Abstract
Background
Persistent (chronic) pain is a frequent complaint in survivors of torture, particularly but not exclusively pain in the musculoskeletal system. Torture survivors may have no access to health care; where they do, they may not be recognised when they present, and the care available often falls short of their needs. There is a tendency in state and non‐governmental organisations' services to focus on mental health, with poor understanding of persistent pain, while survivors may have many other legal, welfare, and social problems that take precedence over health care.
Objectives
To assess the efficacy of interventions for treating persistent pain and associated problems in survivors of torture.
Search methods
We searched for randomised controlled trials (RCTs) published in any language in CENTRAL, MEDLINE, Embase, Web of Science, CINAHL, LILACS, and PsycINFO, from database inception to 1 February 2017. We also searched trials registers and grey literature databases.
Selection criteria
RCTs of interventions of any type (medical, physical, psychological) compared with any alternative intervention or no intervention, and with a pain outcome. Studies needed to have at least 10 participants in each arm for inclusion.
Data collection and analysis
We identified 3578 titles in total after deduplication; we selected 24 full papers to assess for eligibility. We requested data from two completed trials without published results.
We used standard methodological procedures expected by Cochrane. We assessed risk of bias and extracted data. We calculated standardised mean difference (SMD) and effect sizes with 95% confidence intervals (CI). We assessed the evidence using GRADE and created a 'Summary of findings' table.
Main results
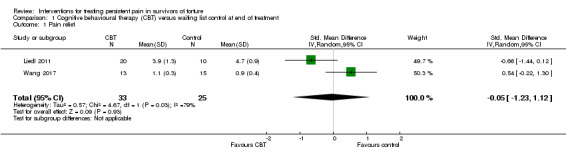
Three small published studies (88 participants) met the inclusion criteria, but one had been retracted from publication because of ethical problems concerned with confidentiality and financial irregularities. Since these did not affect the data, the study was retained in this review. Despite the search including any intervention, only two types were represented in the eligible studies: two trials used cognitive behavioural therapy (CBT) with biofeedback versus waiting list on unspecified persistent pain (58 participants completed treatment), and one examined the effect of complex manual therapy versus self‐treatment on low back pain (30 participants completed treatment). Excluded studies were largely either not RCTs or did not report pain as an outcome.
There was no difference for the outcome of pain relief at the end of treatment between CBT and waiting list (two trials, 58 participants; SMD ‐0.05, 95% CI ‐1.23 to 1.12) (very low quality evidence); one of these reported a three‐month follow‐up with no difference between intervention and comparison (28 participants; SMD ‐0.03, 95% CI ‐0.28 to 0.23) (very low quality evidence). The manual therapy trial also reported no difference between complex manual therapy and self‐treatment (30 participants; SMD ‐0.48, 95% CI ‐9.95 to 0.35) (very low quality evidence). Two studies reported dropouts, one with partial information on reasons; none of the studies reported adverse effects.
There was no information from any study on the outcomes of use of analgesics or quality of life.
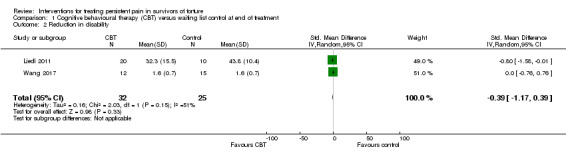
Reduction in disability showed no difference at the end of treatment between CBT and waiting list (two trials, 57 participants; SMD ‐0.39, 95% CI ‐1.17 to 0.39) (very low quality evidence); one of these reported a three‐month follow‐up with no difference between intervention and comparison (28 participants; SMD 0, 95% CI ‐0.74 to 0.74) (very low quality evidence). The manual therapy trial reported superiority of complex manual therapy over self‐treatment for reducing disability (30 participants; SMD ‐1.10, 95% CI ‐ 1.88 to ‐0.33) (very low quality evidence).
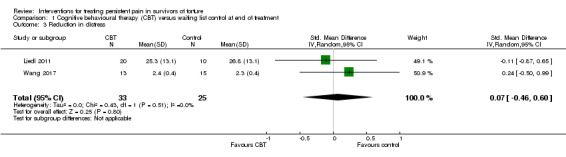
Reduction in distress showed no difference at the end of treatment between CBT and waiting list (two trials, 58 participants; SMD 0.07, 95% CI ‐0.46 to 0.60) (very low quality evidence); one of these reported a three‐month follow‐up with no difference between intervention and comparison (28 participants; SMD ‐0.24, 95% CI ‐0.50 to 0.99) (very low quality evidence). The manual therapy trial reported superiority of complex manual therapy over self‐treatment for reducing distress (30 participants; SMD ‐1.26, 95% CI ‐ 2.06 to ‐0.47) (very low quality evidence).
The risk of bias was considered high given the small number of trials, small size of trials, and the likelihood that each was underpowered for the comparisons it reported. We primarily downgraded the quality of the evidence due to small numbers in trials, lack of intention‐to‐treat analyses, high unaccounted dropout, lack of detail on study methods, and CIs around effect sizes that included no effect, benefit, and harm.
Authors' conclusions
There is insufficient evidence to support or refute the use of any intervention for persistent pain in survivors of torture.
Keywords: Adult; Female; Humans; Male; Middle Aged; Survivors; Torture; Waiting Lists; Biofeedback, Psychology; Biofeedback, Psychology/methods; Chronic Pain; Chronic Pain/etiology; Chronic Pain/therapy; Cognitive Behavioral Therapy; Cognitive Behavioral Therapy/methods; Low Back Pain; Low Back Pain/therapy; Musculoskeletal Manipulations; Musculoskeletal Manipulations/methods; Patient Dropouts; Patient Dropouts/statistics & numerical data; Randomized Controlled Trials as Topic; Randomized Controlled Trials as Topic/ethics; Self Care; Self Care/methods; Stress, Psychological; Stress, Psychological/therapy
Plain language summary
Treating persistent pain in torture survivors
Bottom line
There is no good evidence about any method of treating long‐lasting pain following torture.
Background
Psychological problems following torture, such as depression and post‐traumatic stress disorder (PTSD), receive a lot of attention in refugee healthcare. Physical problems after torture tend to be overlooked by staff trained in mental health care. Survivors of torture often suffer long‐lasting pain, usually affecting muscles and joints.
Study characteristics
We wanted to know whether any treatments were successful in improving pain, and reducing disability and distress in survivors of torture. We searched the academic literature to February 2017 and found three randomised controlled trials (clinical studies where people are randomly put into one of two or more treatment groups).
Key results
Two studies (58 participants) compared cognitive behavioural therapy (CBT; talking therapy that helps people change the way they think and behave) plus learning to control muscles and breathing with no treatment, and we were able to combine these for analysis. Neither study showed any meaningful improvement in pain, reduction in disability, or reduction in distress, over eight to 13 weeks of treatment. One study (30 participants) compared complex manual therapy with self‐treatment for low back pain but could not be combined with the other two studies; it reported no difference in pain relief, but did report that the physical intervention reduced disability and distress at the end of treatment.
Quality of the evidence
We rated the quality of the evidence from studies using four levels: very low, low, moderate, or high. Very low quality evidence means that we are very uncertain about the results. High quality evidence means that we are very confident in the results. The quality of the evidence was very low for pain relief, reduction in distress, and reduction in disability. This was due to the small size of the studies, poor study design, and substantial dropout of participants from studies.
Summary of findings
Summary of findings for the main comparison. CBT with biofeedback ± physical exercise versus waiting list control for pain in torture survivors.
| CBT with biofeedback ± physical exercise versus waiting list control for pain in torture survivors at the end of treatment (data insufficient for analysis at follow‐up) | ||||||
|
Patient or population: adult torture survivors with chronic pain Settings: various Intervention: CBT with biofeedback ± physical exercise Comparison: waiting list | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Intervention | |||||
|
Pain relief At least 30% pain relief or pain < 5/10 Scales: VRS 0‐6; SFMPQ‐PRI (0‐45) |
Not known | The mean change at the end of the intervention was 0.05 standard deviations lower (1.23 lower to 1.12 higher) | ‐ | 58 (2 RCTs) |
⊕⊝⊝⊝ Very low1,2,3 | Change was too small for any clinical relevance. |
| Adverse effects, including dropout and attrition | Not known | No data | ‐ | ‐ | ‐ | Where reasons were given for dropout, they did not constitute adverse effects. |
| Reduced use of analgesics | Not known | No data | ‐ | ‐ | ‐ | No study reported use of analgesics. |
|
Reduction in disability Pain Coping Questionnaire behavioural subscale (12 items: 0‐7); WHODAS‐II (12 items: 1‐5) |
Not known | The mean change in the intervention groups was 0.39 standard deviations lower (1.17 lower to 0.39 higher) | ‐ | 57 (1 missing) (2 RCTs) |
⊕⊝⊝⊝ Very low1,2,3 | This represents < 15% improvement on baseline score. In Liedl 2011, participants still scored only around half of the non‐disabled total; in Wang 2017, participants appeared to have low disability at baseline. |
| Quality of life | Not known | No data | ‐ | ‐ | ‐ | No study reported quality of life. |
|
Reduction in distress PDS (17 items: 0‐3) HTQ‐Part IV (30 items: 1‐4) |
Not known | The mean change in the intervention groups was 0.07 standard deviations higher (0.46 lower to 0.60 higher) | ‐ | 58 (2 RCTs) |
⊕⊝⊝⊝ Very low1,3 | Change was too small for any clinical relevance. |
| Global improvement, satisfaction | Not known | No data | ‐ | ‐ | ‐ | No study reported global improvement/satisfaction. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CBT: cognitive behavioural therapy; CI: confidence interval; FESV: Fragebogen zur Erfassung der Schmerzverarbeitung (German Pain Coping Questionnaire); HTQ: Harvard Trauma Questionnaire; PDS: Post‐traumatic Diagnostic Scale; RCT: randomised controlled trial; SFMPQ‐PRI: Short‐Form McGill Pain Questionnaire ‐ Pain Rating Index; VRS: Verbal Rating Scale; WHODAS‐II: World Health Organization Disability Assessment Schedule. | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different. Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1 Serious limitations in design: loss to follow‐up; completer analysis, not intention‐to‐treat. Downgraded one level for serious limitations and two levels for very serious limitations.
2 Inconsistency: could not explain heterogeneity. Downgraded one level.
3 Imprecision of results: very small sample sizes; wide confidence intervals that included no effect, substantial risk and substantial benefit. Downgraded one level for serious limitations and two levels for very serious limitations.
