Abstract
Association between pre-ablation levels of biomarkers of cardiac and endothelial dysfunctions, CHADS2, CHA2DS2-VASc, and APPLE scores and the recurrence of atrial fibrillation (AF) after radiofrequency catheter ablation has not been fully studied. A total of 254 patients with nonvalvular AF were prospectively followed for AF recurrence after a single ablation procedure. During a two-year follow-up period, AF recurred in 65 (25.6%) patients. Patients with AF recurrence had significantly greater baseline ln brain natriuretic peptide (BNP) than those without AF recurrence (P < 0.01), whereas there were no significant differences in the levels of biomarkers of endothelial dysfunction and points of scoring systems. In the Cox regression analyses, the baseline ln BNP was significantly independently associated with AF recurrence (adjusted HR =1.286, 95% CI =1.000–1.655, P < 0.05). The baseline levels of ln BNP were significantly associated with rhythm at blood collection, age, sex, and left atrial diameter, and left ventricular ejection fraction (P < 0.05).The subgroup analysis showed a significant interaction on the risk of AF recurrence between ln BNP, sex difference, and rhythm at blood collection (P for interaction < 0.05). In conclusion, the results suggest that the pre-ablation levels of ln BNP are useful to evaluate the risk of AF recurrence after ablation therapy; however, there is a need to be careful while using BNP as a biomarker for the risk of AF recurrence by taking account of the effects of rhythm status at blood collection and sex difference.
Keywords: Atrial fibrillation, Catheter ablation, Recurrence, Biomarkers, Brain natriuretic peptide
Introduction
Atrial fibrillation (AF), one of the commonest arrhythmias [1], is associated with an increased morbidity and mortality [2,3]. Haïssaguerre et al. have reported that the pulmonary veins are the dominant sources of triggers for initiating AF in most patients [4]. Catheter ablation of AF with isolation of the pulmonary veins, which has become the standard therapy for symptomatic patients with AF that is refractory to medical therapy [5], is highly effective at curing paroxysmal or persistent AF [6]. However, AF recurs after ablation therapy in some patients and the risk of such recurrence has been difficult to predict [7].
Inflammatory, oxidative stress [8–10] and atrial remodeling [11,12] have been reported as the etiology of AF development. In addition, it has been reported that multiple risk scores and biomarkers considering these etiologies may be predictors of recurrence after atrial fibrillation ablation treatment. The CHADS2 and CHA2DS2-VASc scores, both of which comprise common cardiovascular risk factors, has been originally developed for predicting stroke and thromboembolism [13]. These scores have been reported to be associated with AF recurrence in patients with paroxysmal AF after a single ablation procedure [14], and with long-term outcomes in patients with paroxysmal AF and persistent AF after AF ablation [15]. However, studies on the predictive value of the CHADS2 and CHA2DS2-VASc scores on the recurrence of AF after ablation had inconsistent results [16]. Then, the APPLE score has been developed to predict AF recurrence after an ablation procedure in patients with paroxysmal and persistent AF. This score comprises five clinical variables such as age, type of AF, renal function, and echocardiographic variables [17]. The APPLE had better prediction of AF recurrence between 3 and 12 months after catheter ablation than CHADS2 and CHA2DS2-VASc scores [17]. Of biomarkers, brain natriuretic peptide (BNP), an intensively studied biomarker of cardiac dysfunction, has been reported being a predictor of the recurrence of AF [18,19]. Biomarkers of endothelial dysfunction caused by inflammatory, oxidative stress, such as inflammation-related leukocyte adhesion molecules (vascular cell adhesion molecule-1 [VCAM1]; intercellular adhesion molecule-1 [ICAM1]; and endothelial cell-leukocyte adhesion molecules-1 [ELAM1]), a physiological endothelial anticoagulant (thrombomodulin [TM]), and a platelet adhesion molecule (von Willebrand factor [VWF]) have been reported to be associated with risk of incident AF [20–24]. However, there were significant heterogeneities between studies to test associations between BNP and the recurrence of AF in meta-analysis studies, and such heterogeneities have not been fully explained [18,19]. Moreover, associations between biomarkers of endothelial dysfunction and the recurrence of AF have not been fully studied. Furthermore, associations of the risk scores, biomarkers and atrial remodeling with the recurrence of AF have not been deeply and systematically studied.
In this study, we measured pre-ablation levels of biomarkers of cardiac and endothelial dysfunction, and evaluated scores of CHADS2 and CHA2DS2-VASc, and APPLE scoring systems in patients with nonvalvular paroxysmal or persistent AF. We then examined associations between these pre-ablation variables and the recurrence of AF after radiofrequency catheter ablation. Moreover, a variable significantly and independently associated with the recurrence of AF was tested for associations with a number of key risk variables such as age, sex, type of AF, history of heart failure, history of hypertension, history of diabetes mellitus, history of stroke or transient ischemic attack, history of coronary or peripheral vascular disease, renal function, LAD, and LVEF [25]. Finally, we performed subgroup analyses and tested interactions for a baseline variable significantly associated with the recurrence of AF.
Methods
Study cohort and design
Consecutive patients with nonvalvular paroxysmal or persistent AF who underwent a single catheter ablation from March 2013 to December 2015 in Tottori University Hospital, Japan were enrolled and followed prospectively for the recurrence of AF after ablation. Paroxysmal AF was defined as self-terminating AF lasting for up to 7 days or AF episodes cardioverted within 7 days, and persistent AF as AF lasting between 7 days and 1 year or AF episodes terminated by cardioversion either with drugs or by direct current cardioversion after 7 days or more [5]. Levels of estimated glomerular filtration rate (eGFR) were calculated with the following equation established by the Japanese Society of Nephrology: eGFR (mL/min/1.73 m2) = 194 × serum creatinine level−1.094 × age−0.287 (× 0.739 if female).[3] The CHADS2 score comprised congestive heart failure, hypertension, age ≥ 75, diabetes mellitus, and stroke/transient ischemic attack and the CHA2DS2-VASc score comprised congestive heart failure, hypertension, age ≥ 75 years, diabetes mellitus, stroke/transient ischemic attack, vascular disease, age 65–74 years, and female sex [13]. The APPLE score comprised age > 65 years, persistent AF, reduced eGFR < 60 ml/min/1.73 m2, left atrial diameter (LAD) ≥ 43 mm, and left ventricular ejection fraction (LVEF) < 50%. The APPLE had better prediction of AF recurrence between 3 and 12 months after catheter ablation than CHADS2 and CHA2DS2-VASc scores [17]. Patients with one or more of the following were excluded from candidates for ablation of AF in this study: age less than 20 years or over 85 years; cerebral or myocardial infarction within 6 months of onset; uncontrolled heart failure or left ventricular ejection fraction < 40%; severe chronic obstructive pulmonary disease; contraindications to anticoagulants; thrombus formation within the left atrial appendage; LAD > 60 mm; moderate or severe valvular insufficiency or stenosis; connective tissue disease; and active cancer. It was also planned to exclude patients with hypertrophic/dilated cardiomyopathy or old myocardial infarction, end-stage renal disease or on hemodialysis: five patients with hypertrophic cardiomyopathy and six with end-stage renal disease or on hemodialysis were thus excluded. This study was approved by the Ethics Committee of Faculty of Medicine, Tottori University, and conducted in compliance with the ethical principles of the Declaration of Helsinki. Written informed consent was obtained from all individual participants included in the study.
