Abstract
An annual OSHA fit test is required for all U.S. employees required to wear a respirator during work, but there are limited data demonstrating a link between fit test results and respirator fit during work. The goal of this research is to determine if the fit factor (FF) achieved during an abbreviated ambient aerosol condensation particle counter (CPC) quantitative fit test is predictive of fit achieved during a simulated workplace protection factor (SWPF) scenario that includes realistic healthcare activities. Fifteen subjects (7 male; 8 female) were recruited for a range of facial sizes. Each subject donned an N95 filtering facepiece respirator and performed a single 29-min routine consisting of initial and final 2.5 min fast fit tests (five 30-sec exercises: normal breathing, head side to side, head up and down, talking, and bending over) and three repetitions of three 6-min simulated healthcare activities (CPR, ultrasound, and making a hospital bed). Two CPC instruments simultaneously collected second-by-second measures of particle concentration inside and outside of the respirator facepiece. FFs or SWPFs were calculated by dividing outside by inside facepiece concentrations. Overall FFs and SWPFs were highly correlated. Each exercise FF was highly correlated with the overall SWPF. Normal breathing, head up and down, and talking were most predictive of overall SWPF. Normal breathing and talking together were predictive of each of the three simulated healthcare activities. For CPR and bed making activities, head movement exercises were also found to be predictive. A quantitative fit test using a small set of exercises is highly predictive of an individual’s fit during simulated work activities. Some exercises (e.g. talking and head movements) are predictive of fit during simulated workplace activities. Limitations include only one respirator model, a small subject pool not representative of the full range of face sizes. This paper uses an innovative second-by-second assessment method that collects information about in- and outside-facepiece concentrations throughout the test period.
Keywords: Respiratory Protection, Real-Time Respirator Fit, Simulated Workplace Protection Factor
INTRODUCTION
An annual OSHA fit test is required for all U.S. employees required to wear a respirator during work, but there are limited data demonstrating a link between fit test results and respirator fit during work.(1) Except for the controlled negative pressure fit testing methods, quantitative fit tests involve eight exercises: normal breathing, deep breathing, head up-and-down, head side-to-side, talking, grimace, bending over, and normal breathing. These exercises were originally selected to be representative of respirator fit in the workplace.(2) There is limited evidence that these are the most representative exercises of work where jobs and tasks can involve a wide variety of movements or if the same results could be achieved from a fewer or different set of test exercises.
Workplace protection factors (WPF) – respirator fit measured during work - have been evaluated in industries using gravimetric methods to compare personal aerosol exposures inside and outside of the respirator.(3–7) In all cases, initial fit was evaluated with a qualitative test that does not allow for statistical comparisons of individuals’ fit factors (FFs) and WPFs.
Because WPF studies are expensive and difficult to conduct, more recent investigations have evaluated fit during simulated work tasks in controlled laboratory settings to obtain measures of simulated workplace protection factors (SWPFs).(8–10) The advantages of such studies include the use of less hazardous test agents, more sensitive instruments that detect lower concentrations over shorter sampling periods, and increased ability to replicate and repeat the results. The important disadvantages are that simulated tasks may not be representative of real working conditions, fit is not measured over the full workday, and subjects may be unfamiliar with work tasks if not drawn from a representative workforce.
Hauge et al.(8) used two instruments simultaneously measuring particle numbers inside and outside the mask to asses simulated workplace protection factors of healthcare workers while they performed three healthcare tasks (patient assessment, IV treatment, wound care). They identified differences in respirator fit between the healthcare tasks but were unable to compare respirator fit to quantitative fit test results due to the Portacount software (FitPro+, TSI Inc, Shoreview, MN) truncating fit factors at 200 for N95 respirators. This work extends that of Hauge et al. through advancement of knowledge surrounding how quantitative fit factors are predictive of respirator fit during simulated activities.
METHODS
Experimental Set-Up
All tests were conducted in a chamber consisting of two side-by-side 1.5 m (width) x 1.5 m (length) x 2.7 m (height) portable tents with clear plastic sides and zipper access at all corners (total volume = 12 m3) (VUE Canopy, Canopy Max E-Z UP®, Murrieta CA). Three salt aerosol generators (TSI Model 8026, Shoreview MN), two ultrasonic humidifiers used to generate an increased concentration of particles (Vicks V5100ns, Cincinnati, OH and Holmes HM2610, Boca Raton, FL), and a floor fan were used to maintain a steady uniform aerosol concentration inside the test chamber.
