Abstract
Background:
Sexual minority young adults have higher smoking rates than the general young adult population, but reasons for this disparity are poorly understood. The current study aimed to: 1) identify real-time predictors of smoking among sexual minority and heterosexual smokers and 2) examine between-group differences in these predictors.
Methods:
We conducted an ecological momentary assessment (EMA) study in the San Francisco Bay Area, California in 2016–2017. Data from 84 young adult smokers (44% identified as sexual minority, including 29 bisexual and 8 gay/lesbian) with 6498 EMA assessments were analyzed. Both internal and external predictors and interaction terms between each predictor and sexual group were examined using generalized estimating equation models.
Results:
Common correlates of smoking were found for both groups (e.g., craving, absence of smoking bans, presence of other smokers, outside location, and seeing triggers). Unique factors for sexual minority smokers were being at a bar (aOR = 1.75, 95% CI = 1.06‒2.90) and the number of other smokers present (aOR = 1.12, 95%CI = 1.04‒1.20), while the presence of a smoking family member reduced the odds of smoking in this group (aOR = 0.13, 95%CI = 0.02–0.85). In interaction models, the number of other smokers exerted a greater influence on sexual minority participants compared to their heterosexual counterparts (aOR = 1.10, 95%CI = 1.01‒1.20), while craving (aOR = 0.84, 95%CI = 0.75–0.93) and presence of a smoking family member (aOR = 0.11, 95%CI = 0.01–0.82) had weaker influences.
Conclusions:
Our study highlights unique situational factors associated with smoking among sexual minority young adults and differences in these factors by sexual identity. Future interventions targeting sexual minorities should address bar attendance and specific triggers.
Keywords: Tobacco, Cigarette smoking, Real-time predictor, Health disparities, LGBTQ+
1. Introduction
Disparities in cigarette use and associated disease burden among sexual minorities are a growing public health concern. Worldwide, the smoking rates among lesbian, gay, bisexual, and other sexual minorities are approximately double those observed among heterosexuals (Baskerville et al., 2017; Blosnich et al., 2013; Burkhalter, 2015; McCabe et al., 2018). Data from the 2012‒2013 National Adult Tobacco Survey found that 27.7% of American sexual minority adults reported current cigarette use, corresponding to 2.3 million smokers (Johnson et al., 2016). Likewise, in the 2014 Bay Area Young Adult Health Survey, 18.6% of sexual minority participants smoked compared to 14.7% of heterosexuals (Holmes and Ling, 2017). Among sexual minority subgroups, bisexuals have higher tobacco use rates than gays or lesbians (Emory et al., 2016), and bisexuality is the fastest growing sexual identity in the United States, especially among young people (Copen et al., 2016). There are likely a variety of factors influencing this growth, such as the increasing visibility in popular culture of individuals that are neither hetero- nor homosexual (e.g., pop stars and television show characters), which may increase the social acceptability of bisexual identity (Callis, 2014). The elevated smoking rates among sexual minorities coupled with lower access to healthcare (Trinh et al., 2017) lead to an increased risk for negative health consequences (e.g., cancer, respiratory illnesses, cardiovascular diseases) (Blosnich et al., 2013; Caceres et al., 2017). Moreover, tobacco use disparities among sexual minority individuals are likely established in smoking initiation during adolescence and young adulthood (Burkhalter, 2015; Corliss et al., 2013). Sexual minority smokers start smoking and transition to daily smoking earlier than their heterosexual peers (Johnson et al., 2016; Watson et al., 2018). Hence, it is critical to understand determinants of smoking behavior among sexual minorities during young adulthood.
Risk factors for smoking among sexual minority young adults are not fully understood. Sexual minorities experience unique risk factors for smoking (e.g., minority stress, internalized homophobia) in addition to common risk factors all people experience (Blosnich et al., 2013; Meyer, 2003). However, little is known about situational drivers of real-time smoking in the natural environment for this vulnerable group. Data on situational drivers are difficult to gather reliably using traditional methods (e.g., interviews, surveys), as these retrospective methods are subject to recall bias. Ecological momentary assessment (EMA) is a data collection method that can provide reliable, real-time data on the situational drivers of smoking. EMA usually consists of multiple momentary assessments of real-time smoking and nonsmoking situations with emphasis on immediate internal experiences (e.g., mood) and external situational factors (e.g., smoking cues) (Shiffman, 2009). This method has been widely adopted in substance use research, particularly in tobacco research.
A growing body of EMA studies has demonstrated that smoking is systematically associated with particular environmental contexts (e.g., smoking regulations, presence of other smokers) (Ferguson et al., 2015; Serre et al., 2015; Shiffman, 2009; Shiffman et al., 2002; Shiftman et al., 2004; Thrul et al., 2014). Most EMA studies, however, have focused on the general population, and only a few have examined smoking among sexual minority samples. A quantitative study in which daily EMA assessments were conducted among 50 sexual minority adults reported that discrimination was associated with nicotine use (Livingston et al., 2017). Additionally, an EMA mixed-methods study described situational factors, perceptions of smoking contexts, and the roles of smoking therein among bisexual smokers (McQuoid et al., 2018). These studies, however, did not measure both internal and external factors and did not include a comparison group (i.e., heterosexual individuals). It is unclear whether the same real-time predictors that are relevant for heterosexuals are also found among sexual minority smokers and whether specific predictors play different roles in cueing smoking for this population.
To address this gap, we conducted an EMA study among sexual minority (mostly bisexual) and heterosexual young adult smokers in the San Francisco Bay Area. Our aims were: 1) to identify real-time predictors of cigarette smoking among sexual minority and heterosexual young adult smokers and 2) to examine differences in these predictors between both groups.
2. Materials and methods
2.1. Study design and setting
The study was conducted in Alameda and San Francisco Counties in the San Francisco Bay Area, California in 2016 and 2017. At baseline, participants completed an online survey via Qualtrics that asked about their demographics, smoking history, and alcohol use. During every day of the 30-day study period, participants were asked to report every time they smoked a cigarette (cigarette reports), immediately before smoking, by pushing a button on the study app which could potentially prompt them to complete an assessment (smoking surveys). The likelihood of being prompted to complete a smoking survey was based on the average number of cigarettes smoked per day at baseline (e.g., if a participant reported smoking 10 cigarettes per day, they had a 33% chance that a cigarette report would trigger a smoking survey). Respondents were also prompted randomly to complete surveys in non-smoking situations (random surveys). To limit participant burden, a maximum of 6 EMA surveys per day (3 random surveys and 3 smoking surveys) were sent to each participant. Incentives ranged from $0 to $180 gift cards according to participant compliance in completing the EMA surveys. More information about the EMA data collection protocol is provided elsewhere (McQuoid et al., 2018).
