Key Points
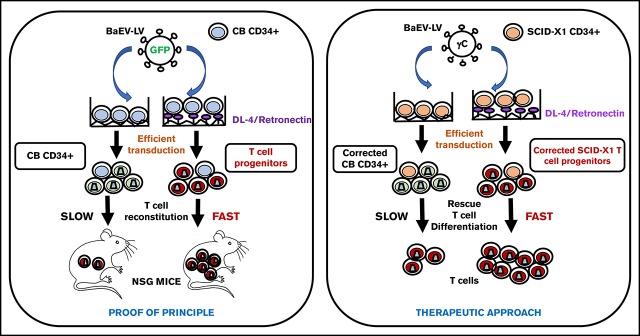
BaEV-LVs efficiently transduce progenitor T cells, providing accelerated T-cell reconstitution in vivo.
BaEV-LVs efficiently correct human SCID-X1 progenitor T cells.
Abstract
T cells represent a valuable tool for treating cancers and infectious and inherited diseases; however, they are mainly short-lived in vivo. T-cell therapies would strongly benefit from gene transfer into long-lived persisting naive T cells or T-cell progenitors. Here we demonstrate that baboon envelope glycoprotein pseudotyped lentiviral vectors (BaEV-LVs) far outperformed other LV pseudotypes for transduction of naive adult and fetal interleukin-7–stimulated T cells. Remarkably, BaEV-LVs efficiently transduced thymocytes and T-cell progenitors generated by culture of CD34+ cells on Delta-like ligand 4 (Dll4). Upon NOD/SCIDγC−/− engraftment, high transduction levels (80%-90%) were maintained in all T-cell subpopulations. Moreover, T-cell lineage reconstitution was accelerated in NOD/SCIDγC−/− recipients after T-cell progenitor injection compared with hematopoietic stem cell transplantation. Furthermore, γC-encoding BaEV-LVs very efficiently transduced Dll4-generated T-cell precursors from a patient with X-linked severe combined immunodeficiency (SCID-X1), which fully rescued T-cell development in vitro. These results indicate that BaEV-LVs are valuable tools for the genetic modification of naive T cells, which are important targets for gene therapy. Moreover, they allowed for the generation of gene-corrected T-cell progenitors that rescued SCID-X1 T-cell development in vitro. Ultimately, the coinjection of LV-corrected T-cell progenitors and hematopoietic stem cells might accelerate T-cell reconstitution in immunodeficient patients.
Visual Abstract
Introduction
Gene transfer into T lymphocytes is a crucial step in the development of therapeutic strategies for the treatment of genetic dysfunctions of the hematopoietic system, such as severe combined immunodeficiency (SCID1,2) as well as cancers3,4 and acquired diseases.5 More than 15 years ago, children suffering from monogenetic diseases such as adenosine deaminase SCID (ADA-SCID) and SCID-X1were successfully treated with T-cell gene therapy (ADA-SCID)6 or hematopoietic stem cells (HSCs) (SCID-X16,7; ADA-SCID8). T-cell gene therapy might also become an important treatment option for HIV-infected patients because several new combinatorial strategies have been proposed.9-11 To avoid graft-versus-host disease in HSC transplantation, retroviral marking of allogenic T cells with a suicide gene is performed, and these T cells can then be eliminated by administering a specific drug.3,12-14 A promising anticancer strategy is based on engineered T cells that express a tumor-specific T-cell receptor (TCR) or a chimeric antigen receptor (CAR).15-17 Ongoing clinical trials have described durable rejection of previously refractory B-cell malignancies in patients after CD19-directed CAR therapy,4,18-21 with a complete response rate as high as 86% in patients with leukemia. The successful application of CARs directed to other molecular targets has broadened the indications for this approach to other cancers.22-28
The clinical efficacy of adoptively transferred T lymphocytes is correlated with their ability to persist in vivo,29 which is correlated with a less differentiated T-cell phenotype.15,17,30 Naive T cells are especially important as gene therapy target cells because they maintain the capacity to respond to novel antigens and can generate the entire spectrum of immunologic memory.31,32 Indeed, upon infusion, less differentiated naive and central memory T cells display superior proliferation, persistence, and antitumor responses when compared with the effector memory subset.15,31,33 Accordingly, naive T cells might constitute the best T-cell target population for gene therapy. Human cord blood (CB) T cells are mostly naive and differ from their adult naive counterparts in that the former represent mainly recent thymocyte emigrants,33,34 which express CD31+.35,36 Naive CB T cells proliferate significantly more than their adult counterparts in response to interleukin-7 (IL-7).37,38 Interestingly, IL-7 maintains naive CD31+ CD4+ T cells during adult life.39 These characteristics prompted the development of the first CAR-based CB T-cell strategies for the treatment of cancer and infectious diseases.16,40-42
Other even more immature targets for gene modification are the T-cell progenitors, which are normally found in the thymus and are important for treatment of autoimmune disorders.43-46 Early T-cell development depends on the interaction between thymocytes and Notch ligand signaling pathways. Delta-like ligand 4 (Dll4) has been identified as the essential Notch1 activator in the T-cell engagement of HSCs.47-49 We have previously demonstrated that T-cell progenitors can be generated from CD34+ hematopoietic stem and progenitor cells (HSPCs) in a feeder-cell–free culture system based on Dll4.50,51 They displayed the phenotypic and molecular signatures of immature thymic precursors and were capable of differentiating into T cells and accelerating T-cell reconstitution in vivo compared with HSPCs.50
It is now generally accepted that resting T cells cannot readily be transduced by classical vesicular stomatitis virus G (VSV-G) protein pseudotyped lentiviral vectors (LVs)52-54 because of the absence of the VSV receptor.55 The latter is upregulated by TCR stimulation and is correlated with high-level transduction by VSV-G-LVs.55 However, TCR stimulation of T cells alters their half-life and immune competence and is associated with the loss of naive T-cell subsets and a skewed TCR repertoire.56,57 Exposure of T cells to cytokines such as IL-7 renders them permissive to transduction by VSV-G-LVs,52,54,58-60 preserving a functional T-cell repertoire without skewing the T-cell populations.38,54,58 However, VSV-G-LVs do not allow high-level transduction of IL-7–stimulated naive T cells.52,54,59 We previously pseudotyped LVs with measles virus envelope glycoproteins (GPs) H and F (H/F-LVs). They allowed, for the first time, efficient transduction of quiescent memory and naive human T (hT) cells and B cells, with conservation of the T- and B-cell phenotypes.61-63 Furthermore, we engineered LVs that displayed the feline retrovirus GP RD114, which conferred efficient transduction of hT cells upon TCR stimulation.64 The baboon envelope retrovirus (BaEV) belongs to the same betaretrovirus family as RD114. Both viruses use the neutral alanine/serine/cysteine amino acid transporter-2 (ASCT-2) present on T cells.65,66 Interestingly, BaEV-LVs also bind to ASCT-167 and far outperform VSV-G- and RD114-LVs for human HSC and B-cell transduction.68-70 Therefore, we hypothesized that BaEV-LVs might be excellent candidates for gene delivery into naive hT cells and T-cell progenitors.
Materials and methods
Plasmids
RD114TR, BaEVTR, BaEVRless, and HΔ24 and FΔ30 envelope GPs were previously described.64,69,71 All chimeric envelope GPs were expressed in the phCMV-G expression plasmid.72 The SIN-HIVSFFVGFP vector was described previously.71
The native IL-2RγC complementary DNA (cDNA) fragment from pRRL.PPT.SF91.IL2RGpre (a gift from A. Shambach, Medizinische Hochschule Hannover, Hannover, Germany) was cloned into the pHEF1-MCS-IRES-GFP vector by ligation of BamHI-SalI digested fragments.
Self-inactivating HIV-1–derived vectors encoding green fluorescent protein (GFP) or γC under the control of an SFFV or EF1α promoter, respectively, were generated by transfection of 293T cells as described in detail elsewhere.71 Titration of LVs69,71 is described in detail elsewhere, and isolation of human primary T cells, thymocytes, and CD34+ cells is described in the supplemental Methods.
Transduction of primary cells
Peripheral blood (PB) T lymphocytes were prestimulated for 24 hours with anti-human CD3 (hCD3)/anti-hCD28 (1 μg/mL, BD Pharmingen) in the presence of hIL-2 (1 ng/mL), and CB and PB T cells were prestimulated with recombinant human IL-7 (rhIL-7; 10 ng/mL; BD Biosciences) for 2 and 3 days, respectively.54
Next, 5 × 104 CB or PB T cells were seeded in 48-well plates upon TCR stimulation or cytokines and transduced with LVs at the indicated multiplicity of infection (MOI). Cell cultures were replenished with cytokines every 3 days. At 3 and 6 days after transduction, the percentage of GFP+ cells was determined by fluorescence-activated cell sorting (FACS). Where indicated, transductions were performed on RetroNectin-coated plates (Takara Bio, Shiga, Japan).
In all, 5 × 105 freshly isolated thymocytes were seeded in RetroNectin-coated 48-well plates in RPMI-1640 and 10% fetal calf serum in the presence of rIL-7 (20 ng/mL) and transduced with LVs at the indicated MOIs. Cell cultures were replenished with cytokines after 3 days. Four days after transduction, the percentage of GFP+ cells was determined by FACS.
