Abstract
We evaluated the evolving structure of radiation oncology in Japan in terms of equipment, personnel, patient load, and geographic distribution to identify and overcome any existing limitations. From March 2011 to June 2013, the Japanese Society for Radiation Oncology conducted a questionnaire based on the Japanese national structure survey of radiation oncology in 2010. Data were analyzed based on the institutional stratification by the annual number of new patients treated with radiotherapy per institution. The estimated annual numbers of new and total (new plus repeat) patients treated with radiation were 211 000 and 251 000, respectively. Additionally, the estimated cancer incidence was 805 236 cases, with ~26.2% of all newly diagnosed patients being treated with radiation. The types and numbers of treatment devices actually used included linear accelerator (LINAC; n = 829), telecobalt (n = 9), Gamma Knife (n = 46), 60Co remote afterloading system (RALS; n = 28), and 192Ir RALS (n = 131). The LINAC system used dual-energy functions in 586 units, three-dimensional conformal radiotherapy functions in 663, and intensity-modulated radiotherapy (IMRT) functions in 337. There were 564 JASTRO-certified radiation oncologists, 959.2 full-time equivalent (FTE) radiation oncologists, 1841.3 FTE radiotherapy technologists, 131.3 FTE medical physicists, 121.5 FTE radiotherapy quality managers, and 649.6 FTE nurses. The frequency of IMRT use significantly increased during this year. To conclude, although there was a shortage of personnel in 2010, the Japanese structure of radiation oncology has clearly improved in terms of equipment and utility.
Keywords: structure survey, radiotherapy institution, radiotherapy personnel, radiotherapy equipment
PREFACE
We greatly appreciate the substantial contributions of the many radiation oncologists (ROs), radiation technologists, and other staff to the national structure survey of radiation oncology. Despite some delays, the updated Japanese national structure survey data for radiation oncology in 2010 is now available.
Since 1991, the Japanese Society for Radiation Oncology (JASTRO) has conducted national structure surveys every 2 years [1–24]. From March 2011 to June 2013, the Japanese Society for Radiation Oncology conducted a questionnaire based on the Japanese national structure survey of radiation oncology in 2010, which included the number of treatment systems by type, number of personnel by category, and number of patients by type, site, and treatment modality. To measure variables over a longer time period, data for the year 2010 were also considered. In total, 705 of 780 active institutions attempted the survey; the response rate was 90.4%.
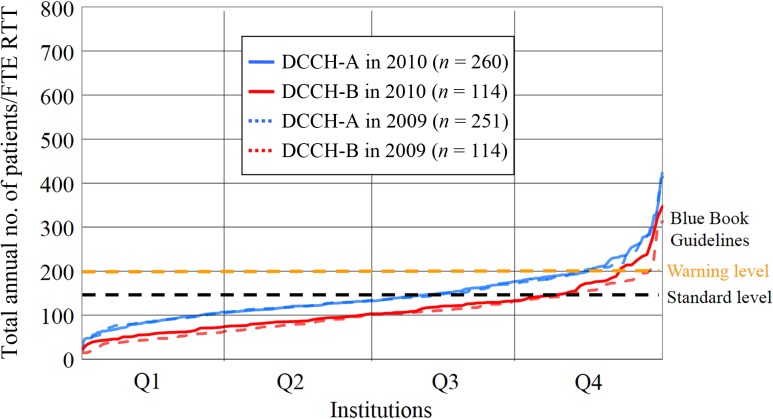
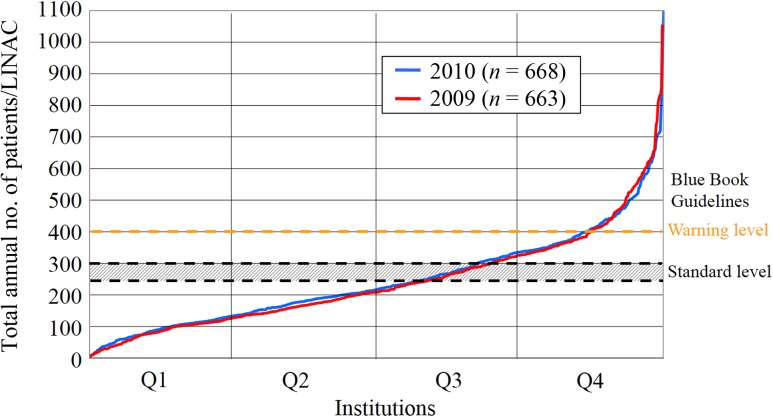
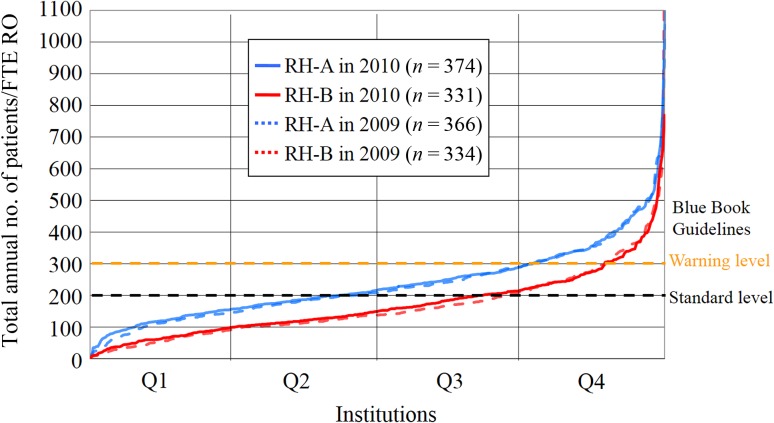
The current report analyzes these institutional structure data (equipment, personnel, patient load, and geographic distribution) based on institutional stratification according to the annual number of new patients treated with radiotherapy at each institution. The clinical working hours of each staff member performing radiotherapy were derived from full-time equivalent (FTE; 40 h per week for radiation oncology work only) data. The Japanese Blue Book Guidelines (JBBG) [25, 26] were used for comparison with the results of this study. These guidelines pertain to the structure of radiation oncology in Japan based on the Patterns of Care Study (PCS) [27, 28] data. The standard guidelines were set at 250–300 (warning level, 400) for annual patient load per external beam machine, at 200 (warning level, 300) for annual patient load per FTE RO, and at 120 (warning level, 200) for annual patient load per FTE radiotherapy technologist. Furthermore, we analyzed data from the designated cancer care hospitals accredited by the Ministry of Health, Labor, and Welfare. As at 1 August 2013, Japan had 397 designated cancer care hospitals [29]. Twenty-three institutions did not return the survey; therefore, the structure data for 374 designated cancer care hospitals were analyzed and compared with the data for all radiotherapy hospitals. The analysis was conducted in two groups: institutions with <1.0 FTE RO and those with ≥1.0 FTE RO.
Here, preliminary results have been presented as tables and figures (Tables 1–18 and Figs 1–6). We have briefly summarized the Japanese national structure survey of radiation oncology for 2010. In total, 780 radiotherapy institutions were surveyed, and the estimated number of new patients was ~211 000; the estimated total number of patients (new plus repeat) was 251 000. In 2010, based on Japanese cancer registries, the cancer incidence was estimated at 805 236 cases [30], with ~26.2% (211 000 of 805 236) of all newly diagnosed patients being treated with radiation. Overall, 829 linear accelerators (LINACs), 9 telecobalt units, 46 Gamma Knife, 28 60Co remote afterloading systems (RALS) and 131 192Ir RALS were actually used. The LINAC system used dual-energy functions in 586 units, three-dimensional conformal radiotherapy functions in 663, and intensity-modulated radiotherapy (IMRT) functions in 337. There were 564 JASTRO-certified ROs, 959.2 FTE ROs, 1841.3 FTE radiotherapy technologists, 131.3 FTE medical physicists, 121.5 FTE radiotherapy quality managers, and 649.6 FTE nurses. Approximately 50.0% of all radiotherapy institutions had >200 new radiotherapy patients per year, whereas 31.6% of the institutions had >300. Additionally, 47.5% of all radiotherapy institutions had <1.0 FTE ROs. We expect that this updated national structure survey of radiation oncology for 2010 will aid the continuous improvement of all aspects of radiation oncology in Japan.
Table 1.
