Abstract
Long-acting reversible contraceptives (LARCs) are highly effective at preventing pregnancy but do not protect against sexually transmitted infection (STI). Recent efforts to improve access to intrauterine devices (IUDs) and implants have raised concerns about STI prevention and reduced condom use, particularly among teenagers and young women. We evaluated whether a provider-targeted intervention to increase LARC access negatively impacted dual method use and STI incidence among an at-risk patient population.
We conducted a cluster randomized trial in 40 reproductive health centers across the United States from May 2011 to May 2013. After training providers at 20 intervention sites, we recruited 1500 sexually-active women aged 18–25 years who did not desire pregnancy and followed them for one year. We assessed intervention effects on dual method use, condom use and STI incidence, modeling dual method use with generalized estimating equations and STI incidence with Cox proportional hazard regression models, accounting for clustering.
We found no differences between intervention and control groups in dual method use (14.3% vs. 14.4%, aOR 1.03, 95% CI 0.74–1.44) or condom use (30% vs. 31%, aOR 1.03, 95% CI 0.79–1.35) at last sex at one year. STI incidence was 16.5 per 100 person-years and did not differ between intervention and control groups (aHR 1.20, 95% CI 0.88–1.64).
A provider training intervention to increase LARC access neither compromised condom use nor increased STI incidence among young women. Dual method use was very low overall, highlighting the need to bolster STI prevention efforts among adolescents and young women.
Keywords: Female adolescents, Female contraceptive devices, Intrauterine contraceptive devices, Etonogestrel, Condoms, Sexually transmitted diseases
1. Introduction
Reducing the unintended pregnancy rate in the United States (US) is a national public health goal (U.S. Department of Health and Human Services and Office of Disease Prevention and Health Promotion, 2015; Kost, 2015). Approximately 45% of all pregnancies are unintended, with the highest proportions among teenagers (75%) and women in their early twenties (59%) (Finer and Zolna, 2016). Increasing access to long-acting reversible contraceptives (LARCs) is recommended by the Centers for Disease Control and Prevention (CDC) (Division of Reproductive Health et al., 2013). The American College of Obstetricians and Gynecologists and the American Academy of Pediatrics endorse offering intrauterine devices and implants to teens and young women (American College of Obstetricians and Gynecologists, 2012; Ott and Sucato, 2014), the age group of highest risk of both unintended pregnancy and sexually transmitted infection (STI) (Finer and Zolna, 2016; Satterwhite et al., 2013). Because of these dual risks, ensuring that young women are offered a full range of contraceptive options while maintaining focus on the prevention of STIs is imperative.
Long-acting reversible contraceptives (LARCs), including intrauterine devices (IUDs) and the subdermal implant, have higher effectiveness levels compared to short-term user-dependent methods, with both perfect and typical use failure rates of under 1% (Kulier et al., 2007; O'Brien et al., 2008; French et al., 2004; Power et al., 2007). While LARC method use has historically been low in the US compared to other developed countries, adoption of LARC methods has been increasing over the past decade (Romero et al., 2015; Branum and Jones, 2015); 12% of contracepting women in the US now rely on LARC methods (Daniels et al., 2014) including 4.5% of 15 to 19 year olds and 8.3% of women aged 20 to 24 Finer et al., 2012). Recent research demonstrates successful efforts to increase access to LARC methods, particularly among young women (Winner et al., 2012; Harper et al., 2015; Ricketts et al., 2014); thus, observed increases in LARC adoption are expected to continue.
While increased LARC access has important implications for unintended pregnancy rates, concerns have been raised that dual method use, that is condom use with a hormonal method, copper intrauterine device or sterilization, may decrease in the context of increasing LARC use (Steiner et al., 2016). Dual method use remains a critical reproductive health strategy, especially in youth populations for concurrent protection against pregnancy and STI. Nationally-representative data show that 50% of incident infections occur among individuals aged 15 to 24 years (Satterwhite et al., 2013). CDC guidelines for primary prevention of STIs among this age group include vaccination and health care provider counseling on evidence-based risk-reduction behaviors including abstinence, consistent and correct condom use and reduction in number of sex partners (Centers for Disease Control and Prevention, 2015).
Previous research suggests that concurrent condom use may be lower among LARC users compared to users of other contraceptive methods (Darney et al., 1999; Roye, 1998; Cushman et al., 1998; Pazol et al., 2010; Santelli et al., 1995). However, a difference in dual use by LARC users is not consistent across all prior studies (Polaneczky et al., 1994). A recent cross-sectional analysis of adolescents in the U.S. found lower condom use among LARC users, as well as injectable, patch and vaginal ring users, as compared to oral contraceptive users, and the authors questioned what might transpire with a LARC scale-up in the US (Steiner et al., 2016). Research with randomized designs and current contraceptive methods is scarce, with only one recent intervention trial on the subdermal implant showing no difference in condom use assessed via prostate-specific antigen, a biological marker of recent semen exposure, among women using the implant compared to women using another contraceptive method (Rattray et al., 2015). However, this intervention study was not US-based, included women of all reproductive ages, with short-term follow-up (3 months), and did not evaluate STI incidence. A gap exists in the literature on concurrent condom use among high-risk young US populations within the context of interventions to increase LARC access.
