Abstract
Objectives
The aim of this study was to report the health-related quality of life (HRQoL) over the first year after osteoporotic hip fracture and to identify the factors associated with HRQoL in Police General Hospital in Thailand.
Methods
A prospective cohort study was conducted. 139 subjects who had osteoporotic hip fracture were recruited, which they will be assessed during the preinjury recall and at 3, 6, and 12 months after the fracture. HRQoL was measured as Thailand health state utility values (THSUVs), which derived from EuroQol-5-Dimension-3-Level. Factors associated with the change in QoL were analyzed.
Results
One hundred thirty-six patients with a hip fracture were included for analysis. Their mean age was 82 ± 11 years old. The mean ± standard deviation (SD) of QoL score and EQ VAS at 12-month follow-up period were lower than before the fracture ([0.68 ± 0.105 vs. 0.55 ± 0.183] and [85 ± 10.5 vs. 79 ± 19.2]). The mean ± SD of QoL score and EQ VAS, compared before and after the fracture was estimated at −0.13 ± 0.164 and −6 ± 14.7 (P = 0.01). The positive influences on the change in QoL score were present in the subject, who are younger than 80 years old, had normal or high body mass index (BMI), and had operative treatment.
Conclusions
Osteoporotic hip fractures incurred substantial loss in HRQoL which was markedly impaired at first 3 months after hip fracture and after that HRQoL was improved but did not return to prefracture levels. So primary prevention of fall is more important. The changes in HRQoL, was influenced by age, BMI, and operative treatment.
Keywords: Quality of life, Hip fracture
1. Introduction
Among all types of fragility fracture, hip fracture is one of the main causes of disability in elderly patients [1]. According to a multinational study, the incidence of hip fracture has been on the rise, e.g., a fivefold increase in Singapore between 1960 and 1990 [2] and a 4-fold increase in South Korea between 1991 and 2001 [3]. Twenty-six percent of worldwide hip fractures occurred in Asia in 1990 and is expected to rise to 37% and 45% of worldwide hip fracture by 2025 and 2050, respectively [4]. All types of fragility fractures typically result in a significant posttraumatic pain, and loss of physical and social well-being [5,6], hip fracture is accounted for the most severe disabilities [[7], [8], [9]]. At one year after hip fracture, 20% are deceased, 30% have permanent disability, 40% are unable to walk independently and 80% cannot carry out at least one essential tasks of daily living [10,11].
Although the advancement in orthopedic interventions has led to a great improvement in the outcome of hip fracture [12], the recovery remains slower than expected and the rehabilitation can be a lengthy process [12,13]. Many traits, such as age, sex, preinjury walking ability, fracture type, comorbidity, and cognitive function are accounted as important prognostic factors [13,14]. Some studies in Europe have shown that posthip fracture quality of life (QoL) does not return to prehip fracture levels. In addition, hip fracture patients often experience anxiety and depression, leading to a loss of health-related quality of life (HRQoL), which leads to a higher risk of subsequent fractures [15,16]. The epidemiological investigations of these issues in Thailand have been scarce at present.
In this study, we aim to identify the HRQoL using the European Quality of Life 5 Dimensions Index: EuroQol-5-Dimension-3-Level (EQ-5D-3L) at 3, 6, and 12 months after a hip fracture and to define the factors associated with HRQoL specifically for Thai population.
2. Methods
2.1. Study design
We performed a hospital-based single center prospective study of hip fracture patients at Police General Hospital (Tertiary trauma center, Bangkok, Thailand) between October 2015 and February 2017. Patients were evaluated within 1 day after admission, 3, 6, and 12 months after their admission. The inclusion criterion was all patients at least 50 years of age with a low trauma hip fracture. Exclusion criteria included high-energy trauma, secondary osteoporosis, bone tumors, and severe cognitive dysfunction.
All treatment procedures were selected and performed by a senior surgeon in Police General Hospital with an early hip surgery and fracture liaison service protocol. The choices of treatment were selected based on patient's age, preinjury health status, fracture type, and fracture configuration. The treatment options in this study were conservative treatment, close or open reduction and internal fixation with cephalomedullary nail, -with dynamic hip screws, -with multiple screws and hip arthroplasty.
