Abstract
Objective:
Work disability rates are high among people with rheumatic and musculoskeletal conditions. Effective disability preventive programs are needed. We examined the efficacy of a modified vocational rehabilitation approach delivered by trained occupational therapists and physical therapists on work limitation and work loss over two years among people with rheumatic and musculoskeletal conditions.
Methods:
Eligibility criteria for this single-blind parallel-arm randomized trial included 21–65 years of age, 15 or more hours/week employment, self-reported doctor-diagnosed rheumatic or musculoskeletal condition, and concern about staying employed. The intervention consisted of a 1.5 hour meeting, an action plan, written materials on employment supports, and telephone calls at 3-weeks and 3-months. Control group participants received the written materials. The primary outcome was the Work Limitations Questionnaire (WLQ), Output Job Demand subscale. The secondary outcome was work loss. Intent to treat analyses were performed. This study is registered with ClinicalTrials.gov number NCT01387100.
Results:
Between October 2011 and January 2014, 652 individuals were assessed for eligibility. 287 participants were randomized: 143 intervention and 144 control participants. 264 participants (92%) completed two-year data collection. There was no difference in the mean WLQ change scores from baseline to two year follow-up (−8.6 ± 1.9 intervention vs. −8.3 ± 2.2 control (p=.93)). Of the 36 participants who experienced permanent work loss at two years: 11 (8%) were intervention participants and 25 (18%) control participants (p=.03).
Conclusion:
The intervention did not have an effect on work limitations but reduced work loss. The intervention can be delivered by trained rehabilitation therapists.
Rheumatic and musculoskeletal conditions are leading causes of work disability.(1–3) Nearly a third of employed adults with arthritis between the ages of 18–64 report work limitations due to their health condition(4) and 23–45% of people with inflammatory rheumatic conditions are unemployed within 10 years of diagnosis.(5–8) Arthritis at work productivity loss, also termed presenteeism, is estimated to be $1250 per employee per year in the United States.(9) Preventing permanent work loss is a major priority.
A previous randomized trial by Allaire et al.(10) demonstrated efficacy of a vocational rehabilitation intervention focused on job accommodation, disability employment self-advocacy, and career counseling delivered by rehabilitation counselors to employed persons with rheumatic diseases at risk for work loss compared to an active control. A 40% reduction in work loss occurred in the intervention group compared to the control group that received mailed written employment support information over four years of follow-up.(10)
In the Allaire et al. trial.,(10) the Work Experience Survey (WES),(11) a structured tool for identifying health-related workplace barriers, was used in the experimental group for the job accommodation part of the intervention. The WES is a validated tool for use by rehabilitation professionals to identify an individual’s work-related barriers and possible solutions.(11) The WES was augmented in the Allaire et al. trial to include barriers beyond the workplace, such as commuting difficulties, as these had been identified as arthritis work loss risk factors.(12) Subsequently, the WES was revised to comprehensively reflect barriers important for people with rheumatic conditions; this version is called the Work Experience Survey for Rheumatic Conditions (WES-RC).(13)
Rehabilitation counselors delivered the intervention in the Allaire et al. trial,(10) however, access to these services is generally limited for most employed people with rheumatic or musculoskeletal conditions. Occupational therapists (OTs) and physical therapists (PTs) address work issues(13, 14) and may be able to deliver the key parts of the Allaire et al.(10) intervention.
To determine whether OTs and PTs could successfully reduce work limitations and work loss among people with rheumatic and musculoskeletal conditions, we conducted a two-year randomized controlled trial titled, “Efficacy of a Modified Vocational Rehabilitation Intervention (the Work It Study).” The Work It Study modifies Allaire et al.’s(10) intervention to one in which OTs and PTs used the WES-RC to identify health-related work barriers and to foster a discussion about possible solutions to the barriers and provided information about disability related employment issues and career counseling resources. The primary aim of the Work It Study was to examine whether people who received this work disability prevention program had less work limitation over two years of follow-up compared to persons receiving a minimal control intervention (e.g. printed material about employment resources). The secondary aim was to examine whether persons who received the modified vocational rehabilitation intervention had less work loss over two years compared to those receiving the control intervention.
Methods:
The Work-It Study was a two-year, single-blind parallel-arm randomized controlled trial conducted in Massachusetts, United States. This clinical trial was approved by the Institutional Review Board for Boston University and all participants provided written informed consent. The trial was registered at ClinicalTrials.gov under the number NCT01387100.
Participants were recruited between October 2011 and January 2014 from community and medical sources (e.g., rheumatologists’ practices, medical registries, newspapers, community online postings, flyers, professional organizations (e.g., the Arthritis Foundation), and social support groups. To be eligible for the study, participants were required to be 21–65 years of age, employed at least 15 hours per week, living or working in Massachusetts, self-reported doctor-diagnosed rheumatic or musculoskeletal condition such as rheumatoid arthritis, psoriatic arthritis, osteoarthritis, systemic lupus erythematosus, scleroderma, and fibromyalgia, and self-reported concern about their ability to stay employed due to their health. Exclusion criteria included being on worker’s compensation or disability leave at the time of the telephone screening (unless also working 15 hours or more per week for pay), having plans to leave work or retire in the next two years, participation in other research studies related to employment, and inability to speak or understand English. After one year, eligibility criteria were expanded to allow people with chronic low back pain to participate, yet exclude people with work-related back injuries, to increase enrollment.
