Abstract
Cough is the most common presenting symptom in primary care settings. Cough can impact a child's activity level and ability to sleep, play or attend school and is often a source of parental anxiety. Cough in children differs from that in adults in terms of presentation, etiology and management. The majority of cough attacks in children are related to previous upper respiratory tract infections and have a self-limited nature. Cough management strategies should focus on characterizing the cough by means of clinical assessment to identify and address its underlying etiology accurately. Clinical algorithms based on acute/chronic presentation and specific/non-specific causes of cough have been developed to provide guidance for clinical practice. The application of children-specific guidelines for the management of cough can lead to earlier cough resolution and improved parental quality of life. This paper presents the clinical statement of the Saudi Pediatric Pulmonology Association (SPPA) in relation to the management of cough in children.
Keywords: Cough, Guidelines, Children
1. Introduction
Cough is the most common presenting symptom to primary care settings in many countries [1]. Persistent cough is one of the most common reasons for a child to be referred to a pediatrician or respiratory physician. On average, normal children cough 11 times per day when they are well, and this increases in frequency and severity during winter, when upper respiratory tract infections (URTI) are frequent [2]. Cough can impact a child's activity level and ability to sleep well, play or attend school and is often a source of parental anxiety. Cough in children is different from that in adults in terms of duration, presentation, etiology and management (see Table 1 for possible etiologies based on child age). This paper presents the clinical statement of the Saudi Pediatric Pulmonology Association (SPPA) in relation to the management of cough in children.
Table 1.
Common etiologies of chronic cough based on child age.
| Young children (<5 years) | Older children (>5 years) |
|---|---|
| Infections | Asthma |
| Gastroesophageal reflux | Infection |
| Congenital malformation | Post-nasal drip |
| Asthma | Protracted bacterial bronchitis |
| Protracted bacterial bronchitis | Passive smoking |
| Passive smoking & environmental pollution | Bronchiectasis |
| Foreign body inhalation | Psychogenic cough |
2. Pathophysiology
Cough is one of the most important protective reflexes, and it contributes significantly to the innate immunity of the respiratory system by enhancing mucociliary clearance [3]. Cough is under both voluntary and involuntary control. Cough receptors are terminations of vagal afferent nerves located in the larynx, pharynx and tracheobronchial tree. Extrapulmonary sites, such as the external ear, can trigger cough due to stimulation of the auricular branch of the vagus nerve [4]. These receptors send signals back to the cough center in the medulla oblongata, which then triggers the sequence of events that constitutes a cough. Cough mechanics includes three sequential phases: inspiratory, compressive and expiratory [5]. Factors that influence cough efficiency include adequate airway caliber (airway narrowing decreases efficiency, e.g., malacia), mucus properties and respiratory muscle strength [6]. Given that cough is a protective reflex, it is crucial not to suppress it without identifying and treating its underlying cause.
The sensitivity of the cough receptors are modulated by disease state. Up-regulation of cough receptors has been demonstrated after viral URTI, asthma, gastroesophageal reflux disease (GERD), and treatment with angiotensin-converting enzyme inhibitors. This causes cough to be triggered through relatively non-specific provocation [7]. Cough undergoes considerable developmental phases; it can be elicited in 10% of 27-week gestational age preterm infants and up to 90% of full-term infants [8].
3. Defining cough in children
Cough can be defined based on duration of presentation, suggested etiology, and sound quality. The following terms have been used in various publications.
3.1. Duration of cough
Cough classification based on the duration of presentation in children relies on the available data of coughs related to URTI in children [9]. Between 35% and 40% of school age children continue to cough 10 days after the onset of a common cold, and 10% of preschool children continue to cough 25 days after a respiratory tract infection [10]. Most cases of acute cough in children are associated with viral upper respiratory tract infections and do not require specific diagnostic evaluation. There are no studies that have clearly defined when cough should be labeled as chronic or persistent [11]. The definition of chronic cough in children varies and ranges from 3 to 12 weeks based on some published guidelines [11], [12]. The general basis for the definition of chronic cough is based on the fact that the most common etiology for acute/sub-acute cough in children is viral/post-viral URTI; 10% of children with a viral URTI continue to cough for 25 days [10]. It is important to use definitions of cough duration in the context of individual patient presentations, as some serious etiologies of cough require early attention and intervention. We suggest the following definitions:
-
•
Acute: cough lasting less than 4 weeks.
