Abstract
BACKGROUND:
COPD is common, and inhaled medications can reduce the risk of exacerbations. Incorrect inhaler use is also common and may lead to worse symptoms and increased exacerbations. We examined whether inhaler training could be delivered using Internet-based home videoconferencing and its effect on inhaler technique, self-efficacy, quality of life, and adherence.
METHODS:
In this pre-post pilot study, participants with COPD had 3 monthly Internet-based home videoconference visits with a pharmacist who provided inhaler training using teach-to-goal methodology. Participants completed mailed questionnaires to ascertain COPD severity, self-efficacy, health literacy, quality of life, adherence, and satisfaction with the intervention.
RESULTS:
A total of 41 participants completed at least one, and 38 completed all 3 home videoconference visits. During each visit, technique improved for all inhalers, with significant improvements for the albuterol metered-dose inhaler, budesonide/formoterol metered-dose inhaler, and tiotropium dry powder inhaler. Improved technique was sustained for nearly all inhalers at 1 and 2 months. Quality of life measured with the Chronic Respiratory Questionnaire improved following the training: dyspnea (+0.3 points, P = .01), fatigue (+0.6 points, P < .001), emotional function (+0.5 points, P = .001), and mastery (+0.7 points, P < .001). Coping skills measured with the Seattle Obstructive Lung Disease Questionnaire improved (+9.9 points, P = .003). Participants reported increased confidence in inhaler use; for example, mean self-efficacy for using albuterol increased 3 points (P < .001). Inhaler adherence improved significantly after the intervention from 1.6 at the initial visit to 1.1 at month 2 (P = .045). The pharmacist reported technical issues in 64% of visits.
CONCLUSIONS:
Inhaler training using teach-to-goal methodology delivered by home videoconference is a promising means to provide training to patients with COPD that can improve technique, quality of life, self-efficacy, and adherence.
Keywords: COPD, patient education, self-care, telemedicine, inhaler training
Introduction
COPD is a common respiratory disease in the United States, affecting 12% of adults age ≥ 65 y.1 COPD is characterized by exacerbations that often result in emergency room visits and may require hospitalization. Large clinical trials in COPD have demonstrated that inhaled medications improve symptoms and reduce exacerbations and related hospitalizations.2–6
Each inhaled COPD medication is delivered by an inhaler device that requires correct technique to deliver the medication to the lungs. Unlike oral medications, using an inhaler is a skill that must be taught and reinforced. Many patients use more than one inhaler and are thus required to learn multiple different sets of instructions. Over 90% of COPD patients do not use their inhalers correctly,7–10 and errors in use are associated with worse symptoms and increased hospitalizations.11 Because of this, COPD guidelines recommend inhaler teaching and review at clinic visits and on discharge from the hospital after an exacerbation.12 Unfortunately, a third of patients never receive instructions on inhaler use.13 Up to 69% of patients say their provider has never observed them using their inhalers,14 and many clinical providers are themselves not familiar with how to use the inhaler devices.15–19
Face-to-face counseling on proper inhaler technique has been found to be more effective than reading instructional package inserts or watching instructional videos.20 Although health-care providers, such as primary care physicians, pulmonologists, and nurses, may be able to educate patients, many may lack familiarity with inhaled medications or lack the time to provide this training.18 Pharmacists frequently provide inhaler education,21 and due to their specialized skills, experience, and training, respiratory therapists are also well-suited to provide inhaler education.15,16,22
The educational method used by a health-care provider for inhaler training may be important. Teach-to-goal (TTG) is an educational method with repeated cycles in which patients are observed using their inhaler, provided feedback, and then observed again.10 Inhaler training by TTG has been shown to improve inhaler technique for patients being discharged after an asthma or COPD hospitalization.9 Because studies have also shown that improved skill declines after a single session, multiple educational sessions may be warranted.7 Additionally, repeated instruction has been linked to better medication adherence and health-related quality of life in COPD.23
Traveling to a medical facility to see a trained provider for medical care may be a significant barrier for many patients.24 Therefore, the purpose of this study was to determine the feasibility and acceptability of a videoconferencing inhaler education program delivered at the patient's home and whether the training improved inhaler technique, patient self-efficacy, and health-related quality of life.
QUICK LOOK.
Current knowledge
Many patients with COPD do not use their inhalers correctly, increasing the risk for exacerbations. Although guidelines recommend that patients have inhaler technique reviewed regularly, many patients do not receive inhaler education. Videoconferencing has been used to provide education to patients in their own home and may allow more COPD patients to receive inhaler training.
What this paper contributes to our knowledge
Three monthly inhaler training visits were provided by a pharmacist via videoconference, and the education was acceptable to and feasible for participants. Inhaler technique improved both within each visit and over the 2-month study period. Compared with baseline values, quality of life, self-confidence in inhaler use, and self-reported adherence improved after the intervention.
Methods
Setting/Participants
This pre-post study was conducted at the Veterans Affairs Puget Sound Health Care System in Seattle, Washington. Between November 2014 and June 2015, study staff screened medical records and mailed potentially eligible participants an invitation letter. Participants were contacted by telephone to further assess eligibility, and those who met criteria were invited to participate in the study. Eligibility criteria included: (1) COPD diagnosis, (2) age > 40 y, (3) ≥ 10 pack-year smoking history, (4) COPD-related inhaler used at least once a week, (5) access to a computer with high-speed Internet and email address, (6) enrollment in a primary care clinic, and (7) urban residence. Exclusion criteria included: (1) primary diagnosis of asthma, (2) uncontrolled psychiatric illness, (3) nursing home residence, (4) dementia, and (5) < 1-y life expectancy or receiving hospice care. The study was reviewed and approved by the Veterans Affairs Puget Sound institutional review board (approval 00727), and all participants provided informed consent.
Inhaler Training
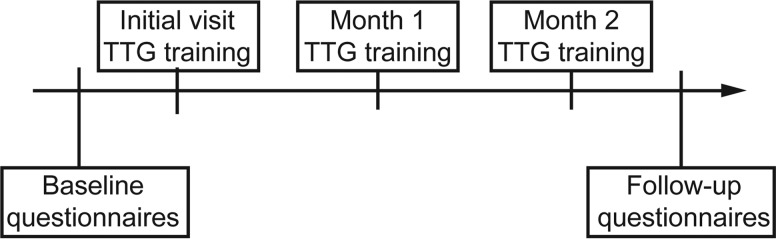
If they did not already have one, participants were mailed a web camera. A technician from the Veterans Affairs Telehealth Department scheduled a telephone visit to help the participant download the videoconferencing software (Cisco Jabber Video for TelePresence 4.5 software) and to complete a test videoconferencing visit. Training was given for prescribed inhalers. After the initial visit, most participants were offered a spacer. Participants were to complete 3 monthly videoconferencing visits (Fig. 1) with a study pharmacist trained in TTG methodology.