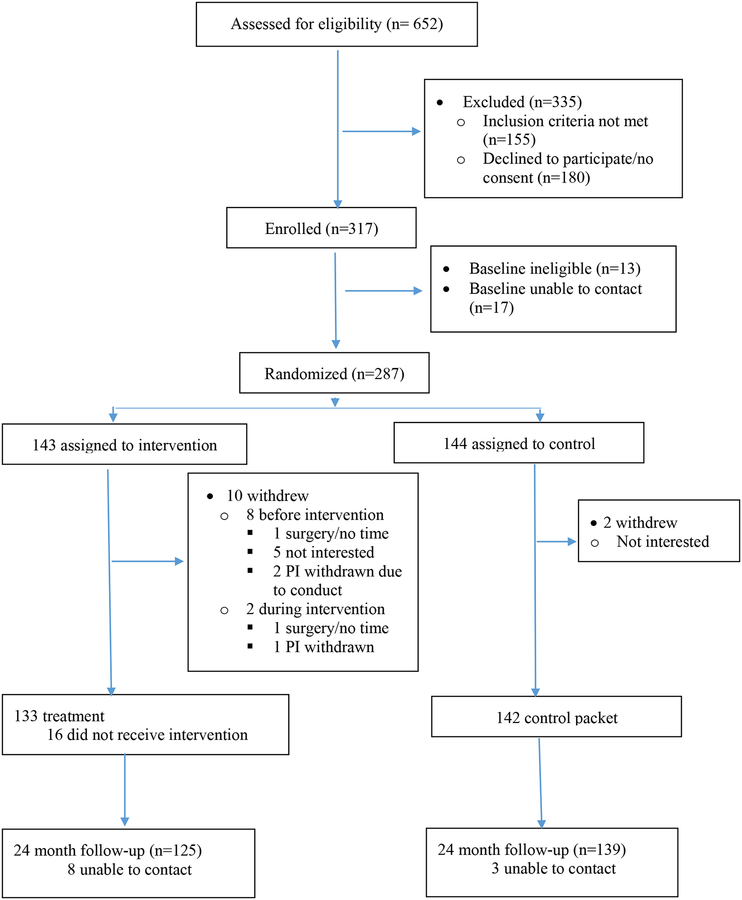
Eligible subjects who agreed to participate in the study were mailed consent forms and once written consent was obtained by mail, participants were screened for eligibility by asking their employment status at baseline. (Figure 1)
Figure 1.
CONSORT Study Flow Diagram
Randomization and Blinding
Participants were randomly assigned to intervention or control using a computer-generated list stratified by age (age <55 vs age ≥ 55) and gender, with an equal probability of assignment to the intervention or control arm. Randomization was conducted using statistical software and assignments were placed in sealed and opaque envelopes in numerical order maintained in a locked file by the study coordinator. Study investigators and data collectors were blinded to the treatment assignments. During the consent process, participants were told they would be assigned to one of two groups: i) receipt of a 1.5 hour meeting with a trained rehabilitation therapist and two telephone calls 3-weeks and 12-weeks after the initial meeting with information on remaining employed, or ii) receipt of written materials on remaining employed for people with rheumatic and musculoskeletal conditions. Data collectors were blinded to group assignment prior to data collection calls.
Intervention
Materials
The Work Experience Survey for Rheumatic Conditions (WES-RC) was used to deliver the work barrier reduction portion of the intervention.(13) The WES-RC consists of demographics, job and health information and checklists of a wide range of potential workplace barriers: i) getting ready for and traveling to and from, or for work (e.g., using public transportation), ii) workplace access (e.g., opening doors), iii) completing work activities (standing on feet too long), iv) relationships with people at work (e.g., supervisor not supportive), v) working conditions and company policies (e.g., lighting), and vi) work, career and home and health care responsibilities(e.g., job mastery)). The WES-RC also contains sections on barrier prioritization and identification of the three most problematic barriers. The WES-RC Solutions Companion Manual was developed through expert consultation to assist the interventionist with identifying possible solutions to these barriers.
A packet of written resource materials, which included information about employment retention organizations (e.g. Job Accommodation Network (JAN)), disability and employment legal resources (e.g. Americans with Disabilities Act), local vocational rehabilitation programs, local disability advocacy centers, voluntary health agencies (e.g. Arthritis Foundation), and chronic disease management websites was provided to participants.
Procedures
Prior to providing the intervention, ten trained, licensed OTs and PTs received a formal 8-hour training by study investigators. Study materials were discussed and the therapists practiced use of the WES-RC and Solution Manual using vignettes.