CB CD34+ cells were cultured in 48-well plates coated with a Dll4 Fc fusion protein (Dll4-Fc, 5 μg/mL; PX′Therapeutics, Grenoble, France50). Cultures were initiated at 1 × 104 CD34+ cells per well in X-VIVO-20 medium (Lonza, Basel, Switzerland) and supplemented with 20% defined fetal calf serum (Hyclone; Thermo Fisher Scientific, Illkirch, France) and cytokines hIL-7, human FMS-like tyrosine kinase 3 ligand (hFlt3-L), human stem cell factor (hSCF), and human thrombopoietin (hTPO) (each 100 ng/mL; Miltenyi Biotech). The vectors were pre-incubated with Vectofusin (12 μg/mL; Miltenyi Biotech) for 10 minutes. After 24 hours of culture, the LVs plus Vectofusin were added to the cells at the indicated MOIs. After 7 days of culture on Dll4, cells were transferred to 24-well plates freshly coated with Dll4-Fc at a concentration of 1 × 105 cells per well. The percentage of GFP+ cells was determined in the thymic subpopulations by FACS.
A total of 1.8 × 105 bone marrow (BM) SCID-X1 CD34+ cells were prestimulated for 16 hours in X-VIVO-20 (Lonza) supplemented with 20% fetal bovine serum and 300 ng/mL hSCF, 100 ng/mL hTPO, 300 ng/mL hFlt3-L, and 20 ng/mL hIL-3 on RetroNectin (25 µg/mL) alone or on RetroNectin and Dll4-Fc ligand (5 µg/mL; PX′Therapeutics)–coated wells. In addition, 100 ng/mL of hIL-7 was added for prestimulation on Dll4–coated wells. The prestimulated cells were incubated with BaEV-IL-2RγC-LVs at an MOI of 10 in the presence of 4 µg/mL protamine sulfate for 6 hours. For cells transduced for 6 hours on Dll4-coated wells, the medium was replaced by Minimum Essential Medium Eagle–Alpha Modification (Gibco, Life Technologies) with 20% fetal bovine serum, 2 mM glutamine (Gibco BRL/Invitrogen), 100 ng/mL hSCF, 100 ng/mL hTPO, 100 ng/mL hFlt3-L, and 100 ng/mL hIL-7. Viability after transduction was determined after exclusion of 7-amino-actinomycin-D+ cells analyzed by FACS.
The in vitro T-cell differentiation assay was performed on OP9-hDL1 stroma; 8 × 104 cells per well were cocultured in 6-well plates with OP9-hDL1.73 From week 2, the medium was changed once per week, and cells were analyzed by FACS (see supplemental Data).
qPCR analysis
IL-2RγC messenger RNA (mRNA) expression was assessed by using semi-quantitative real-time polymerase chain reaction (RT-PCR). RT-PCR was performed with equal amounts of cDNA using IL-2RγC and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) TaqMan Gene Expression Assay in an Applied Biosystems ViiA 7 Real-Time PCR System (Applied Biosystems Inc, Foster City, CA). The IL-2RγC mRNA expression was normalized with the GAPDH mRNA expression as endogenous control. The γC mRNA expression was calculated as 2-ddCt.
Quantification of vector copy number and analysis of TCR repertoire
Duplex quantitative RT-PCR was performed with 100 ng genomic DNA using primers and TaqMan probes specifically designed to amplify the HIV and albumin (ALB) sequences in the Applied Biosystems ViiA 7 Real-Time PCR System. Simultaneously, standard amplification curves were generated by serial dilutions of the plasmid pRRL-LTR-PSI-GK-GFP-WPRE-ALB ranging from 107 to 101 copies per well. All the reactions were performed in duplicate. The data were normalized to ALB. The vector copy number (VCN) per cell was determined from the linear standard curve. Analysis of the TCR repertoire was performed by multiplex PCR followed by GeneScan analysis as described previously.74,75
Conditioning and reconstitution of NSG mice
NOD/SCIDγC−/− (NSG) mice were housed in our animal facility (Plateau de Biologie Expérimentale de la Souris, Lyon, France). Experiments were performed in accordance with the European Union guidelines upon approval of the protocols by the local ethical committee. Two- to 3-day-old newborn NSG mice were irradiated at 1 Gy, and 5 × 105 transduced progenitor T cells derived from hCD34+ cells or 2 × 105 transduced CD34+ cells were injected intrahepatically. Six weeks after reconstitution, the thymocytes of these mice were analyzed by FACS. Statistical analysis was performed using a Student t test.
Results
BaEV-LVs permit high-level transduction of both naive and memory hT cells
We previously obtained efficient LV pseudotyping with 2 cytoplasmic tail mutants of the BaEV GP: BaEVTR, in which the cytoplasmic tail has been replaced by that of the murine leukemia retrovirus, and BaEVRless, which lacks the R-peptide.69 The new BaEV-LVs19 were compared with other reported LV pseudotypes that allow CD3+ T-cell transduction with differing efficiencies: H/F-LVs,62 RD114TR-LVs,64 and VSV-G-LVs.54
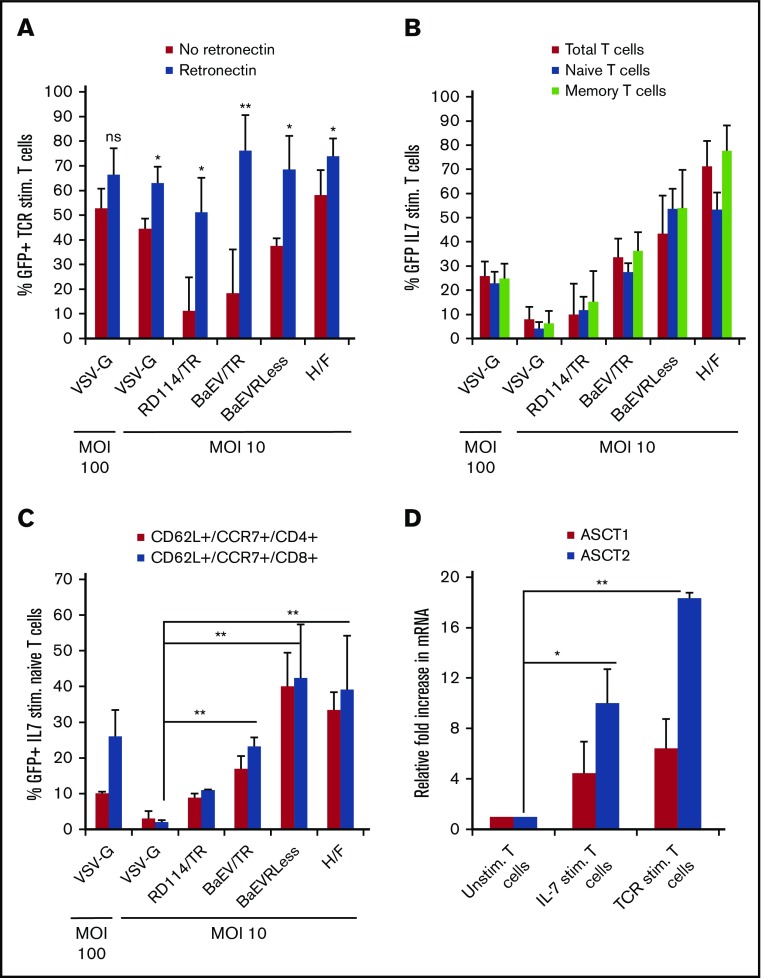
After TCR stimulation, the BaEV-LVs reached 60% to 90% CD3+ T-cell gene transfer in the presence of RetroNectin (MOI, 10; Figure 1A). VSV-G-LVs and H/F-LVs reached similar transduction levels62 (Figure 1A). Both BaEVTR- and BaEVRless-LVs enabled efficient transduction of rIL-7 prestimulated hT cells and were superior to VSV-G-LVs at an MOI of 10 in the presence of RetroNectin (percentage transduction rates: BaEVTR-LVs, 29%-43%; BaEVRless-LVs, 41%-60%; VSV-G-LVs, 2%-12%) (Figure 1B). They permitted efficient high-level transduction of IL-7–prestimulated naive and memory T cells (Figure 1B). The cell viability was not altered by the transduction process (supplemental Figure 1A-B). H/F-LVs resulted in more than 80% transduction of IL-7–stimulated T cells in the presence of RetroNectin. In this case, the H/F-LVs primarily targeted memory T cells for transduction, confirming previous results62 (Figure 1B).
Figure 1.
BaEV-LVs allow high-level transduction of naive as well as memory adult human T cells. (A) Freshly isolated peripheral blood T cells were preactivated through the TCR (anti-CD3 + anti-CD28 antibodies + IL-2) for 24 hours and transduced in the absence and presence of RetroNectin with the different LV pseudotypes at indicated MOIs. Six days after transduction, the percentage of GFP+CD3+ T cells was analyzed by FACS (mean ± standard deviation [SD]; n = 4). (B-C) Freshly isolated CD3+ T cells were prestimulated with IL-7 for 3 days and transduced in the presence of RetroNectin with the different LV pseudotypes at MOI 10 or 100 as indicated. Six days after transduction, the percentage of GFP+CD3+ T cells was analyzed by FACS for total T cells (anti-CD3) and the naive (CD45RA+) or memory (anti-CD45RO+) T cells subsets in panel B. (C) More detailed phenotyping of these cells shows the percentage of GFP+ naive (CD45RA+CD62L+CCR7+) CD4 and CD8 T cells. (B-C; mean ± SD; n = 3; VSV-G-LV MOI 10 vs BaEV-LV). (D) ASCT-1 and ASCT-2 expression levels in unstimulated (unstim.) and TCR- or IL-7–activated total CD3+ T cells (as in panels A and B, respectively). Relative fold increase in ASCT-1 or ASCT-2 mRNA levels in stimulated (stim.) CD3+ T cells compared with unstimulated T cells, for which mRNA levels were normalized to 1 (mean ± SD; n = 3). *P < .05; **P < .01. ns, nonsignificant.