Categories of radiotherapy institution
| Institution category | |
|---|---|
| U: | university hospital |
| G: | cancer center (including national cancer center) |
| N: | national hospital organization (excluding national cancer center) |
| P: | public hospital (excluding national cancer center), red cross hospital, saiseikai hospital, company hospital, public corporation hospital, national health insurance hospital |
| O: | social insurance hospital, mutual insurance hospital, industrial accident hospital, association hospital, Japan agricultural cooperatives hospital |
| H: | medical corporation hospital, medical association hospital, private hospital, other hospitals |
Table 2.
Number of radiotherapy institutions by scale classification and institution category
| Scale category (annual number of new patients) | Institution category | Total | Institution ratio [%] | |||||
|---|---|---|---|---|---|---|---|---|
| U | G | N | P | O | H | |||
| A (1–99) | 5 | 2 | 14 | 44 | 35 | 23 | 123 | 17.6 |
| B (100–199) | 11 | 1 | 27 | 80 | 70 | 38 | 227 | 32.4 |
| C (200–299) | 14 | 3 | 12 | 41 | 36 | 23 | 129 | 18.4 |
| D (300–399) | 14 | 5 | 7 | 20 | 25 | 15 | 86 | 12.3 |
| E (400–499) | 16 | 1 | 1 | 10 | 8 | 9 | 45 | 6.4 |
| F (500–) | 51 | 17 | 2 | 7 | 5 | 13 | 95 | 13.6 |
| Total | 111 | 29 | 63 | 202 | 179 | 121 | 705 | 100.0 |
| Institution ratio [%] | 15.7 | 4.1 | 8.9 | 28.7 | 25.4 | 17.2 | 100.0 | |
Table 3.
Annual number of new patients by scale classification and institution category
| Scale category (number of institutions) | Institution category (number of institutions) | Total (705) | Average | |||||
|---|---|---|---|---|---|---|---|---|
| U (111) | G (29) | N (63) | P (202) | O (179) | H (121) | |||
| A (123) | 162 | 101 | 750 | 2677 | 2498 | 1475 | 7663 | 62.3 |
| B (227) | 1573 | 106 | 4138 | 12 067 | 10 050 | 5693 | 33 627 | 148.1 |
| C (129) | 3601 | 831 | 2734 | 10 009 | 8679 | 5527 | 31 381 | 243.3 |
| D (86) | 4774 | 1656 | 2318 | 6700 | 8521 | 5012 | 28 981 | 337.0 |
| E (45) | 7134 | 476 | 433 | 4266 | 3377 | 4114 | 19 800 | 440.0 |
| F (95) | 36 908 | 14 665 | 1290 | 4054 | 3245 | 8708 | 68 870 | 724.9 |
| Total (705) | 54 152 | 17 835 | 11 663 | 39 773 | 36 370 | 30 529 | 190 322 | 270.0 |
| Average | 492.3 | 615.0 | 185.1 | 196.9 | 203.2 | 252.3 | 270.0 | |
Table 4.
Annual number of total (new plus repeat) patients by scale classification and institution category
| Scale category (number of institutions) | Institution category (number of institutions) | Total (705) | Average | |||||
|---|---|---|---|---|---|---|---|---|
| U (111) | G (29) | N (63) | P (202) | O (179) | H (121) | |||
| A (123) | 178 | 110 | 949 | 3042 | 2871 | 1747 | 8897 | 72.3 |
| B (227) | 1713 | 147 | 4809 | 13 784 | 11 366 | 7188 | 39 007 | 171.8 |
| C (129) | 4288 | 1096 | 3111 | 12 118 | 9991 | 6408 | 37 012 | 286.9 |
| D (86) | 5496 | 2050 | 2588 | 7853 | 10 327 | 6443 | 34 757 | 404.2 |
| E (45) | 8498 | 583 | 490 | 5188 | 4214 | 5293 | 24 266 | 539.2 |
| F (95) | 44 624 | 17 686 | 1678 | 4653 | 3609 | 10 662 | 82 912 | 872.8 |
| Total (705) | 64 797 | 21 672 | 13 625 | 46 638 | 42 378 | 37 741 | 226 851 | 321.8 |
| Average | 583.8 | 747.3 | 216.3 | 230.9 | 236.7 | 311.9 | 321.8 | |
Table 5.
Number of treatment devices and their functions by scale classification
| Treatment devices and their functions | Scale category (number of institutions) | Total (705) | |||||
|---|---|---|---|---|---|---|---|
| A (123) | B (227) | C (129) | D (86) | E (45) | F (95) | ||
| LINAC | 117 | 213 | 132 | 101 | 69 | 197 | 829 |
| with dual-energy function | 63 | 149 | 105 | 83 | 54 | 152 | 606 |
| with 3DCRT function (MLC width ≤1.0 cm) | 83 | 167 | 109 | 93 | 65 | 184 | 701 |
| with IMRT function | 17 | 51 | 54 | 66 | 40 | 147 | 375 |
| with cone-beam CT or CT on rail | 15 | 42 | 37 | 41 | 33 | 71 | 239 |
| with treatment position verification system (X-ray perspective image) | 14 | 42 | 44 | 39 | 33 | 74 | 246 |
| with treatment position verification system (other than those above) | 19 | 49 | 30 | 31 | 17 | 68 | 214 |
| Annual no. patients/LINAC | 76.0 | 183.1 | 280.4 | 344.1 | 351.7 | 420.9 | 273.6 |
| CyberKnife® | 3 | 5 | 1 | 2 | 2 | 4 | 17 |
| Novalis® | 1 | 2 | 4 | 5 | 4 | 9 | 25 |
| Tomotherapy® | 3 | 2 | 1 | 4 | 2 | 3 | 15 |
| Particle | 0 | 0 | 0 | 0 | 0 | 7 | 7 |
| Microtoron | 0 | 5 | 1 | 0 | 2 | 5 | 13 |
| Telecobalt (actual use) | 3 (3) | 4 (3) | 1 (0) | 2 (1) | 0 (0) | 2 (2) | 12 (9) |
| Gamma knife® | 3 | 11 | 10 | 7 | 6 | 9 | 46 |
| Other accelerator | 0 | 0 | 3 | 1 | 0 | 3 | 7 |
| Other external irradiation device | 0 | 1 | 2 | 0 | 0 | 4 | 7 |
| New type 60Co RALS (in actual use) | 0 (0) | 3 (3) | 4 (3) | 3 (3) | 2 (2) | 6 (6) | 18 (17) |
| Old type 60Co RALS (in actual use) | 2 (0) | 7 (2) | 4 (3) | 4 (3) | 3 (2) | 1 (1) | 19 (11) |
| 192Ir RALS (in actual use) | 0 (1) | 8 (6) | 21 (18) | 20 (20) | 17 (17) | 70 (70) | 136 (131) |
| 137Cs RALS (in actual use) | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 0 (0) | 1 (1) |
Table 6.
Numbers of treatment-planning equipment and accessories by scale classification
| Treatment-planning equipment and accessories | Scale category (number of institutions) | Total (705) | |||||
|---|---|---|---|---|---|---|---|
| A (123) | B (227) | C (129) | D (86) | E (45) | F (95) | ||
| X-ray simulator | 58 | 105 | 54 | 40 | 21 | 70 | 348 |
| CT simulator | 91 | 189 | 117 | 86 | 46 | 104 | 633 |
| RTP computer (2 or more) | 128 (13) | 262 (34) | 192 (38) | 192 (46) | 144 (29) | 463 (86) | 1 381 (246) |
| X-ray CT (2 or more) | 219 (79) | 491 (172) | 357 (113) | 275 (80) | 172 (44) | 456 (89) | 1 970 (577) |
| for RT only | 40 | 105 | 84 | 66 | 35 | 95 | 425 |
| MRI (2 or more) | 153 (34) | 321 (89) | 227 (87) | 173 (69) | 107 (41) | 271 (80) | 1 252 (400) |
| for RT only | 1 | 2 | 6 | 3 | 1 | 3 | 16 |
| Computer use for RT recording | 96 | 186 | 109 | 76 | 40 | 86 | 593 |
| Water phantom (2 or more) | 119 (17) | 236 (41) | 165 (41) | 111 (29) | 65 (17) | 174 (44) | 870 (189) |
| Film densitometer (2 or more) | 38 (1) | 89 (1) | 63 (2) | 63 (4) | 34 (2) | 98 (14) | 385 (24) |
| Dosimeter (3 or more) | 311 (56) | 690 (130) | 482 (80) | 358 (59) | 203 (33) | 564 (78) | 2 608 (436) |
The numbers in parentheses indicate the number of institutions. CT = computed tomography, RTP = radiotherapy planning, MRI = magnetic resonance imaging, RT = radiotherapy.