2.2. Assessment tools
Questionnaires administered during hospitalization included the following traits: age, weight, height, sex, number of underlying diseases, fracture type, previous fragility fracture history, type of treatment, Total 25-hydroxy vitamin D level and prehip fracture QoL. QoL was assessed at 3, 6, and 12 months after the patient was discharged from the hospital.
Several QoL assessment tools are available, but most are difficult and lengthy to assess in clinical practice or are not relevant for Thai elderly patients. Therefore, we chose the EuroQoL questionnaire [[17], [18], [19]], which is easy to complete and short [20] and has been used extensively for evaluating QoL associated with various conditions including hip fracture [21,22].
The EuroQoL, which consists of 2 parts: the health status (EQ-5D-3L) part and the visual analog scale (EQ-VAS) part, was used to assess Quality of life. The EQ-5D-3L has 5 questions with respect to mobility, self-care, daily activities, pain/discomfort, and anxiety/depression. Each item is further divided into 3 degrees of severity: no problem, some problem or, major problem. By applying scores from EQ-5D-3L “Value set” from our Thai population samples, health states defined by the 5-dimensional descriptive system were calculated according to the following formula [23,24].
| Utility value = 1–0.202–(0.121 × mo)–(0.121 × sc)–(0.059 × ua)–(0.072 × pd)–(0.032 × ad)–(0.190 × m2)–(0.065 × p2)–(0.046 × a2)–(0.139 × N3). |
where mo is mobility, sc is self-care, ua is usual activities, pd is pain and discomfort, and ad is anxiety and depression. Variable mo is 1 if mobility is level 2, 2 if mobility is level 3, and 0 otherwise; variable sc is 1 if self-care is level 2, 2 if self-care is level 3, 0 otherwise; ua is 1 if usual activities is level 2, 2 if usual activities is level 3, 0 otherwise; pd is 1 if pain and discomfort is 2, 2 if pain and discomfort is 3, 0 otherwise; ad is 1 if anxiety and depression is 2, 2 if anxiety and depression is 3, 0 otherwise. Variable m2 is 1 if mobility is level 3 and 0 otherwise; p2 is 1 if pain and discomfort is level 3 and 0 otherwise; a2 is 1 if anxiety and depression is level 3 and 0 otherwise; and N3 is 1 if any dimension is level 3 and 0 otherwise.
The Thailand health state utility values (THSUVs) ranges from −0.452 (worst) to +0.798 (best). EQ-VAS is a 20-cm visual analog scale on which a participant is asked to mark their state of health on a thermometer-like line ranging from 0 to 100. To fill out the instrument, an orthopedic resident was trained.
Baseline QoL assessments at the admission time determine the prehip injury status for these measures. Since it is not straightforward to prospectively collect information preinjury, pre-injury recall is often used as an alternative method of QoL assessment studies of these patients [12,25,26].
2.3. Statistical analysis
IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA) was used for all statistical analysis in this study. The following statistics were used for continuous data: maximum, minimum, mean and SD. Categorical data were presented as proportions. Repeated measure analysis of variance (ANOVA) with P = 0.05 was used to analyze factors associated with the change in QoL.
2.4. Ethical considerations
Informed consent was obtained from all patients with normal cognitive function. For those with cognitive dysfunction, a family relative was provided the consent on behalf of the patients. Institutional Review Board approval was obtained from the ethical committee of Police General Hospital. (COA No. 116/2018).
3. Results
We had 162 fragility hip fracture patients admitted in Police General Hospital. We classified 139 as primary osteoporotic patients, 16 as secondary osteoporotic patients and 7 as severe cognitive dysfunction. Three of these patients did not complete the 1-year follow-up. One could not be contacted and 2 were deceased. Thus, the group finally comprised 136 patients (Table 1). The proportion of female patients was 77.41% and the mean age was 82 years. Only 7 patients (5.14%) exhibited no comorbidities. In total, 67.65% of patients had vitamin D inadequacy at admission and 20.59% had low body mass index (BMI). Most of the patients (89.71%) enrolled surgical treatment with some of the patients (10.29%) that had severe comorbidities or other contraindication for surgery enrolled nonoperative treatment.
Table 1.
