Abstract
Evidence-based strategies helped reduce opioid doses and identify abuse and misuse in patients referred to an opioid monitoring clinic.
Chronic pain, defined as pain lasting longer than 3 to 6 months in duration, affects about 100 million Americans.1 The use of opioids in the management of chronic nonmalignant pain is common in primary care. The U.S., with only 5% of the global population, nevertheless is the world’s leading opioid consumer.2 For example, it is estimated that the U.S. consumes 56% of the global supply of morphine, 99% of hydrocodone, and 83% of oxycodone; this consumption is a growing problem in the use of chronic opioid therapy in managing chronic nonmalignant pain.2,3 The high rates of use of opioids continues, despite a lack of solid evidence on the long-term effectiveness of opioids for managing chronic nonmalignant pain and on the associated risks of opioid addiction, abuse, and misuse.3,4 Among veterans, the prevalence of opioid abuse and misuse has been reported to be about 30%, a nearly 7-fold occurrence compared with that in the general population.5,6
Due to the pervasiveness of opioid abuse and misuse among veterans, a project was initiated to develop, implement, and evaluate an Opioid Monitoring Clinic (OMC) as a clinical referral system within the primary care service of the VA Southern Nevada Healthcare System (VASNHS) in North Las Vegas. A health care provider (HCP) needs assessment was conducted at the facility, resulting in recommendations to improve adherence to evidence-based clinical practice guidelines in opioid management and regular monitoring of veterans on chronic opioid therapy for the identification of opioid abuse and misuse. Based on the results, an advanced practice registered nurse (APRN) in consultation with the chief of primary care at VASNHS and teamlet support (a registered nurse, licensed practical nurse, and medical support assistant) started the OMC. The OMC was developed consistent with the 2010 VA/DoD clinical practice guidelines for managing opioid therapy for chronic pain.7
After 6 months of OMC operation, the project also was evaluated for efficacy. First, a retrospective chart review of participants was conducted to identify the use of opioid pain agreements, prescription drug monitoring programs (PDMP) for controlled substance use review, and urine drug screens (UDSs). The chart review also included the average daily morphine equivalent dose (MED) for patients and OMC retention rates. Second, an online survey of primary care providers (PCPs) assessed their adherence to evidence-based guidelines in opioid management and satisfaction of the OMC services.
BACKGROUND
In 1997, the average sales and distribution of opioids in the U.S. was 96 mg MED per individual, which increased to 710 mg per individual in 2010.8,9 The MED is a standardized daily dose measure for all opioids.10 At VASNHS North Las Vegas, there were 5,881 patients on opioid therapy in 2013 with about 13% of patients on opioid therapy using about 100 mg MED/d. The potential for abuse and misuse was great. Almost 30% of patients on chronic opioid therapy for chronic nonmalignant pain abuse their opioid prescriptions.5,7 Subsequently, opioid analgesics were responsible for nearly 60% of overdose deaths in 2010.11
In 2010, there were about 12 million people in the U.S. who abused or misused prescription opioids, using them for nonmedical reasons; annually, the prevalence rate of Americans who abuse and misuse opioids is about 2 million people.12 The 5-year prevalence rate of opioid abuse among veterans is at least 3%.6 This results in health care expenditures with an average excess medical cost of $20,546 per year for patients who misuse opioids compared with those who do not.13 The economic burden among veterans is even higher. Baser and colleagues reported that the annual economic cost for veterans who abused their opioid prescriptions was nearly $29,000.6