Table 7.
Numbers of personnel and annual patients by scale classification
| Scale category (number of institutions) | Total (705) | ||||||
|---|---|---|---|---|---|---|---|
| A (123) | B (227) | C (129) | D (86) | E (45) | F (95) | ||
| Scale (annual no. of new patients) | ≤99 | 100–199 | 200–299 | 300–399 | 400–499 | 500≤ | |
| Institution ratio [%] | 17.4% | 32.2% | 18.3% | 12.2% | 6.4% | 13.5% | 100% |
| New patients | 7663 | 33 627 | 31 381 | 28 981 | 19 800 | 68 870 | 190 322 |
| New patients/institution | 62.3 | 148.1 | 243.3 | 337.0 | 440.0 | 724.9 | 270.0 |
| Total patients | 8897 | 39 007 | 37 012 | 34 757 | 24 266 | 82 912 | 226 851 |
| Total patients/institution | 72.3 | 171.8 | 286.9 | 404.2 | 539.2 | 872.8 | 321.8 |
| Beds | 39 816 | 94 885 | 61 173 | 48 128 | 29 179 | 71 577 | 344 758 |
| Institutions with RT beds (%) | 18 (14.6) | 45 (19.8) | 38 (29.5) | 40 (46.5) | 21 (46.7) | 68 (71.6) | 230 (32.6) |
| RT beds | 85.0 | 183.0 | 204.0 | 259.5 | 191.0 | 982.4 | 1 904.9 |
| RT beds/total beds [%] | 0.2% | 0.2% | 0.3% | 0.5% | 0.7% | 1.4% | 0.6% |
| RT beds/institution | 0.7 | 0.8 | 1.6 | 3.0 | 4.2 | 10.3 | 2.7 |
| RT beds/institution with RT beds | 4.7 | 4.1 | 5.4 | 6.5 | 9.1 | 14.4 | 8.3 |
| JRS-certified institutions (%) | 13 (10.6) | 40 (17.6) | 57 (44.2) | 55 (64) | 36 (80) | 79 (83.2) | 280 (39.7) |
| JRS-cooperation institutions (%) | 28 (22.8) | 94 (41.4) | 33 (25.6) | 21 (24.4) | 8 (17.8) | 10 (10.5) | 194 (27.5) |
| JASTRO-certified institutions (%) | 2 (1.6) | 37 (16.3) | 60 (46.5) | 57 (66.3) | 35 (77.8) | 84 (88.4) | 275 (39) |
| JRS membership (full-time) | 69 | 167 | 139 | 136 | 103 | 441 | 1 055 |
| JRS-certified ROs (full-time) | 57 | 149 | 125 | 122 | 79 | 335 | 867 |
| JASTRO membership (full-time) | 37 | 127 | 131 | 120 | 95 | 440 | 950 |
| JASTRO-certified ROs (full-time) | 13 | 67 | 82 | 82 | 56 | 264 | 564 |
| Institutions with full-time RO (%) | 56 (45.5) | 147 (64.8) | 109 (84.5) | 83 (96.5) | 44 (97.8) | 93 (97.9) | 532 (75.5) |
| ROs (full-time) | 85 | 180 | 150 | 146 | 110 | 452 | 1 123 |
| ROs (full-time)/institution | 0.7 | 0.8 | 1.2 | 1.7 | 2.4 | 4.8 | 1.6 |
| FTE RO (full-time) | 34.3 | 121.1 | 120.6 | 117.5 | 85.7 | 373.0 | 852.1 |
| FTE RO (full-time)/institution | 0.28 | 0.53 | 0.93 | 1.37 | 1.90 | 3.93 | 1.21 |
| ROs (part-time) | 107 | 179 | 93 | 45 | 35 | 120 | 579 |
| ROs (part-time)/institution | 0.87 | 0.79 | 0.72 | 0.52 | 0.78 | 1.26 | 0.82 |
| FTE RO (part-time) | 16.6 | 30.0 | 16.5 | 7.6 | 7.4 | 29.1 | 107.1 |
| FTE RO (part-time)/institution | 0.1 | 0.1 | 0.1 | 0.1 | 0.2 | 0.3 | 0.2 |
| FTE RO (full-time plus parttime) | 50.9 | 151.1 | 137.0 | 125.1 | 93.1 | 402.1 | 959.2 |
| FTE RO (full-time plus part-time)/institution | 0.41 | 0.67 | 1.06 | 1.45 | 2.07 | 4.23 | 1.36 |
| Radiologists (full-time) | 174.9 | 381.5 | 377.4 | 298.0 | 299.0 | 865.0 | 2 395.8 |
| Radiologists (parttime) | 132.7 | 380.4 | 203.7 | 117.2 | 76.0 | 184.0 | 1 094.0 |
| RTTs (full-time)a | 346 | 754 | 479 | 387 | 229 | 703 | 2 898 |
| FTE RTT | 155.7 | 416.8 | 282.5 | 253.9 | 175.2 | 557.2 | 1 841.3 |
| Medical physicists (full-time)a | 22 | 69 | 64 | 54 | 36 | 113 | 358 |
| FTE medical physicist | 6.5 | 21.4 | 21.2 | 21.5 | 12.5 | 48.3 | 131.3 |
| RT quality manager (full-time)a | 29 | 105 | 87 | 62 | 49 | 117 | 449 |
| FTE RT quality manager | 6.7 | 23.5 | 25.8 | 16.3 | 13.5 | 35.8 | 121.5 |
| Dosimetrists (full-time)a | 12 | 17 | 20 | 18 | 14 | 51 | 132 |
| FTE dosimetrist | 2.2 | 3.4 | 4.1 | 3.6 | 2.7 | 9.5 | 25.4 |
| Craftworkers (full-time)a | 35 | 63 | 32 | 26 | 12 | 52 | 220 |
| FTE craftworker | 6.8 | 11.6 | 6.3 | 5.0 | 1.4 | 5.7 | 36.7 |
| Nurses (full-time) | 100 | 282 | 220 | 156 | 125 | 269 | 1 152 |
| FTE nurses | 44.76 | 132.3 | 114.5 | 86.1 | 59.4 | 212.5 | 649.6 |
| Nursing assistants | 5.2 | 11.2 | 6.35 | 9.6 | 12.4 | 20.3 | 65.1 |
| Clerks | 29.85 | 54.3 | 53.55 | 59.4 | 39.5 | 121.75 | 358.4 |
aOverlap is included in the total number of each staff (radiotherapy technologist, medical physicist, and radiotherapy quality manager). RT = radiotherapy, JRS = Japan Radiological Society, RO = radiation oncologist, JASTRO = Japanese Society for Radiation Oncology, FTE = full-time equivalent, RTT = radiotherapy technologist.
Table 8.
