Abstract
Purpose: We conducted a systematic review of the effect of early mobility on length of stay (LOS), mortality, and clinical outcomes as a treatment for adults hospitalized with pneumonia. Method: An electronic search of four databases was conducted. Inclusion criteria were (1) acute medical condition of pneumonia in adults and (2) early mobility intervention. Quality appraisal was conducted using the Physiotherapy Evidence Database scale and the Newcastle-Ottawa Scale. Results: Four studies (three randomized controlled trials and one retrospective cohort study) met the inclusion criteria. Meta-analysis demonstrated that early mobility did not reduce the risk of mortality compared with usual care (risk ratio 0.9 [95% CI: 0.27, 2.97]; p = 0.86) but did reduce the mean LOS (–1.1 days [95% CI: 2.21, –0.04]; p = 0.04). Early mobility also did not affect the rate of hospital readmissions or emergency department visits. One study demonstrated an improvement in functional exercise capacity and quality of life related to physical function and faster completion of a measure of activities of daily living. Conclusions: Early mobility reduced LOS in adults hospitalized with community-acquired pneumonia, although there was no effect on mortality or rate of hospital readmissions. Further research is needed to determine the effect of early mobility in this population and establish guidelines.
Key Words: early mobilization, hospitalization, pneumonia, treatment, systematic review
Abstract
Objectif : analyse systématique de l’effet de la mobilité précoce sur la durée d’hospitalisation (DH), la mortalité et les résultats cliniques dans le traitement des adultes hospitalisés à cause d’une pneumonie. Méthodologie : recherche dans quatre bases de données. Les critères d’inclusion étaient 1) une pneumonie aiguë chez l’adulte et 2) une intervention de mobilité précoce. Les chercheurs ont procédé à l’évaluation de la qualité au moyen de l’échelle de la base de données de la physiothérapie fondée sur les preuves et de l’échelle de Newcastle-Ottawa. Résultats : quatre études (trois essais cliniques aléatoires et une étude de cohorte rétrospective) respectaient les critères d’inclusion. La méta-analyse a démontré que la mobilité précoce ne réduisait pas le risque de mortalité par rapport aux soins habituels (risque relatif de 0,9 [IC 95 % : 0,27, 2,97]; p = 0,86), mais réduisait la DH moyenne (−1,1 jour [IC à 95 % : 2,21, −0,04]; p = 0,040). Par ailleurs, la mobilité précoce n’avait pas d’incidence sur le taux de réhospitalisations ou de consultations à l’urgence. Une étude a démontré une amélioration de la capacité fonctionnelle à l’exercice et à la qualité de vie liée à la fonction physique ainsi qu’une exécution plus rapide des mesures d’activités de la vie quotidienne. Conclusion : la mobilité précoce réduisait la DH chez les adultes hospitalisés à cause d’une pneumonie extra-hospitalière, mais n’avait pas d’effet sur la mortalité ni sur le taux de réhospitalisations. Avant d’établir des lignes directrices, il faudra réaliser d’autres recherches pour déterminer l’effet de la mobilité précoce auprès de cette population.
Mots-clés : analyse systématique, hospitalisation, mobilisation précoce, pneumonie, traitement
Medical research has described community-acquired pneumonia as a lower respiratory tract infection characterized by cough, fever, chills, fatigue, dyspnoea, rigors, and pleuritic chest pain, which may be accompanied by new infiltrates on chest radiography.1,2 It is a leading cause of morbidity and mortality and an economic burden worldwide.2–4 Pneumonia is a leading infectious cause of hospitalization and death among adults in the United States,5,6 with medical costs exceeding $10 billion (US) in 2011.7 Mortality is highest in the United States for patients with pneumonia requiring hospitalization, with a 30-day mortality rate of 23%.8 In addition, the average length of stay (LOS) for patients admitted with pneumonia is 5.2 days, and 10%–20% of patients require admission to an intensive care unit.9
In addition to antimicrobial therapy prescribed to manage pneumonia,10 evidence supports early mobility as part of treatment.11 Early mobilization is frequently prescribed to manage postoperative complications and to treat atelectasis and sputum retention, and it is associated with reducing LOS, improving functional mobility, and promoting airway clearance.12–17 The benefits of early mobilization have been further recognized as mitigating adverse multisystem sequelae of bedrest, including muscle weakness, microvascular dysfunction, deconditioning, physical activity intolerance, and decline in functional capacity in hospitalized patients.18,19
The literature supports the safety and effectiveness of early mobility and recommends it as a core treatment in the physiotherapy management of critically ill patients.18–20 Current guidelines for managing individuals with complicated pneumonia incorporate mobilization, with recommendations including sitting out of bed for 20 minutes within the first 24 hours after admission, in addition to traditional airway clearance techniques and continuous positive airway pressure.21 However, the benefits of early mobility as a treatment for community-acquired pneumonia remain unclear.
