Abstract
Background:
Institutional rearing is associated with increased risk for reactive attachment disorder (RAD) and disinhibited social engagement disorder (DSED). Disorders of attachment involve disturbances in children’s primary caregiving relationships, and are likely to disturb multiple domains of social functioning.
Objective:
To examine associations between signs of RAD and DSED and social functioning in early adolescence.
Participants and setting:
Our participants were 110 children with a history of institutional rearing and 50 community comparison adolescents from the Bucharest Early Intervention Project, based in Bucharest, Romania. Participants were assessed at age 12 years (M age in years=12.80, SD=0.71).
Method:
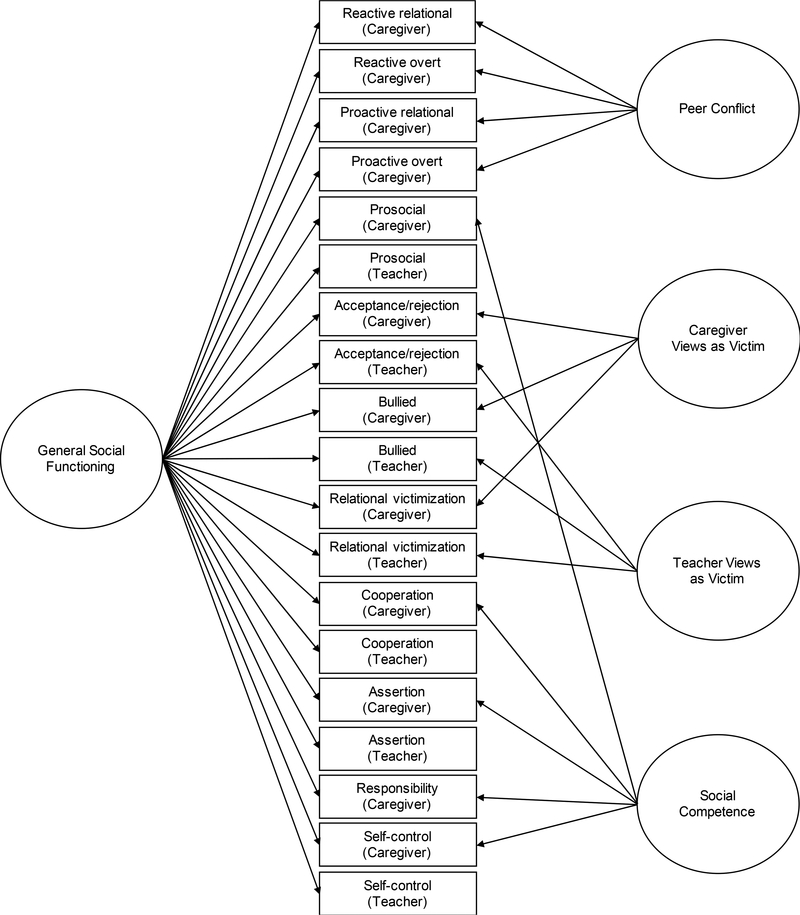
Signs of RAD and DSED were obtained through caregiver report. Reports of social functioning were provided by caregivers and teachers. General and specific domains of social functioning were identified using bi-factor modeling. A general social functioning factor and four specific factors were revealed: peer conflict, caregiver views as victim, teacher views as victim, and social competence.
Results:
Signs of RAD predicted poorer general social functioning (β=−.36, p<.01, 95% confidence interval [CI] [−.33, −.09]) and poorer social competence (β=−.38, p<.01, 95% CI[−.05, −.01]) above and beyond time spent in institutional care and placement disruptions. Signs of DSED (β=−.38, p<.001, 95% CI[−.49, −.16]) along with placement disruptions (β=−.22, p<.05, 95% CI[−.29, −.01]) predicted poorer general social functioning above and beyond time spent in institutional care. Signs of DSED predicted higher scores on caregiver views as victim (β=.29, p<.05, 95% CI[.02, .14]) and lower scores on social competence (β=−.29, p<.01, 95% CI[−.06, −.01]) above and beyond time spent in institutional care and placement disruptions.
Conclusions:
Attachment disorder signs in early adolescence are problematic for social functioning, although the manifestation of these social difficulties differs based on whether RAD or DSED signs are present.
Keywords: Reactive Attachment Disorder, Disinhibited Social Engagement Disorder, Social functioning, Institutionalization, bi-factor modeling
Deficits in social functioning among children with a history of institutional care have been extensively documented (Almas et al., 2012; Caprin, Benedan, Ballarin, & Gallace, 2017; Hodges & Tizard, 1989; Humphreys, Gabard-Durnam, et al., 2017; McCall et al., 2015; O’Connor & Rutter, 2000; Roy, Rutter, & Pickles, 2004; E. J. Sonuga-Barke, Schlotz, & Kreppner, 2010; Tarullo & Gunnar, 2005; Tizard & Hodges, 1978). Among very young children, the earliest building blocks of social functioning lie in the quality of the attachment relationships formed with caregivers. Like other aspects of social functioning, disturbances in the formation of attachment relationships are particularly common among children raised in institutions, as children in these circumstances have few opportunities to form lasting relationships with safe and supportive adults (Gleason et al., 2014; O’Connor & Rutter, 2000; Zeanah, 2000; Zeanah & Gleason, 2015; Zeanah, Smyke, Koga, & Carlson, 2005). Attachment disorders (i.e., reactive attachment disorder, RAD, and disinhibited social engagement disorder, DSED), are characterized by aberrant ways of interacting with others. Importantly, although these two disorders have shared etiology in the form of caregiver neglect, they differ in their presentation (Gleason et al., 2011), as well as potential psychosocial outcomes. RAD defines behaviors in children such as being socially withdrawn and emotionally inhibited when interacting with others, whereas DSED is characterized by social disinhibition and boundary violations in children’s interactions with others (American Psychiatric Association, 2013; ZERO TO THREE, 2016).