We conducted a cluster randomized study across 40 clinics in the US evaluating a provider-targeted LARC training intervention to improve access to IUDs and implants among young women (n = 1500). In primary analyses, the intervention successfully reduced unintended pregnancy in family planning clinics (Harper et al., 2015). In this analysis, we evaluated the impact of the intervention on two secondary outcomes: dual method and condom use among adolescents and young women. We tested the hypothesis that the intervention to increase LARC access would lead to lower dual method use. Strengthening the evidence base on any unintended consequences of LARC method accessibility can help guide policy and clinical practice that prioritizes concurrent reductions in unintended pregnancy and STI acquisition.
2. Methods
The current study is an analysis of a cluster randomized trial of an educational intervention for clinic staff to increase access to LARC methods among young women. Randomization was conducted by clinic, and allocation was concealed until study initiation. The study design and primary results are described in detail elsewhere (Harper et al., 2015), and the study was registered at ClinicalTrials.gov (NCT01360216). Briefly, the trial was conducted at 40 Planned Parenthood health centers across the US that met the following criteria: 400 or more annual patients, patient method use <20% IUDs and implants, no specific LARC intervention program and no shared staff with another study clinic. Study clinics serve largely young and low-income women from diverse racial and ethnic groups. The intervention consisted of a multifaceted half-day training to improve providers' LARC method-specific knowledge, and patient-centered counseling and IUD placement skills. The provider training on implant insertion was conducted separately with the manufacturer. The LARC training curriculum noted that these methods were effective protection from pregnancy but not STIs and that condoms were necessary for STI prevention. All staff at intervention clinics (n = 20) underwent training, whereas staff at control clinics (n = 20) followed standard care.
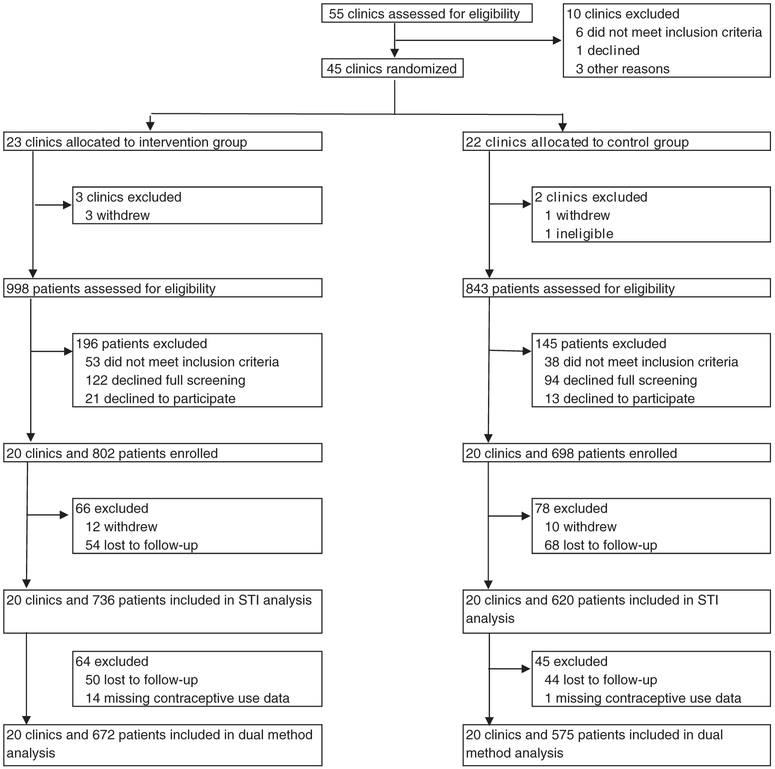
After the intervention, women were invited to participate in the study upon presentation to a study clinic if aged 18–25 years, at risk of pregnancy (sexually active within the prior 3 months and not pregnant), received contraceptive counseling on the day of enrollment, and did not desire pregnancy within the next 12 months. The study was conducted from May 2011 to May 2013. A total of 1500 women participated in the study, with 802 in intervention and 698 in control clinics (Fig. 1). Self-administered questionnaires were completed by participants at baseline, 3 months, 6 months, 9 months and 12 months. Questions asked about contraceptive methods used, pregnancies and new diagnoses of sexually transmitted infections. We collected additional participant data from medical record review over the 12-month study period including contraception and STIs. Baseline characteristics of clinics and participants were similar across study arm. The study was approved by the University of California, San Francisco Committee on Human Research and the Allendale Investigational Review Board.