Strict gating on CD45RA-, CD62L-, and CCR7-expressing CD4+ and CD8+ naive T cells confirmed the highly efficient transduction of these subpopulations by BaEV-LVs (Figure 1C). The RD114TR-LVs resulted in much lower transduction efficiency of rIL-7–prestimulated naive and memory T cells compared with BaEV-LVs (RD114TR-LVs, 5%-12%).
We have previously shown that H/F-LVs allow gene transfer into resting CD3+ T cells.62,76 The RD114TR- as well as BaEVTR- and BaEVRless-LVs performed poorly on these quiescent target cells (supplemental Figure 1C). Importantly, mRNA levels of both BaEV receptors (ASCT-1 and ASCT-2) were upregulated upon IL-7 stimulation, and the upregulation was even more pronounced after TCR activation of T cells (Figure 1D). This coincided with higher transduction levels obtained in these prestimulated T cells compared with their resting counterparts (Figure 1C vs supplemental Figure 1C). Overall, our results show that the novel BaEVTR- and BaEVRless-LVs are promising gene transfer tools for adult T-cell gene therapy because they can target long-lived naive T cells at low vector doses.
BaEV-LVs GPs allow high-level transduction of recent thymic emigrants
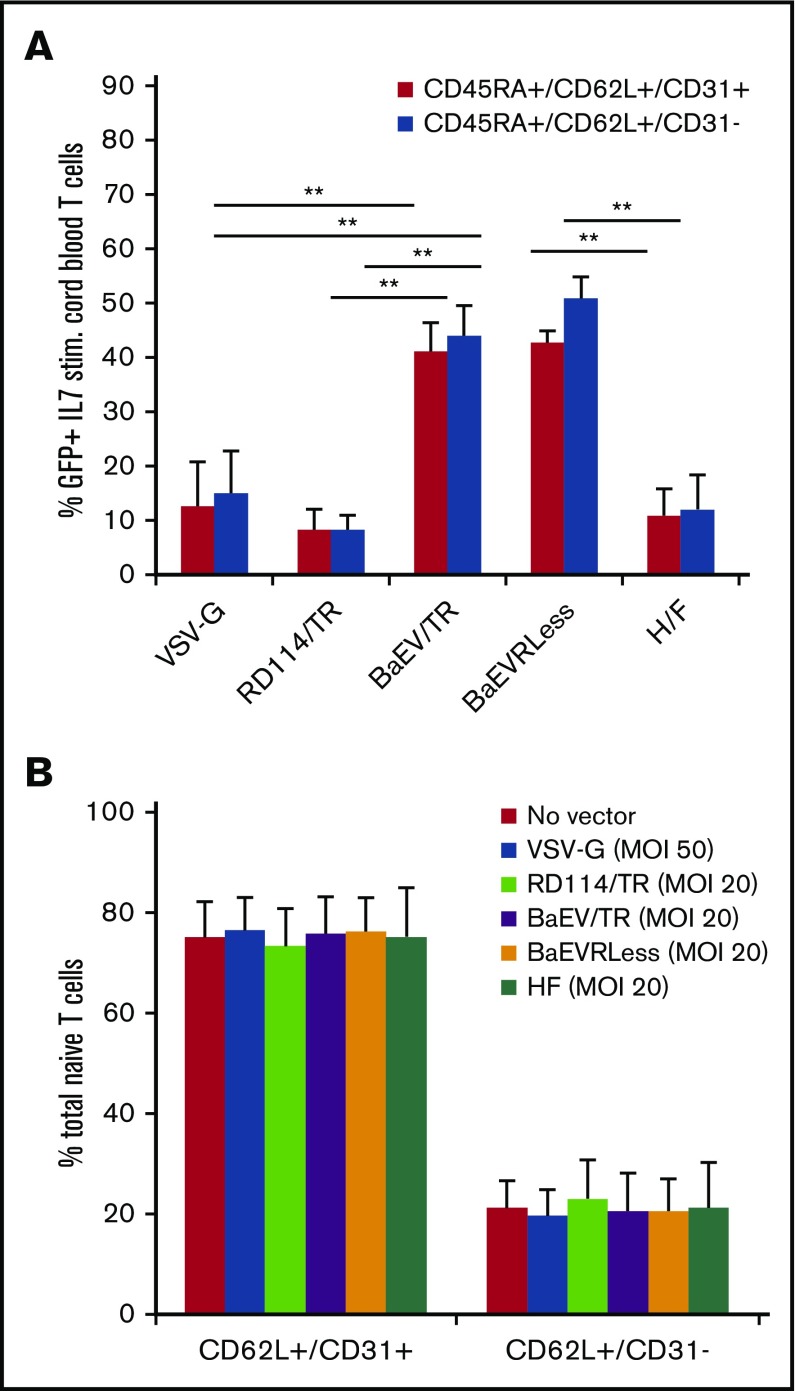
T-cell gene therapy or immunotherapy would benefit from genetically modified naive T cells that are able to persist for the individual’s entire life span. Here, we tested the different LV pseudotypes for their ability to efficiently transduce CB CD4+ T cells, which are phenotypically similar to recent thymic emigrants (RTEs).
To conserve the naive T-cell phenotype, CB T cells were prestimulated with IL-7 and subsequently transduced with the different LV pseudotypes encoding GFP at MOI 10 (Figure 2A). BaEVTR- and BaEVRless-LVs permitted 40% to 55% transduction of the target cells at MOI 10 and thus outperformed VSV-G-LVs (<20%) and RD114TR-LVs (<10%; Figure 2A). In contrast, RTEs and mature naive CB T cells were poorly permissive for H/F-LVs62 (Figure 2A). Importantly, BaEVTR- and BaEVRless-LVs easily reached 55% to 70% transduction when the MOI was doubled to 20 (Figure 2A vs supplemental Figure 2). The RTEs (CD31+) were transduced to the same extent as the mature naive CB CD4+ T cells (CD31–; Figure 2A) without an effect on the distribution of these 2 naive CB T-cell populations (Figure 2B).
Figure 2.
BaEV-LV GPs allow efficient transduction of immature naive CB T cells. (A) Freshly isolated total CB CD4+ T cells were prestimulated with IL-7 for 48 hours and subsequently transduced in the presence of RetroNectin with VSV-G-, RD114TR-, BaEVTR-, BaEVRless-, and H/F-LV, encoding the GFP reporter at an MOI of 10. Three days after transduction, cells were stained for human surface markers CD45RA, CD62L, and CD31, and the percentage of GFP+ cells in recent thymocyte emigrants (CD45RA+, CD62L+, CD31+) and more mature naive CB CD4+ T cells (CD45RA+, CD62L+, CD31–) was determined by FACS analysis (mean ± SD; n = 3; **P < .01). (B) Distribution of the recent thymocyte emigrants (CD45RA+, CD62L+, CD31+) and more mature naive CB (CD45RA+, CD62L+, CD31–) CD4+ T cell subpopulations upon incubation of CB T cells with the different vector pseudotypes as in panel A compared with untransduced T cells (mean ± SD; n = 4).
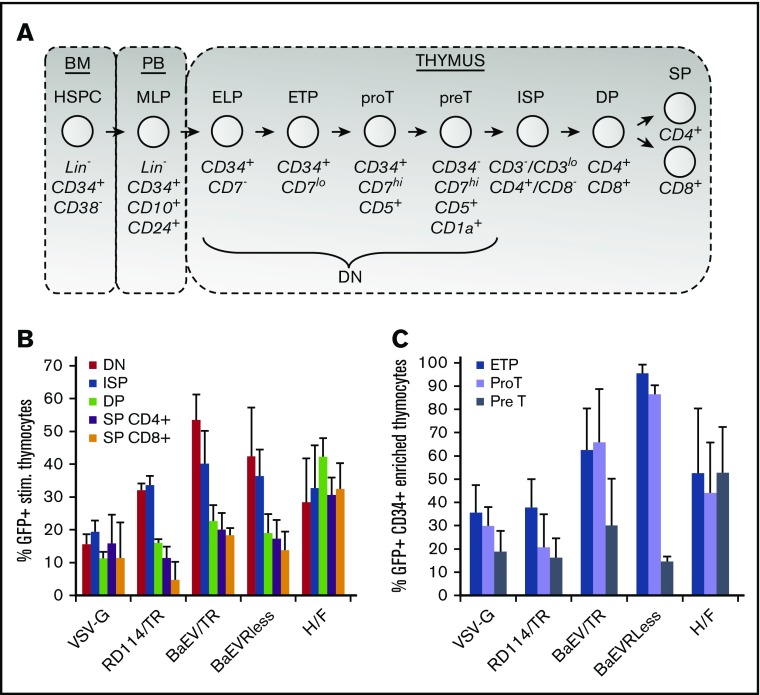
BaEV-LVs promote highly efficient transduction of human thymocytes
It would be of major interest to correct T cells or genetically change T-cell functions as early as possible, ideally during thymic development, which is a tightly regulated process (Figure 3A). We transduced human thymocytes with RD114TR-, BaEVTR-, BaEVRless-, and H/F-LVs (MOI, 10) in the presence of RetroNectin and IL-7. VSV-G-LVs were used at an MOI of 50. Four days later, we determined the transduction levels by FACS in the thymic subsets using CD4/CD8/CD3 staining. VSV-G-LVs transduced only 10% to 20% of the different thymic subpopulations (Figure 3B). RD114TR-, BaEVTR-, and BaEVRless-LVs preferentially transduced early thymocytes (ie, double-negative [DN] and immature single-positive cells; Figure 3A-B). The efficiency of RD114TR-LV transduction of all thymic subpopulations was lower compared with that of BaEV-LVs. Interestingly, H/F-LVs did not show a subpopulation preference and ensured an efficient transduction of all thymic subsets (Figure 3B).