Given that early caregiver–infant relationships provide a framework for the development of future relationships (Ainsworth, 1979; Bowlby, 1969; Fonagy, Steele, Moran, Steele, & Higgitt, 1993), the ability to build and maintain healthy relationships beyond one’s primary caregiving relationship is likely associated with the quality of early relationships with caregivers. In fact, greater attachment security with caregivers has been associated with more positive social skills at age 8 years among children with a history institutional care (Almas et al., 2012). It is possible that signs of disordered attachment are responsible, in part, for observed social difficulties found among children with a history of institutional care. RAD and DSED have been well described in early childhood (see Zeanah & Gleason, 2015). Although their presentation is less well studied in middle childhood and adolescence, we have reported on the persistence of signs of RAD and DSED into adolescence (Guyon-Harris, Humphreys, Degnan, et al., in press; Guyon-Harris, Humphreys, Fox, Nelson, & Zeanah, in press; Sonuga-Barke et al., 2017). Given the persistence of RAD and DSED signs into adolescence and the increasing importance of peer relationships during this developmental period (Brown & Larson, 2009), examining the potential associations between RAD and DSED with social functioning in adolescence is of particular interest.
Hodges and Tizard (1989) provided one of the earliest accounts of the social functioning of adolescents with a history of institutional care. Difficulties in parent–child relationships, as well as peer relationships, were common following institutional care. In general, 16-year-old adolescents who had been reared in institutions had more difficulties with peers, particularly being quarrelsome and less well-liked, as well as more difficulties with siblings and reduced closeness with caregivers, as compared to community comparison children. The adolescents were also rated by caregiver and teachers as seeking more attention and support from adults rather than peers. Although accounts of DSED and RAD type behaviors were reported, these were not explicitly examined in association with broader social functioning difficulties observed.
Few studies have examined associations between signs of RAD and DSED, considered jointly, and social functioning, and such associations are often ancillary to the primary goals of studies and not thoroughly explored or discussed. Moran and colleagues (2017) examined base rates of RAD and DSED among juvenile offenders and associations with multiple outcomes, one of which was peer problems, in a small sample (n=29) of juvenile offenders ages 12–17 years, a majority of whom had experienced maltreatment. Signs of attachment disordered behavior were moderately associated with parent-rated, but not teacher-rated, peer relationship problems. Notably, however, given that signs of RAD and DSED were combined, this study was unable to examine the possibility of distinct associations from each disorder.
Only one study has investigated associations between signs of DSED and peer problems among children in institutional care. In this study, Sonuga-Barke and colleagues (2010) examined the impact of institutional care on peer problems from childhood to adolescence among previously institutionalized Romanian children adopted to families in the United Kingdom (i.e., the English and Romanian Adoptees Study ERAS). Caregiver reported peer problems were positively correlated with signs of DSED, further supporting a potential link between signs of DSED and social functioning.
Social functioning is not a unitary construct. Domains of social functioning include appropriate assertiveness, self-regulation, and navigating social conflict (e.g., relational victimization and bullying), and reports of social functioning can differ based on context and informant (e.g., home/caregivers vs. school/teachers). Recent findings suggest that difficulties in social functioning observed among children with a history of institutional care include a lack of social approach and increased aggression/overarousal with peers (Humphreys, Gabard-Durnam, et al., 2017). Therefore, assessing multiple domains of social functioning will allow for a more comprehensive understanding of which domains of social functioning are most associated with RAD and DSED.
The aim of the present study was to examine the impact of signs of RAD and DSED on social functioning in early adolescence. Several assessments of social functioning were considered with reports were obtained from both caregivers and teachers. These reports were combined using bi-factor modeling (Holzinger & Swineford, 1937; Schmid & Leiman, 1957) to capture the complexity of social functioning in early adolescence. This approach allows for the identification of an overall general factor as well as specific, unique factors within the construct.
We hypothesized that signs of both RAD and DSED will be associated with general (i.e., across domains and reporters) difficulties in social functioning. Given that bi-factor modeling results in additional unique factors of social functioning, we planned to probe whether signs of RAD and DSED would be differentially associated with each factor, given the unique behavioral presentations for each disorder.
Method
Participants
Participants included children residing in institutions in Bucharest, Romania (average age of placement into institutional care=2.57 months, range=0.00–17.49 months) from the Bucharest Early Intervention Project (BEIP) and community comparison children from Bucharest, Romania without a history of institutional care. The BEIP is a randomized control trial (RCT) of foster care compared to care as usual in an institutional setting. The original sample consisted of 136 infants and toddlers (M age at randomization=22 months) living in institutions in Bucharest, Romania, recruited between 1998 and 2000. These children were randomized to a care as usual group (CAUG) and foster care group (FCG), each comprising 68 children and a never institutionalized group (NIG) of community comparison children that included 72 children. Children in the FCG were placed into foster care at an average of 22.63 months (range=6.81–33.01 months). Additional details about the original sample are available elsewhere (Nelson, Fox, & Zeanah, 2014; Zeanah et al., 2003). Data for the present study were drawn from a follow-up assessment conducted at age 12 years (M age in years=12.80, SD=0.71) and are available for 55 children each from the CAUG and FCG and 50 from the NIG.
Prior to study initiation, approval was obtained by the local Commissions on Child Protection in Bucharest as well as the institutional review boards of the three principal investigators (BLINDED). The BEIP was conducted in collaboration with the Institute of Maternal and Child Health of the Romanian Ministry of Health. Consent for participation was obtained from each child’s legal guardian at the beginning of the study. Child assent was obtained at age 12 years. Special ethical considerations were made in the planning of the BEIP and discussions by us and by others are available elsewhere (Miller, 2009; Millum & Emanuel, 2007; Nelson et al., 2014; Rid, 2012; Zeanah, Fox, & Nelson, 2012).
Procedure
Following assessment at baseline, children were randomized to the CAUG or FCG. Children in the FCG were placed with foster parents recruited and trained to provide high-quality care by study personnel (Smyke, Zeanah, Fox, & Nelson, 2009; Zeanah et al., 2003). The foster parents were supported by social workers in Bucharest who received regular consultation from clinicians in the U.S. Parents were explicitly encouraged to care for their foster children as if they were their own children and to make full and lasting commitments to them.
Data for the present study were cross-sectional and drawn from the age 12 years assessment wave. Caregiver reports were completed by the biological, foster, or adoptive mother in the case of the NIG and FCG children as well as the CAUG who were placed into families throughout the course of the study. For children still in the institution, caregiver reports were completed by a staff member who knew the child best. Teacher reports were completed by each child’s current teacher. All measures were administered in Romanian. Measures were translated into Romanian, back translated into English and assessed for meaning at each step by researchers fluent in both English and Romanian.
Measures
Disturbances of attachment.