The aim of this systematic review was to evaluate the effectiveness of early mobility on primary outcome measures—LOS and mortality—and secondary outcomes—rates of hospital readmission, emergency department visits, physical function, exercise capacity, dyspnoea, and quality of life—in adults with community-acquired pneumonia. This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.22
METHODS
Inclusion criteria
We considered randomized controlled trials (RCTs) and observational studies that compared an in-patient-based early mobility intervention with a control treatment. All participants were adults (aged 17 y or older) and were diagnosed with an acute medical condition of community-acquired pneumonia but were not intubated or ventilated. Early mobility was defined as movement out of bed, with a change from the horizontal to the upright position for at least 20 minutes during the first 24 hours after hospitalization; this definition is consistent with guidelines for managing complicated pneumonia,21 with movement progressing each subsequent day during hospitalization.23 The word early reflects recommendations that mobility be initiated immediately after physiological stabilization in acutely ill patients with the requisite cognitive function and that early mobilization activities need to be sufficient to challenge the cardiopulmonary, musculoskeletal, and neuromuscular systems.18,20
Exclusion criteria
We excluded studies in which participants had been diagnosed with acute medical conditions other than pneumonia, including pulmonary embolism, pleural effusion, pneumothorax, congestive heart failure, lung neoplasm, acute respiratory distress syndrome, lung abscess, acute respiratory failure, acute bronchitis, chest trauma (including rib fractures), and acute myocardial infarction. We also excluded studies if they had not been published in English and if they included physiotherapy interventions administered to patients only in a recumbent position.
Outcome measures
The primary outcome measures were LOS and mortality. The secondary outcome measures were rate of hospital readmission and emergency visits and measures of physical function, exercise capacity, symptoms, and quality of life.
Search strategy
We conducted an electronic search of PUBMED, CINAHL, MEDLINE, and EMBASE for studies published before July 2015. An updated search was performed in January 2017. Keywords used were pneumonia AND adult AND treatment AND hospital OR ICU or CCU or critical care OR acute care or intensive care AND physical therapy OR physiotherapy OR rehabilitation. An example of the completed search strategy on PUBMED is included in the Appendix.
Selection of studies and data extraction
Two groups of two reviewers each (MR and JV, OV and SM) independently assessed abstracts, full text, or both as necessary to identify relevant articles on the basis of the specified inclusion and exclusion criteria. Kappa values were calculated to determine interrater agreement for the included and excluded studies. Any discrepancies between the reviewers in a group were resolved by another independent reviewer (TL). Data for participant description, intervention description, severity and type of pneumonia, and outcome measures were extracted using a standardized template.
Assessment of risk of bias
Two independent reviewers conducted quality appraisal on the selected studies on the basis of the Physiotherapy Evidence Database (PEDro) scale (for the RCTs)24 or the Newcastle-Ottawa Scale (for the non-randomized studies).25 The Newcastle-Ottawa Scale contains eight items categorized into three dimensions of selection, comparability, and outcome, with scores ranging from 0 to 9.25 Any differences were resolved by another independent reviewer (TL).
Data analysis
Meta-analysis was planned for two or more studies that were considered clinically homogeneous (having a similar model of intervention and outcome tools).26 Data were entered using Review Manager, version 5.3 (Cochrane Collaboration, Copenhagen). The pooled estimate of treatment effect for LOS was reported as mean difference, and mortality was reported using a risk ratio (RR), with random effects analysis applied. Forest plots were generated to depict results, and heterogeneity was tested according to the overlap in confidence intervals, interpretation of the χ2 test, and the I2 statistic, with substantial heterogeneity represented by an I2 greater than 50%.27 The reviewers attempted to contact the authors of two studies to determine mean LOS and received a response from the authors of one.28 When study findings could not be combined, a narrative format was used to report the results.
