Abstract
Osteoporosis is a serious public health concern worldwide, and community-based public health programs that increase osteoporosis preventive behaviors are ideal to combat this major public health issue. A review of community-based public health programs for osteoporosis prevention show that programs vary in numerous ways and have mixed results in increasing osteoporosis preventive behaviors, although most programs have had success in significantly increasing calcium intake, only a few programs have had success in significantly increasing weight-bearing exercise. Regarding calcium intake, all community-based public health programs that implemented: 1) at least one theoretical behavior change model, such as the health belief model, or 2) bone mineral density (BMD) testing for osteoporosis screening, have shown success in significantly increasing calcium intake. As community-based public health programs for osteoporosis prevention have shown limited success in increasing weight-bearing exercise, an additional review of community-based public health programs incorporating osteoporosis exercise showed that they have high compliance rates to increase weight-bearing exercise, but require high-intensity weight-bearing exercise of 80–85% 1-repetition maximum to significantly increase BMD to prevent osteoporosis. In the prevention of osteoporosis, for community-based public health programs to be most effective, they should implement theoretical behavior change models and/or BMD testing for osteoporosis screening, along with high-intensity resistance training. Recommendations for future research to further study effective community-based public health programs are also provided.
Keywords: Osteoporosis, Prevention, Calcium, Exercise, Community-based
1. Introduction
Osteoporosis is a severe bone disease that increases morbidity and mortality in individuals, and it is also a serious public health concern in populations all around the world. Osteoporosis is clinically diagnosed as having a bone mineral density (BMD) of 2.5 standard deviations below the adult peak mean [1], which weakens bones and makes them more susceptible to fragility fractures, particularly in the hip, spine, and wrist. Osteoporosis is currently incurable as there is no treatment that can fully replenish reduced BMD cause by the disease. This disease decreases the quality of life from reduced independence and hindered physical, mental, and social well-being [2], as well as increased frailty, morbidity, and mortality in individuals diagnosed with it [3], [4]. The United States Surgeon General has addressed the importance of promoting bone health and preventing osteoporosis in public health [5], as it has become both a national public health issue affecting 50 million Americans in the United States [6], as well as a global public health issue affecting hundreds of millions of individuals worldwide [7]. Osteoporosis and osteoporotic fractures, especially hip fractures, can lead to permanent physical disability, decreased self-sufficiency, hospitalization, and increased mortality, requiring the need for public health osteoporosis prevention interventions to prevent the disease and premature death [4].
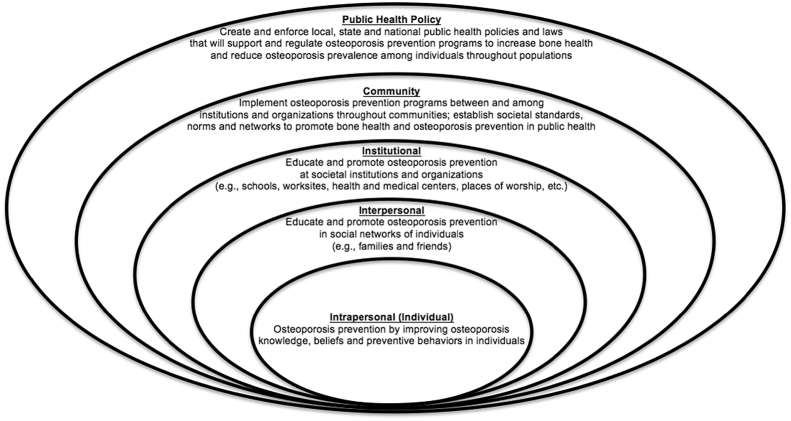
Fortunately, the National Institute of Health Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy [8] states that although osteoporosis affects all populations, this disease is preventable by achieving maximal BMD with the osteoporosis preventive behaviors of adequate calcium intake and weight-bearing exercise. Therefore, to combat this global public health problem, public health leadership should place focus on preventing osteoporosis with the implementation of strategies that increase these osteoporosis preventive behaviors throughout populations [9]. For instance, community-based public health programs for osteoporosis prevention will be more impactful towards improving the bone health of populations than the more common individual-based health care programs. Most osteoporosis prevention programs are designed to prevent or manage the disease in individuals, but in order to have a greater impact and prevent the disease among populations, osteoporosis prevention programs must be implemented for communities, not just for individuals. Based on the social ecological model by McLeroy, Bibeau, Steckler and Glanz [10], when adapted for osteoporosis prevention in public health (see Fig. 1), the least direct link to prevent osteoporosis in public health is through the individual approach; however, the most direct connection is through the community, such as with community-based public health programs for osteoporosis prevention, that will directly lead to public health policies to improve bone health in populations. To establish public health policies that successfully promote bone health and reduce the prevalence of osteoporosis in populations, a review of the literature was conducted with the objective to assess the effectiveness of community-based public health programs for osteoporosis prevention, in order to provide evidence-based recommendations that support and regulate public health policies.
Fig. 1.
Social ecological model for osteoporosis prevention in public health.
2. Osteoporosis prevention in community-based public health programs
2.1. Community-based public health programs for osteoporosis prevention effectiveness on increasing calcium intake and weight-bearing exercise
To assess the effectiveness of community-based public health programs for osteoporosis prevention, a review of the literature was conducted with a search in four databases: PubMed (United States National Library of Medicine at the National Institutes of Health), PsycINFO (American Psychological Association), ERIC (Education Resources Information Center: Institute of Education Sciences of the United States Department of Education), and Google Scholar. Search terms entered into these databases were “osteoporosis community,” and after a thorough review of all search results, 14 studies were found to be community-based public health programs for osteoporosis prevention, as each included analysis to assess effectiveness of a community-based osteoporosis prevention intervention designed to increase osteoporosis preventive behaviors. Table 1 provides specifics of different aspects of 14 studies on community-based public health programs for osteoporosis prevention found in the review of the literature [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24]. Various study designs were used to investigate their effectiveness of increasing osteoporosis preventive behaviors that included the use of experimental, intervention, and prospective cohort designs, and the duration of these studies varied from as short as 6 weeks to as long as 5 years, with 1 study not reporting duration. The community-based public health programs for osteoporosis prevention studies were also conducted in various community settings and in various locations globally, including locations in North America, Europe, Asia, and Australia, which were expected as osteoporosis affects hundreds of millions of individuals worldwide. The specific designs and implementations of the studied community-based public health programs for osteoporosis prevention varied from study to study, with various components used in different studies that included, but were not limited to, BMD testing for osteoporosis screening, use of theoretical behavior change models, lectures and lessons on various osteoporosis-related topics, presentations, demonstrations, counseling, group discussions, and hands-on activities. All 14 studies included participants that were women who were mostly older adults, with only 6 that included men that were mostly a very small portion of the total participants in their respective studies.
Table 1.