Fig. 1.
Study timeline. TTG = teach-to-goal.
The TTG method breaks down the technique for each inhaler into a standardized checklist of 12–17 steps, depending on the inhaler.7,9,10 With pharmacist input, the checklists were adapted. Each TTG training visit began with the pharmacist assessing the participant's baseline inhaler technique and assigning a pre-training score. The pharmacist then demonstrated correct technique and gave verbal instruction. After that educational intervention, the participant re-demonstrated inhaler technique, and each round was assigned a score of post-training 1, post-training 2, etc. The training was repeated until the participant demonstrated mastery (missed ≤ 2 steps) or after 3 cycles. TTG scores were used both as an educational tool to assist with inhaler training and as an objective measure of inhaler technique.
Data Collection/Measurements
Questionnaires.
Participants completed mailed questionnaires at baseline and when their training sessions were completed, generally 2 months after the baseline data collection occurred.
At baseline, COPD severity was measured with the COPD severity score (score range 0–35; higher score = more severe COPD).25 Because the COPD severity score was originally validated using telephone responses, we compared participant written responses with telephone responses from the first 18 participants. Also at baseline, participants reported the number of exacerbations in the last year that were treated with prednisone and/or antibiotics and those requiring an emergency department visit or hospitalization. Dyspnea was measured using the modified Medical Research Council dyspnea scale (1 item, score range 0–4; higher score = worse shortness of breath).26 Alcohol use was assessed using the Alcohol Use Disorders Identification Consumption Test (3 questions, score range 0–12; unhealthy alcohol use = score ≥3 for women and ≥4 for men).27–29 Health literacy was measured with 1 item on self-reported confidence filling out medical forms (from extremely to not at all; the response of “somewhat” or less indicates inadequate health literacy).30 Comorbidity was ascertained with the Charlson comorbidity index31,32 (weighted range 0–36 with 1 point for COPD omitted from all scores; higher score = greater risk for 1-y mortality or higher resource use).
At baseline, and again after finishing the training sessions, participants completed mailed questionnaires including: (1) The 20-item Chronic Respiratory Disease Questionnaire measuring 4 domains (dyspnea, fatigue, emotional function, and mastery) of COPD-specific quality of life (each domain has a range of 1–7; higher score = better health-related quality of life)33,34; (2) the 4-item Seattle Obstructive Lung Disease Questionnaire coping skills scale, an additional measure of COPD quality of life (range 0–100; higher score = better coping)35; (3) a 10-point Likert scale rating participant self-efficacy, or confidence in their ability to use each inhaler correctly (0 = not confident to 10 = very confident); and (4) the 4-item (yes/no) inhaler adherence questionnaire36 (range 0–4, higher score = worse adherence).
In addition, after participants completed the training sessions, change in confidence in inhaler technique over the study period was assessed using a global rating of change scale (1-item, score range −7 to +7; higher score = improvement) as well as participant satisfaction with the program (23 questions).
Modified Mini-Mental State Examination.
To evaluate whether cognitive impairment affected study results, the Modified Mini-Mental State Examination37 was administered by the research coordinator with slight adjustments made for videoconference administration. The Modified Mini-Mental State Examination is a 100-point, global cognitive measure with higher scores indicative of better cognitive function. In a sample of > 2,000 community-dwelling adults without dementia age 65–69 y, the mean Modified Mini-Mental State Examination score was 90.0 ± 7.6,38 and a cut-off of 87 has been suggested as providing maximal sensitivity to dementia.39
Spirometry.
If available, we abstracted spirometry results from the electronic medical record.
Analyses
We computed descriptive statistics of demographic and baseline factors, including means, SD values, and proportions. To assess the improvement in inhaler technique, we used a Wilcoxon signed-rank test for the following 2 comparisons of TTG scores: (1) within-visit comparisons between pre-training TTG scores and the post-training scores for each inhaler during a single inhaler training session and (2) between-visit comparisons of pre-training TTG scores to assess the durability of the training at 1-month and 2-month time points. Because not all participants with metered-dose inhalers (MDIs) used a spacer at each visit, and some changed from no spacer to using a spacer at their second or third visit, we combined the TTG scores with and without spacers for participants using either an albuterol MDI or a budesonide/formoterol MDI for the analyses.
Self-reported baseline and final inhaler quality of life and adherence were compared using a paired t test; self-reported baseline and final self-efficacy were compared with a Wilcoxon signed-rank test. All analyses were completed using Stata 14 (StataCorp, College Station, Texas).