Background
Reports of torture and other ill‐treatment come from over 150 countries (AI 2010). The International Rehabilitation Council for Torture Victims (IRCT) (IRCT 2010) estimates that around 400,000 torture survivors live in the EU alone, with similar estimates in the USA (Jaranson 1995). Many diverse injuries are inflicted during torture and ill‐treatment, usually in conditions of poor nutrition and hygiene, to a highly stressed person, and without health care. The violence, extent, and complexity of injuries often lie outside medical problems addressed in textbooks and in the scientific literature (Amris 2007), and persistent pain is a common finding in survivors of torture (Amris 2007; Rasmussen 1990). Pain is defined by the International Association for the Study of Pain as "an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage" (IASP 1994). Persistent or chronic pain is commonly defined as pain that is present for more than three months, assuming the initial injury to have healed in that time. In the case of injury from torture, which commonly goes untreated, this may not be the case.
Unlike many other client groups, the health concerns of torture survivors are defined not primarily by diagnosis or recognised classification systems but by their experience of torture and other ill‐treatment. Torture is a deliberate assault upon the body, psyche, identity and integrity of the person, aiming to dehumanise, degrade, destroy, or debilitate and render the person helpless. It is defined by the United Nations Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment (CAT), Article 1 (UN 1984) as "any act by which severe pain or suffering, whether physical or mental, is intentionally inflicted on a person for such purposes as obtaining from him or a third person information or a confession, punishing him for an act he or a third person has committed or is suspected of having committed, or intimidating or coercing him or a third person, or for any reason based on discrimination of any kind, when such pain or suffering is inflicted by or at the instigation of or with the consent or acquiescence of a public official or other person acting in an official capacity. It does not include pain or suffering arising only from, inherent in or incidental to lawful sanctions" (UN 1984). By extension, torture undermines communities and groups whose members are targeted, spreading distrust and fear (Patel 2007). We will use the wider definition from the World Medical Association (WMA 2006): "the deliberate, systematic or wanton infliction of physical or mental suffering by one or more persons acting alone or on the orders of any authority, to force another person to yield information, to make a confession, or for any other reason."
Physical health problems related to torture have been widely documented (Jacobs 2001; Moreno 2002; Norredam 2005; for reviews see Jaranson 2011; Montgomery 2011; Quiroga 2005), as have psychological health problems (e.g. Basoglu 2006; Johnson 2008; Patel 2007). Torture‐related physical health problems not only cause disability and restricted functioning but also produce psychological problems, compounding the impact on overall personal and social functioning. Additionally, torture survivors in countries of exile can experience many social, legal, and practical difficulties (e.g. seeking asylum, being subject to racist attacks, inadequate housing, inability to communicate in the language of the host country, and concerns for family and friends with whom they have lost contact) which may take priority over their health problems; they may also be uncertain about their rights to health care, which may be restricted, and fearful of any perceived authority (Burnett 2001).
Torture survivors may not be recognised as such within the health service (Crosby 2006; Eisenman 2003), and the health care offered or accessible to them falls short of their needs (Amris 2007; Amris 2015; Berliner 2004; Burnett 2001; Quiroga 2005). Psychological services offered by non‐governmental organisations have very variable methods and skills (Patel 2014); both they and mainstream mental health services tend to have a poor understanding of persistent pain, and may attribute it to evident psychological disturbance, in particular post‐traumatic stress.
Description of the condition
Physical torture is in most instances directed towards the musculoskeletal system, aiming at producing soft tissue lesions and pain and usually at leaving either no visible, or non‐specific, findings after the acute stage. Random beatings, systematic beating of specific body parts (head, palms, soles, and lumbar region), strapping/binding, suspension by the extremities, forced positions for extended periods, and electrical torture are frequent (Rasmussen 1990; Williams 2010). Other physical methods include asphyxiation, near‐drowning, stabbing, cutting, burning, and sexual assaults, including hetero‐ and homosexual rape (Olsen 2007; Rasmussen 2006).
Persistent pain in the musculoskeletal system is recognised as one of the most frequent physical complaints presented by torture survivors (Amris 2007; Burnett 2001; Edston 2005; Olsen 2006; Rasmussen 1990; Rasmussen 2006), but other pain has been described and is often hard to classify or describe in terms of mechanism (Amris 2007; Lund 2008; Rasmussen 1990; Williams 2010). Survivors of torture are likely to present with complex and multiple pains, and often with moderate to severe symptoms of depression, anxiety, and traumatic stress (Berliner 2004; el Serraj 1996). There is no basis for the widespread belief that pain from torture is in some way produced by psychological disturbance, other than pain triggered by re‐experiencing traumatic events (Taylor 2013); the origin of pain in torture does however add to the complexity of assessment and treatment (Sjölund 2009).
Description of the intervention
Any treatment intended to relieve pain or improve function despite ongoing pain was a possible intervention. Thus, interventions eligible for this review included pharmacotherapy by various routes (oral, sublingual, topical), peripheral nerve blockade and other injections, physiotherapy, psychological rehabilitative treatment, peripheral stimulation such as transcutaneous electrical nerve stimulation, acupuncture, neuromodulation (including spinal cord stimulation), and complementary and alternative therapies.
How the intervention might work
There is no suggestion that interventions would work differently in survivors of torture than in anyone who is not a survivor of torture, only that pain resulting from torture can be difficult to understand in the light of current knowledge, and that survivors are, because of their experience, often hypersensitive to medical procedures required for diagnosis and treatment.
Why it is important to do this review
In the era of evidence‐based health care, there is considerable emphasis on services providing treatments demonstrated to be effective. However, health care of torture survivors is almost entirely addressed within the psychological literature, with serious neglect of physical sequelae and their treatment. Populations are diverse in cultural, ethnic, religious, and political backgrounds and are often unable to express themselves adequately in the language of the host country. Compared to the many reviews of interventions for psychological problems (see Jaranson 2011; Patel 2014), there are few reviews of interventions for medical problems, and all are either brief and generalised (e.g. Quiroga 2005), or specific to particular injuries or treatments (e.g. Amris 2000a; Amris 2000b). Most of the literature on physical health difficulties experienced by torture survivors (before or without treatment) consists of clinical opinions and case studies (for review, see Mckenna 2012; Mollica 2011). There are also descriptive studies which enumerate the variety of health problems of survivors, often published with the main aim of raising awareness and concern about the issues (Jaranson 2011; Montgomery 2011; Quiroga 2005).
Of more concern here is that in high‐income countries, which have contributed most to the literature on health care for refugee survivors of torture, the focus of clinical and research effort has been on the psychological sequelae, often described in terms of post‐traumatic stress disorder (PTSD), rather than on the physical sequelae. This, combined with the slow spread of understanding of pain mechanisms among some medical and paramedical specialities, including psychology and psychotherapy, means that reported pain is often recorded as a psychosomatic presentation of psychological disorder, reducing usefulness for the pain clinician or researcher.
Objectives
To assess the efficacy of interventions for treating persistent pain and associated problems in survivors of torture.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), cluster RCTs, and quasi‐RCTs. We wished to be as inclusive as possible and, since we expected to find a very small number of RCTs, quasi‐RCTs were included because some methods of quasi‐randomisation used in low‐income country settings are unlikely to introduce bias.
There were no restrictions on publication type, status, language, or date, to maximise search yield. We included conference abstracts and other reports if full details could be obtained from the study authors, as relevant material is often published by torture survivor centres themselves.
Types of participants
Participants must have been identified as survivors of torture or ill‐treatment, consistent with the UN 1984 definition, or at least 50% of the study population identified as such.
Torture survivors may be found among refugees, asylum seekers, war survivors, and survivors of organised violence, and in diverse settings, such as prison, detention centres, refugee camps, accommodation centres, healthcare facilities, and in the community. We included participants of all ages.
Types of interventions
Interventions could be of any modality and provided by any practitioner, or self‐administered, as long as they were primarily aimed at pain relief. Comparators could be any alternative condition: no intervention, waiting list, care as usual, standard care, alternative treatment, or placebo condition. Studies needed to have at least 10 participants in each arm for inclusion.
Types of outcome measures
Primary outcomes
Pain relief or reduction in pain as reported by the participant, without which the study was not eligible for inclusion in this review. Pain or pain relief may have been measured by any type of scale: numerical (including percentage), verbal, or pictorial. The desired outcome was 30% pain relief or pain less than 5/10 or equivalent on a numerical scale, or 'none' or 'mild' on a verbal scale.
Adverse effects, including dropout or attrition.
Secondary outcomes
Reduced use of analgesics, as rescue analgesia or ongoing analgesic intake.
Reduction in disability, improved overall function, reduced interference of pain with normal life, or improved quality of life.
Reduction in distress, including anxiety, depression, traumatic stress symptoms, overall mood.
Global improvement, satisfaction, as rated by participant.
Search methods for identification of studies
We conducted searches on electronic databases and websites; we handsearched reviews and reference lists.
Electronic searches
We used Medical Subject Headings (MeSH) or equivalent and text word terms. There were no language restrictions. Searches were tailored to individual databases. The search strategies used can be found in Appendix 2.
We searched the following electronic databases on 1 February 2017:
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 1) via CRSO;
MEDLINE and MEDLINE in Process (via Ovid) 1946 to 1 February 2017;
Embase (via Ovid) 1974 to 1 February 2017;
Web of Science (ISI) SCI, SSCI, A&HCI, CPCI‐S, CPCI‐SSH searched to 1 February 2017;
CINAHL (via EBSCO) 1982 to February 2017;
LILACS (via Bireme)1985 to February 2017;
PsycINFO (via Ovid) 1806 to February week 1 2017.
Searching other resources
We searched the following:
OpenGrey (online database of reports and other grey literature produced in Europe);
trials registers for details of ongoing trials: (www.clinicaltrials.gov); the metaRegister of controlled trials (www.controlled‐trials.com/mrct); the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/);
reference lists of reviews and retrieved full papers;
citation searches on key articles;
Online Library of the Rehabilitation and Research Centre for Torture Victims (RCT, now Dignity);
tables of contents from the top 10 most frequently cited sources emerging from the search (expected to be journal issues).
We contacted or attempted to contact study authors where necessary for additional information.
Data collection and analysis
Selection of studies
Two authors (AW, EB) independently undertook an initial screening of titles and abstracts, using the inclusion criteria, to identify studies which might be eligible and for which the full paper should be obtained. Where abstracts were not available electronically, or were unclear about the criteria applied, we sought the full paper.
Two authors (EB, LH) independently read and selected the full papers using the inclusion criteria. The final list was achieved after comparison, with disagreements resolved by discussion; where there continued to be doubt or difference, a third review author (KA) was consulted to achieve consensus.
We included a Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flowchart to show the status of identified studies (Moher 2009), as recommended in Part 2, Section 11.2.1 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We included studies in the review irrespective of whether the measured outcome data were reported in a 'usable' way.
Data extraction and management
Two authors (EB, LH) independently extracted the following data where available, using a form developed in previous reviews, and checked for agreement before entry into Review Manager 5 (RevMan 2014). Where there was disagreement, a third author (AW or KA, depending on the topic) was consulted to resolve the difference.
