Abstract
Pott's puffy tumor (PPT) is a very rare, nearly forgotten condition. We describe a 9-year-old girl with PPT due to trauma and surgical cultures that revealed Aspergillus fumigatus.
Keywords: Potts puffy tumor, Sinusitis, Osteomyelitis, Aspergillus fumigatus
1. Introduction
Pott's puffy tumor (PPT) is a condition that is characterized by frontal bone osteomyelitis, which may be associated with sub periosteal abscess [1]. An English surgeon, Sir Percival Pott, first described Pott's puffy tumor in 1760 and explained it in his own words as “a puffy, circumscribed, indolent tumor of the scalp, and a spontaneous separation of the pericranium from the skull under such a tumor” [2]. Sir Pott initially thought that trauma was the only cause for this condition, but he later discovered that frontal sinus infection is the leading cause of PPT. Due to the wide use of broad spectrum antibiotics, its incidence has dramatically decreased [3], but the exact incidence is unknown. However, Clayman et al found that PPT may be seen in up to 0.5% of cases of acute and chronic sinusitis [4], [5].
The infection in PPT typically spreads from the frontal sinus into the frontal bone via direct extension or through septic emboli [3].
PPT can affect all age groups and has a male: female ratio of 9:1. It is noted that adolescents are affected more frequently. This is thought to be due to high vascularity of the diploic venous system, and the accelerated growth of the frontal bone at this particular age [6], [7], [8]. The most common factors leading to PPT are frontal sinusitis and trauma [9]. Other rare etiologies include hematogenous spread of sinusitis, retrograde thrombophlebitis through the diploic veins, or even an insect bite [10], [11]. Signs and symptoms of PPT include forehead swelling and frontal headaches with or without fever. These clinical manifestations usually progress slowly, however, rapid progression may suggest the development of complications [12]. The most common cultured organisms are the same organisms causing chronic sinusitis: streptococci, staphylococci, and anaerobes [13].
PPT is a serious condition because it is associated with high rate of intracranial complications such as meningitis, subdural and epidural empyema, cerebral abscess, and cavernous sinus thrombosis or superior sagittal sinus thrombosis [14], [15]. The diagnostic modality is the contrast enhanced CT scan of the brain and sinuses. The most important aspect in the management of PPT is early diagnosis, early use of proper antimicrobial therapy, and urgent surgical intervention to prevent serious complications [16], [17], [18].
2. Case report
A previously healthy 9-year-old girl presented with a one-month history of intermittent moderate frontal headaches after head trauma. She stated: “A swing fell over her forehead”. She subsequently developed forehead swelling, which was later diagnosed as frontal sinusitis. She made a complete recovery after a course of oral antibiotic. Two weeks later, the swelling reappeared, and she was treated with a course of both IV and oral antibiotics but without significant improvement. She denied any history of fever, nasal discharge, or cough.
Upon examination, she had an undulating erythematous firm swelling over the right frontal area with mild right periorbital swelling (Figure 1, Figure 2). Normal pupillary reflexes and extra-ocular eye movements were intact. There were no meningeal signs that were elicited, and no neurological deficits were present.
Figure 1.

Frontal view of fluctuant firm swelling over the right frontal area with mild right periorbital swelling.
Figure 2.

Lateral view of Fluctuant firm swelling over the right frontal area with mild right periorbital swelling.
Laboratory tests showed a normal CBC and normal inflammatory markers.
Brain imaging including a CT scan and MRI showed signs of frontal bone osteomyelitis with sequestrum formation and abnormal communication between the two frontal sinuses, both of which were filled with fluid (Fig. 3).
Figure 3.