Signs of RAD and DSED at age 12 years were assessed using the Disturbances of Attachment Interview—Early Adolescence (DAI-EA; Humphreys, Nelson, Fox, & Zeanah, 2017), which is a semi-structured interview of caregivers about signs of disordered attachment. Trained researchers rated caregivers’ responses to the items on a scale from 0 to 2. The inhibited social behavior scale comprised 7 items and ranged 0 to 14 and identified signs of RAD. The disinhibited social behavior scale comprised 5 items and ranged 0 to 10 and identified signs of DSED (see Humphreys, Nelson, Fox, & Zeanah, 2017, for more information on the specific items included). Higher scores on both scales indicated greater signs of RAD and DSED.
Social Functioning.
Social functioning at age 12 years across multiple domains and reporters was assessed using the Peer Conflict Scale (PCS; Marsee & Frick, 2007), the MacArthur Health and Behavior Questionnaire (HBQ; Essex et al., 2002), and the Social Skills Rating System (SSRS; Gresham & Elliott, 1990).
PCS.
The PCS is a caregiver-report assessing reactive and proactive forms of overt (e.g., physical) and relational aspects of peer conflict. The reactive overt, reactive relational, proactive overt, and proactive relational aggression subscales were used. The reactive overt subscale contains behaviors such as acting out aggressively as a response to provocation. The reactive relational subscale involves relational retaliation such as sharing someone’s secrets when provoked. The proactive overt subscale refers to physical violence or aggression that is unprovoked. Finally, the proactive relational subscale includes relational aggression that is unprovoked. Internal consistency of the subscales and expected relations with emotional regulation, callous/unemotional traits, and delinquency have been reported (Marsee et al., 2011; Marsee & Frick, 2007).
HBQ.
The HBQ is a questionnaire assessing multiple domains of child functioning including emotional and behavioral adjustment. We used the prosocial, acceptance/rejection, bullied, relational victimization subscales from the caregiver and teacher reports. The prosocial subscale contains items that reflect the child’s awareness of and respect for others in social situations such as being considerate of other’s feelings and offering help to those in need. The acceptance/rejection subscale concerns the degree to which the child is liked and accepted by peers. The bullied subscale contains items pertaining to whether the child is picked on or teased by others. The relational victimization subscale focuses specifically on relational conflict such as having rumors spread about oneself, being talked about behind ones back, and being intentionally left out by others. The HBQ has been successfully used with previously institutionalized children in past research (Wiik et al., 2011) and demonstrated good test-retest reliability and discriminant validity (Ablow et al., 1999).
SSRS.
The SSRS is a questionnaire assessing social and behavioral problems in children by caregiver and teacher report. We used the cooperation, assertion, responsibility, and self-control subscales from the caregiver report and the cooperation, assertion, and self-control subscales from the teacher report; there is no responsibility subscale on the teacher report. The cooperation subscale includes items such as volunteering to help family members with tasks and giving compliments to others. The assertion subscale includes items involving taking initiative in social situations such as joining into an activity without being told to. The responsibility subscale (parent report only) contains items such as introducing oneself to others without being told and asking an adult for permission when needed. Finally, the self-control subscale captures the child’s ability to control their feelings and reactions appropriately in social situations such as refusing unreasonable requests from others or controlling their temper when in conflict. Internal consistency as well as good convergent validity with another measure of social skills have been established (Gresham, Elliott, Vance, & Cook, 2011).
Data Analysis
Domains of social functioning reported by caregivers and teachers were analyzed using exploratory and confirmatory bi-factor models (Holzinger & Swineford, 1937; Schmid & Leiman, 1957) to identify latent factors of general and unique aspects of social functioning across the entire sample (i.e., CAUG, FCG, and NIG). Bi-factor modeling is a type of factor analysis that allows elements of a construct (e.g., items or subscales) simultaneously to load onto two factors: a general factor as well as additional specific factors (Reise, Moore, & Haviland, 2010). Therefore, the result is a final model which consists of a general factor comprising all elements of the construct, as well as unique specific factors that account for additional variance and specificity in the construct not fully captured by the general factor. Thus, bi-factor modeling was used in the present study to identify associations of a general measure of social functioning as well as with more nuanced, specific measures of social functioning with signs of RAD and DSED. Exploratory models were used to examine how well each subscale loaded onto the general factor as well as to identify potential specific factors. The initial exploratory model included 19 subscales (see measures above; i.e., four caregiver reported subscales from PCS, four caregiver reported and four teacher reported subscales from the HBQ, and four caregiver reported and three teacher reported subscales from the SSRS). Confirmatory bi-factor modeling was then used to further examine models identified in the exploratory stage. Modification indices were examined to assist with the evaluation and reconfiguration of models to arrive at the best fitting solution. The final model was evaluated based on commonly used fit indices including the comparative fit index (CFI; Bentler, 1990), Tucker-Lewis index (TLI; Tucker & Lewis, 1973), root mean square error of approximation (RMSEA; Steiger, 1990), and standardized root mean square residual (SRMR; Bentler, 1995). Factor scores were extracted and used in further analyses.
Bi-variate associations between the social functioning factors and attachment disorder signs were examined along with differences in the strength of the association between RAD and domains of social functioning compared to DSED and domains of social functioning. Differences in the strength of correlations were computed following guidelines of Lee and Preacher (2013). Hierarchical ordinary least square regression was used to examine the impact of attachment disorder signs on domains of social functioning above and beyond institutional care variables including time spent in the institution and the number of placement disruptions upon leaving the institution. Sex of the child was entered into the model as a dummy-coded covariate. These analyses were conducted only on children with a history of institutional care (i.e., CAUG and FCG).
Results
Exploratory bi-factor models indicated that a model with a general factor containing all PCS, HBQ, and SSRS subscales and four additional specific factors was the best fit for the data. A confirmatory model based on the exploratory model was then examined. The final conceptual model is depicted in Figure 1. Modification indices suggested specifying correlations between the proactive overt and reactive overt and the proactive relational and proactive overt subscales on the PCS and between caregiver reported cooperation and assertion on the SSRS, which improved model fit. All loadings were significant at the p<.01 level (see Table 1) and the model demonstrated adequate fit (χ2136=234.57, CFI=.93, TLI=.91, RMSEA=.07). The general factor contained all parent and teacher reported subscales from the PCS, HBQ, and SSRS. Four specific factors were also revealed. Factor one, labeled “Peer Conflict,” comprised all four subscales of the PCS (reactive overt, reactive relational, proactive overt, and proactive relational aggression). Higher scores indicated greater caregiver-reported conflict with peers. Factor two, labeled “Caregiver Views as Victim” comprised the bullied, relational victimization, and acceptance/rejection subscales of the HBQ from the caregiver report. Similarly, factor three, labeled “Teacher Views as Victim” also comprised the bullied, relational victimization, and acceptance/rejection subscales of the HBQ however from the teacher report. Higher scores on both factors indicated that the child was perceived by the reported as less accepted by peers and more likely to be a victim in peer interactions. Finally, factor four, labeled “Social Competence,” comprised the caregiver-reported prosocial subscale on the HBQ and the caregiver-reported cooperation, responsibility, self-control, and assertion subscales on the SSRS. Higher scores indicated greater caregiver-reported scores on the Social Competence factor.
