Abstract
Background.
In 1997 the U.S. Environmental Protection Agency set the first annual National Ambient Air Quality Standard (NAAQS) for fine particulate matter (PM2.5). Although the weight of scientific evidence has determined that a causal relationship exists between PM2.5 exposures and cardiovascular effects, few studies have concluded whether NAAQS-related reductions in PM2.5 led to improvements in public health.
Methods.
We examined the change in cardiovascular (CV) mortality rate and the association between change in PM2.5 and change in CV-mortality rate before (2000-2004) and after implementation of the 1997 annual PM2.5 NAAQS (2005-2010) among U.S. counties. We further examined how the association varied with respect to two factors related to NAAQS compliance: attainment status and design values (DV). We used difference-in-differences and linear regression models, adjusted for sociodemographic confounders.
Findings.
Across 619 counties, there were 1.10 (95% CI: 0.37, 1.82) fewer CV-deaths per year per 100,000 people for each 1 μg/m3 decrease in PM2.5. Nonattainment counties had a twofold larger reduction in mean annual PM2.5, 2.1 μg/m3, compared to attainment counties, 0.97 μg/m3. CV-mortality rate decreased by 0.59 (95% CI: −0.54, 1.71) in nonattainment and 1.96 (95% CI: 0.77, 3.15) deaths per 100,000 people for each 1μg/m3 decrease in PM2.5 in attainment counties. When stratifying counties by DV, results were similar: counties with DV greater than 15 μg/m3 experienced the greatest decrease in mean annual PM2.5 (2.29 μg/m3) but the smallest decrease in CV-mortality rate per unit decrease in PM2.5, 0.73 (95% CI: −0.57, 2.02).
Interpretation.
We report a significant association between the change in PM2.5 and the change in CV-mortality rate before and after the implementation of NAAQS and note that the health benefits per 1 μg/m3 decrease in PM2.5 persist at levels below the current national standard.
Funding.
US EPA intermural research.
INTRODUCTION
Air quality across U.S. communities has widely improved since the enactment of the 1970 Clean Air Act (CAA) and its amendments1,2. Among a number of provisions, the CAA mandates the establishment of National Ambient Air Quality Standards (NAAQS) for criteria air pollutants to protect public health and the environment. After a new NAAQS is established, the U.S. Environmental Protection Agency (EPA) conducts a process with state and tribal governments to designate “nonattainment ” areas. A nonattainment area includes at least one ambient air quality monitoring site having data that does not meet the new NAAQS, and it includes the nearby area with emissions sources that contribute to poor air quality. The states with areas in nonattainment are required to outline permanent and enforceable control measures to improve air quality and achieve attainment. Because the measures taken to attain a standard impose costs on public and private sectors, it is important to demonstrate whether public health improvements have been achieved as a result of improving air quality.
The first annual NAAQS for fine particulate matter (PM2.5) was set in 1997 at 15 μg/m3 by EPA (Federal Register. 1997. p. 38652-760). The first designations for this NAAQS were published on January 5, 2005 (Federal Register. 2005. p. 944-1019). States with designated nonattainment areas were required to meet the standard no later than 2010 (Federal Register. 2007. p. 20585-667). During this time frame, EPA also proceeded with the promulgation of other national programs which sought to reduce emissions from stationary sources (40 CFR 60), mobile sources (40 CFR 86), and fuels/ fuel additives (40 CFR 80) as well as the regional interstate transport of criteria pollutants (40 CFR 96). Many of these measures also contributed to the reduction of PM2.5 concentrations across the country.
Previous epidemiologic studies have demonstrated that mortality and morbidity are associated with both short-term3,4 and long-term5,6 exposures to PM2.5 and that temporal reductions in long-term exposures are associated with improved health outcomes7-11. Fewer studies, however, have focused specifically on reductions in particle pollution following the establishment of a NAAQS and consequent benefits on public health. Chay, Dobkin12 reported that there was little or no improvement in mortality in the years immediately following the now revoked 1970 standard for total suspended particulates. In contrast, Zigler, Dominici13 reported reduced mortality due to regulations regardless of whether coarse particulate matter (PM10) concentrations were reduced due to 1991 PM10 NAAQS. Studies on the effectiveness of regulations, often termed "accountability studies," have not yet focused on improvements in health attributed to the annual PM2.5 NAAQS.
In this study, we examined whether the change in the cardiovascular (CV) mortality rate before (2000-2004) and after (2005-2010) the first annual PM2.5 NAAQS implementation was associated with the change in PM2.5. We further considered two factors related to NAAQS compliance—attainment status and design values—and examined whether the change in CV-mortality rates, overall as well as relative to change in PM2.5, varied among counties stratified by those factors.
METHODS
Data
Individual level mortality data was obtained from the U.S. National Center for Health Statistics (NCHS). The data was used to calculate crude cardiovascular mortality rates for each individual year from 2000 through 2010 by dividing the number of cardiovascular deaths14 in a five-year age group, county, and year by the total population of that age group in the corresponding county and year. County level CV-mortality rates were calculated as an open cohort and crude rates were further age-standardized to the U.S. age distribution of 2000. The standard errors for the CV-mortality rates were calculated using NCHS standard formulas which assume the population is known, and the number of deaths has a Poisson distribution. Uncertainty in the mortality rates arises from short-term fluctuations in the number of deaths from random factors (e.g. extreme weather or changes to available medical care) and short-term fluctuation in population estimates (e.g. transient or seasonal moves) for years between decennial census counts, regardless of a constant long-term mortality rate and population. Annual data was averaged before (2000-2004) and after (2005-2010) implementation of the 1997 annual PM2.5 NAAQS. Similarly, we calculated standardized age-adjusted mortality rates for chronic obstructive pulmonary disease (COPD) to approximate accumulated exposure to smoking8.
