Abstract
Cannabis use represents a major public health issue throughout the globe. Yet, we still lack the most fundamental knowledge on long-term effects of cannabis on neural, cognitive, and behavioral function. Part of this stems from how cannabis has been measured historically. To this end, most empirical examinations of cannabis have consolidated all types of cannabis collectively. However, this approach obscures differences in how cannabinoids operate. In this commentary, we address the contrasting properties of tetrahydrocannabinol (THC) and cannabidiol (CBD) and their opposing effects on cognitive function. In addition, we address the increase in cannabis potency throughout the past two decades and how that impacts generalizability of early data to evaluations of contemporary public health. We underscore the urgent need for future research to disaggregate examination of THC from CBD, along with the importance of measuring cannabis potency to more effectively unravel its influence on cognitive function and other health issues.
Keywords: Cannabis, Delta-9-tetrahydrocannabinol, Cannabidiol, Potency, Cognition, Memory, Learning
This paper is a commentary on the review “A systematic review of the effect of cannabidiol on cognitive function: Relevance to schizophrenia” that evaluated preclinical and clinical literature on the effects of cannabidiol (CBD) on cognitive domains relevant to schizophrenia, and points to the ability of CBD to improve cognition across multiple disorders (Osborne et al., 2017). We seek to use the opportunity of this commentary to extend the implications of these findings to the field of addiction, where the convention in empirical examination is to consolidate all types of cannabis use collectively, despite considerable variations in nature of delta-9-tetrahydrocannabinol (THC) and CBD. The timeliness of this is further supported by the increase in cannabis potency over the past two decades (Dujourdy and Besacier, 2017), which challenges generalizability of data gathered more than 20 years ago on contemporary estimates of the effects of cannabis on cognitive function.
For most quantitative brain and behavioral studies of cannabis, the standard empirical approach within addiction neuroscience and treatment is to collapse all types of cannabis use in collective examinations (National Academies of Sciences, 2017). Thus, individuals who use a wide range of products with varying levels of THC/CBD and across a vast range of potency are assessed together, and outcomes are reported without disaggregating effects for these different types of active ingredients, and/or levels of potency. Importantly, at this time, it is these collective outcomes that are guiding scientific debate and public policy decision-making throughout the globe regarding how cannabis affects brain, cognition, and behavior.
However, this approach obscures real-world differences in how cannabinoids operate. In actuality, cannabis use includes a range of subtypes that vary considerably in potency. This has become particularly evident with the introduction of high potency cannabis types to the market such as sinsemilla or “skunk” that contain high levels of THC (20%) and low levels of CBD (< 0.5%) (Osborne et al., 2017). Cannabis contains more than 80 different cannabinoid compounds, and growing evidence suggests that two of the main cannabinoids, THC and CBD (Fig. 1), display opposing neural, cognitive, and behavioral effects, as reflected in recent comprehensive systematic reviews of CBD’s antipsychotic properties (Iseger and Bossong, 2015) and ability to restore cognitive function (Osborne et al., 2017). While THC is a CB1 and CB2 receptor partial agonist (Pertwee, 2008), CBD is a negative allosteric modulator of the cannabinoid CB1 receptor (Laprairie et al., 2015). Further, THC induces psychotic symptoms and anxiety in healthy volunteers (D’Souza et al., 2004; Morrison et al., 2009), whereas CBD demonstrates antipsychotic and anxiolytic effects (Leweke et al., 2012; Zuardi et al., 2009; Zuardi et al., 2006; Zuardi et al., 1995). Evidence from clinical studies indicates that THC impairs learning and memory (including working memory) in healthy volunteers and cannabis users (D’Souza et al., 2004; Morgan et al., 2012; Morrison et al., 2009), whereas CBD enhances learning and memory and inhibits THC-elicited decline in learning and memory (including working memory) (Das et al., 2013; Englund et al., 2013; Morgan et al., 2012). Moreover, a recent study of cannabis users implicates THC in impaired facial emotional recognition, while CBD improves facial emotional recognition and attenuates THC-induced impairment (Hindocha et al., 2015). These effects are mirrored in functional imaging studies, which reveal opposing acute effects of THC and CBD in areas pivotal to queried cognitive processes including emotional processing (amygdala); salience processing (striatum, hippocampus, prefrontal cortex); and processing of auditory and visual information (auditory and visual cortex) (Bhattacharyya et al., 2010; Borgwardt et al., 2008; Fusar-Poli et al., 2009; Winton-Brown et al., 2011). It is relevant to note however, that research investigating the impact of CBD on human functioning is still sparse and suffers from limitations. For instance, Morgan et al. (2012) base their conclusions on hair samples from users with varying levels of THC and CBD, and Das et al. (2013) only assessed CBD and not its effects on THC. In general, double-blind placebo controlled assessments are needed to improve our knowledge on the impact of THC and CBD, as well as cannabis with and without CBD, on cognition and behavior. Nevertheless, the available studies still reflect critical and relevant cognitive differences that should be further explored in future studies.