Two condensation particle counters (CPCs) consisting of a Portacount Plus Model 8020 (TSI Inc., Shoreview MN) and an electrostatic classifier (N95-Companion™ Model 8095, TSI Inc., Shoreview MN) were used throughout the study: one for measuring one-second particle concentrations inside the respirator and the other for simultaneous one-second measurement of ambient particle concentrations. The limits of detection of the CPCs is 0.01 – 2.5 × 105 particles/cm3. Before and after each experiment, five measurements were taken of the two instruments to ensure a similar (± 15%) and linear response across a range of relevant particle concentrations (300–5000 particles/cm3). The particle concentration in the chamber was altered using particle generators and ultrasonic humidifiers. Each measurement was taken by averaging 30 seconds of particle concentration data obtained from each of the two instruments. A line of best fit across the 10 measurements (five before and five after) was calculated to be used as a correction factor during data analysis.
With assistance, each subject donned a probed N95 filtering facepiece respirator (1860 or 1860s, 3M Company, St Paul, MN) estimated to give the best fit based on facial dimensions.(11) A single pair of sampling tubes was used throughout the experiments; each tube was connected to a separate CPC instrument located inside the chamber. The CPC instruments were connected to a single laptop which collected data from the instruments simultaneously. The laptop was located outside the chamber. A binder clip attached to the subject’s clothing was used to ensure adequate slack in the tubing for head movements without dislodging the respirator.
The two CPCs were first set to count function to allow an initial estimation of respirator fit by comparing displayed outside- and inside-facepiece particle concentration measurements. Count function gives you second-by-second concentrations inside the mask after measuring the ambient concentration of particles. Subjects were instructed to adjust the nose clip and re-position the respirator on the face until an estimated fit factor (outside divided by inside concentration) of 100 was achieved while subjects stood still during normal breathing; if necessary the other respirator size was deployed. The estimated fit may not reflect the fit observed in the study due to not being able to compare to a true ambient concentration and only using one exercise to monitor respirator fit. Subjects not able to achieve an initial estimated fit factor of at least 100 with either respirator size were excluded from the study.
Identifying Healthcare Tasks
In consultation with several key informants, we identified three activities typically performed by healthcare professionals involving head and body motions that might dislodge a respirator: cardiopulmonary resuscitation (CPR), ultrasound examination, and making a hospital bed. A SWPF scenario was developed, consisting of four activities in a set order (normal breathing (30 sec), CPR (90 sec), ultrasound (120 sec), and making a hospital bed (120 sec)), to be repeated three times.
The CPR activity was performed on a torso manikin (Prestan Adult Manikin, Mayfield Village, OH) equipped with indicator lights that signal when compressions are being conducted at the correct rate of 100 per minute. The ultrasound activity required the subject to examine the same manikin using a simulated ultrasound probe while periodically turning their head to observe a simulated ultrasound screen located on the wall to their right. Making a hospital bed involved changing sheets on the table while rotating the manikin, to simulate moving a bed-bound patient.
Subject Recruitment
The goal was to recruit 15 subjects using posted flyers, email, and participants in previous research studies who had agreed to further contact. This pilot project sample size of 15 subjects was chosen to ease time and financial constraints. Initial screening was conducted by telephone or email to assess health conditions and willingness to be clean shaven and refrain from smoking and drinking at least 60 min prior to a test. Subjects were scheduled for a one-hour time period. No compensation was offered. There was no expectation that subjects had prior healthcare or respirator experience. Human subjects’ approval was obtained from the Institutional Review Board prior to recruitment (approval number 2013–1160).
Upon arrival each subject completed a written survey with questions similar to those used in screening, ensuring they had no health conditions that would make wearing a respirator difficult, did not experience claustrophobia, did not have facial impediments that would interfere with fit, were clean shaven, and were between 18 and 65. Subjects were asked to confirm they had refrained from eating and smoking at least 60 min prior to testing. Written informed consent was obtained for each subject meeting these criteria.