Figure 1.
Bi-factor model for social functioning.
Table 1.
Standardized Factor Loadings for the Bi-factor Model
| Scale | General Social Functioning | Peer Conflict | Caregiver Views as Victim | Teacher Views as Victim | Social Competence |
|---|---|---|---|---|---|
| PCS Reactive overt (Caregiver) | −0.50*** | 0.55*** | |||
| PCS Reactive relational (Caregiver) | −0.29** | 0.96*** | |||
| PCS Proactive overt (Caregiver) | −0.42** | 0.54*** | |||
| PCS Proactive relational (Caregiver) | −0.34*** | 0.76*** | |||
| HBQ prosocial (Caregiver) | 0.48*** | 0.47*** | |||
| HBG Acceptance/rejection (Caregiver) | 0.44*** | −0.62*** | |||
| HBQ Bullied (Caregiver) | −0.39*** | 0.60*** | |||
| HBQ Relational victimization (Caregiver) | −0.34*** | 0.88*** | |||
| HBQ prosocial (Teacher) | 0.79*** | ||||
| HBG Acceptance/rejection (Teacher) | 0.89*** | −0.26*** | |||
| HBQ Bullied (Teacher) | −0.61*** | 0.53*** | |||
| HBQ Relational victimization (Teacher) | −0.71*** | 0.68*** | |||
| SSRS Cooperation (Caregiver) | 0.32** | 0.59*** | |||
| SSRS Assertion (Caregiver) | 0.32** | 0.55*** | |||
| SSRS Responsibility (Caregiver) | 0.31*** | 0.70*** | |||
| SSRS Self-control (Caregiver) | 0.48*** | 0.71*** | |||
| SSRS Cooperation (Teacher) | 0.88*** | ||||
| SSRS Assertion (Teacher) | 0.64*** | ||||
| SSRS Self-control (Teacher) | 0.85*** |
p<.01.
p<.001.
Table 2 provides bi-variate associations between signs of RAD and DSED and the social functioning factors, as well as tests of test differences between dependent correlations of RAD and DSED with the social factors. Moderate, negative associations were found for both RAD and DSED with the General Social Functioning factor, and the strength of the associations did not significantly differ from one another. Signs of DSED, but not RAD, were associated with the caregiver’s view of the child as a victim. Furthermore, the magnitude of the relation between DSED and the caregiver’s view of the child as a victim was significantly higher than for RAD, indicating that children with risk DSED may be at greater risk of being victimized by peers compared to children with signs of RAD. Finally, both signs of DSED and RAD were moderately negatively associated with the Social Competence factor, such that children with more signs of attachment disorders are rated by their caregivers as having poorer social competence. The test of the difference between the correlations was not significant. Signs of RAD and DSED were not significantly associated with teacher reported victimization.
Table 2.
Bi-variate Associations between RAD and DSED Signs and Social Functioning Factors
| General Social Functioning | Peer Conflict | Caregiver Views as a Victim | Teacher Views as a Victim | Social Competence | |
|---|---|---|---|---|---|
| RAD signs | −.39*** | .02 | −.12 | −.15 | −.38*** |
| DSED signs | −.38*** | .13 | .27* | .03 | −.32** |
| Test of the difference between correlation (z) | −0.07 | −0.70 | −2.50** | −1.14 | −0.43 |
p<.05.
p<.01.
p<.001.
We examined the associations between signs of attachment disorders and social functioning after statistically covarying for (1) number of placement disruptions, (2) percent time spent in institutional care, both through age 12 years, as well as (3) sex of the child (see table 3 for RAD and table 4 for DSED). Only children in the CAUG and FCG were included in these analyses since the children in the NIG do not have a history of institutional care.
Table 3.
Signs of Reactive Attachment Disorder as a Predictor of Social Functioning
| General Social
Functioning |
Peer Conflict |
Caregiver Views as
Victim |
Teacher Views as
Victim |
Social Competence |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Step 2 |
Step 2 |
Step 2 |
Step 2 |
Step 2 |
||||||||||||||||
| β | β | 95% CI lower | 95% CI upper | β | β | 95% CI lower | 95% CI upper | β | β | 95% CI lower | 95% CI upper | β | β | 95% CI lower | 95% CI upper | β | β | 95% CI lower | 95% CI upper | |
| Disruptions | −.23* | −.17 | −.26 | .02 | .18 | .18 | −.09 | .66 | .15 | .19 | −.01 | .09 | .03 | .06 | −.03 | .04 | −.15 | −.09 | −.03 | .01 |
| Percent time | −.08 | .08 | −.01 | .01 | −.03 | −.02 | −.03 | .03 | .01 | .09 | −.00 | .01 | −.03 | .05 | −.00 | .00 | −.09 | .07 | −.00 | .00 |
| Sex (male=1) | −.32** | −.31** | −1.26 | −.34 | −.07 | −.07 | −1.64 | .81 | −.06 | −.05 | −.21 | .12 | .04 | .04 | −.09 | .14 | .02 | .03 | −.06 | .08 |
| RAD signs | −.36** | −.33 | −.09 | −.01 | −.33 | .30 | −.21 | −.08 | .00 | −.18 | −.05 | .01 | −.38** | −.05 | −.01 | |||||
| R2 | .19 | .29 | .00 | −.01 | −.00 | .02 | −.03 | −.02 | .02 | .11 | ||||||||||
| F | 7.32*** | 9.26*** | 1.04 | 0.78 | 0.86 | 1.45 | 0.06 | 0.62 | 1.48 | 3.98** | ||||||||||
| ΔR2 | .10 | .00 | .03 | .02 | .10 | |||||||||||||||
| ΔF | 12.39** | 0.01 | 3.18 | 2.30 | 11.00** | |||||||||||||||
p<.05.
p<.01
p<.001.
Note. Percent time = the percent of the child’s life spent in institutional care through age 12 years. RAD = Reactive Attachment Disorder.
Table 4.
