Abstract
Purpose
The aim was to evaluate whether neck-specific exercise, with (NSEB) or without (NSE) a behavioural approach, improves health-related quality of life (HRQoL) compared to physical activity prescription (PPA) in chronic whiplash-associated disorders (WAD) grades 2 and 3. A secondary aim was to identify factors associated with HRQoL and HRQoL improvement following exercise interventions.
Methods
This is a secondary analysis of a multicentre randomized clinical trial. Participants (n = 216) with chronic WAD grades 2 and 3 were randomized to 12 weeks of PPA or physiotherapist-led NSE or NSEB. The EQ-5D 3L/EQ-VAS and SF-36v2 physical (PCS) and mental (MCS) component summaries were collected together with several neck-related and psychosocial outcomes at baseline, after 3, 6 and 12 months, and were analysed with linear mixed models (all time points) and multivariate linear regressions (baseline, 6 months).
Results
NSE/NSEB resulted in better outcomes than PPA (EQ-VAS and SF-36 PCS, both groups, p < 0.01) but not in a higher EQ-5D score. Improvement over time was seen in EQ-5D/EQ-VAS for the NSEB group (p < 0.01), and for NSE/NSEB as measured with the PCS (p < 0.01). Factors associated with baseline HRQoL and change to 6 months in HRQoL (R2 = 0.38–0.59) were both neck-related and psychosocial (e.g. depression, work ability).
Conclusion
Neck-specific exercise, particularly with a behavioural approach, may have a more positive impact on HRQoL than physical activity prescription in chronic WAD grades 2 and 3. HRQoL is however complex, and other factors also need to be considered. Factors associated with HRQL and improvements in HRQoL following exercise are multidimensional.
Trial registration number: ClinicalTrials.gov, No. NCT01528579.
Electronic supplementary material
The online version of this article (10.1007/s11136-018-2004-3) contains supplementary material, which is available to authorized users.
Keywords: Quality of life, Whiplash, Spine, Exercise, Physiotherapy, Chronic
Introduction
Neck pain is rated as the 6th leading global cause of years lived with disability, which is higher than for instance diabetes and ischemic heart disease [1]. One cause that presents a significant public health problem is whiplash-associated disorders (WAD). Hospital visits, impairment and disability due to WAD have increased, and the annual incidence of reported whiplash injuries is likely to be at least 300 per 100,000 [2–4]. The recovery rate after a whiplash injury in general is 50%, but among those with neurological deficits, 90% continue to report symptoms after 1 year [5–7]. People with chronic WAD report worse health than people with non-specific chronic neck pain [8, 9]. WAD thus has a clear impact on health-related quality of life (HRQoL). The worse the level of disability, the lower the HRQoL and the higher the costs for society regarding WAD [10]. Lower HRQoL in chronic WAD has also been associated with depression, pain catastrophizing and pain, as well as non-pain-related factors [11, 12]. Physical health in general is strongly associated with age, while mental health is reportedly less so [13]. Health is thus multidimensional, and in the general population comorbidities, age and low social class are the major factors suggested to impact HRQoL in several studies [14]. The World Health Organization defines health as “a state of complete physical, mental and social well-being and not merely absence of disease or infirmity” [15]. Chronic WAD involves a variety of symptoms with considerable overlap between physical and psychosocial origins, thus both aspects may need to be considered when choosing the appropriate treatment. In order to address psychological factors, cognitive behavioural components in physiotherapy management of chronic WAD have been suggested [16].
Looking further into the physical manifestations of longstanding WAD, dysfunction and characteristic fatty infiltration of predominantly the deep cervical muscles are reported [17–20]. Exercise of these muscles may thus be a feasible treatment. The positive impact general physical activity has on health is well established [21], but to our knowledge only one randomized controlled trial [22] of neck-specific exercise has included both chronic WAD grade 2 (with pain and local physical findings) and grade 3 (also including neurological findings) as defined by the Quebec Task Force [23]. The study reported reduced disability following neck-specific exercise without (= NSE) or with (= NSEB) a behavioural approach compared to physical activity prescription (PPA) [22, 24]. However, whether this also translates into better HRQoL in chronic WAD grades 2 and 3 has not previously been reported in the literature. Furthermore, to our knowledge factors that can explain improvement in health following exercise interventions in this group are also unknown.
The aim of this analysis was to evaluate whether neck-specific exercise, with or without a behavioural approach, improves HRQoL compared to physical activity prescription in chronic WAD grades 2 and 3. A secondary aim was to identify factors associated with HRQoL and HRQoL improvement, which can explain the variance of the improvement, following these three exercise interventions. We hypothesized that NSE/NSEB would have a more positive impact on HRQoL than PPA.
Methods
Design and procedure
This is a secondary analysis of a multicentre randomized clinical trial [22]. Informed consent was collected before randomization into one of three exercise groups, using a computer-generated list. It was handled by an independent researcher who put the results into opaque envelopes for further distribution to the treating physiotherapists. The data, collected at baseline and at 3, 6 and 12 months, were registered by another independent researcher. The number of participants at each time point is presented in Fig. 1.
Fig. 1.
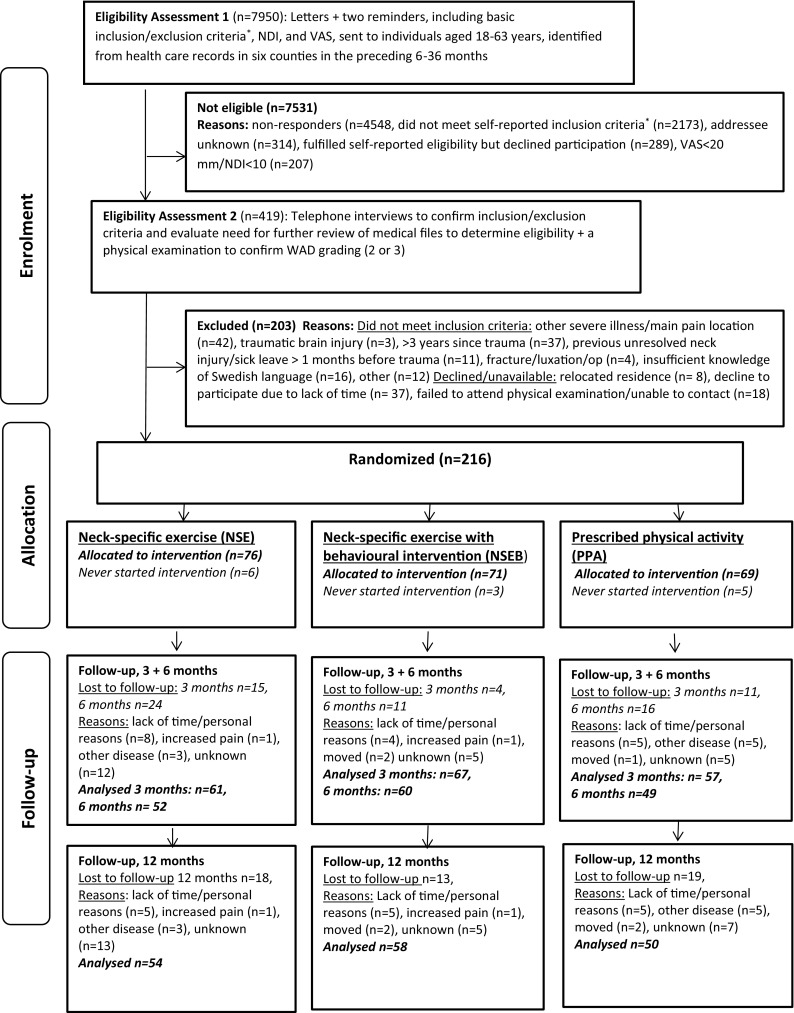
Flow chart of participants. The numbers indicate participants who answered the EQ-5D/SF-36
*Whiplash injury in the preceding 6–36 months, reported to be the onset of current symptoms, unconsciousness/loss of memory in connection with the whiplash injury, previous neck trauma with unresolved symptoms, previous neck surgery, ongoing malignant disease, severe psychiatric disorders, drug abuse, difficulties understanding the Swedish language
Participants
The 216 participants, aged 18–63, with WAD grade 2 or 3 for 6–36 months, were recruited in 2011–2012. Additional inclusion criteria were a Neck Disability Score (NDI) [25] of > 10/50 points and/or an average neck pain intensity over the past week on the Visual Analogue Scale (VAS) of > 20/100 mm. Exclusion criteria included previous neck trauma with unresolved symptoms, more dominant pain elsewhere, insufficient knowledge of the Swedish language and conditions that were potentially detrimental to completing the study interventions [22].