Characteristics of the study population (total 136 cases).
| Characteristic | No. of patients (%) |
|---|---|
| Sex | |
| Male | 30 (22.59) |
| Female | 106 (77.41) |
| Age, years old | |
| <80 | 65 (47.81) |
| ≥80 | 71 (52.19) |
| No. of underlying diseases | |
| 0 | 7 (5.14) |
| 1 | 65 (47.79) |
| ≥2 | 64 (47.07) |
| Body mass index, kg/m2 | |
| ≤8.49 | 28 (20.59) |
| 18.5–22.99 | 78 (57.35) |
| ≥23 | 30 (22.06) |
| Total 25(OH)D level (at admission) | |
| <30 | 92 (67.65) |
| ≥30 | 44 (32.35) |
| Type of treatment | |
| Conservative | 14 (10.29) |
| Fixation | 66 (48.53) |
| Arthroplasty | 56 (41.18) |
25(OH)D, 25-hydroxy vitamin D.
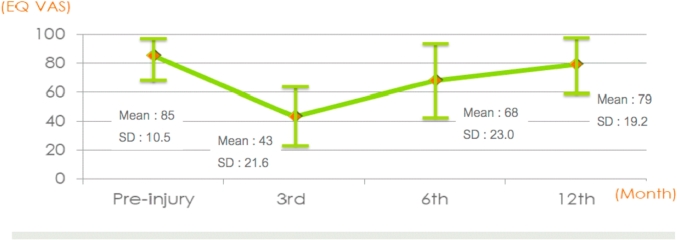
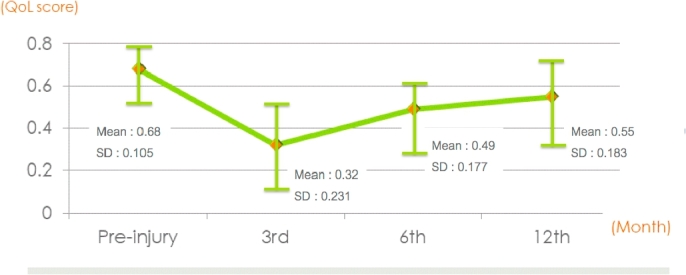
As shown in Fig. 1, Fig. 2, QoL score (THSUV) and EQ VAS decreased between the recalled preinjury period and 3 months of follow-up after the hip injury. Between 3 months and 12 months of follow-up, both indicators were increased but did not return to prehip injury levels. Table 2 showed the change in mean of QoL score and EQ VAS between the preinjury recall period (baseline) and the 1-year follow-up period after the injury. The mean difference was −0.13 ± 0.164 for QoL score and −6 ± 14.7 for EQ-VAS. (P = 0.01).
Fig. 1.
Quality of life (QoL) score (THSUV) in patients at preinjury, and postinjury at 3rd, 6th, 12th month. THSUV, Thailand health state utility value; SD, standard deviation.
Fig. 2.
EuroQoL-visual analogue scale (EQ VAS) in patients at preinjury, and postinjury at 3rd, 6th, 12th month. SD, standard deviation.
Table 2.
Change in mean of QoL score (THSUV) and EQ VAS.
| Variables | Pre-injury | 1 year post-injury | Change from baselinea |
|---|---|---|---|
| QoL score | 0.68± 0.105 | 0.55± 0.183 | −0.13± 0.164 |
| EQ VAS | 85± 10.5 | 79 ± 19.2 | −6± 14.7 |
Values are presented as mean ± standard deviation.
QoL, quality of life; THSUV, Thailand health state utility value; EQ VAS, EuroQoL-visual analogue scale.
Change from baseline was computed as the score at 1-year postinjury minus score at preinjury.