Results
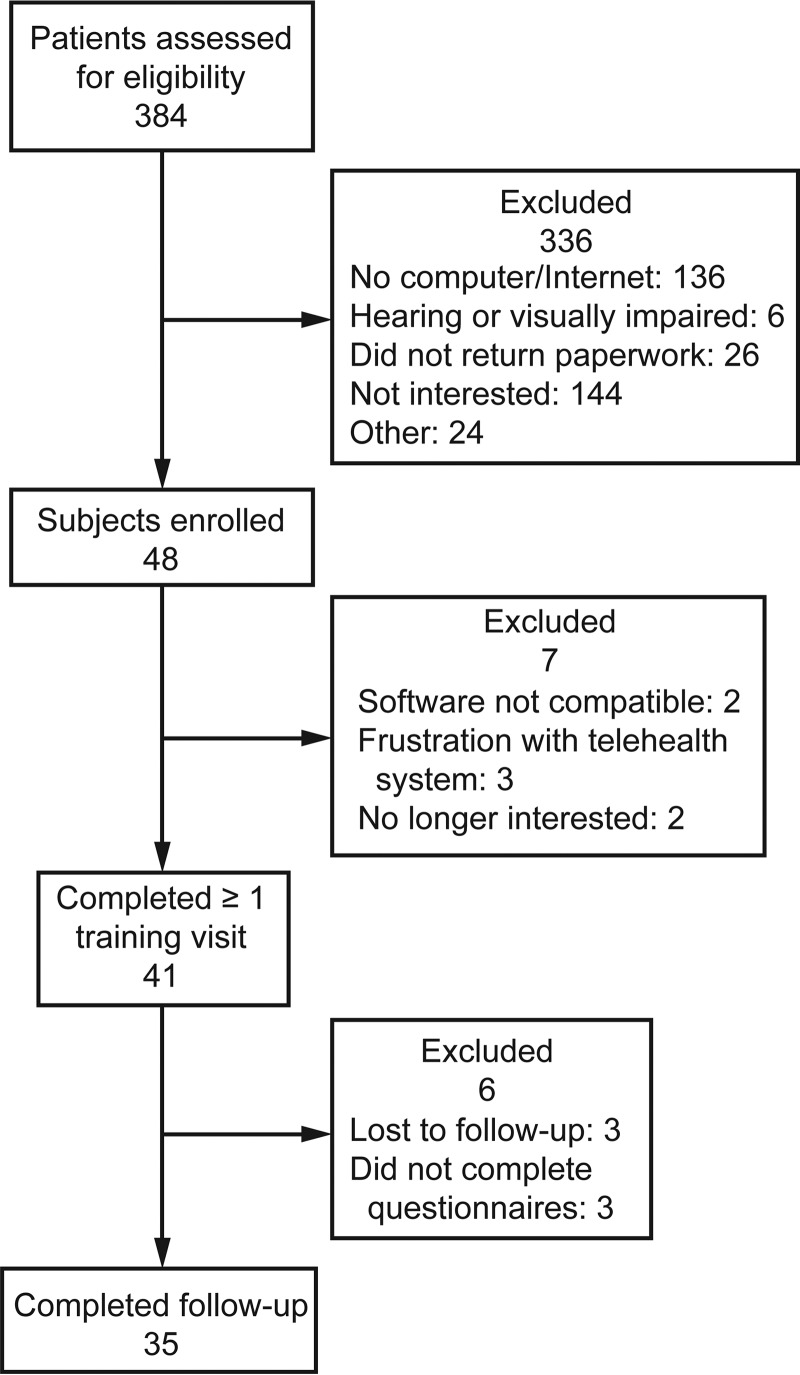
Of 384 patients contacted by telephone and invited to participate in the study, 35% (n = 136) did not have a computer or Internet access, 37% (n = 144) were not interested in participating, and 8% (n = 30) were ineligible for other reasons (Fig. 2). Required enrollment documents were completed by 48 patients (12.5%), although 7 withdrew before the intervention due to technical difficulties on the test call or frustrations with the videoconferencing software. Forty-one participants had at least one Internet-based home videoconferencing visit, 38 (77%) completed all 3 visits, with 35 who also completed questionnaires.
Fig. 2.
Flow chart.
For each participant, an initial test visit was scheduled and completed by a telehealth technician. Inhaler training visits with the pharmacist occurred during a half-day clinic. During each half-day clinic, an average of 2.5 ± 1.5 participants had visits with an average time for each inhaler training visit of 33.7 ± 11.8 min. A study coordinator contacted all participants the day before their visit to remind them of their appointment and was available throughout the half-day clinic to assist with any technical issues experienced by the participant.
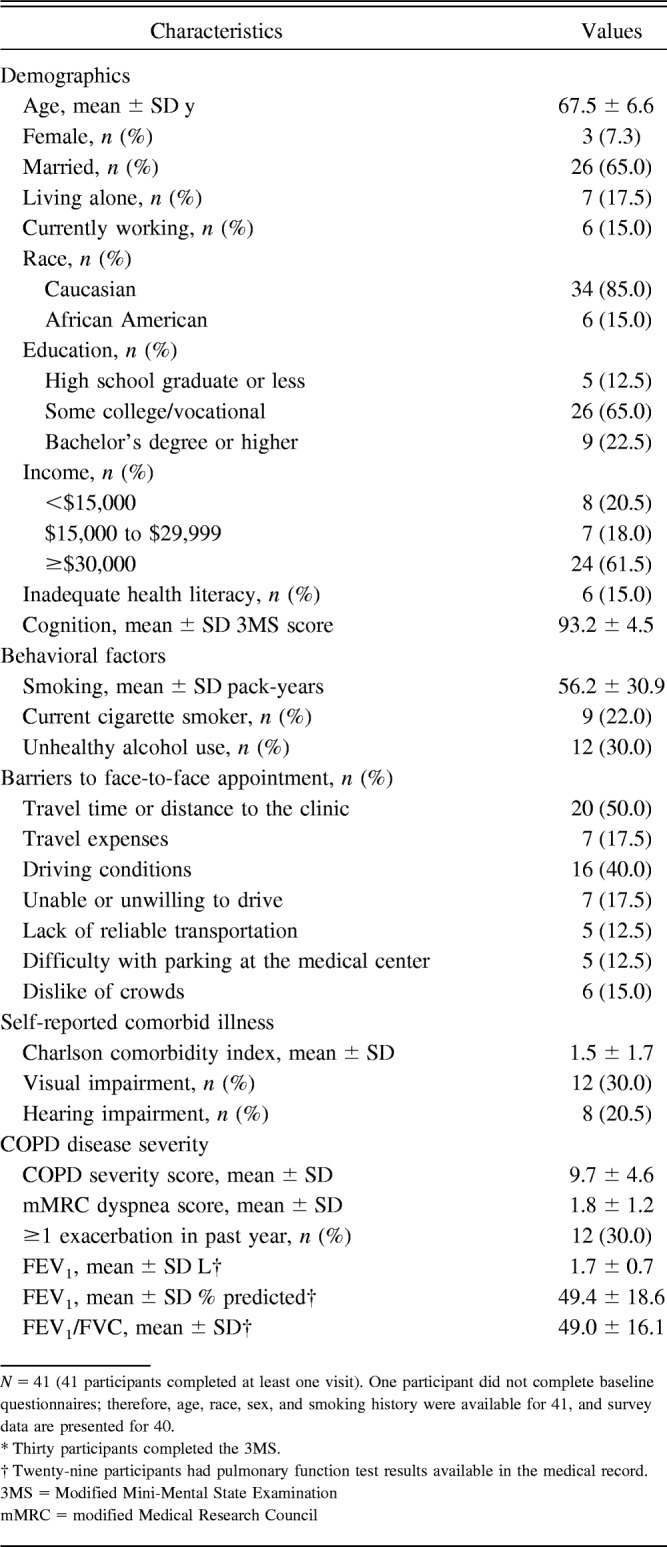
Participants were predominantly male (93%) and white (85%) with a mean age of 67.5 y; 22% were current smokers (Table 1). More than 87% had attended some college, and 15% had evidence of inadequate health literacy. Average cognitive function score among 30 (73%) Modified Mini-Mental State Examination completers was 93.2 ± 4.5, suggesting that this sample had intact global cognition. Concerns about travel time and distance to the clinic were barriers to receiving inhaler training for 50% of participants. The mean COPD severity score was 9.7 ± 4.6, and among 29 participants with spirometry results in the medical record, the mean percent-of-predicted FEV1 was 49 ± 19%.
