Abstract
Background
Clavicle fractures are common, accounting for 2.6% to 4% of all fractures. Eighty per cent of clavicle fractures are located in the middle third of the clavicle. Although treatment of these fractures is usually non‐surgical, displaced clavicle fractures may be considered for surgical treatment because of their greater risk of non‐union. This is an update of a Cochrane Review first published in 2013.
Objectives
To assess the effects (benefits and harms) of surgical versus conservative interventions for treating middle third clavicle fractures.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Specialised Register, CENTRAL, MEDLINE, Embase, LILACS, trials registries and reference lists updated to December 2017. We did not apply any language or publication restrictions.
Selection criteria
We considered randomised and quasi‐randomised controlled trials evaluating surgical versus conservative interventions for treating fractures in the middle third of the clavicle. The primary outcomes were shoulder function or disability, pain and treatment failure, defined as the number of participants who had been given a non‐routine secondary surgical intervention (excluding hardware removal), for symptomatic non‐union, malunion or other complications.
Data collection and analysis
At least two review authors selected eligible studies, independently assessed risk of bias and cross‐checked data. Where appropriate, we pooled results of comparable studies.
Main results
We included 14 studies involving 1469 participants with acute middle third clavicle fractures. All studies included adults, with the overall range from 17 to 70 years. Of the studies that reported gender, men were over‐represented. Ten studies compared plate fixation with sling or figure‐of‐eight bandage, or both, and four studies compared intramedullary fixation with wearing either a sling or a figure‐of‐eight bandage. Almost all studies had design features that carry a high risk of bias, thus limiting the strength of their findings.
Low‐quality evidence from 10 studies (838 participants), showed that, compared with conservative treatment, surgical treatment of acute middle third clavicle fractures may not improve upper arm function at follow‐up of one year or longer: standardised mean difference (SMD) 0.33, 95% confidence interval (CI) −0.02 to 0.67. We downgraded the quality of the evidence because of risk of bias and high statistical heterogeneity (I2 = 83%). This corresponds to a mean improvement of 2.3 points in favour of surgery (0.14 points worse to 4.69 points better), on the 100‐point Constant score; this does not represent a clinically important difference. There may be no difference in pain measured using a visual analogue scale (0 to 100 mm; higher scores mean worse pain) between treatments (mean difference (MD) −0.60 mm, 95% CI −3.51 to 2.31; 277 participants, 3 studies; low‐quality evidence reflecting risk of bias and imprecision). Surgery may reduce the risk of treatment failure, that is, number of participants who had non‐routine secondary surgical intervention (excluding hardware removal), for symptomatic non‐union, malunion or other complication (risk ratio (RR) 0.32, 95% CI 0.20 to 0.50; 1197 participants, 12 studies; low‐quality evidence, downgraded for risk of bias and imprecision). The main source of treatment failure was mechanical failure (3.4%) in the surgery group and symptomatic non‐union (11.6%) in the conservative‐treatment group.
We are uncertain whether surgery results in fewer people having one or more cosmetic problems, such as deformities, which were more common after conservative treatment, or hardware prominence or scarring, which only occurred in the surgery group (RR 0.55, 95% CI 0.31 to 0.98; 1130 participants, 11 studies; I2 = 63%; very low‐quality evidence downgraded for risk of bias, imprecision and inconsistency). We are uncertain whether there is any difference between surgery and conservative treatment in the risk of incurring an adverse outcome that includes local infection, dehiscence, symptomatic malunion, discomfort leading to implant removal, skin and nerve problems: RR 1.34, 95% CI 0.68 to 2.64; 1317 participants, 14 studies; I2 = 72%; very low‐quality evidence, downgraded for risk of bias, imprecision and inconsistency). Hardware removal for discomfort was a common adverse outcome in the surgery group (10.2%) while symptomatic malunion was more common in the conservative‐treatment group (11.3% versus 1.2% in the surgery group). Infection occurred only in the surgery group (3.2%). There may be no between‐group difference in quality of life at one year (SF‐12 or SF‐36 physical component scores: 0 to 100 scale, where 100 is the best score): MD 0.30 (95% CI −1.95 to 2.56, 321 participants, 2 studies; low‐quality evidence downgraded for risk of bias and imprecision).
Authors' conclusions
There is low‐quality evidence that surgical treatment has no additional benefits in terms of function, pain and quality of life compared with conservative treatment, but may result in fewer treatment failures overall. Very low‐quality evidence means that we are very uncertain of the findings of a slightly better cosmetic result after surgery and of no difference between surgical and conservative treatment in the risk of adverse events. For both composite outcomes, there is a need to consider the balance of risks between the individual outcomes; for example, surgical adverse events, including wound infection or dehiscence and hardware irritation, against risk of adverse events that may be more commonly associated with conservative treatment such as symptomatic malunion and shoulder stiffness.
Treatment options must be chosen on an individual patient basis, after careful consideration of the relative benefits and harms of each intervention and of patient preferences.
Plain language summary
Surgical versus conservative interventions for treating broken collarbones in adolescents and adults
This summary presents what we know from research about the effects of surgery compared with non‐surgical (conservative) treatments, such as wearing a sling or a figure‐of‐eight bandage for two to six weeks to treat a fractured (broken) collarbone.
Background
The collarbone, or clavicle, acts as a bridge across the front of the chest to connect the arm and the rib cage. It helps to stabilise the shoulder while allowing the arm to move freely, and provides an area of attachment for muscles, functioning also as part of the musculoskeletal apparatus used in breathing. The collarbone also protects nerves and blood vessels and plays an important aesthetic role in a person's physical appearance. The most common site of clavicle fracture is the middle third of the clavicle. The injury typically occurs in youths and older adults. It usually results from a fall directly onto the outer side of the shoulder. Most middle third collarbone fractures are treated conservatively (non‐surgically). However, outcome can be unsatisfactory for the more serious fractures. Surgical treatment involves putting the bone back in place and, usually, performing internal fixation by using a plate and screws or a metal rod, which is inserted into the inner cavity (medulla) of the clavicle bone.
Results of the search
We searched medical databases up to December 2017 and included 14 studies involving 1469 participants with displaced or angulated middle third clavicle fractures. All participants were adults, ranging in age from 17 to 70 years, and there were more men than women. Ten studies compared plate fixation with conservative intervention (sling and/or figure‐of‐eight bandage), and four studies compared intramedullary fixation with wearing either a sling or a figure‐of‐eight bandage.
Key results
The review showed that surgery compared with conservative treatment may not improve upper arm function, pain and quality of life one year later. However, surgery may reduce the risk of treatment failure where secondary surgery is required for fractures that did not heal or that healed incorrectly. We are uncertain whether surgery provides a better cosmetic result overall. Although surgery reduces shoulder deformity, it can result in unsightly scars and prominent metalwork. We are also uncertain if there is a difference between surgery and conservative treatment in the risk of having a complication. However the nature of such complications often differs according to treatment. Complications of surgery, such as wound infection and opening, or hardware irritation requiring additional surgery, need to be balanced against complications more likely to occur with a sling, such as shoulder stiffness and failure of the fracture to heal properly.
Quality of the evidence
All 14 studies had weaknesses that could affect the reliability of their results. We considered that the evidence for all outcomes was either of low or very low quality.
Conclusion
Low‐quality evidence indicates that surgery may not result in benefits over conservative treatment, or in more complications. However we are uncertain about these effects and further studies may change these conclusions.
Summary of findings
Summary of findings for the main comparison. Surgical versus conservative interventions for treating fractures of the middle third of the clavicle.
| Surgical versus conservative interventions for treating fractures of the middle third of the clavicle | ||||||
|
Patient or population: adults with acute fracture of the middle third of the clavicle
Settings: hospital (tertiary care)
Intervention: surgery (e.g. plate fixation or intramedullary fixation) Comparison: conservative intervention (e.g. arm sling or figure‐of‐eight bandage) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conservative treatment | Surgical treatment | |||||
| Function (overall) Various toolsa; higher values mean better function (0 to 100 scale, 100 is best function) Follow‐up: 12 months | Mean (SD) population Constant score 89 (7)b | The standardised mean difference in function (overall) in the surgery groups was 0.33 standard deviations higher (0.02 lower to 0.67 higher) | 838 (10 studies) |
⊕⊕⊝⊝ lowc,d | The SMD resultb equates to a mean improvement of 2.3 points (0.14 points worse to 4.69 points better) in favour of surgery on the Constant scale (0 to 100 scale; higher scores mean better function). This does not represent a clinically important difference. The MCID of Constant scale ranges from 5.7 to 10.4 points. | |
|
Pain VAS: 0 to 100 mm (0 is no pain and 100 mm is the worst score) Follow‐up: 12 months |
The mean pain in the control groups was 7 mm | The mean pain in the surgery groups was reduced by 0.6 mm (‐3.51 lower to 2.31 higher) | 277 (3 studies) |
⊕⊕⊝⊝ lowc,e | This is not a clinically important effect. The MCID of VAS for shoulder injury is 14 mm. |
|
| Treatment failuref Indication for non‐routine secondary surgery Follow‐up: 12 months | 132 per 1000g | 43 per 1000 (27 to 66) | RR 0.32 (0.20 to 0.50) | 1197 (12 studies) | ⊕⊕⊝⊝ lowc,e | The main source of treatment failure in the conservative treatment group was symptomatic non‐union (61 cases/527 (11.6%); 10 studies) and in the surgical group it was mechanical failure (16/468 (3.4%); 7 studies). Overall treatment failure in the conservative group is dominated by the results of 2 studiesh (289 participants): 33/77 = 43%. 2 studies (118 participants) reported that they had no treatment failures in either group. |
| Cosmetic problemi Follow‐up: 12 months | 218 per 1000g | 120 per 1000 (68 to 214) |
RR 0.55 (0.31 to 0.98) |
1130 (11 studies) | ⊕⊝⊝⊝ very lowc,e,j | The derivation of this outcome (number of people with ≥ 1 cosmetic problems) varied across the studies. Cosmetic deformity and/or asymmetry was greater in the conservative group and hardware prominence not requiring implant removal and scarring occurred only in the surgical group.k |
| Total of participants with adverse event outcomel Follow‐up: 12 months | 107 per 1000g |
144 per 1000 (73 to 282) |
RR 1.34 (0.68 to 2.64) | 1317 (14 studies) | ⊕⊝⊝⊝ very lowc,e,m | The derivation of this outcome (number of people with ≥ 1 adverse events) varied across the studies. Hardware, removed likely due to discomfort, was most frequent in the surgical group (52/508 (10.2%); 9 studies), and symptomatic malunion (45/397 (11.3%); 9 studies), in the conservative group. Infection and/or dehiscence occurred only in the surgical group (22/686 (3.2%); 11 studies).n |
| Health‐related quality of life: SF‐36 or SF‐12 physical component score at 1 year (0 to 100 points, 100 is best) | The mean health‐related quality of life: SF‐36 or SF‐12 physical component score at 1 year was 54.7 | MD 0.30 higher (1.95 lower to 2.56 higher) | 321 (2 studies) |
⊕⊕⊝⊝ lowc,e | This does not represent a clinically important difference. The MCID of SF‐36 ranges from 2.0 to 7.8 points (scale 0 to 100). | |
| *The basis for the assumed risk for dichotomous outcomes is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MCID: minimal clinical important difference; MD: mean difference; RR: risk ratio; SD: standard deviation; SMD: standardised mean difference; VAS: visual analogue scale | ||||||
| GRADE Working Group grades of evidence: High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aPatient‐reported functional scores were Constant score (7 studies), the Disability of the Arm, Shoulder, and Hand questionnaire (DASH; 1 study), the UCLA score (1 study) and Single Assessment Numeric Evaluation (SANE) score (1 study). bThis is based on the mean (SD) Constant score in a healthy population as reported in Yian 2005; mean improvement in Constant score back‐translated from SMD using the SD from the healthy population. cAll studies had methodological flaws; only two adequately concealed treatment allocation, and all were susceptible to detection bias in the measurement of self‐reported outcomes due to lack of blinding of the participant. All outcomes were downgraded one level for serious risk of bias. dThere was considerable heterogeneity (I2 = 83%), and thus we downgraded the quality of the evidence by one level for serious inconsistency. eTotal number of events and/or number of participants were small, and thus we downgraded the quality of the evidence by one level for serious imprecision. fTreatment failure, measured by the number of participants who had undergone or were being considered for a non‐routine secondary surgical intervention for symptomatic non‐union, malunion or other complications (e.g. mechanical failure defined as a condition in which an implant loses its capacity to carry a load). This does not include plate removal for hardware irritation. gThe assumed risk was the mean risk in the control group. hThese two studies had 13 of the 16 symptomatic malunions: 9 were from one study. This is an unusually high number: most malunions are asymptomatic or with mild symptoms with no need for other types of treatment. iThe number of people with one or more cosmetic problems, primarily deformity, asymmetry and/or shoulder droop, hardware prominence not requiring removal, unsightly scar and bump at fracture site. These data were often provided for individual outcomes and we applied a rule to avoid potential unit of analysis issues. jThere was considerable heterogeneity (I2 = 63%) with results from different studies spread on both sides of the line of no effect; thus we downgraded the evidence by one level for serious inconsistency. kCosmetic deformity and/or asymmetry was greater in the conservative group (21/398 versus 93/361; RR 0.16, 95% CI 0.05 to 0.46). Hardware irritation not requiring implant removal (28/308), and unsightly but otherwise not problematic scars (14/273) occurred only in the surgical group. lTotal of participants with adverse event outcome: one or more of local infection, dehiscence, discomfort leading to implant removal, skin and nerve problems, stiffness, refracture, symptomatic malunion and other adverse events (e.g. thrombosis, shoulder impingement, cardiovascular event and transient plexus irritation). mThere was considerable heterogeneity (I2 = 72%) with results from different studies spread on both sides of the line of no effect; thus the evidence was downgraded one level for serious inconsistency. nSkin and nerve problems were also more common after surgical treatment (75/338 versus 17/310; RR 4.86, 95% CI 1.85 to 12.76; 6 studies). oHealth‐rerelated quality‐of‐life score was the physical component of SF‐36 and SF‐12; the two studies did not report the full score.
Background
The clavicle or collarbone has several important functions. It acts as a bridge connecting the upper limb to the thoracic cage, which helps to stabilise the shoulder girdle, while allowing the arm to perform a full range of movement. In addition, it functions as an attachment for muscles, provides protection to vital neurovascular structures, supports respiratory function and has a significant aesthetic role in a person's physical appearance. These important functions can be damaged by fracture of the clavicle (Kotelnicki 2006; Lazarus 2001).
Description of the condition
Clavicle fractures are common, accounting for 2.6% to 4% of all fractures, with an overall incidence of 36.5 to 64 per 100,000 people per year (Nordqvist 1994; Postacchini 2002). The most common site of fracture is the middle third of the clavicle, which accounts for 80% of all clavicle fractures (Neer 1984). Incidence is bimodal, with peak incidence in youth and in later life, with more men in the younger age‐group, and more women in later life (Court‐Brown 2006). A study in Uppsala, Sweden, reported that the incidence of clavicle fractures was 50 per 100,000 population, with a higher incidence in men (71 per 100,000) compared with women (30 per 100,000) (Nowak 2000).
Two mechanisms of injury most typically result in clavicle fracture. The most common occurs after a fall onto the outer side of the shoulder, and is seen in around 90% of cases. The other mechanism of clavicle injury happens after a fall onto an outstretched arm. The force of the fall is transmitted through the upper extremity to the clavicle, producing the fracture. Although this was previously believed to be the most frequent cause of injury, it represents only 2% to 5% of clavicle fractures (Jeray 2007; Kotelnicki 2006). Falls as a result of sporting activities such as cycling and skiing are common causes of clavicle fracture (Nowak 2000).
The diagnosis of clavicle fracture is easily made clinically on the basis of a typical history and the presence of bruising and deformity, which are often noted on examination. A single antero‐posterior radiograph might confirm the diagnosis, and a second antero‐posterior radiograph with a 45° cephalic tilt view could reveal characteristics of the fracture such as degree of displacement (Jeray 2007).
Allman 1967 proposed a classification for clavicle fractures by dividing them into three groups according to their location along the bone: group I consists of fractures in the middle third of the bone; group II includes fractures in the outer or lateral third of the bone; and group III contains fractures in the inner or medial third. In a large epidemiological trial, Nordqvist 1994 classified 76% of all fractures as group I fractures, and found a median age of 13 years for participants in this group. Recently, because of the absence of a single system that has both prognostic and therapeutic value, Robinson 1998 proposed a modification of the Allman categories that includes prognostically important variables, such as degree of displacement and comminution (fragmentation of the bone).
Description of the intervention
Conservative or non‐surgical interventions are widely used and are recommended for treating middle third clavicle fractures (Robinson 2004), given the generally low incidence of non‐union after conservative treatment ‐ with rates ranging from 3.1% to 5.9% (Nordqvist 1998; Robinson 2004; Zlowodzki 2005). Numerous conservative treatment options are available, the most common being the use of a sling or a figure‐of‐eight bandage (also known as a figure‐of‐eight splint, or a backpack bandage), or a combination of these two methods (Andersen 1987; Eiff 1997; Hill 1997). No consensus has been reached on the optimal duration of immobilisation; some have recommended two to six weeks (Eiff 1997; Jeray 2007; Lazarus 2001).
Although absolute indications for surgical treatment are controversial, the most common indications for surgery include open fracture (an injury where a broken bone is open through the skin), severe displacement caused by comminution, high risk that the fracture will become open, and neurovascular injuries. Several surgical techniques of fixation can be implemented including internal fixation with screws, pins, wire loops, or plates; and external fixation with external fixators (Bradbury 1996; Ebraheim 1997; Jupiter 1987; Mullaji 1994). Bone grafting may also be used.
Other relative indications for surgery are being considered nowadays, including high‐energy fractures, complete displacement and severe comminution. There are quite a few techniques of open reduction and internal fixation using a plate and screw or intramedullary fixation used for these cases. The advantages of surgical treatment are to provide the anatomical reduction of the fracture with shorter immobilisation period as well as faster return to activities (Donnelly 2013; Khan 2009; King 2015). Currently, many models of pre‐contoured anatomical plating systems are used promoting high fitting accuracy and low discomfort related to the implant. However, these types of implants may not be superior to other types of plates (Bauer 2018).
How the intervention might work
While undisplaced fractures have relatively low rates of non‐union (Nordqvist 1998; Robinson 2004; Zlowodzki 2005), high non‐union rates for displaced fractures up to 15% have been reported (Canadian 2007; Hill 1997; McKee 2006). Fracture‐related risk factors for non‐union include open fracture, associated polytraumatic lesions, refracture, initial fracture displacement, comminution and shortening (Jupiter 1987; Marti 2003). Robinson 2004 observed that advanced age and female gender also predispose to non‐union. These findings have prompted a recent increase in preference for surgical treatment, provided through the usual techniques of open reduction and internal fixation, using a plate and screw, or intramedullary fixation, using a metal rod that is inserted into the inner cavity (medulla) of the clavicle bone, approaching or not approaching the focus of the fracture (Canadian 2007; Meier 2006).
Why it is important to do this review
This is an update of a Cochrane Review first published in 2013 (Lenza 2013). Based on evidence from eight studies at high risk of bias, Lenza 2013 concluded that there was low‐quality evidence that surgical interventions may not result in significant improvement in upper arm function.
Middle third fracture of the clavicle is one of the most common fractures of the body. It frequently results in short‐term disability and pain, eventually causing longer‐term deformity and disability.
A recent cross‐sectional study using a descriptive questionnaire completed by Brazilian and other surgeons in Latin America demonstrated that the main indications for surgery were shortening and imminent skin exposure; and that conservative treatment was indicated if there was cortical contact between fracture fragments (Oliveira 2017). For immobilisation, surgeon preference was for the use of a simple sling for up to six weeks. The blocked plate was the top option for surgery (Oliveira 2017). A survey based on the surgeons' preferences in all hospitals in Sweden, Denmark and Finland found that patients with displaced middle third clavicle fractures are mainly treated surgically with a locking plate; in addition, more than 80% of surgeons preferred this approach (Ban 2016). Current literature indicates that the treatment of clavicle fracture remains controversial. For example, most US surgeons prefer to use a simple sling for treating patients conservatively (94% prefer simple sling versus 6% who prefer figure‐of‐eight bandage; Heuer 2014). Conversely, a German survey on conservative treatment of clavicle fractures concluded that simple clavicle fractures are treated in a non‐surgical way, with orthopaedic surgeons preferring the use of figure‐of‐eight bandage in 88% of cases (Pieske 2008).
Before the current review update, Cochrane authors updated two Cochrane Reviews that separately considered different conservative interventions or different surgical interventions (Lenza 2016; Lenza 2015). Lenza 2016 concluded that evidence from three studies, with 296 participants, is insufficient to establish the relative effects on final functional outcome of a figure‐of‐eight bandage compared with a sling, although the bandage may be associated with increased early pain. A fourth study provided no evidence that therapeutic ultrasound accelerates recovery, including clinical fracture healing. Lenza 2015 concluded that there is very limited and low‐quality evidence regarding the effectiveness of different methods of surgical intervention for treating acute fracture and non‐union of the clavicle. Most acute fractures used to be treated conservatively; however, current treatment of some types of clavicle fracture is more interventional, thus involving surgery (Judd 2009). This change merits investigation. An informed decision about the best treatment can be put forth only after available evidence is again systematically reviewed to determine whether surgical or conservative interventions are preferred to treat some or all middle third clavicle fractures.
Objectives
To assess the effects (benefits and harms) of surgical versus conservative interventions for treating middle third clavicle fractures.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), or quasi‐RCTs (method of allocating participants to a treatment that is not strictly random, e.g. by date of birth, hospital record number, or alternation), that compared surgical versus conservative interventions for treating middle third clavicle fractures.
Types of participants
We included all studies of adolescents (aged over 10 years), and adults who had been diagnosed with middle third clavicle fracture. We included studies with children younger than 10 years of age if the proportion of children of this age was less than 10%, or if separate data were available.
We also included studies involving people who had a history of other shoulder injuries, provided separate data were presented for this population or the numbers included were small and balanced between the two groups. The same approach applied to studies including people with other concurrent shoulder injuries.
Types of interventions
We considered all surgical and conservative interventions used to treat fractures of the middle third of the clavicle.
We excluded studies comparing different techniques of surgical interventions alone, or different techniques of conservative interventions alone. Surgical interventions may include internal fixation using a plate‐and‐screw, Kirschner wires, titanium nail, and Knowles pin, and external fixation with an external fixator. Conservative interventions may include slings, strapping, figure‐of‐eight bandages and splints, or other physical treatments, as well as adjunctive therapies, such as therapeutic ultrasound. We also considered for inclusion any study that compared surgery with no treatment.
Closed reduction (re‐aligning the fragments of the fracture), is not usually performed for clavicle fractures because the reduced position is practically impossible to maintain. However, we included all studies regardless of whether reduction was attempted or not.
Types of outcome measures
Primary outcomes
Function or disability (mean or mean change), measured by upper limb functional outcome measures. Ideally, these should be participant‐reported measures of function, validated for people with clavicle fractures (however, we are not aware of any outcome measures in this category). Validated patient‐reported measures include the Disability of the Arm, Shoulder, and Hand questionnaire (DASH; Hudak 1996), and the Constant score (Constant 1987), which is a composite score for shoulder function that includes subjectively rated pain and activities of daily living, as well as objectively rated range of movement and strength.
Pain: preference was given to reports of pain measured using validated pain scales (visual analogue scale (VAS) or numerical rating scale (NRS)), and reported as a dichotomous outcome, for example, number with a clinically important change in pain score in the short‐term phase (e.g. proportion with at least 30% improvement in pain), or participant‐reported long‐term pain (e.g. proportion above 30/100‐mm VAS scale, i.e. worse than mild pain). Examples are drawn from recommendations in Eccleston 2010 and Moore 2010. When data were not reported as a dichotomous measure, we used a continuous measure: mean pain or mean change in pain.
Treatment failure measured by the number of participants who have undergone or are being considered for a non‐routine secondary surgical intervention for symptomatic non‐union, malunion or other complications (e.g. mechanical failure, defined as a condition in which an implant loses its capacity to carry a load). This does not include plate removal for hardware irritation.
Secondary outcomes
Cosmetic result: number of participants with one or more of deformity, asymmetrical result, unsightly scar, or hardware prominence that did not require implant removal.
Composite adverse event outcome: number of participants with one or more events that include local infection, dehiscence, symptomatic malunion, refracture, discomfort leading to implant removal, skin and nerve problems, shoulder stiffness or restricted range of motion.
Health‐related quality of life: mean or mean change in Short Form‐36 (Ware 1992), or other quality‐of‐life measures.
Numbers of participants returning to previous activities (work, sport, activities of daily living, etc.), or time to time to return if the outcome was not reported dichotomously.
Asymptomatic non‐union (i.e. the fracture has not healed radiographically and is not surgically treated), defined as incomplete cortical bridging between proximal and distal fragments and radiographic malunion.