Air quality data was retrieved from the EPA’s Air Quality System (AQS). Environmental monitoring sites across the U.S. are located primarily based on an area’s population; therefore, sparsely populated counties rarely have monitors. First, we calculated annual average PM2.5 concentrations at each monitoring site for each year between 2000 and 2010. We then averaged the annual means across the monitors located in the same county to calculate annual averages for counties. To coincide with a requirement that at least 75% of days per reporting quarter must be collected assuming a minimum recording frequency of one in six days (40 CFR 50 App N), monitors were only included if they reported for at least 45 days (365/6*0.75≈45) of the year. Annual PM2.5 county concentrations were then averaged for periods before (2000-2004) and after (2005-2010) the publication of the first annual PM2.5 NAAQS designations.
The complete annual PM2.5 monitoring data included 775 counties. However, 69 counties did not have PM2.5 records between 2000 and 2004, and 89 counties did not have records in 2005-2010. The lack of data may be attributed to several different factors, including location change of monitor within a metropolitan statistical area, monitor malfunction or shut down. Thus, the final analysis considered 619 counties with monitored annual mean PM2.5 concentrations in both periods.
County-level socioeconomic status (SES) and demographic variables were obtained from the U.S. Bureau of the Census for 2000 and 2010. Variables included total income (in tens of thousands of U.S. dollars), percent with at least a high school diploma (of population 25 years and older), percent Hispanic (of total population), and percent black (of total population). For the purpose of this study, changes in socio-demographic variables refer to the differences between Census 2010 and Census 2000 statistics (2010 minus 2000). We also calculated average annual temperature for each county using the National American Regional Reanalysis. Annual temperatures were then averaged to two time periods, and the change in temperature was calculated such that a positive value indicates an increase in temperature (2005-2010 minus 2000-2004).
Mortality rates, air monitoring data, Census data, and temperature data were matched by five-digit county federal information processing standard codes, providing complete data for 619 counties.
Statistical Analysis
We used a difference-in-differences modeling approach to compare the change in CV-mortality rates between the two time periods, defined as before and after first designations (2000-2004 minus 2005-2010). We also used a linear regression model to estimate the association between the change in cardiovascular mortality rate and the change in PM2.5 in U.S. counties adjusted for confounders. A directed acyclic graph was used to visually represent the model and the confounders (Figure S1). We controlled for the effects of confounding (boxed variables in Figure S1) from all identified variables as no pathway between exposure and outcome was left unblocked.
The association between the change in CV-mortality rate and change in PM2.5 concentrations was evaluated for three different covariate models—models 1, 2, and 3 (Table 2)— in order to evaluate the influence of confounding on the association of interest. Similar covariate models were used in Correia, Pope 7 and Pope, Ezzati8. Model 1 adjusted for initial CV-mortality rate. Model 2 adjusted for only the strongest confounders of the PM2.5 -mortality relationship—initial cardiovascular mortality rate, change in COPD rate, and change in total income. Model 3 was adjusted by (a) initial period cardiovascular mortality rate, (b) change in COPD, (c) change in total income, (d) change in percent with high school diploma, (e) change in percent Hispanic, and (f) change in percent black. The model with the lowest Bayesian Information Criteria (BIC) was used as a preferred model. All models in the statistical analysis were weighted by the inverse variances of the changes in mortality rate. The weights were proportional to the total population (weighted Pearson correlation, ρ=0.96), giving more weight to counties with greater populations.
Table 2.
Results of Regression Models for County-Level Analysis; The reported values are the estimated changes in age-adjusted cardiovascular mortality rate associated with each variable listed on the left. Positive coefficients indicate improvement in mortality rate, fewer deaths per year per 100,000 people. Standard error of average effect estimate is given in parentheses. n = 619.
| Variable | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Weighted Mean Δ in Mortality between two time periods (deaths/ 100,000 people) | 63.14 (0.48) | 63.14 (0.47) | 63.14 (0.46) |
| PM2.5 (μg/m3) | 1.44 (0.36) | 0.99 (0.37) | 1.10 (0.37) |
| Cardiovascular Mortality Rate, 2000-2004 (deaths/ 100.000 people) | 0.12 (0.01) | 0.14 (0.01) | 0.17 (0.01) |
| Δ COPD Mortality Rate | -- | 0.36 (0.13) | 0.26 (0.13) |
| Δ Income Total (in $10K USD) | -- | 0.53 (0.16) | 0.30 (0.17) |
| Δ % High School Educated Adults | -- | -- | −1.52 (0.31) |
| Δ % Hispanic Population | -- | -- | 0.43 (0.21) |
| Δ % Black Population | -- | -- | −0.31 (0.27) |
Factors related to NAAQS compliance
Additionally, we examined whether the association between the change in CV-mortality rate and the change in PM2.5 varied based on two factors related to NAAQS compliance—attainment status and 2003 design values (DV). We retrieved attainment status from the EPA Green Book and DVs from AQS. The EPA designates NAAQS attainment status based on multiple factors including ambient monitor values, meteorology, geography and topography, contributions to nearby violations, etc. Design values are used to meet the first of these criteria and are calculated at each monitor as the three year rolling average concentration, based on annual weighted average of the quarterly means (40 CFR 50 App N). In our analysis we used 2003 DVs, which were employed to make the first designations for the 1997 NAAQS on January 5th, 2005. Specifically, we used the highest recorded 2003 DV in each county, to be consistent with methods used in a regulatory setting. We note that counties with DVs below the NAAQS may still be declared nonattainment because of the other factors.