RESULTS
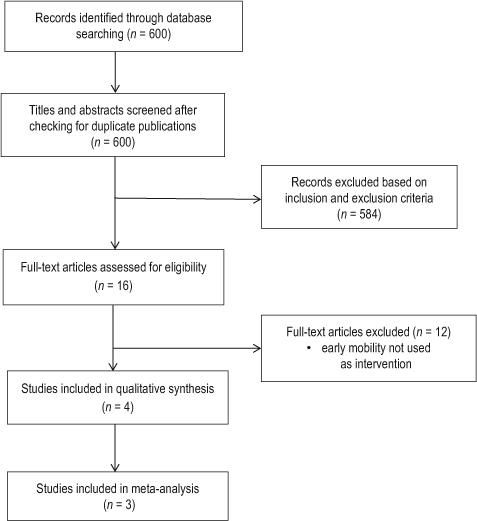
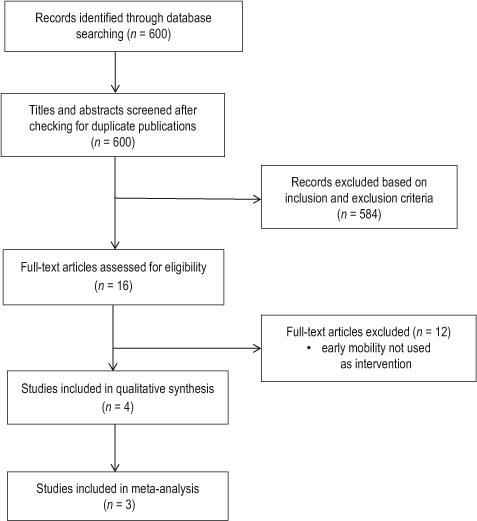
A total of 600 original articles were retrieved from the four electronic databases. Of these, 16 abstracts met the inclusion criteria, warranting full-text investigation; 12 articles were excluded because they did not meet the early mobility intervention inclusion criteria.23 Four trials met the inclusion criteria (see Figure 1): three RCTs conducted in the United States,23 Brazil,28 and Spain,29 respectively, and one retrospective cohort study from Japan.30
Figure 1.
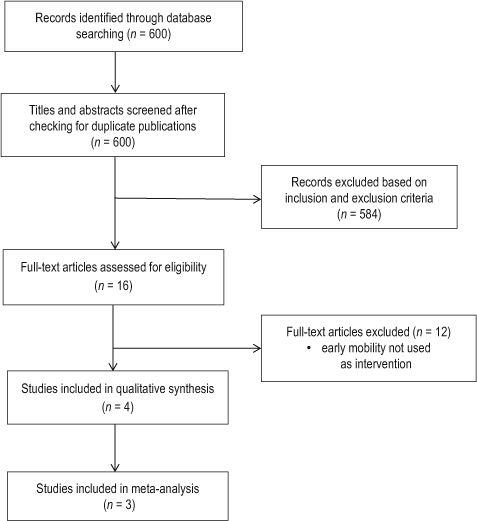
Flowchart of studies undergoing review.
The characteristics of the participants in the included studies and the comparison of within-group outcomes are outlined in Table 1. In total, 69,492 (RCTs 908, retrospective cohort 68,584) patients (32,961 male) were included. Patients ranged in age from 17 to 103 years. The diagnostic criteria for pneumonia were based on consensus guidelines in one study,28 based on set criteria in two studies,23,29 or were according to the International Statistical Classification of Diseases.30 Two studies reported the severity of pneumonia:23,29 in these studies, 405 patients had mild, 316 patients had moderate, and 138 patients had severe pneumonia.
Table 1.