The mean age was 40.5 (range 18–63, SD 11.4) years, and 142 (65%) women and 74 (35%) men were included. Further baseline characteristics are presented in Table 1. Comorbidity was evaluated with question number 4 from the Work Ability Index (WAI) [26], where participants were asked to report whether they currently suffer from any other diseases (circulatory, respiratory, disease of the nervous system, eye/ear, gastrointestinal system, urinary system/genitals, skin, blood, tumours, metabolic disease, eating disorders, psychological distress, congenital disabling deformity or other).
Table 1.
Baseline variables
| Variable | NSE (n = 76) | NSEB (n = 71) | PPA (n = 69) | p value |
|---|---|---|---|---|
| WAD grade 2/3 [n (%)] | 49/27 (64/36) | 33/38 (46/54) | 41/28 (58/42) | 0.08 |
| Gender female [n (%)] | 57 (75) | 47 (66) | 38 (55) | 0.04 |
| Age, mean (range) SD | 38 (18–62) 11.3 | 40 (19–63) 11.6 | 43 (19–63) 10.7 | 0.03 |
| Months since injury, mean (range) SD | 19 (6–36) 8.7 | 20 (6–36) 8.9 | 20 (6–36) 10.3 | 0.69 |
| Smoker [n (%)] | 17 (22) | 8/62 (11/89) | 12/55 (18/82) | 0.22 |
| Educational level [n (%)] | 0.44 | |||
| Educational level, elementary | 4 (5) | 6 (9) | 6 (9) | |
| Educational level, high school | 38 (50) | 40 (57) | 34 (51) | |
| Educational level, university | 31 (41) | 21 (30) | 24 (36) | |
| Educational level, other | 3 (4) | 3 (4) | 3 (4) | |
| Use of analgesic drugs yes [n (%)] | 40 (53) | 44 (62) | 45 (67) | 0.23 |
| Employed [n (%)] | 61 (80) | 57 (80) | 52 (75) | 0.71 |
| Physical activity level, IPAQ | 0.74 | |||
| Physical activity level, low | 16 (30) | 14 (26) | 25 (34) | |
| Physical activity level, medium | 26 (48) | 25 (45) | 26 (36) | |
| Physical activity level, high | 12 (22) | 16 (29) | 22 (30) | |
| Comorbidity yes [n (%)]a | 56 (74) | 52 (73) | 49 (71) | 0.76 |
| Mental disorder/distress | 15 (20) | 20 (29) | 18 (27) | |
| Gastrointestinal disease | 17 (23) | 18 (27) | 21 (32) | |
| Respiratory disease | 17 (22) | 12 (18) | 6 (9) | |
| Skin disease | 16 (21) | 12 (18) | 7 (11) | |
| Cardiovascular disease | 8 (11) | 8 (11) | 6 (9) | |
| Endocrine/metabolic disease | 9 (12) | 8 (12) | 11 (17) | |
| Neurological/sensory disease (eye, ear) | 10 (13) | 4 (6) | 9 (13) | |
| Digestive disease | 9 (12) | 8 (12) | 11 (17) | |
| Number of comorbidities, mean (SD) | 1.8 (1.3) | 1.7 (1.4) | 1.8 (1.4) | 0.90 |
| Pain catastrophizing (PCSc), mean (SD) | 19 (10) | 20 (13) | 17 (10) | 0.46 |
| HADS, depression, mean (SD) | 4.5 (3.8) | 4.8 (4.3) | 5.0 (4.3) | 0.89 |
| HADS, anxiety, mean (SD) | 5.8 (3.9) | 5.9 (5.1) | 6.3 (3.6) | 0.78 |
| Neck disability (NDI), mean (SD) | 31 (12.5) | 34 (13.6) | 34 (13.7) | 0.39 |
| Current pain, VAS, mean (SD) | 39 (24) | 46 (24) | 42 (26) | 0.26 |
| Pain disability (PDI), mean (SD) | 19 (12) | 23 (16) | 20 (13) | 0.30 |
| Work ability (WAI), mean (SD) | 35 (6) | 36 (7) | 35 (7) | 0.64 |
| Kinesophobia (TSK), mean (SD) | 22 (5) | 22 (6) | 22 (6) | 0.99 |
HADS Hospital Anxiety and Depression Scale, IPAQ International Physical Activity Questionnaire, NDI Neck Disability Index (% score), NSE neck-specific exercise, NSEB neck-specific exercise with behavioural approach, PCSc Pain Catastrophizing Scale, PDI Pain Disability Index, PPA prescription of physical activity, SD standard deviation, TSK Tampa Scale of Kinesiophobia, VAS Visual Analogue Scale, WAD whiplash-associated disorder
aComorbidity: non-musculoskeletal diseases with > 5 participants in all of the groups are specified. Tumours, blood, genital/urinary disease, birth defects and “other” with < 5 participants and are not presented
Interventions and settings
The interventions were led by experienced primary care physiotherapist in six Swedish counties. The physiotherapists were selected and matched to the interventions to work within their field of interest and knowledge as far as possible. A one-day training workshop was held by the project leaders. The workshops were matched to the interventions, and included manual end exercise training, theoretical information, and standardized oral and written information about the interventions. The timeframe and specific components of the interventions during the 12-week intervention period have been previously published [22], but are presented briefly below.