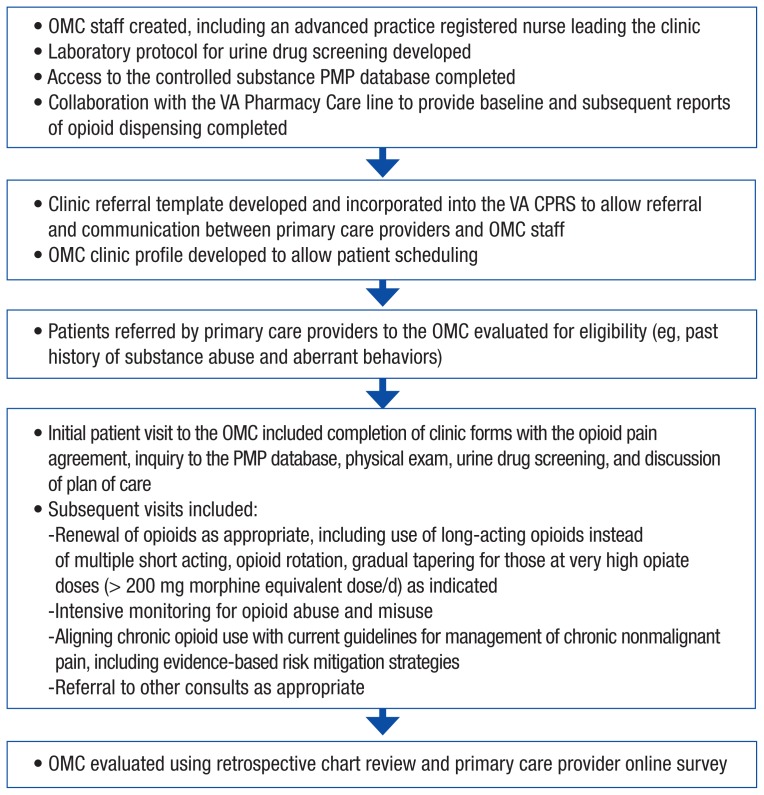
Unfortunately, injudicious opioid prescribing by HCPs is often cited as a contributor to the growing problem of opioid abuse and misuse in the U.S.14 Health care provider education on the proper and judicious use of opioids and adherence to clinical practice guidelines in the management of chronic pain is a crucial factor in reducing the complications of chronic opioid therapy.3,14 Hence, the OMC was developed to address the prevailing problem of opioid abuse and misuse by implementing strict monitoring of high-risk veterans on chronic opioid therapy, using mitigation strategies based on the 2010 VA/DoD clinical practice guidelines to help identify abuse as early as possible. The OMC was implemented and took over opioid prescription renewal, dose adjustments, opioid substitution as appropriate, and patient opioid monitoring that was consistent with the 2010 VA/ DoD guidelines (Figure).
Figure.
Development and Implementation of the OMC
Abbreviations: CPRS, Computerized Patient Record System; OMC, opioid monitoring clinic; PMP, prescription monitoring program.
METHOD
This project evaluated the APRN-led OMC with both quantitative and qualitative data from patients and PCPs. The OMC was implemented at VASNHS North Las Vegas, which serves almost 60,000 veterans. Patients referred to the OMC who were eligible for admission were veterans aged ≥ 18 years, who had chronic nonmalignant pain for at least 3 months, were receiving chronic opioid therapy, and were considered high risk for abuse or misuse of opioids. Patients were considered high risk if they had documented aberrant behaviors, such as multiple early refill requests, history of lost medications, drug screens not showing prescribed opioid(s), positive drug screens for controlled substance not prescribed, nonadherence with plan of care, or a history of substance abuse, including alcohol, cocaine, heroin, and marijuana. Veterans found to be suicidal or homicidal were excluded from the OMC and instead were referred to appropriate specialty care for further evaluation. A total of 61 veteran participants were successfully recruited.
Primary care physicians, physician assistants, and APRNs working at VASNHS on a full-time and part-time basis were eligible for participation as PCPs in this project. Thirty of 42 eligible PCPs participated and responded to the secure online provider survey (71% response rate).
Risks and benefits were discussed, and a written informed consent was obtained for each participant. There were no apparent risks or adverse effects encountered during project implementation and evaluation. Prior to data collection, permission for the study was obtained from the VA facility. An institutional review board application through the University of Nevada, Las Vegas’ Office of Research Integrity-Human Subjects was also submitted and approved through an expedited review.
RESULTS
Table 1 details patient data, including demographics on the veteran participants. The average age was 53 years, the majority were male, and back pain was the most common source of chronic nonmalignant pain. Many used opioids and benzodiazepines concurrently. The majority had signed an opioid pain agreement (OPA) and had a UDS prior to being seen in the OMC. Positive screens were noted among 38% of the participants. The UDS included detection of illicit use, which was found in 12 participants (ie, methamphetamines, barbiturates, cocaine, heroin, and/or benzodiazepines or methadone when none were expected). A negative opioid level despite opioid prescription was found in 9 UDSs, while 2 detected both illicit substances and negative opioid levels.
Table 1.
