Abstract
Background:
While outcomes of primary anatomic total shoulder arthroplasty (aTSA) are generally favorable, results after revision procedures are less reliable. This study examines the functional outcomes, complications, and implant survival in patients who underwent revision of aTSA to aTSA.
Methods:
Patients who underwent revision aTSA were identified from 2008-2015. Demographic, clinical, surgical, and outcomes data were analyzed. Patient-reported outcomes including the American Shoulder and Elbow Surgeons Score (ASES), Single Assessment Numerical Evaluation (SANE), Visual Analog Scale for pain (VAS), the Short Form-12 Health Survey (SF-12), and patient satisfaction were recorded.
Results:
Twenty patients underwent revision from a primary aTSA to aTSA (55% male, 62.0±6.8 years-old). Revision aTSA occurred at 2.5±3.4 years after index surgery. Seven (35%) required future revision at 1.8±1.9 years after revision aTSA. Among the 13 patients who did not undergo revision, twelve (92.3%) had over two-year follow-up (4.0±2.4 years). Average ASES score was 70.1±23.5, SANE 66.0±29.4, VAS 2.7±3.0, SF-12 Mental 52.4±10.5, SF-12 Physical 36.8±8.9, and satisfaction of 3.6±1.2.
Conclusion:
Results of revision aTSA to aTSA were unpredictable and the revision rate was high. The cases that do not undergo revision had satisfactory, but inconsistent functional results. Reverse arthroplasty may be more reliable in this patient population.
Key Words: Anatomic total shoulder arthroplasty, Complications, Reoperations, Revision shoulder arthroplasty
Introduction
As the utilization of anatomic total shoulder arthroplasty (aTSA) continues to increase, appropriate management of failed aTSA will become increasingly important (1–3). While aTSA has shown survival rates of over 80% at 15 years of follow-up, revision arthroplasty, when necessary, has unfortunately been associated with inferior outcomes to the primary arthroplasty (4–11). Failure of aTSA can occur as a result of multiple etiologies (including instability, rotator cuff tear, glenoid component loosening, humeral component loosening, or infection) (11).
Given concerns regarding poor outcomes and complications in revision aTSA, the reverse shoulder arthroplasty (RSA) has increased in popularity due to its semi-constrained design and less reliance on rotator cuff integrity (12,13). As experience with the reverse prosthesis has increased since Boileau et al first described its use in the revision setting, outcomes have improved and complication rates have decreased (14–17). However, while RTSA has performed adequately in the short to mid-term, concerns remain about the long-term survivorship of the implant and outcomes after revision of an RTSA (18). The purpose of this study was to analyze outcomes of patients who underwent revision of aTSA to another aTSA.
Materials and Methods
Following approval by our hospital system’s Institutional Review Board, all shoulder arthroplasties performed between January of 2008 through September of 2015 were identified by querying of an institutional shoulder arthroplasty database constructed using the common procedural (CPT) codes 23472 (total shoulder arthroplasty), 23473 (revision of total shoulder arthroplasty, humeral or glenoid component), and 23474 (revision of total shoulder arthroplasty, humeral or glenoid component). A direct retrospective chart review was performed to identify all patients who were revised from an aTSA to another aTSA at a single institution. Each patient’s primary aTSA was not necessarily performed at this institution.
Details of each patient’s case were then collected and analyzed. The data collected included demographics (age, gender, and body mass index [BMI]), surgical variables (indication for revision, culture results of revision, surgical approach of revision, rotator cuff integrity, and concomitant procedures), and outcomes (range of motion [ROM], reoperations, postoperative complications, and patient-reported outcomes). Patient-reported outcomes analyzed were visual analog scale (VAS) pain score, Single Assessment Numeric Evaluation (SANE) score(19), American Shoulder and Elbow Surgeons (ASES) scores (20), Short-Form 12 (SF-12) Physical (21), SF-12 Mental (21), and patient satisfaction (on a scale of 1-5, 1 being very dissatisfied and 5 being very satisfied).