Timing of primary outcomes measurement
We extracted outcome data at the following time periods: short‐term follow‐up (up to six weeks following treatment); intermediate follow‐up (more than six weeks and up to six months after the end of treatment), and long‐term (longer than six months after the end of treatment), for function and pain. We extracted the remaining outcomes at the end of follow‐up.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Specialised Register (to 22 December 2017), the Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 12) via Central Register of Studies Online, PubMed (1966 to 14 December 2017), Ovid MEDLINE (including Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE; 1 December 2012 to 22 December 2017), Embase (1980 to 22 December 2017), and Latin American and Caribbean Literature in Health Sciences (LILACS; 1982 to 22 December 2017). We also searched the WHO International Clinical Trials Registry Platform (WHO ICTRP) and the ClinicalTrials.gov registry for ongoing and recently completed studies (to August 2017). For this update, the search results were limited from 2012 onwards. Details of the search strategies used for the previous version of the review are given in Lenza 2013. We didn't apply any restrictions based on language or publication status. The search strategies for all databases are reported in Appendix 1.
Searching other resources
We checked the reference lists of articles and reviews for possible relevant studies.
Data collection and analysis
The intended methodology for data collection and analysis was described in our published protocol (Lenza 2011), which was based on the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). The main changes from protocol, mainly relating to outcomes measures, are summarised in Differences between protocol and review.
Selection of studies
Two authors (ML and FF), independently selected potentially eligible studies for inclusion in the review, using a pre‐piloted form. Any disagreements were resolved by discussion and, when necessary, with adjudication by a third author (BASF). The review authors were not blinded to the journal or to the authors.
Data extraction and management
Two review authors (ML and BASF), extracted the following data using a pre‐piloted data extraction form: characteristics of the study methods including study design, duration of the trial, whether the protocol was published before recruitment of participants, funding sources and details of study registration; characteristics of the study participants including place of trial, number of participants assigned, number of participants assessed, inclusion criteria, exclusion criteria, age and classification of injury; characteristics of the study interventions including timing of intervention, type of surgical intervention, type of conservative intervention, rehabilitation and any co‐interventions; characteristics of the study outcomes including length of follow‐up, loss to follow‐up and outcome measures; and the methodological domains as outlined later in Assessment of risk of bias in included studies.
A third review author (RB), resolved any disagreements. Two review authors (ML and BASF), entered data into Review Manager 5 (Review Manager 2014). We sent requests seeking additional information or data to study authors.
Assessment of risk of bias in included studies
Two review authors (ML and BASF), independently assessed the risk of bias of included studies. As recommended by the Cochrane 'Risk of bias' tool (Higgins 2017), we assessed the following domains:
Random sequence generation
Allocation concealment
Blinding of participants and personnel
Blinding of outcome assessment
Incomplete outcome data
Selective reporting
Other bias (e.g. major baseline imbalance; inappropriate influence of funders; risk of bias associated with inexperience of surgeons and other care providers with the interventions, differences in rehabilitation).
We judged each of these criteria explicitly on the basis of low risk of bias, high risk of bias, and unclear (either lack of information or uncertainty over the potential for bias). We resolved disagreements between authors regarding the risk of bias for domains by consensus.
Measures of treatment effect
We calculated risk ratios (RRs) together with 95% confidence intervals (CIs) for dichotomous outcomes.
We expressed continuous outcome data as mean differences (MDs) with 95% CIs when continuous outcomes were reported using the same instrument in the studies. We used the standardised mean difference (SMD) with 95% CI when studies measured the same outcome but employed different measurement instruments (e.g. function).
We back‐transformed the pooled SMD for function to the 0 to 100 Constant scale by multiplying the SMD and 95% CIs by a representative pooled standard deviation in normal shoulders (mean (SD) population Constant score 89 (7)) from Yian 2005.
When we observed a statistically significant difference between surgery and conservative‐treatment groups, we planned to report the number needed to treat for an additional beneficial outcome (NNTB) with 95% CIs and the number needed to treat for an additional harmful outcome (NNTH) with 95% CIs. For dichotomous outcomes, in the case of adverse events, we would have calculated the NNTB or the NNTH from the control group event rate and the relative risk using the Visual Rx NNT calculator (Cates 2008).
Unit of analysis issues
The unit of randomisation in the studies included in this review is the individual participant.
There are potential unit of analysis problems with composite outcomes, namely treatment failure, composite adverse events, and overall cosmetic result, where studies have reported on numbers of participants with specific complications instead of numbers of study participants with one or more complications. For these composite outcomes, we have extracted the number of participants with one or more complications, as far as it can be presumed from the study reports. Where the composite event rate is not clearly reported or cannot be deduced, and the number of cases are reported for each individual component event of the composite only, to avoid double‐counting of cases, we have extracted the number of participants with one of the component events as a proxy (we chose the component event with the most cases in each treatment group). We have reported our decisions in Notes of the Characteristics of included studies table; thus, the number of cases with each component event of the composite event, and the number of cases we used in our analyses.
Dealing with missing data
We attempted to extract outcome data for all participants randomly assigned into each trial. We tried to contact the authors of primary studies to request missing data, such as numbers of participants, details of dropouts, means, measures of variance (standard deviation or standard error), and numbers of events.
For continuous outcomes with no standard deviations reported, we planned to calculate standard deviations from standard errors, P values, or confidence intervals, according to the methods outlined in Higgins 2011. We described missing data and data on dropouts for each included study in the 'Risk of bias' table, and we discussed the degree to which missing data could change the results and conclusions of this review.
The effects of dropouts and exclusions were investigated by conducting worst‐ and best‐case scenario analyses. For dichotomous outcomes, we analysed the worst‐case scenario using the number randomly assigned as denominator, with the assumption that any participants missing at the end of treatment did not have a positive outcome (e.g. for the outcome number of participants experiencing treatment failure, we assumed that any missing participants had an adverse event). We analysed the best‐case scenario using the number randomly assigned in the denominator, and ignoring the dropouts in our analyses of dichotomous outcomes (overall treatment failure).
Assessment of heterogeneity
We assessed the heterogeneity of estimate effects between included studies by visual inspection of the forest plot (analysis), along with consideration of the test for heterogeneity and the I² statistic (Higgins 2003). We quantified the possible magnitude of inconsistency (i.e. heterogeneity), across studies, using the I² statistic with a rough guide for interpretation as follows: 0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; and 75% to 100% considerable heterogeneity (Deeks 2017). In cases of considerable heterogeneity (defined as I2 of 75% or more), we explored the data further by comparing the characteristics of individual studies and conducting subgroup analyses.
Assessment of reporting biases
We planned to generate funnel plots of primary outcomes to assess the potential publication bias (small study effects). However, the small number of included studies precluded this form of analysis. We assessed the presence of small study bias in the overall meta‐analysis by checking whether the random‐effects estimate of the intervention effect was more beneficial than the fixed‐effect estimate (Sterne 2008).
We also assessed outcome reporting bias by comparing results extracted from published journal reports with results from other sources (e.g. correspondence) and by checking study registrations (at the WHO International Clinical Trials Registry Platform), or published protocols.
Data synthesis
When appropriate, we pooled results of comparable groups of studies in meta‐analysis using the random‐effects model as a default.
Assessing the quality of the evidence and the 'Summary of findings' table
We used the GRADE approach to assess the quality of evidence related to all outcomes listed in the Types of outcome measures (Schünemann 2011). The four levels of evidence certainty are 'high', 'moderate', 'low' or 'very low'. Quality may be downgraded due to study limitations (risk of bias), imprecision, inconsistency, indirectness or publication bias. We presented the main results of the surgical versus conservative treatment comparison in a 'Summary of findings' table, which provides key information concerning the quality of the evidence, the magnitude of effect of the interventions examined and the sum of available data on the main outcomes. We produced the 'Summary of findings' table via RevMan (Review Manager 2014).
Outcomes for 'Summary of findings' table
We included the following outcomes in our 'Summary of findings' table: function; pain; treatment failure (non‐routine secondary surgical intervention); number with unsatisfactory overall cosmetic result; composite adverse event outcome (one or more of local infection, dehiscence, symptomatic malunion, discomfort leading to implant removal, skin and nerve problems, stiffness); and health‐related quality of life. We converted the SMD result for the upper limb function outcome to a clinically meaningful measure of function (Constant score) by multiplying the SMD by the SD of the Constant score in healthy people as reported in Yian 2005.
For the purpose of pooling data where studies included more than one measure of function, we preferentially included one measure according to the following hierarchy: Constant score (Constant 1987), DASH score (Hudak 1996), University of California Los Angeles (UCLA) score (Amstutz 1981), Single Assessment Numeric Evaluation (SANE) score (Williams 1999) and L'Insalata score (L'Insalata 1997). We restricted follow‐up for function to at least 12 months because the results are more consistent during this period; after 12 months there is typically no modification in function of patients with clavicle fractures.
Subgroup analysis and investigation of heterogeneity
We planned to perform subgroup analyses for the following:
Age (adolescents, adults and people older than 65 years)
Type of surgical intervention: intramedullary fixation versus plate fixation
Timing of surgery: immediate versus delayed (from one week to four weeks after injury)
Two fragments versus more than two fragments
Primarily undisplaced versus displaced
Details of the actual subgroup analyses conducted are given in Effects of interventions. We investigated whether the results of subgroups were significantly different by inspecting the overlap of CIs and by performing the test for subgroup differences available in Review Manager 5 (Review Manager 2014).
Sensitivity analysis
We planned sensitivity analyses to assess the effects of including studies at risk of selection bias (inadequate or unclear allocation concealment), or detection bias (inadequate or unclear blinding of outcome assessor); and of including participants with a history of shoulder injuries. We also planned to assess the presence of small study bias (i.e. intervention effect is more beneficial in smaller studies), in the meta‐analysis by comparing the fixed‐effect estimate with the random‐effects estimate for primary outcomes.
We conducted sensitivity analyses to investigate the effects of any missing data by conducting worst‐ and best‐case scenario analyses.
Results
Description of studies
See: Characteristics of included studies, Characteristics of excluded studies and Characteristics of ongoing studies.
Results of the search
The searches for this update (run from December 2012 to December 2017), identified a total of 1270 new records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (10); CENTRAL (126), MEDLINE (272), Embase (639), LILACS (30), ClinicalTrials.gov (35) and the WHO International Clinical Trials Registry Platform (158). We also identified four potentially eligible studies from other from the references of other studies.
The search update resulted in the identification of 28 reports of potentially eligible studies, for which we obtained full reports where possible. Of these, we included six studies, reported in 14 articles published between 2012 and 2017 in the review (Ahrens 2017; Melean 2015; Naveen 2017; Robinson 2013a; Tamaoki 2017; Woltz 2017a), we excluded eight (Dugar 2013; Jones 2014; Khorami 2014; Madhukar 2015; Malkoc 2016; McIntosh 2016; Parry 2017; Shukla 2014), and two await assessment (Dhakad 2016; Shetty 2017). We also found additional reports for two already included studies: COTS 2007 (three abstracts and two separate publications), and Smekal 2009 (one abstract).
Overall, there are 14 included studies, 20 excluded studies, five studies awaiting classification and three ongoing studies.
A flow diagram summarising the study selection process is shown in Figure 1. The results from the previous searches (up to December 2012) are reported in Appendix 2.
1.
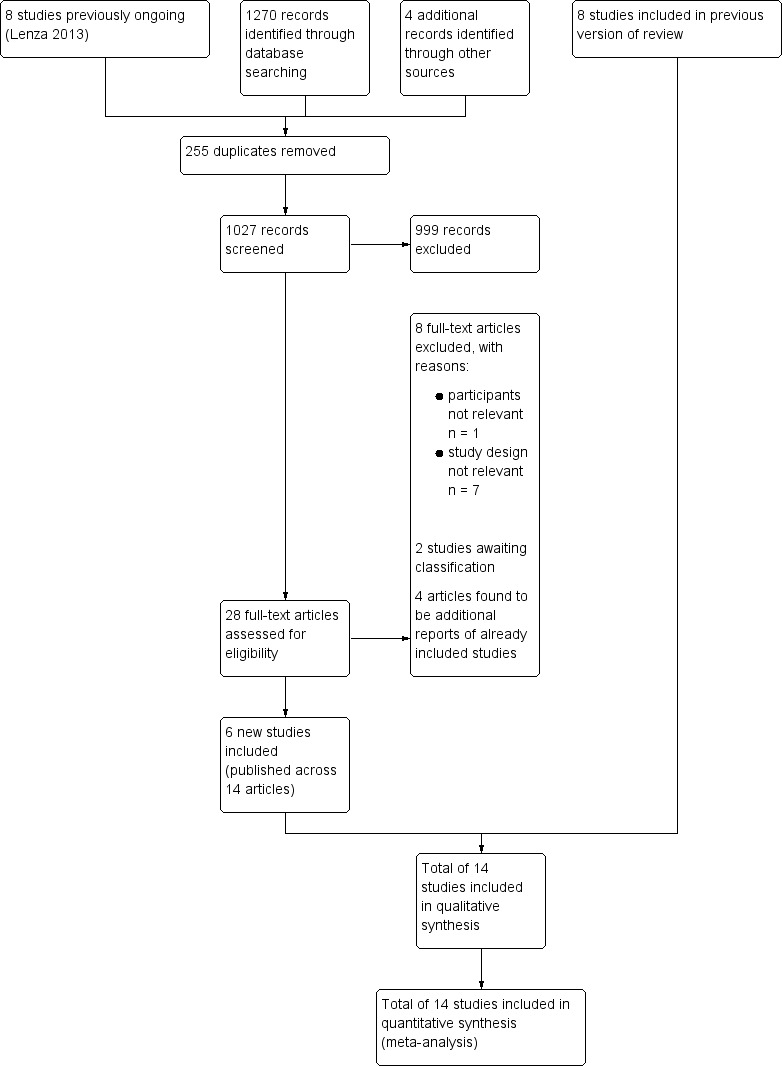
Study flow diagram
Included studies
Details of the 14 included studies can be found in Characteristics of included studies.
Only two studies published their study protocol before their results: Ahrens 2017, protocol published in 2011 (Longo 2011); and Woltz 2017a, protocol published in 2011 (Stegeman 2011). Five studies registered their protocol before publication in national or international trials registers (Ahrens 2017; Robinson 2013a; Tamaoki 2017; Virtanen 2012a; Woltz 2017a).
COTS 2007 reported its results in four conference abstracts (Hall 2006; Hall 2008; McKee 2010a; Schemitsch 2012), and also presented different results (different time points or outcomes, or both), across five separate full publications (Altamimi 2008; COTS 2007; Neuhaus 2013; Pearson 2010; Schemitsch 2011). Judd 2009 was initially reported in 2005 in an abstract (American Academy of Orthopaedic Surgeons (AAOS)), and then published in full in 2009. Koch 2008 reported the same results in two papers (Koch 2008; Witzel 2007). The results of Melean 2015 were also commented on in a letter. Robinson 2013a also reported different results across three separate publications (Goudie 2017; Robinson 2013a; Robinson 2013b). Smekal 2009 also presented its results in abstract format (Vinzenz 2008). The results of Virtanen 2012a were also reported as a conference proceeding and it was commented on in a letter. Each of the remaining five studies reported results in a single publication (Chen 2011; Figueiredo 2008; Mirzatolooei 2011; Naveen 2017; Tamaoki 2017). We did not use conference abstract data in our analyses.
We sent requests seeking additional information or data to authors of 12 studies (Ahrens 2017; Chen 2011; COTS 2007; Judd 2009, Koch 2008; Melean 2015; Mirzatolooei 2011; Naveen 2017, Robinson 2013a, Smekal 2009; Tamaoki 2017; Woltz 2017a). We obtained standard deviations and means of DASH and Constant scores by personal contact with the authors of two studies (Ahrens 2017; Mirzatolooei 2011), and standard deviations and means of VAS scores by personal contact with the authors of Woltz 2017a. Tamaoki 2017 provided some information regarding the structure of the study. The authors of two studies declined to provide further information or missing data (COTS 2007; Melean 2015). We tried unsuccessfully to contact the authors of six studies to obtain further information and missing data (Chen 2011; Judd 2009; Koch 2008; Naveen 2017; Robinson 2013a; Smekal 2009).
All studies were reported in English, except Koch 2008 (in German), and Figueiredo 2008 (in Portuguese). One review author (ML) translated both into English.
Design
All studies were parallel‐group controlled studies with two intervention groups; 13 were RCTs and one was a quasi‐RCT (Naveen 2017). Ahrens 2017 was conducted in 20 centres in England, COTS 2007 in eight centres in Canada, Robinson 2013a in three centres in the UK, Tamaoki 2017 in two centres in Brazil, and Woltz 2017a in 16 centres in the Netherlands. All other studies were single‐centre studies. Chen 2011 took place in China; Figueiredo 2008 in Brazil; Judd 2009 probably in Hawaii; Koch 2008 in Germany; Melean 2015 in Chile; Mirzatolooei 2011 in Iran; Naveen 2017 in India; Smekal 2009 in Austria; and Virtanen 2012a in Finland.
Sample sizes
The 14 studies enrolled a total of 1469 participants. Outcome data allowing analysis by the study authors were available for a maximum of 1267 participants (86.2% of those enrolled). The number of randomised participants in individual studies ranged from 50 (Figueiredo 2008) to 301 (Ahrens 2017).
Participants
Age and gender
Ahrens 2017, Chen 2011, Mirzatolooei 2011 and Smekal 2009 included adults between 18 and 65 years old; COTS 2007 and Robinson 2013a stipulated an age limit between 16 and 60 years; Figueiredo 2008, Melean 2015 and Tamaoki 2017 excluded participants who were younger than 18 years of age; Judd 2009 excluded participants who were younger than 17 years of age or older than 40 years, Naveen 2017 included participants between 20 and 50 years, Virtanen 2012a included participants between 18 and 70 years, and Woltz 2017a included participants between 18 and 60 years. Koch 2008 did not specify age in the inclusion criteria. Overall, the review population was adults with older people generally excluded. The mean age of participants in individual studies ranged from 26.5 years in Judd 2009 to 38.5 years in Chen 2011.
With the exception of Melean 2015, gender data provided for assigned or assessed participants showed there were more male participants overall (1128/1344; 83.9%), with the proportion of men in individual studies ranging from 53.3% in Chen 2011 to 91.3% in Woltz 2017a.
Types/classification of fractures
All studies included only participants with displaced or angulated middle third clavicle fracture. Ahrens 2017, Melean 2015, Naveen 2017, Robinson 2013a and Woltz 2017a used the Robinson's classification (Robinson 1998), to characterise their populations. Chen 2011, Smekal 2009, Tamaoki 2017 and Virtanen 2012a used the AO (Arbeitsgemeinschaft fur Osteosynthesefragen) classification (Muller 1991). The AO or AO/OTA (Orthopaedic Trauma Association) is an alphanumeric classification used by trauma surgeons and physicians dealing with orthopaedic trauma surgery (Kellam 2018). All studies apart from Mirzatolooei 2011 excluded potential participants with open fractures, in which 20% of study participants had an open clavicle fracture. All studies reported that they treated participants with acute clavicle fracture.
Interventions
Details of the 14 interventions of the included studies can be found in Table 2.
1. Treatment interventions of included studies.
| Study ID | No. centres | No. participants (assessed/assigned) | Surgical fixation | Conservative treatment |
| Ahrens 2017 | 20 | 204/301 (67.8%) | Plate fixation: LCP (precontoured titanium plate) | Simple sling |
| Chen 2011 | 11 | 60/60 (100%) | Intramedullary fixation: TEN | Simple sling |
| COTS 2007 | 8 | 111/132 (84.1%) | Plate fixation: limited DCP/3.5 mm reconstruction plates/pre‐contoured plates/other plates | Simple sling |
| Figueiredo 2008 | 1 | 40/50 (80%) | Plate fixation: 3.5 mm DCP plate fixation | Simple sling |
| Judd 2009 | 1 | 57/57 (100%) | Intramedullary fixation: modified Hagie pin | Simple sling |
| Koch 2008 | 1 | 68/68 (100%) | Intramedullary fixation: 2 mm pin | Figure‐of‐eight bandage |
| Melean 2015 | 1 | 76/76 (100%) | Plate fixation: 3.5 mm LCP/LCP reconstruction plates | Simple sling |
| Mirzatolooei 2011 | 1 | 50/60 (83.3%) | Plate fixation: 3.5 mm reconstruction plates | Simple sling |
| Naveen 2017 | 1 | 60/60 (100%) | Plate fixation: 3.5 mm DCP plate fixation | Figure‐of‐eight bandage |
| Robinson 2013a | 3 | 178/200 (89%) | Plate fixation: LCP (precontoured titanium plate) | Simple sling |
| Smekal 2009 | 1 | 60/68 (88.2%) | Intramedullary fixation: TEN | Simple sling |
| Tamaoki 2017 | 2 | 98/117 (83.8%) | Plate fixation: 3.5 mm reconstruction plates | Figure‐of‐eight bandage |
| Virtanen 2012a | 1 | 51/60 (85%) | Plate fixation: 3.5 mm reconstruction plates | Simple sling |
| Woltz 2017a | 16 | 154/160 (96.2%) | Plate fixation: most operatively treated participants (80%) were treated with a precontoured clavicular plate | Simple sling |
DCP: dynamic compression plates; LCP: locking compression plate; TEN: titanium elastic nail
Based on the method of surgical fixation (plate or intramedullary), the included studies could be grouped into two comparisons:
Surgical intervention using plate fixation versus conservative intervention using a sling (Ahrens 2017; COTS 2007; Figueiredo 2008; Melean 2015; Mirzatolooei 2011; Naveen 2017; Robinson 2013a; Tamaoki 2017; Virtanen 2012a; Woltz 2017a). Follow‐up data were available for 1022 participants (534 with surgical and 488 with conservative intervention).
Surgical intervention using intramedullary fixation versus conservative intervention using sling or figure‐of‐eight bandage (Chen 2011; Judd 2009; Koch 2008; Smekal 2009). Follow‐up data were available for 245 participants (124 with surgical and 121 with conservative intervention).
Participants underwent intervention on average within 22 hours in Chen 2011, and within three days in Smekal 2009 to 28 days in COTS 2007 after injury.
Outcome measures
The studies varied in timing of follow‐up. Ahrens 2017 conducted follow‐up up to nine months. Naveen 2017 reported follow‐up data for six months. Eight studies specified follow‐up time points at one or two years: COTS 2007 reported follow‐up data for one year, and a subsequent publication (Schemitsch 2011), presented data for two years; Judd 2009, Melean 2015, Mirzatolooei 2011, Robinson 2013a, Virtanen 2012a, Tamaoki 2017 and Woltz 2017a conducted follow‐up to one year; and Smekal 2009 reported data after two years of follow‐up. Three studies reported mean follow‐up: Chen 2011 presented a mean follow‐up of 15 months, Figueiredo 2008 reported a mean follow‐up of 16 months and Koch 2008 reported a mean follow‐up of 19 months.
Primary outcomes
Function or disability
Ahrens 2017, Chen 2011, COTS 2007, Mirzatolooei 2011, Robinson 2013a, Smekal 2009 and Virtanen 2012a evaluated shoulder function or disability by the DASH questionnaire and the Constant score. Woltz 2017a, Melean 2015 and Naveen 2017 used only the Constant score to assess function or disability. Tamaoki 2017 used only the DASH score. Figueiredo 2008 used the UCLA score and Judd 2009 used both the SANE and L'Insalata shoulder scores to assess shoulder function or disability. Koch 2008 did not evaluate this primary endpoint.
Pain
The four studies that assessed pain used a VAS scale, either ranging from 0 to 10 cm (with 0 indicating no pain and 10 indicating maximum pain), or 0 to 100 mm (maximum pain) (Koch 2008; Tamaoki 2017; Virtanen 2012a; Woltz 2017a). We present data on a 0 to 100 mm scale in our analyses.
Treatment failure
All the studies measured treatment failure as the number of participants who had undergone a non‐routine secondary surgical intervention (excluding hardware removal), for symptomatic non‐union, malunion or other complication.
Secondary outcomes
Cosmetic results
Eleven studies reported cosmetic results, which could usually be categorised as one or a combination of deformity, asymmetry, shoulder droop; hardware irritation or prominence not requiring removal; unsightly scar; and bump at fracture site (Ahrens 2017; Chen 2011; COTS 2007; Figueiredo 2008; Judd 2009; Koch 2008; Mirzatolooei 2011; Naveen 2017; Robinson 2013a; Tamaoki 2017; Woltz 2017a).
Adverse events
All studies reported adverse events. Eight studies reported infection or dehiscence, or both (Chen 2011; COTS 2007; Judd 2009; Mirzatolooei 2011; Naveen 2017; Robinson 2013a; Tamaoki 2017; Woltz 2017a). Tem studies reported hardware irritation requiring removal (Ahrens 2017; COTS 2007; Judd 2009; Melean 2015; Mirzatolooei 2011; Robinson 2013a; Smekal 2009; Tamaoki 2017; Virtanen 2012a; Woltz 2017a). Sevem studies reported skin and nerve problems (Ahrens 2017; COTS 2007; Judd 2009; Mirzatolooei 2011; Robinson 2013a; Tamaoki 2017; Woltz 2017a). Ahrens 2017, Figueiredo 2008, Koch 2008 and Naveen 2017 reported stiffness or restricted of range of shoulder movement. Judd 2009 and Virtanen 2012a reported refracture. Four studies reported other adverse events; Chen 2011 and Smekal 2009 reported participants with transient plexus irritation; Robinson 2013a reported adverse events relating to shoulder injuries (impingement); and Woltz 2017a reported thrombosis of the cephalic vein and a cardiovascular event. Nine studies reported symptomatic malunion (Chen 2011; COTS 2007; Mirzatolooei 2011; Naveen 2017; Robinson 2013a; Smekal 2009; Tamaoki 2017; Virtanen 2012a; Woltz 2017a).