Using these two factors related to NAAQS compliance (attainment status and 2003 DV), we stratified counties to compare changes to health between groups. Counties were stratified using the 2003 DV: below 12 μg/m3 (the current annual PM2.5 standard set in 2012), between 12 and 15 μg/m3, and above 15 μg/m3 (the 1997 annual PM2.5 standard). If a county did not have at least five DVs recorded from 2000 to 2010—with at least one value in each of the periods (2000-2004) and (2005-2010)—or if it did not have a 2003 DV, it was considered lacking sufficient records and removed from the analysis. The total difference in CV-mortality rate between (2000-2004) and (2005-2010) as well as the incremental change in CV-mortality rate per unit decrease in PM2.5, both adjusted for covariates, were used to depict changes to health.
RESULTS
The association between the change in cardiovascular mortality rate and the change in PM2.5 as well as modification of that association by attainment status was analyzed for 619 counties, capturing 70% of the U.S. population (2010). Modification of the association by design value was analyzed in 467 counties, capturing 61% of the U.S. population.
Between the two periods, the CV-mortality rate decreased on average by 61.2 deaths per year per 100,000 people, with an interquartile range of 22.1 deaths per year per 100,000 people (Table 1). Annual PM2.5 decreased on average by 1.2 μg/m3 with an IQR of 1.3 μg/m3. COPD mortality rates also decreased on average by 0.1 deaths per year per 100,000 people, representing a reduction in smoking rates among the population. From 2000 to 2010, total household income increased by $3,950 and there was a 4.8% increase in the population of those aged 25 and older possessing, at minimum, a high school diploma. Percentage of Black and Hispanic populations also increased over the study period by 1.0% and 2.8%, respectively (Table 1).
Table 1.
Summary statistics, means and interquartile ranges, for PM2.5 concentrations, mortality rates, and covariates for all counties and by factors related to NAAQS compliance strata. Changes (Δ) for PM2.5, cardiovascular mortality, and COPD mortality were calculated as 2000-2004 period minus 2005-2010 period so positive values represent improvement in air quality or health. Changes (Δ) for covariates were calculated as 2010 minus 2000 so positive values represent increase in value over time.
| All Counties | Attainment | Nonattainment | DV03 ≤ 12 | 12< DV03 ≤15 | 15 > DV03 | |
|---|---|---|---|---|---|---|
| Number of Counties | 619 | 486 | 133 | 165 | 221 | 81 |
| Cardio. Mortality Rate * 2000-2004 | 323.3 (72.1) | 320.1 (78.7) | 334.9 (43.6) | 298.8 (59.4) | 339.1 (71.3) | 344.5 (50.4) |
| Cardio. Mortality Rate, 2005-2010 | 262.1 (67.7) | 260.6 (69.3) | 267.8 (54.3) | 242.2 (53.2) | 273.9 (59.0) | 279.8 (50.2) |
| Δ Cardio. Mortality Rate | 61.2 (22.1) | 59.5 (25.4) | 67.1 (16.3) | 56.6 (25.8) | 65.1 (20.9) | 64.8(16.0) |
| PM2.5 (μg/m3), 2000-2004 | 12.0 (3.9) | 11.1 (3.4) | 15.3 (2.1) | 9.7 (2.6) | 13.6 (1.5) | 16.2 (1.2) |
| PM2.5 (μg/m3), 2005-2010 | 10.8 (3.3) | 10.2 (3.3) | 13.2 (2.0) | 8.9 (2.8) | 12.0 (1.4) | 13.9 (1.1) |
| Δ PM2.5 (μg/m3) | 1.2 (1.3) | 1.0 (1.3) | 2.1 (0.8) | 0.8 (1.0) | 1.5 (0.9) | 2.3 (1.2) |
| COPD Mortality Rate*,2000-2004 | 47.5 (15.6) | 48.3 (14.9) | 44.7 (17.2) | 47.3 (15.6) | 46.3 (15.0) | 47.4 (17.1) |
| COPD Mortality Rate, 2005-2010 | 47.4 (17.1) | 48.5 (16.5) | 43.6 (19.0) | 46.5 (17.6) | 46.7 (15.9) | 47.0 (18.9) |