Community-based public health programs for osteoporosis prevention on osteoporosis preventive behaviors.
| Study reference (n = 14) | Study design and duration | Setting and location | Depictions and description of participants | Details and description of community-based public health program for osteoporosis prevention | Types and outcomes of osteoporosis preventive behaviors |
|---|---|---|---|---|---|
| Oh et al., 2014 [11] | Experimental Study, 12 weeks | Rural Community; Community Health Care Center in One Province in South Korea | Treatment Group that received intervention (n = 21): Postmenopausal Korean women, mean age = 65.95 years old (S.D. ± 8.59). Individuals with osteoporosis at pretest (n = 7, 33%) | Therapeutic Lifestyle Modification (TLM) with 4 parts: (1) Individualized Health Monitoring – general health assessment, blood pressure, pulse rate, body weight, food diary [all twice weekly]; (2) Group Health Education – osteoporosis definition, risk factors, diagnosis and classification, symptoms and treatment, management and prevention; calcium intake for bone health, exercise for bone health pts. 1 & 2, osteoporotic fracture prevention [each 2 weeks]; (3) Group Exercise – “Be BoneWise” warm-up stretching, rhythm aerobics, resistance band strength training, floor exercise, cool-down exercise [twice weekly]; (4) calcium-vitamin D supplementation – 600 mg calcium carbonate and 400 IU vitamin D [daily] | At Posttest – (1) Calcium Intake: Significant increase in the intake of dairy foods (p < 0.001), calcium-rish fish (p < 0.001), nuts (p < 0.001), and vitamin D-rich foods such as fish (p < 0.001) and vegetables (p < 0.001) in the TLM group, but slightly in the control group. (2) Weight-Bearing Exercise: Significant increase in regular weekly exercise (p = 0.005) in TLM group at baseline and among the control group |
| Plawecki & Chapman-Novakofski, 2013 [12] | Experimental Study, 8 weeks | Osher Lifelong Learning Institute at the University of Illinois at Urbana–Champaign; Illinois, United States | Treatment Group that received intervention (n = 35). Article included description and demographic information for total participants in the study, but did not include separate description and demographic information for the treatment and control group. For all participants, mean age = 65.5 years old (S.D. ± 9.6), 83% female, 90% White, 53% retired, 67% with no history of osteoporosis (but did not specify if meant individual and/or family history of osteoporosis), and 81% had previous bone scan | Bone health program based on 2 theoretical behavioral change theories: Health Belief Model (HBM) and Theory of Reasoned Action (TRA). Each week consisted of 1-h sessions of topics that included lectures with hands-on active learning. Sessions 1–8: (Topic in quotations with Activities): (1) “Overview of Bone Health, Severity of Bone Health” with bone density testing; (2) “Susceptibility to Osteoporosis and Risk Factors” with body frame measurement and risk factor quiz; (3) “Overcoming Barriers to Reducing Risk Factor: Healthy Bone Diet” with serving size estimation and meal planning; (4) “Self-Efficacy: Achieving Benefits From Reducing Risk Factors: Healthy Bone Diet” with food label critique taste tests; (5) “Overcoming Barriers to Reducing Risk Factors: Improving Exercise Habits” with heel drops; (6) “Overcoming Barriers to Reducing Risk Factors: Fall Prevention & Balance” with balance and posture exercises; (7) “Medications, Supplements & Soy” with smoothie taste testing; (8) “Better Bone Graduate” with bone healthy meal “Bone Health Jeopardy” | At Posttest – (1) Calcium Intake: Significant increase in calcium intake (p = 0.005, p = 0.001) and vitamin D intake (p < 0.001) in the treatment group from the start to the end of the study, but there was no significant difference between the treatment and the control group at the end of the study. (2) Weight-Bearing Exercise: No significant difference in the treatment or control group |
| Babatunde, Himburg, Newman, Campa, & Dixon, 2011 [13] | Experimental Study, 6 weeks | Church and community-based organizations; 3 south Florida counties, United States | Treatment Group that received intervention (n = 59). All Black adults, 51 women and 8 men, ages 50–92 years of age with mean age = 70.2 years old | Program based on a revised HBM. Each week consisted of 30–45 min lessons of topics that included short presentations/lectures, hands-on activities, and demonstrations involving participants to increase their self-efficacy. Lessons 1–6: (1) Severity of osteoporosis; (2) Susceptibility of osteoporosis; (3) Benefits of changing calcium intake [with hands-on activities]; (4) Barriers to reducing risk factors (calcium intake) – lactose intolerance [with hands-in activities]; (5) Barriers to reducing risk factors – improving vitamin D, reducing alcohol intake and smoking, supplements considerations [with hands-on activities]; (6) Facts and fallacies or additional considerations – other dietary considerations, medications, and bone density testing, with a summary | At Posttest – (1) Calcium Intake: Significant increase in calcium intake (p < 0.001) in the treatment group, but not the control group (wait-list group) |
| Teems, Hausman, Fischer, Lee, & Johnson, 2011 [14] | Intervention Study (Non-Experimental), 16 weeks | Senior Centers; Georgia, United States | 691 participants, mean age = 74.7 years old (S.D. ± 7.8), 83.9% women and 16.1% men; 53.7% White, 45.6% Black, 0.7% Other | Program based on the HBM. 16 wellness lectures with 8 lessons about fall and fracture prevention, each administered once and lasting 45–60 min and incorporated 30 min of physical activity. Lessons 1–8: (Title in quotations and topics) (1) “Five Goals to Fight Falls and Fractures-First Talk To My Doctor” about osteoporosis risk factors and consequences; and introduction to 5 key messages of the program (a) be physically active, (b) eat healthy and use calcium and vitamin D supplements if needed, (c) take doctor-recommended medicines, (d) fall prevention at home, (e) discuss medications, fall risk, vision, bone mineral testing with doctor; (2) “Be Physically Active Everyday” about physical activity benefits; (3) “Calcium and Vitamin D Supplements-Part of Healthy Eating” about reading supplement labels and determining amounts needed; (4) “Eat Healthy-Calcium and Vitamin D in Foods” about calcium and vitamin D sources, lactose intolerance; (5) “Eat Healthy-Other Foods for Bone Health” about foods that positively/negatively affect bone; (6) “Take My Medicines” about medications that treat osteoporosis and increase fall risk; (7) “Fight Falls with a Safe Home” about improving home safety and preventing falls; (8) “Putting it All Together to Fight Falls and Fractures” that reviewed the 5 key messages from Lesson 1 | At Posttest – (1) Calcium Intake: Significant increase in the intake of calcium-rich and vitamin D-rich foods (p < 0.001) as well as use of calcium and vitamin D supplements (p < 0.001). (2) Weight-Bearing Exercise: Significant increase in days of week of physical activity (p < 0.001). (3) Other: Significant increase in fall preventive home safety behaviors (p < 0.001) |
| Francis, Matthews, Van Mechelen, Bennell, & Osborne, 2009 [15] | Experimental Study, 6 weeks | Australian community; Australia | Treatment group that received the intervention (n = 103). Article included description and demographic information for total participants in the study, but did not include separate description and demographic information for the treatment and control group. For all participants, mean age = 63 years old, 92% women | The Osteoporosis Prevention and Self-Management Course (OPSMC). Participants received “Everybody's Bones” course manual and attended 4 weekly 2–2.5 h sessions for first 4 weeks (posttest 2 weeks after 4th week). Sessions 1–4: (1) Participants identify what osteoporosis means to them and motivational factors for attending, introduction to self-management and osteoporosis [basic bone physiology and osteoporosis consequences], dispelling myths, weight-bearing physical activity benefits and different forms of exercise, starting a personal exercise regimen, and goal setting for osteoporosis prevention or management; (2) Action plan feedback and problem solving, examine osteoporosis risk factors [modifiable and unmodifiable], the importance of exercise and solutions for common obstacles to exercise, and reviewing calcium and how to acquire recommended levels even for lactose intolerance, calcium supplements, and action planning; (3) Bone density measurement techniques and for those who need it, managing emotions, osteoporosis medications, communicating with healthcare professionals, and action planning; (4) Good posture and safe bending/lifting demonstrations, pain management review, outside and local support groups, longer-term goals, review of topics covered in all 4 sessions | At Posttest – (1) Other: Health-Directed Behavior: Significant difference between groups (p = 0.020) and significant increase in positive and active engagement of life (p = 0.048), skill and technique acquisition (p = 0.006), and social integration and support (p = 0.033). (These are general health behaviors, but can be applied to osteoporosis preventive behaviors, such as those related to calcium intake and weight-bearing exercise.) |
