Abstract
Objectives:
Electronic medical record (EMR) is not only being welcomed by healthcare providers as a way to improve care delivery but also serves as a catalyst for development. The purpose of this study is to examine benefits of EMR and its ultimate contribution to development of healthcare delivery.
Design:
This is a qualitative, explorative, and descriptive study using survey questionnaires and a sample size of 50 at the Korle-Bu Teaching Hospital in Accra, Ghana.
Results:
Results from the research indicate the importance of an EMR system in developing countries to facilitate effective and efficient data collection, data entry, information retrieval and report generation, and research. However, developed nations are not doing enough to help developing countries implement modern technology necessary to facilitate care delivery.
Conclusions:
To achieve the Millennium Development Goal (MDG) number 8 by 2015, developed nations must assist poor countries to develop their human capital, funds and work with the local community to design and implement system friendly with their environment to transform and improve care delivery development.
Keywords: Medical record systems, Computerized, Developing countries, Information systems, Hospital information systems
1. Introduction/background
Electronic medical record (EMR) is not only being welcomed by healthcare providers as a way to improve care delivery but also serves as a catalyst and gold standard for development (Porter, Kohane, & Goldman, 2005; Reifsteck, Swanson, & Dallas, 2006). After Hurricane Katrina the importance of EMR has been reemphasized, since it destroyed or left inaccessible the medical records of untold number of people. This focused new attention on the need for computerized medical records—health records that follow patients, even if their doctors’ offices no longer exist. A disaster does not mean restarting care from the scratch (Endsley, Kibbe, Linares, & Colorafi, 2006).
Unfortunately, Africa, a continent faced with many challenges ranging from epidemics, civil wars, and disasters, also lacks robust healthcare infrastructure in the form of information and communications technology (ICT) to ensure continuity of patient health which many researches considered a lifesaving resource (Azubuike & Ehiri, 1999; Simba, 2004). For instance, Ghana has the best health institutions in the regions such as the Korle-Bu Teaching Hospital and the Social Security and National Insurance Trust Hospital (SSNIT). Korle-Bu Teaching Hospital, for example, is currently the only institution in the West African sub-region which performs bloodless surgery. Due to the quality of outcome, it now receives referrals from most parts of the continent namely the Gambia, Sierra Leone, Liberia, Togo Benin, Tanzania, Nigeria, Cameroon, Cote d’ Ivoire, and Ethiopia. Despite its exemplary performance, the hospital has no automated hospital information system (HIS) which can help improve care delivery in the region. Therefore, the purpose of this study is to examine the potential benefits of EMR and its ultimate contribution to improving healthcare delivery development in less developed countries like Ghana.
2. Methods
The study is an exploratory study conducted in Accra, Ghana, to examine the potential benefits of EMR and its contribution to improving healthcare delivery; it is largely descriptive, and categorized as a non-experimental qualitative study. Initial contacts were made with the Chief Executive Officer (CEO), Public Relations Officer (PRO), and the Chief Administrator of the Korle-Bu Teaching Hospital to help solicit participants for the study.
2.1. Overall study design
2.1.1. Survey methodology
Survey approach was used to gather data from healthcare professionals who were considered principal users of EMR. Copies of the questionnaires were sent through e-mail to participants and were followed up with hard copies that were hand delivered to subjects. In all, a total of 70 surveys containing 19 questions were sent out, of which 45 were returned.
2.1.2. Development of survey instrument
The content of the instrument designed was open-ended questions based on the following areas: knowledge of EMR, benefits and challenges of EMR, transition from paper-based system to EMR, security issues associated with EMR use, assistance given to developing countries by developed nations to implement or use EMR, and demographic details of participants based on profession, length of practice, age, and sex. The survey instrument can be found in the Appendix.
2.1.3. Pre-test or pilot survey
Ten questionnaires were administered to selected healthcare professionals at the University of Missouri Health Care (Columbia, MO, USA). The purpose was to discover potential problems and identify questions that may be misinterpreted, so that the questionnaire could be revised before it was administered to the larger population.