Patient Data (N = 61)
| Characteristics | n (%) |
|---|---|
|
| |
| Gender | |
| Male | 57 (93) |
| Female | 4 (7) |
|
|
|
| Pain source | |
| Back | 37 (61) |
| Other | 24 (39) |
|
|
|
| Concurrent controlled substance use | 25 (41) |
|
|
|
| Prior pain agreement | 54 (89) |
|
|
|
| Prior urine drug screen | 49 (80) |
|
|
|
| Positive urine drug screen | 23 (38) |
|
|
|
| Doctor shopping | 12 (20) |
Review of PDMPs revealed that 20% of the participants received controlled substances from other HCPs. Consequently, all OMC patients completed and had reinforced OPAs that served 2 purposes. First, the content in the agreement provided patient education regarding the potential hazards of opioid use. Second, the content provided specific expectations from the patient if opioid therapy is continued, including opioid risk reduction strategies (ie, random UDSs and pill counts, PDMP for controlled substance utilization review), and the consequences of lack of adherence to opioid management.
The majority of patients remained as patients and continued to be monitored after 6 months at the OMC (Table 2). However, only 64% were retained in the OMC, in large part because 36% had their opioids discontinued due to discovery of active illicit substance use, opioid abuse, “doctor shopping,” nonadherence with the treatment plan, self-discharge from the OMC, and/or their care was transferred to the VA pain clinic. As part of the protocol for the OMC, veterans who were found to be abusing and/or misusing their prescription opioids were referred for treatment to the VA Alcohol and Drug Treatment Program, or care was transferred to the VA Integrated Pain Clinic for nonpharmacologic interventional management as appropriate.
Table 2.
Patient Retention Outcomes (N = 61)
| Outcomes | n (%) |
|---|---|
| Retained in opioid monitoring clinic | 39 (64) |
| Discharged to VA alcohol and drug treatment program | 12 (20) |
| Transfer of care to VA Integrated Pain Clinic | 9 (15) |
| Self-discharge from opioid monitoring clinic | 1 (1) |
The mean MED/d among OMC participants was 54 mg/d before admission, which decreased gradually to 22 mg/d after 6 months of OMC care; this represented a 59% MED reduction (Table 3). Using the exact single-tailed Wilcoxon signed rank test, before and after, MED difference was found to be highly significant; P < .001.
Table 3.
Morphine Equivalent Dose (N = 39)
| MED/d Before OMC | MED/d After OMC | Change in MED | P Value |
|---|---|---|---|
| 54 mg | 22 mg | −59% | P < .001 |
Abbreviations: MED, morphine equivalent dose; OMC, opioid monitoring clinic.
Primary Care Providers
Based on the survey of PCPs, 40% of respondents referred at least 1 patient to the OMC. The majority (90%) acknowledged following the VA/DoD guidelines for opioid management, with 80% using an OPA more than usual since the implementation of the OMC, and 54% routinely accessing a PDMP for controlled substance utilization review. Moreover, 93% of PCPs routinely ordered a UDS when indicated.
For 3 months prior to opening the OMC in 2013, 1,606 UDSs were ordered at VASNHS. The UDS number steadily increased, and 6 months after opening the OMC, UDSs increased to 2,293 from months 4 to 6, representing a 30% increase. This was an expected outcome from the OMC— more PCPs now were following the VA/DoD clinical practice guidelines regarding the monitoring of patients on chronic opioid therapy.
A survey assessed the level of satisfaction among PCPs who had referred their patients to the OMC. Although only 11 PCPs responded to this question, a large majority found the OMC to have a positive effect on primary care services; many noted receiving fewer complaints regarding pain medications and fewer walk-ins. The majority recognized the advantage of the OMC in facilitating more PCP time for managing other medical problems beyond opioid use, which tends to be challenging and time consuming. Overall, 100% were satisfied with the OMC service.
Finally, 82% of PCPs reported that the OMC referral process did not need improvement. Two PCPs (18%) left positive feedback, reporting that the OMC was “simple, easy and accessible” and that the referral process “so far, it is great.” Another PCP noted, “I want patients who are suicidal but still need pain control with narcotics to be addressed.”
DISCUSSION
The OMC has shown great promise in identifying abuse and misuse of opioids through evidence-based guidelines and risk-mitigation strategies. In the past, VA clinics specifically focused on opioid renewal have been implemented. In 2002, the Philadelphia VAMC opened an opioid renewal clinic (ORC) to assist PCPs in the management of patients with chronic pain on chronic opioid therapy. 15 The Philadelphia VAMC ORC was operated collaboratively by PCPs and Pharmacy Service. They reported that 51% of their patients initially had documented aberrant behaviors, and 45% of these patients resolved their aberrant behaviors through intensive opioid monitoring using random UDSs.14 Thirteen percent of their patients were found to have an opioid addiction disorder and eventually were referred to addiction treatment; and 4% were weaned off opioids due to consistently negative UDSs.14
In the same manner, the OMC has effectively identified patients who abused and misused their opioids and consequently referred these patients for pain interventional management or to the VASNHS alcohol and drug treatment program as appropriate, which falls under the VASNHS Mental Health Care line, a service that is vital for veterans who are suicidal and homicidal. The importance of mental health care cannot be understated, as many patients with chronic pain also experience mental health challenges.