Neck-specific exercise (NSE)
Neck-specific exercise without pain provocation and with a focus on the deep cervical muscles was performed with a physiotherapist twice weekly, with additional home exercises. After initial unresisted activation of the deep muscles in lying and sitting, gym exercises without pain provocation were introduced, with progressive head resistance training using a weighted pulley, focusing on good posture and low load endurance. A detailed description of the exercises can be found at the Academic Archive On-line [27].
Neck-specific exercise with a behavioural approach (NSEB)
The exercises were the same as those undertaken by the NSE group, but in accordance with the concept of behavioural graded exercise, participants were encouraged not to focus on a temporary increase in neck pain, but rather on success in exercise progression [28]. They also received basic behavioural intervention training, led by the physiotherapist. This included oral education regarding physiological and psychological aspects of pain, as well as activities aimed at pain management (such as relaxation, breathing exercises, etc.), goal setting and problem-solving, including the management of symptomatic relapses. Patients were encouraged to consider what they learnt and practise relevant pain management skills, for instance relaxation exercises, at home between sessions [22].
Physical activity prescription (PPA)
Based on medical history and a short motivational interview [29], participants were prescribed individually tailored general physical activity (e.g. gym classes, Nordic walking) to be performed outside the health care system. One follow-up visit or phone call was encouraged.
Outcomes
Two generic measurements were used to measure HRQoL, the EQ-5D 3L and the SF-36v2®. The two instruments do not provide interchangeable results for people with neck pain, unlike in many other clinical areas [30, 31]. Furthermore, the SF-36 can be presented as separate physical and mental health summaries, which is not the case with EQ-5D. Both measurements come with sets of preference weights obtained from the general population in the UK, using standard gamble (SF-36) and time-trade-off (EQ-5D) techniques. The EQ-5D index score can be used in cost-effectiveness analyses, while the SF-36 separated summary scores cannot.
The main outcome for this analysis was the EQ-5D questionnaire which is commonly used, and is recommended by the National Institute for Health and Clinical Excellence [NICE] [32] in cost-effectiveness analyses, which are becoming increasingly important in health care. The EQ-5D consists of a descriptive system and the EQ-VAS. The score is a five-dimensional health state classification [33] focusing on mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension is assessed by one question on a three point scale (no problems, some problems, extreme problems) on the day the questionnaire is completed. The results are scored and converted to a single summary index between − 0.59 and 1.00, with 1.00 indicating ‘full health’ and 0 representing ‘dead’. Negative EQ-5D scores represent health states valued as worse than dead. The EQ-5D also consists of a separate vertical VAS scale (EQ-VAS) from 0 (worst imaginable health state) to 100 (best imaginable health state), which records the respondent’s self-rated health. Thus, other individual aspects of perceived health, not covered by the five questions, can also be considered. The EQ-5D is considered valid and reliable [34]. In general western populations, aged 18–64, the average EQ-5D scores are reported to range from 0.776 (older ages) to 0.979 (younger ages), and in EQ-VAS, 71 (older ages) to 89 (younger ages) [35]. Permission to use the EQ-5D was obtained from the EuroQol Group Foundation.
The secondary outcome was the valid and reliable Short Form 36 (SF-36v2) Health Survey [36, 37]. It contains 36 items, measuring eight health-related quality of life domains—physical functioning, role limitation (physical), bodily pain, general health, vitality, social functioning, role limitation (emotional) and mental health, with a four-week recall period. Scores from the eight domains are weighted and aggregated into two summary measures as t-scores, the physical component summary (PCS) and the mental component summary (MCS), where higher scores represent better health. In general western populations, mean PCS and MCS scores are reported to be around 51 [38], with a range from PCS 47/MCS 52 (ages 55–64) to PCS 54/MCS 46 (ages 18–24) [39]. A licence to use the SF-36 was obtained from Quality Metrics Inc., USA.
Factors potentially associated with HRQoL and change in HRQoL score
To examine factors associated with baseline, and change in the EQ-5D index, EQ-VAS, PCS and MCS, scores from baseline and the six-month follow-up were chosen, where all self-reported measures of primary interest were collected. (At 3 months, the Hospital Anxiety and Depression Scale (HADS scored 0–21) [40] and the Tampa Scale for Kinesiophobia, TSK-11 short form, TSK scored 11–44 [41], were not collected). Factors were chosen from predictors presented in the literature of health in general, together with other measurements of relevance to longstanding WAD from our RCT study: gender, age, WAD grade, comorbidities (number), months since injury, neck pain intensity (VAS scale 0–100), neck-related disability (NDI, 0–50 [25]), pain catastrophizing (the Pain Catastrophizing Scale, (PCSc) 0–52 [42]), kinesiophobia (TSK), self-efficacy despite pain (Self-Efficacy Scale, SES, 0–200, [43]), the Work Ability Index (WAI, 7–49 [26]), anxiety and depression (HADS), and general pain-related disability [Pain Disability Index (PDI (0–70)] [44]. For the analysis of factors associated with change in the EQ score, the change scores of these measurements were used, and randomization group and adherence (more or less than 50%) were also added.
Statistics
The sample size was based on the primary outcome of the main study (the NDI) as previously reported [22]. Descriptive statistics and group comparisons with one-way ANOVA, the Kruskal–Wallis test or Χ2 test as appropriate were used for baseline characteristics. The EQ-5D can be regarded as a continuous outcome [45]. Linear mixed models were used to analyse the EQ-5D score/VAS and both SF-36 summary scores, including all available data at all four time points, and three group levels. A factor analytic, first-order heterogeneous covariance matrix was used, with randomization group and time as fixed factors. To control for the significant differences between groups, gender and age were added as covariates. The Bonferroni correction was used for post hoc estimated marginal means main effects.
To test factors associated with change in the HRQoL scores, bivariate correlations were first tested with Spearman’s (non-parametric) test and Pearson’s (parametric and biserial for gender) test. The purpose of these analyses was to find out which factors to include in the multivariate linear regression model. Significant variables were entered into a multivariate linear regression model after checking independent variables for collinearity with linear regressions for each variable. There was no collinearity between any of the independent variables (all variance inflation factors < 5 and tolerance levels > 0.36). The multivariate linear regression of significant factors was performed with stepwise backward regression, with p ≥ 0.1 as a limit for removal of variables to reduce the risk of overlooking potential important factors.
The significance level was set at p ≤ 0.05. Analyses were performed with SPSS 23.0 (SPSS Inc., Chicago, IL, USA).
Results
Adherence and drop-out analysis
The percentage of adherent participants (at least 50% attendance) during the 12-week intervention period was 70% and 71% in the NSE and NSEB groups and 47% in the PPA group (p = 0.07). The questionnaires were completed by 170–185 participants (79–85%) at the follow-ups (Fig. 1). There was no difference between completers and 12-month dropouts regarding baseline EQ-5D score, EQ-VAS, PCS/MCS, gender, age or comorbidities (all p > 0.29). No serious adverse events were reported but two participants dropped out due to increased pain (Fig. 1), which may be associated with registered deviation from the exercise protocol.
