Abstract
Despite high rates of mental health problems among juvenile justice-involved youth, mental health stigma among juvenile probation officers (JPOs) is under-studied. This cross-sectional study examined effects of job burnout and workplace participatory atmosphere on mental health stigma among JPOs across Indiana (n=226). Participatory atmosphere moderated the relationship between JPO burnout-related cynicism and mental health stigma (interaction β=−0.14, p=.04); burnout was related to greater mental health stigma at low levels of participatory atmosphere. Findings suggest participatory atmosphere mitigates effects of burnout on mental health stigma among JPOs. Organizational-level interventions might help to reduce mental health stigma and combat negative effects from burnout among JPOs.
Keywords: juvenile probation officers, mental health stigma, burnout, organizational climate
Introduction
The work of juvenile probation officers (JPOs) is stressful due to high job demands, including addressing mental health issues among probationers. It is estimated that 60–70% of justice-involved youth have mental health and substance-related problems (Fazel, Doll, & Langstrom, 2008; Vincent, Grisso, Terry, & Banks, 2008). As a result, JPOs are in a position to act as “gateway providers” and connect clients with mental health services (Holloway, Brown, Suman, & Aalsma, 2013; Stiffman, Pescosolido, & Cabassa, 2004). Given the significant burden of mental health concerns among probationers, mental health stigma is one concern among JPOs that has been understudied. Mental health stigma refers to negative attitudes and stereotypes regarding mental health (and persons with mental health issues) and likely influences probation officers’ decision-making regarding case management, and in turn, the well-being of probationers (Link & Phelan, 2001; Tomar et al., 2017). Research among mental health professionals has shown that burnout and workplace atmosphere are two factors related to mental health stigma. Although some research has focused on burnout and workplace atmosphere among adult probation officers, associations between burnout, workplace atmosphere, and mental health stigma are unknown. Further, even less research has examined burnout, workplace atmosphere, and mental health stigma among juvenile probation officers. The current study sought to examine relationships between burnout, participatory atmosphere, and mental health stigma among JPOs.
Burnout
Burnout is a result of prolonged or repeated exposure to work-related stressors and can be characterized by emotional exhaustion, depersonalization, and reduced sense of personal accomplishment or self-efficacy (Maslach, Schaufeli, & Leiter, 2001). One theory that is widely utilized to conceptualize burnout among workers is the job demands-resources model (Demerouti, Bakker, Nachreiner, & Schaufeli, 2001). According to the job demands-resources model, burnout results from an imbalance of job demands and job resources. Job demands are strains that have a negative impact on one’s physical, emotional, and mental health and job performance, while job resources mitigate negative effects of job demands (Demerouti et al., 2001). JPOs likely are at risk for burnout given their high number of job demands, including challenging clients and large caseloads, with concurrent minimal job resources, such as poor social support and limited funding (Gayman & Bradley, 2013; Slate & Johnson, 2013). Further, JPOs are increasingly expected to act as “gateway providers” for clients despite JPO’s lack of education and training in mental health (Tomar et al., 2017).
Although there is scant evidence for associations between burnout and mental health stigma among JPOs (White et al., 2015), burnout has been associated with stigma and negative attitudes towards clients among mental health professionals (Holmqvist & Jeanneau, 2006; Morse, Salyers, Rollins, Monroe-DeVita, & Pfahler, 2012) and other health service providers. For example, among mental health and substance use health professionals, stigma and negative attitudes regarding clients are related to greater burnout (Holmqvist & Jeanneau, 2006; Vilardaga et al., 2011), lower job satisfaction (Ford, Bammer, & Becker, 2008, 2009), and risk of turnover (Kulesza, Hunter, Shearer, & Booth, 2017). Given their lack of associated training, JPOs are poised to be even more likely to experience challenges assisting clients with behavioral and mental health needs (Wasserman et al., 2008). It thus seems likely that burnout might also influence mental health stigma among JPOs—the hypothesis of the current study.
Participatory Atmosphere
Aside from burnout, workplace atmosphere also affects job stress and job performance. In fact, previous research suggests that internal organizational issues are the most significant stressors that probation officers experience (Simmons, Cochran, & Blount, 1997). One important aspect of internal organizational climate is the participatory atmosphere for decision-making. Participatory atmosphere encompasses employees’ opportunities for being involved in workplace decision-making and ability to share ideas and voice concerns (Slate & Vogel, 1997). Importantly, high participatory atmosphere has been related to lower levels of physical, emotional, and job-related stress, greater job satisfaction, and greater job performance among adult probation officers (Slate, Wells, & Johnson, 2003) and other law enforcement personnel (Lee, Joo, & Johnson, 2006; Slate & Vogel, 1997). In fact, it has been recommended that organizations implement participatory management (increase workplace participation in decision-making) as a means of improving job performance and mitigating negative effects of job stress among professionals in the criminal justice system (Simmons et al., 1997).
Consistent with these findings, workplace environment also has been associated with stigma and negative patient attitudes among health professionals (Van Boekel, Brouwers, Van Weeghel, & Garretsen, 2013). For example, across studies of nurses, lack of organizational support and role support are consistently related to greater stigma and more negative attitudes towards patients’ mental health and substance use (Ford et al., 2008; van der Kluit & Goossens, 2011). Conversely, greater cohesion within the organization and greater communication are related to lower patient stigma (Ford et al., 2009). Among substance use treatment providers, more supportive workplace climate is associated with lower stigma towards clients (Kulesza et al., 2017). Given this evidence, it is plausible that participatory atmosphere might protect against negative mental health stigma among JPOs.