Experimental group program
The intervention was delivered in a 1.5-hour meeting with a therapist at a convenient location. During the 1.5 hour meeting the therapists used the WES-RC to assess a participant’s health and vocational background and work barriers. Therapists used the solution companion manual to suggest solutions to WES-RC barriers indicated. All participants were provided the packet of written resource materials. Referrals to resources or other providers were given as needed. At the completion of the meeting a written action plan was developed and kept by both participant and therapist. After the 1.5 hour meeting, the participant received phone calls at 3-weeks and 3-months to address progress towards implementing the strategies and identifying new solutions if needed.
A few participants called the study coordinator as a means to reach the interventionist beyond the scheduled 3-month follow-up but this was minimal. Where feasible, additional contact from the interventionist (by telephone) was made.
Control group program
Participants in the control group received the packet of written resource materials by mail.
Outcomes and assessments
All participants were interviewed at baseline, 6-, 12-, and 24-months by three trained interviewers blinded to treatment assignment. Data were collected over the telephone.
Our main outcomes fall into two categories: presenteeism and work status. The primary outcome of this study was work limitation assessed with the Work Limitations Questionnaire (WLQ), a measure of presenteeism.(15) The WLQ assesses limitations in a person’s ability to perform work activities due to a health condition and consists of four separate subscales. To minimize participant burden, the Output Job Demand subscale was selected from among the four WLQ subscales since it was most likely to be impacted by the intervention. The five items in this subscale pertain to difficulty performing specific work tasks over the prior two weeks due to a physical or emotional health condition or problem (e.g., “in the past two weeks, how much of the time did your physical health or any emotional problems make it difficult for you to finish your work on time?”). The responses range from none of the time (0%) to all of the time (100%). The subscale value is the average of these time proportions across the WLQ items. Validity and reliability in assessing work limitation for people with arthritis is established.(16, 17) The last item of the subscale was unintentionally left off the assessment form and was treated as a missing value for all subjects. WLQ directions state that a missing value should be reported for a subscale when a majority of items are missing. So, if two subscale items were missing in addition to the item that was excluded inadvertently, the WLQ score was considered missing.
The main secondary outcome of this study was employment. To ascertain employment status, participants were asked, “Are you employed (by “employed” we mean full time paid work, part-time paid work, or short-term leave of absence)? If persons indicated they were unemployed, they were asked if they were i) retired, ii) disabled (long-term), iii) laid off, or iv) other. People who indicated they were ‘disabled’ were asked if they were on long-term or short-term disability. If the person became unemployed (i.e., they experienced work loss), they were asked the date they became unemployed and whether they had any temporary unemployment (i.e., work loss) since the last time the data collectors spoke with them. Unemployment responses of ‘retired,’ ‘long-term disabled,’ ‘laid off’, and ‘other’, were considered as ‘unemployment’; whereas, ‘short-term disabled’ was deemed as still employed. Permanent work loss was defined as becoming unemployed during the follow up period and remaining unemployed at the end of the study. Any work loss was defined as becoming unemployed at any time over the follow-up period even if the participant became employed again.
Other secondary outcomes included the World Health Organization Health and Work Performance Questionnaire, Presenteeism subscale (HPQ). Three items inquiring about one’s self-assessment of his or her usual work performance over the past 4 weeks were used. Two scores are computed from these three items: i) the absolute score assessing one’s self-rated work performance, and ii) a relative score comparing one’s self-rated work performance to self-performance compared to peers.(18) The relative score was computed with anchors between 0.25 and 2, with 0.25 as the worst performance and 2.0 is the best performance. Absenteeism, a work status outcome, was ascertained by self-report count of days of work missed over the past 3 months due to health.
Statistical analyses
Based on previous studies using the output demand scale of the WLQ, a standard deviation of 24.5 was expected(16, 17, 19) Previous research showed the WLQ score changed 13 points in an observational study over 18 months(20) with similar findings in a depression medication trial.(21) We expected a slightly smaller effect since we were not providing pharmacological treatment. Based on Allaire et al.,(10) we anticipated we could recruit 350 over a two year time period. Using 350 as a sample size we could detect a difference of 7.5 units on the WLQ output job demand scale using a two-sided t-test at the 0.05 significance level with 80% power.
An intent-to-treat analysis approach was used. All randomized subjects were used in analyses regardless of participation in the intervention or completeness of follow-up. Multiple imputation was used to fill in missing WLQ subscale values. Missing values were due to missed visits, participants being unemployed at the time of an assessment visit (and thus unable to report difficulty with their work), or participants having two or more missing items on the WLQ subscale. Imputation was done using the MCMC method within the SAS procedure PROC MI. The imputed values were generated using the WLQ subscale score for baseline and all follow up visits as well as treatment group, age, gender, race, marital status and education level. The imputation was replicated 25 times and PROC MIANALYZE was used to combine the estimates across imputations for all analysis involving the imputed values. An additional ‘worst case’ imputation analysis was performed where subjects unemployed at the time of an assessment visit were assigned the highest possible value on the subscale (WLQ subscale = 100). A similar imputation approach was used for the HPQ and absenteeism outcomes.