| Δ COPD Mortality Rate | 0.1 (7.9) | −0.1 (8.7) | 1.1 (5.6) | 0.8 (8.2) | −0.4 (7.9) | 0.5 (4.9) |
| Total Income ($10K), 2000 | 8.0 (7.7) | 6.0 (5.3) | 15.5 (14.8) | 7.9 (8.1) | 8.1 (6.7) | 16.3 (12.7) |
| Total Income ($10K), 2010 | 8.4 (8.5) | 6.4 (5.8) | 15.8 (15.5) | 8.6 (9.1) | 8.4 (7.0) | 16.4 (14.5) |
| Δ Total Income | 0.4 (0.5) | 0.4 (0.5) | 037 (0.9) | 0.7 (0.8) | 0.3 (0.5) | 0.1 (0.8) |
| % age>25 with High School diploma, 2000 | 80.7 (8.3) | 80.6 (8.4) | 80.7 (8.0) | 82.3 (8.1) | 79.9 (8.8) | 78.7 (7.4) |
| % age>25 with High School diploma, 2010 | 85.5 (6.6) | 85.5 (6.8) | 85.5 (6.2) | 86.6 (6.3) | 84.7 (6.9) | 83.9 (6.3) |
| Δ % with High School diploma | 4.8 (2.7) | 4.8 (2.7) | 4.9 (2.3) | 4.3 (2.8) | 4.8 (2.6) | 5.2 (1.8) |
| % Black Population, 2000 | 11.7 (14.9) | 11.2 (15.1) | 13.6 (14.9) | 7.2 (9.1) | 15.7 (19.8) | 16.3 (16.7) |
| % Black Population, 2010 | 12.7 (15.7) | 12.1 (15.4) | 15.1 (15.9) | 8.1 (10.3) | 17.0 (20.3) | 17.6 (19.5) |
| Δ % Black Population | 1.0 (1.4) | 0.9 (1.4) | 1.5 (1.5) | 0.8 (1.2) | 1.3 (1.7) | 1.3 (1.5) |
| % Hispanic Population, 2000 | 7.8 (6.5) | 7.5 (5.5) | 8.9 (9.3) | 11.3 (10.2) | 5.4 (5.1) | 9.8 (6.8) |
| % Hispanic Population, 2010 | 10.6 (10.0) | 10.2 (8.5) | 12.0 (13.3) | 14.5 (14.4) | 8.0 (7.3) | 12.7 (10.0) |
| Δ % Hispanic Population | 2.8 (2.8) | 2.7 (2.7) | 3.1 (3.6) | 3.2 (3.1) | 2.6 (2.6) | 2.9 (3.1) |
deaths per year per 100,000 people
We included the CV-mortality rate for 2000-2004 as a predictor in all models because it was the strongest predictor of the change in CV-mortality rate between two periods (ρ=0.43, Figure S2). Initial CV-mortality rates were also correlated with the average PM2.5 concentrations in that period (ρ=0.39, Figure S3). Finally, there was a strong correlation between the initial concentrations of PM2.5 and the change in PM2.5 concentrations between periods (ρ=0.76, Figure S4), indicating areas with the highest initial levels of PM2.5 had the largest declines in PM2.5. The estimated decrease in CV-mortality rate with respect to the decrease in PM2.5 was consistent across the three models, ranging from 0.99 (95% CI 0.27, 1.71) to 1.44 (95% CI 0.73, 2.14) fewer deaths per year per 100,00 people per unit (1 μg/m3) decrease in PM2.5 (Table 2). Added variables altered the estimated mean effect and improved the model fit (BIC analysis), suggesting confounding effects of additional predictors on the association between of the decrease in PM2.5 and decrease in cardiovascular mortality rate. The BIC analysis identified Model 3 as the best fit for the data, estimating a decrease in mortality rate of 1.10 (95% CI 0.37, 1.82) fewer deaths per year per 100,000 people for a 1 μg/m3 reduction in PM2.5 across U.S. counties. All results presented henceforth used Model 3.
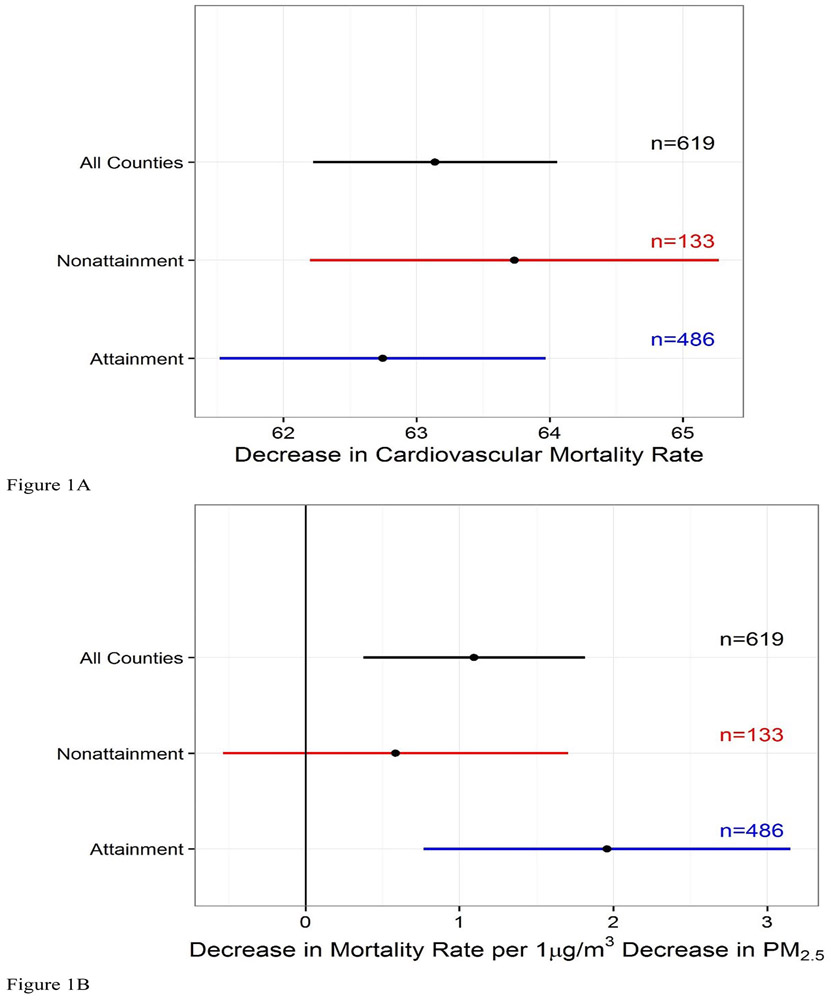
We examined effect modification by two unique factors related to PM2.5 NAAQS compliance. The average decrease in PM2.5 in nonattainment counties between periods, 2.1 μg/m3, was roughly twice that in attainment counties, 1.0 μg/m3 (Table 1; Figure S5). Between the two periods, nonattainment counties (spatial distribution mapped in Figure S6) experienced 63.74 (95% CI: 62.20, 65.27) fewer total CV-deaths (per year per 100,000 people) and 0.59 (95% CI: −0.54, 1.71) fewer CV-deaths for each μg/m3 decrease in PM2.5 (Figure 1). Attainment counties had on average 62.75 (95% CI: 61.52, 63.97) fewer total CV-deaths and 1.96 (95% CI: 0.77, 3.15) fewer CV-deaths per μg/m3 decrease in PM2.5 between the two periods.