2.2. Study participants
Participants were recruited through advertisements on Facebook, Instagram, and the websites of sexual minority youth organizations. Ads contained a link to the study’s website. All Facebook and Instagram recruitment ads were posted from a Facebook page that was specifically set up for this study (“Smartphone Smoking Study”). To conduct a nested qualitative substudy (McQuoid et al., 2018), we oversampled women identifying as a sexual minority. Eligible participants were 18–26 years of age, had smoked at least 100 cigarettes in their lifetime, currently smoked at least one cigarette per day at least three days per week, and made daily use of a smartphone with Global Positioning System capabilities. Electronic informed consent was obtained on the study’s website. Eligible participants were required to send a picture of their ID to verify their identity.
2.3. Measures
2.3.1. Outcome variable
The binary outcome was smoking vs. non-smoking. Smoking surveys (triggered by cigarette reports) of real-time smoking situations were compared to random surveys of non-smoking situations.
2.3.2. Independent variables
Based on several theories of smoking motives (Best and Hakstian, 1978; Russell et al., 1974) and previous EMA studies (Shiffman et al., 2002; Thrul et al., 2014), we developed items capturing smoking antecedents in naturalistic settings. Each EMA survey asked about both internal and external factors of the situation the participant was in the time of the survey.
Three items were used to assess internal factors including affect, arousal, and craving intensity. The response for each item was coded on a 7-point Likert scale (from 1-Very unpleasant to 7-Very pleasant for affect; 1-Very low to 7-Very high for arousal and craving intensity). In addition, we tested a created variable, “stress,” by combining two measures (i.e., low affect and high arousal) based on the Affect Grid (Russell et al., 1989). To combine these two measures, affect and arousal were dichotomized (low vs. high) based on median cut-offs. However, stress operationalized this way did not predict smoking in either group (data not shown). We are not reporting this combined variable but instead presenting the individual measures (i.e., affect and arousal) separately.
External situational factors included whether smoking was banned at the participant’s current location (yes/no), type of current location (e.g., work, home), current activity (e.g., working, inactivity), type of food/beverage consumption (e.g., food, alcohol), and whether specific smoking triggers were present (e.g., seeing a tobacco product, seeing lighters/matches). In addition, participants were asked about the presence of other smokers (yes/no), their relationship to the people who were smoking (e.g., friend, family), and the number of other smokers around (0, 1, 2‒4, 5‒20, and more than 20). To approximate a continuous number of other smokers for analysis, midpoints of categories were used; 23.5 was used for the highest category, as suggested by previous EMA studies (Thrul and Kuntsche, 2015; Thrul et al., 2017).
2.3.3. Baseline characteristics
Data on demographics (e.g., age, gender, race/ethnicity, educational attainment) and alcohol use in the last 30 days were collected. Sexual minority status was dichotomized into two groups: heterosexuals vs. sexual minorities (i.e., gay/lesbian, bisexual/pansexual/ queer). Characterization of current smoking behavior was also obtained, including average smoking days per month, number of cigarettes smoked per day, smoking within 30 min of waking, intention to quit smoking, and use of non-cigarette tobacco products.
2.4. Statistical analysis
In EMA studies, the validity of findings is threatened by non-compliance (Stone and Shiffman, 2002). To address this issue, we included only respondents who completed 50% or more of their EMA surveys in this analysis. There is no standard rule for a compliance cut-off, but we decided that a cut-off of 50% would give us the best combination of data quality at the case level with retention of a sufficiently large sample for analysis.
Descriptive statistics of baseline characteristics were summarized to compare the two groups (sexual minorities vs. heterosexuals). T-tests and Wilcoxon-Mann-Whitney tests were computed to examine differences between means of normally and non-normally distributed variables, respectively. Chi-square tests were used for categorical variables. To examine situational predictors of smoking, we employed generalized estimating equations (GEE) to account for the nesting of multiple observations within each participant (Zeger et al., 1988). As recommended by Shiffman, GEE is an appropriate analysis method to contrast, across persons, the likelihood of the presence of a particular situational predictor (e.g., other smokers, alcohol consumption) over multiple smoking and nonsmoking occasions (Shiffman, 2014). First, we fit unadjusted GEE models to assess crude relationships between predictors and the outcome in a given EMA report (data not shown). Adjusted GEE models were then used to examine if crude relationships changed when controlling for potential confounders. For example, GEE models for internal factors were adjusted for drinking alcohol and the presence of other smokers, while those for external factors were adjusted for smoking bans and the presence of other smokers. These confounders were selected based on previous research (Shiffman et al., 2002; Thrul et al., 2014). Finally, to examine if relationships between predictors and smoking differed between sexual minority and heterosexual smokers, we included interaction terms between the group and each predictor in additional GEE models. In accordance with previous studies (Shiftman et al., 2004; Thrul et al., 2014), the relationships between the two internal factors (i.e., arousal and affect) and the outcome were examined in both linear and quadratic trends. Sensitivity analyses were conducted by performing all GEE analyses within the total sample (n = 149), and the results were largely similar to those reported here regarding magnitude and direction of the associations (data not shown). All tests of hypotheses were two-tailed with a significance level of α less than 0.05. Statistical analyses were performed with Stata version 15 (StataCorp, 2017).
2.5. Ethical approval
Ethics approval for this study was granted by the University of California, San Francisco Institutional Review Board.
3. Results
3.1. Sample description
Overall, 230 smokers were screened successfully, 184 completed the baseline assessment, and 149 responded to at least one EMA survey. Participant compliance, defined as percentage of EMA surveys to which participants responded, ranged from 0.8 to 100%. We excluded 65 participants who completed less than 50% of their EMA surveys. The final sample included 84 participants with an average compliance of 73.4% (range 51.8‒100%). There were no significant differences between the included and excluded participants on any demographic characteristics or smoking history (data not shown).
