Abstract
Background:
The blue laser imaging is a kind of new endoscopic system, sending 2 different wavelengths of laser.
Result:
It can observed that the gastrointestinal mucosa shallow capillaries and mucosal surface microstructure are shown in bright and high resolution images, thus being helpful to the diagnosis of early digestive tract cancer. It has unique advantages compared with the existing technique. This article reviewed the application of blue laser imaging in diagnosis of early gastrointestinal carcinoma.
Keywords: blue laser imaging, early carcinoma of gastrointestinal tract, colorectal lesion, diagnosis, surface microstructure
The digestology has already entered the era of endoscopy, and the early detection, early diagnosis, and early treatment of digestive tract tumors have been the development trend of digestive endoscopy at home and abroad. The premise of the effective endoscopic treatment can improve the screening rate and the correct diagnosis rate of early cancer and can increase the emphasis of the global digestive endoscopy doctors on the accurate diagnosis. OLYMPUS took the lead in developing narrow-band imaging (NBI), which uses optical filter to filter out the red broadband spectrum sent by the endoscopic xenon light, while preserving the blue and green narrow-band spectrum to diagnose the digestive tract mucosal and submucosal lesions, so as to improve the accuracy of endoscopic diagnosis. But due to the limitations of working principle, NBI, with the broadband spectrum filled out, cannot be used for distant functional observation so as to achieve the goal of cancer screening, due to the nonideal brightness. Blue laser imaging (BLI) system was firstly put into use in Japan in 2011. Fuji film officially launched out LASEREO—the blue laser endoscopic system in 2012. In addition to the white light observation mode, the blue laser endoscopy system has also increased 3 narrow-band laser observation modes: BLI, BLI-bright, and linked color imaging modes.
LASEREO endoscopic system adopts laser instead of the halogen or high intensity discharge (HID) lamp, with 2 different wavelengths of laser to form white light images and narrow-band light images. Due to the laser light sources, the images are brighter, clearer, and more hierarchical, and combined with the unique image processing technology, endoscopy could explore as deeper as the capillaries and microstructure of the mucosal surface, which improves the distinguishment of pathological changes in early digestive tract tumor, and provides more possibility for accurate diagnosis and treatment of gastrointestinal cancer. Its application in the diagnosis of the gastrointestinal tract disease has still been preliminarily studied. A comprehensive review was carried out on the application of BLI in diagnosis of early gstrointestinal carcinoma.
Characteristics of Blue Laser Imaging
Characteristic of Light Source and BLI Imaging Principle
The blue laser endoscopy system adopts 2 different wavelengths of lasers: white light laser (wavelength of 450 nm) and BLI laser (wavelength of 410 nm). The white light laser, by the fluorescent body, sends white light with broad spectrum and high brightness which is suitable for the routine inspections, and the images are natural, bright, and clear; while BLI laser, with shorter wavelength and narrow spectrum, presents a narrow-band light images, which can highlight the capillaries and microstructure of the mucosal surface, so as to observe the pathological changes in microscopic structure and is helpful to diagnose the gastrointestinal tract cancer.1–3
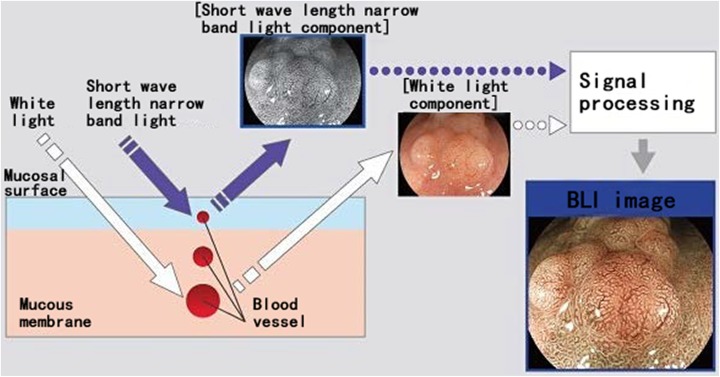
Blue laser imaging is a kind of endoscopic imaging to observe and diagnose the surface and deep vessels, based on the absorption and reflection of mucous membrane to light, the absorption properties of hemoglobin to the laser light with a wavelength of 410 nm optical and the reflection characteristics of mucosal membrane to light. Short wavelength is easy to be absorbed by hemoglobin in the blood, and blood vessel is dark in color after absorption, which is contrasted with surrounding tissues; thus, the vascular morphology is prominent. Due to the rich glandular structure on the surface of digestive tract mucosa, and rich capillaries around the gland, short wave length can lead to a strong contrast of capillaries and glands (Figure 1).