Face length (menton sellion) and width (bizygomatic breadth) were measured using sliding and spreading calipers (Seritex, East Rutherford, NJ, Models 104 and 106 respectively), to determine each subject’s cell in the NIOSH bivariate fit test panel.(12)
Experimental Protocol
Each subject performed a 29-min routine consisting of an initial 2.5 min fit factor (FF1) (five 30-sec exercises: normal breathing, head side to side, head up and down, talking, and bending over), three repetitions of the SWPF scenario (each consisting of four 6-min activities: normal breathing for 30 sec, CPR for 90 sec, ultrasound for 120 sec, and making a hospital bed for 120 sec), and a final 2.5 min fit factor (FF2) (Figure 1). Richardson et al.(13) demonstrated that the 2.5 min fit test yields fit factors equivalent to the current set of eight OSHA exercises; we selected this test to minimize total experimental time.
Figure 1.
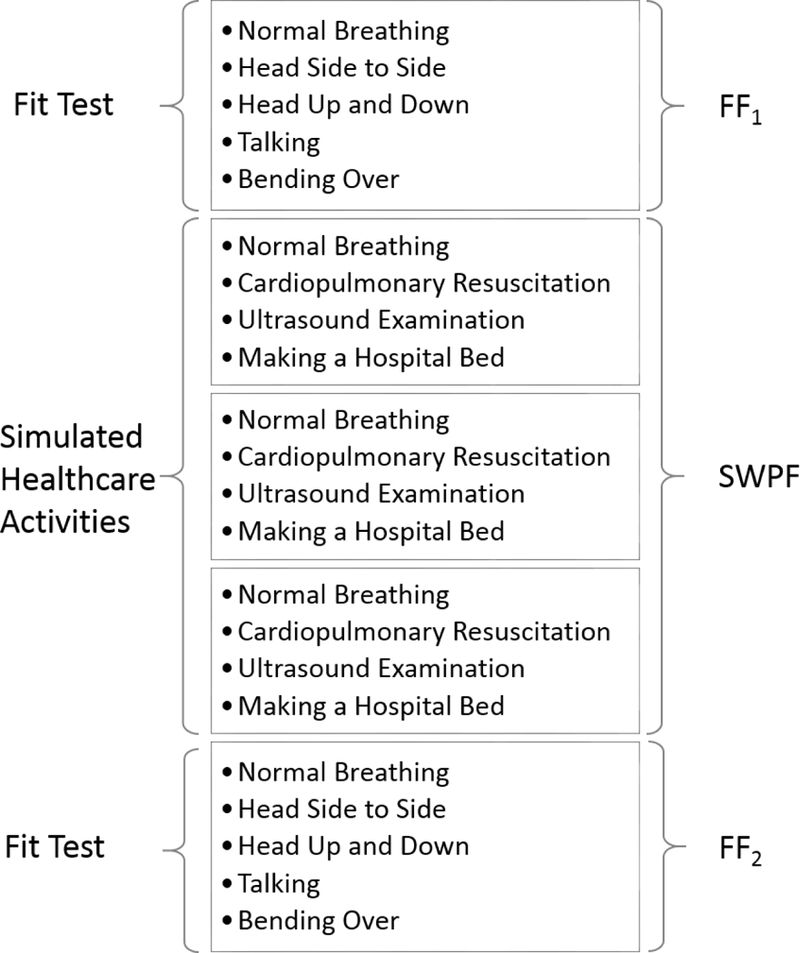
Experimental protocol
Data Analysis
Ambient particle concentrations ranged from 193 to 3850 particles/cm3 and inside mask concentrations ranged from 0 to 634 particles/cm3 when measured with the TSI N95 Companion (Model 8095, TSI Inc., Shoreview MN). Data were transferred to Microsoft Excel spreadsheets for data cleaning and preliminary analyses. Inside-mask data points that were below the limit of detection were replaced with a concentration of 1 particle/cm3 for consistency with test software (FitPro+, TSI Inc., Shoreview MN) protocols. Data from one CPC were then adjusted using the previously described correction factor to ensure instrument comparability.
A second-by-second FF or SWPF was calculated by dividing outside- by inside-facepiece particle concentrations. Data were lognormally distributed; thus, descriptive measures and statistical analyses were conducted with log-transformed data. Geometric means were calculated for each fit test exercise (FF) and each simulated healthcare activity (SWPF). Each subject’s overall, initial, and final FF and SWPF were obtained by calculating the geometric harmonic mean of the five exercise FFs and the three activity SWPFs, respectively. Similarly, overall FF and overall SWPF were calculated as a geometric harmonic mean of FF1 and FF2, or SWPF1, SWPF2, SWPF3, respectively.