Catheter ablation protocol
The protocol for catheter ablation of AF has been reported previously [11]. Briefly, prior to the ablation procedure, all patients received effective oral anticoagulation therapy for at least four weeks and underwent transesophageal echocardiography and enhanced cardiac computed tomography for 3D mapping. Antiarrhythmic drugs were discontinued for more than five times their half-lives. Oral anticoagulants were discontinued before the procedure: direct oral anticoagulants for one day and warfarin for five days, and replaced with unfractionated heparin until 6 h prior to the ablation procedure. Bipolar electrograms were continuously recorded on a digital recording system (Labsystem PRO; Bard Electrophysiology, Lowell, MA, USA). A 20-pole three-sited mapping catheter (BeeAT; Japan Lifeline, Tokyo, Japan) was used to record bipolar electrograms of the superior vena cava, right atrium, and coronary sinus. After transseptal puncture, heparin was continuously infused to maintain an activated clotting time of 300–400 s. Two decapolar circular mapping catheters (Lasso; Biosense Webster, Diamond Bar, CA, USA) were located in the pulmonary veins. A 3.5 mm irrigated-tip ablation catheter (Thermocool; Biosense Webster) was advanced into the LA to achieve bilateral circumferential pulmonary vein isolation with the endpoint of bidirectional conduction block between the LA and pulmonary vein. A point-by-point radiofrequency current was delivered for 30 s with a power of up to 40 watts and a target temperature less than 43°C using a 3D mapping system (CARTO3; Biosense Webster), whereas the power was limited to 20 watts at the site close to the esophagus. After achieving pulmonary vein isolation, a bidirectional conduction blocking line was created at the cavotricuspid isthmus in all patients. The ablation procedure was performed under conscious sedation with continuous monitoring of blood pressure and oxygen saturation.
Blood sample collection and processing
Blood was sampled from the femoral vein (FV) with an 18 gauge needle prior to the ablation procedure on the day of ablation therapy, placed immediately on ice and centrifuged at 3,000g for 15 min at 4°C. The resultant serum or plasma was aliquoted to different tubes to avoid repeated freeze–thaw cycles and stored at − 80°C till use. Serum soluble ELAM1 (sELAM1; ng/mL), soluble VCAM1 (sVCAM1; ng/mL), and soluble ICAM1 (sICAM1; ng/mL) were measured by enzyme-linked immunosorbent assay (ELISA; R&D systems, Minneapolis, MN, USA); plasma VWF activity (%) by latex agglutination immunoassay (LAIA; Siemens Healthcare Diagnostics Products GmbH, Marburg, Germany); serum soluble TM (sTM; FU/mL) by ELISA (Kyowa Pharma Chemical, Takaoka, Toyama, Japan); plasma BNP (pg/mL) by chemiluminescent enzyme immunoassay (CLEIA; Fujirebio, Shinjuku, Tokyo, Japan). The within-run reproducibility was < 8% for ELISAs and CLEIA and < 20% for LAIA. All assays were performed by investigators who were blinded to all clinical information about the participants.
Clinical outcomes and follow-up
The primary clinical outcome was recurrent AF lasting over 30 s off antiarrhythmic drugs. Episodes during the blanking period of the first 90 days after the ablation procedure were not considered as recurrences [5]. All patients underwent continuous ECG monitoring for 3 days following the procedure until discharge. Follow-up checks were performed 1, 2, 3, 6, 9, 12, 16, 20, and 24 months after the ablation procedure and comprised physical examination, 12-lead electrocardiogram, and 24-h Holter monitoring. Patients were instructed to self-monitor their pulses daily and report any irregularity of pulse immediately, at which point event monitoring or 14-day Holter monitoring was performed. Oral anticoagulant therapy was continued in all patients with CHA2DS2-VASc scores of two or more points after the procedure, but discontinued at 6 months in those whose scores were less than 2 points.
Statistical analysis
Categorical data are presented as frequency (percentage [%]) and were compared with Fisher’s exact test. Continuous data are presented as mean (standard deviation [SD]) or as median (interquartile range) for skewed distributions. Normality was tested with the Kolmogorov–Smirnov test. Normally distributed continuous variables were compared using the independent Student’s t test and skewed data using the non-parametric Mann–Whitney U test. Analyses were performed after natural logarithmic transformation (ln) of skewed biomarkers. Freedom from AF was reported as crude event rates and by means of a time-to-event analysis using the Kaplan–Meier method. Variables with P value < 0.10 in the group comparison were further evaluated by the Cox proportional hazards regression analyses to determine their associations with the recurrence of AF. The variables with P value < 0.10 in the univariate Cox proportional hazards regression analysis were further evaluated by the multivariate Cox proportional hazards regression analysis. Multiple regression analysis via the forced entry procedure was performed to test correlations of a normally distributed continuous variable with other variables. Statistical analyses were performed using R software (version 3.4.0; R Foundation for Statistical Computing, Vienna, Austria), and P value < 0.05 was considered to denote statistical significance.
Results
Patient characteristics in patients with and without the recurrence of AF
In total, 254 patients with AF (mean age of 65.5 [SD =9.3]; 68.9% paroxysmal and 31.1% persistent; all first session) were included in this study (Table 1). All ablation procedures were successful. The median length of follow-up for censored cases was 730 days. AF recurred in 65 (25.6%) patients during follow-up. Ln BNP was significantly greater in patients with the recurrence of AF than those without the recurrence of AF (P = 0.006) and was an only variable which significantly differed between the groups (Table 1). Although statistically not significant, uses of β-blocker and loop diuretics were more frequent and ln sTM were lower in patients with the recurrence of AF than those without the recurrence of AF (P value < 0.10, Table 1).