The Malcom Randall VAMC in Gainesville, Florida, structured a nurse-led, multidisciplinary ORC in 2003.16 A retrospective review of their program showed that 33% of patients had a positive UDS for marijuana, cocaine, or alcohol. The ORC had increased patient involvement in substance abuse treatment, resulting in some patients taking lower opioid dosages than before.
The New York Harbor VAMC reduced opioid cost by effectively switching veterans on expensive long-acting opioids, such as oxycodone and fentanyl, to less expensive alternatives, such a long-acting morphine. 17 A secondary purpose of the New York initiative was to reduce the potential for inappropriate use of expensive long-acting opioids. Accordingly, the initiative reduced the number of expensive long-acting and potentially inappropriate opioids from 165 to 69 prescriptions in less than 6 months (November 2007 through March 2008). Similarly, after 6 months of operation, the OMC significantly reduced opioid prescription from 54 mg to 22 MED/d. This reduction represents a significant pharmacy cost savings. The combination of the discontinuation of opioids for patients found to be abusing and misusing opioids coupled with the decrease in pill burden resulting from changes from short-acting to long-acting opioids also resulted in significant savings for VA facilities.
The impact of the OMC on PCP adherence to opioid management guidelines as well as PCP satisfaction with the OMC services was significant. Similarly, Wiedemer and colleagues found significant PCP satisfaction with the ORC.15 The ability to spend more time with patients on other medical problems while allowing the OMC to focus on opioid and pain management was found to be beneficial. Buy-in among PCPs coupled with their concerns for chronic opioid therapy for high-risk patients facilitated the success of the OMC. The commitment of the VASNHS leadership to the OMC and their support for the APRN in leading this initiative were important facilitators in the success of the OMC.
Limitations
Long-term evaluation of the OMC with a larger sample is needed to fully evaluate its impact on decreasing opioid misuse and abuse. This project was limited by a small sample size, although the results are promising. Pharmacy costs, emergency department visits, as well as patient satisfaction, physical and emotional function, and pain levels are outcomes that need to be considered over the long term. Incorporating mental health counseling, cognitive behavior therapy, self-management programs, and group educational sessions have the potential to be important OMC services. The continued success and cost-effectiveness of the OMC can be a potentially significant model for this type of service that can be applied to clinics outside the VA system.
Implications
Possible implications to practice settings that are considering an OMC or ORC include the chance that patients will want to be discharged from such a clinic and return to the PCP for opioid management. Collaborative relationships and communication between PCPs and OMC providers are important to facilitate adherence and consistency with pain care. Collaboration and effective communication can be facilitated by electronic recording and reporting. For example, the VA Computerized Patient Record System can alert PCPs to patient discharges from the OMC along with OMC provider recommendations for patient care. Another challenge for the OMC would be a lack of referrals for patients who are at high risk for opioid abuse or misuse. These challenges can be mitigated by providing inservices, educational flyers, and advertisement promotions regarding OMC services. With the high prevalence of opioid abuse and misuse as well as the subsequent exorbitant health-related costs and deaths associated with opioids, OMCs and ORCs are viable options for improving opioid management in the treatment of patients with nonmalignant chronic pain.
CONCLUSION
The OMC effectively reduced the MED of patients referred to the clinic by 59%. The significant reduction in the opioid dose of patients referred to the OMC resulted from the implementation of evidence-based strategies that were used to identify abuse of prescription opioids, the use of illicit substances that can cause opioid-related complications, and the discovery of doctor shopping, coupled with gradual dose reductions for patients when appropriate. Provider satisfaction and increased use of evidence-based guidelines in opioid management and risk mitigation strategies, such as OPAs, PDMP databases, and UDS were evident. These results suggest that an OMC can be an effective program to help identify abuse and misuse of prescription opioids among high-risk patients and can improve patient safety and provider satisfaction.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the VA Southern Nevada Healthcare System.