The sample had a mean age of 23.1 years (SD = 2.3), 39% were non-Hispanic White, and 42.86% had a college degree (Table 1). Approximately 44% of the sample (n = 37) identified as a sexual minority; among those, 78.4% (n = 29) identified as bisexual and 21.6% (n = 8) as gay/lesbian. More than half of participants smoked daily (59.5%), and there was an average of 26.2 (SD = 6.5) smoking days per month. A higher proportion of sexual minorities were female (67.6%) as compared to heterosexual participants (38.3%). The two sexual identity groups did not significantly differ on any other baseline variable.
Table 1:
Baseline characteristics by sexual identity groups
| Characteristics | Total N = 84 (100%) |
Heterosexuals N = 47 (56%) |
Sexual minorities N = 37 (44%) |
Test statistic | p- value |
|---|---|---|---|---|---|
| Demographics, n(%) | |||||
| Age (years), mean (sd) | 23.08 (2.31) | 23.11 (2.13) | 23.05 (2.56) | z = −0.29 | 0.77 |
| Gender female | 43 (51.19%) | 18 (38.30%) | 25 (67.57%) | χ2(1,84)=7.10 | 0.01 |
| Sexual identity | NA | NA | |||
| Heterosexual | 47 (100.00%) | NA | |||
| Lesbian | 6 (16.22%) | ||||
| Gay | 2 (5.40%) | ||||
| Bisexual female | 19 (51.35%) | ||||
| Bisexual male | 10 (27.03%) | ||||
| Participants’ highest education | χ2(3,83) = 3.69 | 0.13 | |||
| Less than or equal to High school | 15 (17.86%) | 11 (23.40%) | 4 (10.81%) | ||
| Some college | 27 (32.14%) | 11 (23.40%) | 16 (43.24%) | ||
| College graduate | 36 (42.86%) | 21 (44.68%) | 15 (40.54%) | ||
| Master | 5 (5.95%) | 4 (8.51%) | 1 (2.70%) | ||
| Race/Ethnicity | χ2(6,84) = 7.70 | 0.26 | |||
| Non-Hispanic White | 33 (39.29%) | 16 (34.04%) | 17 (45.95%) | ||
| Non-Hispanic Black | 3 (3.57%) | 1 (2.13%) | 2 (5.41%) | ||
| Asian | 20 (23.81%) | 15 (31.91%) | 5 (13.51%) | ||
| American Indian Alaska Native | 1 (1.19%) | 1 (2.13%) | 0 (0.00%) | ||
| Hawaiian Pacific Islander | 1 (1.19%) | 1 (2.13%) | 0 (0.00%) | ||
| Hispanic | 15 (17.86%) | 6 (12.77%) | 9 (24.32%) | ||
| Other/Multi-race | 11 (13.10%) | 7 (14.89%) | 4 (10.81%) | ||
| Smoking history, n(%) | |||||
| Daily smokers | 50 (59.52%) | 30 (63.83%) | 20 (54.05%) | χ2(1,84) = 0.82 | 0.37 |
| Smoking days per month, mean (sd) | 26.18 (6.54) | 26.60 (6.65) | 25.65 (6.46) | z = 0.96 | 0.34 |
| Cigarettes per smoking day, mean (sd) | 6.33 (4.60) | 6.45 (4.54) | 6.19 (4.74) | z = 0.47 | 0.64 |
| Smoke during 30 minutes of waking | 26 (30.95%) | 17 (36.17%) | 9 (24.32%) | χ2(1,84) = 1.36 | 0.24 |
| Use any other tobacco in the last month | 46 (54.76%) | 23 (48.94%) | 23 (62.16%) | χ2(1,84) = 1.46 | 0.23 |
| Intention to quit | χ2(2,84) = 0.30 | 0.86 | |||
| No intention in the next 6 months | 39 (46.43%) | 23 (48.94%) | 16 (43.24%) | ||
| Intend to quit in the next 6 months | 39 (46.43%) | 21 (44.68%) | 18 (48.65%) | ||
| Intend to quit in the next 30 days | 6 (7.14%) | 3 (6.38%) | 3 (8.11%) | ||
| Other, n(%) | |||||
| Alcohol use in the last 30 days | 76 (90.48%) | 43 (91.49%) | 33 (89.19%) | χ2(1,84) = 0.13 | 0.72 |
3.2. Real-time predictors of smoking situations among sexual minority and heterosexual participants
Overall, 6498 EMA assessments were analyzed, with 2636 (41%) pertaining to sexual minorities and 3862 (59%) to heterosexuals. Of all situations, 2366 (36%) were smoking situations, and 4132 (64%) were non-smoking situations. No difference in proportion of smoking situations was observed between the two groups.
Table 2 presents the results of GEE models examining internal predictors of smoking for each group. Only craving significantly predicted smoking in all GEE analyses. As expected, smoking situations were positively associated with a higher craving intensity as compared to non-smoking situations. However, craving had less impact on smoking for sexual minority participants than for heterosexual participants as indicated by a significant interaction effect (adjusted odds ratios, OR = 0.84, 95%CI = 0.75–0.93) (Fig. 1). Accordingly, sexual minority participants had 20% higher odds of smoking per 1 unit increased in craving intensity (aOR = 1.20, 95%CI = 1.11‒1.29) compared to 44% for heterosexual participants (aOR = 1.44, 95%CI = 1.33‒1.54). No significant associations between affect, arousal, and smoking were found.
Table 2:
Internal predictors of smoking situations by sexual identity groups
| Predictors | Heterosexual group | Sexual minority group | Group interaction | ||||
|---|---|---|---|---|---|---|---|
| NS-Sit n=2434 (63%) |
S-Sit n=1428 (37%) |
aOR (95%CI) | NS-sit n=1698 (64%) |
S-Sit n=938 (36%) |
aOR (95%CI) | aOR (95%CI) | |
| Affect, mean (sd) | 4.91 (1.49) | 4.67 (1.53) | 4.61 (1.53) | 4.81 (1.51) | |||
| Linear | 0.95 (0.88–1.02) | 1.04 (0.96–1.14) | 1.10 (0.98–1.23) | ||||
| Quadratic | 0.78 (0.55–1.12) | 0.75 (0.51–1.11) | 0.95 (0.56–1.62) | ||||
| Arousal, mean (sd) | 4.23 (1.59) | 4.26 (1.53) | 4.12 (1.53) | 4.33 (1.45) | |||
| Linear | 0.99 (0.92–1.06) | 1.00 (0.92–1.08) | 1.01 (0.90–1.13) | ||||
| Quadratic | 0.96 (0.69–1.32) | 0.89 (0.61–1.29) | 0.91 (0.55–1.51) | ||||
| Craving, mean (sd) | 4.06 (1.79) | 5.25 (1.37) | 1.44*** (1.33–1.54) | 3.99 (1.91) | 4.91 (1.57) | 1.20***(1.11–1.29) | 0.84** (0.75–0.93) |
Note: p<0.05;
p<0.01;
p<0.001;
NS-Sit: Non-smoking situations; S-Sit: Smoking situations; aOR: adjusted odds ratio; CI: Confidence interval.