For the primary analysis, a two-sample t-test was used to assess the effect of treatment on the 24-month change in the WLQ subscale. Adjusted analyses were performed using a linear regression model adjusting for age, sex, race, and education level. We adjusted for age and sex as these factors had been used to stratify the randomization. In addition, we adjusted for race and education level due to their importance for work-related outcomes. A mixed-effects regression model with random intercept term was used to analyze the repeated WLQ subscale values with adjustment for assessment time, age, sex, race and educational level. In this model assessment for treatment effect is based on the interaction between time and treatment. Similar mixed-effects regression models were used to analyze repeated measures of the HPQ. For absenteeism, a negative binomial model for count data was used with a generalized estimating equations correction for the correlation between repeated outcome assessments within subjects.
The treatment effect on time from randomization to permanent work loss was assessed using the Kaplan-Meier procedure and the log-rank test. Cox regression with adjustment for age, sex, race, and education level was used to obtain the hazard ratio for the effect of treatment. The same approach was also used to evaluate the time to the first work loss, temporary or permanent, for a subject.
Sensitivity analyses were also performed to examine: 1) the impact on results of excluding participants randomized to the intervention who did not participate in it, 2) the treatment effects for participants suffering lower back pain since inclusion criteria were broadened to include this diagnosis, and 3) use of ‘worst case’ scores for the WLQ, HPQ and absenteeism for people who became unemployed during follow-up.
Results:
652 individuals were assessed for eligibility between October 2011 and January 2014. 335 individuals were excluded, with 317 persons enrolled. See Figure 1 CONSORT Study Flow Diagram. Of these, 13 were ineligible at baseline and 17 who returned consent forms were unable to be contacted despite repeated attempts. Thus, 287 participants were randomized: 143 to intervention and 144 to control. Twelve participants (10 in intervention; 2 in control group) were randomized but withdrew prior to providing any follow-up information.(See Figure 1) Sixteen participants did not receive the treatment due to scheduling conflicts with the interventionists but provided follow-up data. At 24 month follow-up, data were collected on 264 participants (92% of the randomized participants). 213 WLQ subscale values (20%) were missing across all the visits and were imputed for analyses. 81 of these missing values were due to work loss (57 control group, 24 intervention group).
The mean age for the study population was 50.4 (range 23–66). 73% were female, 69% white, 65% not currently married and 59% had a college degree or higher.(Table 1) Osteoarthritis was the most commonly reported condition (43%), followed by rheumatoid arthritis (23%), chronic back pain (13%), fibromyalgia (11%) and psoriatic arthritis (5%). Systematic lupus erythematosus, psoriatic arthritis, ankylosing spondylitis, and systemic sclerosis were reported by 2%, 1%, 1%, and 1% of respondents respectively. Seven percent also reported a condition classified as ‘other.’
Table 1.
Baseline Characteristics of Trial Participants
| Control | Intervention | P-Value* | |
|---|---|---|---|
| N | 144 | 143 | |
| Baseline Age, Mean ± SD | 50.5 ± 10.6 | 50.3 ± 10.7 | 0.84 |