Figure 1.
(A) Effect estimate for an absolute decrease in cardiovascular mortality rate for all counties (n=619) and by attainment status (n=619) counties—adjusted for confounders but not PM2.5 and corresponding 95% confidence intervals (B) Decrease in cardiovascular mortality rate effect estimate per unit decrease in PM2.5 for all counties, nonattainment counties, and attainment counties—adjusted for confounders and corresponding 95% confidence intervals.
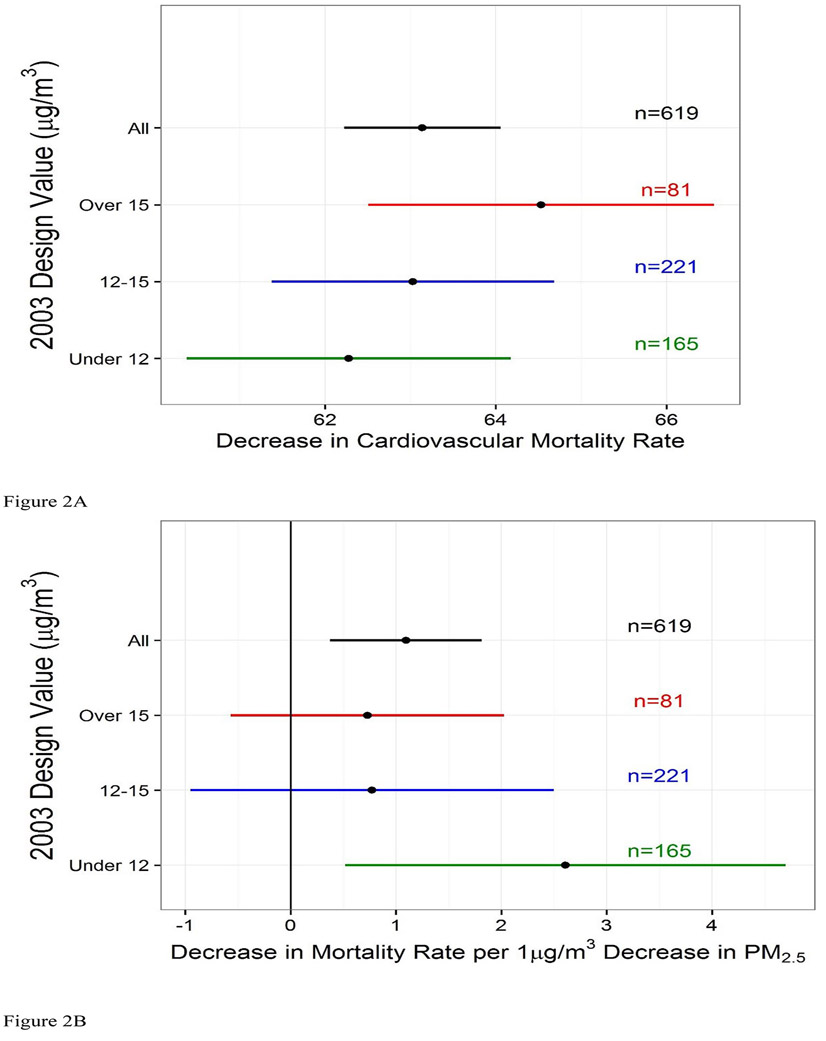
The results for both factors related to NAAQS compliance demonstrate similar trends. Counties with a 2003 DV greater than 15 μg/m3 (spatial distribution mapped in Figure S8) experienced the greatest decrease in mean annual PM2.5 of 2.3 μg/m3 between the two periods (Table 1, Figure S6). These counties with the highest initial PM2.5 concentrations experienced 64.53 (95% CI: 62.51, 66.55) fewer total CV-deaths (per year per 100,000 people) and 0.73 (95% CI: −0.57, 2.02) fewer CV-deaths for each μg/m3 decrease in PM2.5 between the two periods (Figure 2). Counties with 2003 DV less than 12 μg/m3, the lowest initial PM2.5, experienced 62.28 (95% CI: 60.38, 64.17) fewer total CV-deaths and 2.61 (95% CI: 0.52, 4.70) fewer CV-deaths per μg/m3 between the two periods.
Figure 2.