Fig. 1.
Trial and analytic profile.
2.1. Measures
We evaluated the following study outcomes: dual method use at last sex at 12-month follow-up, condom use at last sex at 12-month follow-up, and STI incidence during the study. We also assessed participants' baseline report of whether providers discussed condoms during the contraceptive counseling visit. Participants reported all contraceptive methods used at last sexual intercourse on the final 12-month survey. Dual method use was defined as condom use in conjunction with any hormonal contraception (hormonal IUD, implant, Depo-Provera injection, pill, vaginal ring or transdermal patch), copper IUD or sterilization.1 IUDs and the implant were considered LARC methods, and the injectable, transdermal patch, vaginal ring and oral contraceptives were considered short acting reversible contraceptive (SARC) methods. STI diagnosis was captured via self-report on the quarterly surveys (i.e., “Since the last survey, have you been told by a doctor or nurse that you have any of the following STDs?”: “chlamydia”, “herpes”, “HPV2 or genital warts”, “trich”, “gonorrhea”, “syphilis”, “hepatitis B, “HIV/AIDS”, “other”) and medical record data on diagnosis or treatment (i.e., where study participants sought clinic care for an STI during the 12-month study).
Baseline covariates included age, race/ethnicity (self-identified white, Latina, black or other), insurance type (private, Medicaid/state, none or don't know), STI history (yes vs no/not sure), parity (parous vs nulliparous), primary partner (yes vs casual/no partner), and practice setting (family planning vs abortion).
2.2. Analyses
Analyses followed an intent-to-treat approach with the data analyst blinded to study arm. Our analysis population for the dual use and condom outcomes comprised all participants who completed the 12-month survey and responded to recent contraceptive use questions (n = 1247). For the STI outcome, the survival analysis population was comprised of the 1356 women contributing study follow-up data in the 3, 6, 9 or 12-month surveys. The primary analytic samples for dual method use (n = 1247) and STI outcomes (n = 1356) were subsets of the full cohort of 1500 women (83% and 90.4% respectively) due to study attrition, but were similar with regard to study arm, age, race/ethnicity, marital status, educational attainment, insurance type, parity, contraceptive method at baseline, pregnancy intention, and primary partner. To estimate the effect of the intervention on dual method use and condom use, we used logistic regression models with generalized estimating equations and robust standard errors to account for the clustered study design. We evaluated the relationship between provider discussion of condom use and two study outcomes, dual method use and condom use at 12-month follow-up, similarly. We compared dual method use across two categories of contraceptive users, defined by reported method use at 12-months, LARC users and SARC users, accounting for study arm and other covariates, including having a primary partner (n = 765). This exploratory analysis was conducted to investigate rationale for dual method use.
We estimated rates of sexually transmitted infection with life table analysis and Kaplan-Meier survival estimates. Women who contributed observation time to the survival analysis were censored when diagnosed with an STI, lost to follow-up, or when they exited the study. Incident STI diagnoses from survey data were calculated to have occurred at the mid-point between completion dates of the index survey (survey where STI reported) and the prior survey (last completed survey). The intervention effect on time to first STI was estimated using Cox proportional hazard regression models with robust variance estimates to account for clustering by clinic. Schoenfeld residuals were estimated to confirm that the data met the proportional hazards assumption. Analyses were conducted using unadjusted models and models accounting for covariates age, race/ethnicity, insurance type, primary partner, STI history, parity and setting type. All analyses were conducted in Stata v14 (StataCorp, College Station, TX). Differences were considered statistically significant at p < 0.05.
3. Results
3.1. Baseline characteristics
At baseline, participant characteristics were similar between intervention and control clinics (Table 1). Participants were on average 21.5 years old. Half were white (49%), 27% Latina and 15% black. Eighty-one percent reported having a primary partner at baseline. Condom use at last sex was 30% in intervention and 32% in control. Reported dual method use at last sex was low at 10% in intervention and 13% in control. Over one-quarter of study participants reported a history of any STI: 26% in intervention and 27% in control.
Table 1.