| Hien et al., 2009 [16] | Experimental Study, 18 months | 2 separate community health centers; Thanh Mien rural district of Hai Duong, Vietnam | Treatment group that received the intervention (n = 57). Article included description and demographic information for total participants in the study, but did not include separate description and demographic information for the treatment and control group, though there were no significant differences between groups. For all participants, all postmenopausal women 55–65 years of age, mean age = 57.6 years old (S.D. ± 3.0) | Participants attended training courses and were taught about osteoporosis, and explored seasonal and local calcium-rich foods and were taught how to prepare meals with them based on guided menus while being guided with visual aids such as posters, leaflets, booklets and videos. A loudspeaker daily repeated lession summaries and educational messages such as “Take calcium-rich foods everyday to enhance your bone health.” and “Take guided menu into your meals to reach enough calcium intake.” Participants also tracked calcium-rich foods on recording sheets. And participants attended weekly group discussions with other participants, collaborators, and nutrition experts to share calcium-rich meals brought from home and share experiences in preparing calcium-rich meals in order to assess knowledge and receive feedback from nutrition experts | At Posttest – (1) Calcium Intake: Significant increase in calcium intake (p < 0.01) for the treatment group, but no significant difference in the control group |
| Kronhed, Blomber, Lofman, Timpka, & Moller, 2006 [17] | Quasi-Experimental Study, 3-year and 5-year follow-ups | 2 different communities; Intervention community in Vadstena, a semi-rural town in Ostergotland, Sweden | Intervention community: 3-year follow-up (n = 352), 5-year follow-up (n = 219). All participants at least 65 years of age. Both men and women in the community, but unspecified percentage of each | Vadstena Osteoporosis and fall Prevention Project (VOPP). Participants in intervention community received health education to increase osteoporosis and fall awareness and risk factors, and to promote public physical activity. Posters about osteoporosis were displayed throughout the community. Public seminars, local press and cable television repeatedly discussed osteoporosis and fall consequences. Public was informed on fall prevention and where to purchase fall prevention aids, along with available balance training | At 5-Year Follow-Up – (1) Weight-Bearing Exercise: No significant difference |
| Rohr, Clements, & Sarkar, 2006 [18] | Prospective Cohort Study, Follow-up time unspecified | Screenings at local senior centers, living facilities, and health fairs. Follow-up telephone surveys | 219 older women at follow-up, ages 59–86 years of age with mean age = 74.9 year old. At screening, 77 (35.2%) had normal bone mineral density (BMD), 142 (64.8%) had low BMD (osteoporosis or osteopenia) | Large community-based osteoporosis screening program. Participants were assessed for risk, screening was conducted using dual-energy X-ray absorptiometry (DXA), and referred to follow-up care. Patients also received lifestyle counseling, calcium intake recommendations, and recommendations for follow-up with primary care physicians for osteoporosis prevention and treatment practices | At Follow-Up – (1) Calcium Intake: Significant increase in calcium supplement use in both groups, for the group of women with normal BMD (p = 0.002) and the group of women with low BMD (p = 0.001) |
| Hamel et al., 2005 [19] | Prospective Cohort Study, 3-month follow-up | 2 non-academic BMD testing sites; 1 in eastern Canada in Guelph, Ontario, and 1 in western Canada in Edmonton, Alberta. Follow-up mail | 1057 participants at 3-month follow-up. Article included description and demographic information for total participants at beginning of the study, but did not include separate description and demographic information for only those at follow-up. For all participants at beginning of the study (n = 1323), all were women over 20 years of age with a mean age = 57.8 years old (S.D. ± 11.6), 29% had history of at least 1 fracture after 20 years of age, 24% had normal BMD, 27% had osteopenia, 46% had osteoporosis | BMD testing | At Follow-Up – (1) Calcium Intake: Significant increase in calcium intake (p < 0.001) with greatest increase in participants with BMD results showing osteoporosis, followed by participants with BMD results showing osteopenia, but both were not significantly greater than the increase in participants with normal BMD. (2) Weight-Bearing Exercise: No significant difference |
| Pearson, Burkhart, Pifalo, Palaggo-Toy, & Krohn, 2005 [20] | Intervention Study (Non-Experimental), 8 weeks with 6-month and 2-year follow-ups | Community-based setting; unspecified location | 375 participants (367 women and 8 men), ages 44–90 years of age with a mean age = 67 years old (81% over 60 years of age), and 98% White | Highmark Osteoporosis Prevention and Education (HOPE) program. 2.5-h sessions twice per week for 8 weeks. Each session consisted of supervised exercise with resistance bands and 30–40 min of aerobic exercises, and participants were instructed on strength-training exercises and aerobic weight-bearing exercises to complete on their own time to meet recommendations established by the American College of Sports Medicine (ACSM). Participants were advised on calcium and vitamin D intake recommendations established by the National Institutes of Health/National Osteoporosis Foundation. Participants individually met with program pharmacist to discuss pharmacological interventions based on risk factors for fractures and were advised to discuss this with their primary physician. And conducted in-home safety assessments, proper lifting and bending techniques, and proper body mechanics for fall prevention | At Both 6-Month and 2-Year Follow-Ups – (1) Calcium Intake: Significant increase in calcium intake and vitamin D intake (p < 0.001). (2) Weight-Bearing Exercise: Significant increase in strength-training and aerobic weight-bearing exercise (p < 0.001) |
| Tussing & Chapman-Novakofski, 2005 [21] | Intervention Study (Non-Experimental), 8 weeks | Simulated community class setting; unspecified location | 42 participants, all women, were 32–67 years of age with a mean age = 48 years old. 80% White and 21% had family history of bone fracture | Osteoporosis prevention education program based on 2 theoretical behavioral change theories: HBM and TRA. Each week consisted of lessons of topics that included short lectures with hands-on activities to increase self-efficacy and distribution of handouts to reinforce learned behaviors. Lessons 1–8: (Topic in quotations with example activities): (1) “Severity of osteoporosis” with bone fragility demonstration; (2) “Susceptibility to osteoporosis” with anthropometric measures and risk factor quiz; (3) “Overcoming barriers to reducing risk factors: calcium intake” with portion size identification of calcium-rich foods; (4) “Achieving benefits from reducing risk factors: changing calcium intake” with food label calculations; (5) “Overcoming barriers to reducing risk factors: improving exercise habits, alcohol intake, smoking, protein, caffeine” with balance exercise demonstrations and posture practice; (6) “Medications, hormone replacement therapy, bone density tests” with portion practice of calcium-rich foods; (7) “Facts and fallacies: supplements, lactose intolerance, vitamin D” with lactose-free milk and soy milk tasting and supplement label reading practice; (8) “You can do it-be a better bone graduate” with high-calcium recipe sharing, luncheon of calcium-rich foods, and recipe contest | At Posttest – (1) Calcium Intake: Significant increase in calcium intake (p < 0.0001) |
| Cerulli & Zeolla, 2003 [22] | Intervention Study (Non-Experimental), 3-months | 6 community pharmacies; unspecified location | 107 participants completed posttest, all women at least 18 years of age. Article included description and demographic information for total participants at beginning of the study, but did not include separate description and demographic information for only those at follow-up. For all participants at beginning of the study (n = 140), mean age = 61.3 years old (S.D. ± 13.4); 64 (46%) had low osteoporosis risk, 59 (42%) had medium osteoporosis risk, 17 (12%) had high osteoporosis risk; 16 (11%) were diagnosed with osteoporosis and 47 (34%) were on osteoporosis therapy, and 67 (48%) self-reported calcium supplement use | Community pharmacy-based BMD screening and education program lasting either 1 or 2 days. BMD testing was conducted with a portable ultrasound BMD device that took approximately 3 min. BMD results were printed and pharmacist or final-year doctor of pharmacy student reviewed results with participants to inform their level of osteoporosis risk but reminded that the test did not constitute osteoporosis diagnosis and encouraged reviewing results with their physicians. Education was provided verbally about lifestyle modification on diet, exercise, fall prevention, smoking cessation, and calcium recommendations, with use of supplemented printed education materials from the National Osteoporosis Foundation and the American College of Obstetricians and Gynecologists | At Posttest – (1) Calcium Intake: Increase in calcium and vitamin D intake (p-value unreported). (2) Weight-Bearing Exercise: Increase in exercise habits (p-value unreported) |