Figure 1:
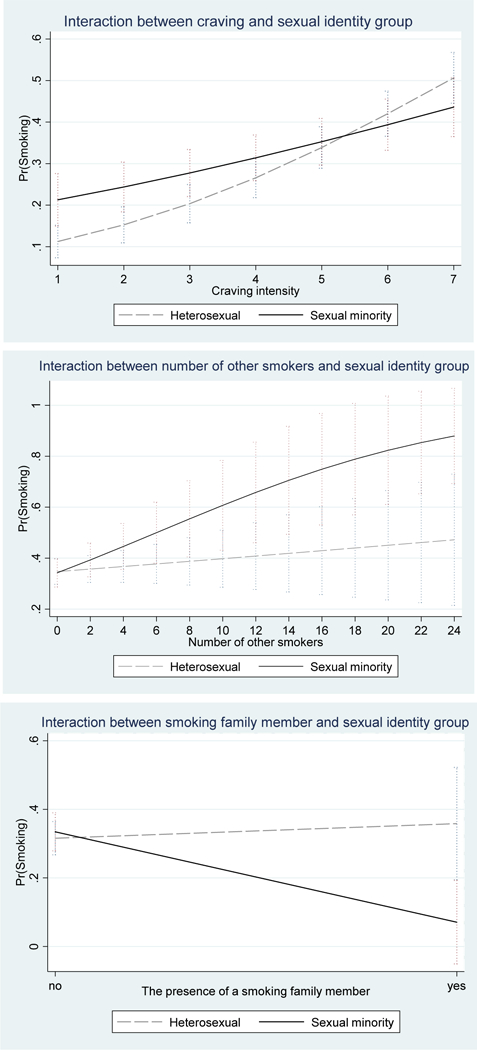
Interaction effects between situational predictors and sexual identity group.
Regarding external predictors, both groups were more likely to smoke in the absence of a smoking ban, in the presence of other smokers, while being in an outside location, in the presence of any trigger, or while seeing certain smoking triggers such as tobacco products or lighters/matches (Table 3). Several external factors predicted smoking differently between the two groups. Among sexual minority participants, being at a bar increased the odds of smoking (aOR = 1.75, 95%CI = 1.06‒2.90), whereas being with smokers who were family members decreased the odds of smoking (aOR = 0.13, 95%CI = 0.020.85). Furthermore, the presence of a family member who was smoking had a weaker impact on smoking for sexual minority participants than for heterosexual participants as indicated by a significant interaction effect (aOR = 0.11, 95%CI = 0.01–0.82) (Fig. 1). Notably, although the presence of other smokers was a significant predictor of smoking for both groups, the dose response relationship between the number of other smokers and the likelihood of smoking in that situation was only significant for sexual minority participants (aOR = 1.12, 95%CI = 1.04‒1.20). Furthermore, the significant interaction term between the number of other smokers and the sexual identity group (aOR = 1.10, 95%CI = 1.01‒1.20) indicated that sexual minorities were more influenced by the presence of a greater number of smokers than heterosexuals (Fig. 1). Among heterosexual participants, being in a vehicle (aOR = 0.67, 95%CI = 0.46–0.98) or inactive/at leisure (aOR = 0.78, 95%CI = 0.62–0.98) reduced the odds of smoking.
Table 3:
External predictors of smoking situations by sexual identity groups
| Predictors | Heterosexual group | Sexual minority group | Group interaction |
||||
|---|---|---|---|---|---|---|---|
| NS-Sit n=2434 (63%) |
S-Sit n=1428 (37%) |
aOR (95%CI) | NS-sit n=1698 (64%) |
S-Sit n=938 (36%) |
aOR (95%CI) | aOR (95%CI) | |
| Smoking ban (%) | 65.04 | 47.34 | 0.51***(0.41–0.65) | 56.65 | 30.28 | 0.35***(0.27–0.47) | 0.74 (0.52–1.05) |
| Location type (%) | |||||||
| Home | 49.01 | 52.24 | 1.19 (0.95–1.50) | 43.58 | 40.30 | 0.93 (0.69–1.25) | 0.83 (0.57–1.20) |
| Work | 18.82 | 15.06 | 0.92 (0.69–1.22) | 19.85 | 14.29 | 1.08 (0.80–1.47) | 1.12 (0.75–1.69) |
| Vehicle | 8.09 | 6.58 | 0.67*(0.46–0.98) | 8.78 | 12.15 | 0.88 (0.59–1.31) | 1.35 (0.78–2.33) |
| Other’s home | 8.18 | 7.84 | 0.99 (0.72–1.35) | 12.01 | 13.11 | 0.82 (0.59–1.15) | 0.85 (0.54–1.33) |
| Bar | 2.01 | 2.73 | 1.53 (0.95–2.47) | 2.47 | 4.16 | 1.75*(1.06–2.90) | 1.09 (0.55–2.17) |
| Restaurant | 3.99 | 3.22 | 0.71 (0.44–1.16) | 3.36 | 3.84 | 1.45 (0.86–2.44) | 1.91 (0.94–3.89) |
| Other place | 9.70 | 12.18 | 1.09 (0.80–1.48) | 9.89 | 12.15 | 0.89 (0.60–1.31) | 0.80 (0.48–1.31) |
| Location (%) | |||||||
| Inside | 80.40 | 59.24 | 1.00 | 78.56 | 57.89 | 1.00 | |
| Outside | 11.30 | 34.10 | 2.96***(2.21–3.98) | 12.66 | 29.96 | 2.02***(1.42–2.87) | 0.87 (0.57–1.31) |
| Activity (%) | |||||||
| Working | 31.35 | 26.68 | 1.04 (0.81–1.33) | 32.33 | 26.55 | 0.92 (0.70–1.21) | 0.86 (0.59–1.23) |
| Inactive/leisure | 41.50 | 34.59 | 0.78*(0.62–0.98) | 38.34 | 39.66 | 0.95 (0.73–1.23) | 1.25 (0.89–1.76) |
| Interacting with others | 11.13 | 11.90 | 1.24 (0.96–1.60) | 11.31 | 12.79 | 1.11 (0.83–1.49) | 0.91 (0.62–1.33) |
| Eating/drinking | 14.67 | 20.59 | 1.14 (0.88–1.48) | 14.55 | 14.93 | 1.32 (0.97–1.78) | 1.12 (0.75–1.67) |
| Between activities | 15.86 | 22.06 | 1.16 (0.87–1.55) | 19.55 | 25.59 | 1.18 (0.86–1.61) | 1.03 (0.67–1.58) |