2.2. Participants or sample
This study used a systematic non-probabilistic sampling procedure. Subjects were selected based on their level of healthcare training. The population set for the study was health-care professionals from the Korle-Bu Teaching Hospital, which include physician consultants, surgeons, anesthetists, pharmacists, nurses/midwives, pathologists, radiologists, and laboratory technologists. Study participants were limited to these previously mentioned health professionals, since they would be the principle users of an EMR system.
2.2.1. Representativeness
The study was conducted at the Korle-Bu Teaching Hospital with a total population of about 1000 professionals. Taking into account this was the first time such a study was being conducted in the country, and the limited knowledge of professionals on the subject, as well as difficulty in getting volunteers, a sample size of 50 was chosen for the study of which data were actually obtained on 45.
2.2.2. Informed consent
The study was reviewed and approved by the University of Missouri Health Sciences Institutional Review Board (IRB) as an exempt project. In the waiver of documentation of consent, it was clearly stated that participation in the study was voluntary, and there was no penalty associated with subjects declining to participate.
2.3. Procedures or administration
After approval by the IRB, surveys questionnaires were converted into a PDF file and mailed electronically to all 50 participants on November 13, 2006. Unfortunately, 20 medical professionals who were initially contacted to participate in the study later declined to take part due to lack of understanding the survey questions. As a result, different participants were contacted to replace the 20 individuals to make up the sample size. An environmental health officer with Accra Metropolitan Assembly (AMA) was also contacted and helped to distribute hard copies of the questionnaire and consent letter to all participants, because the researcher could not travel to Ghana. Participants were requested to fill out the attached survey and return it in a sealed envelop to this person or the chief administrator. After 3 weeks on December 14, 2006, a first reminder was mailed asking for their cooperation and the importance of returning the survey. A final reminder was sent on January 4, 2007, after another 3-week period to those who might have forgotten to return the survey.
2.4. Data quality control
The 45 completed surveys were coded, sorted, and organized into themes by two coders. A database was created in MS-Excel to enter all data for analysis.
2.5. Data analysis
A coding system was designed for each question. All responses were placed into themes and summarized. The survey responses and themes generated were used to determine result interpretation, recommendation, and future research direction.
2.6. Responses
Despite initial difficulties to get volunteers to participate in the study, 45 out of the 70 surveys mailed were returned on January 18, 2007, thus representing 64.29% response rate.
3. Results
Based on the methodology, surveys were mailed to 70 participants at the Korle-Bu Teaching Hospital in Accra, Ghana. Forty-five completed surveys were received which included 19 questions. The results from all participants are as follows.
3.1. Demographics
The 45 respondents comprised 28 males, 16 females, and 1 person who did not indicate his or her gender. The mean age of the group was 30.1 (range 22–40). Table 1 presents professional distribution of participants. *NR* (no response) represents people who did not include their profession. The 10 students, however, included final year medical and dentistry students, as well as nursing, and medical laboratory students. Practicing workers experience ranged between 1 and 11 years.
Table 1.
List of professionals
| Profession | Number |
|---|---|
| Surgeon | 2 |
| Anesthetist | 3 |
| Pharmacist | 3 |
| Physician | 3 |
| Radiologist | 3 |
| *NR* | 4 |
| Midwife | 5 |
| Nurse | 6 |
| Laboratory technologist | 6 |
| Student | 10 |
| Total | 45 |
3.2. Knowledge of EMR
According to Dick and Steen (1997), EMR is the compilation of patient medical information in a computer-based format that allows the collection, storage, retrieval, and communication of this data. Therefore, to analyze this result, these key words, computerized, storage and retrieval, were used to determine respondents understanding of the concept. Subsequently, one-third of respondents (33.3%) who included these three key words were marked as right. While nine people representing 20% who said it is a mechanism for storing patient medical record on computer were classified as partially right and approximately half respondents (46.7%) who just said the use of machine to keep patient medical data were classified as having an idea or understanding of the system.
