Abstract
Background:
Partner notification services (PNS) remain the backbone of syphilis control. The popularity of internet-based apps to meet sex partners among early syphilis (ES) patients may hinder the success of PNS if partners cannot be located.
Methods:
We compared demographic and clinical characteristics between male ES patients indicating sex with men (MSM) and reported in North Carolina between 2013 and 2016 by reported use of an internet-based app to meet sex partners (app user). We used multivariable log-binomial regression to assess the association between app usage and ES exposure notification of ≥1 sex partner.
Results:
Among 3,414 MSM ES patients, 58.6% were app users. App users were more frequently white (33.2% vs. 27.3%; p=0.003), younger (median: 28 vs. 30 years; p=0.0002) and less frequently HIV co-infected (54.1% vs. 58.2%; p=0.02) compared to non-app users. Overall, 94.9% of app users and 89.6% of non-app users reported ≥1 sex partner. App users reported 2.5-times more locatable and 2.7-times more unlocatable sex partners than non-app users. Similar proportions of app (23.6%) and non-app users (25.0%) reported only unlocatable partners (p=0.4). App usage was not associated with ES exposure notification of ≥1 sex partner (adjusted risk ratio: 0.99; 95% confidence interval: 0.87–1.13).
Conclusion:
We observed no difference in the proportion of locatable partners or the likelihood of notifying ≥1 sex partner of exposure among MSM ES patients, by reported use of apps to meet sex partners. PNS continues to be an important mechanism to locate and assure treatment for sex partners in this population.
Keywords: syphilis, internet-based app, partner notification
Summary:
Among men who have sex with men diagnosed with early syphilis, the probability of notifying ≥1 sex partner did not differ by reported internet-based app use to meet sex partners.
Introduction
Case reports of syphilis have been increasing in the United States (US) since 2013, with 2016 primary and secondary (i.e. infectious) syphilis case rates at their highest since 1993.(1) In 2016, North Carolina (NC) had the 8th highest infectious syphilis incidence rate in the US. As seen nationally, the majority of syphilis cases in NC are among men (86%), specifically men who have sex men (MSM). (1) (2)
Partner notification services (PNS) remains the backbone of syphilis prevention and control in NC. The goal of PNS is to interrupt disease transmission by notifying sex partners of confirmed cases, providing risk reduction counseling, and referral to testing and treatment for both cases and their sex partners. NC public health law requires the Division of Public Health (NC DPH) to provide PNS for all individuals newly diagnosed with early syphilis (ES)-clinical or serologic evidence of having acquired the infection in the preceding 12 months. Public health officials responsible for performing PNS, Disease Intervention Specialists (DIS), collect the names and locating information of all sex partners at risk of syphilis infections from the index case.(3) Between 2013 and 2016, NC DIS located and interviewed 94% of all ES index cases.(4)
Despite locating and interviewing ES cases, the continued increase in NC’s syphilis morbidity suggests infected partners of index cases are not being identified or treated before disease transmission. The success of a PNS program depends on the index case’s willingness or ability to provide sufficient locating information for DIS to rapidly locate and treat their sex partners to prevent onward disease transmission. The increasing popularity of internet-based applications (apps) to find sex partners, particularly among MSM (5) can facilitate sex partner finding that does not require identification beyond a screenname, making the subsequent location of those partners difficult.(6) (7) (8) (9) Additionally, frequent changes in screen names or apps used to meet partners and governmental restrictions on DIS access to these apps may present barriers for successful PNS. Because data are needed to support programmatic and policy change, we performed a retrospective review of the surveillance data for all MSM ES cases reported in NC to assess the association between PNS outcomes and reported use of internet-based apps to meet sex partners. Widely-used PNS outcome indices were used to assure comparability of our observations to PNS assessments performed in other jurisdictions.
Methods
DATA:
Surveillance data for syphilis are collected in the North Carolina Electronic Disease Surveillance System (NC EDSS). This system also contains DIS case investigative notes for primary, secondary and early latent syphilis index patients and their reported sex partners. We restricted our analysis to all ES MSM and their sex partners, reported to the NC DPH between January 1, 2013 and December 31, 2016. All patients not known to have late syphilis are assigned to DIS and prioritized for PNS. We classified male patients that self-reported being homosexual, bisexual or reported a male sex partner during their infectious period as MSM.