| Other activity | 4.81 | 4.62 | 0.78 (0.46–1.30) | 6.18 | 5.86 | 0.59 (0.35–1.01) | 0.78 (0.37–1.64) |
| Food (%) | |||||||
| Food | 11.13 | 15.06 | 1.00 (0.74–1.35) | 10.72 | 9.81 | 1.36 (0.95–1.94) | 1.33 (0.83–2.12) |
| Caffeinated drink | 3.12 | 4.06 | 0.97 (0.56–1.67) | 3.36 | 3.94 | 1.95 (0.98–3.89) | 2.05 (0.85–4.96) |
| Non-caffeinated drink | 4.11 | 5.32 | 0.84 (0.52–1.36) | 3.53 | 3.73 | 1.68 (0.99–2.84) | 1.94 (0.95–3.97) |
| Alcohol | 3.66 | 5.81 | 1.28 (0.88–1.86) | 4.12 | 4.90 | 1.10 (0.69–1.75) | 0.84 (0.46–1.51) |
| Presence of other smokers (%) | 6.33 | 13.66 | 2.60***(1.99–3.40) | 6.36 | 13.86 | 2.03***(1.50–2.75) | 0.88 (0.60–1.30) |
| Number of other smokers, mean (sd) | 0.22 (1.35) | 0.32 (1.37) | 1.03 (0.98–1.07) | 0.15 (0.95) | 0.36 (1.57) | 1.12** (1.04–1.20) | 1.10* (1.01–1.20) |
| Type of other smokers (%) | |||||||
| Unknown person | 0.82 | 1.26 | 0.70 (0.36–1.37) | 1.18 | 1.60 | 0.83 (0.41–1.66) | 1.03 (0.41–2.58) |
| Family member | 0.45 | 1.26 | 1.22 (0.56–2.67) | 0.35 | 0.11 | 0.13*(0.02–0.85) | 0.11* (0.01–0.82) |
| Friends | 4.44 | 8.75 | 0.91 (0.58–1.44) | 3.30 | 8.85 | 1.18 (0.70–2.00) | 1.03 (0.64–1.67) |
| Acquaintances | 0.58 | 1.33 | 1.17 (0.57–2.40) | 0.65 | 0.75 | 0.42 (0.16–1.08) | 0.38 (0.12–1.20) |
| Coworkers | 0.86 | 1.68 | 0.67 (0.33–1.39) | 0.77 | 1.39 | 0.99 (0.42–2.31) | 1.22 (0.42–3.55) |
| Partner | 1.11 | 2.10 | 0.72 (0.40–1.29) | 1.00 | 2.45 | 1.24 (0.61–2.48) | 1.44 (0.61–3.37) |
| Presence of any trigger (%) | 24.98 | 40.83 | 2.03***(1.56–2.63) | 31.39 | 47.76 | 2.06***(1.54–2.75) | 1.00 (0.70–1.42) |
| Type of trigger (%) | |||||||
| Tobacco products | 14.71 | 23.25 | 1.48**(1.12–1.97) | 19.14 | 30.38 | 1.99***(1.44–2.76) | 1.24 (0.83–1.84) |
| Tobacco pack | 12.86 | 20.52 | 1.50*(1.09–2.05) | 13.90 | 25.59 | 1.93***(1.36–2.72) | 1.24 (0.79–1.93) |
| Lighter/matches | 15.69 | 22.97 | 1.40*(1.05–1.86) | 21.91 | 32.30 | 2.01***(1.48–2.74) | 1.38 (0.92–2.06) |
| Ashtray | 7.64 | 9.31 | 0.91 (0.62–1.36) | 11.25 | 14.61 | 1.02 (0.70–1.47) | 1.14 (0.68–1.91) |
| Media | 0.94 | 1.40 | 0.47 (0.15–1.48) | 1.30 | 1.92 | 1.58 (0.53–4.70) | 3.24 (0.66–15.75) |
| Advertisement | 0.74 | 0.63 | 1.04 (0.30–3.64) | 1.65 | 0.32 | 0.66 (0.19–2.30) | 0.59 (0.10–3.46) |
| Other | 1.85 | 3.08 | 0.85 (0.46–1.57) | 2.77 | 4.16 | 0.99 (0.51–1.95) | 1.19 (0.48–2.96) |
Note: p<0.05;
p<0.01;
p<0.001;
NS-Sit: Non-smoking situations; S-Sit: Smoking situations; aOR: adjusted odds ratio; CI: Confidence interval.
4. Discussion
This study is among the first to examine real-time predictors of smoking among sexual minority young adults. Sexual minority and heterosexual smokers in our sample shared several common situational predictors of smoking, including experiencing nicotine craving, being in areas without a smoking ban, the presence of other smokers, being at an outside location, and seeing triggers (e.g., cigarette packs or lighters). However, sexual minority participants exhibited unique predictors that increased their likelihood of smoking, including being at a bar and the number of other smokers present, while the presence of a smoking family member reduced their chance of smoking. Craving seemed to be a less important driver of smoking among sexual minorities compared to heterosexuals. Conversely, the number of other smokers was more strongly associated with smoking among sexual minority than heterosexual participants. Collectively, these findings suggest that smoking among sexual minority young adults may be especially influenced by external situational factors.