Fig. 1.
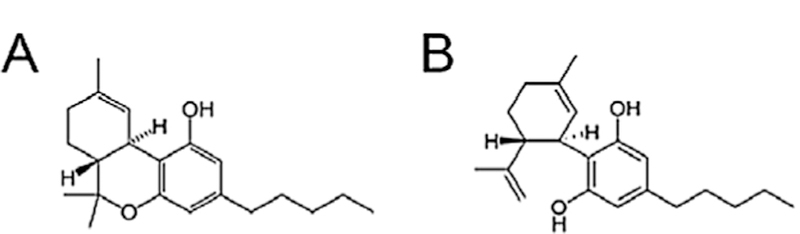
Chemical structure of delta-9-tetrahydrocannabinol (A) and cannabidiol (B). Printed with permission from Hayakawa K, Mishima K, Fujiwara M. − Pharmaceuticals. 2010 Jul;3(7):2197–212. http://dx.doi.org/10.3390/ph3072197, CC BY 3.0, https://commons.wikimedia.org/w/index.php?curid=40172369
At the same time, possible long-term detrimental effects of cannabis on cognitive function continue to be at the center of scientific debate (National Academies of Sciences, 2017). Recent prospective studies (Jackson et al., 2016; Mokrysz et al., 2016) and systematic reviews (Broyd et al., 2016; Curran et al., 2016; National Academies of Sciences, 2017) show limited to mixed findings on the impact of cannabis on cognitive processing, that contrast with highly-cited findings from Meier et al. (2012) linking heavy cannabis use with IQ decline. Importantly, none of these empirical studies disentangled the role of THC from CBD, and/or examined the role of potency (Feldstein Ewing et al., 2017). These types of examinations have yet to be carefully scrutinized in prospective designs to investigate possible long-term effects of cannabis on cognitive functioning. Similarly, an increased focus on disaggregating the role of THC from CBD, and/or the role of potency in studies of acute effects of cannabis, also promises more robust and consistent findings (National Academies of Sciences, 2017).
When examined on a subtype level, cannabis has historically been assigned to two predominant types: herbal cannabis and cannabis resin. These categories contain even more subtypes, which at a minimum, vary considerably in potency (e.g., cannabis plant; shatter). Further, the most comprehensive study available (Dujourdy and Besacier, 2017), which examined cannabis samples from five French forensic police laboratories over 25 years, reflects that during the past two decades, there has been a gradual increase in potency in both subtypes, documented through increases in THC levels as well as calculation of THC/ CBD ratios. In herbal cannabis, mean THC content rose from 2% in 1995–13% in 2016; and in the past four years, the increase in potency in cannabis resin has been dramatic (10% mean THC content in 2009–23% in mid-2016) (Dujourdy and Besacier, 2017). This escalation in cannabis potency is comparable to findings in other European countries (Niesink et al., 2015; Zamengo et al., 2015) and the US (National Academies of Sciences, 2017).
The dramatic increase in potency also presents scientific and public health challenges in the generalizability and extension of early cannabis data on current evaluations of the implication of cannabis use on brain, cognition, and behavior. For example, the dramatic increase in potency in cannabis resin the past four years poses specific challenges in the generalizability of cannabis resin data gathered prior to 2012. We propose that these nuances are, in fact, critical health issues that must be carefully examined and addressed in order to truly begin to co-ordinate and interpret early data on public health from data collected today. At a minimum, these data underscore the urgent need to disaggregate examination of THC from CBD, along with the importance of measuring potency in future studies of cannabis and its impact on cognitive function and other health related issues across the globe.