| Sex, n (%) | 0.82 | ||
| Female | 104 (72) | 105 (73) | |
| Male | 40 (28) | 38 (27) | |
| Race, n (%) | 0.20 | ||
| White | 104 (73) | 94 (66) | |
| Not White | 39 (27) | 49 (34) | |
| Education, n (%) | 0.94 | ||
| College/Graduate Degree | 84 (58) | 84 (59) | |
| High School | 60 (42) | 59 (41) | |
| Marital Status, n (%) | 0.34 | ||
| Not Currently Married** | 90 (63) | 97 (68) | |
| Married | 54 (38) | 46 (32) | |
| Live Alone, n (%) | 0.74 | ||
| No | 94 (65) | 96 (67) | |
| Yes | 50 (35) | 47 (33) |
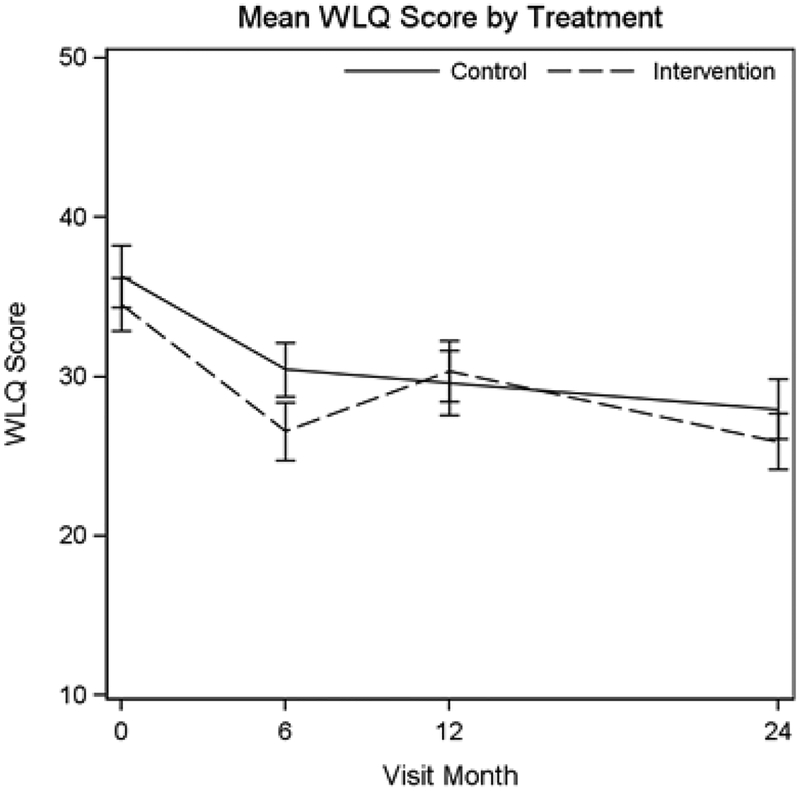
The WLQ score at baseline was 36.29 for the control group and 34.53 for the intervention group (Table 2). The mean change in WLQ job demand output subscale scores from baseline to 24 months was −8.33 ± 2.22 for the control group and −8.60 ± 1.92 for participants in the intervention arm. There was no significant difference between the control and intervention groups in change in WLQ subscale score from baseline to 24 months (p = 0.93) nor at any other visit (Table 2). Additionally, in the repeated measures model the interaction between treatment and time was not significant (p=0.79). Adjusting for age, sex, race and education did not change the effect estimate or level of significance for the effect treatment on change in WLQ subscale score from baseline to 24 months.
Table 2:
WLQ Score at each visit, mean + SE***.
| Control (n = 144) |
Intervention (n = 143) |
P-value* | |
|---|---|---|---|
| Baseline | 36.29 ± 1.93 | 34.53 ± 1.67 | 0.49 |
| 6 Months | 30.43 ± 1.72 | 26.57 ± 1.82 | 0.11 |
| 12 Months | 29.59 ± 2.02 | 30.33 ± 1.92 | 0.79 |
| 24 Months | 27.97 ± 1.86 | 25.93 ± 1.77 | 0.43 |
| Time × Treatment Effect** | 0.79 | ||
| Change from Baseline | |||
| 6 Months | −5.86 ± 2.02 | −7.96 ± 1.80 | 0.43 |
| 12 Months | −6.70 ± 2.15 | −4.20 ± 1.96 | 0.40 |
| 24 Months | −8.33 ± 2.22 | −8.60 ± 1.92 | 0.93 |
Student’s T-test for independent Samples
Mixed-effects regression model
Missing values due to missed visit, work loss and more than 2 missing components on the 4 point scale imputed.
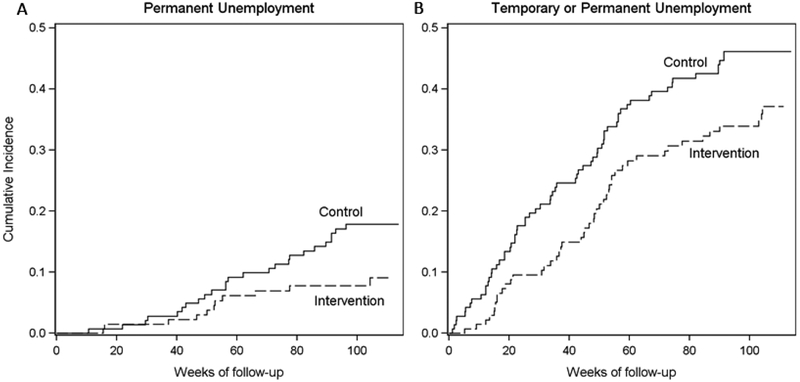
During the follow up period, 36 participants experienced permanent work loss; 25 (18%) in the control arm and 11 (8%) in the intervention arm (Table 3). Kaplan-Meier estimates for the cumulative incidence for time to permanent work loss are shown in figure 3A. There was a significant difference between the control and intervention arms in time to permanent work loss (HR: 0.47 (0.23, 0.95), p = 0.034). Including any temporary work loss, 65 (46%) control participants and 47 (35%) intervention participants experienced any work loss during the follow up period. (See Figure 3B) While the rate for permanent and temporary work loss was lower in the intervention arm, this difference was at the cusp of statistical significance (HR: 0.70 (0.48, 1.01), p = 0.057). There were 2 subjects in the control arm and 3 in the intervention arm who provided no follow-up information on employment and were excluded in all time to event analyses.
Table 3:
Work Loss
| Control | Intervention | P-value* | |
|---|---|---|---|
| All Subjects, n | 142 | 140 | |
| Permanent Work Loss, n (%) | 25 (17) | 11 (8) | 0.03 |
| Any Work Loss**, n (%) | 65 (45) | 47 (33) | 0.06 |
| Subjects with Back Pain, n | 20 | 18 | |
| Permanent Work Loss, n (%) | 5 (25) | 0 (0) | 0.03 |
| Any Work Loss*, n (%) | 12 (60) | 3 17 | 0.01 |
Log-Rank Test
includes permanent work loss or any temporary work loss during the follow up period
Figure 3.