Table 1.
Characteristics of Study Participants
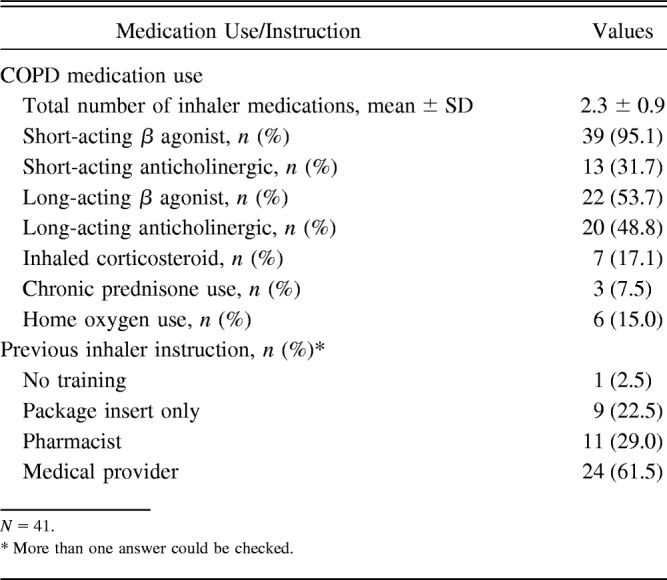
Participants were trained on their current prescription inhalers: short-acting β agonists were prescribed to 39 participants (95%), and 22 (54%) and 20 (49%) were prescribed a long-acting β agonist and long-acting anticholinergic, respectively (Table 2). The average number of inhaled medications prescribed per participant was 2.3 ± 0.9; 2.5% reported never having received inhaler training, and 22.5% reported having gotten instructions on using their inhalers from the package insert only.
Table 2.
COPD Medication Use of Study Participants
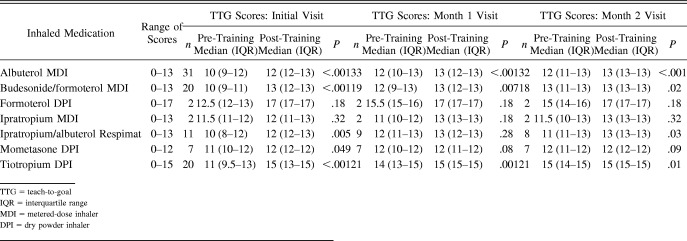
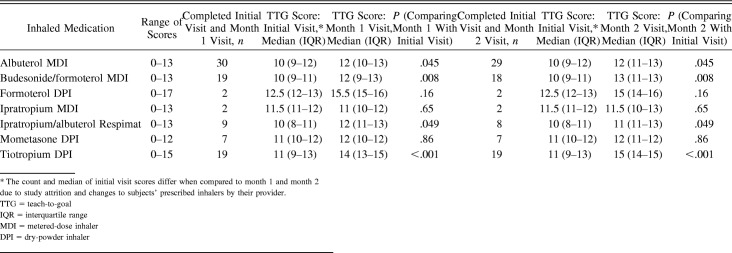
Initial visit pre-training TTG scores ranged from a median (interquartile range) of 10 (9–12) for the albuterol MDI (possible range 0–13) to 12.5 (12–13) for the formoterol dry powder inhaler (possible range 0–17) (Table 3). During the initial visits, repeated TTG scores significantly improved for all inhalers, except for the formoterol dry powder inhaler and ipratropium MDI, which were each only used by 2 participants, limiting statistical analyses due to small sample size (see Table 3). Significant improvement in TTG scores within inhaler training visits continued to occur during the second and third visits. Over time, pre-training inhaler technique scores improved from the initial visits to month 1 and month 2 for nearly all inhalers (Table 4). For example, albuterol MDI TTG pre-training scores significantly increased from 10 at the initial visit to 12 (P = .045) at month 1 and remained improved at month 2 (10–12, P = .045). Similar results were seen for ipratropium/albuterol Respimat (10 at initial visit improved to 11 at month 2, P = .049) and the tiotropium dry powder inhaler (11 at initial visit improved to 15 at month 2, P < .001).
Table 3.
Change in Inhaler Technique During Each Visit: A Comparison of Median Pre- and Post-Test Inhaler Training Teach-to-Goal Scores Within Each Training Visit
Table 4.
Durability of Inhaler Training: Change in Median Pre-Training Teach-to-Goal Scores at Each Visit Comparing Initial Visit With Month 1 and Initial Visit With Month 2, Assessed Before Any Training Provided by the Pharmacist
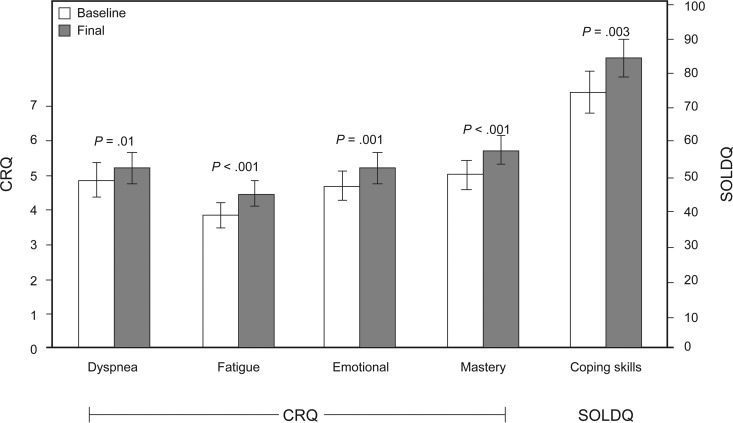
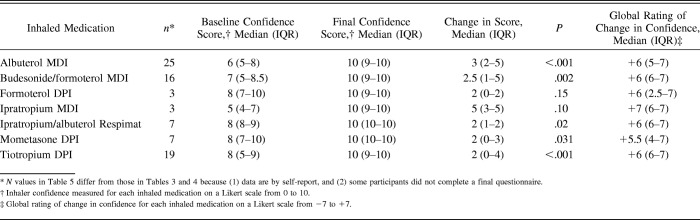
COPD-specific quality of life after the 2-month training period showed both statistical and clinically meaningful improvements in all 4 Chronic Respiratory Disease Questionnaire domains (Fig. 3). The Chronic Respiratory Disease Questionnaire dyspnea scale improved by 0.3 points (P = .01), the fatigue scale improved by 0.6 points (P < .001), the emotional function scale improved by 0.5 points (P = .001), and mastery improved by 0.7 points (P < .001). The Seattle Obstructive Lung Disease Questionnaire COPD coping skills increased from 74.5 at baseline to 84.4 at month 2 (mean improvement 9.9 ± 18.4, P = .003) (see Fig. 3). Self-efficacy in using inhalers improved at 2 months (P < .05 for all except formoterol and ipratropium) (Table 5). For example, median self-efficacy for albuterol MDI increased by 3 points (P < .001) after the intervention period. Self-reported global change in confidence, measuring the extent that participant confidence in technique has improved or deteriorated as a result of study activity, suggested significantly improved confidence (+5.5 to +7 for all inhalers, on a scale from −7 to +7). Overall self-reported adherence measured with a 4-item instrument also improved significantly after the intervention from 1.6 at baseline to 1.1 at month 2 (mean improvement −0.5 ± 1.4, P = .045).