Table 1.
Baseline characteristics of the study patients
| Variable | All patients (n = 254) | Non-recurrence (n = 189) | Recurrence (n = 65) | P value |
|---|---|---|---|---|
| Age, years | 65.5 (9.3) | 66.0 (9.2) | 64.0 (9.4) | 0.141 |
| Type of AF | 0.438 | |||
| Paroxysmal AF, n (%) | 175 (68.9) | 133 (70.4) | 42 (64.6) | |
| Persistent AF, n (%) | 79 (31.1) | 56 (29.6) | 23 (35.4) | |
| Sex, male, n (%) | 184 (72.4) | 139 (73.5) | 45 (69.2) | 0.522 |
| BMI, kg/m2 | 23.6 (3.0) | 23.5 (3.0) | 24.0 (3.2) | 0.207 |
| Mean blood pressure, mmHg | 92.9 (13.0) | 92.9 (12.5) | 93.0 (14.4) | 0.948 |
| Rhythm at blood sampling | 0.106 | |||
| SR, n (%) | 152 (59.8) | 119 (63.0) | 33 (50.8) | |
| AF, n (%) | 102 (40.2) | 70 (37.0) | 32 (49.2) | |
| Current smoker, n (%) | 21 (8.3) | 16 (8.5) | 5 (7.7) | 1.000 |
| CHADS2 score | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 0.170 |
| CHA2DS2-VASc score | 2.0 (1.0–3.0) | 2.0 (1.0–3.0) | 2.0 (1.0–3.0) | 0.271 |
| APPLE score | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 2.0 (1.0–3.0) | 0.481 |
| History of HF, n (%) | 34 (13.4) | 22 (11.6) | 12 (18.5) | 0.204 |
| History of HT, n (%) | 144 (56.7) | 110 (58.2) | 34 (52.3) | 0.469 |
| History of DM, n (%) | 32 (12.6) | 27 (14.3) | 5 (7.7) | 0.198 |
| History of stroke/TIA, n (%) | 23 (9.1) | 19 (10.1) | 4 (6.2) | 0.456 |
| History of vascular disease, n (%) | 13 (5.1) | 10 (5.3) | 3 (4.6) | 1.000 |
| eGFR, mL/min/1.73 m2 | 80.4 (21.7) | 80.4 (20.9) | 80.3 (24.1) | 0.986 |
| LAD, mm | 39.9 (6.8) | 39.7 (6.5) | 40.6 (7.7) | 0.357 |
| LVEF, % | 62.3 (9.1) | 62.4 (9.3) | 62.0 (8.8) | 0.730 |
| Medications | ||||
| Type of anticoagulants | 0.273 | |||
| VKA, n (%) | 48 (18.9) | 39 (20.6) | 9 (13.8) | |
| DOAC, n (%) | 206 (81.1) | 150 (79.4) | 56 (86.2) | |
| Acetylsalicylic acid, n (%) | 16 (6.3) | 12 (6.3) | 4 (6.2) | 1.000 |
| ACEI/ARB, n (%) | 104 (40.9) | 80 (42.3) | 24 (36.9) | 0.468 |
| β-blocker, n (%) | 84 (33.1) | 56 (29.6) | 28 (43.1) | 0.066 |
| CCB, n (%) | 83 (32.7) | 64 (33.9) | 19 (29.2) | 0.542 |
| Digitalis, n (%) | 12 (4.7) | 9 (4.8) | 3 (4.6) | 1.000 |
| Loop diuretics, n (%) | 35 (13.8) | 22 (11.6) | 13 (20.0) | 0.099 |
| Aldosterone antagonist, n (%) | 14 (5.5) | 9 (4.8) | 5 (7.7) | 0.358 |
| Statin, n (%) | 53 (20.9) | 40 (21.2) | 13 (20.0) | 1.000 |
| NCB, n (%) | 100 (39.4) | 69 (36.5) | 31 (47.7) | 0.141 |
| Bepridil, n (%) | 20 (7.9) | 13 (6.9) | 7 (10.8) | 0.299 |
| Amiodarone, n (%) | 11 (4.3) | 7 (3.7) | 4 (6.2) | 0.480 |
| ln BNP | 4.3 (1.1) | 4.2 (1.1) | 4.6 (1.0) | 0.006 |
| ln sTM | 0.95 (0.27) | 0.97 (0.28) | 0.90 (0.26) | 0.079 |
| ln sELAM1 | 3.3 (0.4) | 3.3 (0.4) | 3.3 (0.5) | 0.870 |
| ln sICAM1 | 5.1 (0.4) | 5.1 (0.4) | 5.2 (0.4) | 0.162 |
| ln sVCAM1 | 6.7 (0.3) | 6.7 (0.3) | 6.7 (0.3) | 0.363 |
| VWF activity, % | 166.3 (77.4) | 170.4 (77.2) | 154.4 (77.1) | 0.151 |
The values are presented as number (%), mean (standard deviation), or median (interquartile range)
ACE angiotensin converting enzyme, AF atrial fibrillation, ARB angiotensin receptor blocker, BMI body mass index, BNP brain natriuretic peptide, CCB calcium channel blocker, DM diabetes mellitus, DOAC direct oral anticoagulant, eGFR estimated glomerular filtration rate, HF heart failure, HT hypertension, LAD left atrial diameter, LVEF left ventricular ejection fraction, NCB natrium channel blocker, sELAM1 soluble endothelial cell-leukocyte adhesion molecules-1, sICAM1 soluble intercellular adhesion molecule-1, SR sinus rhythm; sTM = soluble thrombomodulin; sVCAM1 = soluble vascular cell adhesion molecule-1, TIA transient ischemic attack, VKA vitamin K antagonist, VWF von Willebrand factor
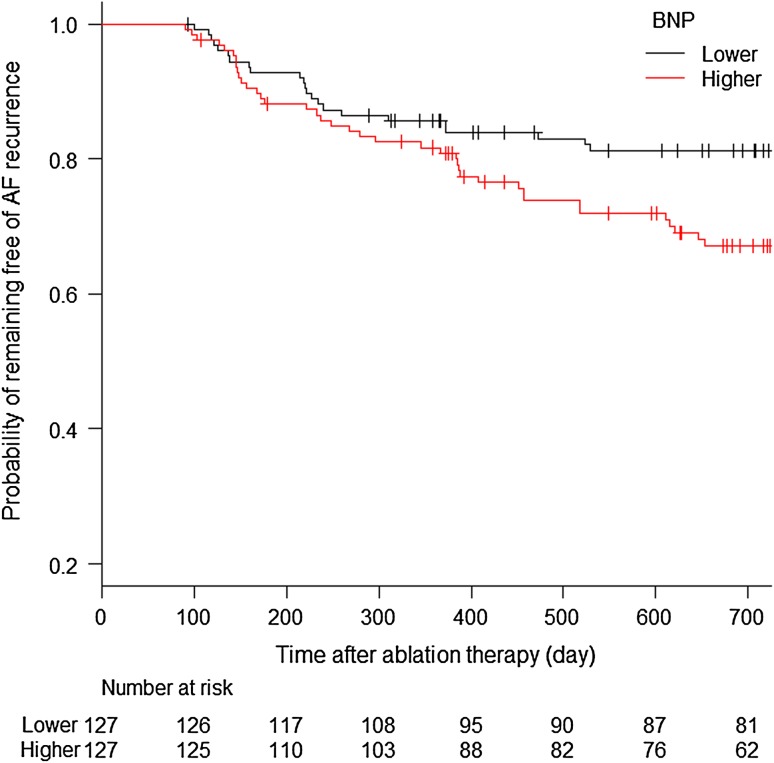