Spearman’s rank correlation paired t-tests were used to compare FFs and SWPFs. Boxplots were used to examine the distribution of FFs achieved from a fit test with those achieved during simulated work activities. Backwards selection linear regression models were employed to determine which exercise FFs were most predictive of activity and overall SWPFs.
RESULTS
Subjects
Twenty-one subjects expressed interest; four subjects were unable to participate (three could not match schedules and one did not think they would be able to perform all of the required healthcare tasks). Two subjects were not able to get a good fit with either respirator size and were excluded. Fifteen subjects (seven male and eight female) completed the experimental protocol. Subjects were located in seven of the ten NIOSH bivariate panel cells (one subject in each of cells 1, 5, 6 and 9, five subjects in cell 3, four subjects in cell 4, and two subjects in cell 7).
Fit factors ranged from 72 to 1368; SWPFs ranged from 58 to 1001. The geometric mean (GM) FF was 239 (geometric standard deviation (GSD) = 2.2). The GM SWFF was 227 (GSD = 2.1) (Table 1). Exercise FFs ranged from a GM of 219 for head up-and-down to 275 for head side-to-side. GM SWPFs for each of the four activities ranged from a GM of 211 for CPR to 264 for ultrasound. Fit factors less than 100 were observed because the initial respirator fit to exclude subjects was only estimated based on normal breathing.
Table 1.
Harmonic geometric means (HGM) fit factors (FF) and simulated workplace protection factors (SWPF) by subject.
| Subject | Initial HGM FF |
First Activity HGM SWPF |
Second Activity HGM SWPF |
Third Activity HGM SWPF |
Final HM FF |
Overall HGM FF |
Overall HGM SWPF |
|---|---|---|---|---|---|---|---|
| 1 | 149 | 182 | 175 | 186 | 219 | 177 | 181 |
| 2 | 98 | 68 | 66 | 63 | 88 | 92 | 65 |
| 3 | 582 | 439 | 404 | 461 | 672 | 624 | 433 |
| 4 | 716 | 714 | 458 | 626 | 763 | 739 | 579 |
| 5 | 147 | 265 | 373 | 340 | 190 | 166 | 319 |
| 6 | 264 | 303 | 270 | 292 | 170 | 207 | 288 |
| 7 | 326 | 282 | 245 | 285 | 416 | 366 | 270 |
| 8 | 394 | 409 | 422 | 475 | 267 | 319 | 434 |
| 9 | 209 | 153 | 120 | 117 | 173 | 189 | 128 |
| 10 | 82 | 58 | 62 | 70 | 72 | 77 | 63 |
| 11 | 80 | 87 | 96 | 104 | 102 | 90 | 95 |
| 12 | 161 | 160 | 209 | 273 | 363 | 223 | 204 |
| 13 | 744 | 509 | 666 | 1001 | 1368 | 964 | 672 |
| 14 | 87 | 131 | 137 | 185 | 167 | 115 | 148 |
| 15 | 342 | 405 | 399 | 396 | 385 | 362 | 400 |
The overall FFs and SWPFs were highly correlated (r = 0.88, p < 0.001) (Figure 2). We also found that each exercise FF was highly correlated with the overall SWPF (r > 0.80) (Figure 3).
Figure 2.
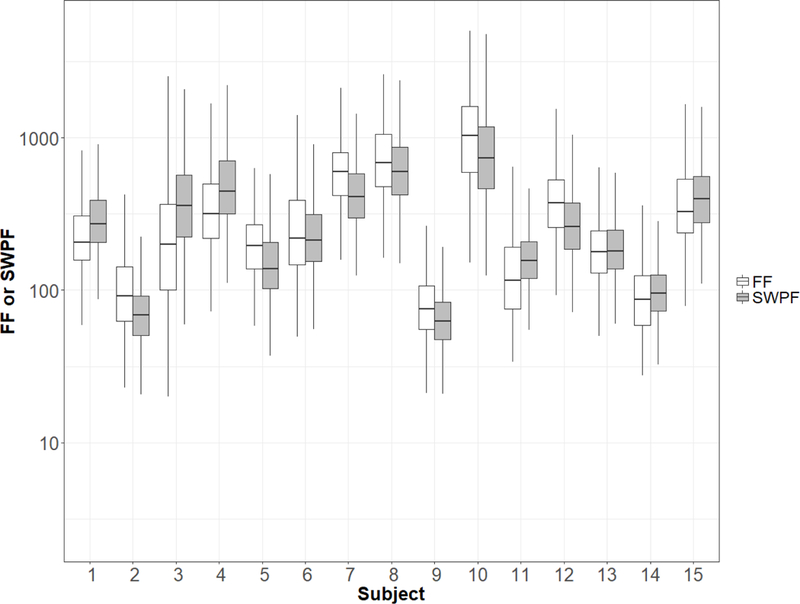
Overall FF and SWPF by subject.