Participant characteristics at study enrollment by study arm.
| Intervention |
Control |
Total |
||||
|---|---|---|---|---|---|---|
| n = 736 |
n = 620 |
n = 1356 |
||||
| n | % | n | % | n | % | |
| Agea | 21.5 (2.3) | 21.5 (2.1) | 21.5 (2.2) | |||
| Race/ethnicity | ||||||
| White | 365 | 49.6 | 304 | 49.0 | 669 | 49.3 |
| Latina | 182 | 24.7 | 185 | 29.8 | 367 | 27.1 |
| Black | 108 | 14.7 | 98 | 15.8 | 206 | 15.2 |
| Other | 81 | 11.0 | 33 | 5.3 | 114 | 8.4 |
| Currently married (n = 1344) | 37 | 5.1 | 41 | 6.7 | 78 | 5.8 |
| Educational attainment (n = 1347) | ||||||
| High school or less | 522 | 71.4 | 453 | 73.5 | 975 | 72.4 |
| Some college | 105 | 14.4 | 85 | 13.8 | 190 | 14.1 |
| College degree | 104 | 14.2 | 78 | 12.7 | 182 | 13.5 |
| Health insurance type | ||||||
| Private | 226 | 30.7 | 185 | 29.8 | 411 | 30.3 |
| Medicaid/state | 199 | 27.0 | 165 | 26.6 | 364 | 26.8 |
| None | 277 | 37.6 | 238 | 38.4 | 515 | 38.0 |
| Don't know | 34 | 4.6 | 32 | 5.2 | 66 | 4.9 |
| Nulliparous (n = 1349) | 547 | 74.7 | 423 | 68.6 | 970 | 71.9 |
| Primary partner (n = 1335) | 588 | 80.8 | 498 | 82.0 | 1086 | 81.4 |
| Most effective contraceptive used in past 3 months (n = 1349) | ||||||
| LARC | 30 | 4.1 | 27 | 4.4 | 57 | 4.2 |
| Depo | 53 | 7.3 | 44 | 7.1 | 97 | 7.2 |
| Pill, vaginal ring or patch | 307 | 42.1 | 230 | 37.2 | 537 | 39.8 |
| Condom | 185 | 25.3 | 181 | 29.2 | 366 | 27.1 |
| None | 155 | 21.2 | 137 | 22.1 | 292 | 21.7 |
| Condom use at last sex (n = 1351) | 220 | 30.0 | 205 | 32.2 | 425 | 31.5 |
| Dual method use at last sex (n = 1346) | 73 | 10.0 | 77 | 12.5 | 150 | 11.1 |
| History of any STI (n = 1307) | 188 | 26.4 | 160 | 26.9 | 348 | 26.6 |
| Provider discussion of condoms (n = 1349) | 315 | 43.0 | 299 | 48.5 | 614 | 45.5 |
Notes: LARC (long-acting reversible contraceptive), STI (sexually transmitted infection).
No significant differences by study arm.
Mean (SD).
3.2. Dual method and condom outcomes at 12-months
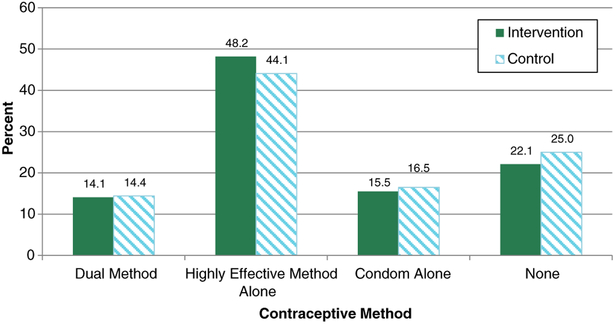
Approximately 14% of participants in both intervention and control groups reported using dual protection at last sex at 12 months (Fig. 2). Results from logistic regression analysis (Table 2) showed no difference in dual method use between the intervention versus control groups in our unadjusted (OR 0.99, 95% CI 0.71–1.37) and multivariable analyses (aOR 1.03, 95% CI 0.74–1.44). Condom use at last sex was also equivalent between study groups; nearly one-third of study participants reported having used a condom at last sex (30% intervention, 31% control), and the odds of condom use were similar by intervention group in unadjusted (OR 0.95, 95% CI 0.72–1.27) and adjusted analyses (aOR 1.03,95% CI 0.79–1.35).
Fig. 2.
Contraceptive method use at last sex at 12 months, by study arm, n = 1247. Notes: Highly effective method alone includes LARC, hormonal methods, and sterilization. No significant differences by study arm.
Table 2.
Intervention effect on dual method use and condom use at 12 months, n = 1247.
| Dual method use |
Condom use |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted |
Adjusteda |
Unadjusted |
Adjusteda |
|||||
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Intervention vs. control | 0.99 (0.71–1.37) | 0.939 | 1.03 (0.74–1.44) | 0.856 | 0.95 (0.72–1.27) | 0.752 | 1.03 (0.79–1.35) | 0.821 |
Control variables: age, race/ethnicity, insurance, primary partner, STI history, parity, and practice setting.