Population size and numbers of patients, institutions, and patient load according to prefecture
| Prefecture | Population (×103) | Institutions | New patients | New patients/institution | Total patients | Total patients/institution |
|---|---|---|---|---|---|---|
| Hokkaido | 5 506 | 30 | 9 520 | 317.3 | 12 200 | 406.7 |
| Aomori | 1 373 | 9 | 2 049 | 227.7 | 2 281 | 253.4 |
| Iwate | 1 330 | 8 | 1 684 | 210.5 | 1 868 | 233.5 |
| Miyagi | 2 348 | 11 | 4 123 | 374.8 | 5 758 | 523.5 |
| Akita | 1 086 | 10 | 1 787 | 178.7 | 2 167 | 216.7 |
| Yamagata | 1 169 | 6 | 1 308 | 218.0 | 1 570 | 261.7 |
| Fukushima | 2 029 | 10 | 3 071 | 307.1 | 3 524 | 352.4 |
| Ibaraki | 2 970 | 15 | 3 638 | 242.5 | 4 444 | 296.3 |
| Tochigi | 2 008 | 8 | 2 751 | 343.9 | 3 534 | 441.8 |
| Gunma | 2 008 | 13 | 3 769 | 289.9 | 4 271 | 328.5 |
| Saitama | 7 195 | 20 | 7 070 | 353.5 | 8 990 | 449.5 |
| Chiba | 6 216 | 23 | 7 398 | 321.7 | 9 034 | 392.8 |
| Tokyo | 13 159 | 67 | 23 116 | 345.0 | 27 951 | 417.2 |
| Kanagawa | 9 048 | 39 | 12 597 | 323.0 | 14 331 | 367.5 |
| Niigata | 2 374 | 15 | 3 930 | 262.0 | 4 410 | 294.0 |
| Toyama | 1 093 | 8 | 1 542 | 192.8 | 1 761 | 220.1 |
| Ishikawa | 1 170 | 7 | 1 994 | 284.9 | 2 386 | 340.9 |
| Fukui | 806 | 6 | 1 250 | 208.3 | 1 487 | 247.8 |
| Yamanashi | 863 | 4 | 1 140 | 285.0 | 1 338 | 334.5 |
| Nagano | 2 152 | 15 | 3 331 | 222.1 | 3 940 | 262.7 |
| Gifu | 2 081 | 12 | 3 245 | 270.4 | 4 244 | 353.7 |
| Shizuoka | 3 765 | 23 | 6 019 | 261.7 | 7 569 | 329.1 |
| Aichi | 7 411 | 37 | 10 113 | 273.3 | 12 088 | 326.7 |
| Mie | 1 855 | 12 | 1 853 | 154.4 | 2 116 | 176.3 |
| Shiga | 1 411 | 10 | 1 832 | 183.2 | 2 238 | 223.8 |
| Kyoto | 2 636 | 13 | 4 032 | 310.2 | 4 710 | 362.3 |
| Osaka | 8 865 | 51 | 13 528 | 265.3 | 15 835 | 310.5 |
| Hyogo | 5 588 | 32 | 8 096 | 253.0 | 9 294 | 290.4 |
| Nara | 1 401 | 8 | 2 200 | 275.0 | 2 499 | 312.4 |
| Wakayama | 1 002 | 10 | 1 717 | 171.7 | 2 063 | 206.3 |
| Tottori | 589 | 7 | 968 | 138.3 | 1 149 | 164.1 |
| Shimane | 717 | 5 | 986 | 197.2 | 1 099 | 219.8 |
| Okayama | 1 945 | 11 | 2 772 | 252.0 | 3 271 | 297.4 |
| Hiroshima | 2 861 | 20 | 5 128 | 256.4 | 6 220 | 311.0 |
| Yamaguchi | 1 451 | 14 | 1 991 | 142.2 | 2 247 | 160.5 |
| Tokushima | 785 | 5 | 1 436 | 287.2 | 1 664 | 332.8 |
| Kagawa | 996 | 6 | 1 194 | 199.0 | 1 266 | 211.0 |
| Ehime | 1 431 | 11 | 2 277 | 207.0 | 2 631 | 239.2 |
| Kochi | 764 | 6 | 1 220 | 203.3 | 1 379 | 229.8 |
| Fukuoka | 5 072 | 26 | 8 585 | 330.2 | 9 903 | 380.9 |
| Saga | 850 | 4 | 901 | 225.3 | 1 017 | 254.3 |
| Nagasaki | 1 427 | 8 | 2 343 | 292.9 | 2 726 | 340.8 |
| Kumamoto | 1 817 | 13 | 3 209 | 246.8 | 3 717 | 285.9 |
| Oita | 1 197 | 11 | 1 616 | 146.9 | 1 913 | 173.9 |
| Miyazaki | 1 135 | 7 | 1 520 | 217.1 | 1 832 | 261.7 |
| Kagoshima | 1 706 | 12 | 2 671 | 222.6 | 2 888 | 240.7 |
| Okinawa | 1 393 | 7 | 1 802 | 257.4 | 2 028 | 289.7 |
| Total | 128 057 | 705 | 190 322 | 270.0 | 226 851 | 321.8 |
Table 9.
Population size and numbers of patients, radiation oncologists, and patient load according to prefecture
| Prefecture | Population (×103) | Total patients | JASTRO-certified RO | FTE RO | Total patients/FTE RO |
|---|---|---|---|---|---|
| Hokkaido | 5 506 | 12 200 | 32 | 51.1 | 238.7 |
| Aomori | 1 373 | 2 281 | 7 | 9.0 | 253.4 |
| Iwate | 1 330 | 1 868 | 5 | 8.0 | 233.5 |
| Miyagi | 2 348 | 5 758 | 11 | 17.9 | 321.7 |
| Akita | 1 086 | 2 167 | 2 | 8.4 | 258.0 |
| Yamagata | 1 169 | 1 570 | 5 | 8.6 | 182.6 |
| Fukushima | 2 029 | 3 524 | 5 | 14.8 | 238.1 |
| Ibaraki | 2 970 | 4 444 | 8 | 15.1 | 294.3 |
| Tochigi | 2 008 | 3 534 | 8 | 14.8 | 238.8 |
| Gunma | 2 008 | 4 271 | 21 | 29.9 | 142.8 |
| Saitama | 7 195 | 8 990 | 18 | 27.0 | 333.0 |
| Chiba | 6 216 | 9 034 | 29 | 48.6 | 185.8 |
| Tokyo | 13 159 | 27 951 | 76 | 119.0 | 235.0 |
| Kanagawa | 9 048 | 14 331 | 35 | 53.0 | 270.4 |
| Niigata | 2 374 | 4 410 | 8 | 16.6 | 265.7 |
| Toyama | 1 093 | 1 761 | 5 | 7.0 | 251.6 |
| Ishikawa | 1 170 | 2 386 | 4 | 6.7 | 356.1 |
| Fukui | 806 | 1 487 | 5 | 8.2 | 181.3 |
| Yamanashi | 863 | 1 338 | 6 | 7.3 | 183.3 |
| Nagano | 2 152 | 3 940 | 6 | 11.2 | 353.4 |
| Gifu | 2 081 | 4 244 | 5 | 9.1 | 466.4 |
| Shizuoka | 3 765 | 7 569 | 18 | 26.4 | 286.7 |
| Aichi | 7 411 | 12 088 | 21 | 49.8 | 242.7 |
| Mie | 1 855 | 2 116 | 4 | 9.8 | 215.9 |
| Shiga | 1 411 | 2 238 | 7 | 11.0 | 203.5 |
| Kyoto | 2 636 | 4 710 | 18 | 26.3 | 179.1 |
| Osaka | 8 865 | 15 835 | 44 | 77.2 | 205.2 |
| Hyogo | 5 588 | 9 294 | 27 | 43.7 | 212.9 |
| Nara | 1 401 | 2 499 | 8 | 12.4 | 201.5 |
| Wakayama | 1 002 | 2 063 | 4 | 10.0 | 206.3 |
| Tottori | 589 | 1 149 | 1 | 4.3 | 267.2 |
| Shimane | 717 | 1 099 | 6 | 8.3 | 132.4 |
| Okayama | 1 945 | 3 271 | 8 | 17.9 | 182.7 |
| Hiroshima | 2 861 | 6 220 | 21 | 26.2 | 237.9 |
| Yamaguchi | 1 451 | 2 247 | 4 | 10.8 | 208.1 |
| Tokushima | 785 | 1 664 | 4 | 8.2 | 202.9 |
| Kagawa | 996 | 1 266 | 3 | 6.5 | 194.8 |
| Ehime | 1 431 | 2 631 | 8 | 13.3 | 197.8 |
| Kochi | 764 | 1 379 | 4 | 3.9 | 353.6 |
| Fukuoka | 5 072 | 9 903 | 24 | 41.8 | 236.9 |
| Saga | 850 | 1 017 | 3 | 4.8 | 211.9 |
| Nagasaki | 1 427 | 2 726 | 4 | 8.1 | 336.5 |
| Kumamoto | 1 817 | 3 717 | 5 | 15.4 | 241.4 |
| Oita | 1 197 | 1 913 | 3 | 9.6 | 199.3 |
| Miyazaki | 1 135 | 1 832 | 4 | 6.2 | 295.5 |
| Kagoshima | 1 706 | 2 888 | 5 | 10.7 | 269.9 |
| Okinawa | 1 393 | 2 028 | 5 | 5.5 | 368.7 |
| Total | 128 054 | 226 851 | 564 | 959.2 | 236.5 |
JASTRO = Japanese Society for Radiation Oncology, RO = radiation oncologist, FTE = full-time equivalent.
