Abstract
Severe osteoporosis is classified as those with a bone mineral density (BMD) T-score of −2.5 or lower, and demonstrate one or more of osteoporotic, low-trauma, fragility fractures. According to the general principle of surgical approach, patients with severe osteoporosis require not only more thorough pre- and postoperative treatment plans, but improvements in surgical fixtures and techniques such as the concept of a locking plate to prevent bone deformity and maximizing the blood flow to the fracture site by using a minimally invasive plate osteosynthesis. Arthroplasty is often performed in cases of displaced femoral neck fracture. Otherwise internal fixation for the goal of bone union is the generally accepted option for intertrochanteric, subtrochanteric, and femoral shaft fractures. Most of osteoporotic spine fracture is stable compression fracture, but vertebroplasty or kyphoplasty may be performed some selective patients. If neurological paralysis, severe spinal instability, or kyphotic deformity occurs, open decompression or fusion surgery may be considered. In order to overcome shortcomings of the World Health Organization definition of osteoporosis, we proposed a concept of ‘advanced severe osteoporosis,’ which is defined by the presence of proximal femur fragility fracture or two or more fragility fractures in addition to BMD T-score of −2.5 or less. In conclusion, we need more meticulous approach for surgical treatment of severe osteoporosis who had fragility fracture. In cases of advanced severe osteoporosis, we recommend more aggressive managements using parathyroid hormone and receptor activator of nuclear factor kappa-B ligand monoclonal antibody.
Keywords: Advanced severe osteoporosis, Fragility fractures, Surgical treatment, Severe osteoporosis
1. Introduction
As per the diagnostic criteria given by the World Health Organization (WHO), as well as most domestic and international guidelines, patients with severe osteoporosis are classified as those with a bone mineral density (BMD) T-score of −2.5 or lower, and demonstrate one or more of osteoporotic, low-trauma, fragility fractures [1], [2]. The T-score guideline of −2.5 was established based on prevalence of osteoporosis and BMD obtained from the spine, femur, and wrist, when the WHO presented the diagnostic criteria for osteoporosis in 1994 [2]. In other words, a T-score of −2.5 in the femoral neck represents a 16% probability of a femur fracture occurring during one's lifetime, as well as a 30% probability of a fracture occurring in either the spine, femur, or wrist [2]. However, the context of classifying osteoporosis using this criterion, severe or established osteoporosis is interpreted as diagnosis based on the general concept of a fragility fracture—a phenomenon that is a common result of pre-existing osteoporosis—in addition to using the −2.5 T-score as a cutoff value. Osteoporosis related fractures can cause significant morbidity and disability, reducing the quality of life, and can even lead to death in severe cases. If hip fracture occurs, 20%–30% of patients die within 1 year [3], [4]. Furthermore, 40% of patients are unable to walk independently, and 60% have difficulty with at least one essential activity of daily living 1 year after hip fracture [4]. The presence of fragility fractures has a clinically significant implication for subsequent fractures. Patients with a vertebral fracture are at about 3–5 fold higher risk for another vertebral fracture within the following year than those without fracture [5], [6]. According to former review article for medical treatment of severe osteoporosis, Choi et al. [7] recommend selective estrogen receptor modulators (SERMs), bisphosphonates, receptor activator of nuclear factor kappa-B ligand (RANKL) monoclonal antibody, and parathyroid hormone (PTH) for the medical treatment of severe osteoporosis, based on the clinical trials and post hoc analyses.
In this topic review, we are going to figure out the general principle and current trend for surgical treatment of severe osteoporosis including postoperative management. We also discuss the limitations of the current WHO definition of severe osteoporosis and proposed a concept of ‘advanced severe osteoporosis’ to provide a more accurate assessment of the disease and allow more proactive managements.
2. Surgical treatment of severe osteoporosis
2.1. General principle
Cases of osteoporosis accompanied by fracture often require surgical treatments, and the challenges facing such surgical treatments include difficulties in achieving firm and stable fixation. In particular, many cases now require more aggressive forms of surgery due to fractures occurring in elderly patients with a clearly diminished ability to regenerate bone and fracture or refracture in patients with weak bone strength due to reduced BMD and bone quality. However, resurgery for osteoporotic fracture is often required due to malunion or nonunion from failed fixation caused by implant loosening or cut outs when attempting fixation using a metal plate and screws on thinned bone cortex and hollow bony trabecula. Therefore, the surgical approach for patients with severe osteoporosis requires not only more thorough pre- and postoperative treatment plans, but improvements in surgical fixtures and techniques as well. Consequently, efforts should be made to achieve successful surgical outcomes through various novel approaches, including, the use of different techniques, such as treatments using the concept of a locking plate to prevent bone deformity due to screw loosening and maximizing the blood flow to the fracture site by using a minimally invasive plate osteosynthesis (MIPO) [8] (Fig. 1).