-
•
Chronic: cough lasting more than 4 weeks.
3.2. Etiology of cough
-
•
Normal or expected cough: the occasional daily cough, as described above, or a mild cough that has an obvious cause (e.g., after URTI) and does not require further intervention.
-
•
Specific cough: cough associated with other symptoms and signs suggestive of an underlying problem (see Table 2 for the indicators of specific cough).
-
•
Non-specific cough: dry cough in the absence of an identifiable respiratory disease of known etiology. The majority of cases are due to non-serious etiology (e.g., post-viral cough and/or increased cough receptor sensitivity) and may spontaneously resolve.
Table 2.
Indicators of the presence of specific cough.
|
3.3. Quality of cough
Cough can be classified based on its quality. The quality of a cough is related to either the sound pattern or its dry or wet nature (see Table 3).
-
•
Classically recognized cough sounds: Data on sensitivity and specificity of each classic type of cough are limited. Parents usually are able to describe the pattern of the cough sound or even to provide recordings of their child's cough. Physician's direct observation of cough sound during clinic assessment should always be used to validate the information obtained from the medical history. The pattern of cough sound can help indicate its underlying etiology.
-
•
Wet vs. Dry Cough: The distinction between dry and wet cough can be valid in directing the differential diagnosis of the cough. Clinicians should be aware that dry cough can be converted to wet cough when airway secretions increase. Even when airway secretions are present, young children rarely expectorate sputum, so wet cough, rather than productive cough, is the preferred term. Wet cough indicates an underlying cause of mucous hypersecretion or impaired mucociliary clearance, whereas a dry cough indicates an underlying cause of airway irritation or inflammation or a non-airway cause [13]. Wet cough warrants detailed investigation whenever it becomes chronic or associated with other manifestations (e.g., failure to thrive or clubbing).
Table 3.
Example of cough classification based on the quality of cough sounds.
| Cough characteristic | Possible etiology |
|---|---|
| Dry, staccato | Chlamydophila |
| Wet | Protracted bacterial bronchitis, cystic fibrosis, bronchiectasis, pneumonia, primary ciliary dyskinesia |
| Barking/brassy | Croup, tracheomalacia |
| Barking/honking | Habit/psychogenic |
| Paroxysmal/spasmodic/whoop | Pertussis or pertussis-like syndrome |
4. Assessment of cough in children
4.1. Clinical history & physical examination
Detailed history and physical examination represent the cornerstones of the evaluation of a child complaining of cough. The history should focus on identifying the duration, quality, triggers, progress and diurnal/seasonal variation of the cough, associated symptoms, neonatal history, family history, environmental exposures, in particular second hand smoking (or other irritants e.g., wood smoke exposure), medications and allergy history. Physical examination should be directed at determining the general well-being of the child and should include the measurement of vital signs and growth parameters, a detailed respiratory system (including ENT) examination, determination of nutritional status and examination for certain physical signs (e.g., noisy breathing and clubbing). Efforts should be directed to directly observe cough quality during the clinical assessment and to obtain respiratory samples, if indicated.
4.2. Investigations
-
•
Acute cough: The majority of acute cough attacks in children are related to viral/post-viral URTI and do not require further investigation. A chest radiograph should be considered when signs indicate lower respiratory tract involvement, progressive nature, hemoptysis or features of an undiagnosed chronic respiratory disorder. If an inhaled foreign body is suspected as the cause of an acute cough, then urgent bronchoscopy should be considered [12].