Methods: study design.
Methods: sources of bias: sequence generation, allocation sequence concealment, blinding, incomplete outcome data, study size; other concerns about bias were therapist qualification, therapist allegiance, language of assessment.
Participants: sample size at baseline and all post‐treatment assessment points used for analysis; adherence to or participation in treatment; setting of intervention; baseline characteristics of the sample (age, gender, nationality, ethnicity, type of torture experienced, legal status if refugees or asylum seekers, living situation, separation from close family members).
Interventions: number of arms; types of interventions (drugs, doses, intervention technique, or school of therapy); types of placebo/control condition; protocol for intervention; training of practitioner/therapists.
Outcomes: assessment points (collected; reported); self‐report versus other‐report versus objective; psychometric properties of assessment instruments; language(s) of assessment and translation or interpretation.
Number of participants in each intervention group; sample size; missing participants; completion rates.
Funding source; key conclusions of study authors; allegiance of the trial authors.
Assessment of risk of bias in included studies
Two authors (EB, LH) independently assessed risk of bias for each study, using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) and adapted from those used by the Cochrane Pregnancy and Childbirth Group, with any disagreements resolved by discussion. We completed a 'Risk of bias' table for each included study, using the 'Risk of bias' tool in Review Manager 5 (RevMan 2014).
We assessed the following for each study, using three categories: low risk, unclear risk (information not provided or effect not clear), and high risk of bias.
Random sequence generation (checking for possible selection bias): we assessed the method used to generate the allocation sequence as: low risk (any truly random process, e.g. random number table; computer random number generator); unclear risk (method used to generate sequence not clearly stated); high risk (any process that is not truly random, e.g. odd or even year of birth).
Allocation concealment (checking for possible selection bias): the method used to conceal allocation to interventions prior to assignment determines whether intervention allocation could have been foreseen in advance of, or during, recruitment, or changed after assignment. We assessed the methods as: low risk (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes); unclear risk (method not clearly stated); high risk (any method that cannot be adequately concealed, e.g. case record number).
Blinding of participants and personnel (checking for possible performance bias): it is not possible in many psychological and physical treatment trials to blind study personnel. We assessed the methods used to blind participants as: low risk (when equivalence of treatment expectations was demonstrated before treatment started and maintenance of blinding was demonstrated by inaccuracy of post‐treatment guesses at allocation); unclear risk (neither equivalence of treatment expectations or maintenance of blinding was reported, or reported ratings showed lack of equivalent expectations or failure of blinding (or both)); high risk (e.g. trial arms clearly identifiable as treatment or control where control would not generate equivalent expectations of benefit to treatment).
Blinding of outcome assessment (checking for possible detection bias): we assessed the methods used to blind study participants and outcome assessors from knowledge of which intervention a participant received as: low risk (study stated that it was blinded and described the method used to achieve blinding, e.g. identical tablets); unclear risk (study stated that it was blinded but did not provide an adequate description of how it was achieved); high risk (treatment staff performed outcome assessments).
Incomplete outcome data (checking for possible attrition bias due to the amount, nature, and handling of incomplete outcome data): we assessed the methods used to deal with incomplete data as: low risk (less than 10% of participants did not complete the study or used 'baseline observation carried forward' analysis, or both); unclear risk (used 'last observation carried forward' analysis); high risk (used 'completer' analysis).
Selective outcome reporting: we assessed studies as being at low risk (all outcomes reported); unclear risk (information unclear); high risk (one or more outcomes not reported).
Size of study (checking for possible biases confounded by small size): we assessed studies as being at low risk (200 or greater participants per treatment arm); unclear risk (50 to 199 participants per treatment arm); high risk (fewer than 50 participants per treatment arm).
Other. Therapist qualification: we assessed therapist qualification as low risk (where therapists were qualified); unclear risk (qualification not clearly stated); high risk (therapists not adequately trained to deliver treatment). Therapist allegiance: we assessed therapist allegiance as low risk (intervention and comparison used separate therapists or no therapist was required for comparison arm); unclear risk (no information on therapist allegiance to intervention method); high risk (clear allegiance of treating therapist to treatment under investigation). Language of assessment: we assessed language of assessment as low risk (assessment in language of participants); unclear risk (language of assessment not clearly stated or standardised translated questionnaires used in multiple languages); high risk (assessment translated for each patient with no standardisation). The overall rating for the 'Other' category represented the most frequently endorsed risk assessment category.
Measures of treatment effect
We planned to analyse dichotomous outcomes (e.g. improved/not improved) using odds ratios with 95% confidence intervals (CIs), using a random‐effects model, combining into two categories those outcomes with more than two categories. We did not plan to calculate numbers needed to treat for an additional beneficial/harmful outcome.
We analysed continuous data using standardised mean differences (SMDs) or effect sizes, using pooled standard deviations and weighting for sample size, and calculating the 95% CI, using a random‐effects model. We interpreted SMDs individually with reference to the quality and reliability of the measure where available. Where data were severely skewed, we planned to normalise them where possible by transformation or, if this did not produce a satisfactory distribution, to dichotomise them (Higgins 2011 section 9.4.6).
Unit of analysis issues
Where treatments were sufficiently similar, we combined two or more treatment groups into a single treatment group for analysis.
We planned to adjust for the effects of clustering using an intraclass correlation coefficient (ICC) in the case of cluster randomisation.
Dealing with missing data
We contacted or attempted to contact study authors to request missing data required for meta‐analysis.
Where standard deviations were missing and unobtainable from study authors, we planned to calculate them where possible from F, t, or P values, or from standard errors. If this was not possible, we planned to treat the trial as having no useable data. We identified intention‐to‐treat (ITT) analysis as an important marker of effort to reduce bias (see Assessment of risk of bias in included studies).
Assessment of heterogeneity
We interpreted heterogeneity, as indicated by the I² statistic, using the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), with reference to variation between studies.
Assessment of reporting biases
The search strategy was broad, particularly in the grey literature, in an attempt to address publication bias.
Data synthesis
We used Review Manager 5 software to conduct meta‐analysis wherever feasible (RevMan 2014). We used a random‐effects model, given the various sources of diversity. Where meta‐analysis was not possible, we provided a narrative summary of evidence relating to the primary and secondary outcomes.
Grading of evidence
Two authors (LH, AW) independently rated the quality of the outcomes. We used the GRADE system to rank the quality of the evidence using GRADEpro Guideline Development Tool software (GRADEpro GDT 2015), and the guidelines provided in Chapter 12.2 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of the body of evidence for each outcome. The GRADE system uses the following criteria for assigning grade of evidence:
high: we are very confident that the true effect lies close to that of the estimate of the effect;
moderate: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different;
low: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect;
very low: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.
We decreased grade if we identified:
serious (‐1) or very serious (‐2) limitation to study quality;
important inconsistency (‐1);
some (‐1) or major (‐2) uncertainty about directness;
imprecise or sparse data (‐1);
high probability of reporting bias (‐1).
'Summary of findings' table
We included a 'Summary of findings' table to present the main findings in a transparent and simple tabular format. In particular, we included key information concerning the quality of evidence, the magnitude of effect of the interventions examined, and the sum of available data on the outcomes of pain relief, reduction in disability, and reduction in distress at the end of the interventions. We found no information for the outcomes of adverse effects, reduced use of analgesics, change in quality of life, and global improvement/satisfaction. Data were insufficient to analyse outcomes at follow‐up.
Subgroup analysis and investigation of heterogeneity
We planned the following subgroup analyses:
child and adult studies separately, since methods and outcomes usually differ, as does the type of torture experienced;
by types of pain or by treatment modality or specific treatment, or both.
Sensitivity analysis
We planned to test sensitivity by successively removing:
quasi‐RCTs to leave only RCTs;
cluster‐RCTs to leave individually randomised trials;
trials using non‐ITT methods to leave only those analysed using ITT (to be considered ITT analysis, the analysis must have included all participants who entered treatment, whether or not they provided data at the end of treatment: Nuesch 2009 found that trials with ITT analyses produce smaller treatment effects in meta‐analyses, and this difference is greater in meta‐analyses in the presence of heterogeneity);
unpublished trials to leave only studies in peer‐reviewed journals. Some treatment studies in this literature are published in non‐peer‐reviewed sources, such as chapters and internal reports of non‐government organisations. This analysis would address concerns about differences in quality between the two types of source.
Results
Description of studies
Results of the search
The search of the databases (see Methods, Electronic searches) retrieved 3573 records after deduplication. Our search of the trials registers identified five further studies. Our searches of other resources (grey literature, reviews, Dignity online library, contents of 10 most cited journals from electronic searches) identified no additional studies that appeared to meet the inclusion criteria. Our screening of the reference lists of the included publications did not reveal any additional RCTs. Therefore, we had a total of 3578 records.
We excluded 3554 records based on titles and abstracts. We obtained the full text of the remaining 24 records. We excluded 21 studies, with reasons (see Characteristics of excluded studies table). We found no trials to be entered under Characteristics of studies awaiting classification and identified one ongoing study (see Characteristics of ongoing studies table; Phaneth 2016).
We included three studies reported in eight published papers. For a further description of our screening process, see the study flow diagram (Figure 1).
1.
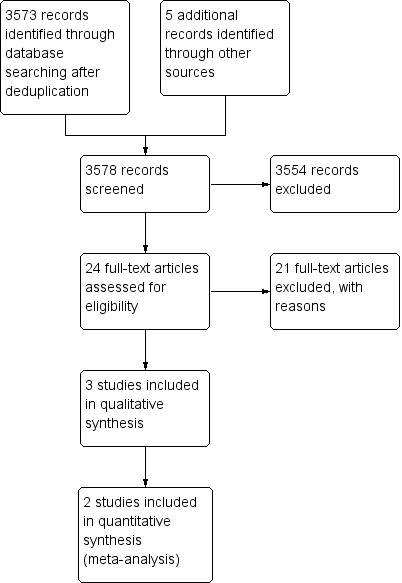
Study flow diagram.
Included studies
Three studies met criteria for inclusion (see Characteristics of included studies table) (Kim 2015; Liedl 2011; Wang 2017). Two provided published data and Wang and coauthors kindly shared data not yet published.