Study Characteristics and Outcome Comparisons between Groups
| Study | Participants | Intervention | Outcome comparisons |
|---|---|---|---|
| Randomized clinical trials | |||
| Mundy et al.23 |
n = 458 (44% male) Age, range, min–max: 17–103 y Pneumonia criteria: new infiltrate on CXR and 1 major criterion (cough, sputum, temperature >37.8°C) or 2 minor criteria (pleuritic chest pain, dyspnoea, altered mental status, pulmonary consolidation on examination, leukocyte count >12,000/μL) |
Experimental: early mobility (movement out of bed, with a change from horizontal to upright position, for at least 20 min during the first 24 h of hospitalization, with progressive movement each d) Control: usual care |
LOS: reduced with early mobility compared with usual care (mean 5.8 vs. 6.9 d) Mortality (hospital and 90 d): no difference (hospital: 2.2% vs. 3.9%; 90 d: 9.7% vs. 8.7%) Hospital re-admission: no difference Emergency visits (30 d and 90 d): no difference |
| Carratala et al.29 |
n = 401 (35% male) Age, range, min–max: 18–97 y Pneumonia criteria: infiltrate on chest radiograph plus ≥1 of fever (≥38.0°C) or hypothermia (<35.0°C), new cough ± sputum production, pleuritic chest pain, dyspnoea, altered breath sounds on auscultation |
Experimental: early mobility (movement out of bed, with a change from horizontal to upright position, for at least 20 min during the first 24 h of hospitalization, with progressive movement each d) Control: usual care |
LOS: reduced with early mobility compared with usual care (median 3.9 d vs. 6.0 d; mean difference 2.1 (95% CI: –2.7, –1.7); p < 0.001 Mortality: no difference Hospital re-admission (30 d): no difference |
| Jose & Dal Corso28 |
n = 49 (55% male) Age: mean 55 (SD 20) y Pneumonia criteria: diagnosis of community-acquired pneumonia according to consensus guidelines* |
Experimental: mobility training (warm up, stretching, resistance exercises, aerobic walking training) 50 min/d × 8 d Control: usual care: 50 min/d × 8 d |
LOS: no difference in median (IQR) d (mobility: 12 [10–18] d; usual care: 13 [11–25] d) Glittre Activities of Daily Living test: mean (SD) time improved more with mobility training (52 [SD 40] sec) than with usual care (12 [SD 26] sec) ISWT distance: mean (SD) distance improved more with mobility training than with usual care (162 [SD 110] min vs. 33 [SD 71] min) Dyspnoea: decreased more in mobility training than in usual care group (mean difference –0.9 [95% CI: –1.4, –0.4]) SF-36: “physical functioning” domain improved more for mobility group (mean difference 14 points [95% CI: 1, 28]); no difference in any other domain |
| Retrospective cohort study | |||
| Momosaki et al.30 |
n = 68,584 (50% male) Population: frail elderly Age: mean 85 (SD 7) y Pneumonia criteria: diagnosis of aspiration pneumonia according to International Statistical Classification of Diseases |
Experimental: early rehabilitation by physical therapists (early ambulation, strengthening and endurance exercises initiated within 3 d of admission and done for at least 7 d) Control: no rehabilitation |
LOS: increased in early vs. no-rehabilitation group (mean 34.2 [SD 34.5] d vs. 26.2 [SD 37.4] d; p < 0.001) Mortality (hospital 30 d): lower in early vs. no-rehabilitation group (5.1% vs. 7.1%; p < 0.001) |
Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. CXR = chest X-ray; LOS = length of stay; ISWT = incremental shuttle walk test; SF-36 = Short Form Health Survey (36 items).
The specifics of the mobility interventions applied in the included studies are described in Table 1. Two studies defined early mobility as movement from bed, with a change from the horizontal to the upright position for at least 20 minutes during the first 24 hours of hospitalization, with subsequent progression.23,29 Momosaki and colleagues30 applied physical therapy interventions, which included early ambulation and adaptive or assistive exercises within 3 days of admission for at least 7 days. One study prescribed a daily session of aerobic exercise (ground-based walking) to a targeted intensity and peripheral muscle resistance training at an initial workload of 70% maximal peripheral muscle strength for 8 days.28
Risk of bias
All three RCTs used randomization processes, although concealed allocation was applied in only two of the studies.28,29 Participants, therapists, and assessors were not consistently blinded. The mean PEDro score for the three RCTs23,28,29 was 7.3 of 10 (see Table 2). For the cohort study,30 the Newcastle-Ottawa Scale scores for the three domains were selection 3, comparability 1, and outcome 2, for a total score of 6 out of 9.
Table 2.