Table 10.
Population size and numbers of patients, staffs, and patient load according to prefecture
| Prefecture | Total patients | FTE RTT | Total patients/FTE RTT | FTE MP | FTE RTQM |
|---|---|---|---|---|---|
| Hokkaido | 12 200 | 72.3 | 168.7 | 6.8 | 7.1 |
| Aomori | 2 281 | 22.1 | 103.2 | 2.6 | 1.6 |
| Iwate | 1 868 | 18.7 | 99.9 | 0.1 | 0.4 |
| Miyagi | 5 758 | 31.5 | 182.8 | 0.1 | 1.8 |
| Akita | 2 167 | 19.9 | 108.9 | 0.5 | 1.3 |
| Yamagata | 1 570 | 13.2 | 118.9 | 0.9 | 1.4 |
| Fukushima | 3 524 | 30.8 | 114.4 | 2.9 | 1.3 |
| Ibaraki | 4 444 | 42.2 | 105.3 | 1.1 | 1.5 |
| Tochigi | 3 534 | 25.9 | 136.4 | 1.6 | 3.1 |
| Gunma | 4 271 | 38.9 | 109.8 | 3.5 | 3.0 |
| Saitama | 8 990 | 50.3 | 178.7 | 2.2 | 4.2 |
| Chiba | 9 034 | 74.2 | 121.8 | 4.4 | 3.0 |
| Tokyo | 27 951 | 228.4 | 122.4 | 14.3 | 9.0 |
| Kanagawa | 14 331 | 125.3 | 114.4 | 6.9 | 8.3 |
| Niigata | 4 410 | 47.7 | 92.5 | 2.1 | 0.7 |
| Toyama | 1 761 | 21.8 | 80.8 | 0.8 | 1.4 |
| Ishikawa | 2 386 | 19.2 | 124.3 | 2.9 | 1.8 |
| Fukui | 1 487 | 15.7 | 94.7 | 1.6 | 0.9 |
| Yamanashi | 1 338 | 7.0 | 191.1 | 0.1 | 0.6 |
| Nagano | 3 940 | 31.1 | 126.7 | 2.2 | 1.6 |
| Gifu | 4 244 | 27.2 | 156.0 | 2.1 | 1.7 |
| Shizuoka | 7 569 | 71.4 | 106.0 | 5.5 | 4.2 |
| Aichi | 12 088 | 100.3 | 120.5 | 6.2 | 4.6 |
| Mie | 2 116 | 25.0 | 84.6 | 1.0 | 1.4 |
| Shiga | 2 238 | 24.3 | 92.1 | 2.1 | 2.0 |
| Kyoto | 4 710 | 33.3 | 141.4 | 5.7 | 4.7 |
| Osaka | 15 835 | 141.7 | 111.8 | 19.7 | 13.5 |
| Hyogo | 9 294 | 82.2 | 113.1 | 6.1 | 4.7 |
| Nara | 2 499 | 22.9 | 109.1 | 0.9 | 2.2 |
| Wakayama | 2 063 | 17.2 | 119.9 | 0.0 | 0.4 |
| Tottori | 1 149 | 12.3 | 93.4 | 0.3 | 2.1 |
| Shimane | 1 099 | 11.9 | 92.4 | 0.3 | 1.3 |
| Okayama | 3 271 | 30.4 | 107.6 | 1.7 | 2.9 |
| Hiroshima | 6 220 | 43.9 | 141.7 | 2.6 | 3.0 |
| Yamaguchi | 2 247 | 22.0 | 102.1 | 0.8 | 1.6 |
| Tokushima | 1 664 | 12.3 | 135.3 | 0.0 | 2.0 |
| Kagawa | 1 266 | 10.6 | 119.4 | 0.8 | 0.2 |
| Ehime | 2 631 | 21.2 | 124.1 | 2.6 | 2.3 |
| Kochi | 1 379 | 10.0 | 137.9 | 1.6 | 0.7 |
| Fukuoka | 9 903 | 67.1 | 147.6 | 4.2 | 5.1 |
| Saga | 1 017 | 7.6 | 133.8 | 0.0 | 0.5 |
| Nagasaki | 2 726 | 15.6 | 174.7 | 2.6 | 1.5 |
| Kumamoto | 3 717 | 28.0 | 132.8 | 2.5 | 2.4 |
| Oita | 1 913 | 21.1 | 90.7 | 1.9 | 1.3 |
| Miyazaki | 1 832 | 14.4 | 127.2 | 1.1 | 0.9 |
| Kagoshima | 2 888 | 20.1 | 143.7 | 1.0 | 0.0 |
| Okinawa | 2 028 | 11.1 | 182.7 | 0.6 | 0.4 |
| Total | 226 851 | 1841.3 | 123.2 | 131.3 | 121.5 |
FTE = full-time equivalent, RTT = radiotherapy technologist, MP = medical physicist, RTQM = radiotherapy quality manager, NS = nurse.
Table 11.
Numbers of institutions and patients receiving special radiotherapy by scale classification
| Specific therapy | 2010 | 2009 | ||||||
|---|---|---|---|---|---|---|---|---|
| A (123) | B (227) | C (129) | D (86) | E (45) | F (95) | Total (705) | Total (700) | |
| Intracavitary radiotherapy | ||||||||
| Treatment institutions | 0 | 10 | 23 | 25 | 21 | 73 | 152 | 151 |
| Patients | 0 | 107 | 335 | 393 | 329 | 2 081 | 3 245 | 3 139 |
| Interstitial radiotherapy | ||||||||
| Treatment institutions | 1 | 8 | 17 | 18 | 12 | 59 | 115 | 109 |
| Patients | 41 | 66 | 319 | 550 | 305 | 2913 | 4 194 | 4 070 |
| Radioactive iodine therapy for prostate | ||||||||
| Treatment institutions | 1 | 4 | 16 | 17 | 11 | 52 | 101 | 96 |
| Patients | 41 | 44 | 312 | 485 | 215 | 2 018 | 3 115 | 3 080 |
| Radioactive iodine therapy for hyperthyroidism | ||||||||
| Treatment institutions | 0 | 5 | 11 | 7 | 11 | 25 | 59 | 97 |
| Patients | 0 | 62 | 427 | 100 | 377 | 1 114 | 2 080 | 4 478 |
| Total body radiotherapy | ||||||||
| Treatment institutions | 9 | 20 | 25 | 31 | 28 | 73 | 186 | 180 |
| Patients | 57 | 148 | 254 | 171 | 294 | 1 013 | 1 937 | 1 790 |
| Intraoperative radiotherapy | ||||||||
| Treatment institutions | 1 | 1 | 2 | 5 | 5 | 10 | 24 | 28 |
| Patients | 2 | 1 | 5 | 18 | 25 | 110 | 161 | 173 |
| Stereotactic brain radiotherapy | ||||||||
| Treatment institutions | 12 | 40 | 37 | 42 | 28 | 52 | 211 | 202 |
| Patients | 511 | 2 364 | 2 108 | 2 629 | 2 214 | 3 974 | 13 800 | 13 855 |
| Stereotactic body radiotherapy | ||||||||
| Treatment institutions | 5 | 29 | 35 | 45 | 22 | 67 | 203 | 165 |
| Patients | 120 | 205 | 482 | 603 | 307 | 1 819 | 3 536 | 2 537 |
| IMRT | ||||||||
| Treatment institutions | 4 | 13 | 17 | 25 | 14 | 63 | 136 | 101 |
| Patients | 165 | 503 | 780 | 1 049 | 646 | 3 213 | 6 356 | 4 296 |
| Thermoradiotherapy | ||||||||
| Treatment institutions | 1 | 2 | 7 | 2 | 3 | 5 | 20 | 20 |
| Patients | 9 | 6 | 38 | 11 | 184 | 111 | 359 | 391 |
| Sr-90 radiotherapy for pterygia | ||||||||
| Treatment institutions | 0 | 0 | 2 | 2 | 0 | 1 | 5 | 11 |
| Patients | 0 | 0 | 8 | 14 | 0 | 11 | 33 | 90 |
| Internal 89Sr radiotherapy | ||||||||
| Treatment institutions | 4 | 25 | 22 | 29 | 15 | 47 | 142 | |
| Patients | 12 | 111 | 80 | 172 | 83 | 335 | 793 | |
| Internal Y-90 radiotherapy | ||||||||
| Treatment institutions | 1 | 3 | 1 | 4 | 4 | 20 | 33 | |
| Patients | 1 | 8 | 3 | 11 | 8 | 122 | 153 | |
IMRT = intensity-modulated radiotherapy, Sr = strontium, Y = yttrium.