Cumulative Incidence of Time to Permanent Work Loss (A) and Temporary or Permanent Work Loss (B)
The relative HPQ score was 0.99 for controls and 1.07 for intervention subjects at baseline (p=0.0275), but the score increased by 0.07 for controls and stayed the same for intervention subjects at 24 months leading to a non-significant treatment effect (interaction p=0.289). The absolute HPQ results had a similar pattern with a baseline difference in means (7.22 controls, 7.62 intervention, p=0.05), with the control mean increasing by 0.40 and the intervention mean increasing by 0.16 at 24 months and a non-significant interaction with time (p=0.677). For our assessment of absenteeism, participants reported similar numbers of missed days in the past 3-months at baseline (3.3 days for control, 3.2 days for intervention, p=0.90), but by 24 months the number reported had dropped in the intervention arm but not the control arm (3.6 days for control, 1.4 days for intervention, p<0.001).
The sensitivity analyses in which the 16 persons who did not complete the intervention were removed did not change the results for any primary or secondary analyses. For the sensitivity analysis of the 38 participants with back pain, there was a significant effect of treatment for both time to permanent work loss (p = 0.03) and time to temporary or permanent work loss (p = 0.01). The ‘worse case’ sensitivity analysis with the lowest scores of the WLQ for people who were unemployed during that time period did not quite attain significance (p=0.0545), but the 7.3 point difference on the WLQ in favor of the intervention groups is suggestive of a treatment benefit. Using 90 days for unemployed subjects also resulted a significant difference between groups at 24 months (p = 0.01).
Discussion
Contrary to our hypothesis that our intervention would prevent work limitations leading to a non-significant positive trend on preventing work loss over 2 years, the intervention had no impact on our measurement of work limitations but did reduce work loss. We encountered more work loss in our sample than expected suggesting a significant unmet need in this population.(10)
The WLQ was selected to ascertain work limitations based on previous studies, (16, 17, 19) and the study was adequately powered to determine an effect. Another trial of an integrated care and coordinated workplace job accommodation program for people with rheumatic conditions also reported no effect of the intervention on WLQ scores.(22, 23) The WLQ may not be responsive to change for work limitation prevention. In our study, the intervention could have increased and decreased scores on specific questions on the WLQ. For example, someone may be encouraged to pace activities during the day resulting in increased difficulty getting work done on time, or someone may be encouraged to take breaks during the day which may make it easier to get work done on time. Furthermore, use of the WLQ subscale could also have reduced responsiveness. A few small studies targeting work related ergonomic interventions have shown short-term improved performance of work-related activities(24–26) but no effect on employment retention or on regaining employment.
Our intervention increased employment retention in an at risk group for whom few if any work retention interventions exist.(10, 27) Programs that involve multiple components including job accommodations, health services systems, and coordinated care may help people maintain work in the context of health related challenges.(28, 29) Now, with two efficacious trials(10) supporting our approach using a structured tool to identify barriers, problem solve solutions, as well as provide resources for community supports, we have strong evidence this approach can prevent work loss.
Our intervention may prevent work loss through several mechanisms. First, the intervention may promote and encourage advocacy by helping participants realize they are not alone in having difficulties related to working with their chronic condition. Second, the approach promotes behavioral changes through problem identification, solution generation, and development of action plans, strategies that are known to promote behavioral changes with complex daily life activities. Our intervention also may have provided valuable resources to maintain employment to people for whom this information is not readily available.
Our study has several strengths. First, this is the largest work disability prevention RCT to date for persons with rheumatic and musculoskeletal conditions and retention was excellent, minimizing internal threats to validity. Second, we recruited people through both clinical and community sources, thereby enhancing generalizability to people self-reporting these conditions in the community. Third, the intervention was nominal and leverages existing resources (PTs and OTs) that are part of most medical systems in the United States rather than rehabilitation counselors that are employed primarily by the public vocational rehabilitation program and disability insurers. PTs and OTs are licensed health care providers trained to people improve function and quality of life and rehabilitation counselors are licensed professionals trained to provide return to work counseling.
This study has a few limitations. First, the WLQ job demands output subscale was used rather than the full WLQ, which could have impacted the responsiveness to our intervention. Second, one item was inadvertently dropped in the job demands scale which could have impacted the responsiveness of the scale. Third, more people became unemployed in the study within the two year period than we anticipated and the WLQ could not be ascertained among those without a job, which created missing data specifically in subjects with the worst employment outcomes. 20% of the WLQ scores were imputed which could have biased the WLQ scores to null. Lastly, it’s possible the data collector was alerted to treatment or control assignment if the participant mentioned information about the therapist meeting during the call.
This simple, non-intensive work disability prevention program can prevent work loss in people with chronic rheumatic and musculoskeletal conditions, a group of diseases where work loss is a dreaded and common outcome. This approach could easily be implemented and widely used.
Figure 2.
Mean WLQ score by Treatment and Visit Occasion
Significance and Innovation.