Signs of Disinhibited Social Engagement Disorder as a Predictor of Social Functioning
| General Social
Functioning |
Peer Conflict |
Caregiver Views as
Victim |
Teacher Views as
Victim |
Social Competence |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Step 2 |
Step 2 |
Step 2 |
Step 2 |
Step 2 |
||||||||||||||||
| β | β | 95% CI lower | 95% CI upper | β | β | 95% CI lower | 95% CI upper | β | β | 95% CI lower | 95% CI upper | β | β | 95% CI lower | 95% CI upper | β | β | 95% CI lower | 95% CI upper | |
| Disruptions | −.23* | −.22* | −.29 | −.01 | .18 | .18 | −.09 | .64 | .15 | .15 | −.02 | .08 | .03 | .03 | −.03 | .04 | −.15 | −.15 | −.03 | .01 |
| Percent time | −.08 | .07 | −.01 | .01 | −.03 | −.08 | −.04 | .02 | .01 | −.11 | −.01 | .00 | −.03 | −.05 | −.00 | .00 | −.09 | .02 | −.00 | .00 |
| Sex (male=1) | −.31** | −.22** | −1.26 | −.35 | −.07 | −.07 | −1.65 | .78 | −.06 | −.07 | −.21 | .11 | .04 | .03 | −.10 | .13 | .02 | .03 | −.06 | .08 |
| DSED signs | −.38*** | −.49 | −.16 | .15 | −.15 | .74 | .29* | .02 | .14 | .05 | −.03 | .05 | −.29** | −.06 | −.01 | |||||
| R2 | .17 | .28 | .00 | .01 | −.00 | .06 | −.03 | −.04 | .02 | .08 | ||||||||||
| F | 7.32*** | 10.27*** | 1.04 | 1.22 | 0.86 | 2.43 | 0.06 | 0.09 | 1.48 | 2.98* | ||||||||||
| ΔR2 | .12 | .02 | .07 | .00 | .07 | |||||||||||||||
| ΔF | 15.67*** | 1.75 | 6.99* | 0.16 | 7.17** | |||||||||||||||
p<.05.
p<.01.
p<.001.
Note. Percent time = the percent of the child’s life spent in institutional care through age 12 years. DSED = Disinhibited Social Engagement Disorder
Placement disruptions and male sex predicted poorer general social functioning in the first step of the model. Once signs of RAD were added in the second step, only male sex and signs of RAD significantly predicted poorer general social functioning. Neither the covariates nor signs of RAD predicted scores on the peer conflict, caregiver views as a social victim, or teacher views as a social victim factors. Signs of RAD were the only predictor of poorer social competence.
In regard to DSED, Placement disruptions and male sex predicted poorer general social functioning in the first step of the model. Once signs of DSED were added in the second step, male sex and placement disruptions remained significant predictors of poorer general social functioning along with sings of DSED. Signs of DSED were the only significant predictor of higher scores on the caregiver views as a social victim factor and lower scores on the social competence factor.
Discussion
Signs of RAD and DSED were examined in relation to general and specific domains of social functioning in early adolescence. Social functioning domains were identified using bi-factor modeling, which revealed a General Social Functioning factor and four specific factors: Peer Conflict, Caregiver Views as Victim, Teacher Views as Victim, and Social Competence. Signs of RAD and DSED were associated with lower scores on the General Social Functioning and Social Competence factors. Furthermore, signs of DSED, but not RAD, were associated with higher scores on the Caregiver Views as Victim factor. Additional analyses revealed that signs of RAD and DSED explained variance in the General Social Functioning and Social Competence factors above and beyond the percentage of time children spent in institutional care and the number of placement disruptions after initially leaving the institution, indicating that the observed associations with signs of attachment disorders are not simply a proxy for adverse caregiving experiences.
This is the first study to examine domains of social functioning from the perspective of multiple reporters. The bi-factor model approach allowed us to include both caregiver and teacher reports of social functioning and to extract multiple specific domains of social functioning to examine in relation to RAD and DSED. Associations between signs of RAD and DSED and social functioning were revealed across the multiple domains of social functioning, highlighting the importance of exploring multiple factors of social functioning through bi-factor modeling. This is also the first study to relate signs of both RAD and DSED to social functioning. The hypothesis that signs of RAD and DSED would be associated with general difficulties in social functioning (i.e., across domains and reporters) was supported. Both signs of RAD and DSED were strongly associated with poorer general social functioning. Additionally, signs of both RAD and DSED were found to be associated with poorer social competence and only DSED signs were associated with greater caregiver’s perceived victimhood in social situations. Our findings mirror past work demonstrating associations between DSED and poorer peer relationships (e.g., Moran, McDonald, Jackson, Turnbull, & Minnis, 2017; Sonuga-Barke, Schlotz, & Kreppner, 2010).
One aim of our study was to probe for whether signs of RAD and DSED are associated with different domains of social functioning, given the unique behavioral presentations of each disorder. Signs of DSED and RAD were both associated with deficits on the General Social Functioning and Social Competence factors. However, adolescents showing signs of DSED were rated by their caregivers as having conflictual peer relationships and were often bullied (Caregiver Views as Victim factor) whereas adolescents with signs of RAD did not seem to have these same social difficulties. Adolescents with signs of DSED may be particularly prone to conflictual peer difficulties relationships compared to adolescents with signs of RAD due to the difference in presentation between the two disorders. Namely, children with DSED appear to seek out relationships with others, whereas children with RAD are more inhibited and tend to withdraw from relationships (Gleason et al., 2011). Furthermore, adolescents with DSED tend to be socially inappropriate (e.g., oversharing intimate details about themselves) and intrusive (e.g., approaching without invitation) in their interactions with adults. Roy and colleagues (2004) reported that children with signs of DSED were as indiscriminant in their interactions with peers as they were with adults, which may lead to conflict with peers. This intrusive social behavior may cause conflict in peer relationships and leave adolescents vulnerable to potential victimization by peers and social rejection.
Time spent in institutional care was not related to social functioning in early adolescence in our sample. Placement disruptions were associated with poorer general social functioning, however, signs of RAD and DSED predicted poorer general social functioning above the effect of placement disruptions. Therefore, our findings suggest that, among adolescents with a history of institutional care, signs of RAD and DSED, rather than merely being markers of more severe institutional care histories or adverse post-placement experiences, may be uniquely important in explaining difficulties in social functioning. Similarly, the English and Romanian Adoptees Study (ERAS) demonstrated that in both childhood and adolescence, length of exposure to deprivation in an institutional setting was not as strongly associated with peer problems when controlling for signs of DSED or other deprivation-specific disorders (O’Connor & Rutter, 2000; Sonuga-Barke et al., 2010). Therefore, although past work has extensively documented poorer social functioning among children and adolescents with a history of institutional care, more recent findings, as we have reported here as well the results reported by Sonuga-Barke and colleagues (2010), suggest that the development of attachment disorders like RAD and DSED may be stronger predictors of poor social functioning than duration of exposure to institutional care.