Because baseline ln BNP was significantly greater in patients with the recurrence of AF than those without the recurrence of AF, the study patients were divided into two groups by the median concentration of BNP (groups with lower and higher levels of BNP) and then a probability of remaining free of the recurrence of AF after ablation procedure with a three-month blanking period was evaluated in the two groups. As a result, patient with the lower level of BNP had a greater probability of remaining free of the recurrence of AF than those with the higher level of BNP (P value by log-rank test = 0.011) as shown in Fig. 1. Two-year recurrence–free survival rates were 0.812 (95% confidence interval [CI] = 0.730–0.871) and 0.672 (95% CI = 0.578–0.749) in patients with the lower and higher levels of BNP, respectively.
Fig. 1.
Probability of remaining free of the recurrence of AF in patients with the lower and higher levels of BNP. Patients were divided into two groups by the median concentration of BNP. Patient with lower level of BNP had a greater probability of remaining free of the recurrence of AF than those with higher level of BNP (P value by log-rank test = 0.011). Two-year recurrence-free survival rates were 0.812 (95% CI = 0.730–0.871) and 0.672 (95% CI = 0.578–0.749) in patients with the lower and higher levels of BNP, respectively. BNP brain natriuretic peptide
Associations of baseline variables with the recurrence of AF
To determine associations of baseline variables with the recurrence of AF, the univariate and multivariate Cox proportional hazards regression analyses. In the univariate Cox proportional hazards regression analyses, only ln BNP was significantly associated with the recurrence of AF (unadjusted HR = 1.353, 96% CI = 1.068–1.713, P = 0.012), whereas use of β-blocker, use of loop diuretics, and ln sTM were not significantly associated with the recurrence of AF (unadjusted HR = 1.582, 96% CI = 0.968–2.585, P = 0.067; unadjusted HR = 1.603, 96% CI = 0.873–2.945, P = 0.128; unadjusted HR = 0.447, 96% CI = 0.180–1.107, P = 0.082, respectively) as shown in Table 2. In the multivariate Cox proportional hazards regression analysis, ln BNP remained significantly associated with the recurrence of AF (adjusted HR = 1.286, 96% CI = 1.000–1.655, P = 0.049) when tested with the use of β-blocker and ln sTM, P values of which were < 0.10 in the univariate Cox regression analysis (Table 2).
Table 2.
Univariate and multivariate Cox regression analyses
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Unadjusted HR | 95% CI | P value | Adjusted HR | 95% CI | P value | |
| β-blocker (use = 1) | 1.582 | 0.968–2.585 | 0.067 | 1.345 | 0.804–2.251 | 0.258 |
| Loop diuretics (use = 1) | 1.603 | 0.873–2.945 | 0.128 | not selected | ||
| ln BNP (per 1 increase) | 1.353 | 1.068–1.713 | 0.012 | 1.2860 | 1.000–1.655 | 0.049 |
| ln sTM (per 1 increase) | 0.447 | 0.180–1.107 | 0.082 | 0.4960 | 0.207–1.190 | 0.116 |
After performing univariate Cox regression analysis, variables with P value < 0.10 were further evaluated by multivariate Cox regression analysis
BNP brain natriuretic peptide, CI confidence interval, HR hazard ratio, ln natural logarithm, sTM soluble thrombomodulin
Correlations between ln BNP and the key risk variables
Because ln BNP remained significantly and independently associated with the recurrence of AF, we performed a multiple regression analysis to test correlations between ln BNP and the key risk variables by the forced entry procedure. In a multivariate regression model controlling simultaneously for rhythm at blood collection, age, sex, type of AF, body mass index (BMI), eGFR, LAD, and LVEF, rhythm at blood collection, age, sex, LAD, and LVEF were significantly associated with the level of ln BNP (Table 3): specifically, AF at blood collection was significantly associated with the substantially increased level of ln BNP (adjusted β = 0.482, 95% CI = 0.213–0.751, P value < 0.001).
Table 3.