First study showing efficacy of an intervention program delivered by trained occupational therapists and physical therapists to prevent premature work loss
This study contributes to the growing literature showing work accommodation and counseling approaches can prevent work disability among people with rheumatic and musculoskeletal conditions
The intervention did not improve work limitations as measured by the Work Limitations Questionnaire, Output Job Demand Scale
Acknowledgements:
We thank Dr. Timothy McAlindon who recruited participants for this study, and Mrs. Inbar Brenner and Ms. Elizabeth Simpson for study and editorial support.
Funding:
National Institute on Disability, Independent Living, and Rehabilitation Research grant number 90RT5009–01. NIAMS Multidisciplinary Clinical Research Center P60 AR47785
Contributor Information
Julie J. Keysor, Department of Physical Therapy and Athletic Training, Boston University Sargent College of Health and Rehabilitation Sciences, Boston, MA.
Michael P. LaValley, Department of Biostatistics, Boston University School of Public Health, Boston, MA.
Carrie Brown, Department of Biostatistics, Boston University School of Medicine, Boston, MA.
David T. Felson, Professor of Medicine & Epidemiology, Boston University, School of Medicine, Boston, MA; Section Chief, Clinical Epidemiology Research & Training Unit, Boston University, School of Medicine, Boston, MA; Director, Clinical Translational Science Award Training Program, Boston University, School of Medicine, Boston, MA; NIHR Manchester Musculoskeletal Biomedical Research Centre, Central Manchester NHS Foundation Trust, Manchester Academic Health Science Centre, Manchester, UK.
Rawan A. AlHeresh, Department of Occupational Therapy, MGH Institute of Health Professions, Boston, MA.
Molly W. Vaughan, RTI International, 307 Waverley Oaks Rd, Suite 101 Waltham, MA.
Robert Yood, Chief of the Division of Rheumatic Diseases and Musculoskeletal Medicine, Saint Vincent Hospital, Worcester, MA Chief of Rheumatology, Reliant Medical Group, Worcester, MA; Clinical Professor of Medicine, University of Massachusetts Medical School, Worcester, MA.
John I. Reed, Reliant Medical Group, Worcester, MA Rheumatologist, Saint Vincent Hospital, Worcester, MA Clinical Associate Professor of Medicine, University of Massachusetts Medical School, Worcester, MA.
Saralynn J. Allaire, Center for Enhancing Activity & Participation among Persons with Arthritis, Boston University, Sargent College of Health and Rehabilitation Sciences, Boston, MA.
References
- 1.McDonald M, DiBonaventura M, Ullman S. Musculoskeletal pain in the workforce: the effects of back, arthritis, and fibromyalgia pain on quality of life and work productivity. J Occup Environ Med 2011;53:765–70. [DOI] [PubMed] [Google Scholar]
- 2.Churcher L, Chan CH, Badley EM. Chronic back problems and labor force participation in a national population survey: impact of comorbid arthritis. BMC Public Health 2013;13:326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bollegala D, Perruccio AV, Badley EM. Combined impact of concomitant arthritis and back problems on health status: results from a nationally representative health survey. Arthritis Care Res (Hoboken) 2011;63(11):1584–91. [DOI] [PubMed] [Google Scholar]
- 4.Theis KA, Murphy L, Hootman JM, Helmick CG, Yelin E. Prevalence and correlates of arthritis-attributable work limitation in the US population among persons ages 18–64: 2002 National Health Interview Survey Data. Arthritis Rheum 2007;57:355–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sokka T, Kautiainen H, Pincus T, Verstappen SM, Aggarwal A, Alten R, et al. Work disability remains a major problem in rheumatoid arthritis in the 2000s: data from 32 countries in the QUEST-RA study. Arthritis Res Ther 2010;12:R42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrett EM, Scott DG, Wiles NJ, Symmons DP. The impact of rheumatoid arthritis on employment status in the early years of disease: a UK community-based study. Rheumatology (Oxford) 2000;39:1403–9. [DOI] [PubMed] [Google Scholar]
- 7.Bultink IE, Turkstra F, Dijkmans BA, Voskuyl AE. High prevalence of unemployment in patients with systemic lupus erythematosus: association with organ damage and health-related quality of life. J Rheumatol 2008;35:1053–7. [PubMed] [Google Scholar]
- 8.Yelin E, Tonner C, Trupin L, Panopalis P, Yazdany J, Julian L, et al. Work loss and work entry among persons with systemic lupus erythematosus: comparisons with a national matched sample. Arthritis Rheum 2009;61:247–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burton WN, Chen CY, Schultz AB, Conti DJ, Pransky G, Edington DW. Worker productivity loss associated with arthritis. Dis Manag 2006;9:131–43. [DOI] [PubMed] [Google Scholar]