Detailed PEDro Scores for Included Randomized Clinical Trials
| Study | Random allocation | Concealed allocation | Groups similar at baseline | Participant blinding | Therapist blinding | Assessor blinding | < 15% dropouts | Intention-to-treat analysis | Between-group difference reported | Point estimate and variability reported | Total (0–10) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mundy et al.23 | Y | N | Y | Y | N | Y | Y | Y | Y | Y | 8 |
| Carratala et al.29 | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7 |
| Jose & Dal Corso28 | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7 |
PEDro = Physiotherapy Evidence Database; Y = yes; N = no.
Effects of intervention
Length of stay
Two studies were pooled for meta-analysis, with early mobility significantly reducing mean LOS: mean difference –1.13 days (95% CI: –2.21, –0.04 days; p = 0.040; see Figure 2).23,28 Carratala and colleagues29 (see Table 1) also reported a significantly reduced median LOS of 3.9 days for early mobility versus 6.0 days for the usual-care group (p < 0.001). One study found no difference in median LOS (12 vs. 13 days),28 whereas Momosaki and colleagues30 found a longer mean LOS (shown in Table 1) among those undergoing early rehabilitation (34.2 (SD 34.5) days vs. 26.2 (SD 37.4) days; p < 0.001).
Figure 2.
Mean difference (95% CI) of the effect of early mobility versus usual care on hospital length of stay (in days) by pooling data from two studies (n = 507).
Mortality
The meta-analysis of two RCT trials,23,29 using random RR analysis, indicated that early mobility did not significantly lower the risk of mortality compared with usual care in adults with pneumonia (RR 0.90 [95% CI: 0.27, 2.97]; p = 0.86; see Figure 3). In the single retrospective cohort study (see Table 1), early rehabilitation was associated with a lower 30-day in-hospital mortality rate (5.1%) than usual care (7.1%).30
Figure 3.
Risk ratio (95% CI) of the impact of early mobility versus usual care on mortality by pooling data from two studies (n = 859).
Hospital readmission rates
Early mobility did not alter the rate of hospital readmissions23,29 or the number of emergency department visits23 compared with usual care (see Table 1).23,29
Physical function, exercise capacity, symptoms, and quality of life
Our study findings for physical function, exercise capacity, symptoms, and quality of life could not be subjected to meta-analysis because they were reported only in narrative format (see Table 1).28 Early mobility improved the incremental shuttle walking distance compared with usual care (mean difference 130 m [95% CI: 77, 182]).28 The early mobility group completed the Glittre Activities of Daily Living test faster by 39 seconds (95% CI: 20, 59).28 Early mobility also improved the physical function domain of the SF-36 quality of life questionnaire (mean difference 14 points [95% CI: 1, 28]) and reduced the severity of dyspnoea to a greater extent (mean difference 0.9 points [95% CI: 0.4, 1.4]).28
DISCUSSION
For adults hospitalized with community-acquired pneumonia, early mobility was associated with a reduced LOS, but no difference was found in mortality, hospital readmission rate, or emergency department presentation rate compared with usual care. The evidence for improved physical capacity, reduced severity of dyspnoea, and improved quality of life is limited.
The pooled findings of a reduced LOS with early mobility23,28 were supported by the lower LOS also reported by Carratala and colleagues.29 Although this result contrasts with the findings of Momosaki and colleagues,30 it may be related to the study design. In that retrospective analysis of consecutive patients admitted to 1,161 acute-care hospitals across Japan over a 2-year time period,30 other factors may have influenced LOS (e.g., undetermined consistency of physical therapy–led early rehabilitation programmes across settings) or the criteria for discharge, and they may differ from the other included trials conducted in the United States,23 Brazil,28 and Spain.29
In particular, Momosaki and colleagues noted that in their study LOS depended on multiple factors apart from clinical criteria such as patient economic status, ability to pay for antibiotics, and variable aspects of hospital administration.30 The type of early mobility prescription differed between the included studies, which may also influence the findings for LOS. A reduced LOS is a positive outcome: a difference of 24 hours of hospitalization can potentially save the health care system between $2,273 and $2,373 (US) for people with community-acquired pneumonia.31 In addition to this economic benefit, lower rates of hospitalization can improve patient outcomes because there is a 2% increased risk of infection and 0.5% risk of adverse drug reactions with each additional night a patient spends in hospital.32
Although meta-analysis did not reveal a decrease in mortality with early mobility, investigators noted that it was not associated with increased adverse outcomes.23,29 Multiple factors will influence the rate of mortality from community-acquired pneumonia, including functional status at the time of hospital admission,33 age, and residence status.34 The lack of change in hospital readmission rates and emergency department presentations may be influenced by the level of mobility sustained by participants beyond hospitalization. However, because no studies commented on this point, it is difficult to determine the effect of this factor.