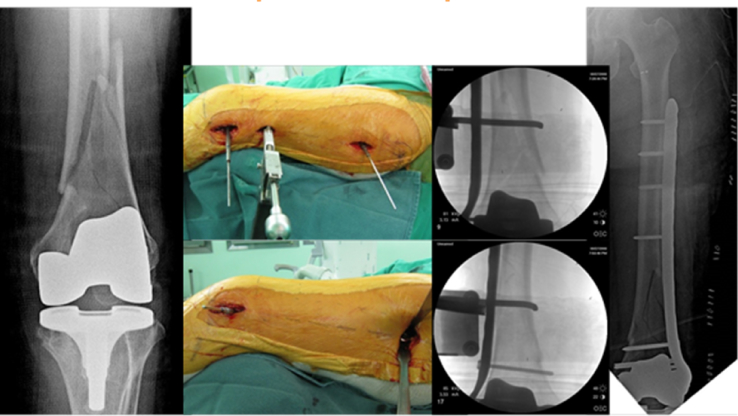
Fig. 1.
The concept of minimally invasive plate osteosynthesis (MIPO). MIPO technique applied periprosthetic fracture at distal femur with minimal incision and biologic fixation.
The major fracture sites of osteoporosis are spine, hip, proximal humerus, and distal radius. When describing the surgical principle, the fracture of the vertebrae and the around joint are completely different. The general principle of joint around fracture is very similar compared to vertebral fracture. In this review, the vertebral and hip fractures are described as the most common and serious osteoporotic fracture.
2.2. Hip fracture
Osteoporotic hip fractures among the elderly often involve existing medical diseases, and these cases also face a high risk of medical complications during the surgical treatment process. Therefore, in cases where surgical treatment is unavoidable, thorough pre- and postoperative precautions against medical issues are required. The general principle and goal of surgical treatment is to allow the patient to recover as much independent function as possible by achieving firm internal fixation in the early stages, or to perform arthroplasty according to the fracture pattern, whereby early movement and gait could be enabled along with rehabilitation therapy. Through such processes, postoperative medical complications can be minimized as well. Osteoporotic proximal hip fractures can be classified as femur neck, intertrochanteric, and subtrochanteric fractures based on the anatomical location of the fracture, while distal fractures include the femoral shaft and diaphyseal fracture (Fig. 2A). Arthroplasty is often performed in cases of displaced femoral neck fracture and minimally displaced femoral neck fracture with high risk of internal fixation failure due to severe osteoporosis (Fig. 2B). Although some surgeons may choose arthroplasty as a surgical treatment for intertrochanteric fractures, internal fixation for the goal of bone union is the generally accepted option for intertrochanteric, subtrochanteric, and femoral shaft fractures. The biggest problem associated with internal fixation on osteoporotic hip fracture is that firm internal fixation is difficult to achieve due to reduced bone quality and strength, which also increases the risk of fracture reduction loss, nonunion, and the failure and fracture of the internal fixture (even after internal fixation). Accordingly, there have been various recent attempts to stabilize internal fixation and improve fracture healing through advances in internal fixtures, development of surgical techniques, and methods that facilitate additional fracture healing. The biggest change involves a transition from the concept of fixation with absolute stability achieved by traditional anatomical reduction through soft tissue detachment and compression of bone fragments to a new concept of biologic fixation with relative stability achieved by indirect reduction of the fracture while minimizing bone and soft tissue damage during internal fixation. For intertrochanteric, subtrochanteric, and femoral shaft fractures, which are proximal hip fractures, the method often performed is an internal fixation that uses intramedullary nail that can minimize soft tissue damage while offering the greater biomechanical advantage than metal plates [9], [10], [11]. If necessary, this procedure can be performed together with autologous bone grafting or augmentation using bone cement or other bone substitutes. When selecting a metal plate for internal fixation of either a subtrochanteric or femoral shaft fracture accompanied by osteoporosis, the metal plate with locking screws would be recommended. Furthermore, MIPO that can minimize soft tissue detachment should be used to increase bone union rate by using long plate for sufficient working length, while also reducing the frequency of adverse events, such as re-fracture and infection [9], [10], [11].