Figure 1.
The blue laser imaging (BLI) imaging principle.
Observation Mode
By adjusting the luminescence intensity of BLI laser and white light laser, 2 observation modes can be achieved, namely BLI and BLI-bright. The BLI mode: BLI with 410 nm wavelength slightly increases the white light, which very clearly and effectively emphasizes the morphology of small vessels and mucosal surface, and even deeper blood vessels. The BLI mode mainly amplifies and closely observes the lesions, with a certain degree of brightness, so as to improve the diagnosis rate. It is easier to distinguish the nature of the lesions and is also useful for boundary identification, which can accurately diagnose the diseases according to the classification standards of early cancer of different parts such as esophagus, stomach, and intestine.
The BLI-bright mode: BLI-bright also adopts 410 nm wavelength, but compared with BLI mode, it has fewer narrow band light component while more white light component, so it is brighter. The BLI-bright is suitable for medium-long short that has lower brightness and is not prone to show good contrast; it can also effectively emphasize the vascular and mucosal surface morphology of medium-long short when the condition of the observation site is poor. The biggest advantage of BLI, which has a narrow-wave observation function, is used for the detection and identification of early tumor, and compared with the traditional image-enhanced endoscopy, BLI can provide clearer and more administrative images, which are more conducive to the inspection of early digestive tract cancer.
Comparison of BLI and Other Endoscopic Technology
The characteristics of BLI have been compared with the common endoscopic technique in observing the early digestive tract cancer in recent years. With the progress of the endoscopic technique, various techniques emerge on the basis of the white light endoscopy, including pigment endoscopy, electronic staining endoscopy, endoscopic ultrasound, confocal laser endomicroscopy, autofluorescence endoscopy, Raman spectroscopy, and son on, which greatly improve the detection rate of early upper gastrointestinal tract cancer.
Narrow-band imaging technology uses narrow-band filter to remove red light while preserving green and blue light. The light, mainly concentrated in the mucosal surface, reduces the scattering and unnecessary intermediate color, to highlight the direction of the blood vessels. It has obvious advantages including displaying mucosal blood vessels and accurately guiding biopsy; thus, it can effectively improve the detection rate of precancerous lesions and early cancer of upper gastrointestinal tract. Multicenter randomized controlled trial showed that NBI was significantly superior to white light endoscopy in detecting the early superficial esophageal squamous carcinoma.4 However, NBI had some defects in the diagnosis of the gastric diseases; due to its lower brightness, the images were darker than that of white light endoscopy, especially in the large lumen, such as stomach; therefore, the clarity was limited even when the lens was close to the mucosa.
Flexible spectral imaging color enhancement (FICE), dividing the white light into different wavelengths, observes the mucosa layer structure and mucosa intravascular hemodynamics, and focuses on the precise examination of early cancer by a remarkable comparison of the lesions to the normal mucosa. However, FICE shows a dark imaging in case of long observation distance, and it has an unsatisfactory imaging of gastric mucosal microstructure.
Blue laser imaging system combines narrow-spectrum blue laser with white light to make up the deficiency of NBI and FICE. During the observation of early cancer, it, under low-medium magnification,3 can observe the white spots and white area on the mucosal surface, which correspond margin crypt epithelium. And this suggests that BLI has a longer visual distance in observation of lesions, and can obtain images with wide observation area and high focusing. This kind of high resolution image is particularly clear in displaying the mucosal surface microstructure missing of undifferentiated gastric cancer.