Fewer than half of participants reported that their provider discussed condom use with them at their baseline contraceptive counseling visit: 43% in intervention and 49% in control (Table 1). There was no significant intervention effect on provider discussion of condoms in unadjusted (OR 0.81,95% CI 0.58–1.14; Table 2) and adjusted analyses (aOR 0.79, 95% CI 0.56–1.10). Provider discussion of condoms did not vary by participant STI history (aOR 0.99, 95% CI 0.74–1.31). However, women who reported that their providers had discussed condom use with them at baseline had 61% higher odds of reporting dual method use at last sex at 12-month follow-up (aOR 1.61, 95% CI 1.11–2.35) and 71% higher odds of reporting condom use at last sex (aOR 1.71, 95% CI 1.24–2.35). (data not shown).
We also explored dual use among LARC users compared to SARC users (not shown). Dual method use was reported by 15% of IUD and implant users compared to 27% of SARC users. Compared to LARC users, SARC users had greater odds of dual method use (aOR 2.60, 95% CI 1.56–4.32). Additionally, having a primary partner was significantly associated with reduced dual method use; individuals reporting a primary partner had 52% lower odds of dual method use (aOR 0.48, 95% CI 0.30–0.76).
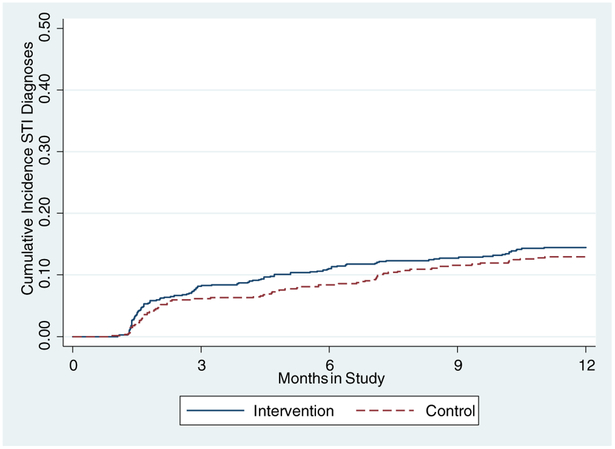
3.3. Incidence of sexually transmitted infection
During the 12-month follow-up period, 184 individuals were diagnosed with at least one STI (15.6 per 100 person-years). The incidence rate was 16.5 per 100 PY in the intervention group and 14.5 per 100 PY in the control group. Overall, the most common STIs diagnosed were chlamydia (6.9%), human papillomavirus (HPV; 4.4%) and herpes simplex virus (HSV; 2.1%) (Table 3). STI incidence did not differ significantly between the intervention and control groups in unadjusted (HR 1.14, 95% CI 0.84–1.54) (Table 4) or adjusted models (aHR 1.20, 95% CI 0.88–1.64; Fig. 3).
Table 3.
Incident sexually transmitted infections by study arm.
| Intervention |
Control |
Overall |
||||
|---|---|---|---|---|---|---|
| n = 736 |
n = 620 |
n = 1356 |
||||
| n | % | n | % | n | % | |
| Any STI | 105 | 13.1 | 79 | 11.3 | 184 | 13.6 |
| Chlamydia | 54 | 6.7 | 40 | 5.7 | 94 | 6.9 |
| Gonorrhea | 9 | 1.2 | 6 | 1.0 | 15 | 1.1 |
| HIV | 2 | 0.3 | 0 | 0.0 | 2 | 0.2 |
| Syphilis | 0 | 0.0 | 1 | 0.2 | 1 | 0.1 |
| Trichomoniasis | 9 | 1.2 | 4 | 0.7 | 13 | 1.0 |
| HSV | 16 | 2.2 | 12 | 1.9 | 28 | 2.1 |
| HPV | 32 | 4.4 | 27 | 4.4 | 59 | 4.4 |
Notes: Totals by STI do not sum to 100% as some individuals were concurrently diagnosed with multiple STIs.
STI (sexually transmitted infection), HIV (human immunodeficiency virus), HSV (herpes simplex virus), HPV (human papillomavirus).
Table 4.
Intervention effect on STI incidence, n = 1356.
| Unadjusted |
Adjusteda |
|||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | |
| Intervention vs. control | 1.14 | (0.84–1.54) | 0.398 | 1.20 | (0.88–1.64) | 0.242 |
Control variables: age, race/ethnicity, insurance, primary partner, STI history, parity, and practice setting.
Fig. 3.
Sexually transmitted infection incidence (12 month) by study arm, n = 1356.