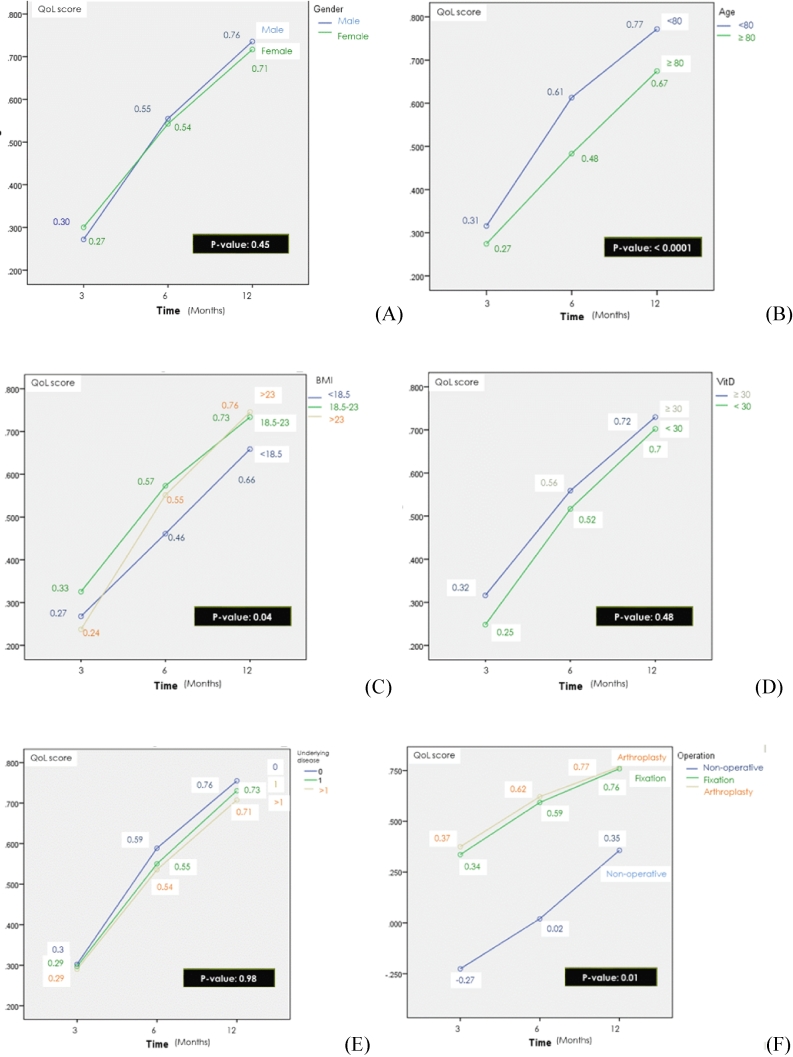
The outcomes of the repeated measure ANOVA model, examining factors associated with the changes in QoL score in the 1-year postinjury, were presented in Fig. 3. Subject's Age, BMI, and choice of treatment were associated with changes in QoL score with statistically significant difference. The younger subject age group (younger than 80 years old) had shown better QoL score than the older patient group (P < 0.0001). The patient with normal and high BMI had a higher QoL score than patients with low BMI (P = 0.04). Patient who had an operative treatment had a better QoL score than those who had a non-operative treatment (P = 0.01).
Fig. 3.
Factors associated with change in quality of life (QoL) score (THSUV): sex (A), age (B), body mass index (BMI) (C), vitamin D (Vit D) level (at admission) (D), number of comorbidities (E), and choice of treatment (F). THSUV, Thailand health state utility value.
4. Discussion
This study describes the changes in HRQoL, following an osteoporotic hip fracture in the subjects aged at least 50 during a 1-year follow-up period in Police General Hospital. The hip fracture patients demonstrated low HRQoL with a significant change in both physical and psychological instability of the patient. According to Adachi, nearly 33% of the patient depended on others to perform their basic daily tasks during the follow-up sessions of patients experiencing a hip fracture [27,28]. Some study showed that HRQoL could vary, depending on the study type, i.e., retrospective or prospective. In addition, progress reports could sometimes be misguided by the patients’ selective memory or from the lack of statistical power [29]. In this study, the mean QoL score and EQ VAS were decreased between the preinjury recalled period and 3 months after the hip injury. After 3-month postinjury, scores for both indicators were increased but did not return to prehip injury levels. Therefore, primary prevention of fall before having a hip fracture is more important than the treatment planning after hip fracture.
Our results revealed that the change in QoL score was improved in those who were in younger age group, normal till high BMI, and received an operative treatment. In comparison, factor such as patient's sex, vitamin D level at admission, and the number of comorbidities showed no influence on the change in QoL score. Therefore, this suggests that after an appropriate choice of treatment, the patient with low BMI (<18.5 kg/m2), who expect to have a good outcome should improve their body weight and nutrition among the follow-up. Even though vitamin D level at admission did not have an influence on the QoL score of the patients, Calcium and vitamin D supplementation could significantly reduce the rate of osteoporotic fracture from future falling in the elderly patients [30]. Hence, it is still combined into the standard treatment regimen.