| Brecher et al., 2002 [23] | Experimental Study, 3 months | Unspecified setting; unspecified location | Treatment group that received the intervention (n = 51). For all participants, all community-dwelling women ages 25–75 years of age with a mean age = 55 years old (S.D. ± 13.7), 46 (94%) White and 3 (6%) Asian, 18 (35%) had family history of osteoporosis but 0 (0%) were diagnosed with osteoporosis | A 3-h multidisciplinary, interactive primary osteoporosis prevention program. Program consisted of: (1) “Medical Issues” with a presentation on osteoporosis risk factors and consequences, osteoporosis prevention and treatment; (2) “Dietary Recommendations” with an experiential presentation on calcium and vitamin D for osteoporosis prevention and treatment, calcium sources and portion sizes, lactose-free calcium options, and factors that hinder calcium absorption, including food models with tasting opportunities and recipe sharing; (3) “Exercise” with an interactive presentation on exercises for spinal flexibility and posture, resistance training and weight-bearing aerobic exercise, proper exercise technique and injury risk reduction, and most beneficial weight-bearing exercises for osteoporosis prevention, while also using available exercise equipment at the on-site fitness center | At Posttest – (1) Calcium Intake: No significant difference in calcium intake. (2) Weight-Bearing Exercise: No significant difference in exercise activity |
| Ribeiro & Blakeley, 2001 [24] | Semi-Experimental, 6 months | Workshop; Canada | Treatment group that received the intervention (n = 59). All women, most (81%) were ages 45–69 years of age, 63% reached menopause, 6% were diagnosed with osteoporosis | Workshop developed by a Canadian community health agency designed to educate women about osteoporosis and encourage them to prevent or treat it. Presented information in lecture format, with question-and-answer and discussion sessions, and practice of weight-bearing exercises | At Posttest – (1) Calcium Intake: No significant difference in calcium intake or calcium and vitamin D supplementation. (2) Weight-Bearing Exercise: No significant difference in weight-bearing exercise |
The effectiveness of community-based public health programs for osteoporosis prevention is determined by the success of increasing osteoporosis preventive behaviors, particularly the behaviors of calcium intake and weight-bearing exercise. All studies, with the exception of 1 study [15], measured the osteoporosis preventive behaviors of calcium intake and/or weight-bearing exercise, with 8 studies measuring both osteoporosis preventive behaviors [11], [12], [14], [19], [20], [22], [23], [24], 4 studies only measuring calcium intake [13], [16], [18], [21], and 1 study only measuring weight-bearing exercise [17]. One of the 8 studies that measured both calcium intake and weight-bearing exercise also measured fall preventive home safety behaviors [14]. The 1 study that did not measure either calcium intake or weight-bearing exercise instead measured health-directed behaviors, such as positive and active engagement of life, skill and technique acquisition, and social integration and support [15], and although these are general health behaviors, they can be applied to specific osteoporosis preventive behaviors, such as calcium intake and weight-bearing exercise.
In terms of their effectiveness to successfully increase osteoporosis preventive behaviors, 9 of the 12 studies (75%) reported significant increases in calcium intake [11], [12], [13], [14], [16], [18], [19], [20], [21], and only 3 of the 9 studies (33%) reported significant increases in weight-bearing exercise [11], [14], [20] (1 study reported increases in both calcium intake and weight-bearing exercise, but did not report statistical significance [22]). Significant increases were also reported in the 1 study that measured fall preventive home safety behaviors [14], as well as the 1 study that only measured health-directed behaviors [15].
The community-based public health programs for osteoporosis prevention varied in numerous ways, but notable trends in those with significant increases in osteoporosis preventive behaviors, particularly in calcium intake, were the inclusion of at least one theoretical behavior change model or BMD testing for osteoporosis screening. Four of the 14 studies were based on at least one theoretical behavior change model, as all 4 of those studies implemented the health belief model (HBM) [13], [14] and 2 of them implemented both the HBM and the theory of reasoned action (TRA) [12], [21], and all 4 of those studies (100%) measured and significantly increased calcium intake, but only 2 of those 4 studies also measured weight-bearing exercise with only 1 of the 2 studies (50%) resulting in a significant increase [14]. Three of the 14 studies implemented BMD testing for osteoporosis screening, and all 3 of those studies (100%) measured and increased calcium intake [18], [19], [22] (2 significantly increased [18], [19], 1 did not report statistical significance [22]), but only 2 of those 3 studies also measured weight-bearing exercise with only 1 of those 2 studies (50%) resulting in an increase (but did not report statistical significance [22]). Although all of the studies that implemented at least one theoretical behavior change model or implemented BMD testing for osteoporosis screening were 100% successful in significantly increasing calcium intake, no study implemented the use of at least one theoretical behavior change model combined with the use of BMD testing for osteoporosis screening.
2.2. Evidence-based recommendations for community-based public health programs for osteoporosis prevention
Community-based public health programs for osteoporosis prevention can vary in designs in implementation, but are effective depending on the osteoporosis preventive behavior. Three-fourths of community-based public health programs for osteoporosis prevention were successful in significantly increasing calcium intake, and all of the programs that implemented either: 1) a theoretical change model, or 2) BMD testing for osteoporosis screening, were successful in significantly increasing calcium intake, and their use is recommended for increased effectiveness in public health policy. However, only one-third of programs were successful in significantly increasing weight-bearing exercise, and further review of the literature was needed to examine how to successfully increase weight-bearing exercise for osteoporosis prevention with community-based public health programs.
In regards to weight-bearing exercise, as community-based public health programs for osteoporosis prevention are usually unsuccessful in encouraging and motivating people to increase weight-bearing exercise on their own, community-based public health programs incorporating osteoporosis exercise can be implemented in which individuals partake in weight-bearing exercise as the focus of attendance to increase this particular osteoporosis preventive behavior. Community-based public health programs incorporating osteoporosis exercise will increase weight-bearing exercise in participants just from attendance and participation, but that weight-bearing exercise must be effective in improving bone health outcomes to actually prevent osteoporosis, such as increasing BMD. As community-based public health programs incorporating osteoporosis exercise are ideal for engagement in weight-bearing exercise to protect bone health in populations, their effectiveness on increasing BMD must be reviewed to determine their applications for policy in public health practice.
3. Osteoporosis exercise in community-based public health programs
3.1. Community-based public health programs incorporating osteoporosis exercise effectiveness on increasing bone mineral density
To assess the effectiveness of community-based public health programs incorporating osteoporosis exercise, a review of the literature was conducted with a search in the same four databases: PubMed, PsycINFO, ERIC, and Google Scholar. Search terms entered into these databases were “osteoporosis community,” and after a thorough review of all search results, 5 studies were found in the recent literature to be community-based public health programs incorporating osteoporosis exercise that included BMD analysis to assess effectiveness of a community-based osteoporosis exercise intervention. Table 2 provides specifics of the different aspects of these 5 studies on community-based public health programs incorporating osteoporosis exercise designed to increase BMD [25], [26], [27], [28], [29]. Watson et al. [25] conducted an 8-month experimental study on program called “LIFTMOR (Lifting Intervention For Training Muscle and Osteoporosis Rehabilitation)” in Australia, Duckham et al. [26] conducted a 6-month experimental study on a program called “ProAct65+” in the United Kingdom, Bello et al. [27] conducted a 32-week experimental study on a program specifically for postmenopausal women with pre-diabetes or type 2 diabetes in Brazil, Gianoudis et al. [28] conducted a 12-month experimental study on a program called “Osteo-cise: Strong Bones for Life” in Australia, and McNamara and Gunter [29] conducted a 12-month experimental study on a program called “Better Bones and Balance” in the United States. All 5 studies included numerous measurements of BMD with dual x-ray absorptiometry (DXA).
Table 2.