Linear regression analyses for ln BNP
| Variables | Single regression | Multiple regression | ||
|---|---|---|---|---|
| Unadjusted β coefficient | P value | Adjusted β coefficient | P value | |
| Rhythm at blood collection (AF = 1, SR =0) | 0.857 (0.613 to 1.101) | < 0.001 | 0.482 (0.213 to 0.751) | < 0.001 |
| Age (per year increase) | 0.036 (0.023 to 0.050) | < 0.001 | 0.027 (0.015 to 0.040) | < 0.001 |
| Sex (male = 1, female = 0) | − 0.284 (− 0.574 to 0.005) | 0.054 | − 0.438 (− 0.722 to − 0.154) | 0.003 |
| Type of AF (persistent AF = 1, paroxysmal AF = 0) | 0.877 (0.617to 1.137) | < 0.001 | 0.125 (− 0.180 to 0.430) | 0.420 |
| BMI (per kg/m2 increase) | 0.007 (− 0.036 to 0.050) | 0.752 | − 0.035 (− 0.072 to 0.001) | 0.058 |
| eGFR (per mL/min/1.73 m2 increase) | − 0.007 (− 0.013 to − 0.001) | 0.015 | − 0.004 (− 0.009 to 0.002) | 0.226 |
| LAD (per mm increase) | 0.074 (0.057 to 0.091) | < 0.001 | 0.049 (0.030 to 0.068) | <0.001 |
| LVEF (per % increase) | − 0.031 (− 0.045 to − 0.017) | < 0.001 | − 0.023 (− 0.035 to − 0.011) | <0.001 |
Abbreviations are shown as in Table 1. In a multiple regression analysis, the regression coefficient estimate (β) was adjusted for all other variables listed.
Subgroup analyses of risks of the recurrence of AF for ln BNP
We further performed subgroup analyses of risks of the recurrence of AF for ln BNP by dividing patients with the risk variables and the interaction effects of ln BNP with other risk variables, specifically with various combinations of rhythm status at blood collection and other risk variables because rhythm status at blood collection was significantly associated with substantially different levels of ln BNP (Table 3). Consequently, there was a significant interaction of ln BNP with sex and rhythm at blood collection (P for interaction = 0.011) as shown in Table 4: higher ln BNP was significantly associated with an increased risk of the recurrence of AF in a subgroup of male sex with sinus rhythm at blood collection (HR = 1.536, 95% CI = 1.095–2.154, P value = 0.013), but not in the other subgroups.
Table 4.
Subgroup analyses of hazard ratios of ln BNP for the recurrence of atrial fibrillation
| Subgroup | Recurrence, n (%) | Hazard ratio (95% CI) of ln BNP | P value | P for interaction |
|---|---|---|---|---|
| Rhythm at blood collection | 0.449 | |||
| Sinus rhythm (n = 152) | 33 (21.7%) | 1.397 (1.022–1.911) | 0.036 | |
| Atrial fibrillation (n = 102) | 32 (31.4%) | 1.153 (0.737–1.806) | 0.533 | |
| Age | 0.328 | |||
| < 65 (n = 105) | 29 (27.6%) | 1.230 (0.872–1.734) | 0.238 | |
| ≥ 65 (n = 149) | 36 (24.2%) | 1.567 (1.126–2.181) | 0.008 | |
| Sex | 0.791 | |||
| Male (n = 184) | 45 (24.5%) | 1.372 (1.036–1.818) | 0.027 | |
| Female (n = 70) | 20 (28.6%) | 1.270 (0.806–2.000) | 0.303 | |
| Type of AF | 0.666 | |||
| Paroxysmal AF (n = 175) | 42 (24.0%) | 1.415 (1.076–1.861) | 0.013 | |
| Persistent AF (n = 79) | 23 (29.1%) | 1.271 (0.710–2.275) | 0.419 | |
| BMI | 0.128 | |||
| < 25 kg/m2 (n = 172) | 40 (23.3%) | 1.204 (0.902–1.606) | 0.207 | |
| ≥ 25 kg/m2 (n = 82) | 25 (30.5%) | 1.821 (1.143–2.898) | 0.012 | |
| eGFR | 0.375 | |||
| ≥ 60 ml/min/1.78 m2 (n = 216) | 55 (25.5%) | 1.297 (0.999–1.684) | 0.051 | |
| < 60 ml/min/1.78 m2 (n = 38) | 10 (26.3%) | 1.790 (0.951–1.684) | 0.071 | |
| LAD | 0.443 | |||
| < 40 mm (n = 129) | 28 (21.7%) | 1.213 (0.855–1.721) | 0.280 | |
| ≥ 40 mm (n = 125) | 37 (29.6%) | 1.467 (1.029–2.090) | 0.034 | |
| LVEF | 0.863 | |||
| ≥ 50% (n = 227) | 58 (25.6) | 1.398 (1.086 1.800) | 0.009 | |
| < 50% (n = 27) | 7 (25.9) | 1.294 (0.431 3.880) | 0.646 | |
| Age and rhythm at blood collection | 0.583 | |||
| Age < 65 with SR (n = 61) | 16 (26.2%) | 1.228 (0.815–1.851) | 0.326 | |
| Age < 65 with AF (n = 44) | 13 (29.5%) | 1.341 (0.538–3.342) | 0.529 | |
| Age ≥ 65 with SR (n = 91) | 17 (18.7%) | 1.867 (1.156–3.015) | 0.011 | |
| Age ≥ 65 with AF (n = 58) | 19 (32.8) | 1.105 (0.635–1.922) | 0.724 | |
| Sex and rhythm at blood collection | 0.011 | |||
| Male with SR (n = 104) | 25 (24.0%) | 1.536 (1.095–2.154) | 0.013 | |
| Male with AF (n = 80) | 20 (25.0%) | 1.221 (0.671–2.223) | 0.513 | |
| Female with SR (n = 48) | 8 (16.7%) | 0.999 (0.432–2.311) | 0.999 | |
| Female with AF (n = 22) | 12 (54.5%) | 0.743 (0.330–1.675) | 0.474 | |
| Type of AF and rhythm at blood collection | 0.436 | |||
| Paroxysmal AF with SR (n = 141) | 30 (21.3%) | 1.391 (0.997–1.943) | 0.052 | |
| Paroxysmal AF with AF (n = 34) | 12 (35.3) | 1.162 (0.641–2.108) | 0.621 | |
| Persistent AF with SR (n = 11) | 3 (27.3%) | 1.920 (0.353–10.430) | 0.450 | |
| Persistent AF with AF (n = 68) | 20 (29.4%) | 1.187 (0.628–2.244) | 0.597 | |
| BMI and rhythm at blood collection | 0.640 | |||
| BMI < 25 kg/m2 mm with SR (n = 109) | 23 (21.1%) | 1.147 (0.791–1.664) | 0.470 | |
| BMI < 25 kg/m2 mm with AF (n = 63) | 17 (27.0%) | 1.225 (0.698–2.151) | 0.479 | |
| BMI ≥ 25 kg/m2 mm with SR (n = 43) | 10 (23.2%) | 2.269 (1.170–4.401) | 0.015 | |
| BMI ≥ 25 kg/m2 mm with AF (n = 39) | 15 (38.5%) | 1.010 (0.437–2.335) | 0.982 | |
| eGFR and rhythm at blood collection | 0.472 | |||
| eGFR ≥ 60 ml/min/1.78 m2 mm with SR (n = 130) | 28 (21.5%) | 1.230 (0.881–1.716) | 0.225 | |
| eGFR ≥ 60 ml/min/1.78 m2 mm with AF (n = 86) | 27 (31.3%) | 1.258 (0.742–2.131) | 0.394 | |
| eGFR < 60 ml/min/1.78 m2 mm with SR (n = 22) | 5 (22.7%) | 3.702 (1.135–12.080) | 0.030 | |
| eGFR < 60 ml/min/1.78 m2 mm with AF (n = 16) | 5 (31.3%) | 1.000 (0.281–3.557) | 1.000 | |
| LAD and rhythm at blood collection | 0.374 | |||
| LAD < 40 mm with SR (n = 100) | 19 (19.0%) | 1.034 (0.684–1.562) | 0.874 | |
| LAD < 40 mm with AF (n = 29) | 9 (31.0%) | 2.033 (0.599–6.904) | 0.255 | |
| LAD ≥ 40 mm with SR (n = 52) | 14 (26.9%) | 2.382 (1.305–4.348) | 0.005 | |
| LAD ≥ 40 mm with AF (n = 73) | 23 (31.5%) | 0.994 (0.590–1.675) | 0.981 | |
| LVEF and rhythm at blood collection | 0.876 | |||
| LVEF ≥ 50% mm with SR (n = 141) | 30 (21.3) | 1.394 (0.997–1.949) | 0.052 | |
