Abstract
Background:
Community-Based Participatory Research (CBPR) is used to guide the design and evaluation of programs aimed at addressing complex health issues. Effective administrative management of CBPR projects is essential to ensuring the success and fidelity of these programs.
Objective:
We identify an administrative framework to support the implementation and management of a community-academic CBPR initiative.
Methods:
The Barbershop Talk with Brothers (BTWB) project was a cluster randomized CBPR intervention designed to reduce HIV among high-risk heterosexual men. Eight-hundred and sixty men, representing 51 barbershops, participated in the project.
Results:
The 3Ps framework is defined by: 1) Partnership, 2) Product, and 3) Process. We describe the implementation of the 3Ps through applied examples including partnership management strategies, planning of shared resources, and flexible budgeting that can support the unique infrastructure of a shared community-academic project.
Conclusion:
The 3Ps are a translatable framework for comparable shared community-academic research projects to adopt.
Keywords: Community Based Participatory Research, community engagement, community partnership, project management
INTRODUCTION
Community-based participatory research (CBPR) first emerged in the 1950’s to bridge then-conventional, clinical research with knowledge attained by engaging community members as equitable partners in the development, implementation, and dissemination of research 1. Community members possess expertise on their community’s health, assets, and needs, which both enhances research focus and ensures prioritization of community-oriented questions that might be approached through research programs. Throughout the past decade, CBPR has been utilized in many health disciplines as an approach to tackle complex public health problems alongside affected communities 2–7.
Increasingly, CBPR has been integrated into health profession curricula to train future public health practitioners in the application of CBPR, and funding has been provided for CBPR-focused interventions 1,2,6,8,9. The literature includes many examples of using CBPR to identify research questions and in formative evaluation work to develop public health strategies to address social and behavioral health interventions and policy development 1,10. Less frequently described are methods of managing and conducting process evaluations of CBPR projects themselves, particularly in regard to larger scale projects with experimental designs. Due to the qualitative nature of CBPR, these administrative and operational components of implementation often prove challenging to researchers 3,11. Here, we detail an approach to the administration of a community-academic CBPR project conducted in a non-traditional setting.
We aim to (i) present an administrative framework and describe its alignment with the tenets of CBPR, and (ii) describe components of the implementation of the administrative framework with the intervention as a case study.
METHODS
Overview of the BTWB Community-Research Project
The Barbershop Talk with Brothers (BTWB) project was a cluster randomized trial funded by the National Institute of Minority Health and Health Disparities. BTWB was designed following a multi-year, CBPR approach to developing a program to reduce sexual risk behavior and disparities in HIV in Black, heterosexual men who do not inject drugs 12,13. The evaluation for the program involved recruitment of 51 community-based barbershops; 22 of these shops were randomly assigned to receive the group-based BTWB intervention, and the remaining shops received a group-based attention control condition focused on cancer screening and treatment. Barbershops were selected from neighborhoods in Central Brooklyn, characterized by high poverty and high rates of HIV incidence. The study enrolled 860 men from participating barbershops from November 2012 through July 2016. Participants were engaged in study activities consistent with barbershop assignment and completed evaluation via a baseline, three-month, and six-month audio computer assisted structured interview (ACASI). The study was approved by the Institutional Review Board (#FWA00003624) and all study participants consented prior to data collection.
Building the Community-Academic Partnership
BTWB represents a collaboration between investigators at the School of Public Health (SPH) at SUNY Downstate Medical Center (DMC), and community partners at the Arthur Ashe Institute for Urban Health (AAIUH), Inc., the Brooklyn Health Disparities Center (BHDC), the Brooklyn Borough President’s Office, and a Community Advisory Board (CAB). The CAB functioned as our Steering Committee and was comprised of a team of 23 members representing the academic, partner organization, and community. From the academic team was the Principle Investigator (PI), a co-investigator, and three staff. From our partner organization, this included one co-investigator and 7 field staff. From the community, this consisted of 2 barbers, 4 barbershop owners, 2 hair stylists, 1 representative from a faith-based organization serving our neighborhoods, and 1 member representing our priority population. The volunteers were compensated for their travel expenditures as part of the CAB, and lunch was provided at most meetings.