Two studies were conducted in European refugee rehabilitation centres under the umbrella of the IRCT: in Kosovo (Wang 2017), and in Germany/Switzerland (Liedl 2011); the third study was conducted in a treatment centre in Korea (Kim 2015). A retraction was issued (for data mishandling and financial irregularities) in 2013 for Liedl 2011 that included the statement, "Data quality, data analyses, and clinical conclusions drawn from the results were not affected," so we retained the study. The studies had 100 participants at the start of treatment and 88 at the end; the losses were in two studies (Liedl 2011; Wang 2017). The participants in the Korean study were male torture survivors, with a mean age of 61 years (Kim 2015): in the other two studies, participants were predominantly male (57% Liedl 2011; 55% Wang 2017), with a majority of torture survivors (70% Liedl 2011; 80% Wang 2017), in their forties (mean ages 42 years Liedl 2011 and 48 years Wang 2017). In one study, the pain condition was exclusively chronic low back pain (Kim 2015), but in the two other studies the pain condition was described as chronic and was not further elaborated on, though Liedl 2011 excluded neuropathic pain. No study explicitly defined chronic pain.
One study had three arms, the two intervention arms being sufficiently similar to be combined for our analysis (Liedl 2011), while the others each had two. The intervention in two studies consisted of biofeedback‐based cognitive behavioural therapy (CBT) (Liedl 2011; Wang 2017), delivered over 10 sessions of 15 hours in total; signals of muscle activity, breathing, or heart rate were used ('biofeedback') to monitor learning of relaxation and stress management techniques. Liedl 2011 used graduate clinical psychology students trained for the trial and working to a manual. The Liedl 2011 study added physiotherapist‐designed instructions to exercise at home to one of the intervention groups, while the Wang 2017 study added group physiotherapy to the biofeedback‐CBT intervention arm. The control group in both studies was a waiting list with no contact with therapists. The third study described a very different form of intervention, manual therapy designed to stretch and relax muscles and delivered by physiotherapists at least twice a week over eight weeks, with a control group who were provided with exercise instructions to be performed for the same total time as the manual therapy but without a therapist present (Kim 2015).
Therapists and participants spoke the same language in one study (Kim 2015), while interpreters and translation of assessment materials were used for Liedl 2011. Interpreted materials were used by Wang 2017: assessment was by someone who spoke the same language as the participants and it was implied that all therapists spoke the same language. Some details of method and of scoring results were missing from Kim 2015. Attempts to contact the study authors by email and post for clarification were unsuccessful.
Excluded studies
We excluded 16 studies: 10 were not RCTs (Blyhammar 2009; Callaghan 1993; Farrag 2005; Highfield 2012; Hinton 2006; Jansen 2011; Kaysen 2013; Müller 2009 RETRACTED; Phaneth 2014; Schwarz‐Langer 2006), and six did not report the outcome pain relief (Adenauer 2011; Bolton 2014a; Bolton 2014b; Johnson 2001; Taing 2011; Weiss 2015).
Three of the non‐RCTs provided psychoeducation about pain, two for Arabic‐speaking refugees in Swedish treatment centres (Blyhammar 2009; Jansen 2011), and one in Cambodia (Phaneth 2014). Three provided some combination of CBT, biofeedback, and relaxation (Hinton 2006; Müller 2009 RETRACTED; Schwarz‐Langer 2006). One study treated Asian refugees in the US with Chinese traditional medicine, predominantly acupuncture (Highfield 2012).
Ongoing studies
We identified one ongoing study, which was a two‐arm study comparing pain school (education) with a waiting list control for torture survivors in Cambodia (Phaneth 2016). The outcomes are pain relief and reduction in disability.
Risk of bias in included studies
We used standard Cochrane methods for assessing risk of bias (see Figure 2; Figure 3).
2.
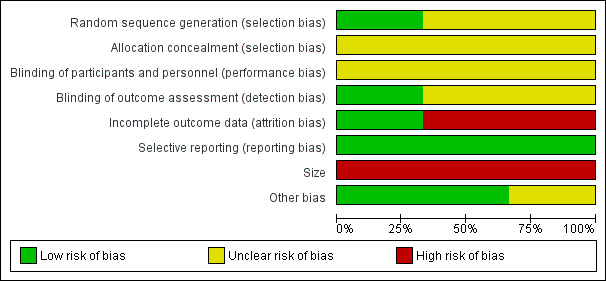
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
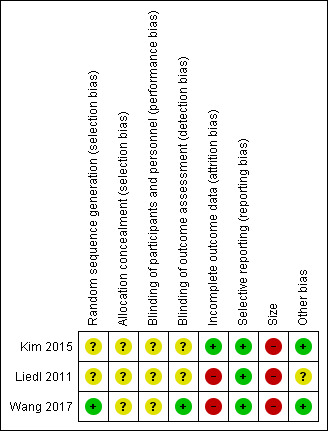
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
One study used a block randomisation method that was rated low risk (Wang 2017). We rated the two other studies as unclear risk: Kim 2015 described a coin toss method used for randomisation but did not explain how this produced equal group sizes, and Liedl 2011 provided no details on randomisation method or information on allocation concealment.
Blinding
Performance bias
There was no information in any study about attempts to blind participants to allocation or to assess their expectation of benefit or post‐treatment guess at allocation group. In the Kim 2015 study, there was a self‐exercise regimen for the control group which might have seemed like an intervention. We would expect that the waiting list control groups in Liedl 2011 and Wang 2017 would have realised that they were not receiving an intervention. Therefore, we rated all three studies at unclear risk of bias.
Detection bias
Since Wang 2017 used an independent psychiatrist speaking the language of participants and blind to which arm participants were in to assess outcomes, it was rated at low risk of bias. Liedl 2011 and Kim 2015 reported assessment of outcomes of interest by self‐report and were rated at unclear risk of bias.
Incomplete outcome data
Kim 2015 reported no withdrawals and was at low risk of bias. Liedl 2011 reported 20% withdrawals and analysed only completers and was at high risk of bias. Wang 2017 analysed data from completers only (82% of participants randomised) but stated that this was an "intent‐to‐treat" analysis. Dropouts from this study were reported but reasons were not stated, despite a specific request to the main author. We rated this study at high risk of bias.
Selective reporting
Kim 2015 and Liedl 2011 reported all the outcome measures listed in their Methods sections, and we found all of the relevant outcomes listed in the Wang 2017 trial protocol, so we rated all three studies at low risk of bias.
Size of study
Numbers of participants ranged from 28 to 30 so all studies were at high risk of bias for size. In no study was the issue of statistical power raised.
Other potential sources of bias
Therapist qualification
We rated two studies at unclear risk since information provided, if any, was insufficient to ascertain therapist qualifications (Kim 2015; Liedl 2011). The third study provided details of therapist professional qualifications and experience so we rated it at low risk of bias (Wang 2017).
Therapist allegiance
We rated all studies at low risk since none of the comparison arms required any substantial therapist involvement.
Language of assessment
We rated two studies at low risk, since they assessed participants in their own language (Kim 2015; Wang 2017). The other study was at unclear risk of bias since at least some questionnaires were translated into several languages at the point of assessment and so were not standardised (Liedl 2011).
Effects of interventions
See: Table 1
For the reported outcomes, we reported SMDs (effect sizes) and 95% CIs, with P values unless they were not significant (ns).
Pain relief
We judged the quality of evidence for pain relief to be very low. At the end of treatment, two studies contributed data to pain relief as an outcome of CBT with biofeedback with or without exercise, compared to waiting list control (Liedl 2011; Wang 2017). There were 58 people included in this analysis, for which both intervention arms of Liedl 2011 were combined. The SMD was ‐0.05 (95% CI ‐1.23 to 1.12; z = 0.09, ns, I² = 79%). The manual therapy study with 30 participants provided an SMD of ‐0.48 (95% CI ‐9.95 to 0.35; z = 1.83, P = 0.07) (Kim 2015). Follow‐up values were only available for Wang 2017: at three months, the SMD was ‐0.03 (95% CI ‐0.28 to 0.23).
We downgraded the quality of evidence by the maximum of three levels: for very small sample size, for imprecision since CIs included no effect, substantial risk and substantial benefit; most risk of bias was unclear due to lack of information; analyses were by completers, not ITT; and the dropout rate was unexplained.
Adverse effects, including dropout or attrition
None of the studies reported adverse effects. One study retained participants to the end of treatment (Kim 2015), while Liedl 2011 lost 6/36 (17%) participants and Wang 2017 lost 6/34 (18%) participants during the study. Wang 2017 reported that one participant found a job, and others left because of illness or surgery; Liedl 2011 gave no reasons.
Reduced use of analgesics
None of the studies reported the levels of analgesic use, though Wang 2017 reported the effect of non‐analgesic medications on other outcomes.
Reduction of disability
We judged the quality of evidence for reduction of disability to be very low. At the end of treatment, two studies measured disability using different scales (behavioural coping subscale for Liedl 2011; WHO disability scale for Wang 2017) at the end of treatment, with 57 participants in the analysis (Liedl 2011; Wang 2017). The SMD was ‐0.39 (95% CI ‐1.17 to 0.39; z = 0.97 ns, I² = 52%). The manual therapy study with 30 participants provided an SMD of ‐1.10 for a translated standard scale of disability (95% CI ‐1.88 to ‐0.33; z = 2.79; P = 0.005) (Kim 2015). None of the studies used either pain‐specific scales or broader quality of life scales. Follow‐up values were only available for Wang 2017: at three months, the SMD was 0 (95% CI ‐0.74 to 0.74; z = 0.00, ns).
We downgraded the quality of evidence by the maximum of three levels: for very small sample size, for imprecision since CIs included no effect, substantial risk and substantial benefit; most risk of bias was unclear due to lack of information; analyses were by completers, not ITT; and the dropout rate was unexplained.
Reduction of distress
We judged the quality of evidence for reduction of distress to be very low. All three studies assessed distress in terms of post‐traumatic stress scales, with additional assessment of depression (Wang 2017), and anxiety (Liedl 2011; Wang 2017). End of treatment values for PTSD were available from two studies using CBT with biofeedback (Liedl 2011; Wang 2017). The SMD was 0.07 (95% CI ‐0.46 to 0.60; z = 0.25, ns, I² = 0%). The manual therapy study also yielded PTSD values (Kim 2015). The SMD was ‐1.26 (95% CI ‐2.06 to ‐0.47; z = 3.12; P = 0.002). Follow‐up values were only available for Wang 2017: at three months, the SMD was ‐0.24 (95% CI ‐0.50 to 0.99; z = 0.64, ns).
We downgraded the quality of evidence by three levels because of serious methodological limitations: for very small sample size, for imprecision since CIs included no effect, substantial risk and substantial benefit; most risk of bias was unclear due to lack of information; analyses were by completers, not ITT; and the dropout rate was unexplained.
Global improvement, satisfaction, as rated by participant
None of the three studies used any assessment of global improvement.
Discussion
Summary of main results
We found only three eligible studies and obtained data for all three, but were only able to combine data for the two similar interventions (biofeedback‐based CBT with or without physiotherapist‐led exercise for mixed chronic pain, compared to waiting list (Liedl 2011; Wang 2017); the third study compared manual therapy for low back pain with exercise at home (Kim 2015). None of the studies demonstrated that their interventions reduced pain, and only the manual therapy study claimed at the end of treatment to have reduced disability and distress.