Community-based public health programs incorporating osteoporosis exercise on bone mineral density.
| Study reference (n = 5) | Study design and duration; and setting and location | Depictions and description of participants | Details and description of community-based public health program incorporating osteoporosis exercise | Outcome for bone health: bone mineral density (BMD) |
|---|---|---|---|---|
| Watson et al. (2015) [25] | Experimental Study Trial Period, 8 months. Community; Queensland, Australia | Treatment Group that received intervention and analyzed (n = 28). All postmenopausal women, mean age = 65.3 years old (S.D. ± 3.9); 13 participants had osteoporosis and 15 had osteopenia | Exercise Program (“LIFTMOR (Lifting Intervention For Training Muscle and Osteoporosis Rehabilitation)”): Community-based program: High-intensity progressive resistance training (HiPRT) 30-min sessions, 2 sessions per week. Bodyweight and low-load exercise for the initial 2–4 weeks to learn correct lifting technique. Three HiPRT are introduced and progressed: (1) deadlift, (2) squat, and (3) overhead press, in addition to jumping chin-ups and drop landings. Two sets of 5 repetitions of deadlifts at 50–70% 1RM are performed as a warm-up, and for the 3 HiPRT exercises, each of the 3 exercises are performed at 5 sets of 5 repetitions progressively increasing to 80–85% 1RM. Impact loading is applied to the jumping chin-ups and drop landings | At Final Analysis (87.2% completed program) – (1) BMD (via dual x-ray absorptiometry [DXA]): significant increases at femoral neck (p = 0.016) and lumbar spine (p = 0.005) in the treatment group, no significant difference in the control group. (2) Other-Back extensor strength: significant increase (p = 0.007) in the treatment group, no significant difference in the control group |
| Duckham et al., 2015 [26] | Experimental Study, 6 months/24 weeks. Home and Community; Nottinghamshire and Derbyshire, United Kingdom | Treatment groups that received an intervention and analyzed at follow-up: Otago Exercise Program (OEP) (n = 75), Fall Management Exercise (FaME) (n = 94). Article included description and demographic information for all groups before losing participants at follow-up. Before follow-up: OEP – 68.2% women, 98.9% White, mean age = 71.4 years old (S.D. ± 4.9), 5.7% on osteoporosis medication; FaME – 60.0% women, 97.1% White, mean age = 71.8 years old (S.D. ± 5.5), 10.5% on osteoporosis medication | Exercise Programs (ProAct65 + trial): Home-based (OEP) and Community-Based (FaME). OEP: (3) 30-min home exercise sessions with at least (2) 30-min walking sessions. Home exercise included progressive leg strengthening and balance exercises with instruction booklet and ankle cuff weights. FaME: Same as the OEP, including (1) 60-miniute exercise class. Exercise class included progressive leg, arm and trunk muscle strengthening using ankle cuff weights and Therabands, flexibility training, functional floor skills, and adapted Tai Chi | At Follow-Up (OEP: 87.5% completed program, FaME: 92.4% completed program) – (1) BMD (DXA): significant decrease at the distal radius for FaME (p = 0.042) although likely not due to intervention but other medical condition or medications, but no significant difference in the OEP, and no significant differences in both groups at the femoral neck, trochanter, total hip, upper neck, lumbar spine, and total body, as well as in section modulus and in femoral strength |
| Bello et al., 2014 [27] | Experimental Study, 32 weeks. Community; Joao Pessoa City in Paraiba, Brazil | Treatment Group that received intervention and analyzed at follow-up (n = 7). Article included description and demographic information for total participants in the study, but did not include separate description and demographic information for the treatment and control group. All were postmenopausal women diagnosed with either pre-diabetes or Type 2 diabetes in the last 6 months, were non-smoker, non-regular exercisers; no history of stroke, myocardial infarction or other serious disease that prevents exercise safety, and mean age = 61.3 years old (S.D. ± 6.0) | Exercise Program: Multicomponent training including moderate-to-vigorous intensity exercise (rating of perceived exertion (RPE) of 12–15 on the 6–20 Borg scale). 2 sessions per week. Monday: aerobic exercise – 40 min of walking. Wednesday: weight-bearing exercise – circuit with dumbbells and ankle weights (both 2–3 kg), including 6 main muscle group exercises (3 sets, 15–20 repetitions); and 1 aquatic session of static stretching (4 exercises, 3 sets, 10 s) and muscular endurance exercises with water dumbbells on major muscle groups (4 exercises, 3 sets, 15–20 repetitions) | At Follow-Up (70% completed program and adhered to an average of 85% of sessions) – (1) BMD (via DXA): significant increase at Ward's triangle (p = 0.043), but no significant difference in BMD for the femoral neck, greater trochanter, total hip and whole body |
| Gianoudis et al., 2014 [28] and Gianoudis et al., 2012 [31] | Experimental Study, 12 months. Local health and fitness centers; Melbourne, Australia | Treatment Group that received intervention and analyzed at final analysis (n = 76). Article included description and demographic information for both groups before losing participants at follow-up. Before follow-up: 74.1% women, mean age = 67.7 years old (S.D. ± 6.5) | Exercise Program (“Osteo-cise: Strong Bones for Life”): Community-based and multifaceted program: (1) “Osteo-cise” – an osteoporosis and falls prevention exercise program with diverse-loading, moderate impact, weight-bearing exercises (60–180 impacts/session) and high-challenge balance/functional exercises 3 days/week that progressed from 2 sets of 12–15 repetitions at 40–60% 1RM (RPE 3–4 on 1–10 Borg scale) to 2 sets of 8–12 repetitions at 60% 1RM progressivley increasing to 70–80% 1RM (RPE 5–8 on 1–10 Borg scale), used machine and free weights for exercises targeting the hip and spine; included weight-bearing impact exercises such as (a) stationary movements (e.g., stomping, mini tuck jumps), (b) forward/backward movement (e.g., box step-ups, backward/forward pogo jumps), and (c) lateral/multidirectional movements (e.g., side-to-side shuffle, lateral box jumps) and 2 of these 3 were completed each session in 3 sets of 10–20 repetitions which progressed by increasing height of jumps and/or adding weight; also included high-challenge balance and functional exercises such as (a) fit ball exercises (e.g., fit ball sitting with heel lifts), (b) standing balance exercises (e.g., single-leg stands), and (c) dynamic functional exercises (e.g., heel-toe walking) and 2 of these 3 were completed each session with each exercise performed up to 30 s or at a given number of repetitions which progressed to more difficult exercises; (2) “Osteo-Adopt” – behavior change strategies to adopt and maintain lifelong exercise; (3) “Osteo-Ed” – community-based osteoporosis education/awareness seminars to improve osteoporosis knowledge, such as risk factors and exercise/nutrition for bone health; (4) “Osteo-Instruct” – instruction for exercise trainers who provide training for participants | At Final Analysis (93.8% completed program) – (1) BMD (via DXA): Significant increases in lumbar spine (p < 0.05) and femoral neck (p < 0.05) compared to control group, but no significant difference in total hip between groups. (2) Other-Fall Risk: Significant increase in leg strength (p < 0.01), back strength (p < 0.001), functional muscle power (p < 0.05), 30-s sit-to-stand (p < 0.001), four square step test (p < 0.05) and timed stair climb (p < 0.05) compared to the control group, but no significant difference timed up and go test. (3) Other-Fracture Incidence: 1 fracture (wrist) in treatment group due to training accident, 0 in the control group |
| McNamara & Gunter, 2012 [29] | Experimental Study, 12 months/1 year. Community; Linn County and Benton County, Oregon | Treatment Group that received intervention and analyzed (n = 69). All postmenopausal women, mean age = 70.1 years old (S.D. ± 7.8), with average years of menopause = 18.9 (S.D. ± 8.8) | Exercise Program (“Better Bones and Balance [BBB]”): Community-based exercise program for older adults to reduce hip fractures by enhancing bone health and reducing fall risk with (3) 50-min sessions per week of lower body resistance training with weighted vests, and impact and balance exercises. Includes several main weight-bearing exercises: stepping on to and off of benches, forward and side lunges, squats, heel drops, jumps, and stomps. At least 30 repetitions of each weight-bearing exercise are performed during each session | At Final Analysis (100% completed program, 91.3% of participants attended at least 10 out of 12 sessions/month, 95.7% attended sessions year round) – (1) BMD (via DXA): No significant differences in hip, spine, or bone structural outcomes between groups. |
Three of the 5 studies were unsuccessful in significantly increasing BMD at all sites they respectively measured, which were the “ProAct65+” program [26], the program investigated by Bello et al. [27], and the “Better Bones and Balance” program [29]. All 3 of these programs implemented various weight-bearing exercises. Each week, the “ProAct65+” program [26] included two (2) 30-min walking sessions and incorporating low-to moderate-intensity resistance training with ankle cuff weights and resistance bands for the legs, arms, and trunk. Each week, the program investigated by Bello et al. [27] included one (1) 40-min walking session and one (1) session of low-to moderate-intensity resistance training with dumbbells and ankle weights at 2–3 kg for 3 sets of 15–20 repetitions for main muscle groups. And each week, the “Better Bones and Balance” program [29] included three (3) 50-min sessions of lower body resistance training with weighted vests for at least 30 repetitions for different exercises, such as stepping onto and off of benches, forward and side lunges, squats, heel drops, jumps, and stomps. While these 3 studies [26], [27], [29] did incorporate weight-bearing exercise, it should be noted that percentages of 1-repetition maximum (1RM) were not calculated nor used in these 3 studies to determine intensity levels, but the given details and descriptions of exercises and amounts of repetitions show that the weight-bearing exercises for those programs were not high-intensity but only low-to moderate intensity.