(A) Effect estimate for an absolute decrease in cardiovascular mortality rate for all counties (n=619) and by counties with respect to 2003 Design Value (DV03) (n=467) —adjusted for confounders but not PM2.5 and corresponding 95% confidence intervals (B) Decrease in cardiovascular mortality rate effect estimate per unit decrease in PM2.5 for all counties and counties with 2003 DV greater than 15 μg/m3, between 12 and 15 μg/m3. and under 12 μg/m3 —adjusted for confounders and corresponding 95% confidence intervals.
Finally, we performed a sensitivity analysis to evaluate whether the association between change in cardiovascular mortality rate and change in PM2.5 was confounded by change in temperature, which had a mean increase of 0.2°C (IQR = 0.44°C). We found that an increase in temperature of 1°C between the two time periods was associated with a decrease in cardiovascular mortality rate (5.52 (95% CI: 2.56, 8.49) fewer CV-deaths per year per 100,000 people) and with a decrease in PM2.5 (0.76 (95% CI: 0.47, 1.06) μg/m3). Change in temperature was also associated with attainment status (nonattainment counties had a mean change in temperature 0.26°C (95% CI: 0.21, 0.32) greater than that of attainment counties) probably due to regional clusters of nonattainment counties at higher latitudes. Therefore, in the sensitivity analysis, we expanded Model 3 to adjust for change in temperature and for attainment status. The new model did not alter the estimated effect, estimating 1.12 (95% CI: 0.28, 1.95) fewer deaths per year per 100,000 people for a 1 μg/m3 reduction in PM2.5 compared to 1.10 (95% CI 0.37, 1.82) fewer deaths per year per 100,000 people for a 1 μg/m3 reduction in PM2.5 (main result as previously reported). Further, when testing for effect modification by attainment status (interaction model), the effect of change in PM2.5 on change in cardiovascular mortality rate was not notably different (Figure S9).
DISCUSSION
This is the first study to consider the impact of 1997 NAAQS designations for annual PM2.5. We examined whether the change in the CV-mortality rate before (2000-2004) and after (2005-2010) the first annual PM2.5 NAAQS implementation was associated with the change in PM2.5. The results showed a significant improvement to health per unit decrease in PM2.5, 1.10 (95% CI: 0.37, 1.82) fewer CV-deaths per year per 100,000 people per 1 μg/m3 decline in PM2.5. As we stratified counties based on two factors related to NAAQS compliance to further examine this association, the results of our analysis suggest that the health benefit per unit decrease in PM2.5 persists in counties with concentrations below our current national standard for annual PM2.5 (12 μg/m3). The results are consistent with previous literature which suggest that the concentration-response (C-R) function between CV-mortality rate and PM2.5 may be nonlinear with a concave down shape, having perhaps a steeper slope at lower values of PM2.5.
The attributable fraction, the portion of health improvement tied to the decline in air pollution, was approximately 1.24 deaths per year per 100,000 people in nonattainment counties and 1.96 deaths per year per 100,000 in attainment counties. Though multiple risk factors interact to contribute to health improvement, these results suggest that 2.0% and 3.0% of the overall decrease in cardiovascular mortality rate was due to the decline in PM2.5 in nonattainment and attainment counties, respectively (2.1*0.59/63.22 and 1.0*1.96/63.86).
A significant association between the decline in annual PM2.5 and health improvements is consistent with previously published epidemiologic results. Most notably, Pope, Ezzati8 estimated an increase in life expectancy of 0.61±0.2 years was associated with a 10 μg/m3 decrease in PM2.5 in the 1980s and 1990s, and Correia, Pope 7 reported a 0.35 years increase in life expectancy per 10 μg/m3 decrease in PM2.5 from 2000 to 2007. Additionally, a number of studies have reported the persistence of the association at PM2.5 concentrations at or below the current NAAQS of 12 μg/m3, indicating that health will continue to improve as ambient concentrations of PM2.5 decline 15-20. In 2008, Schwartz, Coull20 examined closed cohorts in six U.S. cities for the association between duration of survival and long-term exposure to PM2.5 (annual mean in the year before each death) and found stronger associations at lower levels among 10, 15, 20, 25, or 30 μg/m3 cutpoints. Our study is in agreement with these reports suggesting that health benefits persist at levels below the current standard. A nonlinear concentration-response function was supported in a study on six U.S. cities where stronger associations were found when higher concentrations (25-30 μg/m3) were excluded from the analysis4. The analyses of Marshall, Apte 18, Pope, Cropper15, and others have also proposed a supralinear (concave downward) PM2.5-mortality C-R function15,16,18,21.
“Quasi-experimental” studies—i.e. studies that focus on abrupt improvements to air quality that have occurred as a result of a local event or source-control action—have reported significant absolute improvements to health22-27. For example, daily mortality in the Utah Valley significantly dropped due to a temporary closure of a steel mill in 198622; more recently, Su, Hampel25 suggested that unique air pollution controls for the 2008 Beijing Summer Olympics may have led to decreased cardiovascular mortality and CV-mortality significantly increased once the control measures were relaxed ; finally, Yorifuji, Kashima28 reports that diesel emission controls implemented in Tokyo led to a decline in PM2.5 and a 11% decrease in cardiovascular disease when adjusted for a reference population which didn’t have the emission controls. Our report of overall improvement in health after the implementation of PM2.5 NAAQS, though over a significantly longer time period, is in accordance with these studies.