Table 12.
Annual numbers of new patients by disease sitea
| Primary site | n | % |
|---|---|---|
| Cerebrospinal | 8 065 | 4.4 |
| Head and neck (including thyroid) | 17 513 | 9.6 |
| Esophagus | 10 207 | 5.6 |
| Lung, trachea and mediastinum | 35 149 | 19.3 |
| Lung | 32 540 | 17.8 |
| Breast | 43 315 | 23.7 |
| Liver, biliary tract, pancreas | 6 835 | 3.7 |
| Gastric, small intestine, colorectal | 8 741 | 4.8 |
| Gynecologic | 8 563 | 4.7 |
| Urogenital | 25 832 | 14.2 |
| Prostate | 20 303 | 11.1 |
| Hematopoietic and lymphatic | 8 587 | 4.7 |
| Skin, bone and soft tissue | 4 601 | 2.5 |
| Other (malignant) | 2 377 | 1.3 |
| Benign tumors | 2 706 | 1.5 |
| Pediatric ≤15 years (included in totals above) | 858 | 0.5 |
| Total | 182 491 | 100 |
aThe total numbers of new patients in Table 3 differ from these data, because no data on primary sites were reported by some institutions.
Table 13.
Annual number of total patients (new plus repeat) treated for brain metastasis and bone metastasis by scale classification
| Metastasis | Scale category (number of institutions) | Total (705) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A (123) | B (227) | C (129) | D (86) | E (45) | F (95) | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Brain | 761 | 8.6 | 4 504 | 11.5 | 3 345 | 9.0 | 3 622 | 10.4 | 2 317 | 9.5 | 7 216 | 8.7 | 21 765 | 9.6 |
| Bone | 1 414 | 15.9 | 5 847 | 15.0 | 5 059 | 13.7 | 4 812 | 13.8 | 2 629 | 10.8 | 9 235 | 11.1 | 28 996 | 12.8 |
Data presented as number of patients, with percentages in parentheses.
Table 14.
Classification of institutions by number of FTE radiation oncologists in all radiotherapy institutions and designated cancer care hospitals
| Institution category | Description | Institutions |
|---|---|---|
| RH-A | All radiotherapy hospitals (FTE RO ≥ 1.0) | 374 |
| RH-B | All radiotherapy hospitals (FTE RO < 1.0) | 331 |
| Total | 705 | |
| DCCH-A | Designated cancer care hospitals (FTE RO ≥ 1.0) | 260 |
| DCCH-B | Designated cancer care hospitals (FTE RO < 1.0) | 114 |
| Total | 374 |
FTE = full-time equivalent, RO = radiation oncologist.
Table 15.
Annual numbers of patients receiving radiotherapy, numbers of LINACs, numbers of staff, patient load per LINAC, and patient load per member of staff according to institution category shown in Table 14; all radiotherapy hospitals
| RH-A (374) | RH-B (331) | Total (705) | ||||
|---|---|---|---|---|---|---|
| Average per hospital | Total number | Average per hospital | Total number | Average per hospital | Total number | |
| Total patients | 456.5 | 170 739 | 169.5 | 56 112 | 321.8 | 226 851 |
| New patients | 379.4 | 141 879 | 146.4 | 48 443 | 270.0 | 190 322 |
| LINACs | 1.4 | 514 | 1.0 | 315 | 1.2 | 829 |
| Annual total no. of patients / LINAC | 332.2 | 178.1 | 273.6 | |||
| Annual no. of new patients / LINAC | 276.0 | 153.8 | 229.6 | |||
| FTE ROs | 2.2 | 819.0 | 0.4 | 140.2 | 1.4 | 959.2 |
| JASTRO-certified ROs (full time) | 1.3 | 503 | 0.2 | 61 | 0.8 | 564 |
| Annual total no. of patients / FTE RO | 208.5 | 400.3 | 236.5 | |||
| Annual no. of new patients / FTE RO | 173.2 | 345.6 | 198.4 | |||
| FTE RT technologists | 3.5 | 1297.1 | 1.6 | 544.2 | 2.6 | 1841.3 |
| Annual total no. of patients / FTE RTT | 131.6 | 103.1 | 123.2 | |||
| Annual no. of new patients / FTE RTT | 109.4 | 89.0 | 103.4 | |||
| FTE RT technologists / LINAC | 2.5 | 1.7 | 2.2 | |||
| FTE medical physicists | 0.28 | 103.9 | 0.08 | 27.5 | 0.19 | 131.3 |
| Annual total no. of patients / FTE MP | 1644.1 | 2044.2 | 1727.7 | |||
| Annual no. of new patients / FTE MP | 1366.2 | 1764.8 | 1449.5 | |||
| FTE RT quality managers | 0.24 | 90.0 | 0.10 | 31.5 | 0.17 | 121.5 |
| Annual total no. of patients / FTE RTQM | 1897.1 | 1781.3 | 1,867.1 | |||
| Annual no. of new patients / FTE RTQM | 1576.4 | 1537.9 | 1566.4 | |||
| FTE RT quality managers / LINAC | 0.18 | 0.10 | 0.15 | |||
Table 16.
Annual numbers of patients receiving radiotherapy, numbers of LINACs, numbers of staff, patient load per LINAC, and patient load per member of staff according to institution category shown in Table 14; designated cancer care hospitals
| DCCH-A (260) | DCCH-B (114) | Total (374) | ||||
|---|---|---|---|---|---|---|
| Average per hospital | Total number | Average per hospital | Total number | Average per hospital | Total number | |
| Total patients | 529.8 | 137 744 | 203.8 | 23 234 | 430.4 | 160 978 |
| New patients | 440.8 | 114 609 | 178.0 | 20 295 | 360.7 | 134 904 |
| LINACs | 1.5 | 401 | 1.0 | 117 | 1.4 | 518 |
| Annual total no. of patients / Linac | 343.5 | 198.6 | 310.8 | |||
| Annual no. of new patients / Linac | 285.8 | 173.5 | 260.4 | |||
| FTE ROs | 2.5 | 637.5 | 0.5 | 62.4 | 1.9 | 699.9 |
| JASTRO-certified ROs (full time) | 1.6 | 426 | 0.2 | 28 | 1.2 | 454 |
| Annual total no. of patients / FTE RO | 216.1 | 372.6 | 230.0 | |||
| Annual no. of new patients / FTE RO | 179.8 | 325.5 | 192.8 | |||
| FTE RT technologists | 3.9 | 1013.1 | 1.9 | 219.9 | 3.3 | 1233.0 |
| Annual total no. of patients / FTE RTT | 136.0 | 105.7 | 130.6 | |||
| Annual no. of new patients / FTE RTT | 113.1 | 92.3 | 109.4 | |||
| FTE RT technologists / LINAC | 2.5 | 1.9 | 2.4 | |||
| FTE medical physicists | 0.31 | 80.9 | 0.05 | 5.6 | 0.23 | 86.5 |
| Annual total no. of patients / FTE MP | 1702.6 | 4186.3 | 1862.1 | |||
| Annual no. of new patients / FTE MP | 1416.7 | 3656.8 | 1560.5 | |||
| FTE RT quality managers | 0.27 | 70.9 | 0.11 | 12.6 | 0.22 | 83.5 |
| Annual total no. of patients / FTE RTQM | 1944.2 | 1844.0 | 1929.0 | |||
| Annual no. of new patients / FTE RTQM | 1617.6 | 1610.7 | 1616.6 | |||
| FTE RT quality managers / LINAC | 0.18 | 0.11 | 0.16 | |||
LINAC = linear accelerator, FTE = full-time equivalent, RO = radiation oncologist, RTT = radiotherapy technologist, MP = medical physicist, RTQM = radiotherapy quality manager.
Table 17.