Footnotes
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
REFERENCES
- 1.Institute of Medicine (IOM) Relieving pain in America: a blueprint for transforming prevention, care, education, and research. [Accessed August 25, 2016]. http://iom.nationalacademies.org/~/media/Files/Report%20Files/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research/Pain%20Research%202011%20Report%20Brief.pdf. Published June 2011.
- 2.International Narcotics Control Board. Report of the International Narcotics Control Board on the availability of internationally controlled drugs. [Accessed August 25, 2016]. https://www.incb.org/documents/Publications/AnnualReports/AR2010/Supplement-AR10_availability_English.pdf. Published January 2011.
- 3.Manchikanti L, Helm S, II, Fellows B, et al. Opioid epidemic in the United States. Pain Physician. 2012;15(3) suppl:ES9–ES38. [PubMed] [Google Scholar]
- 4.Krebs EE, Ramsey DC, Miloshoff JM, Bair MJ. Primary care monitoring of long-term opioid therapy among veterans with chronic pain. Pain Med. 2011;12(5):740–746. doi: 10.1111/j.1526-4637.2011.01099.x. [DOI] [PubMed] [Google Scholar]
- 5.Von Korff M, Kolodny A, Deyo RA, Chou R. Long-term opioid therapy reconsidered. Ann Intern Med. 2011;155(5):325–328. doi: 10.1059/0003-4819-155-5-201109060-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baser O, Xie L, Mardekian J, Schaaf D, Wang L, Joshi AV. Prevalence of diagnosed opioid abuse and its economic burden in the Veterans’ Health Administration. Pain Pract. 2014;14(5):437–445. doi: 10.1111/papr.12097. [DOI] [PubMed] [Google Scholar]
- 7.Department of Veterans Affairs, Department of Defense. VA/DoD Clinical Practice Guideline for Management of Opioid Therapy for Chronic Pain. Guideline summary. [Accessed August 25, 2016]. http://www.va.gov/painmanagement/docs/cpg_opioidtherapy_summary.pdf. Published May 2010.
- 8.Centers for Disease Control and Prevention (CDC) CDC grand rounds: prescription drug overdoses— a U.S. epidemic. MMWR Morb Mortal Wkly Rep. 2012;61(1):10–13. [PubMed] [Google Scholar]
- 9.Hansen H, Noe CE, Racz GB. Hansen H, Racz GB, Noe CE, editors. The evolving role of opioid treatment in chronic pain management. Pain and Treatment. [Accessed October 5, 2016]. http://www.intechopen.com/books/pain-and-treatment/the-evolving-role-of-opioid-treatment-in-chronic-pain-management. Published July 10, 2014.
- 10.McAuley D. Opioids—equianalgesic dosages. [Accessed October 5, 2016]. http://www.globalrph.com/narcotic.htm. Updated August 5, 2016.
- 11.U.S. Department of Health and Human Services. Addressing prescription drug abuse in the United States: current activities and future opportunities. [Accessed August 25, 2016]. https://www.cdc.gov/drugoverdose/pdf/hhs_prescription_drug_abuse_report_09.2013.pdf.
- 12.Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services, RTI International. Results from the 2010 National survey on drug use and health: summary of national findings. [Accessed October 5, 2016]. http://archive.samhsa.gov/data/NSDUH/2k10NSDUH/2k10Results.htm. Published September 2011.
- 13.Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12(4):657–667. doi: 10.1111/j.1526-4637.2011.01075.x. [DOI] [PubMed] [Google Scholar]
- 14.Federation of State Medical Boards. Model policy on the use of opioid analgesics in the treatment of chronic pain. [Accessed October 5, 2016]. http://www.fsmb.org/Media/Default/PDF/FSMB/Advocacy/pain_policy_july2013.pdf. Published July 2013.
- 15.Wiedemer NL, Harden PS, Arndt IO, Gallagher RM. The opioid renewal clinic: a primary care, managed approach to opioid therapy in chronic pain patients at risk for substance abuse. Pain Med. 2007;8(7):573–584. doi: 10.1111/j.1526-4637.2006.00254.x. [DOI] [PubMed] [Google Scholar]
- 16.Sampson JM, Havens S, Marsh B, Murrhee R. Managing chronic, nonmalignant pain in patients with a substance use disorder. Fed Pract. 2005;22(11):10, 16, 18, 25–26, 29. [Google Scholar]
- 17.Kharlamb V. VISN Opioid cost avoidance plan. New York Harbor VA, New York: Unpublished raw data; 2008. [Google Scholar]