4. Discussion
We used data from a cluster randomized trial to examine whether a provider intervention to integrate IUDs and implants into contraceptive care would result in lower dual method use and increased STI incidence among contraceptive clients. These results showed that the intervention to increase provider knowledge and skills regarding long-acting contraceptives did not inadvertently compromise condom use nor increase STI incidence among this group of young women 18 to 25 years old. This is the first large study across the US that has examined dual method use and STI incidence within a randomized experiment to increase access to long-acting contraceptives.
Prior literature on concurrent condom use with adoption of LARC methods has largely found lower condom usage among women using LARC methods when compared to women using other methods. Nationally-representative cross-sectional studies, as well as prospective analyses on smaller cohorts in narrow geographical or clinical settings, have shown that contraceptive implant and IUD users had low condom use, both overall and when compared to other contraceptive method users (Steiner et al., 2016; Darney et al., 1999; Cushman et al., 1998; Pazol et al., 2010). Most of these studies were not randomized, so other factors affecting method choice may have contributed to lower condom use such as having a primary sexual partner. Our analysis also identified oral contraceptive, injectable, patch and ring users as having greater odds of dual method use. Additionally, the results highlighted the important role of relationship status; women reporting a primary sexual partner at baseline had an approximately 50% reduced odds of dual method use. These results may be indicative of the reasons different women use different methods; women using highly effective LARC methods only need to use condoms for STI prevention whereas women using SARCs may use them both for STI prevention and additional pregnancy prevention. Similarly, women in primary relationships might have a lower perceived risk of STI and thus be less likely to use a condom.
Consistent with our overall findings, a few other studies have also found that access to LARC methods did not compromise dual use. One cohort and one cross-sectional study among urban adolescents found no difference in dual method use among implant or IUD users compared to users of other contraceptive methods (Roye, 1998; Polaneczky et al., 1994). Also similar to our results, a recent RCT of immediate versus delayed levonorgestrel implant insertion among Jamaican women attending maternal/child health and family planning clinics found no difference in the detection of prostate-specific antigen across intervention groups through 3 months post-enrollment (Rattray et al., 2015). However, these studies were small and the study populations were from one clinic or geographic area.
Overall, we found very low dual method use across both intervention and control arms (14%) in a study population at high risk of both unintended pregnancy and STI acquisition in 40 sites throughout the US. This finding is consistent with national data; Eisenberg et al. report that 23% of a representative sample of US women under 20 years and 12% of women aged 21 to 25 indicated dual method use at last sex within the 12 months preceding the survey, with steep declines with increased age (Eisenberg et al., 2012). A review of the literature on dual use of LARCs and condoms shows that age and relationship factors, such as steady or primary partner, are negatively associated with dual method use (Williams and Fortenberry, 2013).
Within our data, individuals who were counseled on condom use at baseline had higher odds of condom use at last sex at 12-month follow-up, similar to previous research on long-acting contraceptives and condom counseling (Cushman et al., 1998). This finding highlights the importance of counseling specifically on dual method use.
Our results showed that the intervention did not adversely affect the incidence of sexually transmitted infections. Overall, the proportion of participants who developed at least one incident STI in our study, 13.6%, was lower than that reported by Polaneczky et al. (1994), at 42% of implant users and 36% of oral contraceptive users, and similar to rates reported by Darney et al., at 15% of implant users and 10% of oral contraceptive users (Darney et al., 1999). Polaneczky et al. found that condom use overall was quite low at 19% among Norplant users and 16% of other contraceptive method users, which may explain the higher STI incidence compared to our study (Polaneczky et al., 1994). Darney et al. observed a statistically significant reduction in condom use among LARC users over the 2-year follow-up, whereas no reduction was observed among hormonal and other method users (Darney et al., 1999). At 2-year follow-up, 28% of LARC users indicated condom use at last sex compared to 59% and 56% of oral contraceptive and condom users, respectively. However, neither of these studies were randomized intervention trials.
While the current findings are from a large cluster-randomized trial, which represents a robust intervention design, and we had high follow-up, a number of limitations affect the interpretation of our results. First, the study was conducted within a network of specialized reproductive health clinics serving a young, low-income and diverse patient population; thus, our results may not be generalizable to different patient and provider contexts. Second, while we supplemented our survey data collection with medical record abstraction, our two primary outcomes for this analysis, dual method use and STI incidence, were largely self-reported. The implication of any potential bias would likely be overestimation of dual method use and underestimation of STI (where not captured by clinic data) due to social desirability bias; however, we have no reason to believe that any such bias would have differentially impacted intervention versus control participants. Finally, sample size for our trial was calculated to estimate the primary outcomes of LARC uptake and pregnancy prevention (Harper et al., 2015) whereas the current analysis focuses on secondary outcomes of the trial; the sample size is sufficiently large for hypothesis testing for dual use, but our STI findings should be interpreted cautiously as a larger sample would be needed for a definitive analysis (Schumi and Wittes, 2011).