Results of the randomized study
Mean scores and p values of differences between groups and over time are presented in Table 2.
Table 2.
Health-related quality of life scores from baseline to 12 months
| n | Mean EQ-5D score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 95% CI | 3 months | 95% CI | 6 months | 95% CI | 12 months | 95% CI | p value | ||
| NSE | 76 | 0.649 (0.217) | 0.599–0.698 | 0.685 (0.233) | 0.626–0.745 | 0.680 (0.258) | 0.611–0.749 | 0.708 (0.243) | 0.643–0.773 | 0.52 |
| NSEB | 70 | 0.552 (0.307) | 0.478–0.625 | 0.686 (0.212) | 0.633–0.738 | 0.704 (0.250) | 0.638–0.771 | 0.673 (0.276) | 0.602–0.745 | < 0.01 |
| PPA | 69 | 0.631 (0.249) | 0.570–0.692 | 0.622 (0.291) | 0.545–0.699 | 0.627 (0.285) | 0.547–0.707 | 0.618 (0.289) | 0.536–0.639 | 0.90 |
| n | Mean EQ-VAS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 95% CI | 3 months*** | 95% CI | 6 months | 95% CI | 12 months*** | 95% CI | p value | ||
| NSE | 75 | 65 (16) | 60–69 | 70 (18) | 63–74 | 70 (21) | 65–76 | 70 (21) | 64–76 | 0.14 |
| NSEB | 70 | 61 (20) | 54–65 | 66 (20) | 61–73 | 71 (20) | 66–78 | 71 (20) | 67–78 | < 0.01 |
| PPA | 69 | 64 (18) | 60–69 | 61 (21) | 54–66 | 64 (20) | 59–70 | 62 (21) | 55–67 | 0.12 |
| n | Mean SF-36 physical component score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 95% CI | 3 months*** | 95% CI | 6 months | 95% CI | 12 months*** | 95% CI | p value | ||
| NSE | 74 | 42.54 (6.41) | 40.66–44.41 | 45.44 (7.40) | 43.24–47.63 | 45.93 (7.93) | 43.24–47.23 | 46.01 (8.46) | 43.65–48.54 | < 0.01 |
| NSEB | 70 | 43.02 (6.80) | 41.15–44.48 | 44.85 (6.76) | 42.98–46.91 | 45.46 (7.25) | 43.49–47.42 | 46.22 (7.56) | 44.15–48.28 | < 0.01 |
| PPA | 69 | 42.14 (6.23) | 40.26–44.01 | 42.95 (9.20) | 40.23–45.68 | 43.89 (7.70) | 41.63–46.14 | 42.72 (8.47) | 40.21–45.23 | 0.33 |
| n | Mean SF-36 mental component score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 95% CI | 3 months*** | 95% CI | 6 months | 95% CI | 12 months | 95% CI | p value | ||
| NSE | 74 | 47.89 (8.74) | 44.43–51.34 | 49.37 (12.74) | 44.35–54.38 | 49.75 (9.63) | 45.98–53.53 | 50.71 (10.82) | 46.56–54.87 | 0.38 |
| NSEB | 70 | 47.17 (10.73) | 43.97–50.37 | 49.20 (10.05) | 46.14–52.26 | 49.48 (11.23) | 46.16–52.80 | 48.71 (13.44) | 44.54–52.89 | 0.21 |
| PPA | 65 | 46.50 (12.03) | 41.83–51.17 | 47.37 (11.42) | 43.02–51.73 | 46.09 (13.57) | 40.85–51.32 | 46.21 (12.74) | 41.39–51.04 | 0.91 |
Adjusted for age and gender
NSE Neck-specific exercise group, NSEB Neck-specific exercise group with a behavioural approach, PPA physical activity group, EQ-5D Euroqol 5 dimension questionnaire, SF-36 Short Form health questionnaire 36, CI confidence interval
***p < 0.01 difference between groups
Regarding the EQ-5D score, there was a significant group-by-time interaction (F = 3.1, p < 0.01) with significant difference over time (F = 3.3, p = 0.02). There was a significant improvement in the NSEB group from baseline to three months, which was maintained over all time points (F = 5.1, p < 0.01). However, the changes in the NSE (F = 1.6, p = 0.20) and PPA groups (F = 0.1, p = 0.9) were insignificant. There was no difference between groups (F = 1.3, p = 0.28) (Table 2).
Regarding the EQ-VAS, there was a significant group-by-time interaction (F = 4.3, p = 0.49) with significant difference over time (F = 4.3, p < 0.01) and between groups (F = 10.0, p < 0.01). There were significant differences between both the NSE and NSEB groups compared to the PPA group (NSE, NSEB p < 0.01) at 3 and 12 months. The NSEB group improved over time (F = 8.0, p < 0.01), and the significant change at 6 months was maintained at 12 months. The changes over time in the NSE (F = 1.9, p = 0.14) and PPA (F = 2.0, p = 0.12) groups were insignificant (Table 2).
Regarding the SF-36 PCS, there was a significant difference between groups (F = 12.7, p < 0.01) and time (F = 4.7 p < 0.01). There were significant differences between both the NSE and NSEB groups compared to the PPA group (p < 0.01). Both the NSE/NSEB groups improved over time (NSE F = 6.5, p < 0.01, NSEB F = 6.6, p < 0.01), as opposed to the PPA group (p = 0.33). The NSE group remained improved at all follow-ups, and the NSEB group had improved at the 6- and 12-month follow-ups. The group-by-time interaction effect was insignificant (F = 0.9, p = 0.48) (Table 2).
For the MCS, there was a significant group difference (F = 5.9, p < 0.01), between both the NSE and NSEB groups compared to the PPA group (NSE p = 0.03, NSEB p < 0.01) at 3 months. The time (F = 0.4, p = 0.78) and interaction effects (F = 0.7, p = 0.65) were insignificant (Table 2).
There were no differences between the NSE/NSEB groups in any of the HRQoL outcomes at any time point.
At baseline, 69% of the participants reported comorbidity (n = 148). The two most common comorbidities were psychological distress (24%, n = 51) and pulmonary disease, e.g. asthma/bronchitis (16%, n = 34). Participants who reported comorbidities tended to report worse health than those without: EQ-5D score 0.593 (SD 0.270) versus 0.653 (SD 0.240), p = 0.12, EQ-VAS 62 (SD 17) versus 67 (SD 18) mm, p = 0.05, PCS 42.3 versus 44.1 and MCS 45.2 versus 49.9, p = 0.07 for both.
Factors associated with the HRQoL scores and change scores
Baseline score
At baseline, a bivariate significant correlation was found between the different HRQoL measurements and most scores and comorbidity. Months since injury was not associated with any of the outcomes, whereas for instance age, educational level, pain, depression and WAD grade were correlated with some of the HRQoL outcomes (Supplement 1).