Health‐related quality of life
Robinson 2013a measured health‐related quality of life using the SF‐12 questionnaire (health and function status), and Woltz 2017a using SF‐36 questionnaire (physical and mental component scores).
Health‐related quality of life was also reported to have been measured using the SF‐36 questionnaire (health and function status) in a publication of COTS 2007 (Pearson 2010); however, the study authors did not report their results. No other study reported health‐related quality‐of‐life data.
Return to previous activities
Figueiredo 2008, Melean 2015, Robinson 2013a and Tamaoki 2017 described return to previous activities endpoints (work and activities of daily living) and Koch 2008 reported sport activities.
Asymptomatic non‐union and malunion
Seven studies reported asymptomatic non‐union (Ahrens 2017; Chen 2011; Mirzatolooei 2011; Robinson 2013a; Tamaoki 2017; Virtanen 2012a; Woltz 2017a).
Funding sources
Three studies reported that they had been funded (Ahrens 2017; Virtanen 2012a; Woltz 2017a); none of the sources were commercial or would have influenced the conduct and reporting of the trial. COTS 2007 referred to funding, including from a commercial entity, for individual authors in support of the research; however, it was also made clear that the authors were not obliged to provide benefits to the commercial entity in relation to the research. Absence of external funding was either confirmed or likely in the other 10 studies.
Excluded studies
We excluded 20 studies because they did not meet our inclusion criteria. The full reasons for excluding these studies are provided in Characteristics of excluded studies.
Overall, the main reason for excluding the majority of the 20 studies was irrelevant study design (not a RCT or quasi‐RCT). We excluded three registered studies (ACTRN12610000948099; ISRCTN00825817; NCT01311219). In ACTRN12610000948099, the registration for the study was withdrawn in February 2016 and we were unable to identify any other study registration. NCT00642265 was listed as an ongoing study in the first version of the review. It planned to compare osteosynthesis versus sling, with a start date of April 2008 and end date July 2015. However, the contact author reported that for a variety of reasons the study was ended and no data were available. In NCT01311219, the registration for a multicentre study was withdrawn before enrolment because it was "a duplicate study". The other study registration was not identified.
Studies awaiting classification
There were five studies classified as studies awaiting classification.
Dhakad 2016 stated in the Abstract: "Alternate patients were operated", which implies alternation, thus a quasi‐RCT. However, there is no description of the study design and method of allocation in the main text and no reassurance of balance in baseline characteristics. We were unsuccessful in our attempt to get further details from the study authors on methods, baseline characteristics split by treatment group and loss to follow‐up.
Shetty 2017 reported in the Abstract: "They were divided into two groups randomly" and thus warrants being an included trial. However, this study was likely to be compromised by excess loss to follow‐up. We were unsuccessful in our attempt to get further details from the study authors on methods, on participant flow and baseline characteristics split by treatment group.
One study (Smith 2001), is awaiting classification pending the receipt of further information on study characteristics and data. Given that this study was presented in 2000 and in 2001 at conferences, it seems likely that the full results will remain unpublished. Two other studies, whose details are available only in a study registry, are classified as awaiting classification because of their "completed" status; however, we have not identified any reports of these studies (ISRCTN00825817; ISRCTN57483251). Details of these studies can be found in Characteristics of studies awaiting classification.
Ongoing studies
Our search for ongoing studies found three studies (NCT00590850; NCT01078480; NCT01483482); see the Characteristics of ongoing studies. All ongoing studies are parallel RCTs comparing surgical versus conservative interventions to treat middle third clavicle fractures. They appear to be single‐centre studies, taking place in the USA (NCT00590850) and Denmark (NCT01078480; NCT01483482), and should enrol a total of 740 participants.
Risk of bias in included studies
All studies had methodological flaws, rendering them at high risk of bias (see Figure 2 and Figure 3).
2.
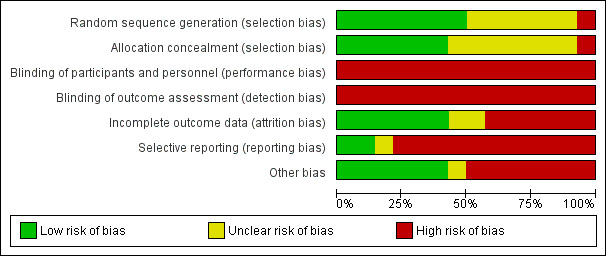
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.
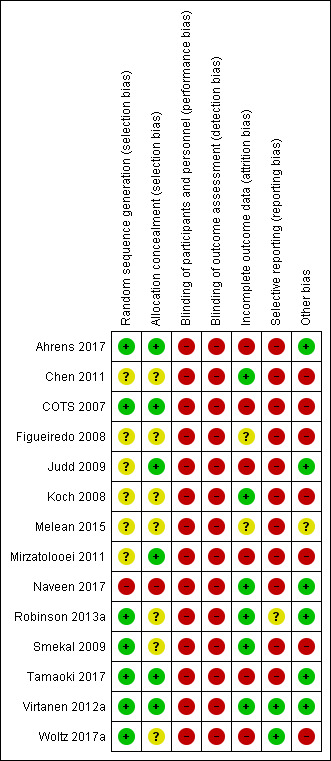
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Ahrens 2017, COTS 2007, Robinson 2013a, Tamaoki 2017, Virtanen 2012a and Woltz 2017a reported that they performed random sequence generation using a computer random number generator, and Smekal 2009 by throwing dice; thus we judged them at low risk of selection bias. Naveen 2017 was quasi‐randomised based on alternation and thus at high risk of bias for this item. The six remaining studies (Chen 2011; Figueiredo 2008; Judd 2009; Koch 2008; Melean 2015; Mirzatolooei 2011), did not provide sufficient information about the sequence generation process to permit a judgement about bias; thus we judged them at unclear risk of bias for this item.
Concealment of allocation before assignment was adequate for Ahrens 2017, COTS 2007, Judd 2009, Mirzatolooei 2011, Tamaoki 2017 and Virtanen 2012a (opaque and sealed envelopes); thus we judged them at low risk of selection bias. Chen 2011, Figueiredo 2008, Koch 2008, Robinson 2013a and Woltz 2017a did not describe their methods of allocation concealment. Melean 2015 and Smekal 2009, which used envelopes, provided insufficient information to permit judgement. We judged these seven studies to be at unclear risk of selection bias. There was no concealment of allocation in Naveen 2017, which we assessed at high risk of selection bias.
Blinding
We judged all studies to be at high risk of performance bias. As they all compared surgery with conservative treatment, it was not possible to blind treatment providers. No studies included sham surgery; therefore participants were not blinded.
It may have been possible to blind outcome assessors; however, none of the studies mentioned correctly blinding assessors. Thus, for self‐reported outcomes (function; pain; quality of life; and possibly, cosmetic result), there was a high risk of detection bias. Notably, Lack of blinded outcome assessors of the more objective outcomes (treatment failure as indicated by non‐routine secondary surgery; infection or dehiscence; hardware irritation leading to removal) would be less likely to lead to detection bias.
Incomplete outcome data
We considered studies to be at low risk of bias if more than 80% of participants completed the follow‐up, missing outcomes data were balanced in number across intervention groups, and studies reported an intention‐to‐treat analysis for the primary outcomes. As a result, six studies (Chen 2011; Koch 2008; Naveen 2017; Robinson 2013a; Smekal 2009; Virtanen 2012a), were at low risk of attrition bias, six (Ahrens 2017; COTS 2007; Judd 2009; Mirzatolooei 2011; Tamaoki 2017; Woltz 2017a), were at high risk, and we classified two as unclear (Figueiredo 2008; Melean 2015).
We judged Ahrens 2017, COTS 2007, Judd 2009, Tamaoki 2017 and Woltz 2017a to be at high risk of bias because more participants in the conservatively treated group were lost to follow‐up at the end of the follow‐up period. Mirzatolooei 2011 and Smekal 2009 did not perform an intention‐to‐treat analysis.
We judged Figueiredo 2008 to be at unclear risk because data were available at 15 months post‐intervention for only 40/50 (80%) participants, and they did not provide any information on the numbers missing from each group to allow assessment of whether there was an imbalance. We classified Melean 2015 as unclear because the study authors did not explicitly report if any participants were lost to follow‐up.
Selective reporting
Only two studies (Virtanen 2012a; Woltz 2017a) were considered at low risk of bias because the study protocol was available and all of the study pre‐specified outcomes that are of interest for this review have been reported in the pre‐specified way.
We classified 11 included studies at high risk of bias (Ahrens 2017; Chen 2011; COTS 2007; Figueiredo 2008; Judd 2009; Koch 2008; Melean 2015; Mirzatolooei 2011; Naveen 2017; Smekal 2009; Tamaoki 2017). The reasons for this assessment are as follows. Ahrens 2017; Chen 2011, COTS 2007, Figueiredo 2008, Melean 2015 and Naveen 2017 reported one or more outcomes of interest in the review incompletely. Judd 2009 assessed function or disability using non‐standard validated participant‐reported measures. Koch 2008 did not measure function or disability by validated participant‐reported measures. Neither Mirzatolooei 2011 nor Smekal 2009 presented baseline data for efficacy outcomes and reported only P values. Tamaoki 2017 registered the study protocol, and reported all of their pre‐specified (primary and secondary), outcomes that were of interest for this review in the pre‐specified way. However, the time points differ: the protocol plan was to follow up at 3, 6 and 12 months, but the results paper reports outcomes at six weeks, six months and one year for DASH and VAS, plus three months for VAS only, with no explanation given for these changes.
We judged Robinson 2013a to be at unclear risk because, despite the study protocol being registered, the pre‐specified outcomes were not recorded and were not available.
Other potential sources of bias
Six studies (Ahrens 2017; Judd 2009; Naveen 2017; Robinson 2013a; Tamaoki 2017; Virtanen 2012a), were at low risk of other bias, seven studies (Chen 2011; COTS 2007; Figueiredo 2008; Koch 2008; Mirzatolooei 2011; Smekal 2009; Woltz 2017a), were at high risk of other potential threats to validity, and one study (Melean 2015), was at unclear risk.
Chen 2011 and Figueiredo 2008 did not specify time points of outcomes. Four studies did not provide baseline outcome data, so we were unable to assess whether groups were balanced at baseline (COTS 2007; Koch 2008; Mirzatolooei 2011; Smekal 2009). There were unexplained imbalances in the numbers allocated into the two groups assigned (86 surgical; 74 conservative) in Woltz 2017a. Additionally, there were insufficient data to assess whether or not the two groups were balanced at baseline for this trial. The same insufficiency applied to Melean 2015, which we judged at unclear risk of other bias.
We were not able to analyse performance bias related to differences in rehabilitation and experience of surgeons and other care providers because the included studies did not report information related to these aspects.
No study was judged at risk of bias relating to inappropriate influence of funders.
Effects of interventions
See: Table 1
The primary comparison in this review was any surgical intervention versus any conservative intervention. We have presented secondary subgroup analyses by types of surgical interventions (plate fixation and intramedullary fixation), for function and primary treatment failure. Further subgroup analyses were precluded by insufficient data.
Comparison: surgical versus conservative interventions for treating middle third clavicle fractures
Function or disability (primary outcome)
The variety of measures used to demonstrate overall function in the included studies is displayed in the analyses. Pooled data from 10 studies (838 participants), favoured the surgical group (standardised mean difference (SMD) 0.33, 95% CI −0.02 to 0.67) at follow‐up of one year or more; however, these results were highly heterogeneous (I² = 83%; Figure 4; Analysis 1.1). Moreover, this result equates to a mean improvement of 2.3 points (0.14 points worse to 4.69 points better), in favour of surgery on the Constant scale (0 to 100 scale; higher scores mean better function), which is not a clinically important difference. Thus there is low‐quality evidence, downgraded one level for serious risk of bias and one level for serious inconsistency, that there may be little or no difference between surgery and conservative treatment in function measured at one year. The minimal clinical important difference (MCID) of Constant scale ranges from 5.7 to 10.4 points (Henseler 2015; Kukkonen 2013; Simovitch 2018; Torren 2016).
4.
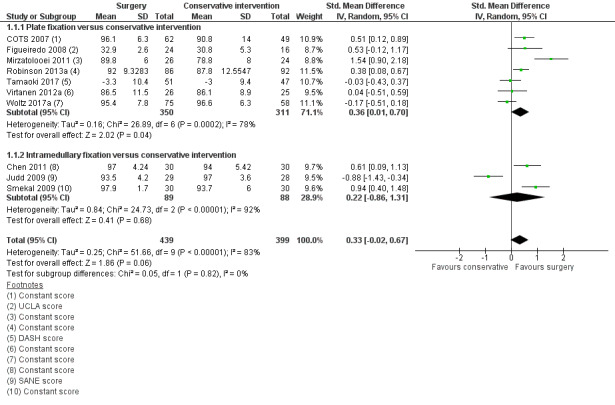
Forest plot of comparison 1. Surgical versus conservative interventions, outcome: 1.1 Function (overall at the end of follow‐up ‐ one year or more)
1.1. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 1 Function (overall at the end of follow‐up ‐ one year or more).
The results are subgrouped by types of surgical interventions (plate fixation versus intramedullary fixation), for exploratory purposes. The test for subgroup differences does not support a difference between the two surgical interventions (Chi² = 0.05, df = 1, P = 0.82, I² = 0%).
Upper limb functional outcome measures
DASH questionnaire (0 (best function) to 100 (worst function))
Pooled data (8 studies, 896 participants), demonstrated no apparent clinically important difference in disability (mean difference (MD) −3.87 points, 95% CI −7.75 to 0.01 points), at follow‐up of nine months or more, but the results were highly heterogeneous (I² = 90%; Analysis 1.2). The magnitude of the pooled difference and the 95% CI was less than 10 points, which is not considered a clinically relevant difference (Gummesson 2003; Hudak 1996). It is notable, however, that two studies found evidence of clinically important differences (COTS 2007; Mirzatolooei 2011). In particular, Mirzatolooei 2011 strongly favoured surgery (MD −12.70 points, 95% CI −15.22 to −10.18), with unusually high mean DASH scores in the conservative group.
1.2. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 2 DASH questionnaire at the end of follow‐up (0 (best function) to 100 (worst function)).
Constant score (0 (worst function) to 100 (best function))
The pooled analysis showed a small, clinically unimportant improvement in function in favour of surgical intervention (MD 3.83 points, 95% CI 1.75 to 5.91; 9 studies, 867 participants), at follow‐up of nine months or more; see Analysis 1.3. As above, there was substantial heterogeneity (I² = 75%); Mirzatolooei 2011 was again an outlier.
1.3. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 3 Constant score at the end of follow‐up (0 (worst function) to 100 (best function)).
UCLA score (2 (worst function) to 35 (best function))
A single study (Figueiredo 2008), found no significant difference between the two intervention groups (MD 2.10 points, 95% CI −0.70 to 4.90; 40 participants; Analysis 1.4).
1.4. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 4 UCLA score at the end of follow‐up ‐ one year or more (2 (worst function) to 35 (best function)).
Other scores
Based on the SANE score (0% to 100% scale with 100% being normal; MCID = 11.8 (Zhou 2018)), and L'Insalata score (0% to 100% scale with 100% being normal; MCID = not reported), Judd 2009 found better functional results at short‐term follow‐up in the surgical group (the result was clinically relevant at 3 weeks in assessing the SANE score: MD 13.4), but not at long‐term follow‐up, where the scores were higher in the conservative group (Analysis 1.5; Analysis 1.6).
1.5. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 5 SANE score (0 (worst function) to 100 (best function)).
1.6. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 6 L'Insalata score (0 (worst function) to 100 (best function)).
Pain (primary outcome)
Four studies reported pain, measured using a visual analogue scale. The pooled analysis from three studies (Tamaoki 2017; Virtanen 2012a; Woltz 2017a), showed a small improvement, of no important clinical significance, in pain (VAS: 0 to 100 mm (worst score)), at six weeks (MD ‐4.27 mm, 95% CI −8.18 to −0.37; MCID = 14 mm). There was no difference between the two groups at three months (MD −0.08 mm, 95% CI −3.64 to 3.48), or at one year (MD −0.60 mm, 95% CI −3.51 to 2.31; low‐quality evidence, downgraded one level for serious risk of bias and one level for serious imprecision; Analysis 1.7). The minimal clinical important difference (MCID) of visual analogue scale for shoulder injury is 14 mm (Simovitch 2018; Tashjian 2009; Tashjian 2017).
1.7. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 7 Pain (measured by VAS: 0 to 100 mm (worst score)).
We could not include data in the analysis from Koch 2008, which reported significantly better short‐term pain outcomes (VAS: 0 to 10 cm (worst score)), in the surgical group (mean VAS on days 5, 19 and 33 was 3.9, 2.9 and 1.6 cm for the surgery group and 5.1, 4.0 and 2.1 cm for the conservatively treated group; reported P < 0.05).
Virtanen 2012a found no significant differences between the two groups at three weeks (MD ‐6.00 mm, 95% CI −14.34 to 2.34 mm).
Treatment failure (primary outcome)
The difference in overall treatment failure was in favour of the surgical group (24/618 versus 77/579; risk ratio (RR) 0.32, 95% CI 0.20 to 0.50; 1197 participants, 12 studies; Analysis 1.8). We rated this low‐quality evidence, downgraded one level for serious risk of bias and one level for serious imprecision. We could not enter results on failure of treatment from Chen 2011 and for 13 participants from Naveen 2017 into the meta‐analysis because they reported data incompletely.
1.8. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 8 Treatment failure (participants who have a non‐routine secondary surgical intervention).
The most common cause of treatment failure in the conservatively managed group was symptomatic non‐union (8/561 (1.4%) versus 61/527 (11.6%); RR 0.20, 95% CI 0.10 to 0.40; 1088 participants, 10 studies); the percentage of symptomatic non‐union in the conservative‐treatment group ranged from 3.6% (1/28) in Judd 2009 to 15.4% in Ahrens 2017. The most common cause of treatment failure, reported in seven studies, in the surgically managed group was early mechanical failure (16/468 (3.4%)). Nine of the 16 cases of symptomatic malunion were reported in one study (COTS 2007).
When we subgrouped results for overall treatment failure by types of surgical interventions (plate fixation versus intramedullary fixation), for exploratory purposes, the test for subgroup differences did not show a difference between the two surgical interventions (Chi² = 0.48, df = 1, P = 0.49, I² = 0%; Analysis 1.9).
1.9. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 9 Total treatment failure ‐ subgrouped by type of surgery.
Cosmetic result
Deformity or asymmetry, or both, were more frequent in the conservative group (RR 0.16, 95% CI 0.05 to 0.46; 759 participants; 8 studies; I2 = 70%), and hardware prominence or irritation not requiring removal (RR 7.75, 95% CI 2.33 to 25.78; 592 participants; 6 studies; I2 = 0%), in the surgical group (Analysis 1.10). The pooled results for participants with cosmetic problems (e.g. deformities or imperfections such as scarring or bumps) favoured surgery (RR 0.55, 95% CI 0.31 to 0.98; 1130 participants, 11 studies; I2 = 63%; very low‐quality evidence downgraded one level for risk of bias, one level for imprecision, and one of inconsistency; Analysis 1.11). Full data on cosmetic results, either relating to individual cosmetic outcomes or participants with one or more unfavourable cosmetic outcomes, were not available. A sensitivity analysis, in which we replaced the derived data for two studies with that for participant dissatisfaction with cosmetic result, showed less difference between the two groups (RR 0.68, 95% CI 0.33 to 1.40; I2 = 70%).
1.10. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 10 Cosmetic result ‐ individual complications.
1.11. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 11 Participants with cosmetic problems.
Adverse events
Analysis 1.13 presents separate analyses by types of adverse events. These show that infection or dehiscence, or both, occurred only after surgery (22/686 versus 0/641; RR 5.62, 95% CI 1.95 to 16.15; 11 studies). This applied also to hardware irritation requiring removal (52/508 versus 1/483; RR 9.75, 95% CI 3.91 to 24.31; 9 studies), except in Woltz 2017a, which, following the intention‐to‐treat principle, included one participant who was randomised to non‐operative treatment but received plate fixation within a week because of pain. Skin and nerve problems were also more common after surgical treatment (75/338 versus 17/310; RR 4.86, 95% CI 1.85 to 12.76; 6 studies). Conversely, symptomatic malunion was much more common in the conservative‐treatment group (5/425 versus 45/397; RR 0.17, 95% CI 0.09 to 0.35; 9 studies); this analysis was dominated by Mirzatolooei 2011, which reported, without details of the symptoms, nearly half of the malunions (24 of 50). Potentially linked with this was the slightly greater number of the more serious cases of stiffness or restriction of shoulder movement in the conservative group (3/220 versus 8/202; RR 0.41, 95% CI 0.11 to 1.48; 4 studies). There were no obvious between‐group differences in the rarer reported adverse outcomes such as refracture (6 cases); complex regional pain syndrome (1 case); or other adverse events, such as thrombosis, cardiovascular events, impingement symptoms, transient plexus irritation and adhesive capsulitis (Analysis 1.13).
1.13. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 13 Adverse events ‐ individual complications.
Total of participants with adverse event outcome
This outcome included participants with any complication, such as wound infection and dehiscence, hardware irritation requiring removal of the fixation device typically associated with surgery, and complications such as shoulder stiffness and symptomatic malunion that occur more commonly with conservative treatment. These adverse events did not include non‐union or other treatment failures. Several studies did not report this outcome and so we established a rule to avoid the risk of unit of analysis problems where individual complications could have occurred together in one person. Although slightly favouring non‐surgical treatment, the heterogeneous data pooled from all 14 studies did not confirm a difference between the two treatment groups (109/678 versus 72/639; RR 1.34, 95% CI 0.68 to 2.64; 1317 participants; I2 = 72%; very low‐quality evidence downgraded one level for risk of bias, one level for imprecision, and one for inconsistency; Analysis 1.14). A sensitivity analysis based on reported complications that disregarded the potential unit of analysis problems had a similar finding (Analysis 1.15). When we subgrouped the results by type of surgical intervention (plate fixation versus intramedullary fixation), for exploratory purposes, the test for subgroup differences did not show a difference between the two surgical interventions (Chi² = 0.22, df = 1, P = 0.64, I² = 0%; Analysis 1.16).
1.14. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 14 Participants with adverse events.
1.15. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 15 Sensitivity analysis: participants with adverse events.
1.16. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 16 Participants with adverse events ‐ subgrouped by type of surgery.
Health‐related quality of life
The two studies that reported health‐related quality of life reported separate physical and mental component scores for either the SF‐12 (Robinson 2013a), or the SF‐36 ( Woltz 2017a). Pooled data from the two studies (321 participants), at 12 months indicates that there is no statistical nor clinical difference in quality of life (0 to 100 scale, where 100 is best score), either for physical component (MD 0.30 points, 95% CI −1.95 to 2.56) or mental component (MD 1.31 points, 95% CI −0.34 to 2.97; Analysis 1.17). We consider this to be low‐quality evidence, downgraded one level for serious risk of bias and one level for serious imprecision. Analysis 1.17 also presents the six‐week and three‐month results from Woltz 2017a. The minimal clinical important difference (MCID) of SF‐36 ranges from 2.0 to 7.8 points (scale 0 to 100; Andresen 2018; Angst 2001; Laucis 2015).
1.17. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 17 Health‐related quality of life: SF‐36 or SF‐12 (0 (worst quality of life) to 100 (best quality of life).
Return to previous activities
Pooled data from three studies (Figueiredo 2008; Melean 2015; Tamaoki 2017), found significantly better results in favour of the surgical group with respect to time to return to previous activities in days (MD −24.64 days, 95% CI −36.36 to −12.91 days; low‐quality evidence, downgraded one level for serious risk of bias and one level for serious imprecision; Analysis 1.18). Robinson 2013a reported that there was no difference between the two groups in the time to return to work (mean 22.0 versus 24.2 days; reported P = 0.7).
1.18. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 18 Time to return to previous activities (days).
Data from Koch 2008 showed a greater return in the surgical group to sport activities after two months (28/35 versus 18/33; RR 1.47, 95% CI 1.03 to 2.09; very low‐quality evidence, downgraded one level for serious risk of bias and two levels for very serious imprecision; Analysis 1.19). Robinson 2013a reported that there was no difference between the two groups in the numbers returning to their former sports activities or in the time for them to do this.
1.19. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 19 Number of participants returning to sport activities after two months.
Asymptomatic non‐union
Pooled data from seven studies showed higher numbers with asymptomatic non‐union in the conservative group (3/434 versus 43/411; RR 0.12, 95% CI 0.05 to 0.30; Analysis 1.20).
1.20. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 20 Asymptomatic non‐union.