Fig. 3.
Improvement in quality of life from baseline to 3-month follow-up. SOLDQ = Seattle Obstructive Lung Disease Questionnaire, CRQ = Chronic Respiratory Disease Questionnaire.
Table 5.
Comparison of Inhaler Self-Efficacy at Baseline and Final Questionnaire and Global Rating of Change in Inhaler Confidence
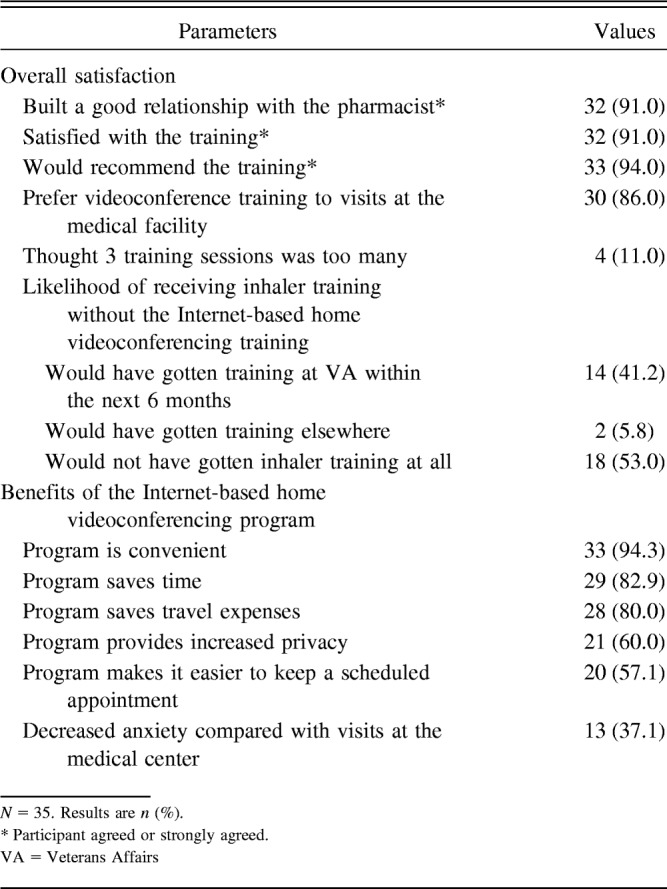
Most participants agreed that setting up the equipment was easy (91%), but 8 (23%) reported technical problems > 50% of the time (Table 6). Five appointments were rescheduled due to technical issues. Of completed visits, the pharmacist reported technical issues in 64% of visits lasting from 1 to 69 min. Technical issues included problems with the software program and glitches with the audio and video feed as well as participant-level issues, such as difficulty navigating the steps necessary to log in to Internet videoconference visits and unfamiliarity with basic computer skills. Despite technology-related issues, overall participant satisfaction was high: 91% were satisfied with the training, and 94% would recommend the training to others (Table 7). More than half (53%) said that they would not have received any inhaler training without this intervention, and 86% would rather have training in their home setting instead of traveling to the Veterans Affairs facility for instruction.
Table 6.
Technical Issues With Internet-Based Home Videoconferencing as Reported by Participants and Pharmacist
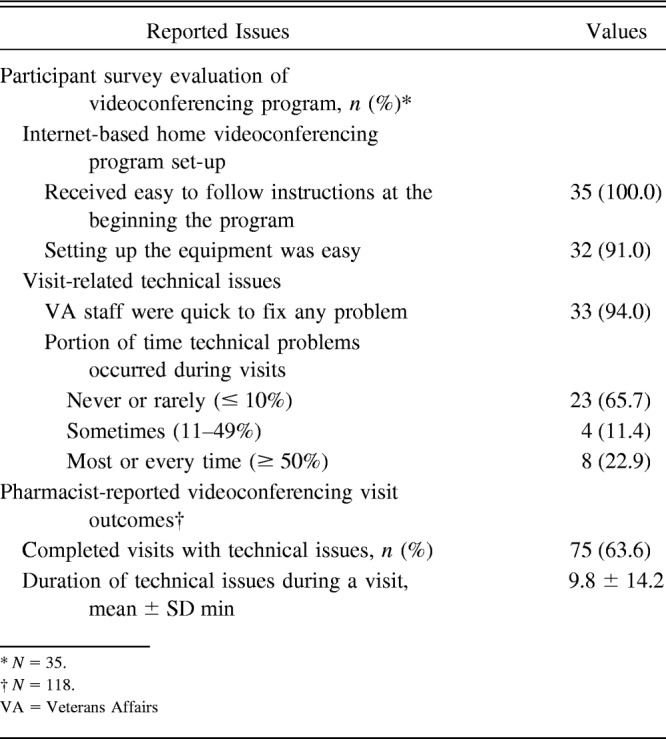
Table 7.
Participant Evaluation of the Telehealth Internet-Based Home Videoconferencing Inhaler Training Program
Because the COPD severity score was originally validated using telephone responses, we compared participant written responses with telephone responses from the first 18 participants. Among these, the mean written COPD severity score was 9.2 ± 3.4, and the mean telephone COPD severity score was 8.5 ± 3.7, with a correlation of 0.63 (P = .003). We present the written COPD severity scores in Table 1.