| LVEF ≥ 50% mm with AF (n = 86) | 28 (32.6) | 1.230 (0.765–1.977) | 0.392 | |
| LVEF < 50% mm with SR (n = 11) | 3 (27.3) | 1.487 (0.353–6.257) | 0.589 | |
| LVEF < 50% mm with AF (n = 16) | 4 (25.0) | 0.933 (0.137–6.338) | 0.944 | |
Abbreviations are shown as in Table 1.
Discussion
In the present study, baseline ln BNP levels were significantly higher in patients with than without the recurrence of AF, whereas there were no significant differences in clinical and echocardiographic variables, points of risk scores, and levels of biomarkers of endothelial dysfunction between patients with and without the recurrence of AF. During a 2-year follow-up period, patients with the higher level of ln BNP had a significantly higher recurrent rate of AF than those with the low level of ln BNP. Moreover, baseline ln BNP was significantly and independently associated with the recurrence of AF in the univariate and multivariate Cox regression analyses. Furthermore, baseline ln BNP levels were significantly associated with rhythm at blood collection, age, sex, and LAD, and LVEF. Finally, the subgroup analyses showed a significant interaction of ln BNP with rhythm status at blood collection and sex difference.
Baseline clinical variables and scoring systems in the recurrence of AF
Many observational studies have reported predictors of the recurrence of AF after catheter ablation including the key risk variables [25]. Persistent AF and LAD, both of which are related to atrial remodeling [11,12], are most consistently recognized as important baseline predictors for the recurrence of AF [25]. A study showed that the APPLE score for the prediction of rhythm outcomes after catheter ablation of AF, which comprises age, type of AF, renal function, LAD, and LVEF, had a better prediction of the recurrence of AF than CHADS2 and CHA2DS2-VASc scores [17]. However, in this study, above-mentioned baseline clinical variables, CHADS2, CHA2DS2-VASc, APPLE scores were not significantly different between patients with and without the recurrence of AF. Mean age of patients enrolled in this study was 65.5 years, whereas those of patients in other studies to identify predictors of late recurrence after AF ablation, to evaluate the values of CHADS2, CHA2DS2-VASc, and the APPLE scores were 57–61 years old [16,17,25]. Furthermore, BMI and LAD of patients in this study were smaller, a period of follow-up longer than those of patients in other studies, and races of patients differed between studies. Therefore, these differences between the current study and other studies may have caused inconsistent results of predictive values of baseline clinical variables and scoring systems for the recurrence of AF.
Biomarkers in the recurrence of AF
Inflammation and oxidative stress have been reported as the etiology of AF development [8–10] and biomarkers of endothelial dysfunction caused by inflammatory, oxidative stress have been reported to be associated with risk of incident AF [20–24]; however, an association between pre-ablation concentrations of endothelial dysfunction biomarkers and the recurrence of AF has not yet been investigated. In the current study, we found no significant endothelial dysfunction biomarkers associated with risk of the recurrence of AF. It has been reported that the risk associated with endothelial dysfunction for arrhythmia recurrence following catheter ablation was age-dependent and was higher in younger than older patients with AF [23]. Therefore, it is possible that baseline concentrations of endothelial dysfunction biomarkers have predictive values for the recurrence of AF in younger patients than those enrolled in the current study. Further study is needed to confirm this possibility.
Associations between natriuretic peptide and the recurrence of AF have been intensively studied. Meta-analyses have shown that the recurrence of AF was associated with higher pre-ablation concentrations of BNP than non-recurrence although results of the studies were significantly heterogeneous; however, such heterogeneities have not been fully explained [18,19]. In the current study, we found that baseline ln BNP was significantly and independently associated with the recurrence of AF. We also found that AF at blood collection was significantly associated with the substantially increased level of ln BNP. Moreover, the subgroup analyses showed a significant interaction of ln BNP with sex and rhythm at blood collection, which may explain the heterogeneities between studies to test associations between BNP and the recurrence of AF [18,19]. Taken together, in patients with nonvalvular AF, baseline BNP was suggested as a useful biomarker for the risk of late recurrence of AF after ablation; however, there is a need to be careful while using BNP as a biomarker for the recurrence of AF by taking account of the effects of rhythm status at blood collection and sex difference.
Study limitations
Several limitations of our study need to be considered. This study was performed in a single center, which may have resulted in a selection bias: indeed, BMI and LAD of patients in this study were smaller, and age was higher than those of patients in other studies. Asymptomatic episodes of AF may have been missed. We did not evaluate the responses of biomarkers to ablation therapy. We were unable to establish causal relationships between biomarker concentrations and the recurrence of AF because of a prospective observational study. However, our study also had several strengths, including a period of follow-up longer than other studies, deep and systematical evaluation of associations of the risk scores, biomarkers and atrial remodeling with the recurrence of AF, which allowed us to recognize the usefulness of BNP as a predictor of recurrence after ablation treatment of atrial fibrillation and at the same time to recognize the attention at that time.