Sensitivity analyses
We found that overall function at the end of follow‐up (one year or more), did not differ between groups in the primary analysis (i.e. including all studies; SMD 0.33, 95% CI −0.02 to 0.67), nor in the sensitivity analysis, where only studies at low risk of selection bias were included (SMD 0.19, 95% CI −0.17 to 0.55; data not shown). We were unable to assess the effect of including studies at high risk of detection bias, as all studies in the meta‐analysis failed to blind the outcome assessor.
We also performed a sensitivity analysis to investigate the effects of missing data on overall treatment failure. In the worst‐case scenario, we found a significant difference in favour of surgical intervention (RR 0.48, 95% CI 0.37 to 0.61; data not shown); for the best‐case scenario, we also found a statistically significant difference in favour of surgery (RR 0.34, 95% CI 0.22 to 0.54; data not shown).
Given that all included studies were of comparable size, with the exception of the slightly larger COTS 2007, we could not test for small sample bias. We also were unable to assess the effect of including studies of participants with a history of shoulder injury, because of inadequate reporting of this information in the studies.
Discussion
Summary of main results
We included 14 studies involving 1469 participants that assessed the effectiveness of surgical interventions compared with conservative interventions for treating people with middle third clavicle fracture. Ten studies compared plate fixation with sling or figure‐of‐eight bandage, or both, and four studies compared intramedullary fixation with wearing either a sling or a figure‐of‐eight bandage.
Not all of the included studies provided evidence for all the important outcomes, and the quality of evidence for important outcomes was low and, sometimes, very low.
We have summarised the main findings of the review in Table 1. Low‐quality evidence indicates, that compared with conservative treatment, surgery to treat clavicle fracture may not result in a significant improvement in upper arm function at one year or more. We downgraded the quality of the evidence due to risk of bias and high statistical heterogeneity. Low‐quality evidence (downgraded due to serious risk of bias and serious imprecision), indicates that there may be no difference in pain between treatments at one year. Low‐quality evidence (downgraded one level for serious risk of bias and one level for serious imprecision), shows that the risk of treatment failure (number of participants who had non‐routine secondary surgical intervention (excluding hardware removal) for symptomatic non‐union, malunion or other complication), may be lower after surgery. The main source of treatment failure was mechanical failure (3.4%), in the surgery group and symptomatic non‐union (11.6%), in the conservative‐treatment group. We are uncertain whether surgery results in fewer people having one or more cosmetic problems such as deformities, which were more common after conservative treatment, or hardware prominence or scarring that only occurred in the surgery group (very low‐quality evidence downgraded one level each for serious risk of bias, imprecision and inconsistency). Hardware prominence and unsightly scarring occurred only in the surgery group, and cosmetic deformity was more common after conservative treatment. We are uncertain whether there is any difference between surgery and conservative treatment in the risk of incurring an adverse outcome, including local infection, dehiscence, symptomatic malunion, discomfort leading to implant removal, and skin and nerve problems (very low‐quality evidence downgraded one level each for serious risk of bias, imprecision and inconsistency). Common adverse outcomes in the surgery group were hardware removal for discomfort and infection, and in the conservative‐treatment group, symptomatic malunion was common. There was low‐quality evidence (downgraded due to serious risk of bias and serious imprecision), of no between‐group difference in quality of life (physical component or mental component) at one year.
Overall completeness and applicability of evidence
The 13 RCTs and one quasi‐RCT included in this review recruited 1469 participants but there was often a substantial drop in the data available for pooling. For our primary outcomes, there were 838 participants from 10 studies that contributed data to function at 12 months, 277 participants from three studies that contributed data to pain at 12 months, and 1197 participants from 12 studies that contributed data to treatment failure.
Overall, the review population was adults and predominantly male participants, with older people generally excluded. In addition, the main comparison was plate fixation versus simple sling. All 14 included studies assessed only adults with displaced or angulated middle third clavicle fractures, meaning that we were unable to perform subgroup analyses by type of fracture. In addition, the included studies did not present outcome data to allow subgroup analysis based on timing of surgery, two fragments versus more than two fragments, and open versus closed fractures. Information regarding timing of surgery and type of fractures (characteristic of fracture), is also important to planning for trauma centres.
Although all of the included studies are relevant to current practice, it is probable that some interventions are now infrequently used, such as modified Hagie pin in Judd 2009 and reconstruction plates in Mirzatolooei 2011, Tamaoki 2017 and Virtanen 2012a. Currently it is much more common practice to use either a titanium elastic nail for intramedullary fixation and a precontoured clavicular plate for plate fixation. Furthermore, the applicability of the interventions' findings is primarily related to young, mainly male adults, with displaced or angulated middle third clavicle fracture. Therefore, the applicability of the evidence from this review is uncertain in relation to the treatment of undisplaced clavicle fractures or fractures in older women, an important subgroup of the population incurring these fractures.
All the studies failed to measure all the outcomes of importance; notably, only four studies measured pain, with only three of them providing data for long‐term pain. Another important problem is related to the reporting of cosmetic results and adverse events; we observed that individual outcomes contributing to these 'composite' outcomes were variably and poorly reported in the studies and, moreover, data for numbers with a poor cosmetic outcome or adverse event were typically not available.
Quality of the evidence
The evidence was of low quality for function, pain, treatment failure and heath‐related quality of life, and very low quality for numbers of participants with one or more cosmetic problems or those with adverse events; see Table 1. We downgraded the quality of the evidence by one level for all outcomes as the result of methodological flaws, including lack of adequate allocation concealment in the majority of studies and failure to blind the outcome assessor in all studies. Only four included studies (Ahrens 2017; Robinson 2013a; Tamaoki 2017; Woltz 2017a), reported according to the standards of the CONSORT statement (Schulz 2010). We downgraded the quality of evidence for several outcomes (function, cosmetic problem, adverse events), for inconsistency, where there was evidence of statistical heterogeneity, in particular relating to differences in direction of effect among studies. We downgraded for the quality of evidence for all outcomes except function for imprecision due to the small number of events or totals. We did not downgrade for indirectness and we think the possibility of publication bias is low.
Consequently, the quantitative results of this review should be interpreted with caution and viewed, at this stage, as requiring confirmation by evidence from larger studies.
Potential biases in the review process
We planned and conducted this updated review in accordance with criteria and methods set out in a published protocol (Lenza 2011), and previous review (Lenza 2013). We believe that our search strategy was comprehensive, with no language restrictions applied, and it has been maintained properly and regularly updated by the contact author (ML). It included handsearching of conference proceedings and searches for ongoing and recently completed studies. However, it is possible that we have missed some potentially eligible studies. We tried to contact authors of all included studies but with only limited success. We obtained standard deviations of DASH and Constant scores through personal contact with the authors of two studies (Ahrens 2017; Mirzatolooei 2011). Standard deviations and means of VAS scores were also obtained by personal contact with the authors of one study (Woltz 2017a).
Our search date was December 2017. However, in November 2018, during editorial processing of this review update, NCT01078480, one of our listed ongoing studies, was published (Qvist 2018). This multicentre, parallel RCT included 146 participants, who were randomised to either fixation with a pre‐contoured plate and locking screws or treatment with a sling. The study authors reported that after six months and one year, there was no statistically‐significant between‐group difference in the median DASH or Constant scores. The rate of treatment failure was lower in the surgical group. It is notable that these findings, in relation to overall function and treatment failure at 12 months are consistent with our current review findings. Thus we do not consider the date of last search or the non‐inclusion of this study to be an important source of bias.
Currently, a small number of specific validated scores can be used to assess shoulder function. When pooling results from studies that included more than one measure of function, for the purpose of pooling data for the 'Summary of findings' table, we decided to choose the Constant score as the default because it is more specific for shoulder function than the DASH questionnaire score; and, when compared with the UCLA, SANE and L'Insalata scores, the Constant score is most commonly used in the literature.
We had to make assumptions about the data in calculating the composite adverse event and cosmetic result outcomes. The studies counted several types of events, leading to potential unit of analysis issues, as participants were likely to have had more than one complication or cosmetic problem. To minimise the risk of double counting events, we aimed to extract the number of participants with one of the individual events as a proxy; we chose the component event with the most cases in each treatment group. There is some uncertainty about the effect estimates for these outcomes. (We have made our decisions transparent by reporting the number of cases with each component event of the composite event, and the number of cases we used in our analyses in the notes section of the Characteristics of included studies table.)
Agreements and disagreements with other studies or reviews
Many recent systematic reviews demonstrate the ongoing interest in the comparison between surgical versus conservative interventions to treat middle third clavicle fracture in adults. In the first version of our review, we described four published systematic reviews on this topic (Duan 2011; McKee 2012; Virtanen 2012b; Zlowodzki 2005), and discussed their findings in relation to ours (Lenza 2013). We found that our conclusions contrasted with those of these four reviews because we restricted our results to data from RCTs, extracted the data from included studies in accordance with our pre‐established endpoints and developed sensitivity analyses of our results. In addition, our risk of bias was less favourable than that of McKee 2012, as the authors used a scale to assess study quality. We pointed out that scales are not recommended because they provide unreliable assessments of validity (Juni 1999).
Our search update resulted in the identification of 12 new systematic reviews that assessed this comparison: one review was published in 2012 (Ban 2012), two in 2013 (Liu 2013; Xu 2013), three in 2014 (Kong 2014; Rehn 2014; Xu 2014), four in 2015 (Devji 2015; Walton 2015; Wang 2015a; Wang 2015b), and two in 2017 (Smeeing 2017; Woltz 2017b).
Ban 2012 assessed RCTs and cohort studies that evaluated treatments for clavicle fracture; the authors included three RCTs that compared surgery versus conservative treatment, and we included all of them in our review (COTS 2007; Mirzatolooei 2011; Smekal 2009). The reported results of the three RCTs were similar to our review. Ban 2012 also included one prospective cohort study that we excluded from our review (Kulshrestha 2011), and another RCT that compared plate versus intramedullary fixation (Ferran 2010). The authors concluded that surgery with plate fixation resulted in a better functional outcome and lower malunion and non‐union rates than conservative treatment.
Liu 2013 included the results of eight studies with 663 participants, that compared surgical versus conservative interventions, amongst them four RCTs that we evaluated in our review (COTS 2007; Judd 2009; Smekal 2009; Virtanen 2012a), one abstract (Smith 2001), that we listed as a study awaiting classification (see Characteristics of studies awaiting classification), and three controlled clinical studies (Bohme 2011; Jubel 2005; Kulshrestha 2011), that we excluded from our review (see Characteristics of excluded studies). The authors found that there were statistically significant lower incidences of non‐union, malunion and neurological complications after surgery.
Xu 2013 assessed RCTs that compared surgical versus conservative interventions for clavicle fracture. They included three RCTs that we evaluated in our review (COTS 2007; Mirzatolooei 2011; Smekal 2009), and one abstract (Smith 2001). Their results showed that data from three RCTs and one abstract with a total of 321 participants concluded that surgery was more effective than conservative treatment regarding the rate of non‐union, malunion and overall complications. The meta‐analysis that they carried out also showed better functional outcomes in the surgical treatment groups.
Kong 2014 evaluated six RCTs that compared surgical versus conservative interventions for clavicle fracture, all of which we included in our review (COTS 2007; Judd 2009; Mirzatolooei 2011; Robinson 2013a; Smekal 2009; Virtanen 2012a). Their interpretation of risk of bias (qualitative analysis), was similar to ours. The meta‐analyses were also similar, and the authors found benefits of surgery, which included improvement of function, a low rate of non‐union and malunion; and benefits of conservative interventions, such as low rate of adverse events. They concluded that further studies are warranted.
Rehn 2014 included the results of five RCTs, with 369 participants, that we evaluated in our review (COTS 2007; Judd 2009; Smekal 2009; Virtanen 2012a). The authors stated that time to union was shorter and functional endpoints were better with surgery, particularly at short‐term follow‐up. They also reported a higher incidence of complications that required additional major surgery in the conservative group, and minor complications were higher in the surgical intervention groups. Due to the level of evidence included in the review, the authors concluded that the evidence does not support either surgery or conservative treatment to clavicle fractures.
Xu 2014 assessed RCTs that compared surgical versus conservative interventions for clavicle fracture. They included six RCTs that we evaluated in our review (COTS 2007; Judd 2009; Mirzatolooei 2011; Smekal 2009; Virtanen 2012a; Witzel 2007), and one abstract (Smith 2001). Witzel 2007 reported the same results in two papers (Koch 2008; Witzel 2007), and we reported Koch 2008 as default. Their results showed that surgery leads to significantly lower incidence of non‐union and better function scores; their pooled data showed that there was no statistically significant difference regarding total complications between surgery and conservative interventions.
Devji 2015 included 15 RCTs (nine studies comparing surgery and conservative interventions, five comparing implants for surgical treatment, and one comparing conservative treatments). We also evaluated all nine RCTs that compared surgical versus conservative interventions to treat clavicle fractures (Chen 2011; COTS 2007; Figueiredo 2008; Judd 2009; Koch 2008; Mirzatolooei 2011; Robinson 2013a; Smekal 2009; Virtanen 2012a). Their interpretation of risk of bias (qualitative analysis) was similar to ours. The pooled data demonstrated that the incidence of secondary operations and all complications did not differ between the surgical and conservative interventions. There was functional improvement at one year in the surgical group; however, this difference was clinically unimportant. They concluded that the current evidence does not support surgery for treating clavicle fractures.
Walton 2015 systematically reviewed the literature to assess the cost analysis of surgery versus conservative interventions to treat clavicle fractures. They included four RCTs (COTS 2007; Judd 2009; Smekal 2009; Virtanen 2012a), that we assessed in our review. Based on the four RCTs they reported that conservative treatment for clavicle fractures in adults is more cost‐effective than surgical interventions. They concluded that conservative interventions in adults are the optimal financial decision for the payer.
Wang 2015a included 13 studies comparing surgical versus conservative treatment for clavicle fractures, only eight of which were included in our review (Chen 2011; COTS 2007; Figueiredo 2008; Judd 2009; Mirzatolooei 2011; Robinson 2013a; Smekal 2009; Virtanen 2012a). The remaining five studies that they included (Bohme 2011; Jubel 2005; Khorami 2014; Kulshrestha 2011; Smith 2001), we excluded for the reasons stated in Characteristics of excluded studies and Studies awaiting classification. Pooled data from the review showed that surgery was more effective in reducing the rates of non‐union, symptomatic malunion, neurological symptoms and overall complications. Moreover, function scores were significantly improved after surgery at follow‐up of one year or more. The authors concluded that surgery could be better than conservative intervention, however they did not support surgery as routine to be done for all displaced clavicle fractures.
Wang 2015b reported on a Bayesian network meta‐analysis that included 13 RCTs, comprised of four studies comparing implants for surgical treatment and nine studies comparing surgery and conservative interventions (COTS 2007; Dugar 2013; Figueiredo 2008; Judd 2009; Koch 2008; Mirzatolooei 2011; Robinson 2013a; Smekal 2009; Virtanen 2012a). We included and analysed all these studies in our review, except Dugar 2013, which we excluded because it included participants who also had medial and lateral third clavicle fractures (16.6%), and they did not report results separately. The authors of Wang 2015b found higher non‐union rates after conservative treatment than after surgery, but that study did not assess function and treatment failure.
Smeeing 2017 included eight RCTs and 12 observational studies; we included the eight RCTs in our review (Chen 2011; COTS 2007; Judd 2009; Melean 2015; Mirzatolooei 2011; Robinson 2013a; Virtanen 2012a; Witzel 2007). Pooled data from the review showed that rates of non‐union were significantly higher after surgical treatment than after conservative; the risk of malunions did not differ between surgical and conservative treatment; and there was a significant difference in function outcomes that favoured surgical treatment.
Woltz 2017b systematically reviewed the literature of surgery versus conservative interventions for treating clavicle fractures. They included six RCTs (COTS 2007; Melean 2015; Mirzatolooei 2011; Robinson 2013a; Virtanen 2012a; Woltz 2017a), which we assessed in our review. Pooled data showed that plate fixation significantly reduced the rate of non‐union when compared with conservative treatment; in addition, plate fixation also resulted in better function scores, however, the clinical relevance of this difference was unclear. The authors concluded that they did not support routine plate fixation for all patients, but an individualised treatment based on shared decision‐making.
Summary
In summary, the 12 newly listed systematic reviews are now out of date because none of them include three new studies (Ahrens 2017; Naveen 2017; Tamaoki 2017), one of which (Ahrens 2017), is a large multicenter study. Our results, which demonstrated no clinical differences between the two interventions in terms of shoulder function, pain and quality of life, often contrasted with those of the 12 systematic reviews described above.
Authors' conclusions
Implications for practice.
Overall, there is low‐quality evidence available from randomised controlled trials on the relative effectiveness of surgical versus conservative treatment for acute middle third clavicle fracture. Based on low‐quality evidence from 14 studies, surgical intervention may have no additional benefits in terms of function, pain and quality of life compared with conservative treatments, but may result in fewer treatment failures overall (participants who have undergone or are being considered for a non‐routine secondary surgical intervention for symptomatic non‐union, malunion, mechanical failure or other complications). Although we are uncertain whether the overall risk of adverse events differs between surgical and conservative treatment, the nature of the events needs to be taken into account. Thus the risk of surgical adverse events, including wound infection or dehiscence, and hardware irritation, should be balanced against the risk of adverse events that may be more commonly associated with conservative treatment, such as symptomatic malunion and shoulder stiffness. We are also uncertain about the finding that the cosmetic result was marginally in favour of the surgical group, Again, there is need for consideration of the nature of the individual cosmetic outcomes, some of which are specific to surgery, such as unsightly scarring and hardware prominence, and others of which are more common to conservative treatment, such as shoulder deformity.
Until conclusive evidence becomes available, treatment options must be chosen on an individual patient basis, with careful consideration of the relative benefits and harms of each intervention and patient preferences.
Implications for research.
In part as preparation for future studies of treatment interventions for these fractures, research is needed to identify or develop, and then validate, condition‐specific patient‐reported outcome measures of function and satisfaction with outcome. In addition to providing a focus on patient‐reported measures of function and satisfaction, at minimum, all future studies should collect pain outcomes, adverse events and cost outcomes. Systematic data collection to assess short‐, medium‐ and long‐term outcomes after treatment (e.g. during the first month, six months and one year), is important. We also recommend that future RCTs should adhere to reporting standards following the CONSORT statements (Schulz 2010), and provide full data for continuous outcomes and totals for participants with adverse events. Further research could also be helpful in identifying those subgroups of the population with a higher non‐union rate; this could inform study design, such as encouraging people not to smoke as part of the treatment plan, subgrouping within clinical studies, or provide a rationale for focusing on the subgroup of patients most likely to benefit from surgical intervention.
Feedback
Feedback submitted 11 March 2014
Summary
Dear Mr Lenza
I read your review ''Surgical versus conservative interventions for treating fractures of the middle third of the clavicle'' with interest. The review states that there is no statistically significant difference in outcomes between surgical and conservative interventions. However, the review does demonstrate a statistically significant difference between plate fixation and conservative management.
Analysis 1.1 demonstrates that there is no statistically significant difference where the analysis compares all types of surgical intervention with conservative treatment. This would seem to support the conclusion of the review. However, when the surgical interventions are subgrouped, so that intramedullary fixation and plate fixation are separately compared with conservative treatment, there is a significant difference between plate fixation and conservative treatment in favour of plate fixation (SMD is 0.63; 95% CI 0.08 to 1.19; P = 0.03). This finding is not fully reported in the review itself.
In my opinion this is a relevant finding because it shows that one of the surgical interventions (plate fixation) gives a significantly better functional outcome at one year compared with conservative treatment.
Shanti Kersten, Medical Student
Reply
Thank you for your interest in our review. We agree with you that our result for the endpoint function or disability at the end of follow‐up (one year) was statistically significantly better in patients who underwent plate fixation compared with conservative treatment (SMD 0.63, 95% CI 0.08 to 1.19; P = 0.03). However, the test for subgroup differences does not support a difference between the two types of surgical interventions (Chi2 = 0.43; df = 1; P = 0.51; I2 = 0%).
Additionally, though the result for plate fixation is statistically significant, it, like the overall result, is unlikely to correspond to a clinically relevant effect (the findings translate to 4.4 points, 95% CI 0.6 to 8.3 points on the Constant score). Ten points has been reported to be the minimal clinically important difference on the Constant score (Kukkonen 2013; Roy 2010).
While our main focus is on comparing the effects of surgical versus conservative interventions, we anticipate that there will be more evidence to inform subgroup analysis by implant type when we update this review.
Mario Lenza, Contact Author
Contributors
Mario Lenza, Contact Author Xavier Griffin, Feedback Editor for the Bone, Joint and Muscle Group Helen Handoll, Co‐ordinating Editor for the Bone, Joint and Muscle Group
What's new
| Date | Event | Description |
|---|---|---|
| 18 January 2019 | New citation required and conclusions have changed | In this update the byline has changed and some adjustments have been made to the conclusions. |
| 22 January 2018 | New search has been performed | In this update, published in Issue 1, 2019, we made the following changes:
|
History
Protocol first published: Issue 10, 2011 Review first published: Issue 6, 2013
| Date | Event | Description |
|---|---|---|
| 31 March 2014 | Feedback has been incorporated | This review incorporates a response to feedback sent 11 March 2014. There was no change to the review. |
Acknowledgements
For this review update, we are grateful for helpful feedback from Helen Handoll and Joanne Elliott at editorial review and Alison Armstrong at peer‐review. We also thank Joanne Elliott and Maria Clarke for editorial support. We thank Christina Geros, Cochrane Musculoskeletal, for assistance in data extraction of adverse events.
This project was supported by the National Institute for Health Research via Cochrane Infrastructure funding to the Cochrane Bone, Joint and Muscle Trauma. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
For previous acknowledgements see Lenza 2013.
Appendices
Appendix 1. Search strategies (December 2012 to December 2017)
We carried out the searches for this update in two stages: the first search was run from December 2012 to February 2017 and a top‐up search was run from February 2017 to December 2017.
CENTRAL (Central Register of Studies Online)
#1 MESH DESCRIPTOR Clavicle (93) #2 (clavic* or midclavic* or mid‐clavic* or collarbone):TI,AB,KY (277) #3 MESH DESCRIPTOR Fractures, Bone EXPLODE ALL TREES (3666) #4 MESH DESCRIPTOR Fracture Healing EXPLODE ALL TREES (401) #5 MESH DESCRIPTOR Fracture Fixation EXPLODE ALL TREES (1221) #6 fracture*:TI,AB,KY (11159) #7 #1 OR #2 (277) #8 #3 OR #4 OR #5 OR #6 (11175) #9 #7 AND #8 (124) #10 fracture*:TI,AB,KY AND 12/12/2012 TO 28/02/2017:DL (4973) #11 #9 AND #10 (85)
Top up search February 2017 to December 2017: (41)
MEDLINE (Ovid Online)
1 Clavicle/ (5175) 2 (clavic* or midclavic* or mid‐clavic* or collarbone).tw. (8899) 3 Fracture Healing/ or Fracture Fixation/ or Fractures, Bone/ (78785) 4 fracture*.tw. (210764) 5 (1 or 2) and (3 or 4) (3149) 6 Randomized controlled trial.pt. (448750) 7 Controlled clinical trial.pt. (91973) 8 randomized.ab. (389110) 9 placebo.ab. (184016) 10 Drug therapy.fs. (1935975) 11 randomly.ab. (271477) 12 trial.ab. (408002) 13 groups.ab. (1674679) 14 or/6‐13 (3981450) 15 exp Animals/ not Humans/ (4322524) 16 14 not 15 (3440241) 17 5 and 16 (380) 18 (201212* or 2013* or 2014* or 2015* or 2016* or 2017*).ed,dc. (5275296) 19 17 and 18 (176)
Top up search February 2017 to December 2017: (96)
The subject‐specific search (lines 1 to 5) is combined with the sensitivity‐maximizing version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (Lefebvre 2011)
Embase (Ovid Online)
1 Clavicle/ (6757) 2 (clavic* or midclavic* or mid‐clavic* or collarbone).tw. (10711) 3 1 or 2 (12294) 4 exp Fracture Healing/ or exp Fracture Treatment/ or exp Fracture/ (303282) 5 fracture*.tw. (247807) 6 4 or 5 (350730) 7 3 and 6 (3860) 8 Clavicle Fracture/ (2608) 9 7 or 8 (4636) 10 Randomized controlled trial/ (476924) 11 Clinical trial/ (1028761) 12 Controlled clinical trial/ (471567) 13 Randomization/ (84616) 14 Single blind procedure/ (29283) 15 Double blind procedure/ (139687) 16 Crossover procedure/ (55016) 17 Placebo/ (327446) 18 Prospective study/ (397807) 19 randomi#ed.tw. (669824) 20 ((clinical or controlled or comparative or placebo or prospective*) adj3 (trial or study)).tw. (899383) 21 (random* adj7 (allocat* or allot* or assign* or basis* or divid* or order*)).tw. (246558) 22 ((singl* or doubl* or trebl* or tripl*) adj7 (blind* or mask*)).tw. (200784) 23 (cross?over* or (cross adj1 over*)).tw. (86882) 24 ((allocat* or allot* or assign* or divid*) adj3 (condition* or experiment* or intervention* or treatment* or therap* or control* or group*)).tw. (331457) 25 RCT.tw. (23238) 26 or/10‐25 (2604732) 27 (2012* or 2013* or 2014* or 2015* or 2016* or 2017*).dd,dc,yr,dp,em. (29380777) 28 9 and 26 and 27 (558)
Top up search February 2017 to December 2017: (81)
LILACS (Bireme)
Mh clavicle OR Tw clavic$ OR Tw midclavic$ OR Tw mid‐clavic$ OR Tw collarbone [Words]
and
Mh fracture healing OR Mh fracture fixation OR Mh fractures OR Tw fractur$ [Words]
and
((Pt randomized controlled trial OR Pt controlled clinical trial OR Mh randomized controlled trials OR Mh random allocation OR Mh double‐blind method OR Mh single‐blind method) AND NOT (Ct animals AND NOT (Ct human and Ct animal)) OR (Pt clinical trial OR Ex E05.318.760.535$ OR (Tw clin$ AND (Tw trial$ OR Tw ensa$ OR Tw estud$ OR Tw experim$ OR Tw investiga$)) OR ((Tw singl$ OR Tw simple$ OR Tw doubl$ OR Tw doble$ OR Tw duplo$ OR Tw trebl$ OR Tw trip$) AND (Tw blind$ OR Tw cego$ OR Tw ciego$ OR Tw mask$ OR Tw mascar$)) OR Mh placebos OR Tw placebo$ OR (Tw random$ OR Tw randon$ OR Tw casual$ OR Tw acaso$ OR Tw azar OR Tw aleator$) OR Mh research design) AND NOT (Ct animals AND NOT (Ct human and Ct animals)) OR (Ct comparative study OR Ex E05.337$ OR Mh follow‐up studies OR Mh prospective studies OR Tw control$ OR Tw prospectiv$ OR Tw volunt$ OR Tw volunteer$) AND NOT (Ct animals AND NOT (Ct human and Ct animals))) [Words] (17)
Top up search February 2017 to December 2017: (13)
ClinicalTrials.gov
clavicle fracture OR clavicular fracture (35)
WHO ICTRP
clavicle fracture OR clavicular fracture (158)
Appendix 2. Search results reported in previous version of the review (Lenza 2013)
The search strategy (completed December 2012), identified a total of 456 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (30 records); Cochrane Central Register of Controlled Trials (28), PubMed (119), EMBASE (150), LILACS (17), ClinicalTrials.gov (61) and the WHO International Clinical Trials Registry Platform (51). We also identified four potentially eligible studies from other sources (by the studies that were included in other published reviews).