In addition, implementing and running a successful EMR system requires a number of key elements. Accordingly, 27 people identified technical elements (electricity, hardware, software, etc.), 13 stated patient data, while 4 said adequate trained personnel, and 1 person indicated a resource (money to train staff on EMR). Also availability of adequate infrastructure, ICT experts to support and train care providers on EMR is very crucial when implementing EMR system. However, more than half respondents agreed that enough infrastructures are not available in Ghana to support EMR implementation. On the other hand, 18 people believed infrastructures are there, while 4 said available infrastructures are only few.
Despite unavailability of infrastructures, 29 respondents reported there are enough ICT experts in Ghana to train health-care providers to use EMR. Ten reported experts are not available, five stated experts are available but too few to meet the demand and needed training requirement of the healthcare sector. Lastly, one person indicated he has no idea of the subject.
3.3. Assistance given to developing countries by developed nations to implement EMR
Responses concerning how much developed nations are assisting less developed countries like Ghana with HIS infrastructure implementation showed diverse opinions. Nine persons said developed countries are helping, 17 responded no. However, 11 indicated “the help given from developed nations are not enough and sometimes electronic devices sent to less developed countries are inferior and lack quality”. Still others think “some form of assistance comes in to support the country on ICT but not much is channeled to the health sector”. Lastly, seven persons reported they have no idea “if developed nations are helping” and one person did not respond to this question at all.
3.4. Reasons why EMR is not being used at Korle-Bu Teaching Hospital
Paper records are bulky and take up costly space. Filing, retrieval of files, and the re-filing of paper records are very labor-intensive methods with which to store patient information. Plus if a record is checked out for one department, another department cannot access the chart. The impact of not having immediate access to key information in emergency situations can be serious. Paper medical charts also cannot be effectively searched and used to track, analyze, and/or chart voluminous clinical medical information and processes. They cannot be easily copied or saved off-site. Also physician’s orders and the corresponding results (meds, labs, etc.) can be issued and saved in a comprehensive EMR system. Our literature review and results have proven that paper records are costly, cumbersome, easily misplaced and cannot be used for any meaningful decision analysis.
Unfortunately, in spite of Korle-Bu Teaching Hospital’s performance and recognition in the sub-region, it does not have any HIS in place to facilitate care delivery. As noted by participants, “EMR software is not used at Korle-Bu because administration keeps complaining of money. It looks expensive to them and also they are more used to the paper folder”. Nevertheless, four key issues were identified by participants as the main reasons why Korle-Bu does not have EMR system in use. First, 40% of respondents attributed the problem to lack of resources in terms of personnel, infrastructure, etc., 29% blamed it on lack of leadership initiative and priority. While 18% reported cost in terms of equipment and training personnel, 11%, however, stated lack of EMR importance or awareness and fear to change. Lastly, 2.2% respondents did not give any reason.
3.5. Benefits and challenges of EMR
Most developed nations are implementing EMR and other HIS due to the benefits associated with it. According to the survey results, some benefits of EMR are easy accessibility and retrieval of medical documents which represented 31.1%; storage, communication, and consistency in work performance 37.8%; time saving and cost in terms of “number of staff needed to operate the computers as compared to the manual method” 15.6%; easy monitoring and treatment of diseases 6.7%; and finally 4.4% respondents, respectively, stated that it reduces or prevents the possibility of mixing patient’s record loss, and ensures confidentiality and privacy of documents.
Regarding some potential barriers associated with EMR use, 21 respondents representing 47% mentioned lack of power or electricity. According to participants, “hospitals cannot operate effectively when there is power failure”. As a result, it will be difficult accessing and retrieving patient information for decision-making. Eight respondents (18%) attributed the problem to cost in terms of training personnel, maintenance, and cost of acquiring the EMR equipment. Six mentioned lack of technical know-how (personnel and education), another four said people are not prepared to change from the traditional paper-based systems representing 13% and 9%, respectively, and lastly six persons (13%) did not provide any response.