Figure 3.
BaEV-LV GPs confer high-level transduction of human immature thymocyte populations. (A) Schematic representation of T-cell development in the thymus. Phenotypic surface markers are indicated for each differentiation stage. HSCs (CD34+CD1a–) are migrating from the BM to the thymus. The first stages are characterized by the lack of expression of CD8 and CD4 markers (CD8–CD4– DN stage). The DN cells subsequently gain expression of preT and develop into CD4 immature single-positive (ISP) cells. The appearance of the CD8 surface marker together with CD4 and maturation of the TCR is called the DP stage of thymocyte development. Upon selection in the thymus, DP thymocytes develop into CD8+CD4– (SP8) and CD8–CD4+ (SP4) thymocytes. (B) Freshly isolated human thymocytes were transduced in the presence of IL-7 on RetroNectin-coated culture plates with the indicated LV pseudotypes at an MOI of 10, except for VSV-G LVs for which an MOI of 50 was applied. Four days after transduction, the thymocytes were stained for human surface markers (CD3, CD4, and CD8), and the percentage of GFP+ cells in the different thymocyte subpopulations was analyzed by FACS (mean ± SD; n = 5; DN, CD4–CD8–; SP-CD4, CD4+CD3+CD8–; SP-CD8, CD4–CD3+CD8+; DP, CD4+CD8+; ISP, CD4+CD3–CD8–). For BaEV- and RDTR-LVs, the percentage of GFP+, DN, and ISP is significantly higher than the percentage of DP, SP4, and SP8. (C) Freshly isolated human thymocytes were transduced as in panel B. Four days after transduction, the thymocytes were stained for human surface markers (CD34, CD7, CD1a, and CD5), and the percentage of GFP+ cells in the different thymocyte subpopulations was determined (mean ± SD; n = 4). For BaEV-LVs, the percentage of GFP+ ETPs and proT cells was significantly higher than that of preT cells. Gating strategies for FACS analysis are shown in supplemental Figure 5A. P < .01.
The DN CD4–CD8– population can be subdivided into early lymphoid progenitors (ELPs) and early thymocyte progenitors (ETPs), which then differentiate into proT and preT cells (see Figure 3A and supplemental Figure 3 for the gating strategy). BaEV-LVs targeted transduction to the most immature DN thymocytes; BaEVRless-LVs reached 100% of the ETPs and 90% of proT cells (Figure 3C). VSV-G- and RD114TR-LVs resulted in much lower transduction levels. H/F-LVs mediated equivalent high levels of transduction in ETP, proT, and preT cells (Figure 3C).
Our results indicate that BaEV-LVs are better tools than VSV-G- and RD114TR-LVs for the transduction of ETPs and proT cells without population skewing (supplemental Figure 4). This prompted us to test these vectors for transduction of in vitro–generated thymic progenitors.
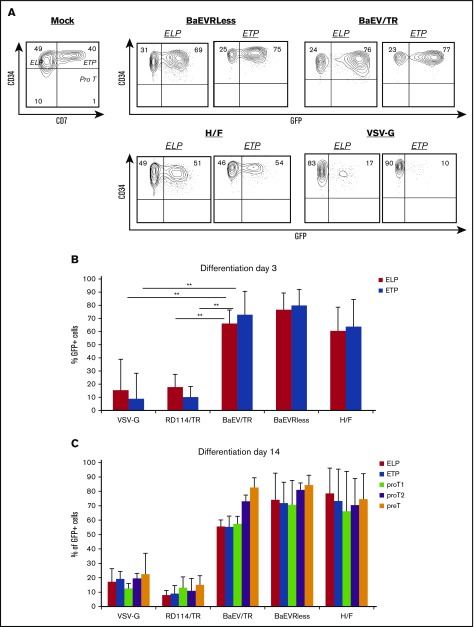
BaEV-LVs mediate efficient transduction of hT-cell progenitors generated in vitro
We made use of our new culture system based on immobilized Dll4, as described previously.50 CB CD34+ cells were cultured on Dll4–coated plates in the presence of cytokines inducing T-cell differentiation. After 24 hours, the different LV pseudotypes were added at an MOI of 10. As observed for freshly isolated thymocytes, BaEV-LVs efficiently transduced ELPs (65%-75%) and ETPs (70%-80%) at high levels when generated in vitro (Figure 3C vs Figure 4A-B). As expected, VSV-G- and RD114TR-LVs permitted only poor transduction of ELPs (15%) and ETPs (10%), whereas H/F-LVs achieved transduction levels of 60%50 (Figure 4A-B). CD7+CD34– proT cells appeared on day 7 of differentiation (supplemental Figure 5A). BaEV-LVs performed stable high-level gene transfer into both ELPs and ETPs but also into proT cells without skewing these T-cell populations, whereas VSV-G- and RD114TR-LVs were much less efficient (supplemental Figure 5B-C) in agreement with Hübner et al.77 In contrast, the H/F- and BaEV-LV transduction levels were equivalent at day 7 (supplemental Figure 5B). On day 14, a subset of CD34–CD7++ started to express CD5, allowing us to distinguish between proT1 (CD7++/CD5–) and proT2 (CD7++/CD5+) T-cell stages followed by CD1a expression (preT-cell stage; supplemental Figure 6A). As expected, the highly efficient transductions obtained with BaEV-LVs persisted at day 14 in the ELPs, ETPs, proT1 and proT2 thymocytes, and also in the preT cells (Figure 4C; supplemental Figure 6A). Importantly, differentiation into ETPs and proT cells was not perturbed by the transduction process (supplemental Figure 6B). Because the original CD34+ cells had expanded 50-fold, on average, after 14 days of T-cell differentiation, they went from 5 × 104 CD34+ cells to 2.5 × 106 T-cell progenitors (ELP, ETP, proT, and preT); these findings confirmed stable transduction in the different T-cell populations.
Figure 4.
BaEV-LV GPs confer efficient gene transfer into in vitro–generated early T-cell progenitors. CB CD34+ cells were plated on Dll4-coated culture wells in the presence of a cytokine cocktail (IL-7, TPO, Flt3-L) for 24 hours, and they were subsequently transduced with VSV-G-, RD114TR-, BaEVTR-, BaEVRless- and H/F-LVs encoding the GFP reporter at an MOI of 10, except for VSV-G-LVs for which a higher vector dose (MOI of 50) was applied. (A-B) At day 3 of culture, the cells were analyzed by FACS for surface expression of CD34 and CD7. The gating strategy to determine GFP expression in the subpopulations of ELP, ETP, and proT cells are shown for differentiation at day 3 in panel A for a representative experiment. The transduction levels for day 3 of differentiation toward T-cell lineage in these subpopulations are summarized in the histograms in panel B (mean ± SD; n = 3). (C) At day 14 of culture, the cells were analyzed by FACS for surface expression of CD34, CD7, CD5, and CD1a (for gating strategy, see supplemental Figure 6). GFP expression in the subpopulations ELP, ETP, proT1, proT2, and preT cells at day 14 of differentiation toward T-cell lineage is shown for the different pseudotypes (mean ± SD; n = 3; VSV-G vs other pseudotypes). **P < .01.
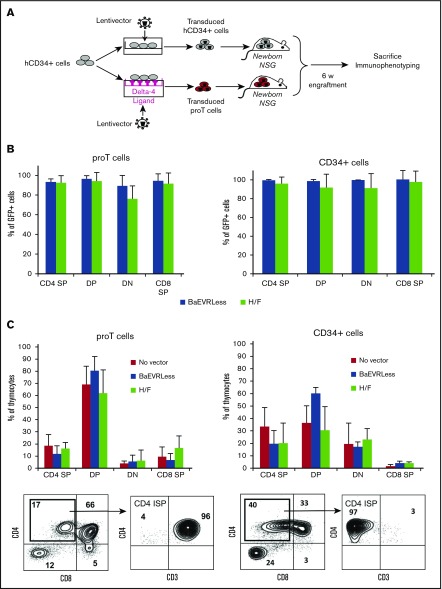
BaEV- and H/F-LV–transduced T-cell progenitors seed the thymus and enable accelerated in vivo thymopoiesis compared with HSCs in NSG mice
The in vivo T-cell differentiation potential of LV-transduced progenitor T cells and HSCs was evaluated by transplantation into NSG mice.50 CD34+ cells were plated on Dll4-coated wells with cytokines and then incubated with BaEV- and H/F-LVs at MOI 10 or without vector in the presence of Vectofusin.78 On day 8 of T-cell differentiation, these transduced T-cell progenitors were injected intrahepatically into NSG neonates. In parallel, CD34+ cells from the same donor were briefly prestimulated with cytokines and were then transduced with BaEV- and H/F-LVs (MOI, 10) or without vector in the presence of RetroNectin. Twenty-four hours after transduction, these transduced CD34+ cells were transplanted into a second group of NSG recipients (Figure 5A). At 6 weeks after engraftment, high levels of transduction were detected by FACS in all thymic subpopulations for both NSG groups (Figure 5B). However, intrathymic T-cell development was accelerated in recipients of T-cell progenitors compared with recipients of hCD34+ cells, which was confirmed by higher percentages of mature CD3+CD4+ and CD3+CD8+ T cells (Figure 5C, left vs right panel). Indeed, the CD4–single-positive (CD4-SP) cells in progenitor T-cell NSG recipients were all CD3+ (Figure 5C, left panel). For the mice that received CD34+ cells, CD4-SP cells did not express CD3 and still corresponded to the earlier immature single-positive CD4 stage (Figure 5C, right dot blots). Overall, mature CD3+ T-cell levels in the thymus and the periphery were significantly higher in progenitor T-cell recipients than in CD34+-cell recipients, and they expressed TCRαβ (Figure 5D-F; supplemental Figure 7). Importantly, this was true for both nontransduced and LV-transduced progenitor T cells, which emphasizes that transduction did not affect T-cell potential in vivo (Figure 5E-F). To summarize, the BaEV- and H/F-LV gene-marked T-cell progenitors generated in vitro allowed efficient thymopoiesis and accelerated T-cell reconstitution in vivo.