Acknowledgments
Funding
This work was funded by a block grant for the Danish Ministry for Social Affairs and the Interior (KRT, MBC) and by 3R01AA023658–02S1 from the National Institutes of Health, USA (SWFE). The funding sources had no role in the writing of the manuscript or the decision to submit it for publication.
Footnotes
Conflict of interest
The authors declare no conflict of interest.
References
- Bhattacharyya S, Morrison PD, Fusar-Poli P, Martin-Santos R, Borgwardt S, Winton-Brown T, Nosarti C, CM OC, Seal M, Allen P, Mehta MA, Stone JM, Tunstall N, Giampietro V, Kapur S, Murray RM, Zuardi AW, Crippa JA, Atakan Z, McGuire PK, 2010. Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology 35, 764–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgwardt SJ, Allen P, Bhattacharyya S, Fusar-Poli P, Crippa JA, Seal ML, Fraccaro V, Atakan Z, Martin-Santos R, O’Carroll C, Rubia K, McGuire PK, 2008. Neural basis of Delta-9-tetrahydrocannabinol and cannabidiol: effects during response inhibition. Biol. Psychiatry 64, 966–973. [DOI] [PubMed] [Google Scholar]
- Broyd SJ, van Hell HH, Beale C, Yucel M, Solowij N, 2016. Acute and chronic effects of cannabinoids on human cognition-a systematic review. Biol. Psychiatry 79, 557–567. [DOI] [PubMed] [Google Scholar]
- Curran HV, Freeman TP, Mokrysz C, Lewis DA, Morgan CJ, Parsons LH, 2016. Keep off the grass? Cannabis, cognition and addiction. Nat. Rev. Neurosci 17, 293–306. [DOI] [PubMed] [Google Scholar]
- D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT, Braley G, Gueorguieva R, Krystal JH, 2004. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology 29, 1558–1572. [DOI] [PubMed] [Google Scholar]
- Das RK, Kamboj SK, Ramadas M, Yogan K, Gupta V, Redman E, Curran HV, Morgan CJ, 2013. Cannabidiol enhances consolidation of explicit fear extinction in humans. Psychopharmacology (Berl.) 226, 781–792. [DOI] [PubMed] [Google Scholar]
- Dujourdy L, Besacier F, 2017. A study of cannabis potency in France over a 25 years period (1992–2016). Forensic Sci. Int 272, 72–80. [DOI] [PubMed] [Google Scholar]
- Englund A, Morrison PD, Nottage J, Hague D, Kane F, Bonaccorso S, Stone JM, Reichenberg A, Brenneisen R, Holt D, Feilding A, Walker L, Murray RM, Kapur S, 2013. Cannabidiol inhibits THC-elicited paranoid symptoms and hippocampal-dependent memory impairment. J. Psychopharmacol 27, 19–27. [DOI] [PubMed] [Google Scholar]
- Feldstein Ewing SW, Lovejoy TI, Choo EK, 2017. How has legal recreational cannabis affected adolescents in your state? A window of opportunity. Am. J. Public Health 107, 246–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Crippa JA, Bhattacharyya S, Borgwardt SJ, Allen P, Martin-Santos R, Seal M, Surguladze SA, O’Carrol C, Atakan Z, Zuardi AW, McGuire PK, 2009. Distinct effects of {delta}9-tetrahydrocannabinol and cannabidiol on neural activation during emotional processing. Arch. Gen. Psychiatry 66, 95–105. [DOI] [PubMed] [Google Scholar]
- Hindocha C, Freeman TP, Schafer G, Gardener C, Das RK, Morgan CJ, Curran HV, 2015. Acute effects of delta-9-tetrahydrocannabinol, cannabidiol and their combination on facial emotion recognition: a randomised, double-blind, placebo controlled study in cannabis users. Eur. Neuropsychopharmacol 25, 325–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iseger TA, Bossong MG, 2015. A systematic review of the antipsychotic properties of cannabidiol in humans. Schizophr. Res 162, 153–161. [DOI] [PubMed] [Google Scholar]