Our review has several limitations. The first is the clinical heterogeneity with respect to the mobility interventions and usual care among the included studies. Across the studies, early mobility was delivered by nurses, suggested to patients by physicians, or provided by physiotherapists.23,28–30 Although each study met the inclusion criteria for early mobility, differing exercise prescriptions and treatment frequencies were applied, and the method of exercise and mobility progression beyond the initial session likely varied among the studies. Only one study commented on the criteria for exercise progression, and this may account for the clinical changes in exercise capacity and quality of life reported.29 Regardless, mobility was only one component of a three-treatment pathway; as such, it was not possible to determine the independent effects of early mobility.29
Second, each study was conducted in a different country, with different usual care, which was poorly defined. Although study outcomes were favourable to early mobility, further study with more rigorous documentation of mobilization procedures and progression is required to confirm these clinical benefits. Despite these limitations, the clinical benefits lend additional support to the recommendations outlined by Bott and colleagues21 for early mobility for individuals with community-acquired pneumonia.
A final limitation of our review was the exclusion of studies not published in English. The three RCTs we included were of moderate to high methodological quality on the basis of PEDro score,13 with the use of randomization procedures and allocation. The lack of blinding for procedures and assessments, however, increases the risk of bias. Future studies of high quality are required to confirm these initial results regarding the clinical benefits of early mobility.
CONCLUSION
This article provides support that early mobility reduces LOS when provided to adults who have been hospitalized with community-acquired pneumonia. Although mortality was not reduced, early mobility was not associated with any detrimental effects and therefore can be considered as an adjunct treatment for pneumonia. Further trials examining early mobility, delivered according to a defined protocol of exercise prescription and progression, are required to determine additional clinical benefits and develop best-practice, evidence-based guidelines.
KEY MESSAGES
What is already known on this topic
Early mobility has demonstrated success as a treatment for various cardiorespiratory conditions, but the research on its effectiveness in treating hospitalized adults with community-acquired pneumonia is limited.
What this study adds
Our systematic review reveals that the evidence for the effectiveness of early mobility as a treatment for patients with pneumonia is limited; this situation warrants further investigation.
APPENDIX: EXAMPLE SEARCH STRATEGY FOR PUBMED
((((rehabilitation) OR (“physical therapy modalities” [MeSH Terms] OR “physical therapy modalities”[All Fields] OR “physiotherapy”[All Fields])) OR (“physical therapy modalities”[MeSH Terms] OR “physical therapy modalities”[All Fields] OR “physical therapy”[All Fields]))) AND (((((((((((hospital) OR “acute care”[All Fields]) OR (“critical care”[MeSH Terms] OR “critical care”[All Fields])) OR icu) OR “intensive care”[MeSH Terms] OR “intensive care”[All Fields]) OR CCU)) AND treatment) AND adult) AND english) AND pneumonia
REFERENCES
- 1.Mandell LA, Wunderink RG, Anzueto A., et al. ; Infections Diseases Society of America, American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–S72. 10.1086/511159. Medline:17278083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nair GB, Niederman MS. Community-acquired pneumonia: an unfinished battle. Med Clin North Am. 2011;95(6):1143–61. 10.1016/j.mcna.2011.08.007. Medline:22032432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mertz D, Johnstone J.. Modern management of community-acquired pneumonia: is it cost-effective and are outcomes acceptable? Curr Infect Dis Rep. 2011;13(3):269–77. 10.1007/s11908-011-0178-8. Medline:21400249 [DOI] [PubMed] [Google Scholar]