Four principals served as the foundation for developing and maintaining the community-academic partnership. These included: 1) identifying collaborators; 2) assessing the compatibility of the potential collaborating entity; 3) formalizing the collaboration; and 4) co-planning program activities. In keeping with the tenets of CBPR, BTWB’s infrastructure included shared management of the project by the community-academic partners14,15. Both entities maintained separate staff who shared responsibilities for recruitment, retention, and intervention delivery. Personnel from each agency maintained continuous communication and met regularly to ensure project objectives were being met. The Consolidated Standards of Reporting Trials (CONSORT) guidelines were used to structure the project and data collection across partners16.
Development of the Administrative Framework: the 3Ps
To support the aim of describing the development of the administrative framework, we outline the framework defined by the 3Ps. The 3Ps are 1) Partnership, 2) Product, and 3) Process. The 3Ps framework maps key management components of the shared community-academic partnership of the BTWB project. Throughout the life of the project, the 3Ps were identified through encountered barriers to project implementation. The mapped process informs the relationships of the shared community-academic partnership, allowing for efficient management of the CBPR model (Figure 1).
Figure 1:
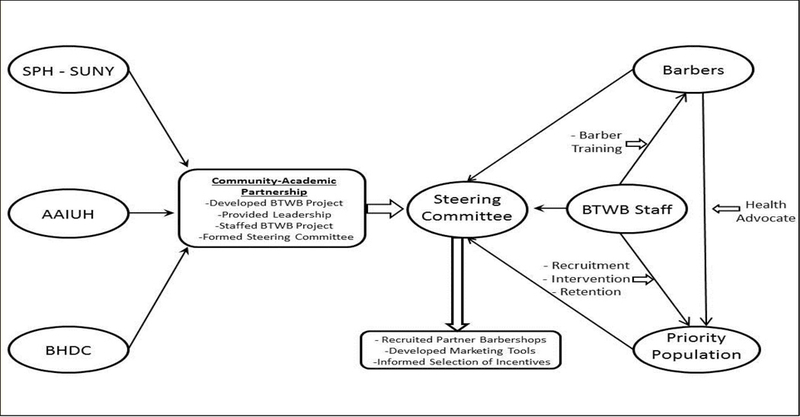
This diagram depicts the interrelationship of the BTWB program partners and their respective roles.
As the 3Ps were developed, we ensured alignment of each domain with core principles of CBPR2, thereby increasing fidelity of the project to these core principles. For the BTWB project, we embedded the 9 CBPR principles in the implementation of the project’s administration. Table 1 delineates the relationship between the 3Ps and Principles of CBPR and notes specific project management components that align with the framework’s domains.
Table #1:
Relationship between 3P model components, CBPR core elements, and practical applications in the BTWB project.
| 3Ps | CBPR Principle | BTWB Examples |
|---|---|---|
| Partnership | Community is the unit of identity. Facilitates a collaborative, equitable partnership in all phases of the research, involving an empowering and power-sharing process that attends to social inequalities; Fosters co-learning and capacity building among all partners; Builds on strengths and resources within the community. |
Partnering with Barbershops in shared local community to accomplish a central goal. Community academic partnership; Steering Committee: Incorporating equitable input from Project Leaders, Study Staff, Barbers, Participants and Community Members at large into project design. Staff, and barbers, as well as project participants learning and drawing from each others’ knowledge and experiences to for example shorten the surveys, and increase staffing. Resources were leverage through our partnership with the Brooklyn Disparities Center, who was able to provide a joint office space for the BTWB project |
| Product | Focuses on Problems relevant to the local community Integrates and achieves a balance between knowledge generation and intervention for mutual benefit of all partners; Involves systems development using a cyclical and iterative process; |
Intervention designed to decrease sexual health risk in priority population. Barbers Trainings: Detailed trainings designed to increase buy- in from community partners and communicate project aims. Co-Branding: All project materials signify the community-academic partnership nature of project. |
| Process | Disseminates results to all partners and involves them in the dissemination process; Involves a long-term process and commitment to sustainability. |
BTRACK: Utilization of a customized tracking database. RRCM: Utilization of community champions as consultants to assist in recruitment and retention activities. |
RESULTS
Here, we describe application of the 3Ps with direct examples from the BTWB project. Examples are meant to be illustrative of how the 3Ps may be used to translate the principles of CBPR to actionable project administration.