There were no data on adverse effects, so possible harms were unknown; where reasons were given for attrition from treatment, they did not indicate harm. Outcomes of analgesic use, quality of life, and global satisfaction were also lacking.
Overall completeness and applicability of evidence
Pain is a defining feature of torture and studies of torture survivors set in specialised centres are consistent in reporting a high prevalence of persistent pain, with overall estimates as high as 83% (Olsen 2006; Williams 2010). Yet the research literature on rehabilitation for survivors of torture is predominantly targeted at mental health problems without specific reference to pain. Therefore, we were not surprised to find very few RCTs on the management of post‐torture pain. As expected, most of the available studies were uncontrolled. The evidence obtained from the included RCTs was relevant to the research question, although lacking several outcomes and follow‐up results, and overall at unclear to high risk of bias, providing evidence of very low quality for outcomes of pain relief, reduction in distress, and reduction in disability.
No studies used current evidence on multicomponent pain rehabilitation programmes for chronic pain (Williams 2012), neither did we find any analgesic trials. Interventions appeared to be informed by peripheral models of pain aetiology for which evidence was poor. The enthusiasm for biofeedback is intriguing, since the muscle tension model of chronic pain used in these trials has long been disputed, with recognition that any benefits from relaxation and biofeedback treatment arise from cognitive change, such as gaining a sense of control (Jensen 2014); further, dependence on biofeedback equipment to achieve relaxation can produce poor maintenance over the longer term after the equipment is withdrawn (Newton‐John 1995).
None of the studies provided evidence that either CBT with biofeedback or manual therapy produced pain relief or reduction of disability or distress for survivors of torture with chronic pain. Pain treatment is ideally integrated into multidisciplinary psychosocial rehabilitation in services for torture survivors (Jaranson 2011). There was a wider range of interventions in non‐RCTs, and many excluded studies tested similar psychological interventions to those included, but with psychological rather than pain outcomes. In the wider literature on rehabilitation of survivors of torture, post‐torture pain is often classified as psychosomatic, reflecting a poor understanding of chronic pain and resulting in failure to address potentially treatable pain.
The few trials found selected a narrow range of outcomes, with none reporting use of analgesics or ratings of global improvement, and neglect of adverse effects. Reporting on attrition, including reasons for dropout, was inadequate, leaving unanswered questions about acceptability of and adherence to treatment, and possible harm. Fundamental to the application of a given intervention is the requirement that it be well tolerated and compatible with the person's understanding of the illness, cultural background, and rehabilitation needs: it is not clear that these have been addressed in these studies. Pain after torture can have multiple meanings, and increased knowledge about torture survivors' preferences, perception of and satisfaction with their health outcomes is therefore important.
We had planned to analyse child and adult studies separately, since methods and outcomes usually differ, as does the type of torture experienced. However, our search identified no studies on child survivors of torture, leaving a substantial gap in the evidence.
Characteristics of participants given in the studies included gender, mean age, legal status (refugee or not), and, in two studies (Kim 2015; Wang 2017), nationality/ethnicity. The studies did not mention type of torture experienced, living situation, and separation from close family members.
In all studies, data were continuous, not dichotomous. Only Wang 2017 gave the funding source for their study.
Quality of the evidence
We identified three studies that met the criteria for inclusion, with 88 participants completing treatment. We judged the overall quality of evidence from these studies to be very low, meaning we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect, for the following reasons.
We downgraded the quality of evidence by the maximum of three levels for the outcomes of pain relief and reduction in disability: for limitations in design, for inconsistency, and for imprecision; and by two levels for the outcome of reduction in distress, for limitations in design and for imprecision.
Limitations in design: there was substantial unexplained loss of participants, and completer analysis, rather than ITT. These limitations are likely to lower confidence in the estimate of effect.
Inconsistency: there was unexplained heterogeneity in the outcomes of pain relief and disability, despite very similar interventions.
Imprecision of the estimate, with no or small and clinically irrelevant change and CIs that included no effect, substantial risk, and substantial benefit.
Potential biases in the review process
The extensive nature of our search, including grey literature, gives us confidence that eligible studies were not missed.
Agreements and disagreements with other studies or reviews
We found no systematic reviews covering the effectiveness of interventions for treating persistent pain in survivors of torture. In most of the literature on health care for torture survivors, the focus of clinical and research efforts has been on the psychological sequelae, often described in terms of PTSD or other trauma‐related psychopathology, and not on pain as a significant cause of distress and disability. In accordance with our findings, one Cochrane Review revealed that, based on very low quality evidence, the effects of psychological, social, and welfare interventions for torture survivors are disappointing, producing changes, if any, which fall far short of recovery (Patel 2014). Several methodological issues and constraints were highlighted, including lack of theoretical framework for provided interventions, use of unstandardised assessment methods, and very small sample sizes.
There are several reasons why evidence in this field is limited. Rehabilitation of torture survivors was initiated and carried out mainly by health professionals working in human rights organisations and to date these services remain largely separate from mainstream healthcare provision. Many of these organisations face a constant struggle for resources, with staff under immense pressure to focus on what many perceive as the core task, providing treatment and care. Combining the skills of those who work with torture survivors with those of pain clinicians and researchers provides the best opportunity for building understanding and increasing the effectiveness of treatment and management interventions.
Authors' conclusions
Implications for practice.
For torture survivors with chronic pain
We found no direct evidence for or against either cognitive behavioural therapy (CBT) with biofeedback or manual therapy, for achieving pain relief, reduced disability, or reduced distress. However, there are very few studies, and the quality of evidence they provide is very low.
For clinicians
We found no direct evidence for or against CBT with biofeedback or manual therapy, for achieving pain relief, reduced disability, or reduced distress in survivors of torture, as the interventions were delivered in the three included trials. As in other chronic pain conditions, any pain treatment should be based on thorough assessment and identification of pain mechanisms involved, including of neuropathic pain and sensitisation phenomena, and should aim not only to reduce pain but to improve function and quality of life. Assessment and treatment should, as is recognised best practice, involve a multidisciplinary team. The patient should be asked about possible countertherapeutic associations of particular treatments with torture methods, such as forcible medication or electrical interventions.
A human rights context, with reference to cultural difference in expressing pain and distress and seeking help, and with reference to the personal meaning of torture, is highly desirable as a basis for treatment initiatives.
For policy makers
The small number of randomised controlled trials and the resulting paucity of information means that no conclusions concerning the management of post‐torture pain can be drawn. As recommended for chronic pain in general, an interdisciplinary, multimodal approach to pain management in survivors of torture is probably optimal, with a focus on agreed goals of improved understanding, functioning, and social participation. This should be applied sensitively to patients who may be seriously traumatised.
For funders of the intervention
Rehabilitation after torture is a human right, yet provision is scant even in well‐resourced countries where refugees settle. It is important that best practice from pain treatment in general is extended to torture survivors, and that pain is not mistakenly assumed to be a symptom of post‐traumatic stress and pain treatment neglected in favour of intervention for post‐traumatic stress disorder. Funders can take a role in requiring robust assessment of the outcomes of interventions, and partnerships with academic teams where intervention teams do not have the necessary expertise.
Implications for research.
General implications
The search yielded only three studies, and one more ongoing. All four used psychological and physical therapy methods: none used pharmacotherapy or other medical interventions for pain. This means that we know almost nothing about whether treatments for pain that are otherwise of known effectiveness can also reduce pain and pain‐associated problems in survivors of torture. The impact of torture, flight, and exile are factors that may complicate behavioural and cognitive aspects of pain and disability, and undermine treatment feasibility, adherence, and outcome. Given the large number of refugees in high‐income countries, healthcare services will be treating pain in survivors of torture, although not necessarily identified as such, but without any research literature to guide clinical decisions.
Our understanding of persistent pain from torture is seriously lacking, so we have little to inform development of research questions or interpretation of outcome study data. Despite contributions from forensic and accident medicine, little is known about the long‐term effects of many forms of torture.
Careful studies of torture survivors are beginning to establish connections between some forms of torture and persistent pain, better described by mechanism than by site (Amris 2015), and this could be used to advance theory development and guide future studies addressing outcome of pain rehabilitation.
Design
Most studies of torture survivors are set in specialised non‐governmental treatment centres in high‐income countries, or in less well‐resourced countries, and academic expertise may be lacking when it is needed to design worthwhile studies. Despite the difficulties of recruitment from what is often an unstable population (in terms of civil status, income, and accommodation), studies must be adequately powered. Ideally, treatment methods are drawn from those showing best outcomes in the general chronic pain population, and delivered by therapists qualified in those methods. The studies included in this review appeared weak in their understanding of pain and of its effective treatment, so interventions fell short of what could be provided and tested.
In the short‐term, careful observational studies of torture survivors in treatment for pain would help to formulate research hypotheses and questions to be addressed by controlled studies.
Measurement
Outcomes in the studies in this review were very narrow and did not consider harm, a significant risk in this population, particularly in participants with moderate to severe post‐traumatic stress symptoms. However, conceptualising psychological distress, whether at baseline or after treatment, only in terms of PTSD diagnosis or caseness is inadequate for the range and extent of psychological problems in this population (Patel 2014; Quiroga 2005). Similarly, many torture survivors' lives are very constrained by lack of resources (money, language, social networks, and others) that both disability and quality of life scales may be difficult to answer in terms only of pain, and care should be taken to select those (perhaps from international bodies such as the WHO) with most appropriate content.
Interview assessment is inevitably unstandardised, and conducting it via an interpreter adds further unreliability. While questionnaires can be translated and checked by back‐translation, this falls short of adequate development of a questionnaire incorporating cultural as well as linguistic equivalence: these methods are well described in Sousa 2011.
Given the impossibility of blinding participants or therapists to most psychologically based treatments, collecting ratings from participants of their expectation of benefit from their assigned treatment (or comparison condition) before it starts, and satisfaction when it ends, is a helpful substitute, particularly when the treatments may be drawn from psychological models and methods that are culturally unfamiliar to participants.
Best practice
The right to rehabilitation after torture is enshrined in international law, as is the right to asylum, but is not yet realised in any country. Apart from the human rights grounds, there are obvious humanitarian grounds for trying to provide best health care to torture survivors with the aim of restoring as far as possible their capacity to participate in their host country and chosen communities. There is no substitute for good quality treatment studies, using best clinical and scientific practice.
What's new
| Date | Event | Description |
|---|---|---|
| 13 February 2019 | Review declared as stable | See Published notes. |
Notes
A restricted search in February 2019 did not identify any potentially relevant studies likely to change the conclusions. Therefore, this review has now been stabilised following discussion with the authors and editors. The review will be re‐assessed for updating in five years. If appropriate, we will update the review before this date if new evidence likely to change the conclusions is published, or if standards change substantially which necessitates major revisions.