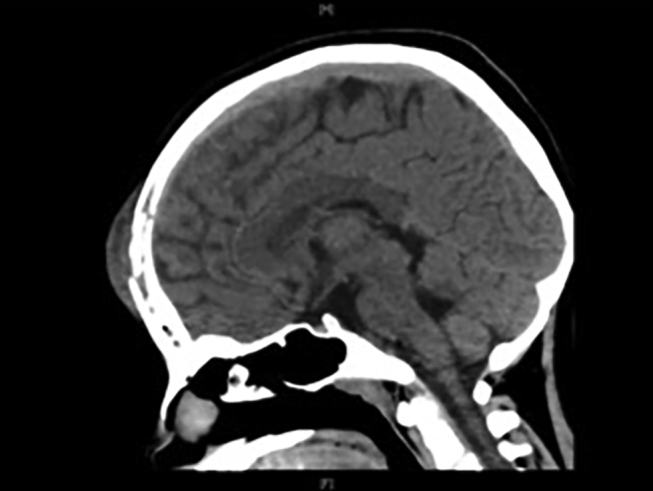
Computed tomography of the brain (CT scan) showing frontal bone osteomyelitis with sequestrum formation and abnormal communication between the two frontal sinuses, both filled with fluid.
A multidisciplinary approach was conducted that involved pediatric infectious diseases, ENT and neurosurgery. The patient was empirically treated with broad spectrum intravenous (IV) antibiotics Clindamycin and ceftriaxone.
Urgent surgical intervention was done by functional endoscopic sinus surgery (FESS) and a craniotomy with a flap to repair the defect (Fig. 4).
Figure 4.

Post functional endoscopic sinus surgery (FESS) and craniotomy with flap to repair the defect.
Sterile culture from the frontal bone, which was taken intra-operatively, grew Aspergillus fumigatus. Bone histopathology showed fungal hyphae. Voriconazole was initiated with a high dose (9 mg/kg/dose) every 12 h. She was kept on the voriconazole for 6 months because of the chronic nature of the osteomyelitis. Laboratory tests were used to closely monitor for signs of voriconazole toxicity. Fortunately, there was no toxicity detected. She showed significant improvement with complete clinical and radiological resolution at the end of her six-month treatment.
3. Discussion
Pott's puffy tumor is a very rare condition and nothing from previously reported cases detailed fungal species as a causative agent. However, the most commonly cultured organisms in PPT are Streptococci, mainly Streptococcus milleri which was found in approximately 50% of the reported cases, Staphylococci, anaerobes, namely Fusobacterium and Bacteroides, and less commonly Proteus and Pseudomonas [11], [19], [20], [21], [22], [23]. In our case, the surgical culture from the frontal bone grew A. fumigatus, which is abnormal to have grown as a fungal organism in an immunocompetent individual.
In regards to diagnosis, computed tomography (CT) of the brain is the best diagnostic modality in such cases. It helps in the critical assessment of the sinuses as well as gauging the extent of the disease to rule out any intracranial complications [24], [25]. In our case, a brain CT scan showed signs of frontal bone osteomyelitis with sequestrum formation, which indicated a chronic infection, and an abnormal communication between the two frontal sinuses, which were both filled with fluid, which could be a posttraumatic occurrence.
Pott's puffy tumor is considered to be an emergency medical condition, and broad spectrum antibiotics should be initiated as soon as possible along with urgent surgical intervention which may include: sinus wash-outs, percutaneous aspiration, trepanation, endoscopic sinus surgery, or craniotomy [23]. Functional endoscopic sinus surgery is a safe and less invasive surgical procedure [26], [27]. The decision of whether or not a craniotomy is indicated depends on the size of the intracranial fluid collection [28].
In our case, a combined surgical approach was coordinated by ENT and neurosurgery. FEES along with craniotomy, aspiration of the sub periosteal collection, sequestrectomy, and frontal bone debridement were all conducted at the same time.
Furthermore, antimicrobial therapy should be tailored according to the cultured organism [29]. In our case, we started voriconazole which is an antifungal agent that is known to be fungicidal against most of the Aspergillus species.
Furthermore, a high dose of voriconazole is the best regimen for such condition [30].