- 4.Niederman MS, Luna CM. Community-acquired pneumonia guidelines: a global perspective. Semin Respir Crit Care Med. 2012;33(3):298–310. 10.1055/s-0032-1315642. Medline:22718216 [DOI] [PubMed] [Google Scholar]
- 5.Pfuntner A, Wier LM, Stocks C.. Most frequent conditions in U.S. hospitals, 2011 [Internet]. HCUP statistical brief 162. Rockville (MD): Agency for Healthcare Research and Quality; 2013 [cited 2017 March] Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb162.pdf. [PubMed] [Google Scholar]
- 6.National Center for Health Statistics. Health, United States, 2012: with special features on emergency care. Hyattsville (MD): National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- 7.Pfuntner A, Wier LM, Steiner C.. Costs for hospital stays in the United States, 2011 [Internet]. HCUP statistical brief 168. Rockville (MD): Agency for Healthcare Research and Quality; 2013. [cited 2017 March] Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb168-Hospital-Costs-United-States-2011.pdf. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention [homepage on the Internet]. Atlanta: The Centers; c2017[cited 2015 June 30]. Pneumonia; [about 2 screens] Available from: https://www.cdc.gov/nchs/fastats/pneumonia.htm. [Google Scholar]
- 9.Broulette J, Yu H, Pyenson B, et al. The incidence rate and economic burden of community-acquired pneumonia in a working-age population. Am Health Drug Benefits. 2013;6(8):494–503. Medline:24991378 [PMC free article] [PubMed] [Google Scholar]
- 10.Lee J, Giesler D, Gellad W, Fine M.. Antibiotic therapy for adults hospitalised with community-acquired pneumonia: a systematic review. JAMA. 2016;315(6):593–602. 10.1001/jama.2016.0115. Medline:26864413 [DOI] [PubMed] [Google Scholar]
- 11.Strickland S, Rubin B, Drescher G, et al. AARC clinical practice guideline: effectiveness of nonpharmacologic airway clearance therapies in hospitalized patients. Respir Care. 2013;58(12):2187–93. 10.4187/respcare.02925. Medline:24222709 [DOI] [PubMed] [Google Scholar]
- 12.Engel H, Needham D, Morris P., et al. ICU early mobilization: from recommendation to implementation at three medical centers. Crit Care Med. 2013;41(9 Suppl 1):S69–S80. 10.1097/CCM.0b013e3182a240d5. Medline:23989097 [DOI] [PubMed] [Google Scholar]
- 13.Tordoff S, DiGiulio F.. Implementing an early mobility program in the ICU. Nurs Crit Care. 2010;5(2):22–4. 10.1097/01.CCN.0000369214.54121.ac. [DOI] [Google Scholar]
- 14.Tusman G, Bohm SH, Warner DO, Sprung J.. Atelectasis and perioperative pulmonary complications in high-risk patients. Curr Opin Anaesthesiol. 2012;25(1):1–10. 10.1097/ACO.0b013e32834dd1eb. Medline:22113182 [DOI] [PubMed] [Google Scholar]
- 15.Mackay M, Ellis E, Johnston C.. Randomised clinical trial of physiotherapy after open abdominal surgery in high risk patients. Aust J Physiotherapy. 2005;51(3):151–9. 10.1016/S0004-9514(05)70021-0. Medline:16137240 [DOI] [PubMed] [Google Scholar]
- 16.Silva Y, Li S, Rickard M.. Does the additional of deep breathing exercise to physiotherapy directed early mobilisation alter patient outcomes following high-risk open upper abdominal surgery? Cluster randomised controlled trial. Physiotherapy. 2013;99(3):187–93. 10.1016/j.physio.2012.09.006. Medline:23206316 [DOI] [PubMed] [Google Scholar]
- 17.Yang M, Yan Y, Yin X, et al. Chest physiotherapy for pneumonia in adults. Cochrane Database Syst Rev. 2013;(2):CD006338 10.1002/14651858.CD006338.pub3. Medline:23450568 [DOI] [PubMed] [Google Scholar]
- 18.Gosselink R, Bott J, Johnson M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med. 2008;34(7):1188–99. 10.1007/s00134-008-1026-7. Medline:18283429 [DOI] [PubMed] [Google Scholar]