While sex differences were found in general social functioning, such that girls, on average, had higher scores than boys, such differences were not examined by attachment disorders. Sex remained a significant predictor of general social functioning even after accounting for signs of RAD and DSED.
Clinical Implications
Young adolescents with signs of RAD and/or DSED are at risk for social disturbances that extend beyond the core features of their disorders. Treatment of children with signs of these disorders should be comprehensively aimed not only at core features of the disorders, such as emotional withdrawal or social impulsivity, but also at broader social functioning with peers and adults. Beyond attempting to prevent early life deprivation and the development of subsequent psychopathology, interventions aimed at improving social functioning among previously institutionalized adolescents with signs of RAD or DSED may also be useful. Our findings suggest that both positive (e.g., assertion, self-control, cooperation) as well as negative (e.g., peer conflict, relational victimization) aspects of social functioning may be useful targets of intervention. However, targeting social functioning may be particularly challenging given that adolescents with a history of institutional care underreport social difficulties compared to parents and teachers, and may have poor insight into their social functioning (Caprin et al., 2017; Moran et al., 2017). Furthermore, evidence for the effectiveness of interventions targeting social skills and functioning with children presenting with other forms of psychopathology such as autism and other pervasive developmental disorders is mixed, with many studies reporting minimal effectiveness (Bellini, Peters, Benner, & Hopf, 2007; Koenig, De Los Reyes, Cicchetti, Scahill, & Klin, 2009; Rao, Beidel, & Murray, 2008). Nevertheless, the clinical imperative for children with signs of these disorders should be to attempt to enhance their social functioning.
Limitations
One limitation of our work is that we did not include reports from the adolescents themselves. While including both caregiver and teacher reports provided benefits to multiple informants, reports from adolescents could provide additional, complimentary information. Yet, given that young children and especially those with a history of institutional care may have poor insight into their social difficulties (Caprin et al., 2017), it is not clear whether the additional reporter would be additive. Another limitation is that only signs and not diagnoses of RAD and DSED were examined. Clearly greater attachment disorder signs were associated with more difficulties, and this approach allows us to examine variation in the non-clinical level, but it remains unclear whether a diagnosis of RAD or DSED is a necessary threshold for observing deficits in social functioning.
It is important to note that we only reported on the social functioning of the children in the present study at the follow-up occurring at approximately age 12 years. Although social problems are likely evident earlier in life for the children in our sample, unfortunately, we do not have a comprehensive assessment of social functioning in early life, when these symptoms are first evident. Equivalent measures of social functioning earlier in life would have allowed for exploration of potential timing and trajectories of social functioning across development in relation to RAD and DSED. We anticipate that social difficulties would present earlier than age 12 years.
Finally, while this study focused on signs of attachment disorders and social functioning in children with a history of institutional care, it is likely that other domains of psychopathology and early life adversity are relevant. For example, symptoms of attention-deficit/hyperactivity disorder (ADHD), a common behavioral phenotype found in children with a history of deprivation, as well as experiences of childhood maltreatment have been associated with deficits in social functioning reported by both caregivers and teachers (Humphreys, Gabard-Durnam, et al., 2017; Rogosch, Cicchetti, & Aber, 1995). The issue of comorbidity between signs of RAD and DSED and other forms of psychopathology in the prediction of social functioning could be important. We considered adjusting for internalizing and externalizing signs of psychopathology in the regression models, however, we were mindful of Kraemer’s (2015) caution that adding covariates post hoc can lead to false conclusions about the relations being studied, and furthermore covarying potential pathways by which attachment disorder symptoms may predict social functioning (e.g., through other forms of psychopathology) is a statistical practice that results in reduced estimation of direct effects. Future studies should explore other forms of psychopathology both as predictors of social functioning as well as potential mediating variables in the relationship between signs of RAD and DSED and social functioning.
Conclusion
Studies of RAD and DESD beyond early childhood are limited though they appear to be increasing in the past few years. Our results indicate that signs of RAD and DSED are associated with deficits in social functioning in early adolescents. Of these attachment disorders, signs of DSED are additionally associated with increased reports of social victimization and conflicted peer relationships. Although institutional care is a necessary condition for the development of signs of RAD and DSED, our findings suggest signs of attachment disorder more strongly predict poor social functioning than duration of exposure to institutional care.
Acknowledgements:
This research was supported by the John D. and Catherine T. MacArthur Foundation Research Network on “Early Experience and Brain Development” (Charles A. Nelson, Ph.D., Chair), NIMH (1R01MH091363; Nelson) (F32MH107129; Humphreys), Brain & Behavior Research Foundation (formerly NARSAD) Young Investigator Award 23819 (Humphreys), and Klingenstein Third Generation Foundation Fellowship (Humphreys).