The significant factors (presented in Supplement 1) were used in the multivariate linear models, and the results of the final models explaining 43–59% of the variance are presented in Table 3. When considering the influence of all other factors, HADS depression was the only factor significantly associated with all four HRQoL outcomes. It was negatively associated, i.e. higher levels of depression predict lower HRQoL with an EQ-5D score of 0.02 or 1.27 mm on the EQ-VAS per HADS point. Work ability (WAI) and pain disability (PDI) were associated with three out of four outcomes.
Table 3.
Factors associated with HRQL baseline and 6-month change scores, results of final multivariate models
| Factors associated with | Baseline EQ-5D score (R2 = 0.52) | Baseline EQ-VAS (R2 = 0.43) | Baseline SF-36 PCS (R2 = 0.59) | Baseline SF-36 MCS (R2 = 0.45) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b (SE) | β | p | b (SE) | β | p | b (SE) | β | p | b (SE) | β | p | |
| WAI | 0.01 (0.00) | 0.34 | < 0.01 | 0.80 (0.22) | 0.30 | < 0.01 | 0.27 (0.08) | 0.28 | < 0.01 | n.a | n.a | n.a |
| HADS depression | − 0.02 (0.01) | − 0.325 | < 0.01 | − 1.27 (0.33) | − 0.29 | < 0.01 | − 0.42 (0.11) | 0.27 | < 0.01 | − 1.14 (0.26) | − 0.24 | < 0.01 |
| HADS anxiety | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a | − 0.50 (0.21) | − 0.19 | 0.02 |
| Comorbidities, numbers | 0.03 (0.01) | 0.125 | 0.03 | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a |
| PDI | − 0.004 (0.02) | − 0.228 | 0.01 | n.a | n.a | n.a | − 0.87 (0.43) | − 0.18 | 0.04 | − 0.18 (0.80) | − 0.21 | 0.03 |
| PCSc | − 0.004 (0.02) | − 0.174 | 0.01 | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a |
| SES | − 0.001 (0.001) | − 0.195 | 0.02 | n.a | n.a | n.a | 0.02 (0.01) | 0.13 | 0.09 | n.a | n.a | n.a |
| Age | n.a | n.a | n.a | n.a | n.a | n.a | − 0.71 (0.31) | − 121 | 0.02 | n.a | n.a | n.a |
| NDI | n.a | n.a | n.a | n.a | n.a | n.a | − 0.42 (0.9) | − 0.44 | < 0.01 | 0.44 (0.16) | 0.27 | 0.01 |
| Pain VAS | n.a | n.a | n.a | − 0.16 (0.53) | − 0.21 | < 0.01 | n.a | n.a | n.a | n.a | n.a | n.a |
| Factors associated with | EQ-5D change score (R2 = 0.42) | EQ-VAS change (R2 = 0.41) | SF-36 PCS change (R2 = 0.45) | SF-36 MCS change (R2 = 0.38) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b (SE) | β | p | b (SE) | β | p | b (SE) | β | p | b (SE) | β | p | |
| Educational level | 0.07 (0.03) | 0.19 | 0.01 | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a |
| HADS depression change | 0.03 (0.01) | 0.36 | < 0.01 | 3.00 (0.57) | 0.44 | < 0.01 | n.a | n.a | n.a | 0.86 (0.25) | 0.32 | 0.01 |
| PCSc change | 0.01 (0.0) | 0.22 | 0.02 | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a |
| VAS change | 0.002 (0.0) | 0.18 | 0.03 | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a | n.a |
| WAI change | n.a | n.a | n.a | 1.01 (0.58) | 0.30 | 0.01 | 0.18 (0.09) | 0.18 | 0.057 | 0.33 (0.14) | 0.25 | 0.02 |
| NDI change | n.a | n.a | n.a | n.a | n.a | n.a | 0.28 (0.05) | 0.54 | < 0.01 | 0.12 (0.07) | 0.17 | 0.01 |
Results of the final regression models
EQ-5D Euroqol 5 dimensions health questionnaire, SF-36 Short Form 36 health questionnaire, PCS Physical component summary, MCS mental component summary, HADS Hospital Anxiety and Depression Scale, PDI Pain disability score, PCSc Pain Catastrophizing Scale, SES Self-Efficacy Scale, VAS Visual Analogue Scale, WAI Work Ability Index, NDI Neck Disability Index, n.a. not applicable due to variable not included in the final step of the regression. β standardized regression coefficient, b unstandardized coefficient, SE standard error
Change scores from baseline to 6 months
For change scores from baseline to 6 months, univariate significant correlations were found between the different HRQoL change scores and the change scores of most outcomes. No correlation was found between the HRQoL change scores and educational level, months since injury or adherence. Age, WAD grade and randomization group were correlated with some of the outcomes, and gender and comorbidity were close to a significant correlation with the EQ-5D index (p = 0.053–0.06) (Supplement 1).
The significant factors were used in the multivariate linear models, and the results of the final models, explaining 38–45% of the variance, are presented in Table 3. No factors were associated with all four HRQoL outcomes, but reduction of depression was associated with improvements in all but the PCS. A decrease of the level of depression was associated with an increase of HRQoL with an EQ-5D score of 0.03 or 3 mm on the EQ-VAS per HADS point. Apart from depression, improvement of both the physical and mental aspects of SF-36 was the same (improvement of work ability (WAI) and neck disability (NDI)). Improvement of work ability was also associated with improvement of EQ-VAS, but it was not associated with the EQ-5D index, which instead was associated with educational level, pain and pain catastrophizing.
Discussion
The results indicate that NSE/NSEB may improve HRQoL compared to PPA in chronic WAD grade 2 or 3, especially when combined with a behavioural approach. There was no difference between groups regarding the EQ-5D score, although the NSEB group improved over time. This was also the case with EQ-VAS, but there was also a group difference favouring the NSE/NSEB groups compared to PPA. Regarding the SF-36 PCS, both the NSE and NSEB groups improved over time. There was also a group difference favouring these two groups over PPA, which was also the case for the SF-36 MCS at 3 months, but the MCS improvement over time was insignificant. Although there were no differences between the NSE/NSEB groups, there was a tendency towards larger improvements with the addition of a behavioural approach to the NSE, which—given the overlap between psychosocial and physical symptoms—could be expected. There were no improvements in HRQoL in the PPA group.
None of the group means reached the norm HRQoL levels of the general public. However, the improvements of the SF-36 PCS in the NSE/NSEB groups (3.47/3.2) were above the suggested minimal clinical important difference (MCID) (2.7) after non-surgical treatment in chronic neck pain [46]. This suggests that the improvements were nonetheless clinically relevant. Regarding EQ-5D we have not been able to find a suggested level of MCID in chronic neck pain following non-surgical interventions. In chronic pain including rheumatoid arthritis, post-herpetic neuralgia, lumbago, etc., the overall MCID of EQ-5D is suggested to be 0.1 following introduction of pain medication [47]. Since the MCID depends on the kind of disease/pain condition and of the intervention in question, this level may not be true in chronic WAD.