Of the 5 studies, the “Osteo-cise: Strong Bones for Life” program [28] was one of only 2 studies found that showed that a community-based public health program incorporating osteoporosis exercise can significantly increase BMD. Each week, the “Osteo-cise: Strong Bones for Life” program included three (3) sessions that incorporated numerous weight-bearing exercises, including use of machines or free weights for exercises targeting the hip and spine that progressed from 2 sets of 12–15 repetitions at 40–60% 1RM up to 2 sets of 8–12 repetitions with increased levels of intensity, along with weight-bearing impact exercises that were either (a) stationary movements, (b) forward/backward movements, and/or (c) lateral/multidirectional movements, with 2 of those 3 exercises in 3 sets of 10–20 repetitions. The current position stand of the American College of Sports Medicine on “Physical Activity and Bone Health” states that weight-bearing exercise for bone health should have an intensity no more than 60% 1RM for children and adolescents for safety reasons [30], but no recommended percentage of 1RM is stated for adults, and the “Osteo-cise: Strong Bones for Life” program did incorporate 1RM higher than 60%. Unlike the 3 studies previously discussed [26], [27], [29], the study on the “Osteo-cise: Strong Bones for Life” program did include the use of high-intensity weight-bearing exercises, with resistance training incorporating sets of high-intensity with lower repetitions of 8–12 of 60% 1RM in an “adoption phase” of the program, and study protocol stating that intensity increased up to 70–80% calculated 1RM [31]. Also unlike the other studies, this program did significantly increase BMD for certain sites measured, and although there was not a significant difference for the total hip, there were significant increases at the spine (p < 0.05) and femoral neck (p < 0.05) between groups. And although fall risk is not a bone health outcome, as reducing fall risk can lead to decreased incidence of fractures, this program was the only one to include analyses of measures for fall risk. The “Osteo-cise: Strong Bones for Life” program did not significantly change all measures to reduce fall risk (i.e., times up and go test), but it did significantly increase leg strength (p < 0.01), back strength (p < 0.001), functional muscle power (p < 0.05), 30-second sit-to-stand (p < 0.001), four square step test (p < 0.05), and timed stair climb (p < 0.05), all of which can reduce the risk of falling that can lead to bone fractures. Furthermore, 93.8% of participants completed this program, and the high-intensity weight-bearing exercise did not substantially compromise safety as only 1 person out of 76 participants who were analyzed in the treatment group reported an injury with a wrist fracture due to a training accident [28].
In addition to the “Osteo-cise: Strong Bones for Life” program [28], the “LIFTMOR” program that implemented high-intensity progressive resistance training (HiPRT) [25] was the other community-based public health program incorporating osteoporosis exercise that significantly increased BMD. The “LIFTMOR” program consisted of a bodyweight and low-load acclimation period for the first 2–4 weeks in order to learn proper and correct lifting technique, and after this period, three (3) HiPRT exercises were introduced and progressed: 1) deadlift, 2) squat, and 3) overhead press, in addition to jumping chin-ups and drop landings. As a warm-up, 2 sets of 5 repetitions of deadlifts at 50–70% 1RM are performed, followed by the 3 HiPRT exercises, with each of the 3 exercises performed at 5 sets of 5 repetitions progressively increasing to 80–85% 1RM, and progressive impact loading is applied to the jumping chin-ups and drop landings. The “LIFTMOR” program did significantly increase BMD at femoral neck (p < 0.05) and lumbar spine (p < 0.01) while also significantly increasing back extensor strength (p < 0.01). Furthermore, “LIFTMOR” also found that HiPRT of up to 80–85% 1RM with impact loading to also be safe and effective in increasing BMD, even in postmenopausal women with low to very low bone mass, as there were no reported injuries with an 87.2% compliance [25].
3.2. Evidence-based recommendations for community-based public health programs incorporating osteoporosis exercise
Community-based public health programs incorporating osteoporosis exercise are effective in increasing weight-bearing exercise, but their effectiveness to increase BMD to prevent osteoporosis depends on the level of intensity of weight-bearing exercise. Each program that incorporated only low-to moderate-intensity weight-bearing exercises was ineffective in significantly increasing BMD; however, both programs that incorporated high-intensity weight-bearing exercises were effective in significantly increasing BMD. Therefore, it is recommended that community-based public health programs incorporating osteoporosis exercise implement high-intensity weight-bearing exercise, such as resistance training of at least 80–85% 1RM, which can increase BMD and still have high rates of compliance, but do not jeopardize safety.
4. Discussion
Community-based public health programs for osteoporosis prevention have been implemented at various locations and in numerous ways with mixed results in increasing osteoporosis preventive behaviors, but much more success is shown in the effectiveness to significantly increase calcium intake than weight-bearing exercise. Every community-based public health program for osteoporosis prevention that implemented at least one theoretical behavior change model or BMD testing for osteoporosis screening was successful in significantly increasing calcium intake, but success in significantly increasing weight-bearing exercise was still limited. The exclusion of a theoretical behavior change model or BMD testing for osteoporosis screening does not necessarily result in an unsuccessful community-based public health program for osteoporosis prevention, as there were a couple of successful community-based public health programs for osteoporosis prevention that did not include the implementation of either, but the inclusion of either of them can substantially increase the likelihood of success in significantly increasing certain osteoporosis preventive behaviors, particularly calcium intake.
Only a few of the community-based public health programs for osteoporosis prevention were successful in motivating participants to significantly increase weight-bearing exercise. The explanations and reasons for how and why the osteoporosis preventive behavior of weight-bearing exercise is more difficult to increase compared to calcium intake is unclear. Calcium intake and weight-bearing exercise are vastly different behaviors, the factors and variables related to adopting and maintaining either one are likely numerous and very different, and the explanations and reasons could vary between each community and/or each individual. Until community-based public health programs for osteoporosis prevention are effective in motivating increased weight-bearing exercise, community-based public health programs incorporating osteoporosis exercise can be used to increase weight-bearing exercise with attendance and participation. In particular, community-based public health programs that incorporate high-intensity weight-bearing exercises, up to 80–85% 1RM, can significantly increase BMD, which will prevent osteoporosis.