3.6. EMR and care delivery development
As shown from the survey results, it is clear that many participants believed implementation of EMR will tremendously improve upon care delivery in the country. For instance, as noted by one respondent, “availability of patient past history in electronic format will enable health care workers have information about patients in seconds and with ease which will facilitate quick diagnosis and treatment hence reducing the state of morbidity and mortality, leading to quality health care delivery”.
3.7. Transition from paper-based system to EMR
There is always some level of fear and resistance to change, especially in the healthcare industry. A question concerning the level of acceptability from the traditional paper-based system to EMR system showed that such change will be met with some difficulties. More than half of respondents said the process would be challenging initially, but eventually care providers will accept the system because it will facilitate care delivery and work performance. Although majority may still prefer the paper-based system, “they will change when they see the importance or need for EMR stated by a participant”. Others also believed it would be “welcome news”.
3.8. How quickly care providers can be trained to use EMR
It is obvious from the survey results that effective implementation and utilization of EMR can improve upon care delivery in developing countries. Further, considering training as one of the key elements to EMR success, a question was asked to determine length of time required to train care providers in Ghana on EMR. Almost 50% of respondents indicated it might take 3–12 months depending on “care providers’ ability to understand the concepts of EMR as well as the user friendliness of the software”. Others believe “for current graduates who are already computer literate may take about 2 weeks, but the old ones in the system will take longer time (approximately over a year)”.
3.9. Security issues
The adequate protection of patient health record requires limitations at all levels, i.e. collection, use, access, and disclosure. Therefore, development of privacy, confidentiality, and security principles is necessary to protect patients’ interests against inappropriate access to their health data. Unfortunately, 21 respondents (47%) did not respond to this important question regarding measures necessary to maintain patients’ privacy, security, and confidentiality at Korle-Bu. However, 13 and 5 persons representing 29% and 11%, respectively, did state all health records must be securely protected by use of password, data encryption, and access restrictions to users. Finally, as noted by one respondent, “physicians must uphold to their Hippocratic Oath to respect the privacy of their patients and federal legislation must be passed to support the system”.
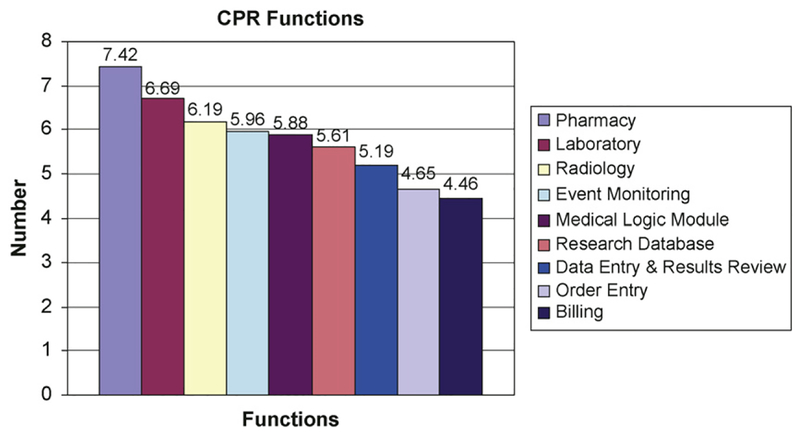
3.10. Functions of computer-based patient record (CPR)
CPR has many components and functions. Participants were asked to rate on a scale of 1–10 nine different functions of CRP according to their order of relevance to their work. Twenty-six respondents (58%) rated the functions correctly, 14 representing 31% rated it wrongly, and 5 persons (11%) did not response at all. Fig. 1 shows the averages of the corrected ratings by the 26 persons in relevance to their work.
Fig. 1.
Functions of CPR in order of importance of job.