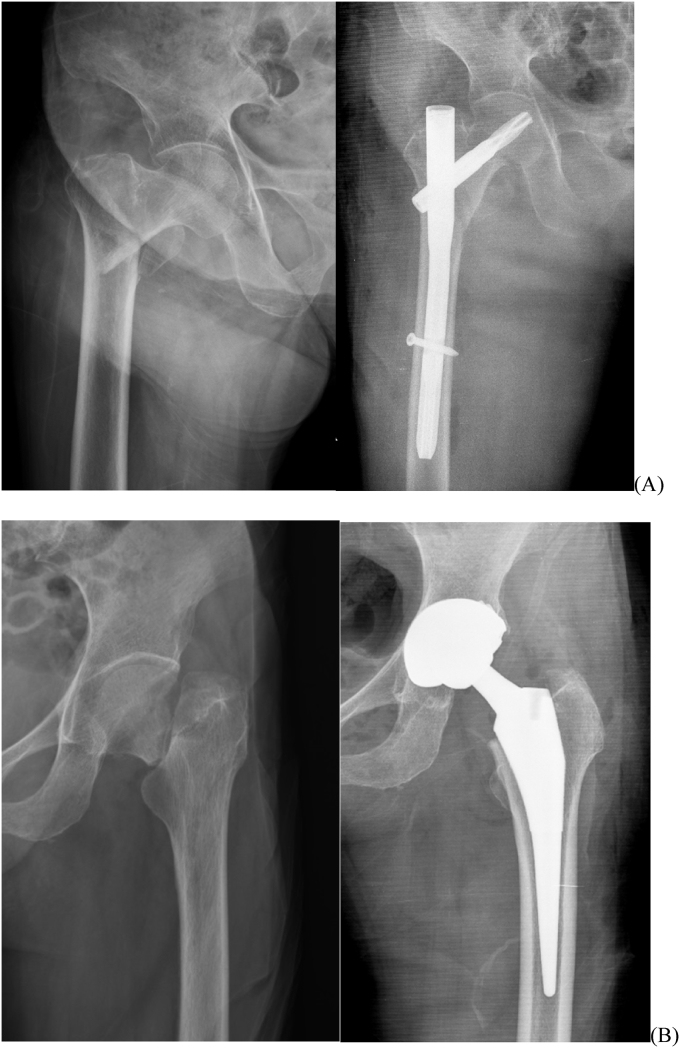
Fig. 2.
(A) Intertrochanteric fracture with intramedullary nail. (B) Femur neck fracture with bipolar arthroplasty.
2.3. Spine fracture
Most of osteoporotic spine fracture is stable compression fracture that can be treated conservatively. Treatment goals for osteoporotic spine fracture can be achieved as early ambulation and prevention of refracture through aggressive pain control and stabilization of the fractured vertebral body. In general, initial treatment involves short-term bed rest, aggressive administration of analgesics, use of assistive devices such as brace, physical therapy and exercise program [12], [13]. If severe pain or a high vertebral compression rate progresses for 2–3 weeks despite such initial conservative treatment, vertebroplasty or kyphoplasty may be performed some selective patients [14], [15]. If neurological paralysis, severe spinal instability, or kyphotic deformity occurs, open decompression or fusion surgery may be considered [14]. Vertebroplasty involves using a bone marrow biopsy needle on the symptomatic vertebral body, under local anesthesia, to inject bone cement through the vertebral pedicle for the purpose of stabilizing the vertebral body and eliminating pain [16]. Kyphoplasty uses a balloon that inflates inside the vertebral body to inject the cement, which offers the advantages of preventing cement leakage and correcting kyphotic deformity in some cases [17]. Although its necessity is currently being disputed, these percutaneous vertebral augmentations are being used in selective cases because it represents a minimally invasive approach for treating osteoporotic vertebral fracture with severe pain, while also offering the advantages of pain relief and early ambulation (Fig. 3) [16], [18], [19]. Open surgery is performed in cases with neurological deficit or severe deformity. Although it has the advantages of enabling recovery of neurological paralysis and the correction of deformity from osteoporotic spinal fracture, decisions should be made carefully since the possibility of complications such as metal loosening, nonunion due to poor vertebral bone quality, and the prevalence of underlying medical diseases in patients. Therefore, thorough preoperative preparation and appropriate surgical techniques are required, while diligent postoperative treatment is also needed to ensure favorable outcomes (Fig. 4) [20], [21].