We conclude that although PPT is rare, it still must be part of the differential diagnosis of forehead swelling and headache, especially if it was preceded by sinusitis or trauma. Broad spectrum antimicrobial therapy should be initiated immediately after surgical intervention. Adequate sampling should be attained for cultures, and serious consideration should be given to the possibility of fungal infections.
Conflict of interest
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
Contributor Information
Zainab Abdulaziz AlMoosa, Email: zay.almo@hotmail.com.
Tariq AlFawaz, Email: talfawaz@kfmc.med.sa.
Fahad AlFawaz, Email: falfawaz@kfmc.med.sa.
References
- 1.Skomro R., McClean K.L. Frontal osteomyelitis (Pott's puffy tumour) associated with Pasteurella multocida: a case report and review of the literature. Can J Infect Dis. 1998;9:115–121. doi: 10.1155/1998/457984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pott P. The chirurgical works of Percivall Pott. Wood and Innes 1808; 1.
- 3.Pott P. Observations on the Nature and Consequences of Wounds and Contusions of the Head. C Hitch and L Hawes 1760.
- 4.Clayman G.L., Adams G.L., Paugh D.R., Koopmann C.F., Jr. Intracranial complications of paranasal sinusitis: a combined institutional review. Laryngoscope. 1991;101:234–239. doi: 10.1288/00005537-199103000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Domville Lewis C. Pott's puffy tumour and intracranial complications of frontal sinusitis in pregnancy. J Laryngology Otology. 2013;127:35–38. doi: 10.1017/S0022215112001673. [DOI] [PubMed] [Google Scholar]
- 6.Shehu B.B., Mahmud M.R. Pott's puffy tumour: a case report. Ann Afr Med. 2008;7:138–140. doi: 10.4103/1596-3519.55663. [DOI] [PubMed] [Google Scholar]
- 7.Furstenberg A.C. Osteomyelitis of the skull. Ann Otol. 1931;40:996–1012. [Google Scholar]
- 8.Woodward F.D. Osteomyelitis of skull. JAMA. 1930;95:927. [Google Scholar]
- 9.Emejulu J.C., Ekweogwu O.C. Complicated Pott's Puffy Tumour Involving both Frontal and Parietal Bones: A Case Report. J Infect Dis Ther. 2014;2(5):166. [Google Scholar]
- 10.Steele R.W., Ward K.J. A “Hickey”. Clin Pediatr. 2003;42:657–660. doi: 10.1177/000992280304200715. [DOI] [PubMed] [Google Scholar]
- 11.Raja V., Low C., Sastry A., Mariarty B. Pott's puffy tumor following an insect bite. J Postgrad Med. 2007;53(2):114–116. doi: 10.4103/0022-3859.32212. [DOI] [PubMed] [Google Scholar]
- 12.Forgie Sarah E. Pott's puffy tumor. Am J Med. 2008;121(12) doi: 10.1016/j.amjmed.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 13.Verbon A., Husni R.N., Gordon S.M., Lavertu P., Keys T.F. Pott's puffy tumor due to Haemophilus influenzae: case report and review. Clin Infect Dis. 1996;23:1305–1307. doi: 10.1093/clinids/23.6.1305. [DOI] [PubMed] [Google Scholar]
- 14.Tsai B.Y., Lin K.L., Lin T.Y., Chiu C.H., Lee W.J., Hsia S.H. Pott's puffy tumor in children. Childs Nerv Syst. 2010;26:53–60. doi: 10.1007/s00381-009-0954-z. [DOI] [PubMed] [Google Scholar]