5. Conclusion
A provider intervention to integrate IUDs and implants into contraceptive care did not jeopardize STI prevention among study participants; however, findings revealed a very low level of dual method use. Currently the condom is the only available multipurpose prevention technology (MPT). While latex condoms are highly effective at preventing HIV infection and some STIs, including gonorrhea, chlamydia and trichomoniasis (Holmes et al., 2004), consistency of condom use among adolescents is generally low (Martinez et al., 2011). We found provider counseling to be associated with higher condom and dual method use; however, the large majority of study participants did not report having used a condom at last sex at follow-up. Contraceptive interventions can be an opportunity to promote dual use. Other topical and barrier MPTs in development include an intravaginal ring, vaginal and rectal gels, films and tablets, and diaphragms with drugs (CAMI Health/Public Health Institute, 2015). Further research and development efforts targeting MPTs may prove to benefit young at-risk populations reluctant to use dual methods or condoms.
Acknowledgments
The study was funded by the William and Flora Hewlett Foundation (#2010-5442). Units for intervention training in intrauterine device insertion were provided by Teva Pharmaceuticals Industries and Bayer HealthCare. We thank the UCSF Bixby Center research team for data collection and management. We thank Johanna Morfesis and Planned Parenthood investigators and research coordinators at these affiliates: Central and Greater Northern New Jersey; Columbia Willamette; Great Northwest and Hawaiian Islands; Greater Ohio; Greater Washington and North Idaho; Mar Monte; Mid & South Michigan; Minnesota, North Dakota, South Dakota; Mt. Baker; Northern California; Pacific Southwest; Pasadena and San Gabriel Valley; Rocky Mountains; South Atlantic; Southeastern Pennsylvania; Southern New England; and Southwest and Central Florida. All these contributors received compensation. We thank Dr. Charles McCulloch for design expertise. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of Planned Parenthood Federation of America, Inc.
Footnotes
Conflict of interest
The authors declare that there is no conflict of interest.
Sensitivity analyses were carried out including report of emergency contraceptive pills and concurrent condom use as dual use; results were consistent.
HPV: human papillomavirus.
References
- American College of Obstetricians and Gynecologists, 2012. Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstet. Gynecol 120 (4), 983–988. [DOI] [PubMed] [Google Scholar]
- Branum AM, Jones J, 2015. Trends in Long-Acting Reversible Contraception Use Among U.S. Women Aged 15–44 NCHS Data Brief, No 188. National Center for Health Statistics, Hyattsville, MD. [PubMed] [Google Scholar]
- CAMI Health/Public Health Institute, 2015. IMPT for reproductive health. MPT Product Development Database. Database of MPT products currently available as well as MPT products in active development [cited 2016 March 16]. [Google Scholar]
- Centers for Disease Control and Prevention, 2015. STDs in adolescents and young adults. [cited 2015 December 11]; Available from:. http://www.cdc.gov/std/stats14/adol.htm.
- Cushman LF, Romero D, Kalmuss D, Davidson AR, Heartwell S, Rulin M, 1998. Condom use among women choosing long-term hormonal contraception. Fam. Plan. Perspect 30 (5), 240–243. [PubMed] [Google Scholar]
- Daniels K, Daugherty J, Jones J, 2014. Current contraceptive status among women aged 15–44: United States, 2011–2013. NCHS Data Brief (173), 1–8. [PubMed] [Google Scholar]
- Darney PD, Callegari LS, Swift A, Atkinson ES, Robert AM, 1999. Condom practices of urban teens using Norplant contraceptive implants, oral contraceptives, and condoms for contraception. Am. J. Obstet. Gynecol. 180 (4), 929–937. [DOI] [PubMed] [Google Scholar]
- Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention (CDC), 2013. U.S. selected practice recommendations for contraceptive use, 2013: adapted from the World Health Organization selected practice recommendations for contraceptive use MMWR Recomm Rep, 2nd edition. Vol. 62(RR-05), pp. 1–60. [PubMed] [Google Scholar]