NSE/NSEB seem to significantly reduce a number of neck-related problems in longstanding WAD grades 2 and 3 [22, 48–51], but the perception of health is complex. For a person with chronic WAD, not only neck symptoms but also many other factors are associated with HRQoL, as shown in Table 3, and Supplement 1. More than two-thirds of the participants in this study reported comorbidity, which was correlated with HRQoL just like most measurements in the univariate analyses. However, the results of the multivariate analyses indicate that when considering the influence of all other factors, the only factor associated with all four baseline outcomes was depression. The significance of depression is in line with previous literature [11, 12]. Work ability and pain disability were also associated with three out of four HRQoL baseline outcomes.
Baseline factors may predict an outcome, but they do not explain whether these factors may also mediate the outcome. To our knowledge, factors associated with change in HRQoL (i.e. factors that can explain the improvement) following exercise interventions in chronic WAD grades 2 and 3 have not been presented before. As seen in Table 3, the factors associated with HRQoL and change of HRQoL are not identical. For instance, age only explained part of the variance in the baseline PCS score, whereas it did not seem to play a role in the improvement of health. On the other hand, factors like depression and work ability were associated with both HRQoL and change of HRQoL. Reducing the level of depression thus seems to be an important factor to consider. Exercise is reported to be more effective at reducing depression in people classified as depressed than those within the normal range [52]. Even though the mean baseline level of depression in this sample indicated no depression (Table 1), 67 participants reported at least borderline scores (HADS depression > 7). When separating the physical aspect from the mental aspect of HRQoL, improvement of depression was only associated with improvement of the mental aspect. Improvements of both work ability and neck disability were however associated with improvements of both the physical and mental aspects according to the SF-36. Factors associated with improvements of the EQ-5D score were partly different, where educational level, improvements of both pain and pain catastrophizing seem to play a larger role than work ability and neck disability. The NSE and/or the NSEB groups have gained larger improvements in pain catastrophizing [48], neck disability, pain [22] and work ability [53] than the PPA group as previously presented in this sample, which may be part of the explanation of the better results of the NSE/NSEB groups also regarding HRQoL. Taking the multidimensional nature of health into account, the R2values, explaining the variance of the outcome, were relatively high. It should be noted that no single factor alone can explain the whole variance. The R2 values are based on a combination of several factors associated with HRQoL, as seen in Table 3, and relate to the included variables only. Other factors, not included in this analysis may also play an important role.
Generic measurements, like the EQ-5D, are not only used to report HRQoL, but are also used in cost-effectiveness analyses. Generic measurements are however generally less responsive than disease-specific measurements [54]. Although improvements were seen in the NSE/NSEB groups in this study and NSE seems to be cost-effective compared to NSEB and PPA in chronic WAD [30], caution is warranted when comparing with other groups of patients. Both the SF-36 and EQ-5D have a greater focus on lower body function than on upper body function, which may reduce the sensitivity in WAD populations and have an impact when comparing different health states. Furthermore, the EQ-5D score, with its fewer items, is less sensitive than the SF-36 [55], but the EQ-VAS also offers an option to consider other aspects not covered by the questions.
Limitations
Since this is a secondary analysis, the sample-size calculation was not based on HRQoL, and there may thus have been insufficient power to detect more differences. There was a small, but significant, baseline difference between groups regarding age and gender; however, they were not correlated with the change scores. Furthermore, they were controlled for in the analysis.
Another limitation is that even though the physiotherapists were experienced and selected to match their interest and competence as far as possible, the one-day training may not have been enough to fully master the interventions. Nonetheless, an important psychological factor, pain catastrophizing, was, as previously presented, improved by up to a mean of 37% following NSE alone and 30% following NSEB [48].
Finally, participants in the PPA group only had 1–2 physiotherapist visits, whereas the other two groups had regular physiotherapist contact which may have influenced the results. However, expectations of the three interventions were similar at baseline and there was no difference between groups regarding fulfilment of expectations [22].
Conclusions
Neck-specific exercise, particularly with a behavioural approach, may have a more positive impact on HRQoL than physical activity prescription in chronic WAD grades 2 and 3. HRQoL is however complex, and other factors also need to be considered. The factors associated with HRQoL and improvements in HRQoL (R2 = 0.38–0.50) following exercise were multidimensional.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank all of the participants in this study, including WAD participants, physiotherapists and staff involved at any stage of the study. This work was supported by funding from Vetenskapsrådet (Grant No. 521-2014-2982), the Swedish Government through the REHSAM Foundation (Grant No. RS2010/009), the Swedish Research Council, the Regional Centre for Clinical Research and the County Council of Östergötland (Grant Nos. LIO-533041, LIO-439541, LIO-197631, IO-276151, LIO-354241 and LIO-439541), the Centre for Clinical Research Sörmland at Uppsala University (Grant Nos. DLL-553281, DLL-465071, DLL-221851, DLL-112241 and DLL-376711), the Medical Research Council of Southeast Sweden (Grant Nos. FORSS-472691, FORSS-302601, FORSS-384421) and the Uppsala-Örebro Regional Research Council (Grant Nos. RFR-384651, RFR-150591, RFR-297301 and RFR-215571).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study, conducted in accordance with the Declaration of Helsinki, was approved by the Regional Ethics Committee of Linköping University, Sweden.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holm LW, Carroll LJ, Cassidy JD, Hogg-Johnson S, Cote P, Guzman J, et al. The burden and determinants of neck pain in whiplash-associated disorders after traffic collisions: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and its Associated Disorders. Spine (Phila Pa 1976) 2008;33(4 Suppl):S52–S59. doi: 10.1097/BRS.0b013e3181643ece. [DOI] [PubMed] [Google Scholar]
- 3.Galasko G, Murray P, Stephenson W. Incidence of whiplash-associated disorder. BCMJ. 2002;44:237–240. [Google Scholar]
- 4.Lamb SE, Gates S, Williams MA, Williamson EM, Mt-Isa S, Withers EJ, et al. Emergency department treatments and physiotherapy for acute whiplash: A pragmatic, two-step, randomised controlled trial. Lancet. 2013;381(9866):546–556. doi: 10.1016/S0140-6736(12)61304-X. [DOI] [PubMed] [Google Scholar]