Implementation Example: Partnership
A core component of a community-engaged project is partnership across research entities, which is vital to ensuring that the culture, norms, resources, and needs of the community are adequately represented in the research. To guide the BTWB project, researchers from SPH-SUNY and the AAIUH leveraged existing relationships to form the Steering Committee. Members of the Steering Committee were tasked with specific deliverables. For example, barbers were tasked with making recommendations on potential shops to enroll for the BTWB project, as well as providing recommendations to optimize recruitment activities including types of incentives. The partnership milestone was measured by signed MOUs from 52 barbershops (1 later declined to participate), yielding participation from 225 barbers. Barbershops that agreed to take part in the BTWB project benefited in several ways. Benefits included being provided with specialized training for their barbers to equip them with skills to discuss important health issues and experiences with their clients and the motivation to engage their clients about the program17.
The community partner, AAIUH, facilitated entry to barbershops, and the SPH-SUNY academic partner provided an established infrastructure to carry out the complex research initiative 18,19. To ensure a balance in the scope of work, all project activities were mirrored across both SPH-SUNY and the AAIUH staff. For example, there were investigators, project managers, interventionists, and field staff representing all organizations. Staff from both organizations worked together on activities related to their respective roles. To address challenges associated with sharing space across multiple organizations, a joint office space was created at the BHDC where the SPH-SUNY and the AAIUH teams conducted project activities ensuring that relevant information was shared.
To bolster partnership among entities and engagement in the BTWB project, a series of formal and informal meetings were scheduled with both groups. This format provided an opportunity for partners to learn from each other’s experiences in the field, and to share possible solutions to address challenges and barriers. For example, at the outset of the project, Field Researchers reported that study participants voiced concern that the outcome evaluation surveys were too lengthy, hypothesizing that study participants were less likely to participate in the study because of the time commitment. As a result, the survey was shortened to address the potential barrier while maintaining the integrity of core research questions. During the first year of the BTWB project, the SPH-SUNY and AAIUH team met twice a month reducing meetings to an as-need basis after full implementation. Investigators and project managers visited shops throughout the project period to monitor project status and ensure partners were engaged and that idea exchange was still occurring. Additionally, during the lifespan of the project, Steering Committee meetings were convened twice annually with the community partners. Agenda items were generated by the community partners in consort with the BTWB investigative team.
Implementation Example: Product
It is important to recognize that in the CBPR model, research findings alone are not the sole product. Rather, the project itself is part of the CBPR product. Here, our product included the shared experience of partner barbershops, participants, and staff. Training barbers not only generated knowledge, but also promoted self-efficacy to address personal health problems and reinforce their value as community advocates 20. These experiences ultimately created the product of the BTWB brand and built community capacity.
At the core of a successful product is the tenet of shared ownership among the community-academic partners 1. This tenet is echoed in the BTWB project where both teams, working collaboratively, created a sense of independence and ownership of the project. One of the ways our approach addressed joint ownership of the BTWB project was through the collaborative production of marketing materials. To increase awareness and provide transparency the AAIUH and SPH-SUNY team worked with the Steering Committee members to actualize the brand as a unified project with increased visibility in the community. The Steering Committee also played an integral role in the selection of the incentive and marketing tools (Appendix A). With a major component of the intervention being the communication of health information, a set of marketing tools including poster flyers, postcards, t-shirts, and barber capes with the project logo served as a tool to start these conversations. Tangible gifts not only incentivized participation, but created buy-in within the communities being reached 21. The increased visibility and the utilization of the posters, flyers, and postcards displayed in the barbershop reinforced the legitimacy of project participation for potential study participants.
Social media was also explored as a tool to promote joint ownership in the BTWB project. A Facebook page was created to keep project participants engaged and aware of program activities online, with both the community and academic partners co-creating content. However, our experience was that study participants’ use of the BTWB Facebook page was limited, and that the cost and time involved in keeping the page active was beyond our resources. Here our learned lesson was that to keep an active social media presence a dedicated staff person is required to identify and post new and relevant information on the site and actively engage with the BTWB study participants. For future researchers where staff time is mostly allocated to field activities, we recommend that the development and maintenance of social media platforms be budgeted separately.
Implementation Example: Process
The third domain of the 3Ps Framework focuses on the process by which project activities are managed. In the BTWB project, the primary activities include data management (which includes data collection, submission, and tracking) and flexible budgeting. While these activities are often considered background to the intervention, they play a critical role in ensuring that the CBPR approach and project protocol are effectively implemented and that resources are accounted for.