Data for active forward elevation (AFE) and active external rotation (AER) was obtained at a minimum of one year follow-up. All ROM data was recorded from direct physical examination by the treating surgeon. Patient-reported outcomes and survival data were obtained at minimum of two-year follow-up from direct chart review or telephone survey. Kaplan-Meier survival analysis was performed to assess implant survivorship with revision arthroplasty as an endpoint. All statistics were calculated with Microsoft Excel (2013; Redmond, WA).
Results
Of the 494 revision shoulder arthroplasties performed at our institution during the study period, there were 20 (4.0%) patients identified who underwent revision of aTSA to another aTSA. This population was 55% male, had an average age of 62.0±6.8 years-old (49.8-73.7) at the time of index revision, and an average BMI of 31.2±5.2 (21.6-38.3). Diagnoses at index primary arthroplasty were osteoarthritis (16/20, 75%), avascular necrosis (2/20, 10%), and post-traumatic arthritis (3/20, 15%). Revision aTSA occurred at an average of 2.5±3.4 (0.3-14.3) years after index surgery. The diagnoses at time of revision were 7 anterior instability with subscapularis insufficiency (two from failed lesser tuberosity osteotomies), 3 posterior instability, 4 malaligned humeral components with stiffness, 3 isolated arthrofibrosis 2 glenoid loosening, and one case of humeral loosening [Table 1].
Table 1.
Surgical details for each patient
| Patient | Diagnosis | Years between index and revision | Surgical approach | Subscapularis Management | Other Procedure | Head Exchange | Stem Retention | Glenoid Retention | Cultures | Bone Graft | Further Revision |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Anterior instability; subscapularis insufficiency | 0.3 | Deltopectoral | Ruptured, repaired | Subscapularis Repair | Yes | No | Yes | P. acnes, CNS | Glenoid | No |
| 2 | Arthrofibrosis | 1.0 | Deltopectoral | Peel | None | Yes | No | Yes | None Drawn | None | No |
| 3 | Malaligned humeral component; Biceps Tendonitis | 14.3 | Deltopectoral | LTO | Biceps Tenodesis | Yes | No | Yes | Negative | None | No |
| 4 | Malaligned humeral component; Biceps Tendonitis | 7.2 | Deltopectoral | Peel | Biceps Tenodesis | Yes | No | Yes | Negative | Glenoid | No |
| 5 | Anterior instability; subscapularis insufficiency | 0.4 | Deltopectoral | Ruptured, repaired | Subscapularis Repair (with patch) | Yes | Yes | Yes | None Drawn | None | No |
| 6 | Anterior instability; failed LTO | 1.0 | Deltopectoral | LTO nonunion, repaired | Subscapularis Repair (with patch) | Yes | Yes | Yes | Negative | Humerus | No |
| 7 | Glenoid loosening (following MVA) | 0.5 | Deltopectoral | Peel | None | Yes | Yes | No | Negative | None | Yes |
| 8 | Arthrofibrosis | 1.3 | Deltopectoral | Peel | None | Yes | Yes | Yes | None Drawn | None | Yes |
| 9 | Anterior instability; subscapularis insufficiency | 1.3 | Deltopectoral | Peel | None | Yes | Yes | Yes | None Drawn | None | No |
| 10 | Malaligned humeral component; Biceps Tendonitis | 0.8 | Deltopectoral | Peel | None | Yes | No | Yes | None Drawn | Glenoid | Yes |
| 11 | Arthrofibrosis; Biceps Tendonitis | 1.4 | Deltopectoral | LTO | Biceps Tenodesis | Yes | Yes | Yes | Negative | None | No |