- 5.Carroll LJ, Holm LW, Hogg-Johnson S, Cote P, Cassidy JD, Haldeman S, et al. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008;33(4 Suppl):S83–S92. doi: 10.1097/BRS.0b013e3181643eb8. [DOI] [PubMed] [Google Scholar]
- 6.Walton DM, Macdermid JC, Giorgianni AA, Mascarenhas JC, West SC, Zammit CA. Risk factors for persistent problems following acute whiplash injury: Update of a systematic review and meta-analysis. Journal of Orthopaedic & Sports Physical Therapy. 2013;43:31–43. doi: 10.2519/jospt.2013.4507. [DOI] [PubMed] [Google Scholar]
- 7.Norris SH, Watt I. The prognosis of neck injuries resulting from rear-end vehicle collisions. The Journal of Bone and Joint Surgery. 1983;65(5):608–611. doi: 10.1302/0301-620X.65B5.6643566. [DOI] [PubMed] [Google Scholar]
- 8.Ris I, Juul-Kristensen B, Boyle E, Kongsted A, Manniche C, Sogaard K. Chronic neck pain patients with traumatic or non-traumatic onset: Differences in characteristics. A cross-sectional study. Scandinavian Journal of Pain. 2017;14:1–8. doi: 10.1016/j.sjpain.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Guez M. Chronic neck pain. An epidemiological, psychological and SPECT study with emphasis on whiplash-associated disorders. Acta Orthopaedica. 2006;77(320):preceding. [PubMed] [Google Scholar]
- 10.Pink J, Petrou S, Williamson E, Williams M, Lamb SE. Economic and health-related quality of life outcomes of whiplash associated disorders. Spine (Phila Pa 1976) 2016;41(17):1378–1386. doi: 10.1097/BRS.0000000000001512. [DOI] [PubMed] [Google Scholar]
- 11.Borsbo B, Peolsson M, Gerdle B. Catastrophizing, depression, and pain: Correlation with and influence on quality of life and health—a study of chronic whiplash-associated disorders. Journal of Rehabilitation Medicine. 2008;40(7):562–569. doi: 10.2340/16501977-0207. [DOI] [PubMed] [Google Scholar]
- 12.Peolsson M, Gerdle B. Coping in patients with chronic whiplash-associated disorders: A descriptive study. Journal of Rehabilitation Medicine. 2004;36(1):28–35. doi: 10.1080/11026480310015530. [DOI] [PubMed] [Google Scholar]
- 13.Sullivan M, Karlsson J. The Swedish SF-36 Health Survey III. Evaluation of criterion-based validity: Results from normative population. Journal of Clinical Epidemiology. 1998;51(11):1105–1113. doi: 10.1016/S0895-4356(98)00102-4. [DOI] [PubMed] [Google Scholar]
- 14.Saarni SI, Harkanen T, Sintonen H, Suvisaari J, Koskinen S, Aromaa A, et al. The impact of 29 chronic conditions on health-related quality of life: A general population survey in Finland using 15D and EQ-5D. Quality of life Research. 2006;15(8):1403–1414. doi: 10.1007/s11136-006-0020-1. [DOI] [PubMed] [Google Scholar]
- 15.The World Health Organisation, W. Constitution of the World Health Organization: Principles 1947. Retrieved April 2, 2018, from http://www.who.int/about/mission/en/.
- 16.Nijs J, Van Oosterwijck J, De Hertogh W. Rehabilitation of chronic whiplash: Treatment of cervical dysfunctions or chronic pain syndrome? Clinical Rheumatology. 2009;28(3):243–251. doi: 10.1007/s10067-008-1083-x. [DOI] [PubMed] [Google Scholar]
- 17.Jull G, Kristjansson E, Dall’Alba P. Impairment in the cervical flexors: A comparison of whiplash and insidious onset neck pain patients. Manual Therapy. 2004;9(2):89–94. doi: 10.1016/S1356-689X(03)00086-9. [DOI] [PubMed] [Google Scholar]
- 18.Peterson G, Nilsson D, Trygg J, Falla D, Dedering A, Wallman T, et al. Novel insights into the interplay between ventral neck muscles in individuals with whiplash-associated disorders. Scientific Reports. 2015;5:15289. doi: 10.1038/srep15289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peterson G, Nilsson D, Peterson S, Dedering A, Trygg J, Wallman T, et al. Changes in dorsal neck muscle function in individuals with chronic whiplash-associated disorders: A real-time ultrasound case-control study. Ultrasound in Medicine and Biology. 2016;45:1090–1102. doi: 10.1016/j.ultrasmedbio.2015.12.022. [DOI] [PubMed] [Google Scholar]
- 20.Elliott JM, Pedler AR, Jull GA, Van Wyk L, Galloway GG, O’Leary SP. Differential changes in muscle composition exist in traumatic and nontraumatic neck pain. Spine (Phila Pa 1976) 2014;39(1):39–47. doi: 10.1097/BRS.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 21.Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: The evidence. CMAJ. 2006;174(6):801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ludvigsson ML, Peterson G, O’Leary S, Dedering A, Peolsson A. The effect of neck-specific exercise with, or without a behavioral approach, on pain, disability, and self-efficacy in chronic whiplash-associated disorders: A randomized clinical trial. The Clinical Journal of Pain. 2015;31(4):294–303. doi: 10.1097/AJP.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: Redefining “whiplash” and its management. Spine (Phila Pa 1976) 1995;20(8 Suppl):1S–73S. [PubMed] [Google Scholar]
- 24.Landen Ludvigsson M, Peterson G, Dedering A, Peolsson A. One- and two-year follow-up of a randomized trial of neck-specific exercise with or without a behavioural approach compared with prescription of physical activity in chronic whiplash disorder. Journal of Rehabilitation Medicine. 2016;48:56–64. doi: 10.2340/16501977-2041. [DOI] [PubMed] [Google Scholar]
- 25.Vernon H. The Neck Disability Index: State-of-the-art, 1991–2008. Journal of Manipulative and Physiological Therapeutics. 2008;31(7):491–502. doi: 10.1016/j.jmpt.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 26.Tuomi KIJ, Jahkola A, Katajarinne L, Tulkki A. Work Ability Index. 2. Finland: Helsinki; 1988. [Google Scholar]
- 27.Landén Ludvigsson, M., Pelosson, A., & Peterson, G. (2015). Retrieved April 25, 2018, fromhttp://urn.kb.se/resolve?urn=urn:nbn:se:liu:diva-113865.
- 28.Pool JJ, Ostelo RW, Knol DL, Vlaeyen JW, Bouter LM, de Vet HC. Is a behavioral graded activity program more effective than manual therapy in patients with subacute neck pain? Results of a randomized clinical trial. Spine (Phila Pa 1976) 2010;35(10):1017–1024. doi: 10.1097/BRS.0b013e3181c212ee. [DOI] [PubMed] [Google Scholar]
- 29.Professional Associations for Physical Activity, YFA. Physical activity in the prevention and treatment of disease. Stockholm: Swedish National Institute of Public Health; 2010. Retrieved May 3, 2018, from http://www.fyss.se/far-fysisk-aktivitet-pa-recept/.
- 30.Landen Ludvigsson M, Peolsson A, Peterson G, Dedering A, Johansson G, Bernfort L. Cost-effectiveness of neck-specific exercise with or without a behavioral approach versus physical activity prescription in the treatment of chronic whiplash-associated disorders: Analyses of a randomized clinical trial. Medicine (Baltimore) 2017;96(25):e7274. doi: 10.1097/MD.0000000000007274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whitehurst DG, Bryan S. Another study showing that two preference-based measures of health-related quality of life (EQ-5D and SF-6D) are not interchangeable. But why should we expect them to be? Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research. 2011;14(4):531–538. doi: 10.1016/j.jval.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 32.National Institute for Health and Care Excellence, NICE. Measuring effectiveness and cost effectiveness: The QALY 2015. Retrieved May 21, 2018, from https://www.nice.org.uk/proxy/?sourceurl=http://www.nice.org.uk/newsroom/features/measuringeffectivenessandcosteffectivenesstheqaly.jsp.