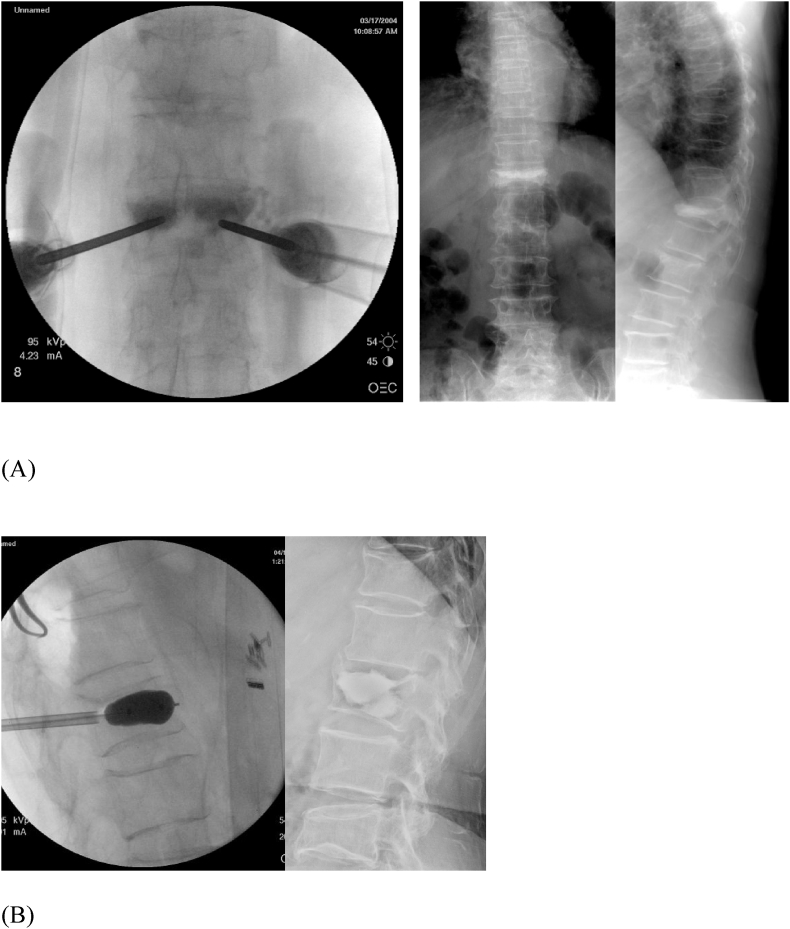
Fig. 3.
Percutaneous vertebroplasty (A) and kyphoplasty (B).
Fig. 4.
Open reconstructive surgery for osteoporotic kyphotic deformity. (A) Preoperative x-ray showed multiple osteoporotic fracture with kyphotic deformity. (B) Postoperative x-ray showed deformity correction with pedicle subtraction osteotomy and long level fusion with meticulous pedicle screw insertion.
Concerning about spinal instrumentation for fracture and deformity, pedicle screw fixation was key role for stability and correction. In the osteoporotic spine, pedicle screw fixation is highly correlated with the BMD [22]. In order to enhance the fixation stability at osteoporotic spine surgery, surgeons need a systematic approach with meticulous preoperative planning, careful intraoperative procedure and detail postoperative management. A couple of principle to reduce stress on bone implant interface are extensive release for the deformity, avoiding forceful reduction, adding anterior structural graft, good sagittal balance and avoiding to increase strain at spinal transition zone. Meticulous insertion technique such as preservation of dorsal cortex at hole, untapping of hole, anterior cortex penetration and proper screw trajectory are important [23], [24], [25]. The pedicle screw design and augmentation can also affect the fixation stability. The screw with larger diameter and expandable shape has some advantage for pullout strength [26]. The most common method for vertebral body augmentation is adding with bone cement [27], [28]. The other techniques for augmentation are multiple point fixations with bone graft, additional laminar hook or sublaminar wire and additional polyethylene tape [29]. Postoperative management with brace and medication can enhance the bone union [30].
