Abstract
A 31‐year‐old female with 10 years indwelled Hickman catheter for idiopathic pulmonary hypertension presented infectious findings. We decided to remove it but simple traction did not work. Although it was an off labeled use, we could remove it using a laser sheath and snare technique without any complication.
Keywords: adhesions, central venous catheter, Hickman catheter, laser, removal
1. INTRODUCTION
Long‐term central venous catheters (CVCs) have been widely used for the intravenous administration of chemotherapy and other medications. Hickman catheter (Bard, Convington, GA, USA) is one of the commonly used catheters in the clinical setting. One of the complications of long‐term CVC placement is infection.1 In some cases, long‐term indwelling can cause CVCs to heavily adhere to the veins, disabling their removal with a simple traction.
Laser sheaths are used for the removal of chronically implanted pacing and defibrillation leads. Removal of foreign bodies is the principle of treatment of infection in such cases with infected pacemakers and implantable cardioverter defibrillators (ICDs), which comprises a class I indication for lead extraction.2
2. CASE REPORT
A 31‐year‐old woman with idiopathic pulmonary hypertension—who had been treated with continuous infusion of epoprostenol for 10 years through a Hickman catheter that was inserted in her left subclavian vein ahead of the superior vena cava (SVC) and tunneled in her left chest wall—was admitted to our hospital with symptoms of swelling and redness of the skin surrounding the subcutaneous catheter. We diagnosed her with a catheter infection and thus, it was decided to remove the Hickman catheter. We got an informed consent from the patients and also got the permission from the nonapproved indication committee in our hospital.
Initially, a cut down procedure and simple traction was attempted by the surgeon. However, it was unsuccessful due to heavy adhesions in the left subclavian vein. A culture performed at that time revealed methicillin‐sensitive staphylococcus aureus. Venography of the left subclavian vein of the patient was performed for more information, which revealed a total occlusion at the proximal side, with the Hickman catheter buried in the tissue. Therefore, we attempted an extraction using a laser sheath, which is originally indicated for the extraction of chronically implanted pacing leads.
The procedure was performed in an operating room under general anesthesia with full back‐up of surgeons for an emergency. A 12‐French (F) excimer laser sheath SLS II (Spectranetics, Colorado Springs, CO, USA) was selected to use. To create a substantial system, we placed a 4‐F catheter over a 0.035 inch guidewire inside the Hickman catheter. Afterward, the femoral vein was punctured to insert a GooseNeck snare (Coviden, Plymouth, MN, USA), which was passed through the femoral vein and inferior vena cava toward the SVC where the distal end of the catheter was floating. The GooseNeck snare was manipulated to grab and tighten the distal end of the system, which included the Hickman catheter, 4‐F catheter, and the guidewire, and was pulled downward to maintain certain tension on the catheter without stretching it. The proximal end of the catheter system outside the vein was tightly tied using a thread. Subsequently, the laser sheath was advanced over the catheter system, which successfully overcame all the adhesions between the Hickman catheter and the veins. We found that laser was applied all the way along the left subclavian vein to the innominate vein. The snare was released afterward and the whole catheter system was removed from the vein without complication (Figure 1). We could remove the whole system. The patient continued receiving antibiotics and was placed on a new CVC on the contralateral side 3 weeks afterward.
Figure 1.
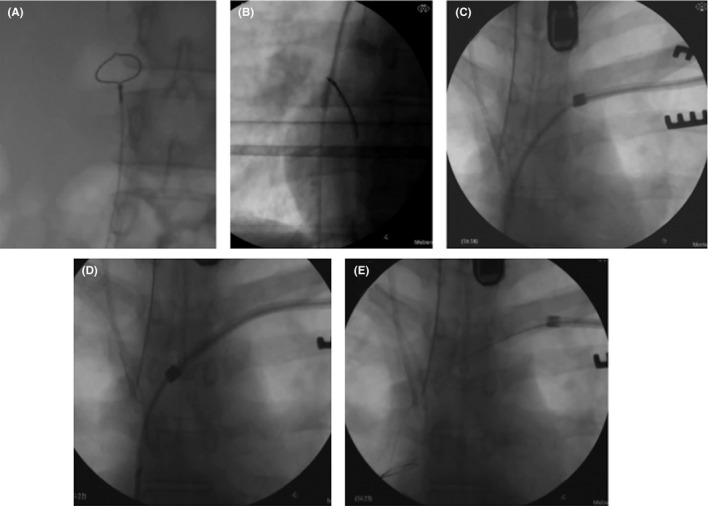
Fluoroscopy images showing the Hickman removal. ➀ A GooseNeck snare passing through the femoral vein and inferior vena cava and approaching the superior vena cava where the distal end of the catheter is floating. ② The GooseNeck snare is manipulated to grab and tighten the distal end of the system and is pulled downward in order to maintain certain tension on the catheter without stretching it. ③,④ The laser sheath is advanced over the catheter system, successfully overcoming all the adhesions between the Hickman catheter and the veins. ⑤ The snare is released and the whole catheter system is removed from the vein
3. DISCUSSION
Infection of a foreign material can cause serious problems. However, in some cases, due to long‐term indwelling in the veins, CVCs can heavily adhere to the veins, disabling their removal with simple traction. A similar case was reported with a hemodialysis catheter.3
Although laser sheaths have high success and low complication rates when used for the removal of long‐term indwelling pacing leads, “tear of the SVC” is a significant complication that can be fatal, with a reported mortality rate of 0.3%.4 In this case, venography revealed total occlusion of the subclavian vein and the catheter seemed to be buried in the tissue, suggesting heavy adhesions between the catheter and the left subclavian vein or the innominate vein. Although the application of a laser sheath for the removal of CVCs is off‐label, it was utilized in this case since the thoracotomy to remove the infected Hickman catheter seemed to be high risk. Following the explanation of the treatment options to the patient, she decided on laser extraction.