Community-based public health programs for osteoporosis prevention that implement either at least one theoretical behavior change model or BMD testing for osteoporosis screening can significantly increase calcium intake, although there was not a program that implemented both at least one theoretical behavior change model and BMD testing for osteoporosis screening in combination with each other. For increasing calcium intake, it is unknown if combining these two successful elements would lead to a stronger effect or have no additional effect than implementation of just one or the other, although additional research examining these two elements in combination compared to independently may be valuable in determining differences in effect size and possible influence on other osteoporosis preventive behaviors, such as weight-bearing exercise. It is also unknown how other theoretical behavior change models besides the HBM or TRA could effectively significantly increase calcium intake and/or weight-bearing exercise or not, and additional research can also examine the effectiveness of other theoretical behavior change models alone and in combinations on increasing these osteoporosis preventive behaviors. Use of various theoretical behavior change models, and in combination with BMD testing for osteoporosis screening, warrant further research on increasing calcium intake and weight-bearing exercise. In addition, other studies have findings that also warrant additional research for community-based public health programs for osteoporosis prevention, such as different community settings that were not often used in the studies in this review, including worksites/workplaces [32] and faith-based locations [33], both which have shown promise in successful implementation in osteoporosis prevention programs and are worth consideration for future programs.
As “Osteo-cise: Strong Bones for Life” [28] and “LIFTMOR” [25] showed potential and promise to significantly increase BMD with community-based public health programs incorporating osteoporosis exercise, more research is warranted and needed to determine what specific and minimal weight-bearing exercise types, frequencies, intensities, and volumes are necessary to consistently increase BMD. For all of the community-based osteoporosis exercise programs, weight-bearing exercise was the only treatment studied to enhance BMD without studying the effects of various calcium intakes. High-intensity weight-bearing exercise can significantly increase BMD to prevent osteoporosis and reduce the risk of bone fractures, and dietary supplementation of calcium with vitamin D has also been shown to decrease bone fracture risk [34]. A community-based public health program effectively increased calcium and vitamin D intake in a community setting via administration of daily supplements that decreased bone fracture incidence in the population [35]; therefore, future studies should examine the effectiveness of community-based public health programs incorporating different combinations and amounts of high-intensity weight-bearing exercise and calcium with vitamin D supplementation to determine if and how much additional increases in BMD can be attained than from high-intensity weight-bearing exercise alone.
Research and practice in bone health promotion and osteoporosis prevention in public health should also focus more on entire populations, which can include more attention on men who account for 20–25% of osteoporosis cases [36]. Less than half of the studies in this review included men as participants, and most of them comprised of men at a much smaller percentage than 20–25% of the total participants, which is the portion of osteoporosis cases affecting men. Osteoporosis in men is a major, yet still largely neglected, public health issue [37], especially since the perceived susceptibility to the disease is low in both older men [38] and particularly younger men [39], and more studies on community-based public health programs for osteoporosis prevention should include men and at higher percentages of the total sample of participants that were used, such as 20–25% of participants, which corresponds with the proportion of osteoporosis cases that they make. In addition, individuals with intellectual disabilities and/or developmental disabilities that are confined in communities that are institution-dwelling are also at high risk of osteoporosis [40], and community-based public health programs for osteoporosis prevention should be considered for this community of individuals and community setting as well.
5. Conclusions
Public health leaders should implement community-based public health programs for osteoporosis prevention and incorporate osteoporosis exercise based on effective evidence-based studies, while encouraging more research that is needed to further investigate and advance the effectiveness of different programs in different communities. Public health practitioners should examine how effective programs have different elements and characteristics that can be utilized, but may need to be modified for each and every individual community it is implemented in. For instance, each and every community is unique, and the application of a community-based public health program could be different depending on each individual community's characteristics and qualities. For example, different community characteristics that could require modification of community-based public health program implementation can include, but are not limited to, population size and demographics, place size and location, geography, weather and climate, wealth and affluence, urban versus rural areas, economics, culture, government, public health infrastructure, food sources and supplies, availability and access to health services and health professionals, along with numerous other variables, and all of the many community characteristics must work together within themselves in order to have a successful community-based public health program unique to its own community needs and resources. As more research is conducted and the body of knowledge grows, all individual communities can modify and customize programs for their own unique community, while implementing common and universal elements of success, such as use of theoretical behavior change models or BMD testing for osteoporosis screening along with high-intensity weight-bearing exercise, in order to implement their own successful community-based public health programs which will prevent osteoporosis that affects many populations in countless communities around the world.
Conflict of interest
The author declares that there is no conflict of interest regarding the publication of this paper.
Footnotes
Peer review under responsibility of The Korean Society of Osteoporosis.
References
- 1.Kanis J.A., Melton L.J., Christiansen C., Johnston C.C., Khaltaev N. Perspective: the diagnosis of osteoporosis. J Bone Mineral Res. 1994;9:1137–1141. doi: 10.1002/jbmr.5650090802. [DOI] [PubMed] [Google Scholar]
- 2.Lips P., van Schoor N.M. Quality of life in patients with osteoporosis. Osteoporos Int. 2005;16:447–455. doi: 10.1007/s00198-004-1762-7. [DOI] [PubMed] [Google Scholar]
- 3.Johnell O., Kanis J.A., Oden A., Sernbo I., Redlund-Johnell I., Petterson C. Mortality after osteoporosis fractures. Osteoporos Int. 2004;15:38–42. doi: 10.1007/s00198-003-1490-4. [DOI] [PubMed] [Google Scholar]
- 4.Leboime A., Confavreux C.B., Mehsen N., Paccou A., David C., Roux C. Osteoporosis and mortality. Jt Bone Spine. 2010;77:S107–S112. doi: 10.1016/S1297-319X(10)70004-X. [DOI] [PubMed] [Google Scholar]
- 5.Benjamin R.M. Bone health: preventing osteoporosis. Public Health Rep. 2010;125:368–370. doi: 10.1177/003335491012500302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright N.C., Looker A.C., Saag K.G., Curtis J.R., Delzell E.S., Randall S. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Mineral Res. 2014;29:2520–2526. doi: 10.1002/jbmr.2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooper C., Campion G., Melton L.J. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 8.NIH Consensus development Panel on osteoporosis prevention, diagnosis, and therapy. Osteoporosis prevention, diagnosis, and therapy. J Am Med Assoc. 2001;285:785–795. [Google Scholar]
- 9.Morales-Torres J. Strategies for the prevention and control of osteoporosis in developing countries. Clin Rheumatol. 2007;26:139–143. doi: 10.1007/s10067-006-0314-2. [DOI] [PubMed] [Google Scholar]