| 12 | Anterior instability; subscapularis insufficiency | 0.9 | Deltopectoral | Ruptured, repaired | Subscapularis Repair (with patch) | Yes | Yes | Yes | None Drawn | None | Yes |
| 13 | Malaligned humeral component; Biceps Tendonitis | 2.0 | Deltopectoral | LTO | 5mm Step Posterior Augment Glenoid | Yes | No | No | Negative | Glenoid | No |
| 14 | Posterior instability; subscapularis insufficiency | 4.3 | Deltopectoral | Ruptured, repaired | 5mm Step Posterior Augment Glenoid, PC | Yes | No | No | CNS | Humerus | No |
| 15 | Posterior instability | 1.3 | Deltopectoral | LTO | 7mm Step Posterior Augment Glenoid | Yes | Yes | No | Negative | None | No |
| 16 | Anterior instability; subscapularis insufficiency | 0.8 | Deltopectoral | Ruptured, repaired | Subscapularis Repair (with patch) | Yes | No | Yes | None Drawn | None | No |
| 17 | Posterior instability | 3.1 | Deltopectoral | Peel | None | Yes | No | No | None Drawn | None | Yes |
| 18 | Glenoid loosening | 1.0 | Deltopectoral | Peel | Tibial Strut Graft and Cerclage | Yes | No | No | Negative | Glenoid | No |
| 19 | Anterior instability; failed LTO | 0.3 | Deltopectoral | LTO nonunion, repaired | Subscapularis Repair | Yes | Yes | Yes | None Drawn | None | Yes |
| 20 | Humeral loosening | 7.8 | Deltopectoral | LTO | None | Yes | No | Yes | Negative | None | Yes |
LTO= Lesser Tuberosity Osteotomy; MVA= Motor Vehicle Accident; P. acnes= Propionibacterium acnes; CNS= Coagulase Negative Staphylococcus; NA= Not applicable; F/U= Follow-Up; PC= Posterior Capsulorrhaphy
All revision aTSAs were performed through a deltopectoral approach. All patients had an intact posterior-superior rotator cuff. All patients underwent a humeral head exchange, 9/20 (45%) underwent revision of the humeral stem, and 6/20 (30%) underwent revision of the glenoid component. There were 5/20 (25%) aTSA that required glenoid bone grafting and 2/20 (10%) that required humeral bone grafting. Eleven of the patients had cultures drawn with 2/11 (18.2%) having positive cultures. One patient grew coagulase negative staphylococcus (1/2 of cultures drawn) while the other grew both coagulase negative staphylococcus (1/6 of cultures drawn) and Propionibacterium acnes (1/6 of cultures drawn). These patients were treated with cephalexin for six weeks and doxycycline for six months, respectively.
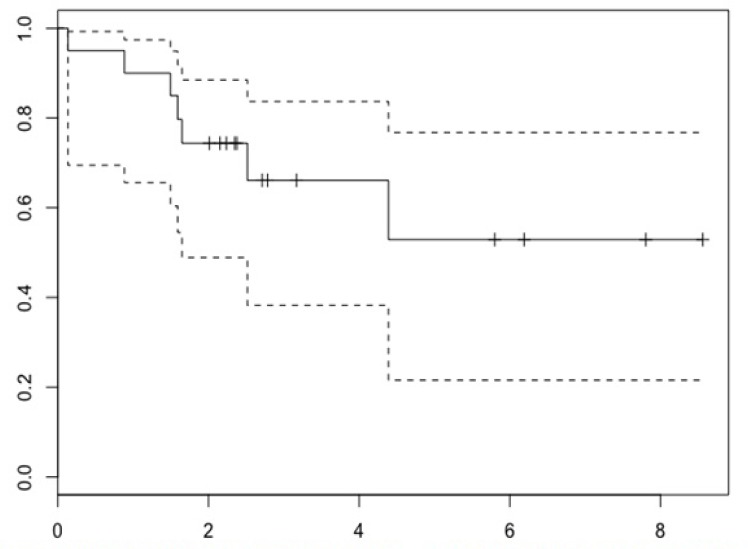
Seven patients out of 20 (35%) underwent revision arthroplasty at an average of 1.8±1.9 (0.1-4.4) after revision aTSA. There was one open reduction and glenoid component removal for a fixed posterior dislocation and six conversions to RSA (two for instability with subscapularis failure, one for persistent stiffness and pain, two performed at outside institutions without known details of the procedure, and one patient with multiple surgeries and eventual two stage exchange to reverse total shoulder arthroplasty for periprosthetic joint infection). Kaplan-Meier survival analysis was performed and found a 66.1% survival at four years post-operatively with a 95% confidence interval of 38.3-83.7% [Figure 1]. In addition to the seven revisions with component failure, one more patient underwent an open reduction and internal fixation of a humeral-sided periprosthetic fracture at eight weeks with implant retention.