3. Postoperative treatment of severe osteoporosis
Elderly patients with osteoporotic hip fractures are known to possess about a 9% probability of a second hip fracture on the contralateral side, with a high probability of such fractures occurring within the first 3 years [31], [32]. Another serious problem is the fact that the mortality rate of these patients increases up to 30% within 1 year. Therefore, in cases involving patients who suffered osteoporotic fractures for the first time, aggressive treatment for osteoporosis must be combined with surgical treatment to prevent additional osteoporotic fractures [33], [34], [35], [36], [37]. When an osteoporotic fracture occurs in a patient who was already taking bisphosphonate, drug compliance to bisphosphonate must be assessed. If compliance is poor, the cause of low compliance must be analyzed so that a different mode of bisphosphonate may be administered or patients can be educated to increase their compliance. If there are no problems with compliance to bisphosphonate, drug action may be insufficient, for which, a switch to denosumab may be considered. Considering that bisphosphonates are excreted by the kidneys, it is a general rule not to use them for estimated glomerular filtration rate <30–35 mL/min. Denosumabs may be prescribed since they do not have specific effects on kidney functions, but caution should be taken since they can exacerbate hypocalcemia. Another point to consider when dealing with patients who suffered an atypical femoral fracture (AFF) is that such fractures may occur bilaterally on both sides in approximately 30%–40% patients, and thus, the contralateral side must be checked for suspected lesions. Moreover, if there is pain and cortical hypertrophy, together with a distinct dreadful black line on the lateral cortex on a radiograph, hot spots on bone scan, or fracture line on magnetic resonance imaging, then preventative internal fixation using intramedullary nail must be performed before a complete fracture occurs [38]. With respect to selecting the right drug for osteoporosis, bisphosphonate, denosumab, SERM, and PTH may be used if the spinal BMD serves as an indication for osteoporosis treatment. In cases with BMD in the hip being the indication for osteoporosis treatment, bisphosphonate (excluding ibandronate) and denosumab may be used. In cases involving patients who were taking bisphosphonate without having a continued risk of osteoporotic fracture as mentioned above (oral administration for 5 years or more or annual IV administration for 3 years or more), a drug holiday is recommended for those taking bisphosphonate, where if spinal BMD corresponds to osteoporosis, switching to denosumab, SERM, or PTH may be considered [34], [35], [36]. For patients in the high-risk group for osteoporotic fracture, continued management is needed to prevent osteoporotic fracture, but more research is needed in regard to the appropriate medication use.
4. Advanced severe osteoporosis
As shown, the incidence of severe osteoporosis has steadily increased in the aging society, while its pattern has become more diverse. There have been recent changes in new clinical environments due to demographic and epidemiological changes in osteoporosis based on increased average lifespan in the past 20 years. This means that an emergence of new forms of fractures in superaged patients, such as AFF, recurrent, multiple, and periprosthetic fractures that are recognized as a phenomenon associated with osteoporosis. The increases in the spectrum of more serious osteoporotic diseases acts as a risk factor for new fractures, and thus, it is difficult to broadly apply the general concept of severe osteoporosis [39]. Moreover, new approaches are also needed since the elderly population, aged 65 years and older, include both individuals who are in relatively good health with few accompanying diseases, as well as those with various chronic comorbidities [40]. Particularly in cases of hip fractures, accompanying diseases have a direct impact on fragility fractures and patient impairment. Being diagnosed with three or more accompanying diseases also has an impact on mortality rate. Thus, they represent a key preoperative risk factor [41]. With such issues being raised, some have claimed that severe osteoporosis should be defined as having two or more fragility fractures regardless of BMD value, in addition to the existing criteria of a T-score of −2.5 or below with one or more of osteoporotic, low-traumatic, fragility fractures [42]. Because of such problems with the diagnostic criteria for osteoporosis, increases in the number of patients with severe osteoporosis, and significant differences in age, BMD, and frequency of fracture among patients with severe osteoporosis due to rapidly aging society, new treatment strategies and approaches have become necessary. This has also led to the need for new guidelines that include changes in treatment modalities and reestablishment of the concept of severe osteoporosis. Therefore, the concept of severe osteoporosis should be subcategorized, so that more severe forms of severe osteoporosis may be classified as advanced severe osteoporosis. Accordingly, it is suggested that advanced severe osteoporosis be defined as “the presence of proximal femur fragility fracture or two or more fragility fractures in addition to BMD T-score of - 2.5 or less.” This new definition is based on consideration of expert opinions and the number of fractures and fracture areas reported by some studies, in addition to the existing definition of severe osteoporosis based on age, BMD value, and fracture status. It is also proposed that regarding the number of fractures, two or more fractures would be required for fractures in areas other than the spine and femur, whereas a femoral fracture may be included within the range of advanced severe osteoporosis even if it occurred as a single fracture.