-
•
Chronic cough: Investigations should include chest radiograph and lung function test, at appropriate ages, and a test of bronchodilator responsiveness should be considered, if applicable. The extended investigation should be individualized based on the clinical presentation of each patient (feeding/swallowing assessment for aspiration, immune work-up for immunodeficiency, sweat chloride test for cystic fibrosis, CT scan for bronchiectasis, bronchoscopy for inhaled foreign bodies and/or to obtain bronchoalveolar lavage). For wet cough, an attempt should be made to obtain a sample of sputum. Allergy testing (skin prick or RAST specific testing) may be helpful in determining if a child is atopic [12]. A therapeutic trial of asthma medication can be used as a diagnostic tool for chronic cough in young children, when there is a lack of other objective indicators of asthma. This trial should be monitored and time-bound (6–8 weeks), and medications should be stopped after the trial period if no benefits are observed. However, in otherwise healthy children with an isolated dry cough and no specific disease indicators, empirical trials of anti-asthma, anti-allergic rhinitis and anti-gastroesophageal reflux therapy are unlikely to be beneficial and are generally not recommended [12].
5. Management of cough in children
5.1. General concepts
-
•
The goal should always be to identify an underlying cause of cough in children.
-
•
In the majority of children presenting with cough, the etiology is related to URTI and requires only supportive measures (e.g., antipyretics, good hydration, and saline washes).
-
•
Over-the-counter antitussives, antihistamines and decongestants are as effective as placebo for acute cough and have the potential to cause adverse effects; thus, they should be avoided in children less than 2 years of age. Intranasal steroids can be effective in children with allergic rhinitis presenting with cough during pollen season.
-
•
Bronchodilators are not effective and should be avoided in non-asthmatic children presenting with acute cough.
-
•
Antibiotics are generally not effective and should be avoided in children presenting with acute cough caused by viral URTI. When pertussis infection is diagnosed, macrolide antibiotics should be prescribed early (1–2 weeks of illness).
-
•
Specific causes of acute cough (e.g., asthma, bronchiolitis, croup, and community-acquired pneumonia) should be managed based on the evidence-based guidelines specific for such entities.
-
•
Honey products are a natural and safe therapeutic option with a slight effect that can be considered for acute cough following URTI in children greater than 2 years of age [14], [15].
-
•
Parental and community education is indicted to increase the awareness of the natural course and supportive measures for acute cough caused by URTI in young children.
5.2. Management of chronic cough
-
•
Efforts should be directed to identify the exact underlying cause of chronic cough in children so that a specific management plan can be initiated.
-
•
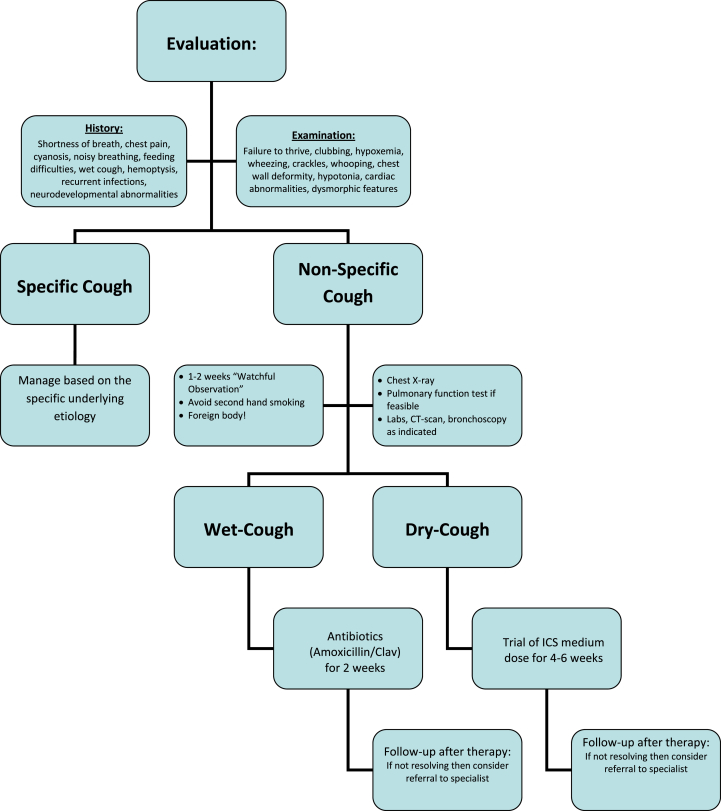
The application of a standardized algorithm in the management of children with chronic cough improves clinical outcomes (earlier cough resolution and improved parental quality of life) [16]. See Fig. 1 for a suggested clinical algorithm for the management of chronic cough in children.