Figure 1.
Kaplan Meier survival analysis curve for implant survival of the index revision from aTSA to aTSA
Of the 13 patients that did not go onto revision, twelve (92.3%) had patient-reported outcomes at over two-year follow-up (4.0±2.4 years; 2.0-8.6 years). Average ASES score was 70.1±23.5 (18.3-98.3), SANE 66.0±29.4 (20-100), VAS 2.7±3.0 (0-8), SF-12 Mental (11 patients) 52.4±10.5 (29.9-63.4), SF-12 Physical (11 patients) 36.8±8.9 (26.4-44.1), and satisfaction of 3.6±1.2 (2-5). Mean AFE was 141.5O +/- 10.5O (100O-160O) in the 10 of 13 (76.9%) patients with available data at 2.6±1.8; 1.0-6.0 years follow-up. Mean AER was 39.8O±10.5O (20O-55O) in the 8 of 13 (66.7%) patients with available data at 2.2±1.4; 1.0-5.4 years follow-up.
Discussion
This analysis identified twenty patients that underwent revision from an aTSA to another aTSA. Notably, the survival rate at four years was relatively low (65%). Patient outcomes and ROM in those that did survive were satisfactory, but inconsistent.
Previous analysis of isolated glenoid revision in aTSA was performed by Cheung et al (7). They treated 33 patients with glenoid loosening by isolated glenoid revision. This study found a lower reoperation rate of 21.2% and a satisfaction rate of 70% at a mean of 3.8 years of follow-up. Another analysis that included 15 cases of revision from aTSA to aTSA by Deutsch et al reported a mean postoperative ASES score of 52.8, and no cases of revision surgery at a mean of 3.5 years after surgery (22). Deutsch et al found that instability at index revision aTSA to be predictive of poor outcome (22). We were likely underpowered to comment on associations between diagnosis for failed aTSA and whether the revision surgery was successful. Finally, Bonnevialle et al studied 42 failed aTSA for glenoid loosening with revision to new aTSA (23). They found a high complication rate (45%), 21% reoperation rate, and 17% revision rate at a mean of 6.2 years of follow-up.
Given the poor clinical results with revision aTSA, RTSA has increased in popularity for revision arthroplasty (4–11, 15–17). Previous analysis by Boileau et al was the first to focus on revision to a reverse arthroplasty (14). There were 19 cases revision of an anatomic arthroplasty revised to an RTSA. They reported a 47% complication rate and poor ASES scores (average of 50). However, this was the earliest series to focus on the technique of revision to a reverse implant. Further study by Patel et al identified a substantially lower complication rate of 10.7% and an average ASES score of 66.2. While these results are an improvement, patient-reported outcomes remain limited when RTSA is used in revision arthroplasty.
The conclusions of this study must be viewed in the context of the limitations. This is a small patient cohort and therefore projecting outcomes onto a wider population are difficult. Specifically, there were not enough patients to determine which patients were more likely to have a successful clinical outcome. Additionally, the lack of pre-operative patient-reported outcomes limits the conclusions that one can make within this population. Finally, this is a purely retrospective study and therefore is subject to all of the limitations of retrospective data especially the inability to elucidate causal relationships rather than simply correlative ones.
Revision of aTSA to aTSA was performed for diverse reasons and had a survival rate of 60% at 4 years. Patient-reported outcomes at short to mid-term and ROM were satisfactory, but inconsistent in those that did not experience failure. Future multi-center study may help determine the best candidates for revision of an aTSA to another aTSA.