Application of Blue Laser in Detection of Digestive Tract Early Stage Cancer
The Diagnosis and Application of Blue Laser in Esophageal Early Stage Cancer
The global incidence of esophageal cancer is also increasing year by year, the 5-year survival rate of early esophageal could reach as high as 80%. Early esophageal cancer has no specific performance under common white light endoscopy, and the flat lesion is especially difficult to discern with a single white light endoscopy.5 Blue laser imaging, with or without magnification, can help the diagnosis of esophageal lesions and it can lead to strong color contrast of brown esophageal squamous cell carcinoma with the surrounding tissues without amplification.1 Normal intraepithelial papillary capillary loop (IPCL) shows brown dots or small circles, with fine diameter and consistent morphology, arranging regularly in BLI. Blue laser imaging can clearly display IPCL in brown lesion area, similar to NBI.3 Arima et al according to the microvascular morphology put forward another kind of superficial esophageal lesion classification method, namely esophageal microvascular classification, which divided microvascular morphology into 4 types, and put forward the concept of avascular area.6 Blue laser imaging can display nonvascular mucosa in various diameters by magnification3; thus, contributing to the judgment of the invasive depth of early esophageal cancer. The Japan Esophageal Society has proposed a more concise new type in 2012 combined with the 2 mentioned classification methods: type A, without IPCL change or with slight change in IPCL; type B, with obvious microvascular morphological changes. Type B can be further divided into 3 subtypes, B1, B2, and B3, which can determine the infiltration depth of tumor. Preliminary verification shows that their accuracy in evaluating the infiltration depth of the superficial esophageal squamous carcinoma is 90% on average.7 Tomie et al included 25 patients with superficial esophageal squamous carcinoma into this study. The BLI-bright mode is superior to NBI and white light mode in the identification of superficial esophageal squamous carcinoma both in the subjective evaluation of endoscopic physicians on lesions scores, and in the objective evaluation of calculation on the color contrast of lesions and the surrounding tissues.8
The Diagnosis and Application of Blue Laser in Gastric Early Stage Cancer
Gastric cancer is the second leading cause of malignant tumor in the world, with about 990 000 new cases every year. If it can be early found and endoscopic treatment is given, the early gastric cancer can be cured over 90%.1,4 The mucosal surface of most gastric cancer is uneven, and BLI can observe irregular microvascular morphology from the fuzzy mucosal surface.3 Yao et al based on the double changes in microvascular morphology and surface microstructure, proposed the “VS” classification, and the irregular dividing line can diagnose the early gastric cancer.9 A single-center prospective study adopted the mentioned diagnostic criteria, combining magnifying endoscopy with BLI (ME-BLI) in the diagnosis of early gastric cancer, and the results suggested ME-BLI had similar performance in diagnosis of early gastric cancer with magnifying endoscopy combined with NBI (ME-NBI).10 Yagi et al also found that ME-BLI had more detailed observation of mucosal microstructure than ME-NBI.11 Kimura-Tsuchiya et al resulted that ME-BLI could better visualize the microstructures of the early gastric cancer with shallow crypts compared with ME-NBI. Therefore, ME-BLI could enable a more accurate diagnosis of early gastric cancer with shallow crypts12; Dohi et al researched that M-BLI and M-BLI-bright provided excellent visualization of microstructures and microvessels similar to M-NBI. Irregular microsurface pattern in a moderately differentiated adenocarcinoma might be frequently visualized using M-BLI and M-BLI-bright compared with using M-NBI.13 Early gastric cancer can be divided into the differentiated and undifferentiated types. Compared with undifferentiated type, differentiated gastric cancer has relatively better lymph node metastasis and prognosis14; thus, it has important clinical significance to accurately distinguish them. The microvascular morphology of the differentiated gastric cancer observed by BLI can be divided into Fine-net-work pattern (FNP) and intralobular loop (ILL); FNP type is characterized by the disappearance of the surface gland and irregular grid microvessels; ILL type is characterized by irregular papillary surface gland, with ring capillaries inside, which form white ring