The search resulted in identification of the citations of 42 reports of potentially eligible studies, for which (where possible) full reports were obtained. A total of eight studies with data published across other publications (18 reports), published between 2007 and 2012, were included in the review (Chen 2011; COTS 2007; Figueiredo 2008; Judd 2009; Koch 2008; Mirzatolooei 2011; Smekal 2009; Virtanen 2012a). Just one trial was preceded by trial registration (Virtanen 2012a).
Overall, there are eight included studies, 10 excluded studies, eight ongoing studies and three studies awaiting classification (Figure 1).
Data and analyses
Comparison 1. Surgical versus conservative interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Function (overall at the end of follow‐up ‐ one year or more) | 10 | 838 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [‐0.02, 0.67] |
| 1.1 Plate fixation versus conservative intervention | 7 | 661 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [0.01, 0.70] |
| 1.2 Intramedullary fixation versus conservative intervention | 3 | 177 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.86, 1.31] |
| 2 DASH questionnaire at the end of follow‐up (0 (best function) to 100 (worst function)) | 8 | 896 | Mean Difference (IV, Random, 95% CI) | ‐3.87 [‐7.75, 0.01] |
| 3 Constant score at the end of follow‐up (0 (worst function) to 100 (best function)) | 9 | 867 | Mean Difference (IV, Random, 95% CI) | 3.83 [1.75, 5.91] |
| 4 UCLA score at the end of follow‐up ‐ one year or more (2 (worst function) to 35 (best function)) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 SANE score (0 (worst function) to 100 (best function)) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 At three weeks | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 At six months | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 At one year | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 L'Insalata score (0 (worst function) to 100 (best function)) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 At three weeks | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 At six months | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 At one year | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain (measured by VAS: 0 to 100 mm (worst score)) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 At 3 weeks | 1 | 51 | Mean Difference (IV, Fixed, 95% CI) | ‐6.0 [‐14.34, 2.34] |
| 7.2 At 6 weeks | 3 | 283 | Mean Difference (IV, Fixed, 95% CI) | ‐4.27 [‐8.18, ‐0.37] |
| 7.3 At 3 months | 3 | 284 | Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐3.64, 3.48] |
| 7.4 At 1 year | 3 | 277 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐3.51, 2.31] |
| 8 Treatment failure (participants who have a non‐routine secondary surgical intervention) | 13 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Symptomatic non‐union | 10 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.10, 0.40] |
| 8.2 Symptomatic malunion | 5 | 601 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.03, 0.54] |
| 8.3 Early mechanical failure | 7 | 895 | Risk Ratio (M‐H, Random, 95% CI) | 5.14 [1.51, 17.50] |
| 8.4 Symptoms of brachial plexus irritation | 3 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.03, 2.81] |
| 8.5 Total treatment failure | 12 | 1197 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.20, 0.50] |
| 9 Total treatment failure ‐ subgrouped by type of surgery | 12 | 1197 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.20, 0.50] |
| 9.1 Plate fixation versus conservative intervention | 9 | 1012 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.18, 0.50] |
| 9.2 Intramedullary fixation versus conservative intervention | 3 | 185 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.13, 1.92] |
| 10 Cosmetic result ‐ individual complications | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 10.1 Deformity and/or asymmetry and/or shoulder droop | 8 | 759 | Risk Ratio (M‐H, Random, 95% CI) | 0.16 [0.05, 0.46] |
| 10.2 Hardware irritation and/or prominence not requiring removal | 6 | 592 | Risk Ratio (M‐H, Random, 95% CI) | 7.75 [2.33, 25.78] |
| 10.3 Unsightly scar | 5 | 515 | Risk Ratio (M‐H, Random, 95% CI) | 5.63 [1.51, 20.96] |
| 10.4 Bump at fracture site | 2 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.06, 0.34] |
| 11 Participants with cosmetic problems | 11 | 1130 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.31, 0.98] |
| 12 Sensitivity analysis: participants with cosmetic problems | 11 | 1130 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.33, 1.40] |
| 13 Adverse events ‐ individual complications | 14 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 Infection and/or dehiscence | 10 | 1327 | Risk Ratio (M‐H, Random, 95% CI) | 5.62 [1.95, 16.15] |
| 13.2 Hardware irritation requiring removal | 9 | 991 | Risk Ratio (M‐H, Random, 95% CI) | 9.75 [3.91, 24.31] |
| 13.3 Skin and nerve problems (incisional numbness or paresthesia)) | 6 | 648 | Risk Ratio (M‐H, Random, 95% CI) | 4.86 [1.85, 12.76] |
| 13.4 Stiffness/restricted of range of shoulder movement | 4 | 422 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.11, 1.48] |
| 13.5 Refracture | 3 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.18, 5.03] |
| 13.6 Symptomatic malunion | 9 | 822 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.09, 0.35] |
| 13.7 Complex regional pain syndrome | 1 | 111 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.01, 6.36] |
| 13.8 Others: various | 5 | 563 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.30, 2.57] |
| 14 Participants with adverse events | 14 | 1317 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.68, 2.64] |
| 15 Sensitivity analysis: participants with adverse events | 14 | 1317 | Risk Ratio (M‐H, Random, 95% CI) | 1.56 [0.77, 3.18] |
| 16 Participants with adverse events ‐ subgrouped by type of surgery | 14 | 1317 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.68, 2.64] |
| 16.1 Plate fixation versus conservative intervention | 10 | 1072 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [0.66, 3.32] |
| 16.2 Intramedullary fixation versus conservative intervention | 4 | 245 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.21, 4.60] |
| 17 Health‐related quality of life: SF‐36 or SF‐12 (0 (worst quality of life) to 100 (best quality of life) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 17.1 Physical Component score at 6 weeks | 1 | 148 | Mean Difference (IV, Random, 95% CI) | 2.60 [0.16, 5.04] |
| 17.2 Physical Component score at 3 months | 1 | 139 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐2.23, 2.43] |
| 17.3 Physical Component score at 1 year | 2 | 321 | Mean Difference (IV, Random, 95% CI) | 0.30 [‐1.95, 2.56] |
| 17.4 Mental Component score at 6 weeks | 1 | 148 | Mean Difference (IV, Random, 95% CI) | ‐1.5 [‐4.03, 1.03] |
| 17.5 Mental Component score at 3 months | 1 | 139 | Mean Difference (IV, Random, 95% CI) | ‐1.30 [‐3.49, 0.89] |
| 17.6 Mental Component score at 1 year | 2 | 321 | Mean Difference (IV, Random, 95% CI) | 1.31 [‐0.34, 2.97] |
| 18 Time to return to previous activities (days) | 3 | 214 | Mean Difference (IV, Random, 95% CI) | ‐24.64 [‐36.36, ‐12.91] |
| 19 Number of participants returning to sport activities after two months | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 20 Asymptomatic non‐union | 7 | 845 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.05, 0.30] |
1.12. Analysis.
Comparison 1 Surgical versus conservative interventions, Outcome 12 Sensitivity analysis: participants with cosmetic problems.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ahrens 2017.
| Methods |
Study design: multicentre RCT (20 centres) Duration of the study: July 2008‐December 2014 Protocol was published before recruitment of participants: yes. doi: 10.1186/1745‐6215‐12‐57 ‐ Trials 2011;12:57. Date of trial registration 7 September 2006, recruitment started 18 December 2007 Details of trial registration: yes. Main ID: United Kingdom Clinical Research Network ID: 8665. Date of registration: 7 September 2006 Funding sources: This study was funded with grants from BUPA Foundation and BESS. Dr. Ahrens reports grants from BESS, grants from BUPA Foundation, during the conduct of the study. |
|
| Participants |
Place of study: 20 acute‐care hospitals in England (UK) Number of participants assigned: 301 participants (154 surgical; 147 conservative) Number of participants assessed to primary outcome (DASH): 204 participants (111 surgical; 93 conservative) Inclusion criteria
Exclusion criteria
Age
Gender of participants assigned (male/female)
Classification of injury: fractures were classified according to the Robinson's Classification (Robinson 1998). |
|
| Interventions |
Timing of intervention: not specified; however, patients with > 14 days after the injury were excluded. In the operative group, the surgical procedure could be done within 3 months after randomisation. Type of surgical intervention: open reduction and plate fixation. Fixation was performed using the Acumed clavicle fixation system, consisting of a precontoured titanium plate. Type of conservative intervention: simple sling for 6 weeks Rehabilitation
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: 47 participants were lost to follow‐up at 9 months (analysed for fracture union) and 97 participants were not assessed the function (measured by DASH)
Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
|
|
| Notes | SDs and means of DASH and Constant scores were obtained by personal contact with the study authors. Composite adverse events: surgery: plate removal (n = 5); frozen shoulder (n = 2). In conservative: frozen shoulder (n = 1). In Analysis 1.14 we used event rates 5 for surgery and 1 for conservative. Cosmetic result events: surgery: minor scar (n = 3); prominent plate (n = 2). Conservative (n = 0). In Analysis 1.11 we used event rates 3 for surgery and 0 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation lists, stratified by centre, were produced using random permuted blocks and equal allocation to the operative and non‐operative groups. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded so there is potential for bias in radiographic outcomes. Participants were unblinded so there is potential for bias in self‐reported outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing function outcome data (DASH) were not balanced in numbers across intervention groups; more participants in the conservative intervention group were lost to follow‐up (43/154) (28%): surgical versus 54/147 (37%) conservative at 9 months. This may have led to an overestimation of the benefits of surgery. |
| Selective reporting (reporting bias) | High risk | Outcomes of interest in the review are reported incompletely, and the author failed to report any measure of variance for DASH and Constant scores. |
| Other bias | Low risk | The study appears to be free of other potential sources of bias. |
Chen 2011.
| Methods |
Study design: single‐centre, 2‐group, parallel‐design RCT Duration of the study: January 2007‐May 2008 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: not reported Funding sources: not reported |
|
| Participants |
Place of study: 1 centre from Wenzhou, China Number of participants assigned: 60 participants (30 surgical; 30 conservative) Number of participants assessed: 60 participants (30 surgical; 30 conservative) Inclusion criteria
Exclusion criteria
Age
Gender of participants assigned (male/female)
Classification of injury: fractures were classified according to the AO/OTA fracture classification and displacement and shortening of the fragments. |
|
| Interventions |
Timing of intervention
Type of surgical intervention: closed reduction and intramedullary fixation using a TEN with a 2‐3 mm diameter. 2 participants needed open reduction. Type of conservative intervention: simple sling for 3 weeks Rehabilitation: not reported Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up (mean/range): 15/10‐20 months Loss to follow‐up: none lost to follow‐up Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
|
|
| Notes | Failure of treatment and adverse events were described incompletely, and we were unable to include these data in the results; therefore, we did not include the endpoints in our analyses (we tried unsuccessfully to contact the study authors to obtain further information on failure and adverse events). Composite adverse events: surgery: superficial skin infection (n = 1); (skin irritation but linked with hardware prominence (n = 3)). Conservative: symptomatic malunion (n = 2); transient plexus irritation (n = 3). In Analysis 1.14 we used event rates 1 for surgery and 5 for conservative. Cosmetic result events: surgery: hardware prominence (n = 3). Conservative (n = 0). In Analysis 1.11 we used event rates 3 for surgery and 0 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The authors did not report missing data |
| Selective reporting (reporting bias) | High risk | Failure of treatment (as primary outcome) was reported incompletely so that we could not enter it in a meta‐analysis |
| Other bias | High risk | The time points of outcomes were not pre‐specified |
COTS 2007.
| Methods |
Study design: multicentre RCT (8 centres) Duration of the study: April 2001‐December 2004 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: not registered Funding sources: some of the study authors received grants or outside funding from the Orthopaedic Trauma Association and Zimmer Inc |
|
| Participants |
Place of study: 8 centres from Canada, including St. Michael's Hospital and Sunnybrook and Women's College Health Sciences Centre, Toronto; McMaster University Medical Center, Hamilton; Brantford General Hospital, Brantford; London Health Sciences Centre, London, Ontario; Royal Columbian Hospital, New Westminster, British Columbia; Montreal General Hospital, Montreal, Quebec; and Foothills Medical Centre, Calgary Number of participants assigned: 132 participants (67 surgical; 65 conservative) Number of participants assessed: 111 participants (1‐year follow‐up: 62 surgical, 49 conservative) and 95 participants (2‐year follow‐up: 52 surgical, 43 conservative). Inclusion criteria
Exclusion criteria
Age:
Gender of participants assessed (male/female)
Classification of injury: fractures were classified according to displacement, angulation and shortening of the fragments |
|
| Interventions |
Timing of intervention: not specified; however, participants with > 28 days after the injury were excluded Type of surgical intervention: open reduction and plate fixation (44 participants with limited contact dynamic compression plates; 15 with 3.5‐mm reconstruction plates; 4 with pre‐contoured plates; and 4 with other plates) Type of conservative intervention: standard sling for 6 weeks Rehabilitation:
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: 21 participants were lost to follow‐up at 1 year (COTS 2007) and 37 participants at 2 years (Schemitsch 2011)
Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
|
|
| Notes | SF‐36 questionnaire was assessed in a publication of COTS 2007 (Pearson 2010); however, the results were not available for analysis because the study authors did not report them. DASH and Constant scores presented graphically only We contacted the study authors to request data (i.e. SD for DASH and Constant scores); however, they declined to provide them. We extracted 12‐month Constant and DASH scores as reported in a review by the same authors (McKee 2012), extracted the (presumed) SEM from the graphical presentation of results and calculated the SD from the SEM. Composite adverse events: surgery: wound infection and/or dehiscence (n = 3); hardware irritation requiring removal (n = 5); incisional numbness (n = 18); sensitive and/or painful fracture site (n = 10); transient brachial plexus symptoms (n = 8). Conservative: symptomatic malunion (n = 9); sensitive and/or painful fracture site (n = 10); complex regional pain syndrome (n = 1); transient brachial plexus symptoms (n = 7). In Analysis 1.14 we used event rates 18 for surgery and 10 for conservative Cosmetic result events: surgery: deformity (n = 2); scar (n = 3); hardware prominence (n = 11). Conservative: deformity (n = 3); asymmetrical results (n= 22). In Analysis 1.11 we used event rates 14 for surgery and 22 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence generation was performed by a computer random number generator (personal contact) |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing outcome data were not balanced in numbers across intervention groups; more participants in the conservative intervention group were lost to follow‐up (5/67) (7%): surgical versus 16/65 (25%) conservative at 12 months; 15/67 (22%) surgical versus 22/65 (34%) conservative at 24 months. This may have led to an overestimation of the benefits of surgery. |
| Selective reporting (reporting bias) | High risk | Outcomes of interest in the review are reported incompletely, and the study author failed to report any measure of variance for DASH and Constant scores. |
| Other bias | High risk | The trial did not permit investigators to tell whether or not the 2 groups were balanced at baseline for the primary outcomes. |
Figueiredo 2008.
| Methods |
Study design: single‐centre, 2‐group, parallel‐design RCT Duration of the study: August 2005‐January 2007 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: not registered Funding sources: none known |
|
| Participants |
Place of study: 1 centre from Taubaté, Brazil Number of participants assigned: 50 participants Number of participants assessed: 40 participants (24 surgical; 16 conservative) Inclusion criteria
Exclusion criteria
Age
Gender of participants assessed (male/female)
Classification of injury: not specified |
|
| Interventions |
Timing of intervention: not reported Type of surgical intervention: open reduction with 3.5‐mm DCP plate fixation (antero‐inferior position) Type of conservative intervention: Velpeau sling for 6 weeks Rehabilitation:
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up (mean/range): 16/12‐24 months. The length of follow‐up was not pre‐specified Loss to follow‐up: 10 participants were lost to follow‐up:
Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
Return to previous activities:
|
|
| Notes |
Composite adverse events: surgery: (n = 0). Conservative: stiffness/restricted range of shoulder movement (n = 2). In Analysis 1.14 we used event rates 0 for surgery and 2 for conservative. Cosmetic result events: surgery: unsightly scar (n = 3). Conservative: deformity (n = 7). In Analysis 1.11 we used event rates 3 for surgery and 7 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The study authors did not specify which groups the 10 participants that were lost to follow‐up belonged to |
| Selective reporting (reporting bias) | High risk | Pain (as primary outcome) was reported incompletely so that it cannot be entered into a meta‐analysis |
| Other bias | High risk | The time points of outcomes were not pre‐specified |
Judd 2009.
| Methods |
Study design: single‐centre, 2‐group, parallel‐design RCT Duration of the study: February 2001‐June 2003 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: not registered Funding sources: study authors reported no potential conflict of interest and no funding sources |
|
| Participants |
Place of study: not reported, probably Hawaii Number of participants assigned: 57 participants (29 surgical; 28 conservative) Number of participants assessed: 57 participants (29 surgical; 28 conservative) Inclusion criteria
Exclusion criteria
Age
Gender of participants assigned (male/female)
Classification of injury: not specified, just fracture pattern (comminuted and displacement/shortening fractures) |
|
| Interventions |
Timing of intervention: participants were treated within 2 weeks Type of surgical intervention: open reduction and intramedullary fixation using a modified Hagie pin (Boehme 1991) Type of conservative intervention: sling for comfort, restrictions of shoulder motion as tolerated and restrictions of activities until healing of fracture occurred Rehabilitation: in both groups, gentle shoulder motion exercises and daily living activities were allowed as tolerated. After fracture healed, physical therapy with strength training and unrestricted activities were allowed. Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up:
Loss to follow‐up: none lost to follow‐up Primary outcomes
Secondary outcomes: Other treatment failure measured by:
Adverse events measured by:
|
|
| Notes | After fracture healing, all pins were removed under local anaesthesia. Composite adverse events: surgery: local infection (n = 6); hardware prominence (n = 3); refracture (n = 2). Conservative: refracture (n = 1). In Analysis 1.14 we used event rates 6 for surgery and 1 for conservative. Cosmetic result events: surgery: prominent pins (n = 9). Conservative: deformity (n = 0). In Analysis 1.11 we used event rates 9 for surgery and 0 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes placed in a random order were used, and neither the treating surgeon nor the participant knew the intervention until the participant consented to participate in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing outcome data were not balanced in numbers across intervention groups; more participants in the conservative intervention group were not assessed at all time points. |
| Selective reporting (reporting bias) | High risk | Function or disability was measured by non‐standard validated participant‐reported measures. |
| Other bias | Low risk | The study appears to be free of other potential sources of bias. |
Koch 2008.
| Methods |
Study design: single‐centre, 2‐group, parallel‐design RCT Duration of the study: January 2002‐December 2006 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: not registered Funding sources: study authors reported no potential conflict of interest and no funding sources. |
|
| Participants |
Place of study: German Number of participants assigned: 68 participants (35 surgical; 33 conservative) Number of participants assessed: 68 participants (35 surgical; 33 conservative) Inclusion criteria
Exclusion criteria
Age
Gender of participants assigned (male/female)
Classification of injury: not specified |
|
| Interventions |
Timing of intervention: not reported Type of surgical intervention: closed reduction and intramedullary fixation using a 2‐mm pin Type of conservative intervention: figure‐of‐eight for comfort 6 ‐8 weeks Rehabilitation: not reported Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: none lost to follow‐up Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
Return to previous activities (sport) |
|
| Notes | When closed reduction failed (60% of participants), a short incision was made to reduce the fracture. After 3 months all pins were removed. Pain was presented in the results of the trial; however, it is not presented in our analyses (we tried unsuccessfully to contact the study authors to obtain further information on SD of VAS). Composite adverse events: surgery: stiffness/restricted range of shoulder movement (n = 1). Conservative: stiffness/restricted range of shoulder movement (n = 4). In Analysis 1.14 we used event rates 1 for surgery and 4 for conservative. Cosmetic result events: surgery: (n = 0). Conservative: deformity (n = 9). In Analysis 1.11 we used event rates 0 for surgery and 9 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The study authors did not report missing data |
| Selective reporting (reporting bias) | High risk | Function or disability (as primary outcome measured by validated participant‐reported measures) was not evaluated by the study authors |
| Other bias | High risk | Information on whether baseline was balanced was insufficient as no outcome data were reported for baseline |
Melean 2015.
| Methods |
Study design: single‐centre, 2‐group, parallel‐design RCT Duration of the study: February 2010‐February 2012 Protocol was published before recruitment of participants: not reported, but no protocol was published. Details of trial registration: not registered Funding sources: none of the study authors received payments or services, either directly or indirectly. |
|
| Participants |
Place of study: 1 centre from Santiago, Chile Number of participants assigned: 76 participants (34 surgical; 42 conservative) Number of participants assessed: 76 participants (34 surgical; 42 conservative) Inclusion criteria
Exclusion criteria
Age
Gender: not reported Classification of injury: fractures were classified according to the Robinson's Classification (Robinson 1998). |
|
| Interventions |
Timing of intervention: not specified; however, participants with intervention > 3 weeks after injury were excluded Type of surgical intervention: open reduction and plate fixation using the 3.5 mm LCP system in 12 participants and LCP reconstruction plates in 22 participants. Study authors said that different implants were used according to availability at the day of the surgery. Type of conservative intervention: standard sling for 6 weeks Rehabilitation
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: none lost to follow‐up Primary outcomes
Secondary outcomes Adverse events measured by:
Time to return to previous activities (work) |
|
| Notes | We contacted the study authors to request data (i.e. SD for Constant score); however, the study authors declined to provide them. Composite adverse events: surgery: discomfort leading to implant removal (n = 4). Conservative: (n = 0). In Analysis 1.14 we used event rates 4 for surgery and 0 for conservative. Cosmetic result events: not distinguished from adverse events |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Used "the method of tables of 4" and those with '0' assigned to conservative treatment and '1' assigned to surgery; unclear if this is random. |
| Allocation concealment (selection bias) | Unclear risk | Unclear, reports that those with '0' assigned to conservative treatment and '1' assigned to surgery, and these placed in envelopes, but not if the envelopes were sequentially numbered or opaque. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not reported. Blinding of participants was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported. As participants were aware of treatment, there was a high risk of detection bias in measurement of function. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The study authors did not explicitly report if any participants were lost to follow up. |
| Selective reporting (reporting bias) | High risk | Pain (as primary outcome measured by validated participant‐reported measures) and other important secondary endpoints were not evaluated by the study authors. |
| Other bias | Unclear risk | The trial did not report baseline data thus it is unclear if 2 groups were balanced at baseline for the primary outcomes. |
Mirzatolooei 2011.