References
- 1.Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010;19(8):1115–20. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93(24):2249–54. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed] [Google Scholar]
- 3.Padegimas EM, Maltenfort M, Lazarus MD, Ramsey ML, Williams GR, Namdari S. Future patient demand for shoulder arthroplasty by younger patients: national projections. Clin Orthop Relat Res. 2015;473(6):1860–7. doi: 10.1007/s11999-015-4231-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sperling JW, Cofield RH, Rowland CM. Minimum fifteen-year follow-up of Neer hemiarthroplasty and total shoulder arthroplasty in patients aged fifty years or younger. J Shoulder Elbow Surg. 2004;13(6):604–13. doi: 10.1016/S1058274604001296. [DOI] [PubMed] [Google Scholar]
- 5.Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217–24. doi: 10.1067/mse.2001.113961. [DOI] [PubMed] [Google Scholar]
- 6.Carroll RM, Izquierdo R, Vazquez M, Blaine TA, Levine WN, Bigliani LU. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: long-term results. J Shoulder Elbow Surg. 2004;13(6):599–603. doi: 10.1016/j.jse.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 7.Cheung EV, Sperling JW, Cofield RH. Revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg. 2008;17(3):371–5. doi: 10.1016/j.jse.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Dines JS, Fealy S, Strauss EJ, Allen A, Craig EV, Warren RF, et al. Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am. 2006;88(7):1494–500. doi: 10.2106/JBJS.D.02946. [DOI] [PubMed] [Google Scholar]
- 9.Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742–7. doi: 10.2106/JBJS.E.00851. [DOI] [PubMed] [Google Scholar]
- 10.Petersen SA, Hawkins RJ. Revision of failed total shoulder arthroplasty. Orthop Clin North Am. 1998;29(3):519–33. doi: 10.1016/s0030-5898(05)70026-2. [DOI] [PubMed] [Google Scholar]
- 11.Sajadi KR, Kwon YW, Zuckerman JD. Revision shoulder arthroplasty: an analysis of indications and outcomes. J Shoulder Elbow Surg. 2010;19(2):308–13. doi: 10.1016/j.jse.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 12.Khatib O, Onyekwelu I, Yu S, Zuckerman JD. Shoulder arthroplasty in New York State, 1991 to 2010: changing patterns of utilization. J Shoulder Elbow Surg. 2015;24(10):e286–91. doi: 10.1016/j.jse.2015.05.038. [DOI] [PubMed] [Google Scholar]
- 13.Schairer WW, Nwachukwu BU, Lyman S, Craig EV, Gulotta LV. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2015;24(1):91–7. doi: 10.1016/j.jse.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 14.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: the Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15(5):527–40. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Chalmers PN, Keener JD. Expanding roles for reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2016;9(1):40–8. doi: 10.1007/s12178-016-9316-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel DN, Young B, Onyekwelu I, Zuckerman JD, Kwon YW. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(11):1478–83. doi: 10.1016/j.jse.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Wagner E, Houdek MT, Griffith T, Elhassan BT, Sanchez-Sotelo J, Sperling JW, et al. Glenoid bone-grafting in revision to a reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2015;97(20):1653–60. doi: 10.2106/JBJS.N.00732. [DOI] [PubMed] [Google Scholar]
- 18.Guery J. Reverse total shoulder arthroplasty Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742–7. doi: 10.2106/JBJS.E.00851. [DOI] [PubMed] [Google Scholar]
- 19.Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the single assessment numeric evaluation method and two shoulder rating scales Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214–21. doi: 10.1177/03635465990270021701. [DOI] [PubMed] [Google Scholar]
- 20.Michener LA, McClure PW, Sennett BJ. American shoulder and elbow surgeons standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587–94. doi: 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- 21.Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Deutsch A, Abboud JA, Kelly J, Mody M, Norris T, Ramsey ML, et al. Clinical results of revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg. 2007;16(6):706–16. doi: 10.1016/j.jse.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Bonnevialle N, Melis B, Neyton L, Favard L, Molé D, Walch G, et al. Aseptic glenoid loosening or failure in total shoulder arthroplasty: revision with glenoid reimplantation. J Shoulder Elbow Surg. 2013;22(6):745–51. doi: 10.1016/j.jse.2012.08.009. [DOI] [PubMed] [Google Scholar]