CASE INVESTIGATION:
During interviews with index patients, DIS elicit information about clinical manifestations of infection, sexual risk behaviors, the names and locating information of all sex partners during the patient’s infectious period (primary=3 months; secondary=6 months; early latent=12 months). Only sex partners reported by the index patient during their infectious window were included in our analysis.
As part of their investigation, DIS ask all index patients whether they met sex partners on an internet-based app in the 12 months preceding their syphilis diagnosis. If an index patient answers yes to this question, DIS ask for the absolute number of both named and unnamed sex partners met on internet-based apps during the patient’s infectious period (internet sex partner). However, we do not know which specific partners were met online. We classified index patients who reported and did not report meeting ≥1 sex partner via an internet-based app in the 12 months preceding their syphilis diagnosis as app users and non-app users, respectively. Patients who did not answer the internet-based app use question were excluded from our analysis. Because the infectious period for primary and secondary syphilis is shorter than the time period used to assign app user exposure (12 months), we estimated potential misclassification bias by calculating the proportion of patients who did not report ≥1 internet sex partner during their infectious period.
Reported sex partners were stratified into 2 groups: named partners (index case provided enough locating information for the DIS to attempt location); and unnamed partners (index case did not provide enough locating information for the DIS to attempt location). Traditionally, a DIS needs at least one of the following pieces of locating information for the partner to initiate PNS: phone number, residential or employment address, or a social security number. Internet partner notification services (IPNS) refers to locating sex partners via internet-based platforms. Locating information needed to initiate IPNS include an e-mail address, social media username, or app screenname. Sex partners met both on- and off-line could be eligible for traditional PNS and/or IPNS; the method of partner notification is dependent only on the types of locating information provided by the index patient to the DIS. Because IPNS for all syphilis investigations are performed by a single individual in NC, sex partners are assigned for IPNS when traditional PNS attempts have failed or when only IPNS identifiers are available.
From NC EDSS, we extracted demographic, clinical, behavioral risk data, and syphilis treatment status information for ES index patients, notification of syphilis exposure, IPNS assignment, and syphilis testing and diagnosis status for named sex partners, and HIV status for both ES index patients and their named sex partners. We matched index patients and their named partners to the enhanced HIV/AIDS Reporting System (eHARS) to determine their HIV status. Index patients were considered to have prevalent HIV if the HIV diagnosis date was before or within 60 days after the syphilis diagnosis date. Named sex partners were considered to have prevalent HIV infection if the HIV diagnosis date was before the PNS initiation date. Sex partners were considered newly diagnosed with HIV if the HIV diagnosis date was on or within the 30 days after the PNS initiation date.
DATA ANALYSIS:
Descriptive and bivariate analyses (Kruskal-Wallis for continuous variables and Chi-squared tests for categorical variables) were used to compare demographic (race/ethnicity and age), clinical (syphilis stage, syphilis treatment and HIV status) and behavioral (prior STI history, frequency of condom use, sexual risk practices, and success in getting patients to name partners) characteristics between app and non-app users. A p-value <0.05 was considered statistically significant. We compared the following PNS outcomes between app and non-app users: partner notification index (number of named sex partners notified of their exposure per index patients interviewed), treatment index (number of named infected or exposed sex partners who received curative or empiric treatment for syphilis per index patients interviewed) and the case finding index (number of named sex partners newly diagnosed with syphilis or HIV infection per index patients interviewed).
Log binomial regression was used to estimate risk ratios (RR) and 95% confidence intervals (CI) to assess the association between app use and DIS notification of ≥1 sex partner of syphilis exposure and other index patient characteristics in univariate and multivariate models. A sensitivity analysis was performed to compare the probability of notifying all versus fewer than all named sex partners, by reported app use. Variables significantly associated with internet sex partner finding in bivariate analysis were included in the multivariate models. Data were analyzed using STATA/IC 11.2 software (College Station, TX).