-
•
Evidence-based recommendations should always be applied in the management of specific causes of chronic cough in children (e.g., asthma, cystic fibrosis, primary ciliary dyskinesia, immunodeficiency, and tuberculosis).
-
•
Foreign body inhalation should always be considered in children with chronic cough. This is important, even if a chocking episode was not witnessed, especially if the cough onset was clearly abrupt.
-
•
Protracted (i.e., persistent) bacterial bronchitis has been recently defined as a common cause of chronic cough in children and is defined as a chronic wet cough with positive bronchoalveolar lavage (Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis) that resolves with antibiotic therapy [17]. Other possible diagnoses (e.g., asthma) should be excluded. For these children, a trial of prolonged antibiotics (typically amoxicillin and clavulanate for 2–4 weeks) is recommended. Such children should be followed at the end of the therapeutic trial for assessment of response and consideration of an alternative diagnosis.
-
•
In otherwise healthy children with non-specific chronic cough, the approach of “watchful observation” with follow-up assessment (in 6–8 weeks) is acceptable. Parental assurance is indicated. This is based on the fact that the majority of non-specific chronic cough cases in otherwise healthy children are self-limiting. It is not recommended to apply empirical therapy of specific chronic cough conditions (e.g., asthma, allergic rhinitis and gastroesophageal reflux).
-
•
A diagnostic trial of anti-asthma therapy (namely inhaled corticosteroids) can be considered for bothersome chronic cough cases, especially in situations where objective assessment (e.g., pulmonary function testing) is lacking. It is important to ensure proper use of the therapy (i.e., dosage, device and compliance) and to have a well-defined period for the trial (6–8 weeks) before assessing the patient's response.
-
•
In obviously atopic children with features of allergic rhinitis, the use of inhaled nasal corticosteroids, anti-histamines and allergen avoidance are recommended.
-
•
Children with features suggestive of habit (psychogenic) cough can benefit from psychotherapy, such as suggestion and/or behavioral therapy. Organic causes should be excluded in those children.
Figure 1.
Clinical algorithm for the evaluation and management of chronic cough in children.
5.3. When to consider referral for sub-specialist advice?
General practitioners should consider referring a child to a pediatric pulmonologist for further evaluation in the following situations:
-
•
Chronic wet cough unresponsive to antimicrobial therapy.
-
•
Specific-cough indicating an underlying disease (e.g., cystic fibrosis or primary ciliary dyskinesia).
-
•
Uncertain diagnosis of chronic non-specific cough.
-
•
Partially resolved, prolonged (>3 months) or recurrent protracted bronchitis (>2 times/year).
-
•
Suspicion of foreign body inhalation.
-
•
Suspicion of congenital/developmental defect.
-
•
Chronic cough associated with persistent hypoxemia.
6. Conclusions
Despite the high prevalence of cough in children, the subject has not been thoroughly investigated. Children with cough should be managed according to child-specific guidelines, which are different from adult guidelines. Treatment of cough in children should be based on the cough's underlying etiology.