| Methods |
Study design: single‐centre, 2‐group, parallel‐design RCT Duration of the study: October 2007‐April 2009 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: not registered Funding sources: none known |
|
| Participants |
Place of study: tertiary trauma centre in Iran Number of participants assigned: 60 participants (29 surgical; 31 conservative) Number of participants assessed: 50 participants (26 surgical; 24 conservative) Inclusion criteria
Exclusion criteria
Age
Gender of participants assessed (male/female)
Classification of injury: not reported |
|
| Interventions |
Timing of intervention: not specified; however, participants with intervention > 3 weeks after injury were excluded. Type of surgical intervention: open reduction and plate fixation with 3.5‐mm reconstruction plates on the superior surface of the clavicle. Type of conservative intervention: a commercial sling was used and an elastic cotton band was wrapped around the participant's chest and arm to limit abduction and external rotation of the arm. No attempt was made for closed reduction. Rehabilitation
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: 10 participants were lost to follow‐up at 1 year
Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
|
|
| Notes | This study population included some participants with open clavicle fractures (7 participants in the surgical group and 5 participants in the conservative group). SDs of DASH and Constant scores were obtained by personal contact with the study authors. Composite adverse events: surgery: infection (n = 1); malunion (n = 4); discomfort leading to implant removal (n = 1); skin dysaesthesia (n = 2). Conservative: malunion (n = 19); neurological claudication (n = 2). In Analysis 1.14 we used event rates 8 for surgery and 19 for conservative. Cosmetic result events: surgery: hardware prominence (n = 1), unsightly scar (n = 2). Conservative: asymmetry (n = 2). In Analysis 1.11 we used event rates 3 for surgery and 2 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of generating the random sequence was not reported. |
| Allocation concealment (selection bias) | Low risk | Opaque and sealed envelopes were used. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7 participants in the conservative intervention did not complete 1‐year follow‐up and the study authors did not perform an intention‐to‐treat analysis. In addition, 3 participants in the surgical group did not undergo surgery and were excluded. |
| Selective reporting (reporting bias) | High risk | The study authors did not report outcomes at each time point. It was unclear when the outcomes were collected, and the study authors reported only P values. |
| Other bias | High risk | No baseline data were provided. |
Naveen 2017.
| Methods |
Study design: single‐centre, 2‐group, parallel‐design, quasi‐RCT Duration of the study: June 2011‐June 2013 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: not reported Funding sources: funding not specified; the study authors declare no conflict of interest |
|
| Participants |
Place of study: tertiary care teaching hospital from India Number of participants assigned: 60 participants (30 surgical; 30 conservative) Number of participants assessed: 60 participants (30 surgical; 30 conservative) Inclusion criteria
Exclusion criteria
Age:
Gender of participants assigned (male/female)
Classification of injury: fractures were classified according to the Robinson's Classification (Robinson 1998) |
|
| Interventions |
Timing of intervention: participants underwent the operation within 7 days of the injury. Type of surgical intervention: open reduction with 3.5‐mm DCP plate fixation (superior position) Type of conservative intervention: figure‐of‐eight bandage and sling for 3 weeks. Rehabilitation
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: none lost to follow‐up Primary outcomes
Secondary outcomes Proportion healed (union at <12 weeks) Proportion with delayed union (12‐24 weeks) Proportion satisfied, partially satisfied and unsatisfied at end of follow‐up Other treatment failure measured by:
Adverse events measured by:
|
|
| Notes | The sample size was not calculated prior to the study. We tried unsuccessfully to contact the study authors to obtain further information. Composite adverse events: surgery: malunion (n = 1). Conservative: malunion (n = 6); restriction of ROM (n = 1). In Analysis 1.14 we used event rates 1 for surgery and 6 for conservative. Cosmetic result events: surgery: deformity (n = 1); unsightly scar (n = 3); hardware prominence (n = 2). Conservative: deformity (n = 6). In Analysis 1.11 we used event rates 6 for surgery and 6 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sequence generated by some rule based on date (alternation): Quote: "Patients were allocated into both the treatment groups on alternate basis, i.e., group 1 followed by group 2" |
| Allocation concealment (selection bias) | High risk | Allocation was not concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants self‐reported Constant score and satisfaction and were not blinded. Outcome assessors for radiographic assessment of non‐union were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The study authors reported that there were no missing data. |
| Selective reporting (reporting bias) | High risk | Pain (as primary outcome measured by validated participant‐reported measures), and other important secondary endpoints were not evaluated by the study authors |
| Other bias | Low risk | The study appears to be free of other potential sources of bias. |
Robinson 2013a.
| Methods |
Study design: multicentre parallel group, 2‐arm RCT (3 centres) Duration of the study: September 2007‐July 2010 Protocol was published before recruitment of participants: unclear; trial was registered but protocol methods could not be found. Details of trial registration: yes. The study was registered on the National Research Register of the National Health Service Institute for Health Research (Number N0256199069). Funding sources: none of the study authors received payments or services, either directly or indirectly. |
|
| Participants |
Place of study: New Royal Infirmary of Edinburgh, Glasgow Royal Infirmary, and Frenchay Hospital, Bristol; UK Number of participants assigned: 200 participants (95 surgical; 105 conservative) Number of participants assessed: 178 participants (86 surgical; 92 conservative) Inclusion criteria
Age:
Gender of participants assigned (male/female)
Classification of injury: fractures were classified according to the Robinson's Classification (Robinson 1998). |
|
| Interventions |
Timing of intervention: participants underwent surgery within 2 weeks after the injury Type of surgical intervention: open reduction and plate fixation Type of conservative intervention: collar and cuff for 3 weeks Rehabilitation
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: 22/200 participants were lost to follow‐up at 1 year
Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
Health‐related quality of life measured by:
Numbers of participants returning to previous activities (work and sport). |
|
| Notes | When conservative method failed after 6 months (26.1%, 24 participants), 13 participants chose to undergo a secondary open reduction and plate fixation. We tried unsuccessfully to contact the study authors to obtain further information. Composite adverse events: surgery: superficial wound infection (n = 2); dehiscence (n = 1); local sensitivity/irritation (n = 17); local numbness (n = 15); plate removal (n = 10); rotator cuff impingement (n = 2); adhesive capsulitis (n = 1). Conservative: symptomatic malunion (n = 1); local sensitivity/irritation (n = 11); local numbness (n = 4); rotator cuff impingement (n = 1). In Analysis 1.14 we used event rates 32 for surgery and 15 for conservative. Cosmetic result events: surgery: dissatisfaction with shoulder droop (n = 1), shoulder asymmetry (n = 2), bump at fracture site (n = 5). Conservative: dissatisfaction with shoulder droop (n = 15), shoulder asymmetry (n = 17), bump at fracture site (n = 26). These are unlikely to be mutually exclusIve. Analysis 1.11 we used event rates 5 for surgery and 26 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence generation was performed by a computer random number generator. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | A research physiotherapist, who was blinded by having the participant wear a t‐shirt, assessed ROM and strength in both limbs. High risk of bias for self‐reported outcomes (function and satisfaction) as participants were aware of treatment group. Unclear if unblinded assessment by radiographer of treatment failure (e.g. symptomatic non‐union) and asymptomatic non‐union was subject to bias. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only 11% of participants were lost to follow‐up. Missing outcome data were balanced in numbers across intervention groups. The study authors said that there were no significant demographic differences between the participants who were lost to follow‐up and those who were followed to 1 year. |
| Selective reporting (reporting bias) | Unclear risk | Despite the study protocol being registered, the pre‐specified outcomes were not recorded and were not available. |
| Other bias | Low risk | The study appears to be free of other potential sources of bias. |
Smekal 2009.
| Methods |
Study design: single‐centre, 2‐group, parallel‐design RCT Duration of the study: April 2003‐November 2005 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: not registered Funding sources: none known |
|
| Participants |
Place of study: tertiary trauma centre from Austria Number of participants assigned: 68 participants (33 surgical; 35 conservative) Number of participants assessed: 60 participants (30 surgical; 30 conservative) Inclusion criteria
Exclusion criteria
Age
Gender of participants assessed (male/female)
Classification of injury: AO classification |
|
| Interventions |
Timing of intervention: not specified; however, the study authors reported that surgery was performed within the 1st 3 days after trauma Type of surgical intervention: closed reduction and intramedullary fixation using a TEN ‐ 2.5 mm for men and 2 mm for women Type of conservative intervention: simple sling for 3 weeks Rehabilitation
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: 8 participants were lost to follow‐up at 2 years
Primary outcomes
Secondary outcomes: Adverse events measured by:
|
|
| Notes | When closed reduction failed (13.3% of participants), a short incision was made to reduce the fracture. 25 participants (89.3%) underwent implant removal after a mean time of 23 (6‐120) weeks. We tried unsuccessfully to contact the study authors to obtain further information. Composite adverse events: surgery: implant removal for cutout or irritation (n = 7). Conservative: symptomatic malunion (n = 2); transient neurogenic compromise (n = 3). In Analysis 1.14 we used event rates 7 for surgery and 3 for conservative. Cosmetic result events: not distinguished from adverse events |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A balanced block randomisation with a block size of 4 was used. By throwing a dice 15 times, a randomisation list with fifteen 4 blocks and therefore 60 treatment options was obtained. Quote: "The assigned treatment options of patients lost to follow‐up were collected and separately put in an envelope in a second box. After using all envelopes from the first box, envelopes were randomly picked from the second box". Comment: it was unclear what lost to follow‐up means; the study authors reported unclear information about the participants who were lost to follow‐up after randomisation. |
| Allocation concealment (selection bias) | Unclear risk | The assigned treatment options were numbered, sealed within an envelope and given in strict rotation in a first box; assigned treatment options of participants lost to follow‐up were collected and separately put in an envelope in a second box. The envelopes of the second box were probably unsealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The authors excluded 8 participants who did not complete follow‐up, and an intention‐to‐treat analysis was not performed; however, only 5 participants were lost from the conservative group and 3 from the surgical group. |
| Selective reporting (reporting bias) | High risk | No baseline data for efficacy outcomes were presented and only P values were reported. |
| Other bias | High risk | Information on whether baseline was balanced was insufficient as no outcome data were reported for baseline. |
Tamaoki 2017.
| Methods |
Study design: 2 centres, parallel‐group RCT Duration of the study: not reported ‐ the study started 1 January 2008 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: yes. Main ID: ISRCTN 66495030. Date of registration: 28 January 2010 Funding sources: there was no external source of funding for this study |
|
| Participants |
Place of study: 2 referral trauma centre hospitals in Brazil (Sao Paulo and Espirito Santo) Number of participants assigned: 117 participants (59 surgical; 58 conservative) Number of participants assessed: 98 participants (51 surgical; 47 conservative) Inclusion criteria
Exclusion criteria
Age
Gender of participants assigned (male/female)
Classification of injury: fractures were classified according to the AO/OTA fracture classification |
|
| Interventions |
Timing of intervention
Type of surgical intervention: open reduction and anteroinferior plate fixation Type of conservative intervention: figure‐of‐eight bandage. participants were instructed to use the ipsilateral arm for normal activities as much as possible Rehabilitation
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: 19 participants were lost to follow‐up at 1 year
Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
Numbers of participants returning to previous activities |
|
| Notes | The majority of participants were recruited by only 1 centre, Vila Velha Hospital in Espirito Santo Brazil. The study authors did not report the numbers. The study authors provided some information regarding the structure of the study. Composite adverse events: surgery: superficial infection (n = 2); discomfort leading to implant removal (n = 3); paraesthesia (n = 7). Conservative: paraesthesia (n = 1). In Analysis 1.14 we used event rates 7 for surgery and 1 for conservative. Cosmetic result events: surgery: shoulder malpositioning (n = 1); droop (n = 14); shortening (n = 8); bone prominence (n = 3). Conservative: shoulder malpositioning (n = 7); droop (n = 17); shortening (n = 27); bone prominence (n = 33). In Analysis 1.11 we used event rates 14 for surgery and 33 for conservative. Notably, participant dissatisfaction with cosmetic result was higher in the surgical group and included dissatisfaction with appearance of the surgical incision: 11/51 versus 7/47 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence generation was performed by a computer random number generator. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | All participants wore a figure‐of‐eight harness and a bandage on the ipsilateral clavicle and were instructed not to reveal the treatment that they had undergone, to minimise detection bias in assessment of radiographic outcomes (e.g. non‐union) Self‐reported outcomes (DASH, pain, satisfaction) assessed by unblinded participants, thus there was potential for detection bias. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing outcome data were not balanced in numbers across intervention groups. Slightly more participants did not return for follow up from the conservative therapy group (11/58, 19%) compared to the surgery group (8/59,14%) for unknown reasons. |
| Selective reporting (reporting bias) | High risk | The study protocol was registered and all of the study's pre‐specified (primary and secondary) outcomes that are of interest for this review have been reported in the pre‐specified way. Time points differ: protocol plan was to follow up at 3, 6 and 12 months, but results paper reports outcomes at 6 weeks, 6 months and 1 year for DASH and VAS plus 3 months for VAS only, with no explanation given for these changes. |
| Other bias | Low risk | The study appears to be free of other potential sources of bias. |
Virtanen 2012a.
| Methods |
Study design: single‐centre, 2‐group, parallel‐design RCT Duration of the study: August 2004‐October 2007 Protocol was published before recruitment of participants: not reported, but no protocol was published Details of trial registration: Main ID: NCT01199653. Date of registration: 10 September 2010 Funding sources: none of the study authors received payments or services, either directly or indirectly. The study was supported by Helsinki University Central Hospital research funds. The founder had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript. |
|
| Participants |
Place of study: Uusimaa, Finland Number of participants assigned: 60 participants (28 surgical; 32 conservative) Number of participants assessed: 51 participants (26 surgical; 25 conservative) Inclusion criteria
Exclusion criteria
Age:
Gender of participants assigned (male/female)
Classification of injury: fractures were classified according to the AO/OTA fracture classification and displacement and shortening of the fragments. |
|
| Interventions |
Timing of intervention: not specified; however, participants with > 7 days after the injury were excluded Type of surgical intervention: open reduction and anterior plate fixation with stainless steel reconstruction plate and screws Type of conservative intervention: simple sling for 3 weeks Rehabilitation:
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: 9 participants were lost to follow‐up at 1 year
Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
|
|
| Notes |
Composite adverse events: surgery: brachial plexus irritation (n = 1); refracture (1). Conservative: mild plate irritation (n = 1); symptomatic malunion (n = 2); refracture (2). In Analysis 1.14 we used event rates 1 for surgery and 2 for conservative. Cosmetic result events: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation was used, and block size varied randomly between 4 and ten. Participants were randomly assigned to 2 parallel groups, initially at a 1:1 ratio, to receive either conservative or surgical intervention. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were not balanced in numbers across intervention groups; however, intention‐to‐treat analysis was performed. |
| Selective reporting (reporting bias) | Low risk | The study protocol was available and all of the study's pre‐specified (primary and secondary) outcomes that were of interest for this review were reported in the pre‐specified way. |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Woltz 2017a.
| Methods |
Study design: multicentre, 2‐arm, parallel‐group, RCT (16 centres) Duration of the study: June 2010‐December 2013 Protocol was published before recruitment of participants: yes. doi: 10.1186/1471‐2474‐12‐196 ‐ BMC Musculoskeletal Disorders 2011;12:196 Details of trial registration: yes. Main ID: NTR 2399. Date of registration: 1 July 2010 Funding sources: the study was financially supported by Fonds NutsOhra, a nonprofit funding organization for improvement in health in the Netherlands. The study authors reported no potential conflict of interest. |
|
| Participants |
Place of study: 16 teaching and non‐teaching hospitals in the Netherlands, including 4 university hospitals Number of participants assigned: 160 participants (86 surgical; 74 conservative) Number of participants assessed: 154 participants (84 surgical; 70 conservative) Inclusion criteria
Exclusion criteria
Age
Gender of participants assigned (male/female)
Classification of injury: fractures were classified according to the Robinson's Classification (Robinson 1998) |
|
| Interventions |
Timing of intervention: not specified; however, participants with > 14 days after the injury were excluded. Type of surgical intervention: open reduction and plate fixation. There were no restrictions regarding incision, plate location, or type of plate. Type of conservative intervention: simple sling for 2 weeks Rehabilitation
Any co‐interventions: not reported |
|
| Outcomes |
Length of follow‐up
Loss to follow‐up: 22 participants were lost to follow‐up at 1 year
Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
Health‐related quality of life measure by:
|
|
| Notes | Besides the 6 participants lost to follow‐up, there were 6 participants (1 in the surgical group and 5 in the conservative group) that were lost to follow up only in the primary outcome, since they didn't have radiographic image to confirm achieved union The type of surgical treatment, relating to plate type, plate position and incision were not pre‐specified. SDs and means of VAS scores were obtained by personal contact with the study authors. Composite adverse events: surgery: wound infection (n = 3); implant removal (n = 14; loss of sensation around scar (n = 15). Conservative: malunion (n = 1); plate removed (n = 1); neurological problems (n = 1). In Analysis 1.14 we used event rates 15 for surgery and 1 for conservative. Cosmetic result events: surgery: unsatisfied with cosmetic result (n = 4). Conservative: unsatisfied (n = 13). Estimates from percentages (5% versus 18%). In Analysis 1.11 we used event rates 4 for surgery and 13 for conservative. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence generation was performed by a computer random number generator using minimisation. |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The authors excluded 6 participants who did not complete follow‐up, and an intention‐to‐treat analysis was performed; however, only 4 participants were lost from the conservative group and 2 from the surgical group. However, there were imbalanced data for availability of function scores. After 1 year, the functional scores of 87% of participants in the surgical group and 78% of participants in the conservative group were available for analysis. |
| Selective reporting (reporting bias) | Low risk | The study protocol was registered and all of the study's pre‐specified (primary and secondary) outcomes that are of interest for this review were reported in the pre‐specified way. |
| Other bias | High risk | There were imbalances in numbers allocated into the 2 groups assigned (86 surgical; 74 conservative). There was insufficient data on baseline characteristics to judge whether or not the 2 groups were balanced at baseline. |
AO: Arbeitsgemeinschaft fur Osteosynthesefragen; OTA: Orthopaedic Trauma Association; AO/OTA: combination of AO and OTA; ASA: American Society of Anesthesiologists; BESS: British Elbow and Shoulder Society; BUPA: British United Provident Association; DASH: Disability of the Arm, Shoulder, and Hand questionnaire;DCP: dynamic compression plate; LCP: locking compression plate; RCT: randomised controlled trial; ROM: range of movement; SANE: Single Assessment Numeric Evaluation; SD: standard deviation; SEM: standard error of the mean; TEN: titanium elastic nail; UCLA: University of California Los Angeles; VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12610000948099 | The registration for the RCT was withdrawn in February 2016. We did not identify the other trial registration. |
| Bernstein 2007 | Design of study not relevant: letter |
| Bohme 2011 | Design of study not relevant: not a RCT or quasi‐RCT |
| Bravo 2009 | Design of study not relevant: narrative review |
| Dugar 2013 | Participants of study not relevant: a quasi‐RCT that also included participants with medial and lateral third clavicle fractures (16.6%) and did not report results separately |
| Jones 2014 | Design of study not relevant: not a RCT or quasi‐RCT: treatment method was based on surgeon choice |
| Jubel 2002 | Design of study not relevant: retrospective comparative study |
| Jubel 2005 | Design of study not relevant: not a RCT or quasi‐RCT ‐ participants could choose the intervention |
| Khorami 2014 | Design of study not relevant: not a RCT or quasi‐RCT ‐ participants could choose the intervention |
| Kulshrestha 2011 | Design of study not relevant: not a RCT or quasi‐RCT ‐ participants could choose the intervention |
| Madhukar 2015 | Design of study not relevant: retrospective comparative study |
| Malkoc 2016 | Design of study not relevant: retrospective comparative study |
| McIntosh 2016 | Design of study not relevant: narrative review |
| McKee 2010b | Design of study not relevant: narrative review |
| NCT00642265 | This study, which was registered in the ClinicalTrials.gov Identifier: NCT00642265, was listed as an ongoing trial in the 1st version of the review. It planned to compare osteosynthesis versus sling, with a start date of April 2008 and end date July 2015. However, the contact author reported that for a variety of reasons the trial was ended and no data are available. |
| NCT01311219 | The registration for a multicentre trial was withdrawn before enrolment because it is "a duplicate study". We did not identify the other trial registration. |
| Parry 2017 | Design of study not relevant: retrospective comparative study |
| Shukla 2014 | Design of study not relevant: case control study |
| Simon 2010 | Design of study not relevant: narrative review |
| Smekal 2011 | Design of study not relevant: not a RCT or quasi‐RCT |
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Dhakad 2016.
| Methods |
Study design: not reported, probably quasi‐RCT (alternation) Random sequence generation: not reported, probably alternation Allocation concealment: not reported Masking: not reported |
| Participants |
Location: Gwalior, India Target sample size (N): 50 participants Inclusion criteria
Exclusion criteria
Age: not reported Classification of injury: fractures were classified according to the Robinson’s Classification (Robinson 1998). |
| Interventions |
Timing of intervention: not reported Type of surgical intervention: open reduction and plate fixation. Fixation was performed using 3.5 mm LCP anterosuperior plate (S‐shaped) Type of conservative intervention: figure‐of‐eight bandage and sling. Not reported for how long Rehabilitation
Any co‐interventions: not reported |
| Outcomes |
Length of follow‐up: regular follow‐up for every 4 weeks was done. Participants were followed up till radiological union. Loss to follow‐up: none lost to follow‐up Primary outcomes
Secondary outcomes Other treatment failure measured by:
Adverse events measured by:
|
| Notes | We tried unsuccessfully to contact the study authors to obtain further information. |
ISRCTN00825817.
| Methods |
Study design: RCT Random sequence generation: not reported Allocation concealment: not reported Masking: not reported |
| Participants |
Location: Preston, UK Target sample size (N): 40 participants Inclusion criteria
Exclusion criteria
Age: not reported Classification of injury: not reported |
| Interventions |
Type of surgical intervention: open reduction and internal fixation (not specified) Type of conservative intervention: not reported |
| Outcomes |
Primary outcomes
Secondary outcomes
Timing of outcomes measurement: not reported |
| Notes | Status: completed/not recruiting. Unpublished: trial registration only |
ISRCTN57483251.
| Methods |
Study design: parallel RCT Random sequence generation: not reported Allocation concealment: not reported Masking: not reported |
| Participants |
Location: Preston, UK Target sample size (N): 40 participants Inclusion criteria
Exclusion criteria
Age: not reported Classification of injury: not reported |
| Interventions |
Type of surgical intervention: not specified Type of conservative intervention: not specified |
| Outcomes |
Primary outcomes Not reported Secondary outcomes Not reported Timing of outcomes measurement: not reported |
| Notes | Status: completed/not recruiting. Unpublished: trial registration only |
Shetty 2017.
| Methods |
Study design: not reported Random sequence generation: not reported Allocation concealment: not reported Masking: not reported |
| Participants |
Location: Karnataka, India Target sample size (N): 30 participants Inclusion criteria
Exclusion criteria
Age: not reported Classification of injury: fractures were classified according to the AO/OTA fracture classification |
| Interventions |
Timing of intervention: not reported Type of surgical intervention: open reduction and plate fixation Type of conservative intervention: clavicle brace and arm pouch for 3 weeks Rehabilitation: not reported Any co‐interventions: not reported |
| Outcomes |
Length of follow‐up
Loss to follow‐up: not reported Primary outcomes
Secondary outcomes Other treatment failure measured by:
|
| Notes | This study is likely to be compromised by excess loss to follow‐up. The study authors reported: "Most of our cases were from distant places and hence, did not appear for the 1st follow‐up and hence, had to be excluded from the study." We tried unsuccessfully to contact the study authors to obtain further information. |
Smith 2001.
| Methods |
Study design: RCT Duration of the study: not reported Protocol was published before recruitment of participants: not reported Details of trial registration: not reported Funding sources: not reported |
| Participants |
Place of study: Tennesse, USA Number of participants assigned: 100 participants Number of participants assessed: 65 participants (30 surgical; 35 conservative) Inclusion criteria
Exclusion criteria: not reported Age: not reported Classification of injury: not reported |
| Interventions |
Timing of intervention: not reported: participants with acute fractures Type of surgical intervention: open reduction and plate fixation with limited contact dynamic compression plates Type of conservative intervention: simple sling or figure‐of‐eight bandage Rehabilitation: not reported Any co‐interventions: not reported |
| Outcomes |
Length of follow‐up: until radiographic union or non‐union, surgical group (mean/range): 16/8‐28 months; conservative group (mean/range): 18.6/8‐32 months Loss to follow‐up: 35 participants were lost to follow‐up Primary outcomes
Secondary outcomes Treatment failure measured by:
Adverse events measured by:
|
| Notes | We tried unsuccessfully to contact the study authors to obtain further information. This trial was presented in 2001 at a conference, and it is unlikely that the full results will ever be published. |
DASH: Disability of the Arm, Shoulder, and Hand questionnaire; LCP: locking compression plate; RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
NCT00590850.
| Trial name or title | A multicentre, prospective, randomised trial of non‐operative versus operative treatment for high‐energy mid‐shaft clavicle fractures |
| Methods |
Study design: parallel RCT Random sequence generation: not reported Allocation concealment: not reported Masking: open‐label |
| Participants |
Location: Greenville Hospital System University Medical Center-South Carolina, USA Target sample size (N): 480 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Type of surgical intervention
Type of conservative intervention
|
| Outcomes |
Primary outcomes
Secondary outcomes
Timing of outcomes measurement: time frame: 12‐month follow‐up |
| Starting date |
Main ID: NCT00590850. Date of registration: 28 December 2007 Last refreshed on: 22 February 2017 Date of 1stenrolment: October 2003 Status: enrolling by invitation Estimated Study Completion date: December 2019 |
| Contact information |
Name: Kyle J Jeray, MD Address: Greenville, South Carolina, USA, 29605 Telephone: not reported Email: not reported Affiliation: Greenville Hospital System |
| Notes |
NCT01078480.
| Trial name or title | Conservative treatment versus plate osteosynthesis using angular stabile screws and pre‐contoured plates in displaced mid‐shaft clavicular fractures. A prospective randomised multi‐centre study |
| Methods |
Study design: parallel RCT Random sequence generation: not reported Allocation concealment: not reported Masking: single‐blind (outcome assessor) |
| Participants |
Location: Northern Orthopaedic Division, Denmark Target sample size (N): 140 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Type of surgical intervention: open reduction and internal fixation with a pre‐contoured titanium plate and screws Type of conservative intervention: sling |
| Outcomes |
Primary outcomes
Timing of outcomes measurement: time frame: 12‐month follow‐up |
| Starting date |
Main ID: NCT01078480. Date of registration: 27 February 2010 Last refreshed on: 21 January 2016 Date of 1stenrolment: April 2010 Status: completed Estimated Study Completion date: December 2015 |
| Contact information |
Name: Carsten Moss Jensen, MD Address: not reported Telephone: not reported Email: cmj@rn.dk Affiliation: Orthopaedic Division, North Denmark Region, Aalborg Hospital-Aarhus University Hospital, Denmark |
| Notes | This trial was published in November 2018, during editorial processing of the review; reference in additional references: Qvist 2018) |
NCT01483482.
| Trial name or title | Treatment of displaced, mid‐shaft clavicle fracture. Sling or plate? |
| Methods |
Study design: parallel RCT Random sequence generation: not reported Allocation concealment: not reported Masking: open‐label |
| Participants |
Location: Hvidovre, Denmark Target sample size (N): 120 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Type of surgical intervention: open reduction and superior locking plate Type of conservative intervention: simple sling until pain |
| Outcomes |
Primary outcomes
Secondary outcomes
Timing of outcomes measurement: time frame: 12‐month follow‐up |
| Starting date |
Main ID: NCT01483482 Date of registration: 29 November 2011 Last refreshed on: 15 March 2016 Date of 1stenrolment: April 2011 Status: active, not recruiting Estimated Study Completion date: August 2016 |
| Contact information |
Name: Ilija Ban, MD Address: 30, Kettegaard Allee – Hvidovre, Denmark, 2650 Telephone: +45 26242662 Email: ilija.ban@gmail.com Affiliation: University Hospital of Hvidovre |
| Notes |
ASA: American Society of Anesthesiologists; DASH: Disability of the Arm, Shoulder, and Hand questionnaire;RCT: randomised controlled trial
Differences between protocol and review
First version of this review (Lenza 2013)
When studies included more than one measure of function, for the purpose of pooling data for the 'Summary of findings' table, we decided to choose the Constant score because it is more specific for the shoulder than the DASH questionnaire; and, when compared with the UCLA, SANE and L'Insalata scores, the Constant score is the most commonly used in the literature (Lenza 2013).