- 10.Allaire SH, Li W, LaValley MP. Reduction of job loss in persons with rheumatic diseases receiving vocational rehabilitation: A randomized controlled trial. Arthritis Rheum 2003;48:3212–8. [DOI] [PubMed] [Google Scholar]
- 11.Roessler RT, Reed CA, Rumrill PD. The Work Experience Survey (WES) manual. Hot Springs: Arkansas Research and Training Center in Vocational Rehabilitation 1995. http://files.eric.ed.gov/fulltext/ED403691.pdf
- 12.Allaire SH, Anderson JJ, Meenan RF. Reducing work disability associated with rheumatoid arthritis: identification of additional risk factors and persons likely to benefit from intervention. Arthritis Rheum 2005;9:349–357. [DOI] [PubMed] [Google Scholar]
- 13.Allaire S, Keysor JJ. Development of a structured interview tool to help patients identify and solve rheumatic condition-related work barriers. Arthritis Rheum 2009;61:988–95. [DOI] [PubMed] [Google Scholar]
- 14.Prior Y, Amanna EA, Bodell SJ, Hammond A. A qualitative evaluation of occupational therapy-led work rehabilitation for people with inflammatory arthritis: perspectives of therapists and their line managers. Br J Occup Ther 2015;78:467–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lerner D, Amick BC, Rogers WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Med Care 2001;39:72–85. [DOI] [PubMed] [Google Scholar]
- 16.Lerner D, Reed JI, Massarotti E, Wester LM, Burke TA. The Work Limitations Questionnaire’s validity and reliability among patients with osteoarthritis. Clin Epidemiol 2002;55:197–208. [DOI] [PubMed] [Google Scholar]
- 17.Walker N, Michaud K, Wolfe F. Work limitations among working persons with rheumatoid arthritis: results, reliability, and validity of the work limitations questionnaire in 836 patients. J Rheumatol 2005;32:1006–12. [PubMed] [Google Scholar]
- 18.Kessler R, Petkhova M, Mcinnes K, Kessler R, Petukhova M, Mcinnes K. World Health Organization Health and Work Performance Questionnaire (HPQ): HPQ Short Form (Absenteeism and Presenteeism Questions and Scoring Rules). Harvard Medical School 2007. https://www.hcp.med.harvard.edu/hpq/ftpdir/absenteeism%20presenteeism%20scoring%20050107.pdf [Google Scholar]
- 19.Lerner D, Adler DA, Chang H, Lapitsky L, Hood MY, Perissinotto C, et al. Unemployment, job retention, and productivity loss among employees with depression. Psychiatr Serv (Washington, DC) 2004;55:1371–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lerner D, Adler DA, Rogers WH, Chang H, Lapitsky L, McLaughlin T, et al. Work performance of employees with depression: the impact of work stressors. Am J Health Promot 2010;24:205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kroenke K, West SL, Swindle R, Gilsenan A, Eckert GJ, Dolor R, et al. Similar effectiveness of paroxetine, fluoxetine, and sertraline in primary care: a randomized trial. JAMA 2001;286:2947–55. [DOI] [PubMed] [Google Scholar]
- 22.van Vilsteren M, Boot CR, Twisk JW, van Schaardenburg D, Steenbeek R, Voskuyl AE, et al. Effectiveness of an integrated care intervention on supervisor support and work functioning of workers with rheumatoid arthritis. Disabil Rehabil 2016:1–9. [DOI] [PubMed] [Google Scholar]
- 23.van Vilsteren M, Boot CR, Twisk JW, Steenbeek R, Voskuyl AE, van Schaardenburg D, et al. One year effects of a workplace integrated care intervention for workers with rheumatoid arthritis: results of a randomized controlled trial. J Occup Rehabil 2017;27:128–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Macedo AM, Oakley SP, Panayi GS, Kirkham BW. Functional and work outcomes improve in patients with rheumatoid arthritis who receive targeted, comprehensive occupational therapy. Arthritis Rheum 2009;61:1522–30. [DOI] [PubMed] [Google Scholar]
- 25.Baldwin D, Johnstone B, Ge B, Hewett J, Smith M, Sharp G. Randomized prospective study of a work place ergonomic intervention for individuals with rheumatoid arthritis and osteoarthritis. Arthritis Care Res (Hoboken) 2012;64:1527–35. [DOI] [PubMed] [Google Scholar]
- 26.Lacaille D, White MA, Rogers PA, Backman CL, Gignac MA, Esdaile JM. A proof-of-concept study of the “Employment and Arthritis: Making It Work” program. Arthritis Rheum 2008;59:1647–55. [DOI] [PubMed] [Google Scholar]
- 27.Hoving JL, Lacaille D, Urquhart DM, Hannu TJ, Sluiter JK, Frings-Dresen MH. Non-pharmacological interventions for preventing job loss in workers with inflammatory arthritis. Cochrane Database Syst Rev 2014;11:CD010208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cullen KL, Irvin E, Collie A, Clay F, Gensby U, Jennings PA, et al. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: an update of the evidence and messages for practitioners. J Occup Rehabil 2017. 10.1007/s10926-016-9690-x]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steenstra I, Cullen K, Irvin E, Van Eerd D. A systematic review of interventions to promote work participation in older workers. J Safety Res 2017;60:93–102. [DOI] [PubMed] [Google Scholar]