Results
Index Cases
Between 2013 and 2016, 5,560 individuals were reported with ES to the NC DPH. Most were male (87.1%, N=4,840), of which 73.9% (N=3,576) were MSM. Reported use of internet-based apps to meet sex partners by MSM ES cases increased slightly throughout this analysis period (54.1% in 2013 to 59.3%; p=0.13). DIS staff interviewed 3,464 (96.7%) MSM ES patients, of which 3,414 (98.6%) answered the internet-based app use question; 1,999 (58.6%, app users) answered “Yes” and 1,415 (41.4%, non-app users) answered “No”. The remaining 50 (1.4%) interviewed index patients were excluded from this analysis (Figure 1). Excluded patients were more frequently older (median age 34 versus 29), reported no sex partners (22.0% versus 7.1%), had no PNS initiated sex partners (46.0% versus 27.2%) and less frequently reported a new sex partner during their infectious period (39.1% versus 69.1%; all p’s<0.05) compared those included.
Figure 1:
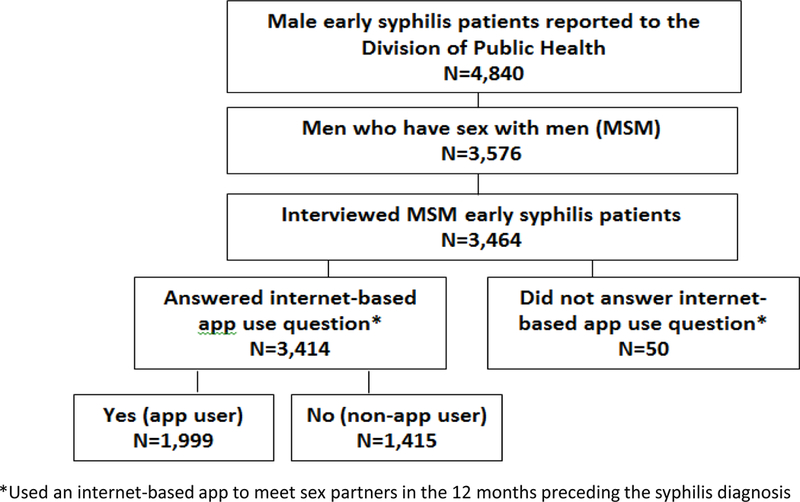
Selection of early syphilis patients included in analysis, North Carolina 2013–2016.
Among app users, 87.4% of P&S index patients reported meeting ≥1 internet sex partner during their infectious period. The most frequently reported apps used to meet sex partners were Adam4Adam (42.3%), Grindr (29.5%), Jack’d (20.7%), Facebook (9.5%) and Craigslist (5.5%). One-third (33.5%) of app users and 24.9% of non-app users also reported meeting sex partners in bars or clubs. We were unable to determine where 75.1% of non-app users met their sex partners.
App using index patients were more frequently non-Hispanic, white (33.2% versus 27.3%; p=0.003) and younger (median 28 versus 30 years; p=0.0002) than non-app users (Table 1). App users were less likely than non-app users to be HIV co-infected (54.1% versus 58.2%; p=0.02), to report a female sex partner (12.5% versus 15.5%; p=0.01) or always using a condom during sexual intercourse (9.8% versus 13.6%; p=0.002) and more likely to report a prior history of a STI (66.0% versus 62.2%; p=0.008). The syphilis stage and the proportion of index cases that received treatment were similar for app and non-app users.
Table 1.
Demographic, clinical characteristics and partner notification outcomes of male index patients diagnosed with early syphilis who reported sex with men (MSM) by reported using an internet-based app to meet sex partners (app user) and (non-app user), January 2013 through December 2016.