Conflict of Interest
The authors have no conflicts of interest to disclose.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
References
- 1.Chang A.B. Chronic non-specific cough in children. Paediatr Child Health. 2008;18(7):333–339. [Google Scholar]
- 2.Munyard P., Bush A. How much coughing is normal. Arch Dis Child. 1996;74:531–534. doi: 10.1136/adc.74.6.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartlett J.A., Fischer A.J., McCray P.B., Jr. Innate immune functions of the airway epithelium. Contrib Microbiol. 2008;15:147–163. doi: 10.1159/000136349. [DOI] [PubMed] [Google Scholar]
- 4.Chang A.B. The physiology of cough. Paediatr Respir Rev. 2006;7:2–8. doi: 10.1016/j.prrv.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 5.Hegland K.W., Troche M.S., Daventport P.W. Cough expired volume and airflow rates during sequential induced cough. Front Physiol. 2013;4:167. doi: 10.3389/fphys.2013.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCool F.D. Global physiology and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006 Jan;129(1 Suppl.):48S–53S. doi: 10.1378/chest.129.1_suppl.48S. [DOI] [PubMed] [Google Scholar]
- 7.O'Connell F., Thomas V.E., Studham J.M., Pride N.B., Fuller R.W. Capsaicin cough sensitivity increases during upper respiratory infection. Respir Med. 1996;90:279–286. doi: 10.1016/s0954-6111(96)90099-2. [DOI] [PubMed] [Google Scholar]
- 8.Chang A.B., Widdicombe J.G. Cough throughout life: children, adults and the senile. Pulm Pharmacol Ther. 2007;20:371–382. doi: 10.1016/j.pupt.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Hay A.D., Wilson A.D. The natural history of acute cough in children aged 0 to 4 years in primary care: a systematic review. Br J Gen Pract. 2002;52:401–409. [PMC free article] [PubMed] [Google Scholar]
- 10.Hay A.D., Wilson A., Fahey T., Peters T.J. The duration of acute cough in preschool children presenting to primary care: a prospective cohort study. Fam Pract. 2003;20:696–705. doi: 10.1093/fampra/cmg613. [DOI] [PubMed] [Google Scholar]
- 11.Chang A.B., William B.G. Guidelines for evaluating chronic cough in pediatrics: ACCP evidence-based clinical practice guidelines. Chest. 2006;129:260S–283S. doi: 10.1378/chest.129.1_suppl.260S. [DOI] [PubMed] [Google Scholar]
- 12.Shields M.D., Bush A., Everard M.L., McKenzie S.A., Primhak R. British Thoracic Society Guidelines: recommendations for the assessment and management of cough in children. Thorax. 2008;63(Suppl. III):iii1–iii15. doi: 10.1136/thx.2007.077370. [DOI] [PubMed] [Google Scholar]
- 13.Shields M.D., Doherty G.M. Chronic cough in children. Paediatr Respir Rev. 2013 Jun;14(2):100–105. doi: 10.1016/j.prrv.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Allan M.G., Korownyk C., Kolber M. Do cough suppressants or honey help pediatric cough. Can Fam Physician. 2011 Apr;57(4):435. [PMC free article] [PubMed] [Google Scholar]
- 15.Cohen H.A., Rozen J., Kristal H., Laks Y., Berkovitch M., Usiel Y. Effect of honey on nocturnal cough and sleep quality: a double-blind, randomized, placebo-controlled study. Pediatrics. 2012 Sep;130(3):465–471. doi: 10.1542/peds.2011-3075. doi: 10. [DOI] [PubMed] [Google Scholar]
- 16.Chang A.B., Robertson C.F., Van Asperen P.P., Glasgow N.J., Masters I.B., Teoh L. A cough algorithm for chronic cough in children: a multicenter, randomized controlled study. Pediatrics. 2013 May;131(5):e1576–e1583. doi: 10.1542/peds.2012-3318. [DOI] [PubMed] [Google Scholar]
- 17.Goldsobel A.B., Chipps B.E. Cough in the pediatric population. J Pediatr. 2010 Mar;156(3):352–358. doi: 10.1016/j.jpeds.2009.12.004. [DOI] [PubMed] [Google Scholar]