Abstract
The 2014–2019 Prevention Research Centers (PRC) Program Funding Opportunity Announcement stated that “all applicants will be expected to collaborate with CDC to collect data to be able to perform cost analysis.” For the first time in the 30-year history of the PRC Program, a cost indicator was included in the PRC Program Evaluation and a cost analysis (CA) instrument developed. The PRC-CA instrument systematically collects data on the cost of the PRC core research project to eventually answer the CDC PRC Program Evaluation question: “To what extent do investments in PRCs support the scalability, sustainability, and effectiveness of the outcomes resulting from community-engaged efforts to improve public health?” The objective of this article is to briefly describe the development of the PRC-CA instrument. Data obtained from the PRC-CA instrument can be used to generate cost summaries to inform decision making within the PRC Program and each individual PRC.
Keywords: cost analysis, economic evaluation, evaluation, evaluation methods, monitoring and evaluation, performance monitoring and reporting system, Prevention Research Centers
In September 2014, the Centers for Disease Control and Prevention (CDC) Prevention Research Centers (PRCs) Program started a new 5-year funding cycle (2014–2019) for 26 academic institutions in 24 states.1 PRCs are located at academic institutions with either an accredited school of public health or an accredited medical school with a preventive medicine residency program.2
Economic evaluation, such as cost analysis, contributes to public health evidence-based decision making and is an integral part of identifying and measuring the impact of public health activities, as well as their scalability and sustainability potential.3–6 Understanding estimated program costs is as important as identifying the size and characteristics of population reached and project impact when deciding on which public health strategies to implement.5,6
In response to the increased demand for economic evidence for public health practice, the 2014–2019 PRC Funding Opportunity Announcement (FOA) stated that “all applicants will be expected to collaborate with CDC to collect data to be able to perform cost analysis.”7 For the first time in the PRC Program’s 30 years, a cost indicator for the PRC core research project is included in the CDC PRC Program evaluation plan. The cost indicator helps answer the PRC Program evaluation question, “To what extent do investments in PRCs support the scalability, sustainability, and effectiveness of the outcomes resulting from community-engaged efforts to improve public health?” This question is operationalized through the PRC core research project cost analysis (PRCCA), and a PRC core research project cost analysis instrument (PRC-CA instrument) was developed and implemented.
The PRC-CA instrument is a module of a larger data collection and reporting system for the overall PRC Program evaluation, called Prevention Research Centers Program Evaluation and Reporting System (PRC-PERS). PRC-PERS is a centralized Web-based data collection system hosted on a secure CDC server; it has audit trails, analyzable data sets through queries, and reporting for various stakeholders. Here, we describe the PRC-CA, as well as the development and implementation of the PRC-CA instrument.
PRC Core Research Project Cost Analysis
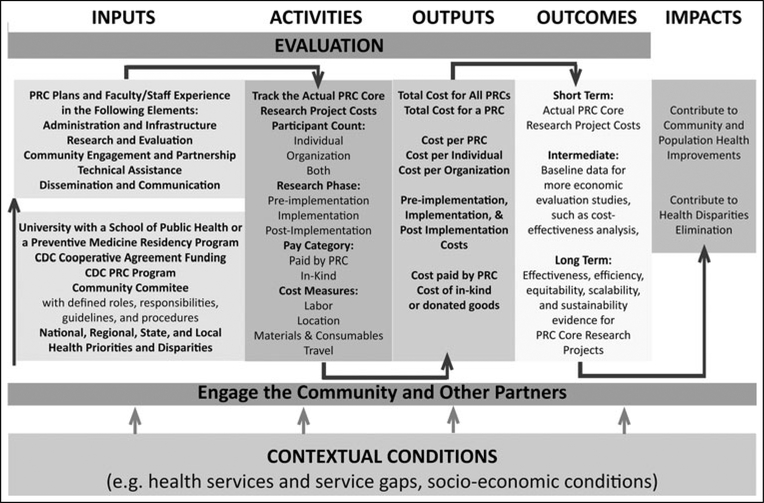
The purpose of the PRC-CA is to measure the cost of the core research project and to obtain baseline data for further economic studies such as cost-effectiveness analysis. We created a logic model (Figure) for the PRC-CA to operationalize data collection through the development and implementation of the PRC-CA instrument. The PRC-CA instrument captures the dollars spent on labor, materials and consumables, travel, and location expenses associated with the PRC core research project (Table).
FIGURE.
PRC Core Research Project Cost Analysis Logic Model
Abbreviations: CDC, Centers for Disease Control and Prevention; PRC, Prevention Research Center.
TABLE.