Number of items of equipment and their functions according to institution category showing Table 14
| RH-A (n = 374) | RH-B (n = 331) | Total (n = 705) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| LINAC | 514 | 95.7 | 315 | 93.7 | 829 | 94.8 |
| with dual-energy function | 397 | 82.6 | 209 | 62.5 | 606 | 73.2 |
| with 3DCRT function (MLC width ≤ 1.0 cm) | 475 | 89.3 | 226 | 68 | 701 | 79.3 |
| with IMRT function | 310 | 57.8 | 65 | 19.6 | 375 | 39.9 |
| with cone-beam CT or CT on rail | 190 | 41.4 | 49 | 14.8 | 239 | 28.9 |
| with treatment position verification system (X-ray perspective image) | 192 | 39 | 54 | 15.7 | 246 | 28.1 |
| with treatment-position verification system (other than those above) | 148 | 32.6 | 66 | 19.9 | 214 | 26.7 |
| CT simulator | 365 | 90.4 | 268 | 76.1 | 633 | 83.7 |
| DCCH-A (n = 260) | DCCH-B (n = 114) | Total (n = 374) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| LINAC | 401 | 98.8 | 117 | 99.1 | 518 | 98.9 |
| with dual-energy function | 318 | 90.4 | 94 | 80.7 | 412 | 87.4 |
| with 3DCRT function (MLC width ≤ 1.0 cm) | 379 | 94.6 | 91 | 78.9 | 470 | 89.8 |
| with IMRT function | 261 | 66.9 | 34 | 29.8 | 295 | 55.6 |
| with cone-beam CT or CT on rail | 158 | 48.1 | 24 | 21.1 | 182 | 39.8 |
| with treatment-position verification system (X-ray perspective image) | 154 | 43.5 | 23 | 19.3 | 177 | 36.1 |
| with treatment-position verification system (other than those above) | 117 | 36.2 | 29 | 25.4 | 146 | 32.9 |
| CT simulator | 264 | 94.2 | 104 | 83.3 | 368 | 90.9 |
LINAC = linear accelerator, 3DCRT = three dimensional conformal radiotherapy, MLC = multileaf collimator, IMRT = intensity-modulated radiotherapy, CT = computed tomography.
Table 18.
Numbers of radiotherapy institutions and treatment devices, and patient load and personnel trend 1990–2010
| Survey year | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 1993 | 1995 | 1997 | 1999 | 2001 | 2003 | 2005 | 2007 | 2009 | 2010 | |
| Institution | 378 | 629 | 504 | 568 | 636 | 603 | 726 | 712 | 721 | 700 | 705 |
| Response rate | 48.5% | 88.3% | 73.9% | 78.6% | 86.3% | 85.3% | 100% | 96.9% | 94.2% | 90.9% | 90.4% |
| New patients | 62 829 | 71 696 | 84 379 | 107 150 | 118 016 | 149 793 | 156 318 | 170 229 | 182 390 | 190 322 | |
| Total patients | 191 173 | 205 087 | 217 829 | 226 851 | |||||||
| Average no. of new patients | 166 | 142 | 149 | 168 | 196 | 206 | 220 | 236 | 261 | 270 | |
| Treatment device (in actual use) | |||||||||||
| LINAC | 311 | 508 | 407 | 475 | 626 | 626 | 744 | 765 | 807 | 816 | 829 |
| Telecobalt | 170 | 213 | 127 | 98 | 83 | 45 | 42 | 11 | 15 | 11 | 9 |
| 192Ir RALS | 29 | 50 | 73 | 93 | 117 | 119 | 123 | 130 | 131 | ||
| Full-time ROs | 547 | 748 | 821 | 889 | 925 | 878 | 921 | 1 003 | 1 007 | 1 085 | 1 123 |
| FTE ROs | 774 | 826 | 939 | 959 | |||||||
| Full-time JASTRO-certified ROs | 308 | 369 | 426 | 477 | 529 | 564 | |||||
| FTE RT technologists | 592 | 877 | 665 | 733 | 771 | 918 | 1 555 | 1 635 | 1 634 | 1 836 | 1 841 |
| Treatment-planning equipment | |||||||||||
| X-ray simulators | 295 | 430 | 394 | 452 | 512 | 464 | 532 | 502 | 445 | 361 | 348 |
| CT simulators | 30 | 75 | 55 | 96 | 164 | 247 | 329 | 407 | 497 | 575 | 633 |
| RTP computers | 238 | 468 | 374 | 453 | 682 | 680 | 874 | 940 | 1 070 | 1 271 | 1 381 |
LINAC = linear accelerator, Ir = iridium, RO = radiation oncologist, FTE = full-time equivalent, JASTRO = Japanese Society for Radiation Oncology, RT = radiotherapy, JRS = Japan Radiological Society, JASTRO = Japanese Society for Radiation Oncology, CT = computed tomography, RTP = radiotherapy planning.
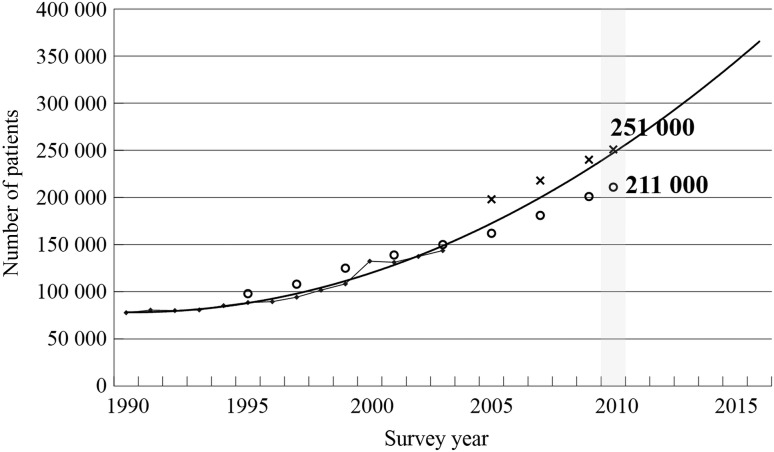
Fig. 1.
Estimate of increase in demand for radiotherapy in Japan, based on statistical correction of annual change in the number of new patients per year at Patterns of Care Study survey facilities [25]. Crosses and circles denote the estimated numbers of total (new plus repeat) and new patients, respectively, from the results in the structure surveys by the JASTRO.
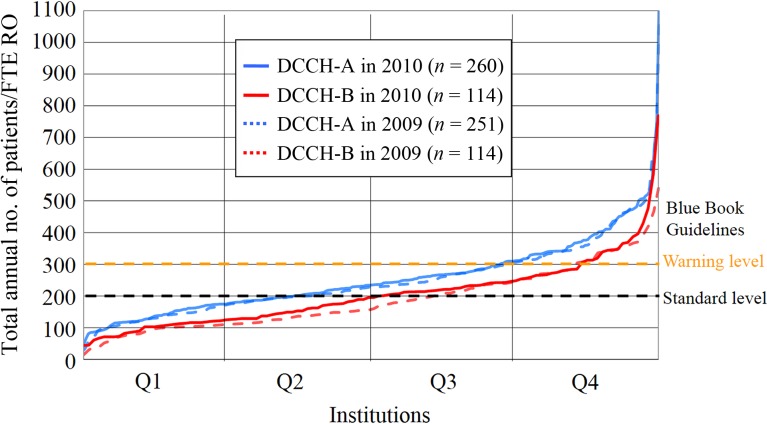
Fig. 6.
Distribution of annual total (new plus repeat) patient load per full-time equivalent (FTE) radiotherapy technologist (RTT) in designated cancer care hospitals. Horizontal axis represents institutions arranged in order of increasing total annual number of patients per FTE RTT within the institution. Q1: 0–25%, Q2: 26–50%, Q3: 51–75%, Q4: 76–100%.
Fig. 2.
Distribution of annual total (new plus repeat) patient load per LINAC in radiotherapy institutions. Horizontal axis represents institutions arranged in order of increasing total annual number of patients per LINAC within the institution. Q1: 0–25%, Q2: 26–50%, Q3: 51–75%, Q4: 76–100%.
Fig. 3.