Figure 5.
LV-transduced progenitor T cells allowed accelerated thymopoiesis in vivo in NSG mice compared with LV-transduced CD34+cells. (A) CD34+ cells were plated on Dll4-coated wells in the presence of a cytokine cocktail (IL-7, TPO, Flt3-L) for 24 hours, and they were subsequently transduced with BaEV- and H/F-LVs encoding GFP at an MOI of 10 or without vector in the presence of Vectofusin, an agent that facilitates transduction.78 At 8 days of T-cell differentiation, these transduced T-cell progenitors were injected intrahepatically into NSG recipient mice. In parallel, CD34+ cells from the same donor were prestimulated briefly with cytokines that maintain HSC potential (SCF, TPO, Flt3-L) for 24 hours and were transduced with BaEV- and H/F-LVs (MOI, 10) or without vector in the presence of RetroNectin. At 24 hours after transduction, the transduced CD34+ cells were engrafted in a second group of NSG recipients. Human thymocyte reconstitution was assessed 6 weeks after injection into NSG mice by FACS. (B) Percentage of GFP+ thymocytes (CD4 SP, CD4+CD8–; DP, CD4+CD8+; DN, CD4–CD8–; CD8 SP, CD8+CD4–) for T-cell progenitor engraftment compared with CD34+ cell engraftment. (C) Distribution of CD4 SP, DP, DN, and CD8 SP thymic subpopulations for proT cells compared with CD34+ cell engraftment. CD4 SP cells were analyzed for CD3 surface expression for proT (left panels) and CD34+ (right panels) engrafted cells. ISP CD4, CD4+CD3– cells. (D) FACS analysis of the percentage of CD3+ T cells per total hCD45+ cells in the thymus. (E) The absolute numbers of mature CD3+ T cells per total human thymocytes for proT cells compared with CD34+ cell engraftment (mean ± SD; n = 3). (F) Percentage of mature CD3+ T cells in the blood per total hCD45+ cells for proT cells compared with CD34+ cell engraftment (mean ± SD; n = 3). *P < .05.
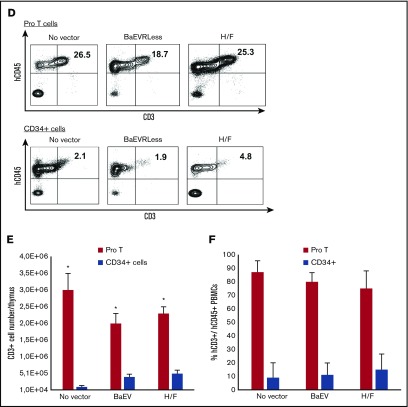
BaEV-LV transduction combined with DLL4 exposure allowed efficient γC-correction of BM SCID-X1 HSPC-derived progenitor T-cells
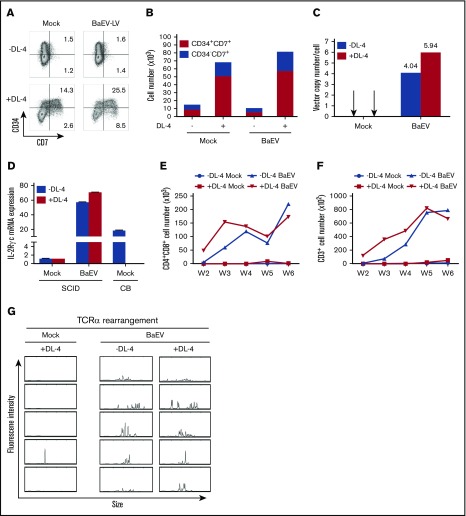
SCID-X1 patients exhibit a severe T-cell defect, which is the result of a blockade in a very early stage of T-cell differentiation caused by a loss-of-function mutation in the γC gene. SCID-X1 γC deficiency can be safely and efficiently corrected by the ex vivo transduction of HSPCs as demonstrated in SCID-X1 patients.79 Because both BaEV- and H/F-LVs performed similarly for transduction of T-cell progenitors, we selected BaEV-LVs encoding the γC receptor to correct the γC deficiency in BM SCID-X1 CD34+ cells under conventional conditions or in combination with the already established Dll4-based T-cell progenitor differentiation technique. Therefore, BM SCID-X1 CD34+ cells were cultured in the presence of RetroNectin alone (conventional) or Dll4 and RetroNectin (Dll4 culture; supplemental Figure 8A) and then transduced or not (mock) with BaEV-LVs encoding the γC receptor at an MOI of 10. FACS analysis did not show any major differences in the frequencies of gated lymphocytes between the transduced and mock groups, and 97% of the gated lymphocytes were viable (supplemental Figure 8B). Thus, BaEV-LV transduction had no toxic effect on the cells. After 4 days of culture, T-cell progenitor differentiation revealed higher frequencies and numbers of CD7+ early T-cell progenitors in the Dll4 culture than in conventional cultures (Figure 6A-B), suggesting that the Dll4 cultures were able to generate early T-cell progenitors. We then evaluated the efficiency of gene correction by testing the ability of transduced cells to differentiate into T cells. Transduced and nontransduced cells were cocultured with an OP9-hDL1 stromal cell layer, and their T-cell differentiation status was analyzed (supplemental Figure 8A). The VCN in CD7+ cells sorted after 5 weeks of coculture reached 4.04 in BaEV-LV transduced conventional cultures and 5.94 in BaEV-LV transduced Dll4 cultures (Figure 6C). IL-2RγC mRNA levels were 60-fold higher in the transduced groups than in the mock groups in CD45+ cells sorted at week 7 and, consistent with the high VCN, approximately threefold higher than in healthy CB CD34+ cells under Dll4 culture conditions (Figure 6D). CD4+CD8+ (DP) cells and CD3+ cells were present as early as week 2 in the transduced Dll4 culture conditions and week 3 in the transduced conventional culture conditions and continued to be detected afterward in higher numbers in the Dll4 culture conditions until week 5. This suggested accelerated restoration of T-cell differentiation in the BaEV-LV transduced Dll4 culture conditions (Figure 6E-F; supplemental Figure 8C). Importantly, the CD3+ cells were found to express either TCRγδ or TCRαβ; this was especially true in the Dll4 culture conditions (supplemental Figure 8D-E). TCR repertoire analysis of the polyclonality in CD7+ cells sorted at week 5 revealed only diverse TCRγδ rearrangement but not TCRαβ rearrangement in nontransduced conditions (Figure 6G; supplemental Figure 8F); this was consistent with the appearance of TCRγδ+CD3+ cells but not TCRαβ+CD3+ cells in the later weeks (supplemental Figure 8D-E). This was also in line with the leaky mutation in the γC gene found in this particular patient. However, the DP and CD3+ cell counts remained very low in these mock groups (Figure 6E-F). Conversely, TCRγδ and TCRαβ rearrangements were polyclonal under BaEV-LV transduction conditions regardless of the presence or absence of Dll4; this confirmed the polyclonality of differentiated cells and the absence of any deleterious effect of Dll4 on the polyclonality of cells (Figure 6G; supplemental Figure 8F). Our data demonstrate the correction of γC deficiency in BM SCID-X1 CD34+ cells under both conventional and Dll4 culture conditions. However, T-cell differentiation was faster and more efficient under Dll4 conditions. Collectively, BaEV-LVs allowed efficient correction of the γC defect in SCID-X1 HSCs with high VCN, high levels of γC expression, and de novo T-cell differentiation from SCID-X1 HSPCs.
Figure 6.
Efficient T-cell differentiation in vitro of SCID-X1 BM CD34+HSPCs after transduction with BaEV-LVs encoding γC receptor. SCID-X1 BM CD34+ HSPCs were transduced (BaEV) or not (mock) with BaEV-LVs encoding IL-2RγC at an MOI of 10 for 6 hours after 16 hours of prestimulation with cytokines in either RetroNectin or Dll4 plus RetroNectin-coated wells (see supplemental Figure 6A). The X-SCID mutation is a breakpoint mutation in intron 3 of the IL-2RG gene, which is a γC leaky mutation. Flow cytometry analyses indicating the percentage (A) and absolute cell number (B) of CD34+CD7+ and CD34–CD7+ T-cell progenitors after 4 days of culture in the presence (+ Dll4) or absence (–Dll4) of Dll4. After 4 days of culture, the cells were further cultured with OP9-hDL1 stromal cells to pursue the T-cell differentiation process. Analyses of VCN per cell in the genome by duplex quantitative PCR in sorted CD7+ cells at week 5 (C) and IL-2RγC mRNA expression by semi-quantitative RT-PCR in hCD45+ cells at week 7 (D) of differentiation (compared with CB CD34+ T-cell differentiation cultures in parallel). During coculture with OP9-hDL1 stromal cells, mock and BaEV-LV transduced cells were analyzed once per week by flow cytometry. Analyses of absolute cell numbers of CD4+CD8+ (E) and CD3+ cells (F) at the indicated weeks after OP9-hDL1 cocultures. (G) TCR repertoire analysis by multiplex PCR followed by GeneScan analysis in CD7+ cells sorted at week 5 after OP9-hDL1 cocultures. All the populations were gated on live 7-amino-actinomycin-D– cells.