Prevention Research Centers Cost Analysis Instrument Cost Measures Descriptions
| Measures | Descriptions | Pay Category |
|---|---|---|
| Labor | The salary and wage of each individual involved with the PRC core research project. Collected on the basis of 2 options: Salary based: Labor cost reported as an individual’s fully loaded salary and percent full-time equivalent spent on a particular activity. A fully loaded salary is the sum of a base salary and any additional compensation such as fringe benefits, endowment accounts, or discretionary funds, which reflect an individual’s full expertise. Hourly based: Labor cost reported as an individual’s hourly wage, working on the PRC core research project. |
PRC paid: Faculty and staff who play active roles in the PRC core research project and are directly compensated with PRC dollars. In-kind: Subject matter experts who lend their expertise to the PRC core research project and are not directly compensated with PRC dollars. Volunteers: Any other individuals who took part in the PRC core research project activities and did not get any direct or indirect compensation fortheir contributions. For example, a volunteer might be a student or community member who recruited PRC core research project participants without getting paid. |
| Materials and consumables | Costs of products or services regularly used and durable or capital goods associated with the PRC core research project. |
PRC paid: Any expenses paid directly with PRC dollars. In-kind: Any donated or gifted materials and consumables, travel, and location costs used for the PRC core research project. |
| Travel | Travel expenses incurred while working on the PRC core research project. | |
| Location | Sum of the percentage of the cost for the primary PRC location attributed to conducting PRC core research project activities and expenses for places or settings outside the PRC office associated with PRC core research project. |
Abbreviation: PRC, Prevention Research Center.
PRC-CA Instrument Development
We developed the PRC-CA instrument as a flexible data collection instrument that can support both retrospective and prospective data elements. Data collection systems used to capture research quality data for public health strategies such as the PRC core research project exist.8–14 We used the Public Health Return on Investment (PH ROI) tool8,9 and the Substance Abuse Services Cost Analysis Program (SASCAP)10 to guide the PRC-CA instrument development decisions. Both the PH ROI tool and SASCAP contain elements such as those we included in the PRC-CA instrument and its logic model such as labor, and materials and consumables costs.8–10 The PRCs played an important role in the PRC-CA instrument development process, as its end users. We piloted the instrument with principal investigators from 9 PRCs by asking them to review it for content, flow, and burden. Then we analyzed the feedback using inductive qualitative content analyses to identify themes of needed improvement for the PRC-CA instrument.15 Three main themes emerged: clarify the purpose of the PRC-CA instrument; address burden concerns because of lack of flexibility; and provide clear instructions and definitions for the instrument. To address these concerns, we clearly defined the purpose of the PRC-CA instrument: The purpose of the PRC-CA instrument, a module within PRC-PERS, is to systematically collect budget year data on the costs related to the PRC core research project for each of the 5 budget years in the 20142019 funding cycle and to complete a cost analysis as directed by the 2014–2019 FOA. The PRC cost analysis will:
Quantify the cost of the PRC core research project;
Provide baseline data for further economic evaluation studies, such as a cost-effectiveness analysis; and
Develop capacity of each PRC and the CDC PRC Program to use economic evidence to assess the core research project’s effectiveness, efficiency, equitability, scalability, and sustainability.
To address the burden concern, we made data input flexible. PRCs can collect each expense individually as it occurs or as aggregates collected on a monthly, quarterly, semiannual, or annual basis. Finally, we created a companion issue tracking system that allows PRCs to submit any technical issues, content and definition clarification requests, process issues, or any other issues they might encounter with the CDC PRC Program Evaluation Team. Each issue is routed to specific subject matter experts within the team. Any issues or concerns that might be relevant to all PRCs are included in the Frequently Asked Questions section of PRC-PERS. We also defined all data elements within PRC-PERS.
The elements included in the PRC-CA instrument are described in Supplemental Digital Content Appendix A (available at http://links.lww.com/JPHMP/A405). It is important to note that PRCs are different from each other. They use different research types, focus on different health topics, and provide different services. Cost comparisons between different PRCs are not feasible beyond aggregated total cost of PRC core research projects for all PRCs. For each individual PRC, different cost summaries can be obtained, such as cost per participant, or by type (eg, labor or travel).
Supplementary Material
Implications for Policy & Practice.
Public health profession should consider building its capacity to collect and use economic data; for example, through curriculums in public health training programs or professional development trainings. Implementing a cost data collection system such as the PRC-CA instrument could be useful for other public health programs, because:
Economic data inform internal budgetary decisions. For example, which category should an individual PRC invest in while developing, implementing, or disseminating its core research project?