Data Management
We used a customized data tracking system, named “BTRACK”, which was developed during the first year of the project to track all components of the study and to merge information from multiple organizations. Program staff worked collaboratively with a programmer to map out the project activities and tracking needs. The programmer adapted the project’s study components into a tracking system with an intuitive layout. Features of the BTRACK database include error reduction safeguards using logic, skip, and fill data validation that limits error rate of data entry. Establishing a tracking system up-front saved money by streamlining data management, and reducing the time and cost associated with staff entering data, maintaining and tracking records (Figure 2 and Table 2). Partner institutions were able to view and edit information in BTRACK, increasing transparency and communication.
Figure 2:

BTRACK Interface
Table 2:
Core data elements and summary capabilities of BTRACK system for process evaluation of BTWB project.
| Participants | Breakdown of all individuals who conducted a screener by study ID |
| Workshops | Breakdown of enrolled participants by workshop attended. |
| Approaches | Breakdown of individuals approached to conduct screener by recruitment visit |
| Schedule | Outline of enrolled participants follow-up windows |
| Screeners | Verification of screeners entered as completed with data file |
| Barbershops | Breakdown of all participating barbershops and barbers trainings |
| Staff | Breakdown of all staff on project. |
| Reconciliations | Tracking and reporting of Incentive, Food, and Travel disbursement |
| Activities | Tracking and reporting of program activities by date. |
| Interviews | Verification of interview entered as completed with data file |
The BTWB project utilized Audio Computer-Assisted Self Interviewing (ACASI) software for data collection to expand opportunities for assessing populations with low literacy and assessing sensitive or potentially stigmatizing behaviors such as unprotected sexual risk behavior 22–24. ACASI data were integrated into the BTRACK system.
The BTRACK system also included separate modules to track staff, study sites, the number of barbers per study site, the number of barbers trained at each study site, the study participants’ incentives disbursement/reconciliation, and the study participants’ enrollment, intervention, and follow-up status. A scheduler and customized real-time reporting platform was available. This multi-user program allowed simultaneous and real time access to project personnel. Tasks were easily distributed among staff to conduct data entry and generate a series of queries (Figures 3 & 4).
Figure 3:

Sample BTRACK Data Entry Screen
Figure 4:

Sample BTRACK Study Participant Incentive Reconcilliation Report
Flexible Budgeting for Recruitment and Retention
To address the complexities of partnership as well as emerging challenges, we found flexibility in budgeting to be critical. While maintaining funder requirements, we sought to promote flexibility in our budget to meet changing project needs. Beginning in the fourth year, for instance, project funds were made available to pilot test a Recruitment/Retention Consulting Model (RRCM). Consultants hired under the RRCM were tasked with the one distinct duty of recruitment except one who was tasked with both recruitment and retention activities. An added advantage to this model was that consultants were both representatives of the priority populations and residents of Brooklyn and used their community knowledge and expertise to conduct program activities in a culturally sensitive and relatable manner 25–27.
Despite the utility of the RRCM, limitations existed. A high turnover rate for consultants may be experienced due to the respective consultant’s personal schedule. Most BTWB consultants were also enrolled in college or graduate level programs, thus their availability fluctuated along with academic calendars. A joint process was used where both SPH-SUNY and AAIUH staff were involved in the selection and training of the consultants. Additionally, SPH-SUNY funded the RRCM consultants and therefore provided supervision and was responsible for consultants’ contracts and regulatory affairs. The RRCM has proven to be successful since implementation by increasing enrollment and retention outcomes while containing cost. Without a flexible budgeting mechanism the RRCM could not have been implemented.
DISCUSSION
Researchers engaged in CBPR programs can utilize the 3Ps and lessons learned through this project to inform the implementation of administrative aspects of similar shared community-academic partnerships. The development of the 3Ps framework contributes to the advancement of infrastructure-focused literature for CBPR projects. The structure of the 3Ps framework was designed to provide the administrative underpinnings of the BTWB project and ensure that it would be possible to gather and report on successful results. A series of project management strategies including communicating on a regular basis with staff through formal and informal mechanisms; developing joint marketing materials; setting up a tracking database with reporting to all collaborators; and utilizing a flexible budget mechanism allowed for the BTWB project to be delivered effectively across partners.