Conclusions
In this study, baseline levels of BNP, but not those of biomarkers of endothelial dysfunction or points of risk scoring systems, were independently associated with the recurrence of AF after radiofrequency catheter ablation. Baseline ln BNP levels were significantly associated with rhythm at blood collection, age, sex, and LAD, and LVEF, and the subgroup analyses showed significant interactions of ln BNP with sex, and rhythm at blood collection. These results suggest that pre-ablation levels of ln BNP are useful to evaluate the risk of AF recurrence after ablation; however, there is a need to be careful while using BNP as a biomarker for the risk of AF recurrence by taking account of the effects of rhythm status at blood collection and sex difference.
Acknowledgements
This work was supported by a Grant from the Faculty of Medicine, Tottori University, Yonago, Japan. We thank Dr. Trish Reynolds, MBBS, FRACP, from Edanz Group for editing a draft of this manuscript.
Funding
Funding was provided by Tottori University.
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 2.Stewart S, Hart CL, Hole DJ, McMurray JJV. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113:359–364. doi: 10.1016/S0002-9343(02)01236-6. [DOI] [PubMed] [Google Scholar]
- 3. LaPar DJ, Speir AM, Crosby IK, Fonner E Jr., Brown M, Rich JB, Quader M, Kern JA, Kron IL Ailawadi G (2014) Postoperative atrial fibrillation significantly increases mortality, hospital readmission, and hospital costs. Ann Thorac Surg 98:527–533 (discussion 533) [DOI] [PubMed]
- 4.Haissaguerre M, Jais P, Shah DC, Takahashi A, Hocini M, Quiniou G, Garrigue S, Le Mouroux A, Le Metayer P, Clementy J. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med. 1998;339:659–666. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 5.Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, Akar JG, Badhwar V, Brugada J, Camm J, Chen PS, Chen SA, Chung MK, Nielsen JC, Curtis AB, Davies DW, Day JD, d'Avila A, de Groot N, Di Biase L, Duytschaever M, Edgerton JR, Ellenbogen KA, Ellinor PT, Ernst S, Fenelon G, Gerstenfeld EP, Haines DE, Haissaguerre M, Helm RH, Hylek E, Jackman WM, Jalife J, Kalman JM, Kautzner J, Kottkamp H, Kuck KH, Kumagai K, Lee R, Lewalter T, Lindsay BD, Macle L, Mansour M, Marchlinski FE, Michaud GF, Nakagawa H, Natale A, Nattel S, Okumura K, Packer D, Pokushalov E, Reynolds MR, Sanders P, Scanavacca M, Schilling R, Tondo C, Tsao HM, Verma A, Wilber DJ, Yamane T. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14:e275–e444. doi: 10.1016/j.hrthm.2017.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuck KH, Hoffmann BA, Ernst S, Wegscheider K, Treszl A, Metzner A, Eckardt L, Lewalter T, Breithardt G, Willems S. Impact of complete versus incomplete circumferential lines around the pulmonary veins during catheter ablation of paroxysmal atrial fibrillation: results from the Gap-Atrial Fibrillation-German Atrial Fibrillation Competence Network 1 Trial. Circ Arrhythm Electrophysiol. 2016;9:e003337. doi: 10.1161/CIRCEP.115.003337. [DOI] [PubMed] [Google Scholar]
- 7.Zaman JAB, Baykaner T, Clopton P, Swarup V, Kowal RC, Daubert JP, Day JD, Hummel J, Schricker AA, Krummen DE, Mansour M, Tomassoni GF, Wheelan KR, Vishwanathan M, Park S, Wang PJ, Narayan SM, Miller JM. Recurrent post-ablation paroxysmal atrial fibrillation shares substrates with persistent atrial fibrillation : an 11-center study. JACC Clin Electrophysiol. 2017;3:393–402. doi: 10.1016/j.jacep.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sardu C, Santulli G, Santamaria M, Barbieri M, Sacra C, Paolisso P, D'Amico F, Testa N, Caporaso I, Paolisso G, Marfella R, Rizzo MR. Effects of alpha lipoic acid on multiple cytokines and biomarkers and recurrence of atrial fibrillation within 1 year of catheter ablation. Am J Cardiol. 2017;119:1382–1386. doi: 10.1016/j.amjcard.2017.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Samman Tahhan A, Sandesara PB, Hayek SS, Alkhoder A, Chivukula K, Hammadah M, Mohamed-Kelli H, O'Neal WT, Topel M, Ghasemzadeh N, Ko YA, Aida H, Gafeer M, Sperling L, Vaccarino V, Liang Y, Jones DP, Quyyumi AA. Association between oxidative stress and atrial fibrillation. Heart Rhythm. 2017;14:1849–1855. doi: 10.1016/j.hrthm.2017.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xie W, Santulli G, Reiken SR, Yuan Q, Osborne BW, Chen BX, Marks AR. Mitochondrial oxidative stress promotes atrial fibrillation. Sci Rep. 2015;5:11427. doi: 10.1038/srep11427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santulli G, D'Ascia SL, D'Ascia C. Development of atrial fibrillation in recipients of cardiac resynchronization therapy: the role of atrial reverse remodelling. Can J Cardiol. 2012;28(245):e217. doi: 10.1016/j.cjca.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 12.D'Ascia SL, D'Ascia C, Marino V, Lombardi A, Santulli R, Chiariello M, Santulli G. Cardiac resynchronisation therapy response predicts occurrence of atrial fibrillation in non-ischaemic dilated cardiomyopathy. Int J Clin Pract. 2011;65:1149–1155. doi: 10.1111/j.1742-1241.2011.02732.x. [DOI] [PubMed] [Google Scholar]
- 13.Kornej J, Hindricks G, Kosiuk J, Arya A, Sommer P, Husser D, Rolf S, Richter S, Piorkowski C, Gaspar T, Lip GY, Bollmann A. Renal dysfunction, stroke risk scores (CHADS2, CHA2DS2-VASc, and R2CHADS2), and the risk of thromboembolic events after catheter ablation of atrial fibrillation: the Leipzig Heart Center AF Ablation Registry. Circ Arrhythm Electrophysiol. 2013;6:868–874. doi: 10.1161/CIRCEP.113.000869. [DOI] [PubMed] [Google Scholar]