sign (white ring for the margin crypt epithelium); the irregular microvessels of undifferentiated type gastric cancer are curled and spiral (corkscrew pattern).3,15–16 Missing of surface microstructure is also a feature of undifferentiated early gastric cancer.17 Some scholars have pointed out that, compared with tubular adenocarcinoma, differentiated gastric carcinoma with papillary adenocarcinoma structure (no matter the main histological type or not) has a higher degree of malignancy.18 For the observation of the microvascular morphology of early gastric cancer, BLI has similar effect with FICE and NBI, which can be used to distinguish the differentiated and undifferentiated lesions3 by high magnification observation. Blue laser imaging can also assist the diagnosis of early gastric cancer by observing the appearance characteristics of the intestinal metaplasia of gastric mucosa.3 Gray nodular protruding is the specific appearance of intestinal metaplasia under the white light endoscopy, but its sensitivity is not high. Blue laser imaging can make the intestinal metaplasia presenting as the green area, in stark contrast to brown stomach area, and helps to detect early cancer in the area of the intestinal metaplasia by observing the color difference and surface microstructure changes. Its effects are similar as the light blue crest (LBC) of NBI, but BLI can strongly indicate brighter LBC in a long distance.3
Application of BLI in the Diagnosis of Early Colorectal Lesions
The judgment of the infiltration depth of early colorectal cancer is of great help to clinician to select surgical method. In order to investigate whether the BLI also helps to determine the infiltration depth of early colorectal cancer, Togashi et al 19 carried out BLI endoscopic examination for 61 patients with pathologically confirmed early colorectal cancer, and the endoscopic classification of the lesions adopted Hiroshima type and Sano type. Results suggested that the infiltration depth of Sano type IIIb and Hiroshima type C3 colorectal cancer was in consistent with the T1b stage of pathology TNM stage, and BLI may be an effective way to determine the submucous infiltration depth of the early colorectal cancer. Yoshida et al 20 conducted a multicenter open study in which the enrolled 104 cases of patients with colorectal cancer were given NBI and BLI magnification observation. The results showed that the accuracy of BLI amplification (74.0% [77/104]) was similar to NBI amplification (77.8% [81/104]) in the diagnosis of early colorectal infiltration depth. It is suggested that BLI amplification can predict the pathologic diagnosis and infiltration depth of early colorectal cancer.
The BLI-bright mode enhances the brightness of the images based on emphasizing the microvessels and microstructure of the mucosal surface; therefore, it shows a strong clinical advantage in the discovery of colorectal polyps. Yoshida et al compared white light image and BLI—bright image of 100 colorectal polyps and found that both experienced and inexperienced endoscopy technicians had higher scores to BLI-bright image than white light images in distinguishing lesions.21 It has been revealed from the clinical experience that the observation results under BLI and BLI-bright mode were affected by the intestinal preparation and the luminosity of the field of vision.
Blue laser imaging as a new technique has the advantages of bright, clear, and strong administrative imaging, which make it possible to deep explore the mucosal superficial capillaries and surface microstructure, improve the discernibility degree of early upper gastrointestinal tract cancer. Although BLI has its unique advantages compared with the existing technique, its introduction time is short. More researches are needed to prove its effect to the diagnosis of early upper gastrointestinal tract cancer, and it is going to take some time before widely used in clinical.
Abbreviations
- BLI
blue laser imaging
- FNP
Fine-net-work pattern
- ILL
intralobular loop
- IPCL
intraepithelial papillary capillary loop
- LBC
light blue crest
- ME-BLI
magnifying endoscopy with BLI
- ME-NBI
magnifying endoscopy combined with NBI
- NBI
narrow-band imaging
Footnotes
Authors' Note: Yiliang Bi and Min Min contributed equally to this work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding.: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Beijing Nova Program (no. Z171100001117090), National Key Research and Development Program of China (no. 2018YFB0407200 ), National Natural Science Foundation of China (no. 81572953),B eijing Natural Science Foundation (no.7182122).