References
- Ablow JC, Measelle JR, Kraemer HC, Harrington R, Luby J, Smider N, … Kupfer DJ (1999). The MacArthur three city outcome study: Evaluating multi-informant measures of young children’s symptomatology. Journal of The American Academy of Child And Adolescent Psychiatry, 38(12), 1580–1590. doi: 10.1097/00004583-199912000-00020 [DOI] [PubMed] [Google Scholar]
- Ainsworth MS (1979). Infant–mother attachment. American Psychologist, 34(10), 932–937. doi: 10.1037/0003-066X.34.10.932 [DOI] [PubMed] [Google Scholar]
- Almas AN, Degnan KA, Radulescu A, Nelson CA, Zeanah CH, & Fox NA (2012). Effects of early intervention and the moderating effects of brain activity on institutionalized children’s social skills at age 8. Proceedings of the National Academy of Sciences, 109(Supplement_2), 17228–17231. doi: 10.1073/pnas.1121256109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association; (2013). DSM-5: Diagnostic and Statistical Manual of Mental Disorders, 5th edition Diagnostic and Statistical Manual of Mental Disorders 4th edition TR. Arlington, VA: American Psychiatric Publishing; Retrieved from https://books.google.com/books?hl=de&lr=&id=-JivBAAAQBAJ&pgis=1 [Google Scholar]
- Bellini S, Peters JK, Benner L, & Hopf A (2007). A meta-analysis of school-based social skills interventions for children with autism spectrum disorders. Remedial and Special Education, 28(3), 153–162. doi: 10.1177/07419325070280030401 [DOI] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. doi: 10.1037/0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1995). EQS structural equations program manual. Encino, CA: Multivariate Software. [Google Scholar]
- Bowlby J (1969). Attachment and loss. 1. Attachment. New York, NY: Basic Books; Retrieved from https://books.google.co.in/books?id=FYEuAAAAMAAJ [Google Scholar]
- Brown BB, & Larson J (2009). Peer relationships in adolescence In Lerner RM & Steinberg L (Eds.), Handbook of adolescent psychology, volume 2: Contextual influences on adolescent development (3rd ed., pp. 74–103). Hoboken, NJ, USA: John Wiley & Sons, Inc. doi: 10.1002/9780470479193.adlpsy002004 [DOI] [Google Scholar]
- Caprin C, Benedan L, Ballarin L, & Gallace A (2017). Social competence in Russian post-institutionalized children: A comparison of adopted and non-adopted children. Children and Youth Services Review, 75, 61–68. doi: 10.1016/j.childyouth.2017.02.020 [DOI] [Google Scholar]
- Essex MJ, Boyce WT, Goldstein LH, Armstrong JM, Kraemer HC, Kupfer DJ, & Group MABW (2002). The confluence of mental, physical, social, and academic difficulties in middle childhood. II: developing the Macarthur health and Behavior Questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 41(5), 588–603. doi: 10.1097/00004583-200205000-00017 [DOI] [PubMed] [Google Scholar]
- Fonagy P, Steele M, Moran G, Steele H, & Higgitt A (1993). Measuring the ghost in the nursery: An empirical study of the relation between parents’ mental representations of childhood experiences and their infants’ security of attachment. Journal of the American Psychoanalytic Association, 41(4), 957–989. doi: 10.1177/000306519304100403 [DOI] [PubMed] [Google Scholar]
- Gleason MM, Fox NA, Drury SS, Smyke AT, Nelson CA, & Zeanah CH (2014). Indiscriminate behaviors in previously institutionalized young children. Pediatrics, 133(3), e657–65. doi: 10.1542/peds.2013-0212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleason MM, Fox NA, Drury S, Smyke AT, Egger HL, Nelson CA, … Zeanah CH (2011). Validity of evidence-derived criteria for reactive attachment disorder: Indiscriminately social/disinhibited and emotionally withdrawn/inhibited types. Journal of the American Academy of Child and Adolescent Psychiatry, 50(3), 216–231. doi: 10.1016/j.jaac.2010.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gresham FM, & Elliott SN (1990). Social skills rating system (SSRS). American Guidance Service. [Google Scholar]
- Gresham FM, Elliott SN, Vance MJ, & Cook CR (2011). Comparability of the Social Skills Rating System to the Social Skills Improvement System: Content and psychometric comparisons across elementary and secondary age levels. School Psychology Quarterly, 26(1), 27–44. doi: 10.1037/a0022662 [DOI] [Google Scholar]
- Guyon-Harris KL, Humphreys KL, Degnan KA, Fox NA, Nelson CA, & Zeanah CH (2018). A prospective study of reactive attachment disorder following early institutional care: Considering variable- and person-centered approaches. Attachment & Human Development. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyon-Harris KL, Humphreys KL, Fox NA, Nelson CA, & Zeanah CH (2018). Course of disinhibited social engagement disorder from early childhood to early adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 57(5), 329–335. doi: 10.1016/j.jaac.2018.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges J, & Tizard B (1989). Social and family relationships of ex‐institutional adolescents. Journal of Child Psychology and Psychiatry, 30(1), 77–97. doi: 10.1111/j.1469-7610.1989.tb00770.x [DOI] [PubMed] [Google Scholar]
- Holzinger KJ, & Swineford F (1937). The Bi-factor method. Psychometrika, 2(1), 41–54. doi: 10.1007/BF02287965 [DOI] [Google Scholar]
- Humphreys KL, Gabard-Durnam L, Goff B, Telzer EH, Flannery J, Gee DG, … Tottenham N (2017). Friendship and social functioning following early institutional rearing: The role of ADHD symptoms. Manuscript under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Nelson CA, Fox NA, & Zeanah CH (2017). Signs of reactive attachment disorder and disinhibited social engagement disorder at age 12 years: Effects of institutional care history and high-quality foster care. Development and Psychopathology, 29(2), 675–684. doi: 10.1017/S0954579417000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig K, De Los Reyes A, Cicchetti D, Scahill L, & Klin A (2009, August 27). Group intervention to promote social skills in school-age children with pervasive developmental disorders: Reconsidering efficacy. Journal of Autism and Developmental Disorders. doi: 10.1007/s10803-009-0728-1 [DOI] [PubMed] [Google Scholar]
- Lee IA, & Preacher KJ (2013). Calculation for the test of the difference between two dependent correlations with one variable in common [Computer software]. Retrieved from http://quantpsy.org
- Marsee MA, Barry CT, Childs KK, Frick PJ, Kimonis ER, Muñoz LC, … Lau KSL (2011). Assessing the forms and functions of aggression using self-report: Factor structure and invariance of the Peer Conflict Scale in youths. Psychological Assessment, 23(3), 792–804. doi: 10.1037/a0023369 [DOI] [PubMed] [Google Scholar]
- Marsee MA, & Frick PJ (2007). Exploring the cognitive and emotional correlates to proactive and reactive aggression in a sample of detained girls. Journal of Abnormal Child Psychology, 35(6), 969–981. doi: 10.1007/s10802-007-9147-y [DOI] [PubMed] [Google Scholar]