In addition to program effectiveness, economic data strengthen the decision-making process when choosing which evidence-based programs to translate and implement in communities.
Economic data allow public health programs to demonstrate their impact to stakeholders and decision makers at the local, state, and federal levels.
Acknowledgments
The activities described in this article are part of the authors’ regular duties as members of the CDC Prevention Research Centers Program. The authors thank Glen P. Mays, J. Edward Coffield, and Adam G. Skelton for their inputs as subject matter experts in public health economics and decision sciences. The authors also thank the members of the CDC Prevention Research Centers Evaluation Workgroup, CDC Prevention Research Centers Program staff, and principal investigators from 9 Prevention Research Centers (PRCs) (Prevention Research Center at Case Western Reserve University, Tulane Prevention Research Center, University of Alabama at Birmingham Center for the Study of Community Health, Illinois Prevention Research Center, University of Iowa Prevention Research Center, University of North Carolina Center for Health Promotion and Disease Prevention, Rochester Prevention Research Center: National Center on Deaf Health Research, University of South Carolina Prevention Research Center, and West Virginia University Prevention Research Center) for their invaluable inputs and feedback to the PRC Cost Analysis Instrument development and improvement processes.
Footnotes
The authors do not have any conflict of interest and financial disclosure to report. Bish, Chandra, Greenlund, Massoudi, and Rabarison do not have financial disclosures to report. Marcelin was supported by Cooperative Agreement Number U36/CCU300430 from the Centers for Disease Control and Prevention, and the Association of the Schools and Programs of Public Health.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the Association of Schools and Programs of Public Health.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (http://www.JPHMP.com).
References
- 1.Centers for Disease Control and Prevention. CDC awards $19.5 million to Prevention Research Centers nationwide. http://www.cdc.gov/media/releases/2014/p0530-research-centers.html. Accessed April 6, 2017.
- 2.Centers for Disease Control and Prevention. Prevention Research Centers | CDC; https://www.cdc.gov/prc. Published December 19, 2016. Accessed April 6, 2017. [Google Scholar]
- 3.Rabarison KM, Bish CL, Massoudi MS, Giles WH. Economic evaluation enhances public health decision making. Front Public Health. 2015;3:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Committee on Public Health Strategies to Improve Health, Board on Population Health, Public Health, Institute of Medicine. For the Public’s Health: Investing in a Healthier Future. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 5.Frieden TR. Six components necessary for effective public health program implementation. Am J Public Health. 2014;104(1):17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frieden TR. Government’s role in protecting health and safety. N Engl J Med. 2013;368(20):1857–1859. [DOI] [PubMed] [Google Scholar]
- 7.Department of Health and Human Services. Centers for Disease Control and Prevention. RFA-DP-14–001—Health Promotion and Disease Prevention Research Centers. https://www.grants.gov/web/grants/search-grants.html?keywords=Health%20Promotion%20and%20Disease%20Prevention%20Research%20Centers. Accessed February 21, 2017.
- 8.Association of State and Territorial Health Officials. Tool for estimating return on investment (ROI) for public health improvement projects. http://www.astho.org/Million-Hearts/State-Learning-Collaborative-To-Improve-Blood-Pressure-Control/ROIProject-Summary. Accessed April 6, 2017.
- 9.Mays GP. Public health return on investment template—demonstration version. http://works.bepress.com/glen_mays/64. Published 2012. Accessed March 9, 2017.
- 10.Zarkin GA, Dunlap LF, Homsi G. The Substance Abuse Services Cost Analysis Program (SASCAP): a new method for estimating drug treatment services costs. Eval Program Plann. 2004;27(1): 35–43. [Google Scholar]
- 11.Centers for Disease Control and Prevention. Chronic diseasecost calculator version 2. https://www.cdc.gov/chronicdisease/calculator. Published February 10, 2015. Accessed April 6, 2017.
- 12.USDA ERS. Cost estimates of foodborne illnesses. www.ers.usda.gov/data-products/cost-estimates-of-foodborneillnesses.; Accessed April 6, 2017.
- 13.Bernet PM, Singh S. Economies of scale in the production of public health services: an analysis of local health districts in Florida. Am J Public Health. 2015;105(suppl 2):S260–S267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernet PM, Singh S. The Cost of Doing Business: Developing a Cost Model of the Minimum Local Public Health Services Package in Ohio. Columbus, OH: Association of Ohio Health Commissioners; http://www.aohc.net/aws/AOHC/asset_manager/get_file/111721?ver=3118. Published 2013. Accessed October 31, 2017. [Google Scholar]
- 15.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.