Current update (2018)
Types of outcome measures
For the purpose of pooling data where studies included more than one measure of function, we preferentially included one measure according to the following hierarchy: Constant score, DASH score, UCLA score, SANE score and L'Insalata score.
We clarified that treatment failure did not include plate removal for hardware irritation.
Adverse events: we did not differentiate between short‐term (local infection, e.g. wound infection, and/or dehiscence), and long‐term outcomes (symptoms of discomfort related to the implant, requiring removal; skin and nerve problems; stiffness/restricted range of shoulder movement).
We changed our measure of adverse events to a composite adverse event outcome that included the number of participants with one of more of the following events: local infection, dehiscence, symptomatic malunion, discomfort leading to implant removal, skin and nerve problems, stiffness/restricted range of shoulder movement).
Outcome measures for the 'Summary of findings' table
Instead of presenting two key surgical complications (infection and/or dehiscence; hardware irritation requiring removal), we presented data for composite adverse event, as defined in Types of outcome measures.
'Risk of bias' assessment
As stated in Lenza 2013, we assessed whether there was inappropriate influence of funders under ‘other bias’.
Contributions of authors
All the review authors contributed to the review and the update. ML, RJ, BASF and RB drafted the review and all authors provided comments and approved the final version. The guarantor of this review is Mario Lenza.
Contributions of the editorial base
Helen Handoll (Co‐ordinating Editor): edited the review, advised on methodology and review content, and approved the final version for publication. Joanne Elliott (Managing Editor): coordinated the editorial process and edited the review. Maria Clarke and Joanne Elliott (Information Specialists): ran search update and edited the search methods section.
Sources of support
Internal sources
Universidade Federal de São Paulo, Brazil.
Monash University, Australia.
Hospital Israelita Albert Einstein, Brazil.
External sources
No sources of support supplied
Declarations of interest
Mário Lenza: no interests to declare Rachelle Buchbinder: no interests to declare Renea V Johnston: no interests to declare Bruno AS Ferrari: no interests to declare Flávio Faloppa: no interests to declare
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Ahrens 2017 {published data only}
- Ahrens P. Clavicle Trial ‐ randomised controlled multicentre study of conservative management versus open reduction and internal fixation of mid‐shaft clavicle fractures. UK Clinical Research Network: public.ukcrn.org.uk/search/StudyDetail.aspx?StudyID=8665 (accessed 18 February 2013).
- Ahrens P, Barber J. Standard deviations and means of DASH and Constant scores used in our review [personal communication]. Email to: M Lenza 5 September 2017.
- Ahrens PM, Garlick NI, Barber J, Tims EM, Clavicle Trial Collaborative Group. The clavicle trial: a multicenter randomized controlled trial comparing operative with nonoperative treatment of displaced midshaft clavicle fractures. Journal of Bone and Joint Surgery. American Volume 2017;99(16):1345‐54. [DOI] [PubMed] [Google Scholar]
- Longo UG, Banerjee S, Barber J, Chambler A, Cobiella C, Corbett S, et al. Conservative management versus open reduction and internal fixation for mid‐shaft clavicle fractures in adults‐‐the Clavicle Trial: study protocol for a multicentre randomized controlled trial. Trials 2011;12:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2011 {published data only}
- Chen QY, Kou DQ, Cheng XJ, Zhang W, Wang W, Lin ZQ, et al. Intramedullary nailing of clavicular midshaft fractures in adults using titanium elastic nail. Chinese Journal of Traumatology 2011;14(5):269‐76. [PubMed] [Google Scholar]
COTS 2007 {published and unpublished data}
- Altamimi SA, McKee MD, Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. Journal of Bone and Joint Surgery. American Volume 2008;90(Suppl 2, Pt 1):1‐8. [DOI] [PubMed] [Google Scholar]
- Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. Journal of Bone and Joint Surgery. American Volume 2007;89(1):1‐10. [DOI] [PubMed] [Google Scholar]
- Hall J. A multicenter randomized control trial of non‐operative and operative treatment of displaced clavicle shaft fractures. Journal of Bone and Joint Surgery. British Volume 2008; Vol. 90‐B, issue Suppl I:105‐6.
- Hall J, McKee MD, Wild LM, Schemitsch EH, Jones AL, Schmidt AH. A multicenter PRCT of non‐operative versus operative treatment of midshaft clavicle fractures [abstract]. American Academy of Orthopaedic Surgeons Annual Meeting; 2006 March 22‐26; Chicago (IL). 2006.
- McKee MD. Standard deviations and means of DASH and Constant scores that could be used in our review [personal communication]. Email to: M Lenza 5 February 2012.
- McKee MD, Thompson C, Wild L, Schemitsch EH. The effect of a clavicle shaft fracture on general health status: results of a prospective, randomized clinical trial PAPER 120. Journal of Bone and Joint Surgery. British Volume 2010; Vol. 92‐B, issue SUPP I:25.
- Neuhaus V, Ring D. Effect of different statistical methods on union or time to union in a published study about clavicular fractures. Journal of Shoulder and Elbow Surgery 2013;22(4):471‐7. [DOI] [PubMed] [Google Scholar]
- Pearson AM, Tosteson AN, Koval KJ, McKee MD, Cantu RV, Bell JE, et al. Is surgery for displaced, midshaft clavicle fractures in adults cost‐effective? Results based on a multicenter randomized, controlled trial. Journal of Orthopaedic Trauma 2010;24(7):426‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schemitsch EH, Schemitsch L, Veillette C, McKee MD, COTS CO. Improved outcome following primary operative fixation of displaced midshaft fractures of the clavicle persists at two years post‐injury: implications for clinical treatment, future trials, and economic analysis. Journal of Bone and Joint Surgery. British Volume 2012;94‐B(SUPP XXXVIII):202. [Google Scholar]
- Schemitsch LA, Schemitsch EH, Veillette C, Zdero R, McKee MD. Function plateaus by one year in patients with surgically treated displaced midshaft clavicle fractures. Clinical Orthopaedics and Related Research 2011;469(12):3351‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Figueiredo 2008 {published data only}
- Figueiredo EA, Neves EJ, Yoshizawa H Jr, Dall'Ara Neto A, Nascimento LFC, Faria GHM, et al. Prospective randomized study comparing surgical treatment using anterior plate to non‐surgical treatment of midshaft clavicle fractures [Estudo prospectivo randomizado comparativo entre os tratamentos cirúrgico utilizando placa anterior e o não cirúrgico das fraturas do terço médio da clavícula]. Revista Brasileira de Ortopedia 2008;43(10):419‐25. [Google Scholar]
Judd 2009 {published and unpublished data}
- Judd DB, Pallis MP, Smith E, Bottoni CR. Acute operative stabilization versus nonoperative management of clavicle fractures. American Journal of Orthopedics (Belle Mead, N.J.) 2009;38(7):341‐5. [PubMed] [Google Scholar]
- Judd DB, Pallis MP, Smith E, Bottoni CR. Intramedullary fixation versus nonoperative treatment for mid‐shaft clavicle fractures: Paper #034. 72nd Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS). 2005 23‐27 February; Washington DC.
Koch 2008 {published data only}
- Koch HJ, Raschka C, Tonus C, Witzel K. The intramedullary osteosynthesis of the diaphyseal fracture of the clavicle compared to conservative treatment [Die intramedulläre osteosynthese der klavikuladiaphysenfraktur im vergleich zur konservativen therapie]. Deutsche Zeitschrift für Sportmedizin 2008;59(4):91‐4. [Google Scholar]
- Witzel K. Intramedullary osteosynthesis in fractures of the mid‐third of the clavicle in sports traumatology [Intramedulläre osteosynthese bei schaftfrakturen der klavikula in der sporttraumatologie]. Zeitschrift für Orthopädie und Unfallchirurgie 2007;145(5):639‐42. [DOI] [PubMed] [Google Scholar]
Melean 2015 {published and unpublished data}
- Melean PA. Randomization used in the trial and standard deviations and means of DASH and Constant scores that could be used in our review [personal communication]. Email to: M Lenza 20 August 2017.
- Melean PA, Marsalli M. Response to letter to the Editor regarding "Surgical treatment of displaced middle‐third clavicular fractures: a prospective, randomized trial in a working compensation population". Journal of Shoulder and Elbow Surgery 2015;24(11):e322. [DOI] [PubMed] [Google Scholar]
- Melean PA, Zuniga A, Marsalli M, Fritis NA, Cook ER, Zilleruelo M, et al. Surgical treatment of displaced middle‐third clavicular fractures: a prospective, randomized trial in a working compensation population. Journal of Shoulder and Elbow Surgery 2015;24(4):587‐92. [DOI] [PubMed] [Google Scholar]
Mirzatolooei 2011 {published data only}
- Mirzatolooei F. Comparison between operative and nonoperative treatment methods in the management of comminuted fractures of the clavicle. Acta Orthopaedica et Traumatologica Turcica 2011;45(1):34‐40. [DOI] [PubMed] [Google Scholar]
- Mirzatolooei F. Standard deviations and means of DASH and Constant scores used in our review [personal communication]. Email to: M Lenza 11 March 2012.
Naveen 2017 {published data only}
- Naveen BM, Joshi GR, Harikrishnan B. Management of mid‐shaft clavicular fractures: comparison between non‐operative treatment and plate fixation in 60 patients. Strategies in Trauma and Limb Reconstruction 2017;12(1):11‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robinson 2013a {published data only}
- Goudie EB, Clement ND, Murray IR, Lawrence CR, Wilson M, Brooksbank AJ, et al. The influence of shortening on clinical outcome in healed displaced midshaft clavicular fractures after nonoperative treatment. Journal of Bone and Joint Surgery. American Volume 2017;99(14):1166‐72. [DOI] [PubMed] [Google Scholar]
- Robinson CM, Goudie EB, Murray IR, Akhtar A, Jenkins P, Read E, et al. Operative fixation of displaced mid‐shaft clavicle fractures: a multi‐centre stratified randomised control trial. bjjprocs.boneandjoint.org.uk/content/95‐B/SUPP_5/3 (accessed 10 June 2017);95‐B(SUPP 5):3. [Google Scholar]
- Robinson CM, Goudie EB, Murray IR, Jenkins PJ, Ahktar MA, Read EO, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. Journal of Bone and Joint Surgery. American Volume 2013;95(17):1576‐84. [DOI] [PubMed] [Google Scholar]
Smekal 2009 {published and unpublished data}
- Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures ‐ a randomized, controlled, clinical trial. Journal of Orthopaedic Trauma 2009;23(2):106‐12. [DOI] [PubMed] [Google Scholar]
- Vinzenz S, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures. a randomized, controlled, clinical trial. 21st Congress of the European Society for Surgery of the Shoulder and Elbow. Brugge, Belgium, 2008 Sept 18.
Tamaoki 2017 {published and unpublished data}
- Tamaoki MJS. Structure used in the trial [personal communication]. Email to: M Lenza 12 August 2017.
- Tamaoki MJS, Matsunaga FT, Costa ARFD, Netto NA, Matsumoto MH, Belloti JC. Treatment of displaced midshaft clavicle fractures: figure‐of‐eight harness versus anterior plate osteosynthesis: a randomized controlled trial. Journal of Bone and Joint Surgery. American Volume 2017;99(14):1159‐65. [DOI] [PubMed] [Google Scholar]
- Costa AR. Treatment of midshaft clavicle fractures: plate fixation versus figure‐of‐eight bandage: randomised controlled clinical trial. apps.who.int/trialsearch/Trial.aspx?TrialID=ISRCTN66495030 (accessed 6 May 2012).
Virtanen 2012a {published and unpublished data}
- Chutkan NB. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: a randomized clinical trial. Orthopedics 2012;35(11):961‐2. [DOI] [PubMed] [Google Scholar]
- Virtanen KJ, Paavola MP, Remes VM, Pajarinen J, Savolainen V, Bjorkenheim JM. Nonoperative versus operative treatment of midshaft clavicle fractures: a randomized controlled trial (Paper no 331). 75th Annual Meeting of the an Academy of Orthopaedic Surgeons; 9‐12 March 2010. New Orleans (LA), 2010.
- Virtanen KJ, Remes V, Pajarinen J, Savolainen V, Björkenheim JM, Paavola M. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures: a randomized clinical trial. Journal of Bone and Joint Surgery. American Volume 2012;94(17):1546‐53. [DOI] [PubMed] [Google Scholar]
- Virtanen KJ, Remes V, Pajarinen J, Savolainen V, Björkenheim JM, Paavola MP. Study comparing plate stabilization to conservative treatment in midshaft clavicle fractures. clinicaltrials.gov/ct2/show/NCT01199653 (accessed 4 May 2012).
Woltz 2017a {published data only}
- Stegeman SA. Displaced midshaft fractures of the clavicle: non‐operative treatment versus plate fixation. A multi‐centre randomised controlled trial in the Netherlands. ‐ Sleutel‐TRIAL. apps.who.int/trialsearch/Trial.aspx?TrialID=NTR2399 (accessed 4 May 2012).
- Stegeman SA, Jong M, Sier CF, Krijnen P, Duijff JW, Thiel TP, et al. Displaced midshaft fractures of the clavicle: non‐operative treatment versus plate fixation (Sleutel‐TRIAL). A multicentre randomised controlled trial. BMC Musculoskeletal Disorders 2011;12:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woltz S. Standard deviations and means of VAS used in our review [personal communication]. Email to: M Lenza 15 August 2017.
- Woltz S, Stegeman SA, Krijnen P, Dijkman BA, Thiel TP, Schep NW, et al. Plate fixation compared with nonoperative treatment for displaced midshaft clavicular fractures: a multicenter randomized controlled trial. Journal of Bone and Joint Surgery. American Volume 2017;99(2):106‐12. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
ACTRN12610000948099 {unpublished data only}
- Clitherow HS. Displaced midshaft clavicle fractures: conservative management vs plate fixation. A multi‐centre randomised controlled trial. apps.who.int/trialsearch/Trial.aspx?TrialID=ACTRN12610000948099 (accessed 4 May 2012).
Bernstein 2007 {published data only}
- Bernstein J. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Journal of Bone and Joint Surgery. American Volume 2007;89(8):1866‐7. [DOI] [PubMed] [Google Scholar]
Bohme 2011 {published data only}
- Bohme J, Bonk A, Bacher GO, Wilharm A, Hoffmann R, Josten C. Current treatment concepts for mid‐shaft fractures of the clavicle ‐ results of a prospective multicentre study [Aktuelle behandlungskonzepte der klavikulaschaftfraktur ‐ Ergebnisse einer prospektiven multicenterstudie]. Zeitschrift für Orthopädie und Unfallchirurgie 2011;149(1):68‐76. [DOI] [PubMed] [Google Scholar]
Bravo 2009 {published data only}
- Bravo CJ, Wright CA. Displaced, comminuted diaphyseal clavicle fracture. Journal of Hand Surgery ‐ American Volume 2009;34(10):1883‐5. [DOI] [PubMed] [Google Scholar]
Dugar 2013 {published data only}
- Dugar N, Hossain E, Bandyopadhyay U, Shaw R. A comparative study of non‐operative and operative management in fracture clavicle. Journal of the Indian Medical Association 2013;111(12):806, 808‐9. [PubMed] [Google Scholar]
Jones 2014 {published data only}
- Jones LD, Grammatopoulos G, Kambouroglou G. Titanium elastic nails, open reduction internal fixation and non‐operative management for middle third clavicle fractures: a comparative study. European Journal of Orthopaedic Surgery & Traumatology: Orthopédie Traumatologie 2014;24(3):323‐9. [DOI] [PubMed] [Google Scholar]
Jubel 2002 {published data only}
- Jubel A, Andermahr J, Faymonville C, Binnebosel M, Prokop A, Rehm KE. Reconstruction of shoulder‐girdle symmetry after midclavicular fractures. Stable, elastic intramedullary pinning versus rucksack bandage [Wiederherstellung der symmetrie des schultergürtels bei klavikulafrakturen elastisch stabile intramedulläre osteosynthese vs. rucksackverband]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 2002;73(10):978‐81. [DOI] [PubMed] [Google Scholar]
Jubel 2005 {published data only}
- Jubel A, Andermahr J, Prokop A, Lee JI, Schiffer G, Rehm KE. Treatment of mid‐clavicular fractures in adults. Early results after rucksack bandage or elastic stable intramedullary nailing [Die Behandlung der diaphysären Kla vikulafraktur Ver gleich der Früher gebnisse nach Rucksackverband und elastisch stabiler intramedullärer Nagelung]. Der Unfallchirurg 2005;108(9):707‐14. [DOI] [PubMed] [Google Scholar]
Khorami 2014 {published data only}
- Khorami M, Fakour M, Mokarrami H, Arti HR, Nasab AM, Shahrivar F. The comparison of results of treatment of midshaft clavicle fracture between operative treatment with plate and non‐operative treatment. Archives of Bone and Joint Surgery 2014;2(3):210‐4. [PMC free article] [PubMed] [Google Scholar]
- Mokarrami H, Shahrivar, F. The comparison of the effect of surgical treatment of midshaft clavicle fracture with plate versus non operative treatment in imam Golestan and Razi hospital during 1390‐1392. apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2013061113633N1 (accessed 26 February 2018).
Kulshrestha 2011 {published data only}
- Kulshrestha V, Roy T, Audige L. Operative versus nonoperative management of displaced midshaft clavicle fractures: a prospective cohort study. Journal of Orthopaedic Trauma 2011;25(1):31‐8. [DOI] [PubMed] [Google Scholar]
Madhukar 2015 {published data only}
- Madhukar KT, Sateesh GS. A comparative study of clavicle fractures by conservative and operative management. Indian Journal of Public Health Research and Development 2015;6(4):226‐31. [Google Scholar]
Malkoc 2016 {published data only}
- Malkoc M, Korkmaz O, Bayram E, Ormeci T, Isyar M, Yilmaz M, et al. Short‐term results of Robinson type 2B2 clavicular fractures treated conservatively or surgically. Orthopedics 2016;39(2):e276‐9. [DOI] [PubMed] [Google Scholar]
McIntosh 2016 {published data only}
- McIntosh AL. Surgical treatment of adolescent clavicle fractures: results and complications. Journal of Pediatric Orthopedics 2016;36(Suppl 1):S41‐3. [DOI] [PubMed] [Google Scholar]
McKee 2010b {published data only}
- McKee MD. Clavicle fractures in 2010: sling/swathe or open reduction and internal fixation?. Orthopedic Clinics of North America 2010;41(2):225‐31. [DOI] [PubMed] [Google Scholar]
NCT00642265 {unpublished data only}
- Vandekerckhove PJ. Status of publication [personal communication]. Email to: M Lenza 17 September 2017.
- Vandekerckhove PJ, Berghs B, Vandendriessche G, Vanonverschelde J, Daele JVD, Wilde LD. The treatment of displaced, midshaft clavicular fractures: operative vs conservative. A prospected, randomized study . apps.who.int/trialsearch/Trial.aspx?TrialID=NCT00642265 (accessed 06 May 2012).
NCT01311219 {unpublished data only}
- White RA. Study comparing intramedullary nailing, plate fixation, and non‐operative treatment of clavicle fractures . apps.who.int/trialsearch/Trial.aspx?TrialID=NCT01311219 (accessed 04 May 2012).
Parry 2017 {published data only}
- Parry JA, Straaten M, Luo TD, Simon AL, Ashraf A, Kaufman K, et al. Is there a deficit after nonoperative versus operative treatment of shortened midshaft clavicular fractures in adolescents?. Journal of Pediatric Orthopedics 2017;37(4):227‐33. [DOI] [PubMed] [Google Scholar]
Shukla 2014 {published data only}
- Shukla A, Sinha S, Yadav G, Beniwal S. Comparison of treatment of fracture midshaft clavicle in adults by external fixator with conservative treatment. Journal of Clinical Orthopaedics and Trauma 2014;5(3):123‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simon 2010 {published data only}
- Simon P. Mid‐clavicle fractures in adults: surgery or not?. European Journal of Orthopaedic Surgery and Traumatology 2010;20(7):521‐5. [Google Scholar]
Smekal 2011 {published data only}
- Smekal V, Irenberger A, Attal RE, Oberladstaetter J, Krappinger D, Kralinger F. Elastic stable intramedullary nailing is best for mid‐shaft clavicular fractures without comminution: results in 60 patients. Injury 2011;42(4):324‐9. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Dhakad 2016 {published data only}
- Dhakad RK, Panwar M, Gupta S. Plating versus conservative treatment in mid shaft fractures of clavicle: a comparative study. Journal of Clinical Orthopaedics and Trauma 2016;7(Suppl 2):166‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN00825817 {unpublished data only}
- ISRCTN00825817. Open reduction and internal fixation (ORIF) versus conservative treatment of high energy clavicle fractures. apps.who.int/trialsearch/Trial.aspx?TrialID=ISRCTN00825817 (accessed 07 May 2012).
ISRCTN57483251 {unpublished data only}
- ISRCTN57483251. Assessment of patients with midshaft clavicular fractures randomised to either conservative or operative treatment. apps.who.int/trialsearch/Trial.aspx?TrialID=ISRCTN57483251 (accessed 07 May 2012).
Shetty 2017 {published data only}
- Shetty SK, Chandran R, Ballal A, Mathias LJ, Hegde A, Shetty A. To operate or not to operate the mid‐shaft fractures of the clavicle: a comparative study of functional outcomes of the two methods of management. Journal of Clinical and Diagnostic Research 2017;11(1):RC01‐RC03. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2001 {published data only}
- Smith CA, Rudd J, Crosby LA. Results of operative versus nonoperative treatment for 100% displaced midshaft clavicle fractures: a prospective randomized clinical trial. 16th Annual Open Meeting of the American Shoulder and Elbow Surgeons. Orlando, FL, 18 March 2000:Paper no 31.
- Smith CA, Rudd JN, Crosby LA. Results of operative versus nonoperative treatment for 100% displaced mid‐shaft clavicle fractures: a prospective randomized clinical trial [abstract]. American Academy of Orthopaedic Surgeons 68th Annual Meeting. San Francisco (CA), 27 February‐4 March 2001.