Recommendations for future application of the 3Ps
Given the nature of CBPR projects, there is no one-size-fits all approach for the administrative design of projects. Thus, we recommend using the 3Ps to guide, but not prescribe, administrative strategies for future CBPR projects. Part of the initial planning process should include assessing the CBPR tenets most aligned with the project and then aligning the principles with the 3Ps framework. The consideration of the 3Ps should be taken at the onset of the project and with input from all project partners and may be used in tandem with CONSORT guidelines for projects using randomized trial designs16.
Identifying community resources to increase staffing and project reach is beneficial to cope with limited funding, particularly funding of administrative components of projects. In our experience, having a strong partnership, with a collaborative culture amongst community-academic partners is critical to foster creative strategies. This draws upon the diverse skill sets to develop solutions to address the unique challenges of a shared community academic CBPR project and ultimately supports the vision of CBPR. For BTWB, it was essential that managers of CBPR projects focus on the development of community partnerships and relationships with participants making the 3Ps an actionable framework.
Limitations
The proposed framework and case study is subject to limitations. The 3Ps framework may be more appropriate for some CBPR projects compared to others. We suggest researchers align the framework only where appropriate to the scope and aims of the CBPR project and carefully consider adapting/informing their own administrative needs to the Principles of CBPR to ensure fidelity to the methods. Application of the 3Ps framework should consider the unique nature of the community and academic entities that formed the project. All communities are unique, in terms of socio-demographics, cohesion, and willingness to participate in CBPR. Similarly, academic institutions vary in critical ways, including funding sources, experience of staff, and institutional policies.
Conclusions
In conclusion, the 3Ps serve as an administrative framework to guide the implementation of CBPR projects while retaining fidelity to the principles of the CBPR method. Utilizing the 3Ps at the onset of a CBPR project will help ensure that CBPR projects consider elements of project planning that will support a collaborative partnership, identify core products to be delivered, and implement processes that will ensure the project meets its goals. As is integral to the CBPR method, the 3Ps should be embedded within the partnerships to promote equity in the research process and enhance project outcomes.
ACKNOWLEDGEMENTS
This study was supported by the National Institute on Minority Health and Health Disparities (P20MD006875, subproject 5174). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. The authors would like to thank the barbers, barbershop owners and managers, our program steering committee, and the faculty and research staff of the Brooklyn Health Disparities Center for their contributions to this work.
Bibliography and References Cited
- 1.Horowitz CR, Robinson M, Seifer S. Community-Based Participatory Research From the Margin to the Mainstream: Are Researchers Prepared?. Journal of the American Heart Association 2009;119:2633–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Israel BA, Schulz AJ, Parker EA, Becker AB. REVIEW OF COMMUNITY-BASED RESEARCH: Assessing Partnership Approaches to Improve Public Health. Annu Rev Public Health 1998;19:173–202. [DOI] [PubMed] [Google Scholar]
- 3.Lantz PM, Viruell-Fuentes E, Israel BA, Softley D, Guzman R. Can Communities and Academia Work Together on Public Health Research? Evaluation Results From a Community-Based Participatory Research Partnershipin Detroit. Journal of Urban Health: Bulletin of the New York Academy of Medicine 2001;78(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norris KC, Brusuelas R, Jones L, Miranda J, Duru K, Mangione CM. PARTNERING WITH COMMUNITY-BASED ORGANIZATIONS:AN ACADEMIC INSTITUTION’S EVOLVING PERSPECTIVE. Ethnicity & disease 2007;17. [PubMed] [Google Scholar]
- 5.Wolff M, Maurana CA. Building Effective Community–Academic Partnerships to Improve Health: A Qualitative Study of Perspectives from Communities. Academic Medicine 2001;76. [DOI] [PubMed] [Google Scholar]
- 6.D’Alonzo KT. Getting started in CBPR: lessons in building community partnerships for new researchers. Nursing Inquiry 2010;7(4):282–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams KJ, Bray PG, Shapiro-Mendoza CK, Reisz I, Peranteau J. Modeling the Principles of Community-Based Participatory Research in a Community Health Assessment Conducted by a Health Foundation. Health Promotion Practice 2009;10(1):67–75. [DOI] [PubMed] [Google Scholar]