- 33.EuroQol G. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 34.Brooks R. EuroQol: The current state of play. Health Policy. 1996;37(1):53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 35.Janssen MF, Szende A, Cabases J, Ramos-Goni JM, Vilagut G, Konig HH. Population norms for the EQ-5D-3L: A cross-country analysis of population surveys for 20 countries. The European Journal of Health Economics. 2018 doi: 10.1007/s10198-018-0955-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sullivan M, Karlsson J, Ware JE., Jr. The Swedish SF-36 Health Survey–I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Social Science & Medicine. 1995;41(10):1349–1358. doi: 10.1016/0277-9536(95)00125-Q. [DOI] [PubMed] [Google Scholar]
- 37.Ware JE. Jr. SF-36 health survey update. Spine (Phila Pa 1976) 2000;25(24):3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 38.Ware JE, Jr., Gandek B, Kosinski M, Aaronson NK, Apolone G, Brazier J, et al. The equivalence of SF-36 summary health scores estimated using standard and country-specific algorithms in 10 countries: Results from the IQOLA Project. International Quality of Life Assessment. Journal of Clinical Epidemiology. 1998;51(11):1167–1170. doi: 10.1016/S0895-4356(98)00108-5. [DOI] [PubMed] [Google Scholar]
- 39.Bess S, Line B, Fu KM, McCarthy I, Lafage V, Schwab F, et al. The health impact of symptomatic adult spinal deformity: Comparison of deformity types to United States population norms and chronic diseases. Spine (Phila Pa 1976) 2016;41(3):224–233. doi: 10.1097/BRS.0000000000001202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lisspers J, Nygren A, Soderman E. Hospital Anxiety and Depression Scale (HAD): Some psychometric data for a Swedish sample. Acta Psychiatrica Scandinavica. 1997;96(4):281–286. doi: 10.1111/j.1600-0447.1997.tb10164.x. [DOI] [PubMed] [Google Scholar]
- 41.Roelofs J, Sluiter JK, Frings-Dresen MH, Goossens M, Thibault P, Boersma K, et al. Fear of movement and (re)injury in chronic musculoskeletal pain: Evidence for an invariant two-factor model of the Tampa Scale for Kinesiophobia across pain diagnoses and Dutch, Swedish, and Canadian samples. Pain. 2007;131(1–2):181–190. doi: 10.1016/j.pain.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 42.Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittmann L. The Pain Catastrophizing Scale: Further psychometric evaluation with adult samples. Journal of Behavioral Medicine. 2000;23(4):351–365. doi: 10.1023/A:1005548801037. [DOI] [PubMed] [Google Scholar]
- 43.Altmaier EM, Russell DW, Kao CF, Lehmann TR, Weinstein JN. Role of self-efficacy in rehabilitation outcome among chronic low back pain patients. Journal of Counseling Psychology. 1993;40(3):335–339. doi: 10.1037/0022-0167.40.3.335. [DOI] [Google Scholar]
- 44.Tait RC, Chibnall JT, Krause S. The Pain Disability Index: Psychometric properties. Pain. 1990;40(2):171–182. doi: 10.1016/0304-3959(90)90068-O. [DOI] [PubMed] [Google Scholar]
- 45.Dolan, P. G. C., Kind, P., & Williams, A. (1995). A social tariff for the EuroQol: Results from a UK general population survey. Centre for Health Economics Discussion Paper, University of York, UK. Vol. 138, pp. 1–24.
- 46.Lauche RLJ, Dobos GJ, Cramer H. Clinically meaningful differences in pain, disability and quality of life for chronic nonspecific neck pain—a reanalysis of 4 randomized controlled trials of cupping therapy. Complement Ther Med. 2013;21(4):342–347. doi: 10.1016/j.ctim.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 47.Yoshizawa K, Kobayashi H, Fujie M, Ogawa Y, Yajima T, Kawai K. Estimation of minimal clinically important change of the Japanese version of EQ-5D in patients with chronic noncancer pain: A retrospective research using real-world data. Health and Quality of Life Outcomes. 2016;14:35. doi: 10.1186/s12955-016-0438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Overmeer T, Peterson G, Landen Ludvigsson M, Peolsson A. The effect of neck-specific exercise with or without a behavioral approach on psychological factors in chronic whiplash-associated disorders: A randomized controlled trial with a 2-year follow-up. Medicine (Baltimore) 2016;95(34):e4430. doi: 10.1097/MD.0000000000004430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ardern CL, Peterson G, Ludvigsson ML, Peolsson A. Satisfaction with the outcome of physical therapist-prescribed exercise in chronic whiplash-associated disorders: Secondary analysis of a randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy. 2016;46(8):640–649. doi: 10.2519/jospt.2016.6136. [DOI] [PubMed] [Google Scholar]
- 50.Peterson GE, Landen Ludvigsson MH, O’Leary SP, Dedering AM, Wallman T, Jonsson MI, et al. The effect of 3 different exercise approaches on neck muscle endurance, kinesiophobia, exercise compliance, and patient satisfaction in chronic whiplash. Journal of Manipulative and Physiological Therapeutics. 2015;38(7):465–476. doi: 10.1016/j.jmpt.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 51.Treleaven J, Peterson G, Ludvigsson ML, Kammerlind AS, Peolsson A. Balance, dizziness and proprioception in patients with chronic whiplash associated disorders complaining of dizziness: A prospective randomized study comparing three exercise programs. Manual Therapy. 2016;22:122–130. doi: 10.1016/j.math.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 52.Wegner M, Helmich I, Machado S, Nardi AE, Arias-Carrion O, Budde H. Effects of exercise on anxiety and depression disorders: Review of meta- analyses and neurobiological mechanisms. CNS & Neurological Disorders-Drug Targets. 2014;13(6):1002–1014. doi: 10.2174/1871527313666140612102841. [DOI] [PubMed] [Google Scholar]
- 53.Kwan Lo H, Johnston V, Landén Ludvigsson M, Peterson G, Overmeer T, David D, Peolsson A. Factors associated with work ability following exercise interventions for individuals with chronic whiplash associated disorders: A secondary analysis of a randomized controlled trial. Journal of Rehabilitation Medicine. 2018 doi: 10.2340/16501977-2374. [DOI] [PubMed] [Google Scholar]
- 54.Wiebe S, Guyatt G, Weaver B, Matijevic S, Sidwell C. Comparative responsiveness of generic and specific quality-of-life instruments. Journal of Clinical Epidemiology. 2003;56(1):52–60. doi: 10.1016/S0895-4356(02)00537-1. [DOI] [PubMed] [Google Scholar]
- 55.Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Economics. 2004;13(9):873–884. doi: 10.1002/hec.866. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