References to ongoing studies
NCT00590850 {unpublished data only}
- NCT00590850. A multicenter, prospective, randomized trial of non‐operative versus operative treatment for high‐energy midshaft clavicle fractures. apps.who.int/trialsearch/Trial.aspx?TrialID=NCT00590850 (accessed 17 September 2017).
NCT01078480 {unpublished data only}
- NCT01078480. Conservative treatment versus plate osteosynthesis using angular stabile screws and precontoured plates in displaced midshaft clavicular fractures. A prospective randomized multicenter study. apps.who.int/trialsearch/Trial.aspx?TrialID=NCT01078480 (accessed 17 September 2017).
NCT01483482 {unpublished data only}
- Ban I. Status of publication [personal communication]. Email to: M Lenza 17 September 2017.
- NCT01483482. Treatment of displaced, midshaft clavicle fractures. Sling or plate?. apps.who.int/trialsearch/Trial.aspx?TrialID=NCT01483482 (accessed 04 May 2012).
Additional references
Allman 1967
- Allman FL Jr. Fractures and ligamentous injuries of the clavicle and its articulation. Journal of Bone and Joint Surgery. American Volume 1967;49(4):774‐84. [PubMed] [Google Scholar]
Altamimi 2008
- Altamimi SA, McKee MD, Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. Journal of Bone and Joint Surgery. American Volume 2008;90(Suppl 2, Pt 1):1‐8. [DOI] [PubMed] [Google Scholar]
Amstutz 1981
- Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clinical Orthopaedics and Related Research 1981;(155):7‐20. [PubMed] [Google Scholar]
Andersen 1987
- Andersen K, Jensen PO, Lauritzen J. Treatment of clavicular fractures. Figure‐of‐eight bandage versus a simple sling. Acta Orthopaedica Scandinavica 1987;58(1):71‐4. [DOI] [PubMed] [Google Scholar]
Andresen 2018
- Andresen AK, Paulsen RT, Busch F, Isenberg‐Jørgensen A, Carreon LY, Andersen MØ. Patient‐reported outcomes and patient‐reported satisfaction after surgical treatment for cervical radiculopathy. Global Spine Journal 2018;8(7):703‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Angst 2001
- Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF‐36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis and Rheumatism 2001;45(4):384‐91. [DOI] [PubMed] [Google Scholar]
Ban 2012
- Ban I, Branner U, Holck K, Krasheninnikoff M, Troelsen A. Clavicle fractures may be conservatively treated with acceptable results ‐ a systematic review. Danish Medical Journal 2012;59(7):A4457. [PubMed] [Google Scholar]
Ban 2016
- Ban I, Nowak J, Virtanen K, Troelsen A. Overtreatment of displaced midshaft clavicle fractures. Acta Orthopaedica 2016;87(6):541‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bauer 2018
- Bauer DE, Hingsammer A, Schenk P, Vlachopoulos L, Imam MA, Fürnstahl P, et al. Are commercially‐available precontoured anatomical clavicle plating systems offering the purported superior optimum fitting to the clavicle? A cadaveric analysis and review of literature. Orthopaedics & Traumatology, Surgery & Research 2018;104(6):755‐8. [DOI] [PubMed] [Google Scholar]
Boehme 1991
- Boehme D, Curtis RJ Jr, DeHaan JT, Kay SP, Young DC, Rockwood CA Jr. Non‐union of fractures of the mid‐shaft of the clavicle. Treatment with a modified Hagie intramedullary pin and autogenous bone‐grafting. Journal of Bone and Joint Surgery. American Volume 1991;73(8):1219‐26. [PubMed] [Google Scholar]
Bradbury 1996
- Bradbury N, Hutchinson J, Hahn D, Colton CL. Clavicular nonunion. 31/32 healed after plate fixation and bone grafting. Acta Orthopaedica Scandinavica 1996;67(4):367‐70. [DOI] [PubMed] [Google Scholar]
Canadian 2007
- Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. Journal of Bone and Joint Surgery. American Volume 2007;89(1):1‐10. [DOI] [PubMed] [Google Scholar]
Cates 2008 [Computer program]
- Dr. Christopher Cates EBM website. Visual Rx. Version 3. Dr. Christopher Cates EBM website, 2008.
Constant 1987
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clinical Orthopaedics and Related Research 1987;214:160‐4. [PubMed] [Google Scholar]
Court‐Brown 2006
- Court‐Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006;37(8):691‐7. [DOI] [PubMed] [Google Scholar]
Deeks 2017
- Deeks JJ, Higgins JPT, Altman DG (editors) on behalf of the Cochrane Statistical Methods Group. Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Churchill R, Chandler J, Cumpston MS (editors), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Devji 2015
- Devji T, Kleinlugtenbelt Y, Evaniew N, Ristevski B, Khoudigian S, Bhandari M. Operative versus nonoperative interventions for common fractures of the clavicle: a meta‐analysis of randomized controlled trials. CMAJ Open 2015;3(4):E396‐405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Donnelly 2013
- Donnelly TD, Macfarlane RJ, Nagy MT, Ralte P, Waseem M. Fractures of the clavicle: an overview. Open Orthopaedics Journal 2013;7:329‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duan 2011
- Duan X, Zhong G, Cen S, Huang F, Xiang Z. Plating versus intramedullary pin or conservative treatment for midshaft fracture of clavicle: a meta‐analysis of randomized controlled trials. Journal of Shoulder Elbow Surgery 2011;20(6):1008‐15. [DOI] [PubMed] [Google Scholar]
Ebraheim 1997
- Ebraheim NA, Mekhail AO, Darwich M. Open reduction and internal fixation with bone grafting of clavicular nonunion. Journal of Trauma‐Injury Infection & Critical Care 1997;42(4):701‐4. [DOI] [PubMed] [Google Scholar]
Eccleston 2010
- Eccleston C, Moore RA, Derry S, Bell RF, McQuay H. Improving the quality and reporting of systematic reviews. European Journal of Pain 2010;14(7):667‐9. [DOI] [PubMed] [Google Scholar]
Eiff 1997
- Eiff MP. Management of clavicle fractures. American Family Physician 1997;55(1):121‐8. [PubMed] [Google Scholar]
Ferran 2010
- Ferran NA, Hodgson P, Vannet N, Williams R, Evans RO. Locked intramedullary fixation vs plating for displaced and shortened mid‐shaft clavicle fractures: a randomized clinical trial. Journal of Shoulder and Elbow Surgery 2010;19(6):783‐9. [DOI] [PubMed] [Google Scholar]
Goudie 2017
- Goudie EB, Clement ND, Murray IR, Lawrence CR, Wilson M, Brooksbank AJ, et al. The influence of shortening on clinical outcome in healed displaced midshaft clavicular fractures after nonoperative treatment. Journal of Bone and Joint Surgery. American Volume 2017;99(14):1166‐72. [DOI] [PubMed] [Google Scholar]
Gummesson 2003
- Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self‐rated health change after surgery. BMC Musculoskeletal Disorders 2003;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hall 2006
- Hall J, McKee MD, Wild LM, Schemitsch EH, Jones AL, Schmidt AH. A multicenter PRCT of non‐operative versus operative treatment of midshaft clavicle fractures [abstract]. American Academy of Orthopaedic Surgeons Annual Meeting; 22‐26 March 2006. Chicago (IL), 2006.
Hall 2008
- Hall J. A multicenter randomized control trial of non‐operative and operative treatment of displaced clavicle shaft fractures. Journal of Bone and Joint Surgery. British Volume 2008; Vol. 90‐B, issue Suppl I:105‐6.
Henseler 2015
- Henseler JF, Kolk A, Zwaal P, Nagels J, Vliet Vlieland TP, Nelissen RG. The minimal detectable change of the Constant score in impingement, full‐thickness tears, and massive rotator cuff tears. Journal of Shoulder Elbow Surgery 2015;24(3):376‐81. [DOI] [PubMed] [Google Scholar]
Heuer 2014
- Heuer HJ, Boykin RE, Petit CJ, Hardt J, Millett PJ. Decision‐making in the treatment of diaphyseal clavicle fractures: is there agreement among surgeons? Results of a survey on surgeons' treatment preferences. Journal of Shoulder Elbow Surgery 2014;23(2):e23‐33. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2017
- Higgins JP, Altman DG, Sterne JA (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Churchill R, Chandler J, Cumpston MS (editors), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June2017), Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Hill 1997
- Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle‐third fractures of the clavicle gives poor results. The Journal of Bone and Joint Surgery. British Volume 1997;79(4):537‐9. [DOI] [PubMed] [Google Scholar]
Hudak 1996
- Hudak PL, Amadio PC, Bombardier C, Boland A, Fischer T, Flatow EL, et al. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). American Journal of Industrial Medicine 1996;29(6):602‐8. [DOI] [PubMed] [Google Scholar]
Jeray 2007
- Jeray KJ. Acute midshaft clavicular fracture. Journal of the American Academy of Orthopaedic Surgeons 2007;15(4):239‐48. [DOI] [PubMed] [Google Scholar]
Juni 1999
- Jüni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta‐analysis. JAMA 1999;282(11):1054‐60. [DOI] [PubMed] [Google Scholar]
Jupiter 1987
- Jupiter JB, Leffert RD. Non‐union of the clavicle. Associated complications and surgical management. Journal of Bone and Joint Surgery. American Volume 1987;69(5):753‐60. [PubMed] [Google Scholar]
Kellam 2018
- Kellam JF, Meinberg EG, Agel J, Karam MD, Roberts CS. Introduction: Fracture and Dislocation Classification Compendium‐2018: International Comprehensive Classification of Fractures and Dislocations Committee. Journal of Orthopaedic Trauma 2018;32 Suppl 1:S1‐S10. [DOI] [PubMed] [Google Scholar]
Khan 2009
- Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. Journal of Bone and Joint Surgery. American Volume 2009;91(2):447‐60. [DOI] [PubMed] [Google Scholar]
King 2015
- King PR, Ikram A, Lamberts RP. The treatment of clavicular shaft fractures with an innovative locked intramedullary device. Journal of Shoulder and Elbow Surgery 2015;24(1):e1‐6. [DOI] [PubMed] [Google Scholar]
Kong 2014
- Kong L, Zhang Y, Shen Y. Operative versus nonoperative treatment for displaced midshaft clavicular fractures: a meta‐analysis of randomized clinical trials. Archives of Orthopaedic and Trauma Surgery 2014;134(11):1493‐500. [DOI] [PubMed] [Google Scholar]
Kotelnicki 2006
- Kotelnicki JJ, Bote HO, Mitts KG. The management of clavicle fractures. Journal of the American Academy of Physician Assistants 2006;19(9):50, 53‐4, 56. [DOI] [PubMed] [Google Scholar]
Kukkonen 2013
- Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aärimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. Journal of Shoulder Elbow Surgery 2013;22(12):1650‐5. [DOI] [PubMed] [Google Scholar]
L'Insalata 1997
- L'Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self‐administered questionnaire for assessment of symptoms and function of the shoulder. Journal of Bone and Joint Surgery. American volume 1997;79(5):738‐48. [PubMed] [Google Scholar]
Laucis 2015
- Laucis NC, Hays RD, Bhattacharyya T. Scoring the SF‐36 in orthopaedics: a brief guide. Journal of Bone and Joint Surgery. American Volume 2015;97(19):1628‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lazarus 2001
- Lazarus MD. Fractures of the clavicle. In: Bucholz RW, Heckman JD editor(s). Rockwood & Greens fractures in adults. 5. Philadelphia: Lippincott‐Wilkins, 2001:1041‐78. [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6.4.11: Search filters. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Lenza 2015
- Lenza M, Faloppa F. Surgical interventions for treating acute fractures or non‐union of the middle third of the clavicle. Cochrane Database of Systematic Reviews 2015, Issue 5. [DOI: 10.1002/14651858.CD007428.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lenza 2016
- Lenza M, Faloppa F. Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database of Systematic Reviews 2016, Issue 12. [DOI: 10.1002/14651858.CD007121.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2013
- Liu GD, Tong SL, Ou S, Zhou LS, Fei J, Nan GX, et al. Operative versus non‐operative treatment for clavicle fracture: a meta‐analysis. International Orthopaedics 2013;37(8):1495‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Longo 2011
- Longo UG, Banerjee S, Barber J, Chambler A, Cobiella C, Corbett S, et al. Conservative management versus open reduction and internal fixation for mid‐shaft clavicle fractures in adults‐‐the Clavicle Trial: study protocol for a multicentre randomized controlled trial. Trials 2011;12:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marti 2003
- Marti RK, Nolte PA, Kerkhoffs GM, Besselaar PP, Schaap GR. Operative treatment of mid‐shaft clavicular non‐union. International Orthopaedics 2003;27(3):131‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
McKee 2006
- McKee MD, Pedersen EM, Jones C, Stephen DJ, Kreder HJ, Schemitsch EH, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. Journal of Bone and Joint Surgery. American Volume 2006;88(1):35‐40. [DOI] [PubMed] [Google Scholar]
McKee 2010a
- McKee MD, Thompson C, Wild L, Schemitsch EH. The effect of a clavicle shaft fracture on general health status: results of a prospective, randomized clinical trial PAPER 120. Journal of Bone and Joint Surgery. British Volume 2010; Vol. 92‐B, issue SUPP I:25.
McKee 2012
- McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta‐analysis of randomized clinical trials. Journal of Bone and Joint Surgery. American Volume 2012;94(8):678‐84. [DOI] [PubMed] [Google Scholar]
Meier 2006
- Meier C, Grueninger P, Platz A. Elastic stable intramedullary nailing for midclavicular fractures in athletes: indications, technical pitfalls and early results. Acta Orthopaedica Belgica 2006;72(3):269‐75. [PubMed] [Google Scholar]
Moore 2010
- Moore RA, Eccleston C, Derry S, Wiffen P, Bell RF, Straube S, et al. "Evidence" in chronic pain‐‐establishing best practice in the reporting of systematic reviews. Pain 2010;150(3):386‐9. [DOI] [PubMed] [Google Scholar]
Mullaji 1994
- Mullaji AB, Jupiter JB. Low‐contact dynamic compression plating of the clavicle. Injury 1994;25(1):41‐5. [DOI] [PubMed] [Google Scholar]
Muller 1991
- Muller M, Allgower M, Schneider R, Willenegger H. Manual of internal fixation: techniques recommended by the AO‐ASIF Group. 3rd Edition. Berlin: Springer‐Verlag, 1991. [Google Scholar]
Neer 1984
- Neer C. Fractures of the clavicle. In: Rockwood CA Jr, Green DP editor(s). Fractures in adults. 2nd Edition. Philadelphia: Lippincott Williams & Wilkins, 1984:707‐13. [Google Scholar]
Neuhaus 2013
- Neuhaus V, Ring D. Effect of different statistical methods on union or time to union in a published study about clavicular fractures. Journal of Shoulder and Elbow Surgery 2013;22(4):471‐7. [DOI] [PubMed] [Google Scholar]
Nordqvist 1994
- Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clinical Orthopaedics and Related Research 1994;300:127‐32. [PubMed] [Google Scholar]
Nordqvist 1998
- Nordqvist A, Petersson CJ, Redlund‐Johnell I. Mid‐clavicle fractures in adults: end result study after conservative treatment. Journal of Orthopaedic Trauma 1998;12(8):572‐6. [DOI] [PubMed] [Google Scholar]
Nowak 2000
- Nowak J, Mallmin H, Larsson S. The aetiology and epidemiology of clavicular fractures. A prospective study during a two‐year period in Uppsala, Sweden. Injury 2000;31(5):353‐8. [DOI] [PubMed] [Google Scholar]
Oliveira 2017
- Oliveira AS Jr, Roberto BB, Lenza M, Pintan GF, Ejnisman B, Schor B, et al. Preferences of orthopedic surgeons for treating midshaft clavicle fracture in adults [Preferências dos cirurgiões ortopédicos para o tratamento da fratura do terço médio da clavícula em adultos]. Einstein (Sao Paulo) 2017;15(3):295‐306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pearson 2010
- Pearson AM, Tosteson AN, Koval KJ, McKee MD, Cantu RV, Bell JE, et al. Is surgery for displaced, midshaft clavicle fractures in adults cost‐effective? Results based on a multicenter randomized, controlled trial. Journal of Orthopaedic Trauma 2010;24(7):426‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pieske 2008
- Pieske O, Dang M, Zaspel J, Beyer B, Löffler T, Piltz S. Midshaft clavicle fractures ‐ classification and therapy. Results of a survey at German trauma departments [Die Klavikulaschaftfraktur ‐ Klassifikation und Therapie. Ergebnisse einer Umfrage an unfallchirurgischen/orthopädischen Kliniken in Deutschland]. Der Unfallchirurg 2008;111(6):387‐94. [DOI] [PubMed] [Google Scholar]
Postacchini 2002
- Postacchini F, Gumina S, Santis P, Albo F. Epidemiology of clavicle fractures. Journal of Shoulder and Elbow Surgery 2002;11(5):452‐6. [DOI] [PubMed] [Google Scholar]
Qvist 2018
- Qvist AH, Vaesel MT, Jensen CM, Jensen SL. Plate fixation compared with nonoperative treatment of displaced midshaft clavicular fractures: a randomized clinical trial. Bone & Joint Journal 2018;100‐B(10):1385‐91. [DOI] [PubMed] [Google Scholar]
Rehn 2014
- Rehn CH, Kirkegaard M, Viberg B, Larsen MS. Operative versus nonoperative treatment of displaced midshaft clavicle fractures in adults: a systematic review. European Journal of Orthopaedic Surgery & Traumatology 2014;24(7):1047‐53. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Robinson 1998
- Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. Journal of Bone and Joint Surgery. British Volume 1998;80(3):476‐84. [DOI] [PubMed] [Google Scholar]
Robinson 2004
- Robinson CM, Court‐Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. Journal of Bone and Joint Surgery. American Volume 2004;86(7):1359‐65. [DOI] [PubMed] [Google Scholar]
Robinson 2013b
- Robinson CM, Goudie EB, Murray IR, Akhtar A, Jenkins P, Read E, et al. Operative fixation of displaced mid‐shaft clavicle fractures: a multi‐centre stratified randomised control trial. bjjprocs.boneandjoint.org.uk/content/95‐B/SUPP_5/3 (accessed 10 June 2017);95‐B(SUPP 5):3. [Google Scholar]
Roy 2010
- Roy JS, MacDermid JC, Woodhouse LJ. A systematic review of the psychometric properties of the Constant‐Murley score. Journal of Shoulder Elbow Surgery 2010;19(1):157‐64. [DOI] [PubMed] [Google Scholar]
Schemitsch 2011
- Schemitsch LA, Schemitsch EH, Veillette C, Zdero R, McKee MD. Function plateaus by one year in patients with surgically treated displaced midshaft clavicle fractures. Clinical Orthopaedics and Related Research 2011;469(12):3351‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schemitsch 2012
- Schemitsch EH, Schemitsch L, Veillette C, McKee MD, COTS CO. Improved outcome following primary operative fixation of displaced midshaft fractures of the clavicle persists at two years post‐injury: implications for clinical treatment, future trials, and economic analysis. Journal of Bone and Joint Surgery. British Volume 2012;94‐B(SUPP XXXVIII):202. [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and 'Summary of findings' tables. In: Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Simovitch 2018
- Simovitch R, Flurin PH, Wright T, Zuckerman JD, Roche CP. Quantifying success after total shoulder arthroplasty: the minimal clinically important difference. Journal of Shoulder Elbow Surgery 2018;27(2):298‐305. [DOI] [PubMed] [Google Scholar]
Smeeing 2017
- Smeeing DPJ, Ven DJC, Hietbrink F, Timmers TK, Heijl M, Kruyt MC, et al. Surgical versus nonsurgical treatment for midshaft clavicle fractures in patients aged 16 years and older: a systematic review, meta‐analysis, and comparison of randomized controlled trials and observational studies. American Journal of Sports Medicine 2017;45(8):1937‐45. [DOI] [PubMed] [Google Scholar]
Stegeman 2011
- Stegeman SA, Jong M, Sier CF, Krijnen P, Duijff JW, Thiel TP, et al. Displaced midshaft fractures of the clavicle: non‐operative treatment versus plate fixation (Sleutel‐TRIAL). A multicentre randomised controlled trial. BMC Musculoskeletal Disorders 2011;12:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2008
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Intervention. Version 5.0.1 (updated September 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org. Available from www.cochrane‐handbook.org.
Tashjian 2009
- Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. Journal of Shoulder Elbow Surgery 2009;18(6):927‐32. [DOI] [PubMed] [Google Scholar]
Tashjian 2017
- Tashjian RZ, Hung M, Keener JD, Bowen RC, McAllister J, Chen W, et al. Determining the minimal clinically important difference for the American Shoulder and Elbow Surgeons score, Simple ShoulderTest, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. Journal of Shoulder Elbow Surgery 2017;26(1):144‐8. [DOI] [PubMed] [Google Scholar]
Torren 2016
- Torrens C, Guirro P, Santana F. The minimal clinically important difference for function and strength in patients undergoing reverse shoulder arthroplasty. Journal of Shoulder Elbow Surgery 2016;25(2):262‐8. [DOI] [PubMed] [Google Scholar]
Vinzenz 2008
- Vinzenz S, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures. a randomized, controlled, clinical trial. 21st Congress of the European Society for Surgery of the Shoulder and Elbow, 18 September 2008. 2008. [DOI] [PubMed]
Virtanen 2012b
- Virtanen KJ, Malmivaara AOV, Remes VM, Paavola MP. Operative and nonoperative treatment of clavicle fractures in adults. Acta Orthopaedica 2012;83(1):65‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walton 2015
- Walton B, Meijer K, Melancon K, Hartman M. A cost analysis of internal fixation versus nonoperative treatment in adult midshaft clavicle fractures using multiple randomized controlled trials. Journal of Orthopaedic Trauma 2015;29(4):173‐80. [DOI] [PubMed] [Google Scholar]
Wang 2015a
- Wang XH, Guo WJ, Li AB, Cheng GJ, Lei T, Zhao YM. Operative versus nonoperative treatment for displaced midshaft clavicle fractures: a meta‐analysis based on current evidence. Clinics (Sao Paulo) 2015;70(8):584‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2015b
- Wang J, Meng XH, Guo ZM, Wu YH, Zhao JG. Interventions for treating displaced midshaft clavicular fractures: a Bayesian network meta‐analysis of randomized controlled trials. Medicine (Baltimore) 2015;94(11):e595. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ware 1992
- Ware JE Jr, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36). I. Conceptual framework and item selection. Medical Care 1992;30(6):473‐83. [PubMed] [Google Scholar]
Williams 1999
- Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. American Journal of Sports Medicine 1999;27(2):214‐21. [DOI] [PubMed] [Google Scholar]
Witzel 2007
- Witzel K. Intramedullary osteosynthesis in fractures of the mid‐third of the clavicle in sports traumatology [Intramedulläre osteosynthese bei schaftfrakturen der klavikula in der sporttraumatologie]. Zeitschrift für Orthopädie und Unfallchirurgie 2007;145(5):639‐42. [DOI] [PubMed] [Google Scholar]
Woltz 2017b
- Woltz S, Krijnen P, Schipper IB. Plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a meta‐analysis of randomized controlled trials. Journal of Bone and Joint Surgery. American volume 2017;99(12):1051‐7. [DOI] [PubMed] [Google Scholar]
Xu 2013
- Xu CP, Li X, Cui Z, Diao XC, Yu B. Should displaced midshaft clavicular fractures be treated surgically? A meta‐analysis based on current evidence. European Journal of Orthopaedic Surgery and Traumatology 2013;23(6):621‐9. [DOI] [PubMed] [Google Scholar]
Xu 2014
- Xu J, Xu L, Xu W, Gu Y, Xu J. Operative versus nonoperative treatment in the management of midshaft clavicular fractures: a meta‐analysis of randomized controlled trials. Journal of Shoulder and Elbow Surgery 2014;23(2):173‐81. [DOI] [PubMed] [Google Scholar]
Yian 2005
- Yian EH, Ramappa AJ, Arneberg O, Gerber C. The Constant score in normal shoulders. Journal of Shoulder and Elbow Surgery 2005;14(2):128‐33. [DOI] [PubMed] [Google Scholar]
Zhou 2018
- Zhou L, Natarajan M, Miller BS, Gagnier JJ. Establishing minimal important differences for the VR‐12 and SANE scores in patients following treatment of rotator cuff tears. Orthopaedic Journal of Sports Medicine 2018;6(7):2325967118782159. [DOI: 10.1177/2325967118782159] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zlowodzki 2005
- Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence‐Based Orthopaedic Trauma Working Group. Journal of Orthopaedic Trauma 2005;19(7):504‐7. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Lenza 2011
- Lenza M, Buchbinder R, Johnston RV, Belloti JC, Faloppa F. Surgical versus conservative interventions for treating fractures of the middle third of the clavicle. Cochrane Database of Systematic Reviews 2011, Issue 10. [DOI: 10.1002/14651858.CD009363] [DOI] [PubMed] [Google Scholar]
Lenza 2013
- Lenza M, Buchbinder R, Johnston RV, Belloti JC, Faloppa F. Surgical versus conservative interventions for treating fractures of the middle third of the clavicle. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD009363.pub2] [DOI] [PubMed] [Google Scholar]