In older group of patients, the deterioration in HRQoL was largest and statistically significant compared to the younger age group. The similar results were seen in the previous studies [27]. Therefore, age is a major determining factor in HRQoL. The patients group aged ≥80 years, reported some problems in physical mobility during the first 30-day postoperation. Furthermore, these patients were mostly affected by the self-care and daily life tasks. These elderly patients group continued to inform extreme problems in the previously mentioned domain during the sixth postoperative month. This could be best explained by the fact that in this age group, the elderly patient has anxiety, mental pain, depression, and fear of permanent disability [29].
For the elderly patients with hip fracture, an early surgery within 24–48 hours with a promptly initiated postsurgical rehabilitation potentially reduces mortality and morbidity by allowing early mobilization [14]. This is consistent with the low mortality rate in this study due to pre- and postoperative protocol in our hospital. In addition, 23 patients were excluded from the study were those with secondary osteoporosis and severe cognitive dysfunction. These patients had high mortality rate within first year [31], so by excluded these patients would significantly reduce the first year mortality rate in our study.
In terms of operative techniques, Tidermark et al. [32] and Blomfeldt et al. [33] mentioned that the total hip arthroplasty patients improved in their HRQoL during 4–12 months after surgery, while those who had internal fixation surgery, had slightly poorer outcomes in the postoperative pain and patient's mobility. In this study, although the comparison between internal fixation and arthroplasty showed no statistically significant difference which could be due to inadequate sample size. However, the patient who had an operative treatment had a better QoL score than those who had a nonoperative treatment. For this reason, it is recommended to perform an operative management in the patient with osteoporotic hip fracture if not contraindicated. Within our context, the surgical choice in hip fractures will also have to consider on many factors such as the fracture type [34], the patient's age, the treatment protocol in the different institution, and the cost of treatment and hospitalization.
A key contribution of this study was the ability to analyze the individual EQ-5D-3L with the THSUVs that is a cardinal measure of the preference for a specific health outcome for Thai population. To our knowledge, this study was the only one focusing on HRQoL 1-year post-osteoporotic hip fracture in Thai population.
There are 2 limitations in this study. First, the survey was done at a single public hospital and the sample size was small. For future work, we aim to include multiple centers and more patients. Second, a recall bias of baseline QoL score and EQ VAS could not be avoided because preinjury recall information is used as previously described.
5. Conclusions
In this study, we showed a decline in HRQoL after the osteoporotic hip fracture. After 3-month follow-up, HRQoL was increased but still was not comparable to prefracture levels in our cohort study of Thai patients. So the priority should be given to the primary fall prevention. Moreover, an improvement in HRQoL was observed in those who were in younger age group, normal till high BMI, and received an operative treatment. In order to improve HRQoL, it was essential for patients to receive proper nutritional supplementation and early surgery unless they were contraindicated.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Acknowledgments
The authors want to thank Dr. Waiyawut Yoonisil, Ph.D for biostatistics assistance, and Dr. Nitirat Stitkitti and Dr. Chatdanai Phan-udom, M.D. for revising manuscript in a native English language. ORCID. Tanawat Amphansap: https://orcid.org/0000-0003-2148-3921; Puttapoom Sujarekul: https://orcid.org/0000-0003-0604-4832.
Footnotes
Peer review under responsibility of The Korean Society of Osteoporosis.