Our study is the first study to consider health impacts before and after area designations for the 1997 annual PM2.5 NAAQS and reports a significant improvement to health per unit decrease in PM2.5 Previously, few other studies examined whether changes in air quality due to national air quality regulations improved public health. In evaluating the changes in total suspended particles (TSPs) induced by the Clean Air Act Amendments in 1970, Chay, Dobkin12 found that TSP concentrations declined significantly more in nonattainment counties compared to attainment counties, but nonattainment status had little association with changes in adult or elderly mortality rates. However, the TSP standards of 1970 were magnitudes higher than our current standards. Considering attainment status for the 1991 annual PM10 NAAQS, Zigler29 reported that the designations overall caused 1.76 fewer deaths per 1,000 Medicare beneficiaries. However, using principal stratification, the authors indicated that the magnitude of negative dissociative effects was similar to the negative associative effects, meaning that the regulation reduced mortality regardless of whether the regulation reduced average concentrations of PM10. Our findings are more consistent with findings reported by Zigler and colleagues.
Our study faces a number of challenges common to long-term accountability studies. First, nonattainment counties are typically clustered in or nearby urban areas and have different socio-economic, demographic characteristics compared to attainment counties. Despite controlling for changes in SES variables in our statistical model, it is possible that confounding by unmeasured factors is not accounted for. Second, technological advancements and decreasing costs of clean technology as well as other national air quality regulations and programs have reduced PM2.5 and its precursors, regardless of NAAQS attainment status. These programs have likely contributed to reductions in PM2.5 in the areas already in attainment and could play an important role in the strong association found in those counties. The EPA also put in place federal rules that target criteria air pollutant reductions, addressing the air pollution due to regional interstate transport of these pollutants. Therefore, we could not directly attribute the changes in PM2.5 and subsequent changes in mortality to a particular program in a particular county or region. Third, we did not consider association between PM2.5 species, which may have been differentially reduced across areas, and changes in cardiovascular mortality rates. The annual PM2.5 NAAQS, like most other regulations, targets a single air pollutant but may influence concentrations of co-pollutants which may interact to affect health through more complex and unaccounted for pathways. While these limitations could not be addressed here, they are valid topics for further research. Finally, the sensitivity analysis indicated an association between the change in temperature and change in mortality, which has been previously documented30, and an association between the change in temperature and attainment status. While the change in temperature did not confound the association of interest, the strong association with the change in mortality could be further explored.
This study has affirmed that reductions in PM2.5 are significantly associated with reductions in age-adjusted cardiovascular mortality rates. Further, we report that the health benefits per unit decrease in PM2.5 varied but were not statistically different between groups based on county-level factors related to NAAQS compliance. We hypothesize that the PM2.5-mortality concentration response function is nonlinear, with cleaner counties experiencing greater improvement per unit PM2.5. The findings of this study ultimately contribute to the discussion on the significance of NAAQS and other EPA regulatory actions as they relate changes in air pollution to observed improvements in public health.
Supplementary Material
Acknowledgements
Supported in part by an appointment to the Internship/Research Participation Program at Office of Research and Development (National Health and Environmental Effects Research Laboratory), U.S. Environmental Protection Agency, administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and EPA. We acknowledge Alice Cates and Jeanette Reyes for their help in data acquisition and management.
Footnotes
Data Attribution and Disclaimers:
Disclaimer: The research described in this article has been reviewed by the National Health and Environmental Effects Research Laboratory, U.S. Environmental Protection Agency, and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the Agency, nor does the mention of trade names of commercial products constitute endorsement or recommendation for use.
Conflicts of interest
None declared.
Contributor Information
Anne E. Corrigan, Oak Ridge Institute for Science and Education at the United States Environmental Protection Agency / National Health and Environmental Effects Research Laboratory / Environmental Public Health Division, NC.
Michelle M. Becker, United States Environmental Protection Agency / Region 5 / Air and Radiation Division, IL.
Lucas M. Neas, United States Environmental Protection Agency / National Health and Environmental Effects Research Laboratory / Environmental Public Health Division, NC.
Wayne E. Cascio, United States Environmental Protection Agency / National Health and Environmental Effects Research Laboratory / Environmental Public Health Division, NC.
Ana G. Rappold, United States Environmental Protection Agency / National Health and Environmental Effects Research Laboratory / Environmental Public Health Division, NC.