In addition to general (lifestyle therapy) and drug treatment guidelines, treatment of such severe and advanced severe osteoporosis would require additional treatment guidelines, including, recommendations for early postoperative ambulation after fracture fixation (surgery) is needed depending on the indication and area where the fracture has occurred. Furthermore, patients need additional strategies for preventing refractures and more liberal drug therapy. With respect to prevention of refractures, once a fracture occurs, the risk of another fracture occurring is extremely high, regardless of BMD. Moreover, since recurrent fractures have poor treatment outcomes and increase the mortality rate, treatment of osteoporosis in response to this and prevention of falls becomes important. Thus, aggressive treatment is needed to prevent additional fractures by simultaneously increasing BMD (bone mass) and improving microstructure (bone quality) after the treatment for the initial fracture. Review of treatment guidelines from countries outside of Korea shows the most guidelines for severe osteoporosis are based on the recommended usage of drug for treatment rather than recommending treatment based on the severity of the disease or the patients' characteristics. The reason why such insufficient guideline has been attributed to the lack of a more specialized concept. However, because changes in treatment guidelines are still needed despite such lacking, recommendations are being made mostly based on therapeutic drugs.
5. Summary
Accordingly, overview of surgical treatment of severe osteoporosis including new concept of advanced severe osteoporosis may be presented as follows:
-
(1)
If a fracture occurs, depending on the area and indication, early postoperative ambulation after fracture fixation (surgery) should be recommended to prevent death or medical complications (pulmonary embolism, pneumonia, urinary tract infections, decubitus ulcer, etc.).
-
(2)
As drug therapy guidelines, for those with no history of taking osteoporosis medications, bisphosphonate, SERM, RANKL monoclonal antibody, and the PTH are recommended according to the general rules for drug therapy.
-
(3)
The definition of severe osteoporosis given by the WHO as having a BMD T-score of −2.5 or lower and having one or more osteoporotic fracture. However, the aging society has observed an increased number of patients with more serious fractures, such as multiple fractures. As a subcategorizing severe osteoporosis, advanced severe osteoporosis, which is being newly adopted, will be limited to cases of patients with the presence of proximal femur fragility fracture or two or more fragility fractures in addition to BMD T-score of −2.5 or less. For advanced severe osteoporosis or an insufficient response to existing drug therapy, anabolic agent (PTH) or a more effective bone resorption inhibitor (RANKL monoclonal antibody or bisphosphonate) is recommended.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Footnotes
Peer review under responsibility of The Korean Society of Osteoporosis.
References
- 1.Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993;94:646–650. doi: 10.1016/0002-9343(93)90218-e. [DOI] [PubMed] [Google Scholar]
- 2.Kanis J.A., Melton L.J., 3rd, Christiansen C., Johnston C.C., Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9:1137–1141. doi: 10.1002/jbmr.5650090802. [DOI] [PubMed] [Google Scholar]
- 3.Keene G.S., Parker M.J., Pryor G.A. Mortality and morbidity after hip fractures. BMJ. 1993;307:1248–1250. doi: 10.1136/bmj.307.6914.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med. 1997;103(2A):12S–17S. doi: 10.1016/s0002-9343(97)90022-x. [DOI] [PubMed] [Google Scholar]
- 5.Lindsay R., Silverman S.L., Cooper C., Hanley D.A., Barton I., Broy S.B. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285:320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 6.Klotzbuecher C.M., Ross P.D., Landsman P.B., Abbott T.A., 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 7.Choi H.S., Park S.Y., Kim Y.M., Kim S.H., Kim K.M., Chung Y.S. Medical treatment of severe osteoporosis including new concept of advanced severe osteoporosis. Osteoporos Sarcopenia. 2016;2:13–19. doi: 10.1016/j.afos.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Capone A., Orgiano F., Pianu F., Planta M. Orthopaedic surgeons' strategies in pharmacological treatment of fragility fractures. Clin Cases Miner Bone Metab. 2014;11:105–109. [PMC free article] [PubMed] [Google Scholar]