Acknowledgements
Cochrane Review Group funding acknowledgement: this project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Cochrane Pain, Palliative and Supportive Care Review Group (PaPaS). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service, or the Department of Health.
Appendices
Appendix 1. GRADE assessment
The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of the body of evidence for each outcome. The GRADE system uses the following criteria for assigning grade of evidence:
high: we are very confident that the true effect lies close to that of the estimate of the effect;
moderate: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different;
low: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect;
very low: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.
We decreased grade if we identified:
serious (‐1) or very serious (‐2) limitation to study quality;
important inconsistency (‐1);
some (‐1) or major (‐2) uncertainty about directness;
imprecise or sparse data (‐ 1);
high probability of reporting bias (‐1).
Appendix 2. Search strategies
CENTRAL (CRSO)
#1 MESH DESCRIPTOR Torture
#2 torture*:TI,AB,KY
#3 #1 OR #2
#4 victim*:TI,AB,KY
#5 MESH DESCRIPTOR Survivors
#6 survivor*:TI,AB,KY
#7 survive*:TI,AB,KY
#8 #4 OR #5 OR #6 OR #7
#9 MESH DESCRIPTOR pain EXPLODE ALL TREES
#10 MESH DESCRIPTOR Stress Disorders, Post‐Traumatic EXPLODE ALL TREES
#11 pain*:TI,AB,KY
#12 MESH DESCRIPTOR chronic pain EXPLODE ALL TREES
#13 MESH DESCRIPTOR Pain, Intractable EXPLODE ALL TREES
#14 (((chronic or persist*) adj2 pain)):TI,AB,KY
#15 #9 OR #10 OR #11 OR #12 OR #13 OR #14
#16 #3 OR #8
#17 #15 AND #16
MEDLINE and MEDLINE in Process (Ovid)
1 Torture/
2 torture*.tw.
3 1 or 2
4 victim*.tw.
5 Survivors/
6 survivor*.tw.
7 survive*.tw.
8 or/4‐7
9 exp Pain/ or Stress Disorders, Post‐Traumatic/
10 pain*.tw.
11 exp chronic pain/ or exp intractable pain/
12 ((chronic or persist*) adj2 pain).tw.
13 or/9‐12
14 3 and (8 or 13)
Embase (Ovid)
1 Torture/
2 torture*.tw.
3 1 or 2
4 victim*.tw.
5 Survivors/
6 survivor*.tw.
7 survive*.tw.
8 or/4‐7
9 exp Pain/ or Stress Disorders, Post‐Traumatic/
10 pain*.tw.
11 exp chronic pain/ or exp intractable pain/
12 ((chronic or persist*) adj2 pain).tw.
13 or/9‐12
14 3 and (8 or 13)
15 limit 14 to embase
PsycINFO (Ovid)
1 Torture/
2 torture*.tw.
3 1 or 2
4 victim*.tw.
5 Survivors/
6 survivor*.tw.
7 survive*.tw.
8 or/4‐7
9 exp Pain/ or Stress Disorders, Post‐Traumatic/
10 pain*.tw.
11 exp chronic pain/ or exp intractable pain/
12 ((chronic or persist*) adj2 pain).tw.
13 or/9‐12
14 3 and (8 or 13)
CINAHL (EBSCO)
S15 S3 AND S14
S14 S7 OR S13
S13 S8 OR S9 OR S10 OR S11 OR S12
S12 ((chronic or persist*) N2 pain)
S11 (MH "Chronic Pain")
S10 pain*
S9 (MH "Stress Disorders, Post‐Traumatic+")
S8 (MH "Pain+")
S7 S4 OR S5 OR S6
S6 survivor* or survive*
S5 (MH "Torture Survivors")
S4 victim*
S3 S1 OR S2
S2 torture*
S1 (MH "Torture")
ISI Web of Science
# 7 #6 AND #1
Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, CCR‐EXPANDED, IC Timespan=All years
# 6 #5 OR #4
Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, CCR‐EXPANDED, IC Timespan=All years
# 5 TOPIC: (pain*)
Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, CCR‐EXPANDED, IC Timespan=All years
# 4 #3 OR #2
Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, CCR‐EXPANDED, IC Timespan=All years
# 3 TOPIC: (victim*)
Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, CCR‐EXPANDED, IC Timespan=All years
# 2 TOPIC: (survivor* or survive*)
Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, CCR‐EXPANDED, IC Timespan=All years
# 1 TOPIC: (torture*)
Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, CCR‐EXPANDED, IC Timespan=All years
LILACS (Birme)
torture$ [Words] and (victim$ or survivor$ or survive$) or (pain$) [Words]
Data and analyses
Comparison 1. Cognitive behavioural therapy (CBT) versus waiting list control at end of treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain relief | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐1.23, 1.12] |
| 2 Reduction in disability | 2 | 57 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.17, 0.39] |
| 3 Reduction in distress | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.46, 0.60] |
1.1. Analysis.
Comparison 1 Cognitive behavioural therapy (CBT) versus waiting list control at end of treatment, Outcome 1 Pain relief.
1.2. Analysis.
Comparison 1 Cognitive behavioural therapy (CBT) versus waiting list control at end of treatment, Outcome 2 Reduction in disability.
1.3. Analysis.
Comparison 1 Cognitive behavioural therapy (CBT) versus waiting list control at end of treatment, Outcome 3 Reduction in distress.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Kim 2015.
| Methods | RCT: 2 arms: treatment, active control; single centre. | |
| Participants |
Inclusion criteria: male torture survivors with low back pain attending treatment centre. Exclusion criteria: referred to but not specified. Pain condition: chronic low back pain. Number of participants: 30 at start of treatment, 15 per arm (no dropouts reported). Mean (SD) age in years: intervention: 59.2 (6.6); control: 62.6 (6.6). Sex: 30 men. |
|
| Interventions |
Experimental group: complex manual therapy 24 × 90‐minute (possibly 2 hour) sessions over 8 weeks. Requests for clarification were unanswered. Control group: self‐exercise for the back, using manual therapy (after education), 90‐minute sessions, 3 × weekly for 8 weeks (36 hours). Therapists: not stated, but presumably physical therapists. |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Time points for assessment: baseline, end of treatment. Language of assessment: Korean. |
|
| Notes | Means and SDs available for all outcomes, pre‐ and post‐treatment. We approached study authors twice via published email address and twice by post to published addresses to clarify discrepancies in intervention descriptions but had no response. Study period: unknown. Country: Republic of Korea. Language of assessment: Korean (language of participants and therapists). Funding source: not stated. Declarations of interest among the primary researchers: not stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Coin toss method used. This was unlikely to result in a 15:15 split. Achievement of parity not explained. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described but difficult to achieve in circumstances. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals reported. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Size | High risk | < 50 participants per treatment arm. |
| Other bias | Low risk | No information on therapist qualifications. No information on therapist allegiance. Language of assessment Korean (language of participants and therapists). |
Liedl 2011.
| Methods | RCT: 3 arms: enhanced treatment, treatment, waiting list; recruited from 2 centres or referred by workers in the field. | |
| Participants |
Inclusion criteria: chronic (excluding neuropathic) pain; refugee status; trauma in home country (70% torture). Exclusion criteria: psychotic symptoms; substance‐related symptoms; suicidal ideation; severe dissociative symptoms. Pain condition: chronic (excluding neuropathic) pain. Number of participants: 36 at start of treatment (12 per arm); 30 at end of treatment (10 per arm). Mean (SD) age in years: 41.7 (10.0). Sex: 17 men; 13 women (completers). |
|
| Interventions |
Experimental groups: CBT‐BF‐PE and CBT‐BF. CBT‐BF: manual‐based; 10 × 90‐minute sessions over 3 months. CBT‐BF‐PE: as above plus PE: physiotherapist‐instructed, handbook‐illustrated, 20 minutes daily, at home. Control group: waiting list (treatment received after 4 months). Therapists: 4 graduate clinical psychology students specially trained in CBT‐BF for such a client group and who had observed a professional CBT‐BF therapist. |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
Time points for assessment: baseline, end of treatment, 3‐month follow‐up. Languages of assessment: questionnaires translated into multiple languages of participants and completed with computer or spoken. |
|
| Notes | Data available for all outcomes, pre‐ and post‐treatment and follow‐up. Study period: recruitment 2007‐2009. Country: Germany and Switzerland. Language of assessment: participants provided with interpreters for interview; questionnaires translated. Funding source: not stated. Declarations of interest among the primary researchers: no conflicts of interest. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given of process. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described but difficult to achieve in the circumstances. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completers only analysed (30/36 participants). |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Size | High risk | < 50 participants per treatment arm. |
| Other bias | Unclear risk | Therapists were graduate students, not authors of study. Therapist allegiance not stated. Language of assessment: interpreted or translated so unstandardised. |
Wang 2017.