In our study, being at a bar was a stronger predictor of smoking for sexual minority participants than for heterosexual participants. This is consistent with previous findings that frequency of bar attendance increases the odds of smoking among sexual minority populations (Holloway et al., 2012; Matthews et al., 2011). For many sexual minority people, young adulthood is a time of seeking a sense of identity, community, and belonging after growing up in predominantly heteronormative social contexts (e.g., a heterosexual nuclear family). Coming of age often involves experiences in spaces that are safer for non-heterosexual individuals (e.g., gay and lesbian bars) where young people can find liberation and support for their identity while also encountering a range of risk behaviors, including smoking (Valentine, 2003). Tobacco use may be more normative in gay and lesbian bars than in straight bars, and all bar settings contain a variety of contextual smoking stimuli such as alcohol consumption, other smokers, and targeted tobacco marketing (Blosnich et al., 2013). Therefore, sexual minorities may be exposed to more frequent triggers as well as a higher burden of second-hand tobacco smoke in bar environments. Our data suggest that, in addition to comprehensive indoor and outdoor smoke-free policies in bars and nightclubs, interventions to change smoking norms in nightlife venues may be particularly relevant to addressing smoking among sexual minority young adults (Fallin et al., 2015).
While the presence of other smokers was a strong predictor for both groups, the number of smokers appeared more relevant to sexual minorities than for heterosexuals. To our knowledge, the present study is among the first to examine the impact of the number of other smokers on smoking behavior, and we found a positive association for sexual minorities. This finding may be partly due to the fact that sexual minority young adults may have a greater desire to experience social belonging due to past experiences of social rejection (Meyer, 2003), making them more willing to engage in social practices like smoking in order to facilitate social interaction and form bonds (Remafedi, 2007). Therefore, when in the presence of more smokers, sexual minorities may be more likely to smoke in order to fit in with the group. Another potential explanation for this finding may be the kind of social relationships that a smoker has with others who are smoking around them, which may differ between sexual minorities and non-minorities. Previous EMA studies have reported a strong influence of the particular types of relationships of smokers (e.g., friends) on participants’ smoking behavior (Cerrada et al., 2016a,b; Thrul et al., 2014). In the current study, we collected only the total number of other smokers present and separately asked about whether any of the other smokers were friends, partners, family members, etc. Therefore, we could not quantify the number of other smokers present who were a friend, family member, and so forth. We did find that sexual minority participants were less likely to smoke while in the presence of smoking family members compared to heterosexual participants. It should be noted that family members were reported in only small numbers of smoking situations for sexual minorities (0.11%) and heterosexuals (1.26%). This finding is aligned with an EMA study among Korean American emerging adult smokers which found that smoking was more likely to occur in the absence of family members (Cerrada et al., 2016a,b). Given that the relationship of a smoker to smoking people in their surroundings appears to differently influence their likelihood of smoking, future studies among sexual minorities should further investigate the impact of not only the number of other smokers present but also quantify the different types of relationships with other smoking people present at the time of smoking (e.g., how many smoking friends or smoking family members are present).
As anticipated, we found smoking was strongly associated with craving for both groups. Craving is a well-documented predictor of smoking (Cronk and Piasecki, 2010; Serre et al., 2015; Shiffman et al., 2002; Shiffman and Paty, 2006; Shiftman et al., 2004; Thrul et al., 2014). However, our findings add more nuance to understanding this relationship. We examined craving on a continuous scale of intensity rather than a dichotomized variable and showed a positive dose-response relationship between the craving intensity and the likelihood of smoking. Notably, this association was less robust for sexual minorities than for heterosexual smokers. This finding may, in part, be due to a higher proportion of females in the sexual minority group, as previous research suggested that women’s smoking is more influenced by external stimuli and less motivated by nicotine-reinforcement (Perkins, 1996). Since our sample was mostly bisexual, more evidence is needed to confirm this difference between sexual minority and heterosexual smokers.
In this study, we examined the relationship between smoking and mood, including affect and arousal, and did not find any situational associations for either sexual identity group. This finding suggests that sexual minorities’ smoking behavior in real-world contexts is more driven by external stimuli than by mood. This may be surprising given the proposed link between experiences of stigma, prejudice, and discrimination and the high prevalence of mental disorders among sexual minority individuals, which may in turn contribute to high smoking rates in this population as in the Minority Stress Model (Meyer, 2003). Nevertheless, evidence on the linkage between mood and smoking is mixed. Several theoretical and empirical studies suggested that arousal and affect are major motives for smoking in the general population and that people smoke to control negative affect or to diminish stress (Shiffman, 2009). A recent EMA study also reported a positive association between discrimination and nicotine use among sexual minority adults (Livingston et al., 2017), which provides further support for the Minority Stress Model. Conversely, ours and other studies (Carter et al., 2008; Shiffman et al., 2002; Shiftman et al., 2004) have not found a link between psychological distress and smoking. Given contradictory findings regarding the role of psychological factors in the general population and little evidence on this association among sexual minority populations, more research is needed to elucidate the underlying mechanisms of mood and smoking, particularly within this vulnerable population.
Taken together, our findings have important implications for developing cessation interventions for sexual minority young adult smokers. Smoke-free bar policies and bar-based interventions to change tobacco use norms may reduce the impact of two of the most important factors associated with smoking in this population: bar attendance and the presence of other smokers. In 1998, California was the first state to implement an indoor smoking ban in all enclosed workplaces, including bars (Labor Code section 6404.5). Since outside locations were strongly associated with smoking among participants in our study, we suggest that smoking bans at bars should include outdoor areas like patios. Comprehensive smoke-free bar policies would also address the disproportionately high rates of secondhand smoke exposure in bars (Fallin et al., 2014) as well as promote smoking cessation (Wintemberg et al., 2017) among sexual minority young adults. As of March 2018, there are only 101 municipalities in California that restrict smoking in all outdoor dining areas of bars and restaurants, and Alameda and San Francisco counties do not have this restriction (The Center for Tobacco Control Policy and Organizing, 2018). In addition, for all participants, triggers such as tobacco products or lighters/matches were a significant proximal cue for smoking behavior (Conklin et al., 2008). Therefore, anti-tobacco interventions that take place in bars and other social environments as well as mobile health cessation interventions (e.g., just-in-time adaptive interventions) for both groups may be needed to counteract these triggers. To date, there have been a few cessation interventions targeting sexual minority smoking (Berger and Mooney-Somers, 2017; Eliason et al., 2012; Fallin et al., 2015; Matthews et al., 2013). Among those, bar and nightclub interventions have been associated with a reduction in smoking among sexual minority young adults (Fallin et al., 2015).