| MSM Early Syphilisa Index Patients | ||||
|---|---|---|---|---|
| Total MSM | App users | Non-app users | ||
| Characteristics | N (% or IQR)b | N (% or IQR)b | N (% or IQR)b | P value |
| Interviewed | 3,414 | 1,999 | 1,415 | |
| Race/Ethnicity | ||||
| White, non-Hispanic | 1,049 (30.7) | 663 (33.2) | 386 (27.3) | 0.003 |
| Black, non-Hispanic | 2,065 (60.5) | 1,172 (58.6) | 893 (63.1) | |
| Hispanic/Latino | 240 (7.0) | 132 (6.6) | 108 (7.6) | |
| Otherc | 60 (1.8) | 32 (1.6) | 28 (2.0) | |
| Median age | 29 (24, 38) | 28 (24, 38) | 30 (24, 40) | 0.0002 |
| Bisexuald | 470 (13.8) | 250 (12.5) | 220 (15.5) | 0.01 |
| Syphilis Stage | ||||
| Primary | 620 (18.2) | 374 (18.7) | 246 (17.4) | 0.47 |
| Secondary | 1,466 (42.9) | 862 (43.1) | 604 (42.7) | |
| Early Latent | 1,328 (38.9) | 763 (38.2) | 565 (39.9) | |
| HIV co-infectede | 1,904 (55.7) | 1,081 (54.1) | 823 (58.2) | 0.02 |
| History of prior STIf | 2,197 (64.5) | 1,318 (66.0) | 879 (62.2) | 0.008 |
| Reported Condom Use | ||||
| Always | 389 (11.4) | 196 (9.8) | 193 (13.6) | 0.002 |
| Never | 440 (12.9) | 245 (12.3) | 195 (13.8) | |
| Sometimes | 2,567 (75.2) | 1,547 (77.4) | 1,020 (72.1) | |
| Missing data | 18 (18) | 11 (0.55) | 7 (0.50) | |
| Treatment status | ||||
| Treatedg | 3,374 (98.8) | 1,977 (98.9) | 1,397 (98.7) | 0.6 |
| Treatment Unknown | 40 (1.2) | 22 (1.1) | 18 (1.3) | |
| No reported partnersh | 250 (7.3) | 103 (5.2) | 147 (10.4) | <0.001 |
| No initiated partnersi | 1,032 (30.2) | 554 (27.7) | 478 (33.8) | <0.001 |
| ≥ 1 new sex partnerj | 694 (67.2) | 445 (80.3) | 249 (52.1) | <0.001 |
| Partner notification Outcomes (PNS) | ||||
|
# Index patients with PNS initiated sex partners |
2,382 | 1,445 | 937 | |
| ≥1 partner notified | 1,960 (82.3) | 1,176 (81.4) | 784 (83.7) | 0.15 |
| # partners notifiedk | 3 (2, 6) | 4 (2, 7) | 2 (1, 3) | 0.0001 |
| Notification indexl | 1.29 | 1.57 | 0.90 | |
| ≥1 partner treated | 961 (40.3) | 594 (41.1) | 367 (39.2) | 0.11 |
| # partners treatedm | 3 (2, 6) | 4 (2, 6) | 2 (1, 3) | 0.0001 |
| Treatment indexn | 0.65 | 0.80 | 0.44 | |
| ≥1 new infection | 255 (7.5) | 140 (7.0) | 115 (8.1) | 0.04 |
| # partners newly diagnosedo | 2 (1, 4) | 3 (2, 5) | 2 (1, 2) | 0.0001 |
| Case finding indexp | 0.14 | 0.16 | 0.12 | |
Early syphilis includes primary, secondary and early latent syphilis stages
Total number (N), Percentage (%) or Interquartile range (IQR)
American Indian Alaskan Native, Asian, Native Hawaiian and Pacific Islander
Index case reported at least one female sexual partner during the infectious period
HIV diagnosis date before or within 60 days after the syphilis diagnosis date as determined through matching to the NC enhanced HIV/AIDS Reporting System (eHARS) database
Sexually Transmitted Infections (STIs) included gonorrhea, chlamydia, syphilis, HIV, viral hepatitis
Treated includes patients DIS brought for prophylactic or curative treatment of syphilis
Index patients who reported no sex partners during the infectious period
Proportion of index patients who reported only unnamed sex partner
Proportion of index patients with no initiated partners that reported having at least one new sex partner during the infectious period
median number of notified sex partners per index case interviewed
number of notified sex partners per index patient interviewed
median number of sex partners treated per index patient interviewed
number of sex partners that received curative or empiric syphilis treatment per index patient interviewed
median number of sex partners newly diagnosed with HIV or syphilis (within 30 days of PNS initiation)
number of sex partners newly diagnosed with HIV or syphilis infection per index patient interviewed.
App users were more likely than non-app users to report ≥1 sex partner during their infectious period (94.9% versus 89.6%; p<0.001) and less likely to have no sex partners initiated for PNS (27.7% versus 33.8%; p<0.001). Among index patients who reported ≥1 sex partner, a similar proportion of app and non-app users reported only unnamed partners (23.6% versus 25.0%; p=0.4). Among index patients with no initiated sex partners, app users were more likely than non-app users to report ≥1 new sex partner during their infectious period (80.3% versus 52.1%; p<0.001) (Table 1). These observations did not change when stratified by HIV serostatus (data not shown).