- Eisenberg DL, Allsworth JE, Zhao Q, Peipert JF, 2012. Correlates of dual-method contraceptive use: an analysis of the National Survey of Family Growth (2006–2008). Infect. Dis. Obstet. Gynecol 2012, 717163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Zolna MR, 2016. Declines in unintended pregnancy in the United States, 2008–2011. N. Engl. J. Med 374 (9), 843–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Jerman J, Kavanaugh ML, 2012. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertil. Steril 98 (4), 893–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French R, Van Vliet H, Cowan F, Mansour D, Morris S, Hughes D, et al. , 2004. Hormonally impregnated intrauterine systems (IUSs) versus other forms of reversible contraceptives as effective methods of preventing pregnancy. Cochrane Database Syst. Rev 3, CD001776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper CC, Rocca CH, Thompson KM, Morfesis J, Goodman S, Darney PD, et al. , 2015. Reductions in pregnancy rates in the USA with long-acting reversible contraception: a cluster randomised trial. Lancet 386 (9993), 562–568. [DOI] [PubMed] [Google Scholar]
- Holmes KK, Levine R, Weaver M, 2004. Effectiveness of condoms in preventing sexually transmitted infections. Bull. World Health Organ 82 (6), 454–61. [PMC free article] [PubMed] [Google Scholar]
- Kost K, 2015. Unintended Pregnancy Rates at the State Level: Estimates for 2011 and Trends Since 2002. Guttmacher Institute, New York. [Google Scholar]
- Kulier R, O’Brien PA, Helmerhorst FM, Usher-Patel M, D'Arcangues C, 2007. Copper containing, framed intra-uterine devices for contraception. Cochrane Database Syst. Rev 4, CD005347. [DOI] [PubMed] [Google Scholar]
- Martinez G, Copen C, Abma J, 2011. Teenagers in the United States: Sexual Activity, Contraceptive Use, and Childbearing, 2006–2010 National Survey of Family Growth National Center for Health Statistics, Washington, DC. [PubMed] [Google Scholar]
- O'Brien PA, Kulier R, Helmerhorst FM, Usher-Patel M, d'Arcangues C, 2008. Copper-containing, framed intrauterine devices for contraception: a systematic review of randomized controlled trials. Contraception 77 (5), 318–327. [DOI] [PubMed] [Google Scholar]
- Ott MA, Sucato GS, 2014. Contraception for adolescents. Pediatrics 134 (4), e1257–e1281. [DOI] [PubMed] [Google Scholar]
- Pazol K, Kramer MR, Hogue CJ, 2010. Condoms for dual protection: patterns of use with highly effective contraceptive methods. Public Health Rep. 125 (2), 208–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polaneczky M, Slap G, Forke C, Rappaport A, Sondheimer S, 1994. The use of levonorgestrel implants (Norplant) for contraception in adolescent mothers. N. Engl. J. Med 331 (18), 1201–1206. [DOI] [PubMed] [Google Scholar]
- Power J, French R, Cowan F, 2007. Subdermal implantable contraceptives versus other forms of reversible contraceptives or other implants as effective methods of preventing pregnancy. Cochrane Database Syst. Rev 3, CD001326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rattray C, Wiener J, Legardy-Williams J, Costenbader E, Pazol K, Medley-Singh N, et al. , 2015. Effects of initiating a contraceptive implant on subsequent condom use: a randomized controlled trial. Contraception. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricketts S, Klinger G, Schwalberg R, 2014. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect. Sex. Reprod. Health 46 (3), 125–132. [DOI] [PubMed] [Google Scholar]
- Romero L, Pazol K, Warner L, Gavin L, Moskosky S, Besera G, et al. , 2015. Vital signs: trends in use of long-acting reversible contraception among teens aged 15–19 years seeking contraceptive services-United States, 2005–2013. MMWR Morb. Mortal. Wkly Rep 64 (13), 363–369. [PMC free article] [PubMed] [Google Scholar]
- Roye CF, 1998. Condom use by Hispanic and African-American adolescent girls who use hormonal contraception. J. Adolesc. Health 23 (4), 205–211. [DOI] [PubMed] [Google Scholar]
- Santelli JS, Davis M, Celentano DD, Crump AD, Burwell LG, 1995. Combined use of condoms with other contraceptive methods among inner-city Baltimore women. Fam. Plan. Perspect 27 (2), 74–78. [PubMed] [Google Scholar]
- Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC, et al. , 2013. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex. Transm. Dis 40 (3), 187–193. [DOI] [PubMed] [Google Scholar]
- Schumi J, Wittes JT, 2011. Through the looking glass: understanding non-inferiority. Trials 12, 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiner RJ, Liddon N, Swartzendruber AL, Rasberry CN, Sales JM, 2016. Long-acting reversible contraception and condom use among female US high school students: implications for sexually transmitted infection prevention. JAMA Pediatr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion, 2015. s. Healthy People:2020 [cited 2015 November 1]; Available from:. http://www.healthypeople.gov/2020/Leading-Health-Indicators.
- Williams RL, Fortenberry JD, 2013. Dual use of long-acting reversible contraceptives and condoms among adolescents. J. Adolesc. Health 52 (4 Suppl), S29–S34. [DOI] [PubMed] [Google Scholar]
- Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, et al. , 2012. Effectiveness of long-acting reversible contraception. N. Engl. J. Med 366 (21), 1998–2007. [DOI] [PubMed] [Google Scholar]