Figure 3.
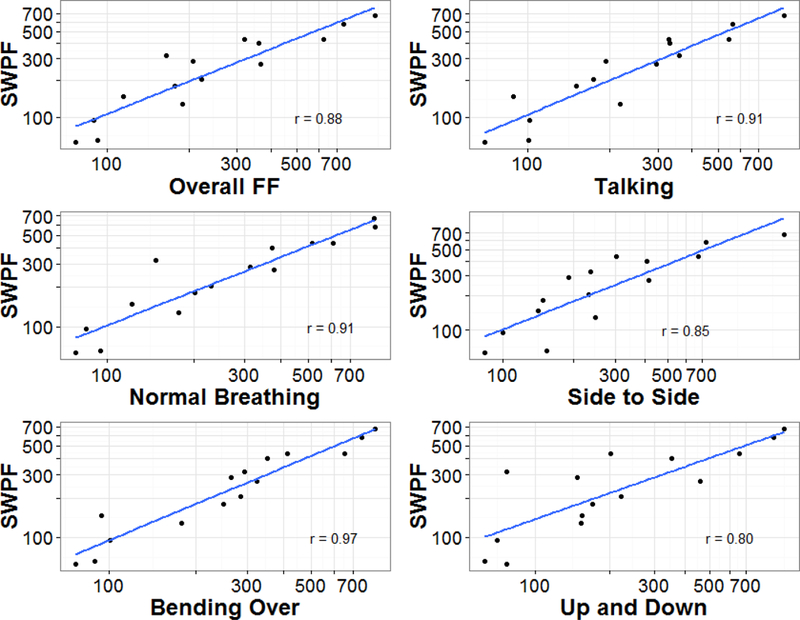
Comparison of overall SWPF to overall FF and to FFs for each exercise (n = 15 subjects).
Multiple linear regression using backward selection indicated that the normal breathing, moving head up-and-down, and talking exercises were most predictive of respirator fit during simulated activities (r2 = 0.96) (Table 2). The bending over exercise, while highly correlated in the single factor regression models, was not an important predictor in the multiple regression model.
Table 2.
Multiple regression model of overall SWPF predicted from fit test exercises.
| Model | Coefficient | Standard Error | p-value |
|---|---|---|---|
| Intercept | 16.32 | 20.92 | 0.45 |
| Normal Breathing | 0.56 | 0.11 | <0.001 |
| Head Up and Down | −0.30 | 0.10 | <0.01 |
| Talking | 0.58 | 0.13 | <0.001 |
Similarly, normal breathing and talking were together predictive of each of the three simulated healthcare activities. For the CPR and bed making activities, head movement exercises (side-to-side or up-and-down, respectively) were also found to be predictive (Table 3).
Table 3.
Multiple regression model of activity SWPFs predicted from fit test exercises.
| Model | Coefficient | Standard Error | p-value |
|---|---|---|---|
| CPR | |||
| Intercept | 31.78 | 28.06 | 0.28 |
| Normal Breathing | 0.42 | 0.12 | 0.005 |
| Head Side to Side | −0.45 | 0.15 | 0.008 |
| Talking | 0.84 | 0.26 | 0.012 |
| BED MAKING | |||
| Intercept | −12.07 | 26.39 | 0.656 |
| Normal Breathing | 0.68 | 0.13 | <0.001 |
| Head Up and Down | −0.72 | 0.12 | <0.001 |
| Talking | 1.07 | 0.16 | <0.001 |
| ULTRASOUND | |||
| Intercept | 6.71 | 20.13 | 0.74 |
| Normal Breathing | 0.59 | 0.10 | <0.001 |
| Talking | 0.44 | 0.11 | 0.002 |
DISCUSSION
Our results suggest that the fit of an N95 filtering facepiece respirator is person-specific (Figures 1 & 2). If subjects achieved a high FF during the initial fit test, they would also experience a high overall SWPF. Hauge et al.(8) found a similar relationship between initial FFs and SWPFs, although statistical comparisons were not possible due to limitations in the FF data. Previous work by these investigators(10) also demonstrated significant correlation between initial FFs, final FFs, and SWPFs.