A similar proportion of app and non-app users with ≥1 initiated sex partner had ≥1 sex partner notified of their exposure (81.4% versus 83.7%) and brought to treatment (41.1% versus 39.2%; all p’s>0.10). A smaller proportion of app users had ≥1 sex partner newly diagnosed with syphilis or HIV infection (10.0% versus 13.0%; p=0.04). The median number of partners located (4 versus 2), treated for exposure or infection (4 versus 2) and newly diagnosed with syphilis or HIV infections (3 versus 2; all p’s=0.0001) were higher for app versus non-app users.
Partners
A total of 11,409 partners were reported by index patients; 8,242 (72%) by app users and 3,167 (28%) by non-app users. Nearly half of all partners reported in each group were unnamed and thus not initiated for PNS (app users: N=4,278; 51.9%; non-app users: N=1,568; 49.5%), (Table 2). Internet sex partners comprised 41.5% (N=3,241) of partners reported by app users; nearly half of whom (46.9%) had enough locating information to initiate PNS or IPNS.
Table 2.
Classification and number of reported sex partners and the testing outcomes for partners named by MSM index patients with early syphilis who reported (app user) and did not report (non-app user) meeting sex partners on an internet-based app, January 2013 through December 2016.
| Total Partners |
Partners of app users | Partners of non-app users | |||||
|---|---|---|---|---|---|---|---|
| Characteristics | N | (%)a | N | (%)a | N | (%)a | P value |
| Reported sex partnersb | 11,409 | 8,242 | 3,167 | ||||
| Unnamed | 5,846 | (51.2) | 4,278 | (52.0) | 1,568 | (49.5) | ref |
| Named | 5,563 | (48.8) | 3,964 | (48.0) | 1,599 | (50.5) | 0.0001 |
| Internet sex partnersc | 3,421 | (41.5) | |||||
| Unnamed | 1,815 | (53.1) | |||||
| Named | 1,606 | (46.9) | |||||
| Named Sex Partners | 5,563 | 3,964 | 1,599 | ||||
| # per index patientd | 1.63 | 1.98 | 1.13 | 0.0001 | |||
| Assigned for IPNSe | 613 | (11.0) | 460 | (11.6) | 153 | (9.6) | 0.03 |
| HIV Positivef | 1,842 | (33.1) | 1,295 | (32.7) | 547 | (34.2) | 0.37 |
| Syphilis testedg | 3,327 | (59.8) | 2,317 | (58.5) | 1,010 | (63.2) | 0.001 |
| New syphilis caseh | 435 | (13.1) | 278 | 157 | (15.5) | 0.005 | |
| HIV testedi | 1,331 | (37.9) | 942 | (37.3) | 389 | (39.6) | 0.66 |
| New HIV casej | 56 | (4.2) | 43 | (4.6) | 13 | (3.3) | 0.31 |
Total number (N) or Percentage (%)
Includes named (initiated for partner notification services (PNS) ) and unnamed (not initiated for PNS) sex partners
Subset of reported sex partners
Number of named sex partners per index patient interviewed
Internet Partner Notification Services (IPNS) –assigned to be located using sex partner’s e-mail address, social media screenname, or geospacial network app username
HIV diagnosis date on or before the PNS initiation date as determined through matching to the NC enhanced HIV/AIDS Reporting System (eHARS) database
Received serologic testing for syphilis infection as part of the DIS investigation
Newly diagnosed with syphilis as part of DIS investigation
Number of named partners without known prevalent HIV infection who were tested for HIV as part PNS
Number of named sex partners tested as part of PNS that were newly diagnosed with HIV infection (on or within 30 days of partner initiation date).
App users named more sex partners per index case interviewed than non-app users (1.98 versus 1.13; p=0.0001), (Table 2). Similar proportions of partners named by app and non-app users had appropriate HIV follow-up: either a record of prevalent HIV infection (32.7% versus 34.2%, respectively) or a record of HIV testing as part of the DIS investigation (37.3% versus 39.6%; p’s>0.10). A lower proportion of partners named by app users received serologic testing for syphilis exposure (58.5% versus 63.2%; p=0.001) or were newly diagnosed with syphilis (12.0% versus 15.5%; p=0.005). The proportion of partners tested for HIV that were newly diagnosed, did not differ if named by an app user or non-app user (4.6% versus 3.3%; p=0.31). Standard PNS outcomes were higher for app versus non-app users; partner notification index (1.57 versus 0.90), treatment index (0.80 versus 0.44) and case finding index (0.16 versus 0.12), (Table 1).