Discussion
Here we highlighted the exceptional capacity of BaEV-LVs to transduce 60% of IL-7–stimulated naive adult T cells and CB RTEs. In contrast, VSV-G- or RD114TR-LVs performed poorly. Remarkably, BaEV-LVs transduced up to 80% of early thymocytes such as ETPs, proT-cell, and preT-cell lineages differentiated from CD34+ cells using a feeder-cell–free Dll4 culture system.50 Hence, BaEV-LVs constitute a promising tool for the transduction of naive and early progenitor T cells, whereas H/F-LVs are complementary because they can efficiently transduce memory T cells and late-stage thymocytes: CD4+CD8+ and CD4-SP or CD8-SP cells. Accordingly, we confirmed the upregulation of the BaEV receptors67,80 upon IL-7 and TCR T-cell stimulation coinciding with increased BaEV-LV–mediated gene transfer.
A successful T-cell immunotherapy consists of engineering autologous or allogenic T cells to express CARs specific for either viruses or tumor antigens.23,28 Recently, this CAR T-cell technology has been translated to naive cells from CB.81 Micklethwaite et al16 transduced CB T cells with a CAR against CD19, which also coexpressed TCRs specific for 3 different viruses that can affect patients after a CB transplant. When compared with adult T cells, naive CB T cells showed a greater tolerance to HLA disparity82,83 and thus induced graft-versus-host disease less frequently. Therefore, naive CB T cells represent a source of allogenic lymphocytes for cell therapy of viral infections or/and cancer, particularly when patients do not have enough autologous T cells. Indeed, IL-7–stimulated CB T cells combined with BaEV-LVs resulted in gene delivery levels of 70%. This might constitute an important advantage for CAR therapy because naive CB T-cell subsets show a high capacity to expand and might provide longer-lasting antitumor responses in vivo than adult T cells, allowing protection against relapse after transplant.38,39
Infections and relapse are the main causes of morbidity and mortality after allogenic HSC transplantation. This is undoubtedly related to delayed T-cell immune reconstitution and impaired de novo thymopoiesis.84-86 The same is true for autologous HSC-mediated gene therapy. Complete restoration of a polyclonal T-cell repertoire takes even longer, and patients can be immunocompromised for more than a year.87,88 In the case of gene therapy, the administration of autologous gene-corrected T-cell progenitors might be an option. We can genetically modify these T-cell progenitors derived from CD34+ cells at high levels using the BaEV- or H/F-LVs. Combination of the transduction with the Dll4 culture of hCD34+ cells, resulted in the expansion of gene-marked ETPs and proT1 cells, the most primitive T cells. Moreover, these cells retained their in vivo intrathymic T-cell differentiation capacity and displayed a conventional CD4, CD8, and TCRαβ/TCRγδ repertoire. Furthermore, T-cell reconstitution was faster than in hCD34+-cell engrafted NSG mice.50
These data suggest that BaEV- or H/F-LVs are valuable treatment options for SCIDs (eg, SCID-X1) and HIV, in which the thymic environment is not ideal for HSC differentiation into T-cell lineages. We have previously evidenced faster immune reconstitution by coinfusion of HSC-derived T-cell progenitors and CB HSPCs in the NSG mouse model.50 Infusion of autologous corrected T-cell progenitors together with corrected HSCs might accelerate immune reconstitution and reduce the gap in immune system recovery. In a clinical setting, part of the patient’s HSPCs would be gene-corrected with the classical protocol and another part would be gene-corrected with the Dll4–based protocol described herein. The 2 products could be transplanted simultaneously. We have shown that T-cell progenitors are able to directly seed the thymus without passing through the BM,50 thus overcoming 2 main obstacles of post-HSCT T-cell generation: the long time required for the first BM and thymic phases and the limited thymic supply by BM progenitors. We are currently testing this hypothesis in a clinical trial of cell therapy for SCID patients who received a transplantation in a haplo-identical setting.
This is supported by our BaEV-LV–based correction of γC-deficient CD34+ cells in the presence of Dll4, resulting in a large amount of T-cell progenitors. We previously confirmed that BaEV-LVs also allow high-level transduction of prestimulated and unstimulated hHSCs.19 Remarkably, γC-encoding BaEV-LVs efficiently rescued SCID-X1 CD34+-derived T-cell development in vitro, showing the clinical feasibility of this approach.
In conclusion, H/F-LVs and, in particular, BaEV-LVs represent very useful new tools for applications in T-cell gene therapy and immunotherapy. In addition, injection of BaEV-LV corrected autologous HSCs and T-cell progenitors might produce both short-term recovery of T-cell immune response and long-term correction in the patients.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
The authors thank the staff of the Plateau de Biologie Expérimentale de la Souris animal care facility at the Ecole Normale Supérieure de Lyon, the flow cytometry platform (SFR BioSciences Lyon [UMS3444/US8], Lyon, France, and Imagine Institute, Paris, France), and Gisèle Froment, Didier Nègre, and Caroline Costa from the lentivectors production facility/SFR BioSciences Lyon (UMS3444/US8, Lyon, France).
This work was supported by French grants from AFM, ANRS, ARC, and LABEX and grants from the European Community (FP7-HEALTH-2007-B/222878 “PERSIST” and “GENTHERTHALPLUS”), by INSERM, a European Union H2020 grant (SCIDNet 666908), an INCA-Plan Cancer grant (2009-2013), and a public grant overseen by the French National Research Agency (ANR) as part of the Investissements d’Avenir program (reference: ANR-10-IAHU-01). R.M. was supported by a scholarship from the French ministry, and K.M. was supported by a scholarship from the China Scholarship Council.
Authorship
Contribution: E.V. coordinated the project, designed and performed experiments, analyzed and discussed the data, and wrote the manuscript; I.A. designed and performed experiments, analyzed and discussed the data, and wrote the manuscript; O.B., F.A., A.G.-G., C.C., C.L., D.N., and R.M. performed experiments, analyzed the data, and discussed results; R.D.M., H.S., C.L.-P., K.M., and M.C. performed T-cell differentiation of SCID-X1 CD34+ cells, analyzed data, discussed results, and corrected the manuscript; V.A. and A.C. provided human thymocytes, critical discussion, and technical advice; C.R. provided technical advice and helped with design of experiments; D.F. provided Vectofusin and technical advice; and F.-L.C. provided critical discussion and read the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests
Correspondence: Els Verhoeyen, Centre International de Recherche en Infectiologie, Enveloppes Virales, Vecteurs et Immunothérapie, Ecole Normale Supérieure de Lyon, 46 Allée d’Italie, 69364 Lyon, France; e-mail: els.verhoeyen@ens-lyon.fr.