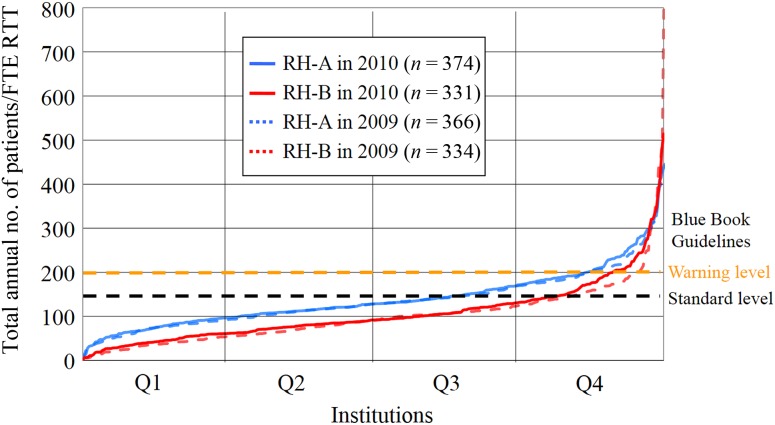
Distribution of annual total (new plus repeat) patient load per full-time equivalent (FTE) radiation oncologist (RO) in all radiotherapy institutions. Horizontal axis represents institutions arranged in order of increasing total annual number of patients per FTE rRO within the institution. Q1: 0–25%, Q2: 26–50%, Q3: 51–75%, Q4: 76–100%.
Fig. 4.
Distribution of annual total (new plus repeat) patient load per full-time equivalent (FTE) radiotherapy technologist (RTT) in all radiotherapy institutions. Horizontal axis represents institutions arranged in order of increasing total annual number of patients per FTE RTT within the institution. Q1: 0–25%, Q2: 26–50%, Q3: 51–75%, Q4: 76–100%.
Fig. 5.
Distribution of annual total (new plus repeat) patient load per full-time equivalent (FTE) radiation oncologist (RO) in designated cancer care hospitals. Horizontal axis represents institutions arranged in order of increasing value of total annual number of patients per FTE RO within the institution. Q1: 0–25%, Q2: 26–50%, Q3: 51–75%, Q4: 76–100%.
CONFLICT OF INTEREST
The authors state that there are no conflicts of interest.
FUNDING
This study was supported by the JASTRO and Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science [JSPS KAKENHI Grant No. JP16K45678].
REFERENCES
- 1. Tsunemoto H. Present status of Japanese radiation oncology: national survey of structure in 1990 [in Japanese]. J Jpn Soc Ther Radiol Oncol (Special Report) 1992;1–30. [Google Scholar]
- 2. Sato S, Nakamura Y, Kawashima K et al. Present status of radiotherapy in Japan—a census in 1990—finding on radiotherapy facilities [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 1994;6:83–9. [Google Scholar]
- 3. Morita K, Uchiyama Y. Present status of radiotherapy in Japan—the second census in 1993 [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 1995;7:251–61. [Google Scholar]
- 4. JASTRO Database Committee Present status of radiotherapy in Japan—the regular census in 1995 [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 1997;9:231–53. [Google Scholar]
- 5. JASTRO Database Committee Present status of radiotherapy in Japan—the regular census in 1997 [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 2001;13:175–82. [Google Scholar]
- 6. JASTRO Database Committee Present status of radiotherapy in Japan—the regular structure survey in 1999 [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 2001;13:227–35. [Google Scholar]
- 7. JASTRO Database Committee Present status of radiotherapy in Japan—the regular structure survey in 2001 [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 2003;15:51–9. [Google Scholar]
- 8. JASTRO Database Committee Present status of radiotherapy in Japan—the regular structure survey in 2003 [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 2005;17:115–21. [Google Scholar]
- 9. Shibuya H, Tsujii H. The structural characteristics of radiation oncology in Japan in 2003. Int J Radiat Oncol Biol Phys 2005;62:1472–6. [DOI] [PubMed] [Google Scholar]
- 10. Teshima T, Numasaki H, Shibuya H et al. Japanese structure survey of radiation oncology in 2005 (first report) [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 2007;19:181–92. [Google Scholar]
- 11. Teshima T, Numasaki H, Shibuya H et al. Japanese structure survey of radiation oncology in 2005 (second report) [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 2007;19:193–205. [Google Scholar]
- 12. Teshima T, Numasaki H, Shibuya H et al. Japanese structure survey of radiation oncology in 2005 based on institutional stratification of patterns of care study. Int J Radiat Oncol Biol Phys 2008;72:144–52. [DOI] [PubMed] [Google Scholar]
- 13. Numasaki H, Teshima T, Shibuya H et al. National structure of radiation oncology in Japan with special reference to designated cancer care hospital. Int J Clin Oncol 2009;14:237–44. [DOI] [PubMed] [Google Scholar]
- 14. Teshima T, Numasaki H, Shibuya H et al. Japanese structure survey of radiation oncology in 2007 (first report) [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 2009;21:113–25. [Google Scholar]
- 15. Teshima T, Numasaki H, Shibuya H et al. Japanese structure survey of radiation oncology in 2007 (second report) [in Japanese with an English abstract]. J Jpn Soc Ther Radiol Oncol 2009;21:126–38. [Google Scholar]
- 16. Teshima T, Numasaki H, Shibuya H et al. Japanese structure survey of radiation oncology in 2007 based on institutional stratification of patterns of care study. Int J Radiat Oncol Biol Phys 2010;72:144–52. [DOI] [PubMed] [Google Scholar]
- 17. Numasaki H, Teshima T, Shibuya H et al. Japanese structure survey of radiation oncology in 2007 with special reference to designated cancer care hospitals. Strahlenther Onkol 2011;187:167–74. [DOI] [PubMed] [Google Scholar]
- 18. Numasaki H, Shibuya H, Nishio M et al. National medical care system may impede fostering of true specialization of radiation oncologists: study based on structure survey in Japan. Int J Radiat Oncol Biol Phys 2012;82:e111–7. [DOI] [PubMed] [Google Scholar]
- 19. Teshima T, Numasaki H, Nishimura T et al. Japanese Structure Survey of Radiation Oncology in 2009 (First Report) [in Japanese]. http://www.jastro.or.jp/aboutus/datacenter.php (1 November 2013, date last accessed).
- 20. Teshima T, Numasaki H, Nishimura T et al. Japanese Structure Survey of Radiation Oncology in 2009 (Second Report) [in Japanese]. http://www.jastro.or.jp/aboutus/datacenter.php (1 November 2013, date last accessed).
- 21. Teshima T, Numasaki H, Nishio M et al. Japanese structure survey of radiation oncology in 2009 based on institutional stratification of patterns of care study. J Radiat Res 2012;53:710–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Numasaki H, Teshima T, Shibuya H et al. Japanese structure survey of radiation oncology in 2009 with special reference to designated cancer care hospitals. Int J Clin Oncol 2013;18:775–783. [DOI] [PubMed] [Google Scholar]
- 23. Teshima T, Numasaki H, Shibuya H et al. Japanese Structure Survey of Radiation Oncology in 2010 (First Report) [in Japanese]. http://www.jastro.or.jp/aboutus/datacenter.php (1 June 2017, date last accessed).
- 24. Teshima T, Numasaki H, Shibuya H et al. Japanese Structure Survey of Radiation Oncology in 2010 (Second Report) [in Japanese]. http://www.jastro.or.jp/aboutus/datacenter.php (1 June 2017, date last accessed).
- 25. Japanese PCS Working Group Radiation oncology in multidisciplinary cancer therapy—basic structure requirement for quality assurance of radiotherapy based on Patterns of Care Study in Japan. Ministry of Health, Labor, and Welfare Cancer Research Grant Planned Research Study 14-6, 2005.
- 26. Japanese PCS Working Group Radiation oncology in multidisciplinary cancer therapy—basic structure requirement for quality assurance of radiotherapy based on Patterns of Care Study in Japan. Ministry of Health, Labor, and Welfare Cancer Research Grant Planned Research Study 18-4, 2010.
- 27. Tanisada K, Teshima T, Ohno Y et al. Patterns of Care Study quantitative evaluation of the quality of radiotherapy in Japan. Cancer 2002;95:164–71. [DOI] [PubMed] [Google Scholar]
- 28. Teshima T; Japanese PCS Working Group Patterns of Care Study in Japan. Jpn J Clin Oncol 2005;35:497–506. [DOI] [PubMed] [Google Scholar]
- 29. The Designated Cancer Hospitals, Ministry of Health, Labor and Welfare : A List of Designated Cancer Hospitals (Point in time: 1 August 2013). http://www.mhlw.go.jp/ (1 November 2013, date last accessed).
- 30. Cancer Registry and Statistics Cancer Information Service, National Cancer Center, Japan http://ganjoho.jp/reg_stat/statistics/dl/index.html (1 October 2014, date last accessed).