4. Discussion
The study focuses on the role of EMR in care delivery, development. Using survey methodology developed, we analyzed 45 people at the Korle-Bu Teaching Hospital in Accra, Ghana, about the benefits of EMR and how it can contribute to care delivery development in developing countries. Results from the research indicate strong importance of EMR system in developing countries to facilitate effective and efficient data collection, data entry, information retrieval and report generation, and research. It also indicated that the use of decision support tools like computerized physician order entry (CPOE) will help in medical errors reduction, improve health-care planning, decision-making, and disease management in the country (Fraser et al., 2005).
Further, due to absence of legislative body such as HIPAA, NIST, etc. in Ghana to enforce regulations against breach of privacy, confidentiality, and security of electronic patient record, findings indicated “passage of laws to back the implementation of the system”. However, in spite of the importance of security, it is essential that the appropriate people are able to access information when they need it. Goedert (2004) explains how a medical center in Washington created a virtual private network (VPN) to secure data sent within the facility and other external sources. However, too many VPN’s were created and the network became too secure, which caused appropriate users to have to go through many authentication procedures before they could log into various applications. Physicians were not able to do two tasks at once during a single session; to resolve this problem, they had to bring in a vendor to re-modify the security settings.
Considering hydropower as the main source of electricity in Ghana, and due to the low level of water in the Akosombo Dam leading to power rationing in the country, more than half of respondents suggested constant electricity supply is the most important thing to take into account when implementing EMR due to the inability of the hospital standby generator to kick in immediately during power outage. This was the most interesting result, because it never occurred to us electricity was a major factor to consider for EMR implementation. Some responses we expected to see were hardware selection and installation, software configuration, space, security, and dealing with paper record. In spite of this problem, study results revealed that developed nations are not doing enough to help developing countries implement modern technology necessary to facilitate care delivery. Finally, results of question number 10 (In what ways can EMR improve or increase your work efficiency as a care provider?) on the survey were not reported, because responses provided were the same as those of question number 2.
5. Conclusions
The potential of EMR system to transform medical care practice has been recognized over the past decades to enhance healthcare delivery and facilitate decision-making process. Subsequently, EMR and other clinical decision support system tools are currently used in both primary and secondary healthcare facilities in most developed nations. However, implementing an EMR system or any HIS in a clinical practice is a daunting task. It requires good planning, strong management and physician leadership, and supportive staff. The most immediate benefits of EMR system include accurate medication lists, legible notes and prescriptions, immediately available charts, decreased chart pulls, lower transcription costs, medical errors reduction, and improved quality care and standard in patient safety. Unfortunately, most countries in sub-Saharan Africa and other poor nations lack the experts, fund, and ICT infrastructure necessary for the implementation of such modern healthcare technology to ensure continuity of care.
6. Recommendations
Research indicates that ICT interventions are contributing to improved efficiency of health service deliveries in the first world. At the same time, many scholars believe one possible area of ICT intervention in the health domain is the automation of medical record system. Further, due to medical knowledge explosion, appropriate decision-making and plan demands accurate, timely, relevant, and appropriately formatted information. Unfortunately, most countries in sub-Saharan African and other poor nations lack ICT infrastructure, fund, and experts to facilitate modern health-care delivery. Therefore, to achieve the MDG number 8, bridging the digital divide between the north and south by the year 2015, and to significantly improve patient care, reduce paperwork, and speed the operations of facilities to promote quality healthcare, it is necessary that international organizations and governments assist poor countries with funds, develop their human capacity, and work effectively with the local experts to design and implement information systems that will strengthen these countries health systems performance, because in the absence of continuity of care, continuity of information is essential to optimize healthcare delivery.
7. Limitations of the study
In the first place, due to difficulty of getting other hospitals involved, the study was limited to only one hospital, hence our findings represent views of that hospital alone. However, we believe the research would have been more interesting and challenging and results more generalized if professionals (subjects) from other hospitals such as the 37 military hospitals, the police hospital, and the trust hospital were involved in the study. Secondly, due to cost of air travel between the United States and Ghana, the researcher was not able to travel to Ghana to collect the necessary data for the study which affected inability of participants to respond to some important questions on the survey.