References
- 1.Gerrard P, Goldstein R, DiVita MA, Slocum C, Ryan CM, Mix J, et al. Functional status and readmissions in unilateral hip fractures. Am J Manag Care 2015;21:e282-e287. [PubMed]
- 2.Koh L.K., Saw S.M., Lee J.J., Leong K.H., Lee J. National working committee on osteoporosis. Hip fracture incidence rates in Singapore 1991-1998. Osteoporos Int. 2001;12:311–318. doi: 10.1007/s001980170121. [DOI] [PubMed] [Google Scholar]
- 3.Rowe S.M., Song E.K., Kim J.S., Lee J.Y., Park Y.B., Bae B.H. Rising incidence of hip fracture in Gwangju City and Chonnam Province, Korea. J Kor Med Sci. 2005;20:655–658. doi: 10.3346/jkms.2005.20.4.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Committee for Osteoporosis Treatment of The Japanese Orthopaedic Association Nationwide survey of hip fractures in Japan. J Orthop Sci. 2004;9:1–5. doi: 10.1007/s00776-003-0741-8. [DOI] [PubMed] [Google Scholar]
- 5.Lips P., van Schoor N.M. Quality of life in patients with osteoporosis. Osteoporos Int. 2005;16:447–455. doi: 10.1007/s00198-004-1762-7. [DOI] [PubMed] [Google Scholar]
- 6.Rabenda V., Manette C., Lemmens R., Mariani A.M., Struvay N., Reginster J.Y. Prevalence and impact of osteoarthritis and osteoporosis on health-related quality of life among active subjects. Aging Clin Exp Res. 2007;19:55–60. doi: 10.1007/BF03325211. [DOI] [PubMed] [Google Scholar]
- 7.Tosteson A.N., Gabriel S.E., Grove M.R., Moncur M.M., Kneeland T.S., Melton L.J., 3rd Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos Int. 2001;12:1042–1049. doi: 10.1007/s001980170015. [DOI] [PubMed] [Google Scholar]
- 8.Taylor B.C., Schreiner P.J., Stone K.L., Fink H.A., Cummings S.R., Nevitt M.C. Long-term prediction of incident hip fracture risk in elderly white women: study of osteoporotic fractures. J Am Geriatr Soc. 2004;52:1479–1486. doi: 10.1111/j.1532-5415.2004.52410.x. [DOI] [PubMed] [Google Scholar]
- 9.Pasco J.A., Sanders K.M., Hoekstra F.M., Henry M.J., Nicholson G.C., Kotowicz M.A. The human cost of fracture. Osteoporos Int. 2005;16:2046–2052. doi: 10.1007/s00198-005-1997-y. [DOI] [PubMed] [Google Scholar]
- 10.Hansson S., Rolfson O., Åkesson K., Nemes S., Leonardsson O., Rogmark C. Complications and patient-reported outcome after hip fracture. A consecutive annual cohort study of 664 patients. Injury. 2015;46:2206–2211. doi: 10.1016/j.injury.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 11.Parsons N., Griffin X.L., Achten J., Costa M.L. Outcome assessment after hip fracture: is EQ-5D the answer? Bone Joint Res. 2014;3:69–75. doi: 10.1302/2046-3758.33.2000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vatansever A., Oziç U., Okcu G. Assessment of quality of life of patients after hemiarthroplasty for proximal femoral fractures. Acta Orthop Traumatol Turc. 2005;39:237–242. [PubMed] [Google Scholar]
- 13.Takeda H., Kamogawa J., Sakayama K., Kamada K., Tanaka S., Yamamoto H. Evaluation of clinical prognosis and activities of daily living using functional independence measure in patients with hip fractures. J Orthop Sci. 2006;11:584–591. doi: 10.1007/s00776-006-1073-2. [DOI] [PubMed] [Google Scholar]
- 14.Fierens J., Broos P.L. Quality of life after hip fracture surgery in the elderly. Acta Chir Belg. 2006;106:393–396. doi: 10.1080/00015458.2006.11679913. [DOI] [PubMed] [Google Scholar]
- 15.Mezuk B., Eaton W.W., Golden S.H. Depression and osteoporosis: epidemiology and potential mediating pathways. Osteoporos Int. 2008;19:1–12. doi: 10.1007/s00198-007-0449-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gold D.T., Solimeo S. Osteoporosis and depression: a historical perspective. Curr Osteoporos Rep. 2006;4:134–139. doi: 10.1007/s11914-996-0021-6. [DOI] [PubMed] [Google Scholar]
