2014;472(5):1638–44. doi: 10.1007/s11999-013-3394-8. [DOI] [PMC free article] [PubMed] [Google Scholar]