REFERENCES
- 1.EPA. AirTrends. 2015. [Google Scholar]
- 2.U.S. Code. Air Pollution Prevention and Control. 1970. [Google Scholar]
- 3.Laden F, Neas LM, Dockery DW, Schwartz J. Association of fine particulate matter from different sources with daily mortality in six US cities. Environ Health Persp 2000; 108(10): 941–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwartz J, Dockery DW, Neas LM. Is daily mortality associated specifically with fine particles? J Air Waste Manage 1996; 46(10): 927–39. [PubMed] [Google Scholar]
- 5.Krewski D, Burnett R, Jerrett M, et al. Mortality and long-term exposure to ambient air pollution: ongoing analyses based on the American Cancer Society cohort. Journal of toxicology and environmental health Part A 2005; 68(13-14): 1093–109. [DOI] [PubMed] [Google Scholar]
- 6.Dockery DW, Pope CA 3rd, Xu X, et al. An association between air pollution and mortality in six U.S. cities. The New England journal of medicine 1993; 329(24): 1753–9. [DOI] [PubMed] [Google Scholar]
- 7.Correia AW, Pope CA 3rd, Dockery DW, Wang Y, Ezzati M, Dominici F. Effect of air pollution control on life expectancy in the United States: an analysis of 545 U.S. counties for the period from 2000 to 2007. Epidemiology 2013; 24(1): 23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pope CA 3rd, Ezzati M, Dockery DW. Fine-particulate air pollution and life expectancy in the United States. The New England journal of medicine 2009; 360(4): 376–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zeger SL, Dominici F, McDermott A, Samet JM. Mortality in the Medicare population and chronic exposure to fine particulate air pollution in urban centers (2000-2005). Environ Health Perspect 2008; 116(12): 1614–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwartz J, Austin E, Bind MA, Zanobetti A, Koutrakis P. Estimating Causal Associations of Fine Particles With Daily Deaths in Boston. Am J Epidemiol 2015; 182(7): 644–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Y, Kloog I, Coull BA, Kosheleva A, Zanobetti A, Schwartz JD. Estimating Causal Effects of Long-Term PM2.5 Exposure on Mortality in New Jersey. Environ Health Persp 2016; 124(8): 1182–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chay K, Dobkin C, Greenstone M. The Clean Air Act of 1970 and adult mortality. J Risk Uncertainty 2003; 27(3): 279–300. [Google Scholar]
- 13.Zigler CM, Dominici F, Wang Y. Estimating causal effects of air quality regulations using principal stratification for spatially correlated multivariate intermediate outcomes. Biostatistics 2012; 13(2): 289–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.International Classification of Diseases (ICD-10). In: Organization WH, editor, p. Codes 0.-79.9. [Google Scholar]
- 15.Pope CA, Cropper M, Coggins J, Cohen A. Health benefits of air pollution abatement policy: Role of the shape of the concentration-response function. J Air Waste Manage 2015; 65(5): 516–22. [DOI] [PubMed] [Google Scholar]
- 16.Crouse DL, Peters PA, van Donkelaar A, et al. Risk of Non accidental and Cardiovascular Mortality in Relation to Long-term Exposure to Low Concentrations of Fine Particulate Matter: A Canadian National-Level Cohort Study. Environ Health Persp 2012; 120(5): 708–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daniels MJ D Francesca; Zeger Scott L.; Samet Jonathan M. The National Morbidity, Mortality, and Air Pollution Study Part III: PM10 Concentration–Response Curves and Thresholds for the 20 Largest US Cities: Health Effects Institute, 2004. [PubMed] [Google Scholar]
- 18.Marshall JD, Apte JS, Coggins JS, Goodkind AL. Blue Skies Bluer? Environ Sci Technol 2015; 49(24): 13929–36. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz J, Laden F, Zanobetti A. The concentration-response relation between PM2.5 and daily deaths. Environ Health Persp 2002; 110(10): 1025–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwartz J, Coull B, Laden F, Ryan L. The effect of dose and timing of dose on the association between airborne particles and survival. Environ Health Persp 2008; 116(1): 64–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu XC, Lin CQ, Li Y, Yao T, Fung JCH, Lau AKH. Assessment of health burden caused by particulate matter in southern China using high-resolution satellite observation. Environ Int 2017; 98: 160–70. [DOI] [PubMed] [Google Scholar]
- 22.Pope CA 3rd, Schwartz J, Ransom MR. Daily mortality and PM10 pollution in Utah Valley. Archives of environmental health 1992; 47(3): 211–7. [DOI] [PubMed] [Google Scholar]
- 23.Clancy L, Goodman P, Sinclair H, Dockery DW. Effect of air-pollution control on death rates in Dublin, Ireland: an intervention study. Lancet 2002; 360(9341): 1210–4. [DOI] [PubMed] [Google Scholar]
- 24.Wang WT, Primbs T, Tao S, Simonich SLM. Atmospheric Particulate Matter Pollution during the 2008 Beijing Olympics. Environ Sci Technol 2009; 43(14): 5314–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Su C, Hampel R, Franck U, et al. Assessing responses of cardiovascular mortality to particulate matter air pollution for pre-, during- and post-2008 Olympics periods. Environ Res 2015; 142: 112–22. [DOI] [PubMed] [Google Scholar]
- 26.Breitner S, Stolzel M, Cyrys J, et al. Short-Term Mortality Rates during a Decade of Improved Air Quality in Erfurt, Germany. Environ Health Persp 2009; 117(3): 448–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peel JL, Klein M, Flanders WD, Mulholland JA, Tolbert PE. Impact of Improved Air Quality During the 1996 Atlanta Summer Olympic Games on Cardiovascular and Respiratory Outcomes. Epidemiology 2008; 19(6): S318–S. [PubMed] [Google Scholar]
- 28.Yorifuji T, Kashima S, Doi H. Fine-particulate Air Pollution from Diesel Emission Control and Mortality Rates in Tokyo. Epidemiology 2016; 27(6). [DOI] [PubMed] [Google Scholar]
- 29.Zigler CM K Chanmin; Choirat Christine; Hansen John Barrett; Wang Yun; Hund Lauren; Samet Jonathan; King Gary; Dominici Francesca. Causal Inference Methods for Estimating Long-Term Health Effects of Air Quality Regulations. 187: Health Effects Institute, 2016. [PubMed] [Google Scholar]
- 30.Kinney PL, Schwartz J, Pascal M, et al. Winter Season Mortality: Will Climate Warming Bring Benefits? Environmental research letters : ERL [Web site] 2015; 10(6): 064016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.