| Methods | RCT: 2 arms: treatment, waiting list. | |
| Participants |
Inclusion criteria: adults aged 18‐65 years; experience of ≥ 1 of torture (80%), sexual violence, extralegal detention, witnessing killings of relatives. Exclusion criteria: conditions impeding assessment; schizophrenia; substance abuse; cancer treatment; previous CBT. Pain condition: any (multiple sites) (all randomised had pain). Number of participants: 34 at start of treatment (17 per arm); 28 at end of treatment (treatment: 13 analysed (12 only for disability assessed by WHO Disability Assessment Schedule‐II; waiting list: 15 analysed). Mean (SD) age in years: 47.7 (SD not reported). Sex: 55% men; 45% women (not clear at which stage calculation made). |
|
| Interventions |
Experimental group: CBT‐BF‐PE plus daily dose of multivitamins. 10 × 90‐minute sessions of individual therapy (total 15 hours); 10 weekly 90‐minute sessions of group PEs and transcutaneous electrical nerve stimulation (total 15 hours). Control group: waiting list (treatment received after 3 months) plus daily dose of multivitamins. Therapists: doctor, physiotherapists, psychologists. |
|
| Outcomes |
Primary outcomes
Secondary outcomes
Other outcomes
Time points for assessment: baseline; 3 months (end of treatment); 6 months (follow‐up). Language of assessment: Albanian; questionnaires part‐translated into Albanian (and Serbian). |
|
| Notes | Data on means and SDs were supplied after email approach to main author. Data not available for all outcomes pre‐ and post‐treatment, and follow‐up, but outcomes of interest were supplied by study authors on request. Study period: recruitment 2012. Country: Kosovo. Language of assessment: participants interviewed in their own language by experienced interviewers and senior clinical psychologist, all Kosovors. Funding source: Novo Nordisk Research Foundation. Declarations of interest among the primary researchers: no conflicts of interest. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Block randomisation procedure using a computerised random number generator by two blocks of size 17 created by a DIGNITY staff not involved in the trial." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described but difficult to achieve in the circumstances. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessment by Kosovo psychiatrist blind to allocation of interviewees. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Completers only analysed (28/34) although described as intention to treat. |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported. |
| Size | High risk | < 50 participants per treatment arm. |
| Other bias | Low risk | Data and clarification of published data supplied on request by first author. Therapist qualifications: qualified healthcare professionals. Therapist allegiance: not stated. Language of assessment: participants interviewed in their own language by experienced interviewers and senior clinical psychologist, all Kosovors. |
BF: biofeedback; CBT: cognitive behavioural therapy; FESV: Fragebogen zur Erfassung der Schmerzverarbeitung (German Pain Coping Questionnaire); HSCL‐25: Hopkins Symptoms Checklist‐25 items; KODI: Korean Oswestry Disability Index; PDS: Post‐traumatic Diagnostic Scale; PE: physical exercise; PTSD: post‐traumatic stress disorder; RCT: randomised controlled trial; SD: standard deviation; WHO: World Health Organization.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adenauer 2011 | No pain outcome. |
| Blyhammar 2009 | Not RCT. |
| Bolton 2014a | No pain outcome. |
| Bolton 2014b | No pain outcome. |
| Callaghan 1993 | Not RCT. |
| Defrin 2017 | Not RCT. |
| Esala 2017 | Not pain. |
| Farrag 2005 | Not RCT. |
| Highfield 2012 | Not RCT. |
| Hinton 2006 | Not RCT. |
| Jansen 2011 | Not RCT. |
| Johnson 2001 | No pain outcome. |
| Jorgensen 2015 | Not RCT. |
| Kaysen 2013 | Not RCT; no pain outcome. |
| Morville 2015 | Not RCT. |
| Müller 2009 RETRACTED | Not RCT. |
| Phaneth 2014 | Not RCT. |
| Puvimanasinghe 2016 | Not RCT. |
| Schwarz‐Langer 2006 | Not RCT. |
| Taing 2011 | No pain outcome. |
| Weiss 2015 | No pain outcome. |
RCT: randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
Phaneth 2016.
| Trial name or title | Randomized Controlled Trial on the Effect of DIGNITY Pain School Initiative. |
| Methods | RCT: 2 arms: treatment, waiting list; single centre; pre‐, post‐treatment, 6 months' follow‐up. |
| Participants | 120 Cambodian torture survivors (Khmer Rouge regimen) with chronic pain. |
| Interventions | 1 week group‐based "pain school:" education programme: 10 sessions × 2 hours. |
| Outcomes | Reduction in chronic pain (Brief Pain Index); improvement in pain‐associated functioning (Disability Rating Index). |
| Starting date | Not stated. |
| Contact information | DIGNITY Danish Institute Against Torture, Bryggervangen 55, DK ‐ 2100 Copenhagen, Denmark. |
| Notes | Not published: information from Polatin. Pain school devised by DIGNITY. Pilot study Phaneth 2014. |
Differences between protocol and review
We added several additional risk of bias items, collectively referred to as 'Other': therapist qualification, therapist allegiance, and language of assessment. We also added assessment of risk of bias from methods of blinding of participants and personnel, and selective outcome reporting.
We did not attempt transformations of skewed data as planned.
Contributions of authors
EB co‐ordinated writing the protocol.
AW and EB screened titles and abstracts.
EB and LH read full papers and extracted data.
AW, KA, and LH contributed to writing the review.
Declarations of interest
EB: none known; EB is a specialist physician who has in the past provided medical treatment to survivors of torture.
AW: none known; AW is a clinical psychologist specialised in pain who has treated survivors of torture with chronic pain, and conducted research on pain from torture.
LH: none known.
KA: none known; KA is a certified specialist in rheumatology who has treated survivors of torture with chronic pain, and conducted research on pain from torture.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Kim 2015 {published data only}
- Kim HJ, Yu SH. Effects of complex manual therapy on PTSD, pain, function, and balance of male torture survivors with chronic low back pain. Journal of Physical Therapy Science 2015;27(9):2763‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liedl 2011 {published data only}
- Editor, Pain Medicine. Retraction. Pain Medicine 2013;14:1616. [PubMed] [Google Scholar]
- Liedl A, Müller J, Morina N, Karl A, Denke C, Knaevelsrud C. Physical activity within a CBT intervention improves coping with pain in traumatized refugees: results of a randomized controlled design. Pain Medicine 2011;12:234‐45. [DOI] [PubMed] [Google Scholar]
Wang 2017 {published data only}
- Wang S‐J. Effectiveness of combined intervention approaches in the treatment of affective disorders and chronic pain in war victims. clinicaltrials.gov/ct2/show/NCT01696578 Date first received: 25 September 2012.
- Wang S‐J, Bytyçi A, Izeti S, Kallaba M, Rushiti F, Montgomery E, et al. A novel bio‐psycho‐social approach for rehabilitation of traumatized victims of torture and war in the post‐conflict context: a pilot randomized controlled trial in Kosovo. BMC Conflict and Health 2017;10:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S‐J, Pacolli S, Rushiti F, Rexhaj B, Modvig J. Survivors of the war in the northern Kosovo (II): baseline clinical and functional assessment and lasting effects on the health of a vulnerable population. BMC Conflict and Health 2010;4:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S‐J, Rushiti F, Sajdiu X, Pacolli S, Gashi B, Salihu F, et al. Survivors of the war in northern Kosovo (III): the role of anger and hatred in pain and PTSD and their interactive effects on career outcome, quality of sleep, and suicide ideation. BMC Conflict and Health 2012;6:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S‐J, Salihu M, Rushiti F, Bala L, Modvig J. Survivors of the war in the northern Kosovo: violence exposure, risk factors and public health effects of an ethnic conflict. BMC Conflict and Health 2010;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S‐JS. A pilot randomized controlled trial of a novel bio‐psycho‐social approach of rehabilitation for victims of torture and war with affective disorders and chronic pain in Kosovo. 143rd APHA Annual Meeting and Expo; 2015 Oct 29‐Nov 4; Chicago (IL). Chicago (IL): DIGNITY, 2015.
References to studies excluded from this review
Adenauer 2011 {published data only}
- Adenauer H, Catani C, Gola H, Keil J, Ruf M, Schauer M, et al. Narrative exposure therapy for PTSD increases top‐down processing of aversive stimuli ‐ evidence from a randomized controlled treatment trial. BMC Neuroscience 2011;12:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blyhammar 2009 {published data only}
- Blyhammar C, Larsson L. Experience from group program for torture survivors. European Journal of Pain 2009;13:S277. [Google Scholar]
Bolton 2014a {published data only}
- Bolton P, Bass JK, Zangana GAS, Kamal T, Murray SM, Kaysen D, et al. A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan, northern Iraq. BMC Psychiatry 2014;14:360. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bolton 2014b {published data only}
- Bolton P, Lee C, Haroz EE, Murray L, Dorsey S, Robinson C, et al. A transdiagnostic community‐based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLoS Medicine 2014;11(11):e1001757. [DOI] [PMC free article] [PubMed] [Google Scholar]
Callaghan 1993 {published data only}
- Callaghan K. Movement psychotherapy with adult survivors of political torture and organized violence. The Arts in Psychotherapy 1993;20:411‐21. [Google Scholar]
Defrin 2017 {published data only}
- Defrin R, Lahav Y, Solomon Z. Dysfunctional pain modulation in torture survivors: the mediating effect of PTSD. Journal of Pain 2017;18(1):1‐10. [DOI] [PubMed] [Google Scholar]
Esala 2017 {published data only}
- Esala JJ, Taing S. Testimony therapy with ritual: a pilot randomized controlled trial. Journal of Traumatic Stress 2017;30:1‐5. [DOI] [PubMed] [Google Scholar]
Farrag 2005 {published data only}
- Farrag M, Abdel‐khaleq H, Kazak A. The psychosocial rehabilitation approach in treating torture survivors. Ethnicity and Disease 2005;15 S1:97‐8. [PubMed] [Google Scholar]
Highfield 2012 {published data only}
- Highfield ES, Lama P, Grodin MA, Kaptchuk TJ, Crosby SS. Acupuncture and traditional Chinese medicine for survivors of torture and refugee trauma: a descriptive report. Journal of Immigrant Minority Health 2012;14:433‐40. [DOI] [PubMed] [Google Scholar]
Hinton 2006 {published data only}
- Hinton DE, Safren SA, Pollack MH, Tran M. Cognitive‐behavior therapy for Vietnamese refugees with PTSD and comorbid panic attacks. Cognitive and Behavioral Practice 2006;13:271‐81. [Google Scholar]
Jansen 2011 {published data only}
- Jansen GB, Nordemar R, Larsson L, Blyhammar C. Pain rehabilitation for torture survivors. European Journal of Pain Supplements 2011;5:284. [Google Scholar]
Johnson 2001 {published data only}
- Johnson C, Shala M, Sejdijaj X, Odell R, Dabishevci K. Thought field therapy ‐ soothing the bad moments of Kosovo. Journal of Clinical Psychology 2001;57(10):1237‐40. [DOI] [PubMed] [Google Scholar]
Jorgensen 2015 {published data only}
- Jorgensen MM, Modvig J, Agger I, Raghuvansh L, Shabana Khan S, Polatin P. Testimonial therapy: impact on social participation and emotional wellbeing among Indian survivors of torture and organized violence. Torture 2015;25(2):22‐33. [PubMed] [Google Scholar]
Kaysen 2013 {published data only}
- Kaysen D, Lindgren K, Zangana GAS, Murray L, Bass J, Bolton P. Adaptation of cognitive processing therapy for treatment of torture victims: experience in Kurdistan, Iraq. Psychological Trauma, Theory, Research, Practice, and Policy 2013;5(2):184‐92. [Google Scholar]
Morville 2015 {published data only}
- Morville A‐L, Amris K, Eklund M, Danneskiold‐Samsoe B, Erlandsson L‐K. A longitudinal study of changes in asylum seekers ability regarding activities of daily living during their stay in the asylum center. Journal of Immigrant & Minority Health 2015;17(3):852‐9. [DOI] [PubMed] [Google Scholar]
Müller 2009 RETRACTED {published data only}
- Müller J, Karl A, Denke C, Mathier F, Dittmann J, Rohleder N, et al. RETRACTED ARTICLE: biofeedback for pain management in traumatised refugees. Cognitive Behaviour Therapy 2009;38(3):184‐90. [DOI] [PubMed] [Google Scholar]
Phaneth 2014 {published data only}
- Phaneth S, Panha P, Sopheap T, Harlacher U, Polatin P. Education as treatment for chronic pain in survivors of torture and other violent events in Cambodia: experiences with implementation of a group‐based "pain school" and evaluation of its effect in a pilot study. Journal of Applied Biobehavioral Research 2014;19(1):53‐69. [Google Scholar]
Puvimanasinghe 2016 {published data only}
- Puvimanasinghe TS, Price IR. Healing through giving testimony: an empirical study with Sri Lankan torture survivors. Transcultural Psychiatry 2016;53(5):531‐50. [DOI] [PubMed] [Google Scholar]
Schwarz‐Langer 2006 {published data only}
- Schwarz‐Langer G, Deighton RR, Jerg‐Bretzka L, Weisker I, Traue HC. Psychiatric treatment for extremely traumatized civil war refugees from former Yugoslavia. Torture 2006;16(2):69‐80. [PubMed] [Google Scholar]
Taing 2011 {published data only}
- Taing S, Strasser J, Chhim S. Culturally sensitive trauma treatment for Khmer Rouge survivors. Asian Journal of Psychiatry 2011;4S1:S35. [Google Scholar]
Weiss 2015 {published data only}
- Weiss WM, Murray LK, Zangana GAS, Mahmooth Z, Kaysen D, Dorsey S, et al. Community‐based mental health treatments for survivors of torture and militant attacks in southern Iraq: a randomized control trial. BMC Psychiatry 2015;15:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Phaneth 2016 {published data only}
- Phaneth S, Polatin P. Randomized controlled trial on the effect of DIGNITY pain school initiative. dignityinstitute.org/what‐we‐do/rehabilitation/projects/randomized‐controlled‐trial‐on‐the‐effect‐of‐dignity‐pain‐school‐initiative/ (accessed 7 January 2017).