Discussion
Inhaler training provided by a pharmacist using home videoconference technology in this pilot study improved inhaler technique during each participant visit, and improvements were sustained at the 1- and 2-month videoconference visits. In addition, participants reported improvements in COPD self-efficacy, COPD health-related quality of life, and inhaler adherence following the inhaler training.
Previous studies using the TTG inhaler training method in hospitalized patients showed reduced inhaler misuse immediately following education that was maintained at 90 d follow-up.7,9 This study extended those findings by testing TTG inhaler training using home videoconference technology in the out-patient setting and found significant improvements in inhaler technique sustained at month 1 and 2 follow-up. Repeated training visits reinforced technique and were acceptable to the participants, with only 11% reporting that 3 visits were too many.
The out-patients in this study had better baseline inhaler technique than hospitalized patients. For example, participants had albuterol MDI median scores of 10 of 13 steps correct, compared with 92% misuse observed in hospitalized patients.7 This is consistent with literature showing that patients with worse inhaler technique and therefore worse adherence are more likely to be hospitalized.40 Good baseline technique may be explained by previous inhaler training, as reported by the study participants: 29.0% received instruction from a pharmacist, 61.5% received instruction from another medical provider, and 22.5% learned by reading the package insert. Additionally, most participants in this study had a high education level (87.5% with at least some college education), a socioeconomic factor that has been linked to better inhaler technique.8,11,41,42
Despite good baseline technique, participants in this study still benefited from inhaler training, evidenced by increased TTG scores and better COPD-related quality of life. This supports clinical guidance that patients using inhalers should have their technique assessed at regular intervals and receive training if not using inhaled medications optimally.12,43
The improvement in inhaler technique was accompanied by improvements in self-efficacy, or the self-confidence that participants had using their inhalers. Although baseline self-efficacy in inhaler use was relatively high (range 5–8), scores increased for all inhalers after the intervention, indicating that even a user who feels confident can improve. Self-efficacy is a key component in behavior change,44 which implies that the improvement in inhaler technique, along with reinforcement over 3 visits, may be sustained during everyday use, resulting in the improvements in quality of life seen at the end of the study period. As seen previously,9,14,45 participants appeared to overestimate their baseline inhaler technique, and when asked to make a global assessment of change, the median change was very positive (+5.5 to +7 on a scale of −7 to +7).
Videoconferencing may permit increased access to needed inhaler training for patients by providing teaching at home using Internet video technology. In the United States, 10–50% report that lack of transportation (ie, poor geographical access to care) is an important potential barrier to receiving needed health-care services, resulting in missed appointments.24 Lack of transportation may be particularly important for the elderly,24 who often have a higher prevalence of chronic lung diseases, such as COPD. In our sample, we found that 50% of participants reported transportation-related barriers to receiving inhaler training, including travel time or distance to the clinic.
In addition to addressing needs of patients with barriers to accessing care at the medical center, there may be other groups that are likely to benefit from home videoconferencing training. For example, low health literacy is associated with poor COPD inhaler technique, and patients with low health literacy may be more likely to benefit from inhaler training.10,46,47 Only 15% of the included participants had evidence of inadequate health literacy; thus, this study was not able to fully explore this hypothesis. Although cognitive impairment is associated with poor inhaler adherence,48 cognition function of study participants was high; thus, it is unknown whether videoconference inhaler training can be successful for persons with cognitive impairment. Future research may determine whether provision of training to caregivers might improve adherence among those with dementia or those who score poorly on the Modified Mini-Mental State Examination.
At least 35% of patients who were invited to participate reported that they had no access to either a computer or the Internet, and technical difficulties with the videoconferencing software occurred frequently. Older patients may have reservations about computers, web cameras, and other technology.49 Strategies to increase participation in a home videoconference inhaler training program could include providing tablets to participants, simplifying the videoconferencing software, using secure cell phone applications, and minimizing the number of mailed enrollment documents needed to participate in the program.
Before the study videoconference visits, participants had some inhaler training. However, ongoing education is important, and more than half reported that without the home videoconferencing program, they would not have received any inhaler training. Home videoconferencing, in which providers communicate with patients at home in a live interactive format, has been primarily used in mental health50 and in rehabilitation delivery.51,52 Videoconferencing for inhaler training is an attractive potential approach because it allows providers to observe patients using an inhaler, something that cannot be done over the telephone.
Almost all participants (> 90%) were satisfied with the training and would recommend it to others. Although program satisfaction was high, 64% of participants experienced technical issues that included difficulties logging in and problems with the video image or audio connection. These technical difficulties delayed or lengthened visits and required ongoing technical support, and they will need to be addressed in future interventions.
In this study, inhaler training was provided by a pharmacist trained in the TTG method. Non-interactive, passive inhaler training videos are available on the Internet, and Veterans Affairs developed YouTube training videos for some inhalers in 2016. However, recent data suggest that in-person instruction is superior to having a patient watch a video20; therefore, there may be a benefit to the interaction with a provider to changing patient behavior and improving inhaler technique. Prior studies of TTG used trained research staff,7,9,10 but studies in both adults and pediatrics show that training provided by respiratory therapists using similar checklists also results in inhaler technique improvements.53–55 For any providers giving inhaler training, continuing professional education is essential to maintain their own knowledge and to ensure confidence and competency.18,19,56,57
This study had several strengths, including high rates of follow up, examining technique for up to 7 rescue and controller devices, and examining retention of learning after 3 visits over a 2-month period. This study also had potential limitations. As a feasibility study with a small sample size, and because participants were on different inhalers, there were some inhalers that were only used by a few participants, and we were limited in the ability to compare TTG scores and self-efficacy for those inhalers. The pre-post design for this pilot study also has limitations inherent to this study design, such as the placebo effect, Hawthorne effect, and inability to establish causation because of the lack of a control group. Therefore, this inhaler training approach should be tested in a prospective randomized clinical trial. If the home Internet-based videoconference inhaler training intervention is found to be effective, an implementation strategy using analytic control chart methods may help to ensure that patients with COPD who are treated with inhalers continue to receive appropriate inhaler training over time.58
This intervention included 3 monthly TTG trainings, with improvement seen within each visit. However, how long patients will maintain technique improvement is unknown, as is the appropriate interval for repeated training. Also, the minimum clinically important difference in TTG scores has not been established. However, although the changes in TTG scores were modest, we did find clinically important improvements in quality of life scores measured with the Chronic Respiratory Disease Questionnaire at the end of the intervention period, suggesting that even modest improvements in TTG scores may lead to improvements in symptoms and respiratory-related quality of life. Resource burden is an important consideration; future studies are needed to analyze costs involved with providing training via home videoconference. Additionally, improved technique was accomplished when trained pharmacists performed visits, but it is not known whether the same can be accomplished with other clinical staff. Finally, results of this study might have limited generalizability to populations who are younger, female, lower income, racial/ethnic minorities, or less educated.