There were 613 (11.0%) named sex partners assigned for IPNS; 460 (11.6%) partners named by app users and 153 (9.6%) named by non-app users (p=0.03) (Table 2). DIS assured the evaluation and treatment of approximately 35% of partners named by app and non-app users assigned for IPNS. The inclusion of IPNS activities increased the overall proportion of named partners that DIS successfully brought to evaluation and treatment from 49.3% to 53.4% for app users and from 48.3% to 51.7% for non-app users.
Regression models
In total, 58.8% (N=1,176) app-users and 55.4% (N=784) non-app users named ≥1 partner notified by DIS of their exposure to syphilis. We observed no difference in the likelihood of the DIS being able to successfully notify ≥1 named partner of their exposure between app and non-app users in unadjusted (RR 0.99 95% CI 0.88–1.12) or adjusted (RR 0.99, 95% CI 0.87–1.13) log binomial regression models, (Table 3). In sensitivity analysis, the probability of notifying all versus fewer than all named partners did not differ between the two groups (data not shown).
Table 3:
Association between reported use of internet-based apps to meet sex partners and notification of at least one sex partner of syphilis exposure among male index patients with early syphilis who report sex with men (MSM), January 2013 through December 2016.
| Characteristics | Total Index patients |
Index patients with ≥1 partner notified (% or IQR)a |
Unadjusted Risk Ratio (95% CI) b |
Adjusted Risk Ratio (95% CI)b |
|---|---|---|---|---|
| 3,414 | 1,960 | |||
| Internet sex Partners | ||||
| No | 1,415 | 784 (55.4) | REF | REF |
| Yes | 1,999 | 1,176 (58.8) | 0.99 (0.88–1.12) | 0.99 (0.87–1.13) |
| Race/Ethnicity | ||||
| White | 1,049 | 624 (59.5) | REF | REF |
| Black | 2,065 | 1,168 (56.6) | 0.94 (0.82–1.07) | 0.95 (0.82–1.10) |
| Hispanic | 240 | 132 (55.0) | 0.92 (0.71–1.18) | 0.92 (0.71–1.19) |
| Otherc | 60 | 36 (60.0) | 1.00 (0.64–1.57) | 1.00 (0.64–1.57) |
| Age, median | 29 | 28 (23, 37) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) |
| Bisexuald | 470 | 271 (57.7) | 0.99 (0.83–1.17) | 0.99 (0.83–1.17) |
| HIV positivee | 1,904 | 998 (52.4) | 0.94 (0.83–1.06) | 0.94 (0.82–1.08) |
| Prior STDf | 2,200 | 1,218 (55.4) | 0.97 (0.86–1.10) | 1.02 (0.88–1.18) |
| New sex partnerg | 2,317 | 1,324 (57.1) | 0.97 (0.86–1.11) | 0.98 (0.85–1.12) |
| Condom use | ||||
| Always | 389 | 176 (45.2) | REF | REF |
| Never | 440 | 290 (65.9) | 1.08 (0.84–1.39) | 1.05 (0.82–1.36) |
| Sometimes | 2,567 | 1,481 (57.7) | 1.01 (0.82–1.24) | 1.00 (0.80–1.23) |
| Missing | 18 | 13 (72.2) | 1.23 (0.56–2.72) | 1.19 (0.53–2.64) |
Total number (N), Percentage (%) or Interquartile range (IQR)
Adjusted model includes all variables listed in table 3
American Indian Alaskan Native, Asian, Native Hawaiian and Pacific Islander
Index case reported at least one female sexual partner during the infectious period
HIV diagnosis date before or within 60 days after the syphilis diagnosis date as determined through matching to the NC enhanced HIV/AIDS Reporting System (eHARS) database
Sexually Transmitted Infections (STIs) included gonorrhea, chlamydia, syphilis, HIV, viral hepatitis
Proportion of index patients with ≥1 named sex partner that reported having at least one new sex partner during the infectious period.