It should be kept in mind that, in these three studies,(current; 8, 10) the respirator was never doffed between the fit test and simulated workplace activities, suggesting that once a respirator is donned properly, the fit will change only slightly.
Single factor linear regression models showed that the bending over exercise had the highest correlation with the overall SWPF. However, when multiple regression using a backwards selection logic was employed, three fit test exercises - normal breathing, head up-and-down, and talking - were most predictive of respirator fit during simulated healthcare activities. The bending over and head side-to-side exercises did not add any further contributions to the model.
Others have found similar results when comparing the seven OSHA fit test exercises (normal breathing, deep breathing, head side-to-side, head up-and-down, talking, bending over, and normal breathing) to the overall FF. Zhuang et al.(14) showed that talking, head up-and-down, and bending over were each highly correlated with overall fit. Crutchfield et al.(15) demonstrated that talking and bending significantly reduced the fit factor when compared to the initial fit (found during the initial normal breathing exercise).
For this study we employed a fast fit protocol with five exercises (13) rather than the eight exercise protocol described in the OSHA respirator standard.(1) Thus, our analyses do not assess the impact on overall or simulated fit of the deep breathing, grimace or final normal breathing exercises. Deep breathing was not found to be an important feature of overall fit by either Zhuang et al.(14) or Crutchfield et al.;(15) thus, we believe it would have had little impact on fit during simulated healthcare exercises.
The grimace exercise was originally included in the eight exercises to represent facial movements that might unseat the respirator seal on the face followed by a final normal breathing exercise to determine the impact of the grimace. The grimace exercise is not included in calculation of the overall fit factor. As with the deep breathing exercise, neither Zhuang et al.(14) nor Crutchfield et al.(15) found the final normal breathing exercise to be an important predictor of overall fit.
Hauge et al. demonstrated in work using healthcare simulated work activities that the fit of the respirator varies by workplace task.(8) This study expands on that work by offering a more thorough analysis of the relationship between FFs and SWPFs. Future studies should examine additional variables, such as different respirator models, different types of respirators, the effect of training on respirator fit, and different simulated work tasks.
Traditional quantitative assessment of respirator fit uses a single Portacount switching back and forth between inside- and outside-facepiece sampling in order to calculate respirator fit. An important strength of this paper is the innovative use of two side-by-side Portacounts to measure respirator fit in real-time.
Limitations
Several limitations should be noted. The results may not be generalizable to all respirator wearers, because the subject pool did not encompass a full 25 subject bivariate panel; large and small faces were under-represented. Subjects did not remove their respirator between the fit test and simulated healthcare activities; re-donning could have an important impact on respirator fit that was not explored. A preliminary 5-min comfort assessment was not included to keep the experimental protocol within 30 minutes; the comfort assessment allows the respirator to settle on the face of the user so it is likely, if any effect was observed, we underestimated true fit.
This study may not be generalizable to all filtering facepiece respirators as only one manufacturer’s models were employed. This does not negate the usefulness of this study as an early examination of the relationship between FFs and SWPFs.
The fast fit test is currently being considered by OSHA as an additional quantitative fit test protocol.(16) Following the ANSI Z88.10 Annex A2 requirements(17), this new protocol was tested and validated against the current OSHA ambient aerosol condensation nuclei counter fit testing protocol(13), which includes 8 exercises and takes approximately 7 min to complete.(18)
While we recognize that the fast fit test is not currently accepted by OSHA, the study by Richardson et al. strongly supports its comparability to the current OSHA protocol in detecting poor- and well-fitting respirators. Our use of the fast fit test protocol does not negate our study results; our findings were similar to those of Hauge et al. who used an initial 8 exercise fit test.(8)
ACKNOWLEDGMENTS
This project was funded by the Division of Environmental and Occupational Health Sciences, School of Public Health, University of Illinois at Chicago. Margaret Sietsema received support from NIOSH Grant No. T42/OH008672. None of the authors has any financial or other conflicts of interest. We would like to thank 3M and NIOSH for lending Portacounts to our lab and 3M and TSI for performing calibrations on the Portacounts.