- 9.Marmor M., Alt V., Latta L., Lane J., Rebolledo B., Egol K.A. Osteoporotic fracture care: are we closer to gold standards? J Orthop Trauma. 2015;29(Suppl 12):S53–S56. doi: 10.1097/BOT.0000000000000469. [DOI] [PubMed] [Google Scholar]
- 10.Wolf J.M., Cannada L.K., Lane J.M., Sawyer A.J., Ladd A.L. A comprehensive overview of osteoporotic fracture treatment. Instr Course Lect. 2015;64:25–36. [PubMed] [Google Scholar]
- 11.Konstantinidis L., Helwig P., Hirschmüller A., Langenmair E., Südkamp N.P., Augat P. When is the stability of a fracture fixation limited by osteoporotic bone? Injury. 2016;47(Suppl 2):S27–S32. doi: 10.1016/S0020-1383(16)47005-1. [DOI] [PubMed] [Google Scholar]
- 12.Kim W.J. Surgical treatment of osteoporotic compression fracture. J Korean Fract Soc. 2009;22:314–318. [Google Scholar]
- 13.Ralston S.H. Osteoporosis. In: Court-Brown C., Heckman J.D., McKee M., McQueen M.M., Ricci W., Tornetta P. III, editors. Rockwood and Green's fractures in adults. eighth ed. Lippincott Williams & Wilkins; Philadelphia (PA): 2014. pp. 609–620. [Google Scholar]
- 14.Lehman R.A., Jr., Kang D.G., Wagner S.C. Management of osteoporosis in spine surgery. J Am Acad Orthop Surg. 2015;23:253–263. doi: 10.5435/JAAOS-D-14-00042. [DOI] [PubMed] [Google Scholar]
- 15.Clark W., Bird P., Gonski P., Diamond T.H., Smerdely P., McNeil H.P. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016;388:1408–1416. doi: 10.1016/S0140-6736(16)31341-1. [DOI] [PubMed] [Google Scholar]
- 16.Kim J.H., Yoo S.H., Kim J.H. Long-term follow-up of percutaneous vertebroplasty in osteoporotic compression fracture: minimum of 5 years follow-up. Asian Spine J. 2012;6:6–14. doi: 10.4184/asj.2012.6.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hulme P.A., Krebs J., Ferguson S.J., Berlemann U. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31:1983–2001. doi: 10.1097/01.brs.0000229254.89952.6b. [DOI] [PubMed] [Google Scholar]
- 18.Kallmes D.F., Comstock B.A., Heagerty P.J., Turner J.A., Wilson D.J., Diamond T.H. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569–579. doi: 10.1056/NEJMoa0900563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buchbinder R., Osborne R.H., Ebeling P.R., Wark J.D., Mitchell P., Wriedt C. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557–568. doi: 10.1056/NEJMoa0900429. [DOI] [PubMed] [Google Scholar]
- 20.Sudo H., Ito M., Kaneda K., Abumi K., Kotani Y., Nagahama K. Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. Spine J. 2013;13:1726–1732. doi: 10.1016/j.spinee.2013.05.041. [DOI] [PubMed] [Google Scholar]
- 21.Suk S.I., Kim J.H., Lee S.M., Chung E.R., Lee J.H. Anterior-posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine. 2003;28:2170–2175. doi: 10.1097/01.BRS.0000090889.45158.5A. [DOI] [PubMed] [Google Scholar]
- 22.McLain R.F., McKinley T.O., Yerby S.A., Smith T.S., Sarigul-Klijn N. The effect of bone quality on pedicle screw loading in axial instability. A synthetic model. Spine. 1997;22:1454–1460. doi: 10.1097/00007632-199707010-00006. [DOI] [PubMed] [Google Scholar]
- 23.Stauff M.P., Freedman B.A., Kim J.H., Hamasaki T., Yoon S.T., Hutton W.C. The effect of pedicle screw redirection after lateral wall breach: a biomechanical study using human lumbar vertebrae. Spine J. 2014;14:98–103. doi: 10.1016/j.spinee.2013.03.028. [DOI] [PubMed] [Google Scholar]
- 24.Kuklo T.R., Lehman R.A., Jr. Effect of various tapping diameters on insertion of thoracic pedicle screws: a biomechanical analysis. Spine. 2003;28:2066–2071. doi: 10.1097/01.BRS.0000084665.31967.02. [DOI] [PubMed] [Google Scholar]
- 25.Lehman R.A., Jr., Polly D.W., Jr., Kuklo T.R., Cunningham B., Kirk K.L., Belmont P.J., Jr. Straight-forward versus anatomic trajectory technique of thoracic pedicle screw fixation: a biomechanical analysis. Spine. 2003;28:2058–2065. doi: 10.1097/01.BRS.0000087743.57439.4F. [DOI] [PubMed] [Google Scholar]