References
- 1.Blaese RM, Culver KW, Miller AD, et al. T lymphocyte-directed gene therapy for ADA- SCID: initial trial results after 4 years. Science. 1995;270(5235):475-480. [DOI] [PubMed] [Google Scholar]
- 2.Bordignon C, Notarangelo LD, Nobili N, et al. Gene therapy in peripheral blood lymphocytes and bone marrow for ADA- immunodeficient patients. Science. 1995;270(5235):470-475. [DOI] [PubMed] [Google Scholar]
- 3.Bonini C, Ferrari G, Verzeletti S, et al. HSV-TK gene transfer into donor lymphocytes for control of allogeneic graft-versus-leukemia. Science. 1997;276(5319):1719-1724. [DOI] [PubMed] [Google Scholar]
- 4.Kalos M, Levine BL, Porter DL, et al. T cells with chimeric antigen receptors have potent antitumor effects and can establish memory in patients with advanced leukemia. Sci Transl Med. 2011;3(95):95ra73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buchschacher GL Jr, Wong-Staal F. Approaches to gene therapy for human immunodeficiency virus infection. Hum Gene Ther. 2001;12(9):1013-1019. [DOI] [PubMed] [Google Scholar]
- 6.Aiuti A, Vai S, Mortellaro A, et al. Immune reconstitution in ADA-SCID after PBL gene therapy and discontinuation of enzyme replacement. Nat Med. 2002;8(5):423-425. [DOI] [PubMed] [Google Scholar]
- 7.Cavazzana-Calvo M, Hacein-Bey S, de Saint Basile G, et al. Gene therapy of human severe combined immunodeficiency (SCID)-X1 disease. Science. 2000;288(5466):669-672. [DOI] [PubMed] [Google Scholar]
- 8.Aiuti A, Slavin S, Aker M, et al. Correction of ADA-SCID by stem cell gene therapy combined with nonmyeloablative conditioning. Science. 2002;296(5577):2410-2413. [DOI] [PubMed] [Google Scholar]
- 9.Centlivre M, Legrand N, Klamer S, et al. Preclinical in vivo evaluation of the safety of a multi-shRNA-based gene therapy against HIV-1. Mol Ther Nucleic Acids. 2013;2:e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung J, Zhang J, Li H, Ouellet DL, DiGiusto DL, Rossi JJ. Endogenous MCM7 microRNA cluster as a novel platform to multiplex small interfering and nucleolar RNAs for combinational HIV-1 gene therapy. Hum Gene Ther. 2012;23(11):1200-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tebas P, Stein D, Tang WW, et al. Gene editing of CCR5 in autologous CD4 T cells of persons infected with HIV. N Engl J Med. 2014;370(10):901-910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bondanza A, Valtolina V, Magnani Z, et al. Suicide gene therapy of graft-versus-host disease induced by central memory human T lymphocytes. Blood. 2006;107(5):1828-1836. [DOI] [PubMed] [Google Scholar]
- 13.Cieri N, Mastaglio S, Oliveira G, Casucci M, Bondanza A, Bonini C. Adoptive immunotherapy with genetically modified lymphocytes in allogeneic stem cell transplantation. Immunol Rev. 2014;257(1):165-180. [DOI] [PubMed] [Google Scholar]
- 14.Marin V, Cribioli E, Philip B, et al. Comparison of different suicide-gene strategies for the safety improvement of genetically manipulated T cells. Hum Gene Ther Methods. 2012;23(6):376-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gattinoni L, Klebanoff CA, Palmer DC, et al. Acquisition of full effector function in vitro paradoxically impairs the in vivo antitumor efficacy of adoptively transferred CD8+ T cells. J Clin Invest. 2005;115(6):1616-1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Micklethwaite KP, Savoldo B, Hanley PJ, et al. Derivation of human T lymphocytes from cord blood and peripheral blood with antiviral and antileukemic specificity from a single culture as protection against infection and relapse after stem cell transplantation. Blood. 2010;115(13):2695-2703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morgan RA, Dudley ME, Wunderlich JR, et al. Cancer regression in patients after transfer of genetically engineered lymphocytes. Science. 2006;314(5796):126-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brentjens RJ, Davila ML, Riviere I, et al. CD19-targeted T cells rapidly induce molecular remissions in adults with chemotherapy-refractory acute lymphoblastic leukemia. Sci Transl Med. 2013;5(177):177ra38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Girard-Gagnepain A, Amirache F, Costa C, et al. Baboon envelope pseudotyped LVs outperform VSV-G-LVs for gene transfer into cytokine-stimulated and resting HSCs. Blood. 2014;124(8):1221-1231. [DOI] [PubMed] [Google Scholar]
- 20.Kochenderfer JN, Wilson WH, Janik JE, et al. Eradication of B-lineage cells and regression of lymphoma in a patient treated with autologous T cells genetically engineered to recognize CD19. Blood. 2010;116(20):4099-4102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Porter DL, Levine BL, Kalos M, Bagg A, June CH. Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia. N Engl J Med. 2011;365(8):725-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown CE, Alizadeh D, Starr R, et al. Regression of glioblastoma after chimeric antigen receptor T-cell therapy. N Engl J Med. 2016;375(26):2561-2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haso W, Lee DW, Shah NN, et al. Anti-CD22-chimeric antigen receptors targeting B-cell precursor acute lymphoblastic leukemia. Blood. 2013;121(7):1165-1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hegde M, Mukherjee M, Grada Z, et al. Tandem CAR T cells targeting HER2 and IL13Rα2 mitigate tumor antigen escape. J Clin Invest. 2016;126(8):3036-3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson LA, Scholler J, Ohkuri T, et al. Rational development and characterization of humanized anti-EGFR variant III chimeric antigen receptor T cells for glioblastoma. Sci Transl Med. 2015;7(275):275ra22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shaffer DR, Savoldo B, Yi Z, et al. T cells redirected against CD70 for the immunotherapy of CD70-positive malignancies. Blood. 2011;117(16):4304-4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gargett T, Yu W, Dotti G, et al. GD2-specific CAR T cells undergo potent activation and deletion following antigen encounter but can be protected from activation-induced cell death by PD-1 blockade. Mol Ther. 2016;24(6):1135-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robbins PF, Morgan RA, Feldman SA, et al. Tumor regression in patients with metastatic synovial cell sarcoma and melanoma using genetically engineered lymphocytes reactive with NY-ESO-1. J Clin Oncol. 2011;29(7):917-924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Robbins PF, Dudley ME, Wunderlich J, et al. Cutting edge: persistence of transferred lymphocyte clonotypes correlates with cancer regression in patients receiving cell transfer therapy. J Immunol. 2004;173(12):7125-7130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosenberg SA, Yang JC, Sherry RM, et al. Durable complete responses in heavily pretreated patients with metastatic melanoma using T-cell transfer immunotherapy. Clin Cancer Res. 2011;17(13):4550-4557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klebanoff CA, Gattinoni L, Torabi-Parizi P, et al. Central memory self/tumor-reactive CD8+ T cells confer superior antitumor immunity compared with effector memory T cells. Proc Natl Acad Sci USA. 2005;102(27):9571-9576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hassan J, Reen DJ. Human recent thymic emigrants--identification, expansion, and survival characteristics. J Immunol. 2001;167(4):1970-1976. [DOI] [PubMed] [Google Scholar]
- 33.Berger C, Jensen MC, Lansdorp PM, Gough M, Elliott C, Riddell SR. Adoptive transfer of effector CD8+ T cells derived from central memory cells establishes persistent T cell memory in primates. J Clin Invest. 2008;118(1):294-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marshall-Clarke S, Reen D, Tasker L, Hassan J. Neonatal immunity: how well has it grown up? Immunol Today. 2000;21(1):35-41. [DOI] [PubMed] [Google Scholar]
- 35.Assing K, Nielsen C, Kirchhoff M, Madsen HO, Ryder LP, Fisker N. CD4+ CD31+ recent thymic emigrants in CHD7 haploinsufficiency (CHARGE syndrome): a case. Hum Immunol. 2013;74(9):1047-1050. [DOI] [PubMed] [Google Scholar]
- 36.Kimmig S, Przybylski GK, Schmidt CA, et al. Two subsets of naive T helper cells with distinct T cell receptor excision circle content in human adult peripheral blood. J Exp Med. 2002;195(6):789-794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Soares MV, Borthwick NJ, Maini MK, Janossy G, Salmon M, Akbar AN. IL-7-dependent extrathymic expansion of CD45RA+ T cells enables preservation of a naive repertoire. J Immunol. 1998;161(11):5909-5917. [PubMed] [Google Scholar]
- 38.Swainson L, Verhoeyen E, Cosset FL, Taylor N. IL-7R alpha gene expression is inversely correlated with cell cycle progression in IL-7-stimulated T lymphocytes. J Immunol. 2006;176(11):6702-6708. [DOI] [PubMed] [Google Scholar]
- 39.Azevedo RI, Soares MV, Barata JT, et al. IL-7 sustains CD31 expression in human naive CD4+ T cells and preferentially expands the CD31+ subset in a PI3K-dependent manner. Blood. 2009;113(13):2999-3007. [DOI] [PubMed] [Google Scholar]
- 40.Pegram HJ, Purdon TJ, van Leeuwen DG, et al. IL-12-secreting CD19-targeted cord blood-derived T cells for the immunotherapy of B-cell acute lymphoblastic leukemia. Leukemia. 2015;29(2):415-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Merindol N, Grenier AJ, Caty M, et al. Umbilical cord blood T cells respond against the Melan-A/MART-1 tumor antigen and exhibit reduced alloreactivity as compared with adult blood-derived T cells. J Immunol. 2010;185(2):856-866. [DOI] [PubMed] [Google Scholar]
- 42.Serrano LM, Pfeiffer T, Olivares S, et al. Differentiation of naive cord-blood T cells into CD19-specific cytolytic effectors for posttransplantation adoptive immunotherapy. Blood. 2006;107(7):2643-2652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khoury SJ, Sayegh MH, Hancock WW, Gallon L, Carpenter CB, Weiner HL. Acquired tolerance to experimental autoimmune encephalomyelitis by intrathymic injection of myelin basic protein or its major encephalitogenic peptide. J Exp Med. 1993;178(2):559-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marodon G, Fisson S, Levacher B, Fabre M, Salomon BL, Klatzmann D. Induction of antigen-specific tolerance by intrathymic injection of lentiviral vectors. Blood. 2006;108(9):2972-2978. [DOI] [PubMed] [Google Scholar]
- 45.Posselt AM, Barker CF, Friedman AL, Naji A. Prevention of autoimmune diabetes in the BB rat by intrathymic islet transplantation at birth. Science. 1992;256(5061):1321-1324. [DOI] [PubMed] [Google Scholar]