REFERENCES
- 1.Occupational Safetyand Health Administration: Respiratory Protection. 29 CFR 1910.134 (1998). [Google Scholar]
- 2.Hyatt EC: Respirator Protection Factors. Los Alamos Scientific Laboratory. LA-6084-MS (1976). [Google Scholar]
- 3.Zhuang Z and Myers WR: Field Performance Measurements of Half-Facepiece Respirators - Paint Spraying Operations. Am. Ind. Hyg. Assoc. J. 57(1):50–51-57 (1996). [DOI] [PubMed] [Google Scholar]
- 4.Myers WR and Zhuang Z: Field Performance Measurements of Half-Facepiece Respirators: Steel Mill Operations. Am. Ind. Hyg. Assoc. J. 59(11):789–795 (1998). [DOI] [PubMed] [Google Scholar]
- 5.Myers WR, Zhuang Z, and Nelson T: Field Performance Measurements of Half-Facepiece Respirators: Foundry Operations. Am. Ind. Hyg. Assoc. J. 57(2):166–174 (1996). [DOI] [PubMed] [Google Scholar]
- 6.Myers WR, Zhuang Z, Nelson T, Sides S, and Wilmes D: Field Performance Measurements of Half-Facepiece Respirators - Study Protocol. Am. Ind. Hyg. Assoc. J. 56(8):765–766- [Google Scholar]
- 7.Janssen L, Nelson T, and Cuta K: Workplace Protection Factors for an N95 Filtering Facepiece Respirator. J. Occup. Environ. Hyg. 4(9):698–707 (2007). [DOI] [PubMed] [Google Scholar]
- 8.Hauge J, Roe M, Brosseau LM, and Colton C: Real-time Fit of a Respirator During Simulated Health Care Tasks. J. Occup. Environ. Hyg.9(10):563–571 (2012). [DOI] [PubMed] [Google Scholar]
- 9.Cohen HJ, Hecker LH, Mattheis DK, Johnson JS, Biermann AH, and Foote KL: Simulated Workplace Protection Factor Study of Powered Air-Purifying and Supplied Air Respirators. Am. Ind. Hyg. Assoc. J. 62(5):595–604 (2001). [DOI] [PubMed] [Google Scholar]
- 10.Sietsema M, Bodurtha P, Dickson E, and Brosseau LM: Evaluating Simulated Workplace Protection Factors for a First Responder Low-Level Protective Ensemble. J. Int. Soc. Resp. Protec. 32(1):(2015). [Google Scholar]
- 11.Zhuang Z, Groce D, Ahlers HW, Iskander W, Landsittel D, Guffey S, et al. : Correlation Between Respirator Fit and Respirator Fit Test Panel Cells by Respirator Size. J. Occup. Environ. Hyg. 5(10):617–628 (2008). [DOI] [PubMed] [Google Scholar]
- 12.Zhuang Z, Bradtmiller B, and Shaffer RE: New Respirator Fit Test Panels Representing the Current US Civilian Work Force. J. Occup. Environ. Hyg. 4(9):647–659 (2007). [DOI] [PubMed] [Google Scholar]
- 13.Richardson AW, Hofacre KC, Weed J, Holm R, and Remiarz RJ: Evaluation of a Faster Fit Testing Method for Filtering Facepiece Respirators Based on the TSI PortaCount. J. Int. Soc. Resp. Protec.31(1):43 (2014). [Google Scholar]
- 14.Zhuang Z, Coffey C, and Lawrence RB: The Effect of Ambient Aerosol Concentration and Exercise on Portacount Quantitative Fit Factor. J. Int. Soc. Resp. Protec. 21(Spring/Summer):11–12-20 (2004). [Google Scholar]
- 15.Crutchfield CD, Fairbank EO, and Greenstein SL: Effect of Test Exercises and Mask Donning on Measured Respirator Fit. Appl. Occup. Environ. Hyg. 14(12):827–837 (1999). [DOI] [PubMed] [Google Scholar]
- 16.Occupational Safety and Health Administration: Additional Portacount Quantitative Fit-Testing Protocols: Amendment to Respiratory Protection Standard. OSHA-2015–0015:29 CFR Part 1910 (2016). [Google Scholar]
- 17.ANSI: American National Standards Institute (ANSI): ANSI/AIHA Z88.10–2010 – Respirator Fit Testing Methods. [Standard] Fairfax, VA: ANSI, 2010 [Google Scholar]
- 18.OSHA: Respiratory Protection - Appendix A: Fit Testing Procedures. 1910.134 App A (1998).