- 26.Cook S.D., Salkeld S.L., Stanley T., Faciane A., Miller S.D. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004;4:402–408. doi: 10.1016/j.spinee.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 27.Choma T.J., Pfeiffer F.M., Swope R.W., Hirner J.P. Pedicle screw design and cement augmentation in osteoporotic vertebrae: effects of fenestrations and cement viscosity on fixation and extraction. Spine. 2012;37:E1628–E1632. doi: 10.1097/BRS.0b013e3182740e56. [DOI] [PubMed] [Google Scholar]
- 28.Zhu Q., Kingwell S., Li Z., Pan H., Lu W.W., Oxland T.R. Enhancing pedicle screw fixation in the aging spine with a novel bioactive bone cement: an in vitro biomechanical study. Spine. 2012;37:E1030–E1037. doi: 10.1097/BRS.0b013e31825a676e. [DOI] [PubMed] [Google Scholar]
- 29.Hamasaki T., Tanaka N., Kim J., Okada M., Ochi M., Hutton W.C. Pedicle screw augmentation with polyethylene tape: a biomechanical study in the osteoporotic thoracolumbar spine. J Spinal Disord Tech. 2010;23:127–132. doi: 10.1097/BSD.0b013e31819942cd. [DOI] [PubMed] [Google Scholar]
- 30.Ohtori S., Inoue G., Orita S., Yamauchi K., Eguchi Y., Ochiai N. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine. 2013;38:E487–E492. doi: 10.1097/BRS.0b013e31828826dd. [DOI] [PubMed] [Google Scholar]
- 31.Zhu Y., Chen W., Sun T., Zhang Q., Liu S., Zhang Y. Epidemiological characteristics and outcome in elderly patients sustaining non-simultaneous bilateral hip fracture: a systematic review and meta-analysis. Geriatr Gerontol Int. 2015;15:11–18. doi: 10.1111/ggi.12368. [DOI] [PubMed] [Google Scholar]
- 32.Lee K.H., Kim J.Y., Yim S.J., Moon D.H., Choi G.H., Moon K.H. Incidence and risk factors of subsequent hip fractures in Korea: multicenter study. J Kor Med Sci. 2014;29:992–994. doi: 10.3346/jkms.2014.29.7.992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sawalha S., Parker M.J. Characteristics and outcome in patients sustaining a second contralateral fracture of the hip. J Bone Joint Surg Br. 2012;94:102–106. doi: 10.1302/0301-620X.94B1.27983. [DOI] [PubMed] [Google Scholar]
- 34.Levis S., Theodore G. Summary of AHRQ's comparative effectiveness review of treatment to prevent fractures in men and women with low bone density or osteoporosis: update of the 2007 report. J Manag Care Pharm. 2012;18(4 Suppl B):S1–S15. doi: 10.18553/jmcp.2012.18.s4-b.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheung A.M., Papaioannou A., Morin S. Osteoporosis Canada scientific advisory council. Postmenopausal osteoporosis. N Engl J Med. 2016;374:2096. doi: 10.1056/NEJMc1602599. [DOI] [PubMed] [Google Scholar]
- 36.Watts N.B., Bilezikian J.P., Camacho P.M., Greenspan S.L., Harris S.T., Hodgson S.F. American association of clinical endocrinologists medical guidelines for clinical practice for the diagnosis and treatment of postmenopausal osteoporosis. Endocr Pract. 2010;16(Suppl 3):1–37. doi: 10.4158/ep.16.s3.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Silverman S. Individualizing osteoporosis medications. Menopause. 2014;21:306–308. doi: 10.1097/GME.0000000000000180. [DOI] [PubMed] [Google Scholar]
- 38.Adler R.A., El-Hajj Fuleihan G., Bauer D.C., Camacho P.M., Clarke B.L., Clines G.A. Managing osteoporosis in patients on long-term bisphosphonate treatment: report of a task force of the american society for bone and mineral research. J Bone Miner Res. 2016;31:16–35. doi: 10.1002/jbmr.2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iolascon G., Resmini G., Gimigliano F. Severe osteoporosis and its identification. Aging Clin Exp Res. 2011;23(2 Suppl):6–7. [PubMed] [Google Scholar]
- 40.Guthrie B., Makubate B., Hernandez-Santiago V., Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995-2010. BMC Med. 2015;13:74. doi: 10.1186/s12916-015-0322-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roche J.J., Wenn R.T., Sahota O., Moran C.G. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nuti R., Brandi M.L., Isaia G., Tarantino U., Silvestri S., Adami S. New perspectives on the definition and the management of severe osteoporosis: the patient with two or more fragility fractures. J Endocrinol Invest. 2009;32:783–788. doi: 10.1007/BF03346537. [DOI] [PubMed] [Google Scholar]