- Jackson NJ, Isen JD, Khoddam R, Irons D, Tuvblad C, Iacono WG, McGue M, Raine A, Baker LA, 2016. Impact of adolescent marijuana use on intelligence: results from two longitudinal twin studies. Proc. Natl. Acad. Sci. U. S. A 113, E500–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laprairie RB, Bagher AM, Kelly ME, Denovan-Wright EM, 2015. Cannabidiol is a negative allosteric modulator of the cannabinoid CB1 receptor. Br. J. Pharmacol 172, 4790–4805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leweke FM, Piomelli D, Pahlisch F, Muhl D, Gerth CW, Hoyer C, Klosterkotter J, Hellmich M, Koethe D, 2012. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl. Psychiatry 2, e94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RS, McDonald K, Ward A, Poulton R, Moffitt TE, 2012. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc. Natl. Acad. Sci. U. S. A 109, E2657–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokrysz C, Landy R, Gage SH, Munafo MR, Roiser JP, Curran HV, 2016. Are IQ and educational outcomes in teenagers related to their cannabis use: a prospective cohort study. J. Psychopharmacol 30, 159–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan CJ, Gardener C, Schafer G, Swan S, Demarchi C, Freeman TP, Warrington P, Rupasinghe I, Ramoutar A, Tan N, Wingham G, Lewis S, Curran HV, 2012. Sub-chronic impact of cannabinoids in street cannabis on cognition, psychotic-like symptoms and psychological well-being. Psychol. Med 42, 391–400. [DOI] [PubMed] [Google Scholar]
- Morrison PD, Zois V, McKeown DA, Lee TD, Holt DW, Powell JF, Kapur S, Murray RM, 2009. The acute effects of synthetic intravenous Delta9-tetrahydrocannabinol on psychosis, mood and cognitive functioning. Psychol. Med 39, 1607–1616. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, E., and Medicine, 2017. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research Washington, DC. [PubMed] [Google Scholar]
- Niesink RJ, Rigter S, Koeter MW, Brunt TM, 2015. Potency trends of Delta9-tetrahydrocannabinol, cannabidiol and cannabinol in cannabis in the Netherlands: 2005–15. Addiction 110, 1941–1950. [DOI] [PubMed] [Google Scholar]
- Osborne AL, Solowij N, Weston-Green K, 2017. A systematic review of the effect of cannabidiol on cognitive function: relevance to schizophrenia. Neurosci. Biobehav. Rev 72, 310–324. [DOI] [PubMed] [Google Scholar]
- Pertwee RG, 2008. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br. J. Pharmacol 153, 199–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winton-Brown TT, Allen P, Bhattacharyya S, Borgwardt SJ, Fusar-Poli P, Crippa JA, Seal ML, Martin-Santos R, Ffytche D, Zuardi AW, Atakan Z, McGuire PK, 2011. Modulation of auditory and visual processing by delta-9-tetrahydrocannabinol and cannabidiol: an FMRI study. Neuropsychopharmacology 36, 1340–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamengo L, Frison G, Bettin C, Sciarrone R, 2015. Cannabis potency in the Venice area (Italy): update 2013. Drug Test Anal 7, 255–258. [DOI] [PubMed] [Google Scholar]
- Zuardi AW, Morais SL, Guimaraes FS, Mechoulam R, 1995. Antipsychotic effect of cannabidiol. J. Clin. Psychiatry 56, 485–486. [PubMed] [Google Scholar]
- Zuardi AW, Hallak JE, Dursun SM, Morais SL, Sanches RF, Musty RE, Crippa JA, 2006. Cannabidiol monotherapy for treatment-resistant schizophrenia. J. Psychopharmacol 20, 683–686. [DOI] [PubMed] [Google Scholar]
- Zuardi AW, Crippa JA, Hallak JE, Pinto JP, Chagas MH, Rodrigues GG, Dursun SM, Tumas V, 2009. Cannabidiol for the treatment of psychosis in Parkinson’s disease. J. Psychopharmacol 23, 979–983. [DOI] [PubMed] [Google Scholar]