8. Future research
Automating the paper-based health record system can have a lot of importance for practitioners (clinicians), patients, administrators, and managers. Therefore, we hope this exploratory study will serve as a baseline for funding organizations to help health informaticians explore and collaborate with any of the universities in Ghana to design and implement EMR and other clinical decision support systems to actually access the level of care delivery development in developing countries. Finally, we will recommend rewording of question number 10 in any future study to enable participants respond appropriately as well as researchers going to Ghana for their data collection.
Appendix
EMR survey
What is your understanding of electronic medical record (EMR)?
What are the things needed to implement EMR?
Are there enough infrastructures in Ghana to support EMR implementation?
Are there available information and communications technology experts to train care providers on EMR?
In your opinion, how much are developed nations helping less developed countries to implement EMR?
What are the reasons why EMR software is not being used at Korle-Bu Teaching hospital
Identify some potential barriers (pitfalls) associated with EMR use?
What do you think are some of the benefits associated with EMR use?
Identify some ways by which EMR can contribute to care delivery development in Ghana?
In what ways can EMR improve or increase your work efficiency as a care provider?
How quickly do you think care providers can be trained to use EMR?
To what extent will care providers accept the process of changes necessary to implement EMR?
What would be the ideal approach necessary in Ghana to maintain patient’s security, privacy and confidentiality?
What would be the challenges associated with the move from traditional paper-based system to computer-based patient record (CPR)?
- On a scale of 1 to 10, with 10 being the highest rate the following functions of CPR on your order of importance to your work.
COMPUTER-BASED PATIENT RECORD FUNCTIONS RATE RADIOLOGY (X-ray results, images etc.) PHARMACY (Drug ordering etc.) LABORATORY (Lab tests, sensitivity & specificity analysis etc.) DATA ENTRY & RESULTS REVIEW(Patient demography, appointments schedules etc.) BILLING & FINANCIAL SYSTEM EVENT MONITOR MEDICAL LOGIC MODULES ORDER ENTRY RESEARCH DATABASES What is your main profession?
How long have you been practicing?
Age
Sex.
THANK YOU.
References
- Azubuike MC, & Ehiri JE (1999). Health information systems in developing countries: Benefits, problems, and prospects. The Journal of the Royal Society for the Promotion of Health, 119(3), 180–184. [DOI] [PubMed] [Google Scholar]
- Dick RS, & Steen EB (1997). The computer-based patient record—An essential technology for health care (revised ed.). Washington, DC: Institute of Medicine, National Academy Press. [PubMed] [Google Scholar]
- Endsley S, Kibbe DC, Linares A, & Colorafi K (2006). An introduction to personal health records. Family Practice Management, 13(5), 57–62. [PubMed] [Google Scholar]
- Fraser HSF, Biodich P, Moodley D, Choi S, Mamlin BW, & Szolovits P (2005). Implementing electronic medical record systems in developing countries. Informatics in Primary Care, 14(1), 83–95. [DOI] [PubMed] [Google Scholar]
- Goedert J (2004). Finding the right HIPPA mix. Health Data Management, 12(13), 48. [PubMed] [Google Scholar]
- Porter S, Kohane Z, & Goldman D (2005). Parents as partners in obtaining the medication history. Journal of the American Medical Informatics Association, 12(3), 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reifsteck M, Swanson T, & Dallas M (2006). Driving out errors through tight integration between software and automation. Journal of Healthcare Information Management, 20(4), 35–39. [PubMed] [Google Scholar]
- Simba DO (2004). Application of ICT in strengthening health information systems in developing countries in the wake of globalization. African Health Sciences, 4(3), 195–199. [PMC free article] [PubMed] [Google Scholar]