Conclusions
This pilot study showed that inhaler training provided by a pharmacist using TTG methodology delivered by novel home Internet-based videoconference technology is a promising approach to improving inhaler technique for patients with COPD that can improve objective measures of inhaler technique both within a single visit and also sustained over time and was accompanied by improved participant self-efficacy in inhaler use and quality of life. Future research is needed to compare this inhaler training approach with other inhaler training interventions and to examine whether TTG training delivered by videoconferencing could improve other clinical outcomes, such as exacerbations.
Footnotes
This research was funded by Department of Veterans Affairs Grant VA HSR&D PPO 13-384 and supported by National Institutes of Health K23 Grant HL118151. The authors have disclosed no conflicts of interest. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government. This material is the result of work supported by resources from the Veterans Affairs Puget Sound Health Care System, Seattle, Washington.
References
- 1. Centers for Disease Control and Prevention. Chronic obstructive pulmonary disease among adults–United States, 2011. MMWR Morb Mortal Wkly Rep 2012;61(46):938–943. [PubMed] [Google Scholar]
- 2. Mackay AJ, Hurst JR. COPD exacerbations: causes, prevention, and treatment. Immunol Allergy Clin North Am 2013;33(1):95–115. [DOI] [PubMed] [Google Scholar]
- 3. Burge PS, Calverley PM, Jones PW, Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ 2000;320(7245):1297–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007;356(8):775–789. [DOI] [PubMed] [Google Scholar]
- 5. Aaron SD, Vandemheen KL, Fergusson D, Maltais F, Bourbeau J, Goldstein R, et al. Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2007;146(8):545–555. [DOI] [PubMed] [Google Scholar]
- 6. Puhan MA, Bachmann LM, Kleijnen J, Ter Riet G, Kessels AG. Inhaled drugs to reduce exacerbations in patients with chronic obstructive pulmonary disease: a network meta-analysis. BMC Med 2009;7:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Press VG, Arora VM, Trela KC, Adhikari R, Zadravecz FJ, Liao C, et al. Effectiveness of interventions to teach metered-dose and Diskus(R) inhaler technique: a randomized trial. Ann Am Thorac Soc 2016;13(6):816–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pothirat C, Chaiwong W, Phetsuk N, Pisalthanapuna S, Chetsadaphan N, Choomuang W. Evaluating inhaler use technique in COPD patients. Int J Chron Obstruct Pulmon Dis 2015;10:1291–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Press VG, Arora VM, Shah LM, Lewis SL, Charbeneau J, Naureckas ET, Krishnan JA. Teaching the use of respiratory inhalers to hospitalized patients with asthma or COPD: a randomized trial. J Gen Intern Med 2012;27(10):1317–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Press VG, Arora VM, Shah LM, Lewis SL, Ivy K, Charbeneau J, et al. Misuse of respiratory inhalers in hospitalized patients with asthma or COPD. J Gen Intern Med 2011;26(6):635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med 2011;105(6):930–938. [DOI] [PubMed] [Google Scholar]
- 12. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007;176(6):532–555. [DOI] [PubMed] [Google Scholar]
- 13. Wieshammer S, Dreyhaupt J. Dry powder inhalers: which factors determine the frequency of handling errors? Respiration 2008;75(1):18–25. [DOI] [PubMed] [Google Scholar]
- 14. Souza ML, Meneghini AC, Ferraz E, Vianna EO, Borges MC. Knowledge of and technique for using inhalation devices among asthma patients and COPD patients. J Bras Pneumol 2009;35(9):824–831. [DOI] [PubMed] [Google Scholar]
- 15. Chopra N, Oprescu N, Fask A, Oppenheimer J. Does introduction of new “easy to use” inhalational devices improve medical personnel's knowledge of their proper use? Ann Allergy Asthma Immunol 2002;88(4):395–400. [DOI] [PubMed] [Google Scholar]
- 16. Hanania NA, Wittman R, Kesten S, Chapman KR. Medical personnel's knowledge of and ability to use inhaling devices: metered-dose inhalers, spacing chambers, and breath-actuated dry powder inhalers. Chest 1994;105(1):111–116. [DOI] [PubMed] [Google Scholar]
- 17. Plaza V, Sanchis J. Medical personnel and patient skill in the use of metered dose inhalers: a multicentric study: CESEA Group. Respiration 1998;65(3):195–198. [DOI] [PubMed] [Google Scholar]
- 18. Leung J, Bhutani M, Leigh R, Pelletier D, Good C, Sin DD. Empowering family physicians to impart proper inhaler teaching to patients with chronic obstructive pulmonary disease and asthma. Can Respir J 2015;22(5):266–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Basheti IA, Armour CL, Reddel HK, Bosnic-Anticevich SZ. Long-term maintenance of pharmacists' inhaler technique demonstration skills. Am J Pharm Educ 2009;73(2):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Axtell S, Haines S, Fairclough J. Effectiveness of various methods of teaching proper inhaler technique: the importance of pharmacist counseling. J Pharm Pract 2017;30(2):195–201. [DOI] [PubMed] [Google Scholar]
- 21. Erickson SR, Landino HM, Zarowitz BJ, Kirking DM. Pharmacists' understanding of patient education on metered-dose inhaler technique. Ann Pharmacother 2000;34(11):1249–1256. [DOI] [PubMed] [Google Scholar]
- 22. Guidry GG, Brown WD, Stogner SW, George RB. Incorrect use of metered dose inhalers by medical personnel. Chest 1992;101(1):31–33. [DOI] [PubMed] [Google Scholar]
- 23. Takemura M, Mitsui K, Itotani R, Ishitoko M, Suzuki S, Matsumoto M, et al. Relationships between repeated instruction on inhalation therapy, medication adherence, and health status in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2011;6:97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013;38(5):976–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Eisner MD, Trupin L, Katz PP, Yelin EH, Earnest G, Balmes J, Blanc PD. Development and validation of a survey-based COPD severity score. Chest 2005;127(6):1890–1897. [DOI] [PubMed] [Google Scholar]
- 26. Fletcher CM. The clinical diagnosis of pulmonary emphysema: an experimental study. Proc R Soc Med 1952;45(9):577–584. [PubMed] [Google Scholar]