Additional references
AI 2010
- Amnesty International. Reports statement and issues briefs. About torture. www.amnestyusa.org/counter‐terrorwith‐justice/reports‐statements‐and‐issue‐briefs/abouttorture/page.do?id=1031032 (accessed 25 February 2010).
Amris 2000a
- Amris K. Physiotherapy for torture victims (I). Chronic pain in torture victims: possible mechanisms of pain. Torture 2000;10:73‐6. [Google Scholar]
Amris 2000b
- Amris K. Physiotherapy for torture victims (II). Treatment of chronic pain. Torture 2000;10:112‐6. [Google Scholar]
Amris 2007
- Amris K, Williams A. Chronic pain in survivors of torture. Pain: Clinical Updates 2007;XV:1‐4. [Google Scholar]
Amris 2015
- Amris K, Williams AC de C. Managing chronic pain in survivors of torture. Pain Management 2015;5(1):5‐12. [DOI] [PubMed] [Google Scholar]
Basoglu 2006
- Basoglu M. Rehabilitation of traumatised refugees and survivors of torture. BMJ 2006;333:1230‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berliner 2004
- Berliner P, Nikkelsen EM, Bovbjerg A, Wiking M. Psychotherapy treatment of torture survivors. International Journal of Psychosocial Rehabilitation 2004;8:85‐96. [Google Scholar]
Burnett 2001
- Burnett A, Peel M. The health of survivors of torture and organised violence. BMJ 2001;322:606‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crosby 2006
- Crosby SS, Norredam M, Paasche‐Orlow MK, Piwowarczyk L, Heeren T, Grodin MA. Prevalence of torture survivors among foreign‐born patients presenting to an urban ambulatory care practice. Journal of General Internal Medicine 2006;21(7):764‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edston 2005
- Edston E. Torture. Torture 2005;15:16‐24. [Google Scholar]
Eisenman 2003
- Eisenman DP, Gelberg L, Liu H, Shapiro MF. Mental health and health‐related quality of life among adult Latino primary care patients living in the United States with previous exposure to political violence. JAMA 2003;290(5):627‐34. [DOI] [PubMed] [Google Scholar]
el Serraj 1996
- Serraj E. Experiences of torture and ill‐treatment and posttraumatic stress disorder symptoms among Palestinian political prisoners. Journal of Trauma and Stress 1996;9:591‐8. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- Brozeck J, Oxman A, Schunemann H. GRADEpro Guideline Development Tool. Hamilton (ON): GRADE Working Group, McMaster University, 2015.
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
IASP 1994
- IASP Taxonomy Working Group. Part three: pain terms a current list with definitions and notes on usage. In: Merskey H, Bogduk N editor(s). Classification of Chronic Pain. 2nd Edition. Seattle (WA): IASP Press, 1994:209‐14. [Google Scholar]
IRCT 2010
- Said M, Sydhoff B, editors. International Rehabilitation Council for Torture Victims. The fight against torture: a key priority for the EU. europa.eu/rapid/pressReleasesAction.do?reference=MEMO/07/254 (accessed 25 February 2010).
Jacobs 2001
- Jacobs U, Iacopino V. Torture and its consequences: a challenge to clinical neuropsychology. Professional Psychology, Research and Practice 2001;32(5):458‐64. [Google Scholar]
Jaranson 1995
- Jaranson JM. Government‐sanctioned torture: status of the rehabilitation movement. Transcultural Psychiatric Research Review 1995;32:253‐86. [Google Scholar]
Jaranson 2011
- Jaranson JM, Quiroga J. Evaluating the series of torture rehabilitation programmes: history and recommendations. Torture 2011;21:98‐140. [PubMed] [Google Scholar]
Jensen 2014
- Jensen MP, Turk DC. Contributions of psychology to the understanding and treatment of people with chronic pain: why it matters to ALL psychologists. American Psychologist 2014;69(2):105‐18. [DOI] [PubMed] [Google Scholar]
Johnson 2008
- Johnson H, Thompson A. The development and maintenance of post‐traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: a review. Clinical Psychology Review 2008;28(1):36‐47. [DOI] [PubMed] [Google Scholar]
Lund 2008
- Lund M, Sorensen JH, Christensen JB, Olholm A. MTV om Behandling og Rehabilitering af PTSD ‐ Herunder Traumatiserede Flygtninge. Udgivet af Region Syddanmark: Centre for Quality, South Denmark, 2008. [Google Scholar]
Mckenna 2012
- Mckenna Longacre MM, Silver‐Highfield E, Lama P, Grodin MA. Complementary and alternative medicine in the treatment of refugees and survivors of torture: a review and proposal for action. Torture 2012;22(1):38‐57. [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, the PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mollica 2011
- Mollica RF. Medical best practices for the treatment of torture survivors. Torture 2011;21(1):8‐17. [PubMed] [Google Scholar]
Montgomery 2011
- Montgomery E, Patel N. Torture rehabilitation: reflections on treatment outcome studies. Torture 2011;21:141‐5. [PubMed] [Google Scholar]
Moreno 2002
- Moreno A, Grodin MA. Torture and its neurological sequelae. Spinal Cord 2002;40(5):213‐23. [DOI] [PubMed] [Google Scholar]
Newton‐John 1995
- Newton‐John TRO, Spence SH, Schotte D. Cognitive behavioral therapy versus EMG biofeedback in the treatment of chronic low back pain. Behaviour Research and Therapy 1995;33(6):691‐7. [DOI] [PubMed] [Google Scholar]
Norredam 2005
- Norredam M, Crosby S, Munarriz R, Piwowarczyk L. Urological complications of sexual trauma among male survivors of torture. Urology 2005;65(1):28‐32. [DOI] [PubMed] [Google Scholar]
Nuesch 2009
- Nuesch E, Trelle S, Reichenbach S, Rutjes AW, Burgi E, Scherer M, et al. The effects of excluding patients from the analysis in randomised controlled trials: meta‐epidemiological study. BMJ 2009;339:b3244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Olsen 2006
- Olsen DR, Montgomery E, Bojholm S, Foldspang A. Prevalent musculoskeletal pain as a correlate of previous exposed to torture. Scandinavian Journal of Public Health 2006;34:496‐503. [DOI] [PubMed] [Google Scholar]
Olsen 2007
- Olsen DR, Montgomery E, Bojholm O, Foldspang A. Prevelance of pain in the head, back and feet in refugees previously exposed to torture: a ten year follow up study. Disability and Rehabilitation 2007;29(2):163‐71. [DOI] [PubMed] [Google Scholar]
Patel 2007
- Patel N. Torture, psychology and the 'War on terror': a human rights framework. In: Roberts R editor(s). Just War: Psychological Terrorism. Ross on Wire (UK): PCCS Books, 2007. [Google Scholar]
Patel 2014
- Patel N, Kellezi B, Williams AC de C. Psychological, social and welfare interventions for psychological health and well‐being of torture survivors. Cochrane Database of Systematic Reviews 2014, Issue 11. [DOI: 10.1002/14651858.CD009317.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Quiroga 2005
- Quiroga J, Jaranson JM. Politically motivated torture and its survivors: a desk study review of the literature. Torture: Journal on Rehabilitation of Torture Victims and Prevention of Torture 2005;15(2‐3):1‐111. [Google Scholar]
Rasmussen 1990
- Rasmussen OV. Medical aspects of torture. Danish Medical Bulletin 1990;37:1‐88. [PubMed] [Google Scholar]
Rasmussen 2006
- Rasmussen OV, Amris S, Blaaow M, Danielson L. Medical physical examination in connection with torture: section two. Torture 2006;16:48‐55. [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Sjölund 2009
- Sjölund BH, Kastrup M, Montgomery E, Persson AL. Rehabilitating torture survivors. Journal of Rehabilitation Medicine 2009;41:689‐96. [DOI] [PubMed] [Google Scholar]
Sousa 2011
- Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross‐cultural health care research: a clear and user‐friendly guideline. Journal of Evaluation in Clinical Practice 2011;17:268‐74. [DOI] [PubMed] [Google Scholar]
Taylor 2013
- Taylor B, Carswell K, Williams AC de C. The interaction of persistent pain and post‐traumatic re‐experiencing: a qualitative study in torture survivors. Journal of Pain and Symptom Management 2013;46(4):546‐55. [DOI] [PubMed] [Google Scholar]
UN 1984
- UN General Assembly. Convention against torture and other cruel, inhuman or degrading treatments or punishments. Treaty Series (available at www2.ohchr.org/english/law/pdfl/cat.pdf). Geneva (Switzerland): United Nations, 10 December 1984; Vol. 1465.
Williams 2010
- Williams AC de C, Peña CR, Rice ASC. Persistent pain in survivors of torture: a cohort study. Journal of Pain and Symptom Management 2010;40:715‐22. [DOI] [PubMed] [Google Scholar]
Williams 2012
- Williams AC de C, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD007407.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
WMA 2006
- World Medical Association. WMA Declaration of Tokyo ‐ guidelines for physicians concerning torture and other cruel, inhuman or degrading treatment or punishment in relation to detention and imprisonment, 2006. www.wma.net/en/30publications/10policies/c18/ (accessed 24 August 2015).