- 8.Burhansstipanov L, Christopher S, Schumacher A. Lessons Learned From Community-Based Participatory Research in Indian Country. Cancer Control 2005;November(12(Suppl 2):70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Las Nueces D, Hacker K, DiGirolamo A and Hicks L . A Systematic Review of Community-Based Participatory Research to Enhance Clinical Trials in Racial and Ethnic Minority Groups. Health services research 2012;47(3):1363–1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bogart LM, Uyeda K. Community-Based Participatory Research: Partnering With Communities for Effective and Sustainable Behavioral Health Interventions. Health Psychology 2009;28 (4):391–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Strickland CJ. Challenges in Community-Based Participatory Research Implementation: Experiences in Cancer Prevention With Pacific Northwest American Indian Tribes. Cancer Control 2006;13(3). [DOI] [PubMed] [Google Scholar]
- 12.Taylor TN, Joseph M, Henny KD, et al. Perceptions of HIV Risk and Explanations of Sexual Risk Behavior Offered by Heterosexual Black Male Barbershop Patrons in Brooklyn, NY. Journal of Health Disparities Research and Practice 2014;7(6): 1–25. [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson TE, Fraser-White M, Williams KM, et al. Barbershop Talk with Brothers: Using Community-Based Participatory Research to develop and Pilot Test A Program To reduce HIV Risk Among Black Heterosexual Men. AIDS Educ Prevention 2014;26 (5):383–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green LW, George MA, Daniel M, Frankish CJ, Herbert CP, Bowie WR. Guidelines for participatory research in health promotion. In: Community-Based Participatory Research for Health 2003:27–52. [Google Scholar]
- 15.Israel BA, Schulz AJ, Parker EA, Becker AB, Allen A, Guzman JR. Critical issues in developing and following community-based participatory research principles. In: Community-Based Participatory Research for Health 2003:56–73.
- 16.Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. BMJ 2010;340:698–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Willock RJ, Mayberry RM, Yan F, Daniels P. Peer Training of Community Health Workers to Improve Heart Health Among African American Women. Health Promotion Practice 2015;16(1):63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams JK, Wyatt GE, Wingood G. The Four Cs of HIV Prevention with African Americans: Crisis, Condoms, Culture, and Community. Curr HIV/AIDS Rep 2010;7:185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Breen LJ, O’Connor M. From consultation to participation in public health research: reflections on a community-based research partnership. Biomedical Central 2014;7(936):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Odedina F, Oluwayemisi AO, Pressey S, et al. Development and Assessment of an Evidence-Based Prostate Cancer Intervention Programme for Black Men: the W.O.R.D. on Prostate Cancer Video. Ecancer Medical Science 2014:1–15. [DOI] [PMC free article] [PubMed]
- 21.Mosavel M, Simon C. Exploratory Health Disparities Research: The Need to Provide a Tangible Benefit to Vulnerable Respondents Ethics and Behavior 2010;20(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dolezal C, Marhefka SL, Santamaria EK, Leu CH, Brackis-Cott E, Mellins CA. A Comparison of Audio Computer-Assisted Self-Interviews to Face-to-Face Interviews of Sexual Behavior Among Perinatally HIV-Exposed Youth. Arch Sex Behav 2012;41(2):401–410. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rogers SM, Willis G, Al-Tayyib A, et al. Audio computer assisted interviewing to measure HIV risk behaviours in a clinic population. Arch Sex Behavior 2012;41(2):401–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haron T, Turner CF, Rogers SM, et al. Impact of T-ACASI on Survey Measurements of Subjective Phenomena. Public Opinion Quarterly 2009;73(2):255–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lewis YR, Shain L, Quinn SC, Turner K, Moore T. Building Community Trust: Lessons from an STD/HIV Peer Educator Program with African American Barbers and Beauticians. Health Promotion Practice 2002;3(2): 133–143. [Google Scholar]
- 26.Black KZ, Corbie-Smith G, Jackson M, et al. Beyond Incentives for Involvement to Compensation for Consultants: Increasing Equity in CBPR Approaches. Progress in Community Health Partnership: Research Education and Action 2013;7(3):263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boutin-Foster C, Phillips E, Palermo AG, et al. The Role of Community–Academic Partnerships: Implications for Medical Education, Research, and Patient Care. Progress in Community Health Partnerships: Research, Education, and Action 2008;2(2):56–60. [DOI] [PubMed] [Google Scholar]