- 19.Korupolu R, Gifford JM, Needham DM. Early mobilization of critically ill patients: reducing neuromuscular complications after intensive care. Contemp Crit Care. 2009;6(9):1–12. [Google Scholar]
- 20.Davidson JE, Harvey MA, Bemis-Dougherty A, Smith JM, Hopkins RO. Implementation of the Pain, Agitation, and Delirium Practice Guidelines and promoting patient mobility to prevent post-intensive care syndrome. Crit Care Med. 2013;41(9 Suppl 1):S136–S145. 10.1097/CCM.0b013e3182a24105. Medline:23989091 [DOI] [PubMed] [Google Scholar]
- 21.Bott J, Blumenthal S, Buxton M, et al. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. Thorax. 2009;64(Suppl 1):i1–i52. 10.1136/thx.2008.110726. Medline:19406863 [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, et al. ; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Int J Surg. 2010;8(5):336–41. 10.1371/journal.pmed.1000097. Medline:20171303 [DOI] [PubMed] [Google Scholar]
- 23.Mundy LM, Leet TL, Darst K, et al. Early mobilization of patients hospitalized with community-acquired pneumonia. Chest. 2003;124(3):883–9. 10.1378/chest.124.3.883. Medline:12970012 [DOI] [PubMed] [Google Scholar]
- 24.PEDro: Physiotherapy Evidence Database [homepage on the Internet]. Camperdown, NSW, Australia: University of Sydney; c2018 [cited 2015 June 30] Available from: http://www.pedro.org.au/english/downloads/pedro-scale/. [Google Scholar]
- 25.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses [Internet]. 2018. [cited 2009 Oct 19] Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm.
- 26.Cochrane Consumers and Communication Review Group. Data Extraction Template for Cochrane Reviews: meta-analysis; 2013. [cited 2015 Nov 24] Available from: https://handbook-5-1.cochrane.org/.
- 27.Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions [Internet]. Version 5.1.0. London: Cochrane Collaboration; 2011. [cited 2018 Nov 15] Available from: https://training.cochrane.org/handbook. [Google Scholar]
- 28.Jose A, Dal Corso S.. Inpatient rehabilitation improves functional capacity, peripheral muscle strength and quality of life in patients with community-acquired pneumonia: a randomised trial. J Physiotherapy. 2016;62(2):96–102. 10.1016/j.jphys.2016.02.014. Medline:26996093 [DOI] [PubMed] [Google Scholar]
- 29.Carratala J, Garcia-Vidal C, Ortega L, et al. Effect of a 3-step critical pathway to reduce duration of intravenous antibiotic therapy and length of stay in community-acquired pneumonia: a randomized controlled trial. Arch Intern Med. 2012;172(12):922–8. 10.1001/archinternmed.2012.1690. Medline:22732747 [DOI] [PubMed] [Google Scholar]
- 30.Momosaki R, Yasunaga H, Matsui H, et al. Effect of early rehabilitation by physical therapists on in-hospital mortality after aspiration pneumonia in the elderly. Arch Phys Med Rehabil. 2015;96(2):205–9. 10.1016/j.apmr.2014.09.014. Medline:25301440 [DOI] [PubMed] [Google Scholar]
- 31.Kozma CM, Dickson M, Raut MK, et al. Economic benefit of a 1-day reduction in hospital stay for community-acquired pneumonia (CAP). J Med Econ. 2010;13(4):719–27. 10.3111/13696998.2010.536350. Medline: 21091099 [DOI] [PubMed] [Google Scholar]
- 32.Hauck K, Zhao X.. How dangerous is a day in hospital? A model of adverse events and length of stay for medical inpatients. Med Care. 2011;49(12):1068–75. 10.1097/MLR.0b013e31822efb09. Medline:21945976 [DOI] [PubMed] [Google Scholar]
- 33.Marrie T, Wu L.. Factors influencing in-hospital mortality in community-acquired pneumonia: a prospective study of patients not initially admitted to the ICU. Chest. 2005;127(4):1260–70. 10.1016/S0012-3692(15)34475-5. Medline:15821203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kothe H, Bauer T, Marre R, et al. ; The Competence Network for Community-Acquired Pneumonia Study Group. Outcome of community-acquired pneumonia: influence of age, residence status and antimicrobial treatment. Eur Respir J. 2008;32(1):139–46. 10.1183/09031936.00092507. Medline:18287129 [DOI] [PubMed] [Google Scholar]