- 15.Gupta M., El-Hakim H., Bhargava R., Mehta V. Pott's puffy tumour in a pre-adolescent child: the youngest reported in the post-antibiotic era. Int J Pediatr Otorhinolaryngol. 2004;68(3):373–378. doi: 10.1016/j.ijporl.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 16.Parida Pradipta Kumar. Pott's puffy tumor in pediatric age group: a retrospective study. Int J Pediatr Otorhinolaryngol. 2012;76:1274–1277. doi: 10.1016/j.ijporl.2012.05.018. [DOI] [PubMed] [Google Scholar]
- 17.Shah P., Mishriki Y.Y. The puffy periorbital protrusion: Pott's puffy tumor. Postgrad Med. 1999;105:45–46. doi: 10.3810/pgm.1999.04.713. [DOI] [PubMed] [Google Scholar]
- 18.Mammen-Prasad E., Murillo J.L., Titelbaum J.A. Infectious disease rounds: Pott's puffy tumor with intracranial complications. N J Med. 1992;89:537–539. [PubMed] [Google Scholar]
- 19.Khan M.A. Pott's puffy tumor: a rare complication of mastoiditis. Pediatr Neurosurg. 2006;42(2):125–128. doi: 10.1159/000090469. [DOI] [PubMed] [Google Scholar]
- 20.Wu C.T., Huang J.L., Hsia S.H., Lee H.Y., Lin J.J. Pott's puffy tumor after acupuncture therapy. Eur J Pediatr. 2009;168(9):1147–1149. doi: 10.1007/s00431-008-0892-x. [DOI] [PubMed] [Google Scholar]
- 21.Marshall A.H., Jones N.S. Osteomyelitis of the frontal bone secondary to frontal sinusitis. J Laryngol Otol. 2000;114:944–946. doi: 10.1258/0022215001904671. [DOI] [PubMed] [Google Scholar]
- 22.Gallagher R.M., Gross C.W., Phillips C.D. Suppurative intracranial complications of sinusitis. Laryngoscope. 1998;108:1635–1642. doi: 10.1097/00005537-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Fenton J.E., Smyth D.A., Viani L.G., Walsh M.A. Sinogenic brain abscess. Am J Rhinol. 1999;13:299–302. doi: 10.2500/105065899782102854. [DOI] [PubMed] [Google Scholar]
- 24.Huijssoon E., Woerdeman P.A., Van Diemen- Steenvoorde R.A.A.M., Hanlo P.W., Plötz F.B. An 8-year-old boy with a Pott's puffy tumor. Int J Pediatr Otorhinolaryngol. 2003;67(9):1023–1026. doi: 10.1016/s0165-5876(03)00183-6. [DOI] [PubMed] [Google Scholar]
- 25.Martinez-Diaz G.J., Hsia R. Pott's Puffy tumor after minor head trauma. Am J Emerg Med. 2008;26(6):739. doi: 10.1016/j.ajem.2007.11.038. [DOI] [PubMed] [Google Scholar]
- 26.Blackman S.C., Schleiss M.R. Forehead swelling caused by Pott's puffy tumor in a 9-year-old boy with sinusitis. Pediatr Int. 2005;47(6):704–707. doi: 10.1111/j.1442-200x.2005.02129.x. [DOI] [PubMed] [Google Scholar]
- 27.Suwan Phillip T. Pott's puffy tumor: an uncommon clinical entity. Case Rep Pediatr. 2012;2012:4. doi: 10.1155/2012/386104. Article ID 386104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DelGaudio J.M., Evans S.H., Sobol S.E., Parikh S.L. Intracranial complications of sinusitis: what is the role of endoscopic sinus surgery in the acute setting. Am J Otolaryngol. 2010;31:25–28. doi: 10.1016/j.amjoto.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 29.McDermott C., O'Sullivan R., McMahon G. An unusual cause of headache: Pott's puffy tumor. Eur J Emerg Med. 2007;14(3):170–173. doi: 10.1097/MEJ.0b013e32801482ea. [DOI] [PubMed] [Google Scholar]
- 30.Dornbusch Hans Jürgen. Invasive fungal infections in children. Pediatr Infect Dis J. 2009;28:734–737. doi: 10.1097/INF.0b013e3181b076b1. [DOI] [PubMed] [Google Scholar]