- McCall RB, Muhamedrahimov RJ, Groark CJ, Palmov OI, Nikiforova NV, Salaway J, & Julian MM (2015). The development of postinstitutionalized versus parent-reared Russian children as a function of age at placement and family type. Development and Psychopathology, 28(1), 251–264. doi: 10.1017/S0954579415000425 [DOI] [PubMed] [Google Scholar]
- Miller FG (2009). The randomized controlled trial as a demonstration project: An ethical perspective. American Journal of Psychiatry, 166(7), 743–745. doi: 10.1176/appi.ajp.2009.09040538 [DOI] [PubMed] [Google Scholar]
- Millum J, & Emanuel EJ (2007). The ethics of international research with abandoned children. Science, 318(5858), 1874–1875. doi: 10.1126/science.1153822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran K, McDonald J, Jackson A, Turnbull S, & Minnis H (2017). A study of Attachment Disorders in young offenders attending specialist services. Child Abuse and Neglect, 65, 77–87. doi: 10.1016/j.chiabu.2017.01.009 [DOI] [PubMed] [Google Scholar]
- Nelson CA, Fox NA, & Zeanah CH (2014). Romania’s Abandoned Children: Deprivation, Brain Development, and the Struggle for Recovery. Cambridge, MA: Harvard University Press. [Google Scholar]
- O’Connor TG, & Rutter M (2000). Attachment disorder behavior following early severe deprivation: Extension and longitudinal follow-up. Journal of the American Academy of Child & Adolescent Psychiatry, 39(6), 703–712. doi: 10.1097/00004583-200006000-00008 [DOI] [PubMed] [Google Scholar]
- Rao PA, Beidel DC, & Murray MJ (2008, February 20). Social skills interventions for children with Asperger’s syndrome or high-functioning autism: A review and recommendations. Journal of Autism and Developmental Disorders. Springer US. doi: 10.1007/s10803-007-0402-4 [DOI] [PubMed] [Google Scholar]
- Reise SP, Moore TM, & Haviland MG (2010). Bifactor models and rotations: Exploring the extent to which multidimensional data yield univocal scale scores. Journal of Personality Assessment, 92(6), 544–559. doi: 10.1080/00223891.2010.496477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rid A (2012). When is research socially valuable? Lessons from the Bucharest Early Intervention Project: Commentary on a case study in the ethics of mental health research. Journal Of Nervous And Mental Disease, 200(3), 248–249. doi: doi:10.1097/NMD.0b013e318247d124 [DOI] [PubMed] [Google Scholar]
- Rogosch FA, Cicchetti D, & Aber JL (1995). The role of child maltreatment in early deviations in cognitive and affective processing abilities and later peer relationship problems. Development and Psychopathology, 7(04), 591. doi: 10.1017/S0954579400006738 [DOI] [Google Scholar]
- Roy P, Rutter M, & Pickles A (2004). Institutional care: Associations between overactivity and lack of selectivity in social relationships. Journal of Child Psychology and Psychiatry and Allied Disciplines, 45(4), 866–873. doi: 10.1111/j.1469-7610.2004.00278.x [DOI] [PubMed] [Google Scholar]
- Schmid J, & Leiman JM (1957). The development of hierarchical factor solutions. Psychometrika, 22(1), 53–61. doi: 10.1007/BF02289209 [DOI] [Google Scholar]
- Smyke AT, Zeanah CH, Fox NA, & Nelson CA (2009). A new model of foster care for young children: the Bucharest early intervention project. Child and Adolescent Psychiatric Clinics of North America, 18, 721–34. doi: 10.1016/j.chc.2009.03.003 [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Kennedy M, Kumsta R, Knights N, Golm D, Rutter M, … Kreppner J (2017). Child-to-adult neurodevelopmental and mental health trajectories after early life deprivation: the young adult follow-up of the longitudinal English and Romanian Adoptees study. The Lancet, 389(10078), 1539–1548. doi: 10.1016/S0140-6736(17)30045-4 [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJ, Schlotz W, & Kreppner J (2010). Differentiating developmental trajectories for conduct, emotion, and peer problems following early deprivation. Monographs of the Society for Research in Child Development, 75(1), 102–124. doi: 10.1111/j.1540-5834.2010.00552.x [DOI] [PubMed] [Google Scholar]
- Steiger JH (1990). Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research, 25(2), 173–180. doi: 10.1207/s15327906mbr2502_4 [DOI] [PubMed] [Google Scholar]
- Tarullo AR, & Gunnar MR (2005). Institutional rearing and deficits in social relatedness: Possible mechanisms and processes. Cognition, Brain, Behavior, IX(3), 329–342. Retrieved from http://www.bu.edu/cdl/files/2013/08/Tarullo-Gunnar-2005.pdf [Google Scholar]
- Tizard B, & Hodges J (1978). The effect of early institutional rearing on the development of eight year old children. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 19(2), 99–118. doi: 10.1111/j.1469-7610.1978.tb00453.x [DOI] [PubMed] [Google Scholar]
- Tucker LR, & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. doi: 10.1007/BF02291170 [DOI] [Google Scholar]
- Wiik KL, Loman MM, Van Ryzin MJ, Armstrong JM, Essex MJ, Pollak SD, & Gunnar MR (2011). Behavioral and emotional symptoms of post-institutionalized children in middle childhood. Journal of Child Psychology and Psychiatry, 52(1), 56–63. doi: doi: 10.1111/j.1469-7610.2010.02294.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah CH (2000). Disturbances of attachment in young children adopted from institutions. Journal of Developmental and Behavioral Pediatrics, 21(3), 230–6. Retrieved from https://www.researchgate.net/profile/Charles_Zeanah/publication/12434999_Disturbances_of_attachment_in_young_children_adopted_from_institutions/links/54c11e290cf25b4b8071b6b4.pdf [PubMed] [Google Scholar]
- Zeanah CH, Fox NA, & Nelson CA (2012). The Bucharest Early Intervention Project: case study in the ethics of mental health research. The Journal of Nervous and Mental Disease, 200(3), 243–7. doi: 10.1097/NMD.0b013e318247d275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah CH, & Gleason MM (2015). Annual research review: Attachment disorders in early childhood - Clinical presentation, causes, correlates, and treatment. Journal of Child Psychology and Psychiatry and Allied Disciplines, 56(3), 207–222. doi: 10.1111/jcpp.12347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah CH, Nelson CA, Fox NA, Smyke AT, Marshall P, Parker SW, & Koga S (2003). Designing research to study the effects of institutionalization on brain and behavioral development: The Bucharest Early Intervention Project. Development and Psychopathology, 15(04), 885–907. doi: 10.1017/S0954579403000452 [DOI] [PubMed] [Google Scholar]
- Zeanah CH, Smyke AT, Koga SF, & Carlson E (2005). Attachment in institutionalized and community children in Romania. Child Development, 76(5), 1015–28. doi: 10.1111/j.1467-8624.2005.00894.x [DOI] [PubMed] [Google Scholar]
- ZERO TO THREE. (2016). DC:0–5TM: Diagnostic classification of mental health and developmental disorders of infancy and early childhood. Washington, DC: Author. [Google Scholar]