Discussion
In this analysis of MSM ES patients, the probability of notifying at least one named partner did not differ by reported use of internet-based apps to meet sex partners. A similar proportion of both reported and named partners were located by DIS for app and non-app users, and nearly half of reported internet sex partners had enough contact information to initiate PNS or IPNS. Due to the larger number of partners named by app users, those investigations identified and treated more partners than investigations of non-app users. Additionally, app and non-app using index patients reported similar proportions of unnamed sex partners, suggesting internet-based app sex partner finding may not be the main or only factor limiting partner investigations for MSM index patients. Our analysis highlights the continued importance of PNS in locating and assuring the evaluation and treatment of named partners.
As observed previously (10) (11) (12) (13) (14), over half of MSM index patients reported using an internet-based app to meet sex partners and internet sex-seeking was correlated with larger numbers of reported sex partners per index patient. Although PNS was able to assure the evaluation and treatment of a similar percentage of named partners, app users still had almost three-times as many partners that were either not located (both named or unnamed) or refused evaluation and treatment compared to non-app users. Additionally, as reported in other studies (15) (14) (16), we observed a positive correlation between meeting sex partners on an internet-based app and reported STI risk factors such as a prior STD history, inconsistent condom use and engaging in sex during the syphilis infectious period. Elevated STI risk behaviors and numbers of reported partners among MSM who meet sex partners on internet-based apps suggest websites used to find sex partners may provide a venue for increased syphilis transmission, and therefore may have contributed to the increasing syphilis epidemic in NC over the course of this analysis.
It is surprising that non-app users reported similar proportions of unnamed sex partners as app users and were more likely to report no sex partners during their infectious period. This may be partly explained by experience with DIS during this and previous interviews. Non-app users were more frequently HIV-positive, which has been previously associated with a lower number of named sex partners and PNS indices among MSM syphilis patients.(10) Prior encounters with DIS at the time of HIV diagnosis may play a role in a patient’s subsequent willingness to cooperate with PNS efforts. Qualitative research is underway in NC to identify, understand and address the barriers MSM syphilis patients experience when reporting sex partners for PNS.
Incorporating IPNS with traditional PNS assured the evaluation and treatment of a similar proportion of partners named by app and non-app users, improving overall PNS outcomes for both groups. Our findings demonstrate the expanded benefit that IPNS could provide in reaching populations who routinely utilize internet-based platforms to communicate. Unfortunately, like many jurisdictions (17), and due to legal concerns in NC regarding the use of government-owned electronic devices to access websites and apps used by patients to meet sex partners, state-employed DIS staff cannot directly perform IPNS. Restricting IPNS activities to one contracted employee has also limited our ability to assess the value IPNS could have if it were an integrated part of all DIS investigations. In addition to enhancing disease intervention efforts, authorizing DIS to access these internet apps and websites for IPNS purposes would ensure DIS maintain cultural competency in the rapidly changing cyber landscape where MSM socialize and meet sex partners.
The routine capture of the number and classification of all sex partners reported during DIS interviews allowed us to assess the contribution of unnamed sex partners to NC’s syphilis epidemic. All index patient risk behavior and partner information obtained during DIS interviews was self-reported and therefore subject to recall or response bias. Limitations in data collection prohibited the identification of which sex partners were met online, therefore we cannot comment on differences in PNS outcomes by where partners were met. Some misclassification of app use exposure was possible among primary and secondary syphilis patients because the infectious period was shorter than the 12 month period used to assess internet sex partner finding. However, we believe this misclassification to be minimal because most of these patients reported at least one internet sex partner during their infectious period.
Given the high proportion of unnamed partners reported by index ES MSM patients, regardless of app usage, further study is necessary to understand how to provide PNS that is supportive of MSM culture and effective for notifying and treating partners. Though internet-based app use to find sex partners was associated with more overall sex partners, reported STI risk behaviors and infected partners, we observed no difference in the proportion of named partners notified of exposure. Our analysis highlights the continued usefulness of PNS for syphilis intervention and the potential benefit that routinizing IPNS into DIS investigations could have on syphilis partner notification outcomes for MSM regardless of app use to meet sex partners.
ACKNOWLEDGEMENTS
We thank all of the North Carolina Disease Intervention Specialists including our IPNS DIS, Steve Beagle, for their hard work and dedication to the health and safety of the patients they serve.