ORCID iD: Min Min, MD, PhD  https://orcid.org/0000-0002-0850-9480
https://orcid.org/0000-0002-0850-9480
Xiaosong Li, MD, PhD  https://orcid.org/0000-0002-5731-8488
https://orcid.org/0000-0002-5731-8488
References
- 1. Osawa H, Yamamoto H, Miura Y, et al. Blue laser imaging provides excellent endoscopic images of upper gastrointestinal lesion. Video J Encycl GI Endosc. 2014;1(3-4):607–610. [Google Scholar]
- 2. Dohi O, Yagi N, Naito Y, et al. Blue laser imaging-bright improves the real-time detection rate of early gastric cancer: a randomized controlled study. Gastrointest Endosc. 2019;89(1):47–57. [DOI] [PubMed] [Google Scholar]
- 3. Osawa H, Yamamoto H. Present and future status of flexible spectral imaging color enhancement and blue laser imaging technology. Dig Endosc. 2014;(26 suppl 1):105–115. [DOI] [PubMed] [Google Scholar]
- 4. Muto M, Minashi K, Yano T, et al. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol. 2010;28(9):1566–1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ishihara R, Tanaka H, Iishi H, et al. Long-term outcome of esophageal mucosal squamous cell carcinoma without lymphovascular involvement after endoscopic resection. Cancer. 2008;112(10):2166–2172. [DOI] [PubMed] [Google Scholar]
- 6. Arima M, Tada M, Arima H. Evaluation of microvascular patterns of superficial esophageal cancers by magnifying endoscopy. Esophagus. 2005;2(4):191–197. [Google Scholar]
- 7. Oyama T, Ishihara R, Takeuch M, et al. Tu1588 usefulness of Japan Esophageal Society Classification of magnified endoscopy for the diagnosis of superficial esophageal squamous cell carcinoma. Gastrointest Endosc. 2012;75(suppl 4):AB456. [Google Scholar]
- 8. Tomie A, Dohi O, Yagi N, et al. Blue laser imaging-bright improves endoscopic recognition of superficial esophageal squamous cell carcinoma. Gastroenterol Res Pract. 2016;2016:6140854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yao K, Anagnostopoulos GK, Ragunath K. Magnifying endoscopy for diagnosing and delineating early gastric cancer. Endoscopy. 2009;41(5):462–467. [DOI] [PubMed] [Google Scholar]
- 10. Dohi O, Yagi N, Majima A, et al. Diagnostic ability of magnifying endoscopy with blue laser imaging for early gastric cancer: a prospective study. Gastric Cancer. 2017;20(2):297–303. [DOI] [PubMed] [Google Scholar]
- 11. Yagi N, Naito Y, Dohi O, et al. Mo1649 The efficacy of a Novel Blue LASER imaging system for the diagnosis of early gastric cancers; a Prospective Single Center Open Trial. Gastrointest Endosc. 2013;77(suppl 5):AB458. [Google Scholar]
- 12. Kimura-Tsuchiya R, Dohi O, Fujita Y, et al. Magnifying endoscopy with blue laser imaging improves the microstructure visualization in early gastric cancer: comparison of magnifying endoscopy with narrow-band imaging. Gastroenterol Res Pract. 2017;2017:8303046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dohi O, Yagi N, Yoshida S, et al. Magnifying blue laser imaging versus magnifying narrow-band imaging for the diagnosis of early gastric cancer: a prospective, multicenter, comparative study. Digestion. 2017;96(3):127–134. [DOI] [PubMed] [Google Scholar]
- 14. Yoshida N, Hisabe T, Hirose R, et al. Improvement in the visibility of colorectal polyps using blue laser imaging. Gastrointest Endosc. 2015;82(3):542–549. [DOI] [PubMed] [Google Scholar]
- 15. Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video). Endoscopy. 2004;36(12):1080–1084. [DOI] [PubMed] [Google Scholar]
- 16. Yokoyama A, Inoue H, Minami H, et al. Novel narrow-band imaging magnifying endoscopic classification for early gastric cancer. Dig Liver Dis. 2010;42(10):704–708. [DOI] [PubMed] [Google Scholar]
- 17. Kanesaka T, Sekikawa A, Tsumura T, et al. Absent microsurface pattern is characteristic of early gastric cancer of undifferentiated type: magnifying endoscopy with narrow-band imaging. Gastrointest Endosc. 2014;80(6):1194–1198.e1. [DOI] [PubMed] [Google Scholar]
- 18. Ito T, Takizawa T, Horiguchi Z, et al. Gastric adenocarcinoma with submucosal invasion: histological appearance and biological behavior [in Japanese]. Stomach Intest. 2007;42:7–13. [Google Scholar]
- 19. Togashi K, Nemoto D, lsohata N, et al. Use of blue laser imaging for identification of colorectal cancer with deep submucosal invasion. Gastrointest Endosc. 2014;79(5):AB476–AB476. [Google Scholar]
- 20. Yoshida N, Hisabe T, Inada Y, et al. The ability of a novel blue laser imaging system for the diagnosis of invasion depth of colorectal neoplasms. J Gastroenterol. 2014;49(1):73–80. [DOI] [PubMed] [Google Scholar]
- 21. Doyama H, Yoshida N, Tsuyama S, et al. The “white globe appearance” (WGA): a novel marker for a correct diagnosis of early gastric cancer by magnifying endoscopy with narrow-band imaging (M-NBI). Endosc Int Open. 2015;3(2):E120–E124. [DOI] [PMC free article] [PubMed] [Google Scholar]