The strengths of our study include application of EMA to capture real-time predictors of smoking among young adult sexual minority smokers, minimizing recall bias and providing a nuanced understanding of smoking antecedents that are difficult to capture using other data collection methods (Shiffman, 2009). One limitation of our study is its reliance on self-reported data, which may be subject to social desirability bias. Second, the generalizability of our results may be limited due to online recruitment of participants in the San Francisco Bay Area, which may differ from other geographic locations with higher stigma associated with non-heterosexual orientation, higher smoking rates, or fewer smoking restrictions. Third, in order to limit participant response burden with EMA surveys, we did not collect data on minority stress experiences (e.g., perceived discrimination, other stressors). Finally, since three quarters of sexual minority smokers in our sample selfidentified as bisexual, our findings may be more representative of the unique experiences of this sexual minority subgroup. Tobacco use disparities may vary by distinct sexual minority identities (e.g., gay, lesbian) or different gender identities (e.g., transgender) (Callis, 2013; Hoffman et al., 2018; Schuler et al., 2018). Further research is warranted to better understand smoking antecedents among distinct sexual and gender identities.
5. Conclusions
Our study provides new empirical evidence on real-time predictors of smoking for sexual minority young adult smokers. In contrast to heterosexuals, sexual minority young adult smoking seems to be driven more by external situational factors, highlighting the importance of addressing social context to decrease tobacco use disparities in this group. Comprehensive smoke-free bar policies and bar-based anti-tobacco interventions may be particularly promising strategies for sexual minority young adult smokers.
Acknowledgments
Role of the funding source
This study was supported by the National Cancer Institute (T32 CA113710; U01 CA154240) and the California Tobacco-Related Disease Research Program (TRDRP 25FT-0009).
Footnotes
Conflict of interest
DR has consulted to Carrot, Inc., which makes a tobacco cessation device.
References
- Baskerville NB, Dash D, Shuh A, Wong K, Abramowicz A, Yessis J, Kennedy RD, 2017. Tobacco use cessation interventions for lesbian, gay, bisexual, transgender and queer youth and young adults: a scoping review. Prev. Med. Rep. 6, 53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger I, Mooney-Somers J, 2017. Smoking cessation programs for lesbian, gay, bisexual, transgender, and intersex people: a content-based systematic review. Nicotine Tob. Res. 19, 1408–1417. [DOI] [PubMed] [Google Scholar]
- Best JA, Hakstian AR, 1978. A situation-specific model for smoking behavior. Addict. Behav. 3, 79–92. [DOI] [PubMed] [Google Scholar]
- Blosnich J, Lee JG, Horn K, 2013. A systematic review of the aetiology of tobacco disparities for sexual minorities. Tob. Control 22, 66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhalter JE, 2015. Smoking in the LGBT community In: Boehmer U, Elk R (Eds.), Cancer and the LGBT Community. Springer, Cham. [Google Scholar]
- Caceres BA, Brody A, Luscombe RE, Primiano JE, Marusca P, Sitts EM, Chyun D, 2017. A systematic review of cardiovascular disease in sexual minorities. Am. J. Public Health 107, e13–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callis AS, 2013. The black sheep of the pink flock: labels, stigma, and bisexual identity. J. Bisex. 13, 82–105. [Google Scholar]
- Callis AS, 2014. Bisexual, pansexual, queer: non-binary identities and the sexual borderlands. Sexualities 17, 63–80. [Google Scholar]
- Carter BL, Lam CY, Robinson JD, Paris MM, Waters AJ, Wetter DW, Cinciripini PM, 2008. Real-time craving and mood assessments before and after smoking. Nicotine Tob. Res. 10, 1165–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerrada CJ, Unger JB, Huh J, 2016a. Correlates of perceived smoking prevalence among Korean American emerging adults. J. Immigr. Minor. Health 18, 1183–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerrada CJ, Ra CK, Shin HS, Dzubur E, Huh J, 2016b. Using ecological momentary assessment to identify common smoking situations among Korean American emerging adults. Prev. Sci. 17, 892–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conklin CA, Robin N, Perkins KA, Salkeld RP, McClernon FJ, 2008. Proximal versus distal cues to smoke: the effects of environments on smokers’ cue-reactivity. Exp. Clin. Psychopharmacol. 16, 207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copen CE, Chandra A, Febo-Vazquez I, 2016. Sexual behavior, sexual attraction, and sexual orientation among adults aged 18–44 in the United States: data from the 2011–2013 National Survey of Family Growth. Natl. Health Stat. Rep. 1–14. [PubMed] [Google Scholar]
- Corliss HL, Wadler BM, Jun HJ, Rosario M, Wypij D, Frazier AL, Austin SB, 2013. Sexual-orientation disparities in cigarette smoking in a longitudinal cohort study of adolescents. Nicotine Tob. Res. 15, 213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronk NJ, Piasecki TM, 2010. Contextual and subjective antecedents of smoking in a college student sample. Nicotine Tob. Res. 12, 997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliason MJ, Dibble SL, Gordon R, Soliz GB, 2012. The last drag: an evaluation of an LGBT-specific smoking intervention. J. Homosex. 59, 864–878. [DOI] [PubMed] [Google Scholar]
- Emory K, Kim Y, Buchting F, Vera L, Huang J, Emery SL, 2016. Intragroup variance in lesbian, gay, and bisexual tobacco use behaviors: evidence that subgroups matter, notably bisexual women. Nicotine Tob. Res. 18, 1494–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallin A, Neilands TB, Jordan JW, Ling PM, 2014. Secondhand smoke exposure among young adult sexual minority bar and nightclub patrons. Am. J. Public Health 104, e148–e153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallin A, Neilands TB, Jordan JW, Ling PM, 2015. Social branding to decrease lesbian, gay, bisexual, and transgender young adult smoking. Nicotine Tob. Res. 17, 983–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson SG, Frandsen M, Dunbar MS, Shiffman S, 2015. Gender and stimulus control of smoking behavior. Nicotine Tob. Res. 17, 431–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman L, Delahanty J, Johnson SE, Zhao X, 2018. Sexual and gender minority cigarette smoking disparities: an analysis of 2016 behavioral risk factor surveillance system data. Prev. Med. 113, 109–115. [DOI] [PubMed] [Google Scholar]