- 17.EuroQol Group EuroQol--a new facility for the measurement of health-related quality of life. Health Pol. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 18.Brooks R. EuroQol: the current state of play. Health Pol. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 19.Rabin R., de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 20.Haywood K.L., Garratt A.M., Fitzpatrick R. Quality of life in older people: a structured review of generic self-assessed health instruments. Qual Life Res. 2005;14:1651–1668. doi: 10.1007/s11136-005-1743-0. [DOI] [PubMed] [Google Scholar]
- 21.Coast J., Peters T.J., Richards S.H., Gunnell D.J. Use of the EuroQoL among elderly acute care patients. Qual Life Res. 1998;7:1–10. doi: 10.1023/a:1008857203434. [DOI] [PubMed] [Google Scholar]
- 22.Ryan T., Enderby P., Rigby A.S. A randomized controlled trial to evaluate intensity of community-based rehabilitation provision following stroke or hip fracture in old age. Clin Rehabil. 2006;20:123–131. doi: 10.1191/0269215506cr933oa. [DOI] [PubMed] [Google Scholar]
- 23.Teerawattananon Y., Tantivess S., Yothasamut J., Kingkaew P., Chaisiri K. Historical development of health technology assessment in Thailand. Int J Technol Assess Health Care. 2009;25(Suppl 1):241–252. doi: 10.1017/S0266462309090709. [DOI] [PubMed] [Google Scholar]
- 24.Chaikledkaew U., Teerawattananon Y., Khongpittayachai S., Suksomboon N. The Graphico Systems; Nonthaburi: 2009. Thai national health technology assessment guidelines. [Google Scholar]
- 25.Röder F., Schwab M., Aleker T., Mörike K., Thon K.P., Klotz U. Proximal femur fracture in older patients--rehabilitation and clinical outcome. Age Ageing. 2003;32:74–80. doi: 10.1093/ageing/32.1.74. [DOI] [PubMed] [Google Scholar]
- 26.Nevalainen T.H., Hiltunen L.A., Jalovaara P. Functional ability after hip fracture among patients home-dwelling at the time of fracture. Cent Eur J Publ Health. 2004;12:211–216. [PubMed] [Google Scholar]
- 27.Adachi J.D., Loannidis G., Berger C., Joseph L., Papaioannou A., Pickard L. The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporos Int. 2001;12:903–908. doi: 10.1007/s001980170017. [DOI] [PubMed] [Google Scholar]
- 28.Lips P., Cooper C., Agnusdei D., Caulin F., Egger P., Johnell O. Quality of life as outcome in the treatment of osteoporosis: the development of a questionnaire for quality of life by the European Foundation for Osteoporosis. Osteoporos Int. 1997;7:36–38. doi: 10.1007/BF01623457. [DOI] [PubMed] [Google Scholar]
- 29.Ramírez-Pérez E, Clark P, Carlos F, Camacho A, Franco-Marina F. Health-related quality of life after surgery for hip fracture: a multicentric study in Mexican population. Medwave 2014;14:e5972. [DOI] [PubMed]
- 30.Harvey N.C., Biver E., Kaufman J.M., Bauer J., Branco J., Brandi M.L. The role of calcium supplementation in healthy musculoskeletal ageing : an expert consensus meeting of the European society for clinical and economic aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO) and the international foundation for osteoporosis (IOF) Osteoporos Int. 2017;28:447–462. doi: 10.1007/s00198-016-3773-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sugeno N., Goto A., Yasumura S., Kikuchi S.I. Quality of life in postoperative Japanese hip fracture patients: a hospital-based prospective study. Arch Osteoporos. 2008;3:7–15. [Google Scholar]
- 32.Tidermark J., Ponzer S., Svensson O., Söderqvist A., Törnkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg Br. 2003;85:380–388. doi: 10.1302/0301-620x.85b3.13609. [DOI] [PubMed] [Google Scholar]
- 33.Blomfeldt R., Törnkvist H., Ponzer S., Söderqvist A., Tidermark J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg Br. 2005;87:523–529. doi: 10.1302/0301-620X.87B4.15764. [DOI] [PubMed] [Google Scholar]
- 34.SALUD, SEDENA, SEMAR . Centro Nacional de Excelencia Tecnológica en Salud; México: 2012. Prevención y diagnóstico de fractura de cadera en el adulto en el primer nivel de atención. Guía de referencia rápida. Catálogo Maestro de Guías de práctica clínica SSA-017-08.http://www.cenetec.salud.gob.mx/descargas/gpc/CatalogoMaestro/017_GPC_FxCadera/SSA_017_08_GRR.pdf [Google Scholar]