- 14.Letsas KP, Efremidis M, Giannopoulos G, Deftereos S, Lioni L, Korantzopoulos P, Vlachos K, Xydonas S, Kossyvakis C, Sideris A. CHADS2 and CHA2DS2-VASc scores as predictors of left atrial ablation outcomes for paroxysmal atrial fibrillation. Europace. 2014;16:202–207. doi: 10.1093/europace/eut210. [DOI] [PubMed] [Google Scholar]
- 15.Jacobs V, May HT, Bair TL, Crandall BG, Cutler M, Day JD, Weiss JP, Osborn JS, Muhlestein JB, Anderson JL, Mallender C, Bunch TJ. The impact of risk score (CHADS2 versus CHA2DS2-VASc) on long-term outcomes after atrial fibrillation ablation. Heart Rhythm. 2015;12:681–686. doi: 10.1016/j.hrthm.2014.12.034. [DOI] [PubMed] [Google Scholar]
- 16.Kornej J, Hindricks G, Kosiuk J, Arya A, Sommer P, Husser D, Rolf S, Richter S, Huo Y, Piorkowski C, Bollmann A. Comparison of CHADS2, R2CHADS2, and CHA2DS2-VASc scores for the prediction of rhythm outcomes after catheter ablation of atrial fibrillation: the Leipzig Heart Center AF Ablation Registry. Circ Arrhythm Electrophysiol. 2014;7:281–287. doi: 10.1161/CIRCEP.113.001182. [DOI] [PubMed] [Google Scholar]
- 17.Kornej J, Hindricks G, Shoemaker MB, Husser D, Arya A, Sommer P, Rolf S, Saavedra P, Kanagasundram A, Patrick Whalen S, Montgomery J, Ellis CR, Darbar D, Bollmann A. The APPLE score: a novel and simple score for the prediction of rhythm outcomes after catheter ablation of atrial fibrillation. Clin Res Cardiol. 2015;104:871–876. doi: 10.1007/s00392-015-0856-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang Y, Chen A, Song L, Li M, Chen Y, He B. Association between baseline natriuretic peptides and atrial fibrillation recurrence after catheter ablation. Int Heart J. 2016;57:183–189. doi: 10.1536/ihj.15-355. [DOI] [PubMed] [Google Scholar]
- 19.Jiang H, Wang W, Wang C, Xie X, Hou Y. Association of pre-ablation level of potential blood markers with atrial fibrillation recurrence after catheter ablation: a meta-analysis. Europace. 2017;19:392–400. doi: 10.1093/europace/euw335. [DOI] [PubMed] [Google Scholar]
- 20.Willeit K, Pechlaner R, Willeit P, Skroblin P, Paulweber B, Schernthaner C, Toell T, Egger G, Weger S, Oberhollenzer M, Kedenko L, Iglseder B, Bonora E, Schett G, Mayr M, Willeit J, Kiechl S. Association between vascular cell adhesion molecule 1 and atrial fibrillation. JAMA Cardiol. 2017;2:516–523. doi: 10.1001/jamacardio.2017.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conen D, Ridker PM, Everett BM, Tedrow UB, Rose L, Cook NR, Buring JE, Albert CM. A multimarker approach to assess the influence of inflammation on the incidence of atrial fibrillation in women. Eur Heart J. 2010;31:1730–1736. doi: 10.1093/eurheartj/ehq146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krishnamoorthy S, Khoo CW, Lim HS, Lane DA, Pignatelli P, Basili S, Violi F, Lip GY. Prognostic role of plasma von Willebrand factor and soluble E-selectin levels for future cardiovascular events in a 'real-world' community cohort of patients with atrial fibrillation. Eur J Clin Invest. 2013;43:1032–1038. doi: 10.1111/eci.12140. [DOI] [PubMed] [Google Scholar]
- 23.Weymann A, Sabashnikov A, Ali-Hasan-Al-Saegh S, Popov AF, Jalil Mirhosseini S, Baker WL, Lotfaliani M, Liu T, Dehghan H, Yavuz S, de Oliveira Sa MP, Jang JS, Zeriouh M, Meng L, D'Ascenzo F, Deshmukh AJ, Biondi-Zoccai G, Dohmen PM, Calkins H, Cardiac Surgery and Cardiology-Group Imcsc-Group IM Predictive role of coagulation, fibrinolytic, and endothelial markers in patients with atrial fibrillation, stroke, and thromboembolism: a meta-analysis, meta-regression, and systematic review. Med Sci Monit Basic Res. 2017;23:97–140. doi: 10.12659/MSMBR.902558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Conway DS, Heeringa J, Van Der Kuip DA, Chin BS, Hofman A, Witteman JC, Lip GY. Atrial fibrillation and the prothrombotic state in the elderly: the Rotterdam Study. Stroke. 2003;34:413–417. doi: 10.1161/01.STR.0000051728.85133.32. [DOI] [PubMed] [Google Scholar]
- 25.D'Ascenzo F, Corleto A, Biondi-Zoccai G, Anselmino M, Ferraris F, di Biase L, Natale A, Hunter RJ, Schilling RJ, Miyazaki S, Tada H, Aonuma K, Yenn-Jiang L, Tao H, Ma C, Packer D, Hammill S, Gaita F. Which are the most reliable predictors of recurrence of atrial fibrillation after transcatheter ablation?: a meta-analysis. Int J Cardiol. 2013;167:1984–1989. doi: 10.1016/j.ijcard.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 26.Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–992. doi: 10.1053/j.ajkd.2008.12.034. [DOI] [PubMed] [Google Scholar]
- 27.Kondo T, Miake J, Kato M, Ogura K, Iitsuka K, Yamamoto K. Impact of postprocedural antiarrhythmic drug therapy with bepridil on maintaining sinus rhythm after catheter ablation for persistent atrial fibrillation. J Cardiol. 2016;68:229–235. doi: 10.1016/j.jjcc.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 28.Matsuzawa Y, Suleiman M, Guddeti RR, Kwon TG, Monahan KH, Lerman LO, Friedman PA, Lerman A. Age-dependent predictive value of endothelial dysfunction for arrhythmia recurrence following pulmonary vein isolation. J Am Heart Assoc. 2016;5:e003183. doi: 10.1161/JAHA.115.003183. [DOI] [PMC free article] [PubMed] [Google Scholar]