Laser extraction requires adequate tension on the catheter during the procedure in order to stabilize the advancing laser sheath. Pacemaker leads are substantial, especially those with locking stylets inside that allow the application of a constant force while the leads are pulled to advance the laser sheath. Unlike pacemaker leads, Hickman catheters are elastic and therefore tend to stretch more when pulled out during extraction, which can create a significant gap between the inner lumen of the laser sheath and the catheter that can subsequently injure the vein. Hence, it was critical in this case to minimize the elasticity of the Hickman catheter in order to facilitate the lead extraction. Accordingly, we inserted a 4‐F catheter and a guidewire into the Hickman catheter to create a substantial system. Afterward, we fixed both ends. It is also essential to maintain a coaxial alignment of the sheath over the CVC to maximize the removal of fibrotic adhesions and minimize trauma to vascular structure and CVC itself.5 The distal end was approached from the femoral vein and grabbed using a GooseNeck snare, while the proximal end was firmly tied using a thread (Figure 2). The femoral approach and snare technique were reportedly used during lead extraction procedures.6 During the procedure, the operator maintained traction on the catheter and it was removed without any complication.
Figure 2.
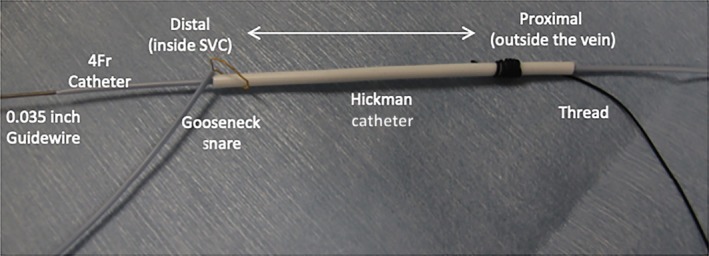
Image showing the set‐up of the Hickman catheter system. A 4‐F catheter and a 0.035‐inch guidewire were placed inside the Hickman catheter to create a substantial system. Both ends of the catheter were fixed; the distal end via a GooseNeck snare and the proximal end using a thread. This system was developed to minimize the elasticity of the Hickman catheter
4. CONCLUSION
Laser sheaths may be utilized for the removal of chronically indwelled CVCs that are heavily adhered to veins. Minimizing the elasticity of catheters during extraction may be essential to avoid complications.
CONFLICT OF INTERESTS
Authors declare no conflict of interests for this article.
Le KV, Okamura H, Homma T, Ohgo T, Noda T, Kusano K. Removal of a Hickman catheter using a laser sheath. J Arrhythmia. 2019;35:158–160. 10.1002/joa3.12147
REFERENCES
- 1. Grover JK, Uppal G, Guleria R, Vats V, Raina V. Acinetobacter infection in Hickman's catheterized patient of multiple myeloma. J Assoc Physicians India. 2003;51:1026–7. [PubMed] [Google Scholar]
- 2. Kusumoto FM, Schoenfeld MH, Wilkoff BL, et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm. 2017;14:e503–51. [DOI] [PubMed] [Google Scholar]
- 3. Carrillo RG, Garisto JD, Salman L, Merrill D, Asif A. A novel technique for tethered dialysis catheter removal using the laser sheath. Semin Dial. 2009;22:688–91. [DOI] [PubMed] [Google Scholar]
- 4. Wazni O, Epstein LM, Carrillo RG, et al. Lead extraction in the contemporary setting: the LExICon study: an observational retrospective study of consecutive laser lead extractions. J Am Coll Cardiol. 2010;55:579–86. [DOI] [PubMed] [Google Scholar]
- 5. Madhavan M, Swale MJ, Gard JJ, Hayes DL, Asirvatham SJ. Contemporary pacemaker and ICD lead management: techniques for lead extraction. Expert Rev Cardiovasc Ther. 2012;10:875–7. [DOI] [PubMed] [Google Scholar]
- 6. Bongiorni MG, Soldati E, Zucchelli G, et al. Transvenous removal of pacing and implantable cardiac defibrillating leads using single sheath mechanical dilatation and multiple venous approaches: high success rate and safety in more than 2000 leads. Eur Heart J. 2008;29:2886–93. [DOI] [PMC free article] [PubMed] [Google Scholar]