- 46.Adjali O, Marodon G, Steinberg M, et al. In vivo correction of ZAP-70 immunodeficiency by intrathymic gene transfer. J Clin Invest. 2005;115(8):2287-2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hozumi K, Mailhos C, Negishi N, et al. Delta-like 4 is indispensable in thymic environment specific for T cell development. J Exp Med. 2008;205(11):2507-2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Koch U, Fiorini E, Benedito R, et al. Delta-like 4 is the essential, nonredundant ligand for Notch1 during thymic T cell lineage commitment. J Exp Med. 2008;205(11):2515-2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lefort N, Benne C, Lelièvre JD, et al. Short exposure to Notch ligand delta-4 is sufficient to induce T-cell differentiation program and to increase the T cell potential of primary human CD34+ cells. Exp Hematol. 2006;34(12):1720-1729. [DOI] [PubMed] [Google Scholar]
- 50.Reimann C, Six E, Dal-Cortivo L, et al. Human T-lymphoid progenitors generated in a feeder-cell-free delta-like-4 culture system promote T-cell reconstitution in NOD/SCID/γc(-/-) mice. Stem Cells. 2012;30(8):1771-1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Simons L, Ma K, de Chappedelaine C, et al. Generation of adult human T-cell progenitors for immunotherapeutic applications. J Allergy Clin Immunol. 2018;141(4):1491-1494.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dardalhon V, Jaleco S, Kinet S, et al. IL-7 differentially regulates cell cycle progression and HIV-1-based vector infection in neonatal and adult CD4+ T cells. Proc Natl Acad Sci USA. 2001;98(16):9277-9282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Korin YD, Zack JA. Progression to the G1b phase of the cell cycle is required for completion of human immunodeficiency virus type 1 reverse transcription in T cells. J Virol. 1998;72(4):3161-3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Verhoeyen E, Dardalhon V, Ducrey-Rundquist O, Trono D, Taylor N, Cosset FL. IL-7 surface-engineered lentiviral vectors promote survival and efficient gene transfer in resting primary T lymphocytes. Blood. 2003;101(6):2167-2174. [DOI] [PubMed] [Google Scholar]
- 55.Amirache F, Lévy C, Costa C, et al. Mystery solved: VSV-G-LVs do not allow efficient gene transfer into unstimulated T cells, B cells, and HSCs because they lack the LDL receptor. Blood. 2014;123(9):1422-1424. [DOI] [PubMed] [Google Scholar]
- 56.Ferrand C, Robinet E, Contassot E, et al. Retrovirus-mediated gene transfer in primary T lymphocytes: influence of the transduction/selection process and of ex vivo expansion on the T cell receptor beta chain hypervariable region repertoire. Hum Gene Ther. 2000;11(8):1151-1164. [DOI] [PubMed] [Google Scholar]
- 57.Marktel S, Magnani Z, Ciceri F, et al. Immunologic potential of donor lymphocytes expressing a suicide gene for early immune reconstitution after hematopoietic T-cell-depleted stem cell transplantation. Blood. 2003;101(4):1290-1298. [DOI] [PubMed] [Google Scholar]
- 58.Cavalieri S, Cazzaniga S, Geuna M, et al. Human T lymphocytes transduced by lentiviral vectors in the absence of TCR activation maintain an intact immune competence. Blood. 2003;102(2):497-505. [DOI] [PubMed] [Google Scholar]
- 59.Ducrey-Rundquist O, Guyader M, Trono D. Modalities of interleukin-7-induced human immunodeficiency virus permissiveness in quiescent T lymphocytes. J Virol. 2002;76(18):9103-9111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Unutmaz D, KewalRamani VN, Marmon S, Littman DR. Cytokine signals are sufficient for HIV-1 infection of resting human T lymphocytes. J Exp Med. 1999;189(11):1735-1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Frecha C, Costa C, Lévy C, et al. Efficient and stable transduction of resting B lymphocytes and primary chronic lymphocyte leukemia cells using measles virus gp displaying lentiviral vectors. Blood. 2009;114(15):3173-3180. [DOI] [PubMed] [Google Scholar]
- 62.Frecha C, Costa C, Nègre D, et al. Stable transduction of quiescent T cells without induction of cycle progression by a novel lentiviral vector pseudotyped with measles virus glycoproteins. Blood. 2008;112(13):4843-4852. [DOI] [PubMed] [Google Scholar]
- 63.Frecha C, Lévy C, Cosset FL, Verhoeyen E. Advances in the field of lentivector-based transduction of T and B lymphocytes for gene therapy. Mol Ther. 2010;18(10):1748-1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sandrin V, Boson B, Salmon P, et al. Lentiviral vectors pseudotyped with a modified RD114 envelope glycoprotein show increased stability in sera and augmented transduction of primary lymphocytes and CD34+ cells derived from human and nonhuman primates. Blood. 2002;100(3):823-832. [DOI] [PubMed] [Google Scholar]
- 65.Rasko JE, Battini JL, Gottschalk RJ, Mazo I, Miller AD. The RD114/simian type D retrovirus receptor is a neutral amino acid transporter. Proc Natl Acad Sci USA. 1999;96(5):2129-2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tailor CS, Marin M, Nouri A, Kavanaugh MP, Kabat D. Truncated forms of the dual function human ASCT2 neutral amino acid transporter/retroviral receptor are translationally initiated at multiple alternative CUG and GUG codons. J Biol Chem. 2001;276(29):27221-27230. [DOI] [PubMed] [Google Scholar]
- 67.Marin M, Tailor CS, Nouri A, Kabat D. Sodium-dependent neutral amino acid transporter type 1 is an auxiliary receptor for baboon endogenous retrovirus. J Virol. 2000;74(17):8085-8093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fusil F, Calattini S, Amirache F, et al. A lentiviral vector allowing physiologically regulated membrane-anchored and secreted antibody expression depending on B-cell maturation status. Mol Ther. 2015;23(11):1734-1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Girard-Gagnepain A, Amirache F, Costa C, et al. Baboon envelope pseudotyped LVs outperform VSV-G-LVs for gene transfer into early-cytokine-stimulated and resting HSCs. Blood. 2014;124(8):1221-1231. [DOI] [PubMed] [Google Scholar]
- 70.Levy C, Fusil F, Amirache F, et al. Baboon envelope pseudotyped lentiviral vectors efficiently transduce human B cells and allow active factor IX B cell secretion in vivo in NOD/SCIDγc-/- mice. J Thromb Haemost. 2016;14(12):2478-2492. [DOI] [PubMed] [Google Scholar]
- 71.Lévy C, Amirache F, Girard-Gagnepain A, et al. Measles virus envelope pseudotyped lentiviral vectors transduce quiescent human HSCs at an efficiency without precedent. Blood Adv. 2017;1(23):2088-2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Maurice M, Verhoeyen E, Salmon P, Trono D, Russell SJ, Cosset FL. Efficient gene transfer into human primary blood lymphocytes by surface-engineered lentiviral vectors that display a T cell-activating polypeptide. Blood. 2002;99(7):2342-2350. [DOI] [PubMed] [Google Scholar]
- 73.Six EM, Benjelloun F, Garrigue A, et al. Cytokines and culture medium have a major impact on human in vitro T-cell differentiation. Blood Cells Mol Dis. 2011;47(1):72-78. [DOI] [PubMed] [Google Scholar]
- 74.van Dongen JJ, Langerak AW, Brüggemann M, et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia. 2003;17(12):2257-2317. [DOI] [PubMed] [Google Scholar]
- 75.Villarese P, Lours C, Trinquand A, et al. TCRα rearrangements identify a subgroup of NKL-deregulated adult T-ALLs associated with favorable outcome. Leukemia. 2018;32(1):61-71. [DOI] [PubMed] [Google Scholar]
- 76.Frecha C, Lévy C, Costa C, et al. Measles virus glycoprotein-pseudotyped lentiviral vector-mediated gene transfer into quiescent lymphocytes requires binding to both SLAM and CD46 entry receptors. J Virol. 2011;85(12):5975-5985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hübner J, Hoseini SS, Suerth JD, et al. Generation of genetically engineered precursor T-cells from human umbilical cord blood using an optimized alpharetroviral vector platform. Mol Ther. 2016;24(7):1216-1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Majdoul S, Seye AK, Kichler A, et al. Molecular determinants of vectofusin-1 and its derivatives for the enhancement of lentivirally mediated gene transfer into hematopoietic stem/progenitor cells. J Biol Chem. 2016;291(5):2161-2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hacein-Bey-Abina S, Pai SY, Gaspar HB, et al. A modified γ-retrovirus vector for X-linked severe combined immunodeficiency. N Engl J Med. 2014;371(15):1407-1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Marin M, Lavillette D, Kelly SM, Kabat D. N-linked glycosylation and sequence changes in a critical negative control region of the ASCT1 and ASCT2 neutral amino acid transporters determine their retroviral receptor functions. J Virol. 2003;77(5):2936-2945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Frumento G, Zheng Y, Aubert G, et al. Cord blood T cells retain early differentiation phenotype suitable for immunotherapy after TCR gene transfer to confer EBV specificity. Am J Transplant. 2013;13(1):45-55. [DOI] [PubMed] [Google Scholar]
- 82.Laughlin MJ, Barker J, Bambach B, et al. Hematopoietic engraftment and survival in adult recipients of umbilical-cord blood from unrelated donors. N Engl J Med. 2001;344(24):1815-1822. [DOI] [PubMed] [Google Scholar]
- 83.Rocha V, Labopin M, Sanz G, et al. ; Eurocord-Netcord Registry. Transplants of umbilical-cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med. 2004;351(22):2276-2285. [DOI] [PubMed] [Google Scholar]
- 84.Admiraal R, de Koning CCH, Lindemans CA, et al. Viral reactivations and associated outcomes in the context of immune reconstitution after pediatric hematopoietic cell transplantation. J Allergy Clin Immunol. 2017;140(6):1643-1650.e9. [DOI] [PubMed] [Google Scholar]
- 85.Heimall J, Logan BR, Cowan MJ, et al. Immune reconstitution and survival of 100 SCID patients post-hematopoietic cell transplant: a PIDTC natural history study. Blood. 2017;130(25):2718-2727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Storek J, Geddes M, Khan F, et al. Reconstitution of the immune system after hematopoietic stem cell transplantation in humans. Semin Immunopathol. 2008;30(4):425-437. [DOI] [PubMed] [Google Scholar]
- 87.Komanduri KV, St John LS, de Lima M, et al. Delayed immune reconstitution after cord blood transplantation is characterized by impaired thymopoiesis and late memory T-cell skewing. Blood. 2007;110(13):4543-4551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Parkman R, Weinberg KI. Immunological reconstitution following bone marrow transplantation. Immunol Rev. 1997;157(1):73-78. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.