Funding: none
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Conflict of Interest: none
References
- 1.Centers for Disease Control and Prevention. 2016. Sexually Transmitted Diseases Surveillance Available at: https://www.cdc.gov/std/stats16/Syphilis.htm. Accessed September 13, 2017.
- 2.Health, North Carolina Department of Health and Human Services/ Division of Public. N.C. Communicable Disease Reports. North Carolina HIV/STD/Hepatitis Surveillance Report. 2016 Available at: http://epi.publichealth.nc.gov/cd/stds/figures.html. Accessed September 13, 2017.
- 3.North Carolina Administrative Code. 10A NCAC 41A.0204 Control Measures-Sexually Transmitted Diseases Available at: reports.oah.state.nc.us/ncac/title%2010a%20.../10a%20ncac%2041a%20.0204.pdf. Accessed September 13, 2017.
- 4.Field Services Unit Performance Report-Syphilis Index Cases Assigned/Interviewed 2013–2016. North Carolina Electronic Disease Surveillance System (database online). Report run September 1, 2017.
- 5.Grov C, Breslow AS, Newcomb ME, et al. Gay and bisexual men’s use of the Internet: research from the 1990s through 2013. J Sex Res 2014; 51(4): 390–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Q, Liu Y, Zhou Z, et al. Online sex-seeking behaviors among men who have sex with men: implications for investigation and intervention. AIDS Behav 2012; 16(6): 1690–8. [DOI] [PubMed] [Google Scholar]
- 7.Wang AL, Peng RR, Tucker JD, et al. Optimizing Partner Notification Programs for Men Who Have Sex with Men: Factorial Survey Results from South China. PLoS One 2016; 11(7): e0157749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan WS, Chen M, Ivan M, et al. Partner Notification Outcomes for Men Who Have Sex With Men Diagnosed With Syphilis Referred to Partner Notification Officers, Melbourne, Australia: Sex Transm Dis 2016; 43(11): 685–689. [DOI] [PubMed] [Google Scholar]
- 9.van Aar F, van Weert Y, Spijker R, et al. Partner notification among men who have sex with men and heterosexuals with STI/HIV: different outcomes and challenges. Int J STD AIDS 2015; 26(8): 565–73. [DOI] [PubMed] [Google Scholar]
- 10.DeSilva M, Hedberg K, Robinson B, et al. A case-control study evaluating the role of internet meet-up sites and mobile telephone applications in influencing a syphilis outbreak: Multnomah County, Oregon, USA 2014. Sex Transm Infect 2016; 92(5): 353–8. [DOI] [PubMed] [Google Scholar]
- 11.Rowlinson E, Goings S, Minnerly S, et al. Differences in Partner Services Outcomes for Men WHo Have Sex With Men Diagnosed With Primary and Secondary Syphilis by HIV Serostatus. SexTransm Dis 2018; Vol. 45(3): 152–157. [DOI] [PubMed] [Google Scholar]
- 12.Hochberg CH, Berringer K, Schneider J Next-Generation Methods for HIV Partner Services: A Systematic Review. Sex Transm Dis 2015; 42(9): 533–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klausner JD, Wolf W, Fischer-Ponce L, et al. Tracing a syphilis outbreak through cyberspace. JAMA 2000; 284(4): 447–9. [DOI] [PubMed] [Google Scholar]
- 14.Liau A, Millett G, Marks G. Meta-analytic Examination of Online Sex-Seeking and Sexual Risk Behavior Among Men Who Have Sex With Men. Sex Transm Dis 2006; 33(9): 576–584. [DOI] [PubMed] [Google Scholar]
- 15.Taylor M, Aynalem G, Bemis C, et al. Correlates of Internet use to meet sex partners among men who have sex with men diagnosed with early syphilis in Los Angeles County. Sex Transm Dis 2004; 31(9): 552–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zou H, Fan S. Characteristics of Men Who Have Sex With Men Who Use Smartphone Geosocial Networking Applications and Implications for HIV Interventions: A Systematic Review and Meta-Analysis. Arch Sex Behav 2016; 46(4): 885–894. [DOI] [PubMed] [Google Scholar]
- 17.Golden MR, Katz DA, Dombrowski JC. Modernizing Field Services for Human Immunodeficiency Virus and Sexually Transmitted Infections in the United States. Sex Transm Dis 2017; 44(10): 599–607. [DOI] [PMC free article] [PubMed] [Google Scholar]