- 10.McLeroy K.R., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 11.Oh E.G., Yoo J.Y., Lee J.E., Hyun S.S., Ko I.S., Chu S.H. Effects of a three-month therapeutic lifestyle modification program to improve bone health in postmenopausal Korean women in a rural community: a randomized controlled trial. Res Nurs Health. 2014;37:292–301. doi: 10.1002/nur.21608. [DOI] [PubMed] [Google Scholar]
- 12.Plawecki K., Chapman-Novakofski K. Effectiveness of community intervention in improving bone health behaviors in older adults. J Nutr Gerontol Geriatrics. 2013;32:145–160. doi: 10.1080/21551197.2013.781421. [DOI] [PubMed] [Google Scholar]
- 13.Babatunde O.T., Himburg S.P., Newman F.L., Campa A., Dixon Z. Theory-driven intervention improves calcium intake, osteoporosis knowledge, and self-efficacy in community-dwelling older black adults. J Nutr Educ Behav. 2011;43:434–440. doi: 10.1016/j.jneb.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 14.Teems J., Hausman D.B., Fischer J.G., Lee J.S., Johnson M.A. Older adults attending Georgia senior centers increase preventive behaviors for falls and fractures following a community-based intervention. J Nutr Gerontol Geriatrics. 2011;30:72–85. doi: 10.1080/01639366.2011.545042. [DOI] [PubMed] [Google Scholar]
- 15.Francis K.L., Matthews B.L., Van Mechelen W., Bennell K.L., Osborne R.H. Effectiveness of a community-based osteoporosis education and self-management course: a wait list controlled trial. Osteoporos Int. 2009;20:1563–1570. doi: 10.1007/s00198-009-0834-0. [DOI] [PubMed] [Google Scholar]
- 16.Hien V.T., Khan N.C., Mai le B., Lam N.T., Phuong T.M., Nhung B.T. Effect of community-based nutrition education intervention on calcium intake and bone mass in postmenopausal Vietnamese women. Public Health Nutr. 2009;12:674–679. doi: 10.1017/S1368980008002632. [DOI] [PubMed] [Google Scholar]
- 17.Kronhed A.-C.G., Blomber C., Lofman O., Timpka T., Moller M. Evaluation of an osteoporosis and fall risk intervention program for community-dwelling elderly. A quasi-experimental study of behavioral modifications. Aging Clin Exp Res. 2006;18:235–241. doi: 10.1007/BF03324654. [DOI] [PubMed] [Google Scholar]
- 18.Rohr C.I., Clements J.M., Sarkar A. Treatment and prevention practices in postmenopausal women after bone mineral density screening at a community-based osteoporosis project. J Am Osteopath Assoc. 2006;106:396–401. [PubMed] [Google Scholar]
- 19.Hamel M.E., Sebaldt R.J., Siminoski K., Adachi J.D., Papadimitropoulos E., Petrie A. Influence of fracture history and bone mineral testing on the treatment of osteoporosis in two non-academic community centers. Osteoporos Int. 2005;16:208–215. doi: 10.1007/s00198-004-1776-1. [DOI] [PubMed] [Google Scholar]
- 20.Pearson J.A., Burkhart E., Pifalo W.B., Palaggo-Toy T., Krohn K. A lifestyle modification intervention for the treatment of osteoporosis. Am J Health Promot. 2005;20:28–33. doi: 10.4278/0890-1171-20.1.28. [DOI] [PubMed] [Google Scholar]
- 21.Tussing L., Chapman-Novakofski K. Osteoporosis prevention education: behavior theories and calcium intake. J Am Dietetic Assoc. 2005;105:92–97. doi: 10.1016/j.jada.2004.10.025. [DOI] [PubMed] [Google Scholar]
- 22.Cerulli J., Zeolla M.M. Impact and feasibility of a community pharmacy bone mineral density screening and education program. J Am Pharm Assoc. 2003;44:161–167. doi: 10.1331/154434504773062618. [DOI] [PubMed] [Google Scholar]
- 23.Brecher L.S., Pomerantz S.C., Snyder B.A., Janora D.M., Klotzbach-Shimomura K.M., Cavalieri T.A. Osteoporosis prevention project: a model multidisciplinary educational intervention. J Am Osteopath Assoc. 2002;102:327–335. [PubMed] [Google Scholar]
- 24.Ribeiro V., Blakeley J.A. Evaluation of an osteoporosis workshop for women. Public Health Nurs. 2001;18:186–193. [PubMed] [Google Scholar]
- 25.Watson S.L., Weeks B.K., Weis L.J., Horan S.A., Beck B.R. Heavy resistance training is safe and improves bone, function, and stature in postmenopausal women with low to very low bone mass: novel early findings from the LIFTMOR trial. Osteoporos Int. 2015;26:2889–2894. doi: 10.1007/s00198-015-3263-2. [DOI] [PubMed] [Google Scholar]
- 26.Duckham R.L., Masud T., Taylor R., Kendrick D., Carpenter H., Iliffe S. Randomised controlled trial of the effectiveness of community group and home-based falls prevention exercise programmes on bone health in older people: the ProAct65+ bone study. Age Ageing. 2015;44:573–579. doi: 10.1093/ageing/afv055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bello M., Sousa M.C., Neto G., Oliveira L., Guerras I., Mendes R. The effect of a long-term, community-based exercise program on bone mineral density in postmenopausal women with pre-diabetes and type 2 diabetes. J Human Kinet. 2014;43:43–48. doi: 10.2478/hukin-2014-0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gianoudis J., Bailey C.A., Ebeling P.R., Nowson C.A., Sanders K.M., Hill K. Effects of a targeted multimodal exercise program incorporating high-speed power training on falls and fracture risk factors in older adults: a community-based randomized controlled trial. J Bone Mineral Res. 2014;29:182–191. doi: 10.1002/jbmr.2014. [DOI] [PubMed] [Google Scholar]
- 29.McNamara A., Gunter K. The influence of participation in Better Bone and Balance on skeletal health: evaluation of a community-based exercise program to reduce fall and fracture risk. Osteoporos Int. 2012;23:1813–1822. doi: 10.1007/s00198-011-1816-6. [DOI] [PubMed] [Google Scholar]
- 30.Kohrt W.M., Bloomfield S.A., Little K.D., Nelson M.E., Yingling V.R. Physical activity and bone health. Med Sci Sports Exerc. 2004;36:1985–1996. doi: 10.1249/01.mss.0000142662.21767.58. [DOI] [PubMed] [Google Scholar]
- 31.Gianoudis J., Bailey C.A., Sanders K.M., Nowson C.A., Hill K., Ebeling P.R. Osteo-cite: strong bones for life: protocol for a community-based randomized controlled trial of a multi-modal exercise and osteoporosis education program for older adults at risk of falls and fractures. BMC Musculoskelet Disord. 2012;13:78. doi: 10.1186/1471-2474-13-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tan A.M., Lamontagne A.D., Sarmugam R., Howard P. A cluster-randomised, controlled trial to assess the impact of a workplace osteoporosis prevention intervention on the dietary and physical activity behaviours of working women: a study protocol. BMC Public Health. 2013;13:405. doi: 10.1186/1471-2458-13-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Forster-Burke D., Ritter L., Zimmer S. Collaboration of a model osteoporosis prevention and management program in a faith community. J Obstetric Gynecol Neonatal Nurs. 2010;39:212–219. doi: 10.1111/j.1552-6909.2010.01111.x. [DOI] [PubMed] [Google Scholar]
- 34.Weaver C.M., Alexander D.D., Boushey C.J., Dawson-Hughes B., Lappe J.M., LeBoff M.S. Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation. Osteoporos Int. 2016;27:367–376. doi: 10.1007/s00198-015-3386-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Larsen E.R., Modekilde L., Foldspang A. Vitamin D and calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents: a pragmatic population-based 3-year intervention study. J Bone Mineral Res. 2004;19:370–378. doi: 10.1359/JBMR.0301240. [DOI] [PubMed] [Google Scholar]
- 36.Szulc P., Garnero P., Marchand F., Delmas P.D. Cross-sectional evaluation of bone metabolism in men. J Bone Mineral Res. 2001;16:1642–1650. doi: 10.1359/jbmr.2001.16.9.1642. [DOI] [PubMed] [Google Scholar]
- 37.Szulc P., Kaufman J.M., Orwoll E.S. Osteoporosis in men. J Osteoporos. 2012;2012:675984. doi: 10.1155/2012/675984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sedlak C.A., Doheny M.O., Estok P.J. Osteoporosis in older men: knowledge and health beliefs. Orthop Nurs. 2000;19:38–46. doi: 10.1097/00006416-200019030-00006. [DOI] [PubMed] [Google Scholar]
- 39.Johnson C.S., McLeod W., Kennedy L., McLeod K. Osteoporosis health beliefs among younger and older men and women. Health Educ Behav. 2008;35:721–733. doi: 10.1177/1090198107301331. [DOI] [PubMed] [Google Scholar]
- 40.Lin L.-P., Hsu S.-W., Yao C.-H., Lai W.-J., Hsu P.-J., Wu J.-L. Risk of osteopenia and osteoporosis in institution-dwelling individuals with intellectual and/or developmental disabsilities. Res Dev Disabil. 2015;36:108–113. doi: 10.1016/j.ridd.2014.09.022. [DOI] [PubMed] [Google Scholar]