- Holloway IW, Traube DE, Rice E, Schrager SM, Palinkas LA, Richardson J, Kipke MD, 2012. Community and individual factors associated with cigarette smoking among young men who have sex with men. J. Res. Adolesc. 22, 199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes LM, Ling PM, 2017. Workplace secondhand smoke exposure: a lingering hazard for young adults in California. Tob. Control 26, e79–e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SE, Holder-Hayes E, Tessman GK, King BA, Alexander T, Zhao X, 2016. Tobacco product use among sexual minority adults: findings from the 2012–2013 National Adult Tobacco Survey. Am. J. Prev. Med. 50, e91–e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston NA, Flentje A, Heck NC, Szalda-Petree A, Cochran BN, 2017. Ecological momentary assessment of daily discrimination experiences and nicotine, alcohol, and drug use among sexual and gender minority individuals. J. Consult. Clin. Psychol. 85, 1131–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews AK, Hotton A, DuBois S, Fingerhut D, Kuhns LM, 2011. Demographic, psychosocial, and contextual correlates of tobacco use in sexual minority women. Res. Nurs. Health 34, 141–152. [DOI] [PubMed] [Google Scholar]
- Matthews AK, Li CC, Kuhns LM, Tasker TB, Cesario JA, 2013. Results from a community-based smoking cessation treatment program for LGBT smokers. J. Environ. Public Health [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Matthews AK, Lee JGL, Veliz P, Hughes TL, Boyd CJ, 2018. Tobacco use and sexual orientation in a national cross-sectional study: age, race/ ethnicity, and sexual identity-attraction differences. Am. J. Prev. Med. 54, 736–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuoid J, Thrul J, Ling P, 2018. A geographically explicit ecological momentary assessment (GEMA) mixed method for understanding substance use. Soc. Sci. Med. 202, 89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, 2003. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol. Bull. 129, 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA, 1996. Sex differences in nicotine versus nonnicotine reinforcement as determinants of tobacco smoking. Exp. Clin. Psychopharmacol. 4, 166–177. [Google Scholar]
- Remafedi G, 2007. Lesbian, gay, bisexual, and transgender youths: who smokes, and why? Nicotine Tob. Res. 9, S65–71. [DOI] [PubMed] [Google Scholar]
- Russell MAH, Peto J, Patel UA, 1974. The classification of smoking by factorial structure of motives. J. R. Stat. Soc. 137, 313–346. [Google Scholar]
- Russell JA, Weiss A, Mendelsohn GA, 1989. Affect grid—a single-item scale of pleasure and arousal. J. Pers. Soc. Psychol. 57, 493–502. [Google Scholar]
- Schuler MS, Rice CE, Evans-Polce RJ, Collins RL, 2018. Disparities in substance use behaviors and disorders among adult sexual minorities by age, gender, and sexual identity. Drug Alcohol Depend. 189, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serre F, Fatseas M, Swendsen J, Auriacombe M, 2015. Ecological momentary assessment in the investigation of craving and substance use in daily life: a systematic review. Drug Alcohol Depend. 148, 1–20. [DOI] [PubMed] [Google Scholar]
- Shiffman S, 2009. Ecological momentary assessment (EMA) in studies of substance use. Psychol. Assess. 21, 486–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, 2014. Conceptualizing analyses of ecological momentary assessment data. Nicotine Tob. Res. 16, S76–S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Paty J, 2006. Smoking patterns and dependence: contrasting chippers and heavy smokers. J. Abnorm. Psychol. 115, 509–523. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Gwaltney CJ, Balabanis MH, Liu KS, Paty JA, Kassel JD, Hickcox M, Gnys M, 2002. Immediate antecedents of cigarette smoking: an analysis from ecological momentary assessment. J. Abnorm. Psychol. 111, 531–545. [DOI] [PubMed] [Google Scholar]
- Shiftman S, Paty JA, Gwaltney CJ, Dang Q, 2004. Immediate antecedents of cigarette smoking: an analysis of unrestricted smoking patterns. J. Abnorm. Psychol. 113, 166–171. [DOI] [PubMed] [Google Scholar]
- StataCorp, 2017. Stata Statistical Software: Release 15. StataCorp LP, College Station, TX. [Google Scholar]
- Stone AA, Shiftman S, 2002. Capturing momentary, self-report data: a proposal for reporting guidelines. Ann. Behav. Med. 24, 236–243. [DOI] [PubMed] [Google Scholar]
- The Center for Tobacco Control Policy and Organizing, 2018. List of Municipalities That Restrict Smoking in Outdoor Dining Areas. The Center for Tobacco Control Policy and Organizing, Sacramento. [Google Scholar]
- Thrul J, Kuntsche E, 2015. The impact of friends on young adults’ drinking over the course of the evening—an event-level analysis. Addiction 110, 619–626. [DOI] [PubMed] [Google Scholar]
- Thrul J, Buhler A, Ferguson SG, 2014. Situational and mood factors associated with smoking in young adult light and heavy smokers. Drug Alcohol Rev. 33, 420–427. [DOI] [PubMed] [Google Scholar]
- Thrul J, Labhart F, Kuntsche E, 2017. Drinking with mixed-gender groups is associated with heavy weekend drinking among young adults. Addiction 112, 432–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinh MH, Agenor M, Austin SB, Jackson CL, 2017. Health and healthcare disparities among U.S. women and men at the intersection of sexual orientation and race/ethnicity: a nationally representative cross-sectional study. BMC Public Health 17, 964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine GST, 2003. Finding oneself, losing oneself: the lesbian and gay ‘scene’ as a paradoxical space. Int. J. Urban Reg. Res. 27, 849–866. [Google Scholar]
- Watson RJ, Lewis NM, Fish JN, Goodenow C, 2018. Sexual minority youth continue to smoke cigarettes earlier and more often than heterosexuals: findings from population-based data. Drug Alcohol Depend. 184, 64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wintemberg J, McElroy JA, Ge B, Everett KD, 2017. Can smoke-free policies reduce tobacco use disparities of sexual and gender minorities in Missouri? Nicotine Tob. Res. 19, 1308–1314. [DOI] [PubMed] [Google Scholar]
- Zeger SL, Liang KY, Albert PS, 1988. Models for longitudinal data: a generalized estimating equation approach. Biometrics 44, 1049–1060. [PubMed] [Google Scholar]