- 27. Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, et al. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med 2003;163(7):821–829. [DOI] [PubMed] [Google Scholar]
- 28. Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res 2007;31(7):1208–1217. [DOI] [PubMed] [Google Scholar]
- 29. Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking: Ambulatory Care Quality Improvement Project (ACQUIP): Alcohol Use Disorders Identification Test. Arch Intern Med 1998;158(16):1789–1795. [DOI] [PubMed] [Google Scholar]
- 30. Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 2008;23(5):561–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 32. Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care 1996;34(1):73–84. [DOI] [PubMed] [Google Scholar]
- 33. Williams JE, Singh SJ, Sewell L, Guyatt GH, Morgan MD. Development of a self-reported Chronic Respiratory Questionnaire (CRQ-SR). Thorax 2001;56(12):954–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Guyatt GH, Berman LB, Townsend M, Pugsley SO, Chambers LW. A measure of quality of life for clinical trials in chronic lung disease. Thorax 1987;42(10):773–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tu SP, McDonell MB, Spertus JA, Steele BG, Fihn SD. A new self-administered questionnaire to monitor health-related quality of life in patients with COPD: Ambulatory Care Quality Improvement Project (ACQUIP) Investigators. Chest 1997;112(3):614–622. [DOI] [PubMed] [Google Scholar]
- 36. Brooks CM, Richards JM, Kohler CL, Soong SJ, Martin B, Windsor RA, Bailey WC. Assessing adherence to asthma medication and inhaler regimens: a psychometric analysis of adult self-report scales. Med Care 1994;32(3):298–307. [DOI] [PubMed] [Google Scholar]
- 37. Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry 1987;48(8):314–318. [PubMed] [Google Scholar]
- 38. Bravo G, Hébert R. Age- and education-specific reference values for the Mini-Mental and modified Mini-Mental State Examinations derived from a non-demented elderly population. Int J Geriatr Psychiatry 1997;12(10):1008–1018. [DOI] [PubMed] [Google Scholar]
- 39. Tschanz JT, Welsh-Bohmer KA, Plassman BL, Norton MC, Wyse BW, Breitner JC, Cache County Study Group. An adaptation of the modified mini-mental state examination: analysis of demographic influences and normative data: the cache county study. Neuropsychiatry Neuropsychol Behav Neurol 2002;15(1):28–38. [PubMed] [Google Scholar]
- 40. Vestbo J, Anderson JA, Calverley PM, Celli B, Ferguson GT, Jenkins C, et al. Adherence to inhaled therapy, mortality and hospital admission in COPD. Thorax 2009;64(11):939–943. [DOI] [PubMed] [Google Scholar]
- 41. Sestini P, Cappiello V, Aliani M, Martucci P, Sena A, Vaghi A, et al. Prescription bias and factors associated with improper use of inhalers. J Aerosol Med 2006;19(2):127–136. [DOI] [PubMed] [Google Scholar]
- 42. Westerik JA, Carter V, Chrystyn H, Burden A, Thompson SL, Ryan D, et al. Characteristics of patients making serious inhaler errors with a dry powder inhaler and association with asthma-related events in a primary care setting. J Asthma 2016;53(3):321–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med 2017;195(5):557–582. [DOI] [PubMed] [Google Scholar]
- 44. Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol 2001;52:1–26. [DOI] [PubMed] [Google Scholar]
- 45. Pinto Pereira L, Clement Y, Simeon D. Educational intervention for correct pressurised metered dose inhaler technique in Trinidadian patients with asthma. Patient Educ Couns 2001;42(1):91–97. [DOI] [PubMed] [Google Scholar]
- 46. Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns 2003;51(3):267–275. [DOI] [PubMed] [Google Scholar]
- 47. Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest 1998;114(4):1008–1015. [DOI] [PubMed] [Google Scholar]
- 48. Sulaiman I, Cushen B, Greene G, Seheult J, Seow D, Rawat F, et al. Objective assessment of adherence to inhalers by COPD patients. Am J Respir Crit Care Med 2017;195(10):1333–1343. [DOI] [PubMed] [Google Scholar]
- 49. Smith A. Older adults and technology use. Pew Research Center, April 2014. http://www.pewinternet.org/2014/04/03/older-adults-and-technology-use/ Accessed June 7, 2017. [Google Scholar]
- 50. Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry 2013;170(3):256–262. [DOI] [PubMed] [Google Scholar]
- 51. Chen J, Jin W, Dong WS, Jin Y, Qiao FL, Zhou YF, Ren CC. Effects of home-based telesupervising rehabilitation on physical function for stroke survivors with hemiplegia: a randomized controlled trial. Am J Phys Med Rehabil 2017;96(3):152–160. [DOI] [PubMed] [Google Scholar]
- 52. Frederix I, Hansen D, Coninx K, Vandervoort P, Vandijck D, Hens N, et al. Medium-term effectiveness of a comprehensive internet-based and patient-specific telerehabilitation program with text messaging support for cardiac patients: randomized controlled trial. J Med Internet Res 2015;17(7):e185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Song WS, Mullon J, Regan NA, Roth BJ. Instruction of hospitalized patients by respiratory therapists on metered-dose inhaler use leads to decrease in patient errors. Respir Care 2005;50(8):1040–1045. [PubMed] [Google Scholar]
- 54. Minai BA, Martin JE, Cohn RC. Results of a physician and respiratory therapist collaborative effort to improve long-term metered-dose inhaler technique in a pediatric asthma clinic. Respir Care 2004;49(6):600–605. [PubMed] [Google Scholar]
- 55. Shrestha M, Parupia H, Andrews B, Kim SW, Martin MS, Park DI, Gee E. Metered-dose inhaler technique of patients in an urban ED: prevalence of incorrect technique and attempt at education. Am J Emerg Med 1996;14(4):380–384. [DOI] [PubMed] [Google Scholar]
- 56. Basheti IA, Qunaibi EA, Hamadi SA, Reddel HK. Inhaler technique training and health-care professionals: effective long-term solution for a current problem. Respir Care 2014;59(11):1716–1725. [DOI] [PubMed] [Google Scholar]
- 57. Silver PC, Kollef MH, Clinkscale D, Watts P, Kidder R, Eads B, et al. A respiratory therapist disease management program for subjects hospitalized with COPD. Respir Care 2017;62(1):1–9. [DOI] [PubMed] [Google Scholar]
- 58. Provost LP. Analytical studies: a framework for quality improvement design and analysis. BMJ Qual Saf 2011;20(Suppl 1):i92–i96. [DOI] [PMC free article] [PubMed] [Google Scholar]