Despite evidence for the role of both participatory atmosphere and burnout on job performance among PO’s, to date, no research has examined juvenile probation officers’ reports of burnout and participatory atmosphere, and more importantly, whether participatory atmosphere may buffer or mitigate effects of burnout on mental health stigma. Although there is evidence that they are related, it is unknown whether participatory management, which aims to increase participatory atmosphere, might protect against or mitigate the impact of burnout on mental health stigma. The current study sought to (1) examine mental health stigma among JPOs, and (2) examine the relationship between burnout, participatory atmosphere, and mental health stigma. Participatory atmosphere was hypothesized to moderate the effects of burnout on mental health stigma, such that greater perceived atmosphere for participation mitigate effects of burnout on mental health stigma.
Method
Participants were juvenile probation officers recruited from detention centers across 18 different counties in Indiana as part of a larger study examining the implementation of a universal mental health screener across detention centers (Aalsma, Schwartz, & Perkins, 2014). The title of JPO denotes those whose primary job is managing a caseload of probationers and who may be supervisors or frontline staff. Individuals were included if they had active adolescent probationers on their caseload.
Procedure
Potential participants were contacted via email and invited to participate. The email contained study information and a link to the study survey. Participants were assured before agreeing to participate that all information would be confidential and participation was voluntary. All study procedures were approved by a local university IRB. Participants completed surveys online in a private location of their choosing or on-site (at the detention center) using iPads provided by the research team. Of 258 JPO’s recruited for the study, n = 245 participated in the study (94.96% response rate) with n = 226 JPOs providing complete and valid data for analyses.
Measures
Job and caseload characteristics.
Participants reported on the number of years they have served in their current position as a JPO, whether they are in a supervisor or management position (0 = non-supervisory/management position, 1 = management/supervisory position), and whether or not they have high-risk clients on their caseload (0 = no, 1 = yes). Level of risk refers to risk for recidivism post-release and is based on scores on the Indiana Youth Assessment System (IYAS), which was created as a uniform risk assessment system for youth (Goodman & Thompson, 2011) and is used throughout the juvenile justice system.
Burnout.
The Maslach Burnout Inventory – General Survey (MBI-GS; Maslach, Jackson, & Leiter, 1996) was used to measure three domains of burnout: depersonalization, characterized by cynical and negative attitudes about work (4 items; I have become more cynical about whether my work contributes anything; α = .89), emotional exhaustion, characterized by feelings of emotional fatigue from work (5 items; I feel emotionally drained from my work; α = .92), and personal accomplishment, characterized by feelings of competence and success in one’s work (6 items; In my opinion, I am good at my job; α = .84). Responses ranged from 0 (never) to 6 (everyday); higher mean scores on the depersonalization and emotional exhaustion subscales denote more burnout, while higher scores on the personal accomplishment subscale denote less burnout.
Participatory atmosphere.
The atmosphere for participation subscale of the Attitudes on Participation Survey (Slate & Vogel, 1997) measured JPOs’ perceptions of participation in the workplace. The scale consists of 7 items (e.g., I am encouraged to offer my opinions at work; My superiors ask me for input on decisions that affect me at work), with responses from 1 (strongly disagree) to 5 (strongly agree); higher mean scores indicate perceptions of greater participation in the workplace (α = .76).
Mental health stigma.
Mental health stigma was measured using the Stigma Scale for Receiving Psychological Help (SSRHP; Komiya, Good, & Sherrod, 2000). Five items assess individuals’ perceptions of how stigmatizing it is to receive mental health treatment (e.g., It is a sign of personal weakness or inadequacy to see a psychologist for emotional or interpersonal problems), with responses ranging from 1 (strongly disagree) to 4 (strongly agree) and higher mean scores indicating greater mental health stigma. Internal consistency in the current sample was acceptable (α = .71), similar to that used in another study of police officers (α = .80 in Wester, Arndt, Sedivy, & Arndt, 2010).
Analytic Strategy
All analyses were conducted using SPSS 24.0. We first conduced a linear regression with mental health stigma on all three subscales of the burnout measure in order to determine which facets of burnout were related to mental health stigma. Based on this analysis, only the depersonalization/cynicism subscale was significantly related to mental health stigma, thus, we only used this subscale with further analyses. To assess effects of participatory atmosphere and burnout-related cynicism on mental health stigma, we first conducted an unconditional linear mixed effects model to estimate variance attributed to (1) JPO-level and (2) county-level differences. Estimates showed that the variance attributed to county-level differences was small (ICC = .02), therefore, we chose to omit the county-level random effect from the model.
Next, to test the moderation, we used SPSS 24.0 to specify a fixed-effects model in which mental health stigma served as the dependent variable. Independent variables were entered in separate steps as follows: (1) gender (0 = male, 1 = female), management status (0 = non-management/supervisory role, 1 = management/supervisory role), and whether there were any “high-risk” clients on the JPO’s caseload (0 = no high-risk cases, 1 = high risk cases); (2) depersonalization/cynicism burnout; (3) participatory atmosphere; and (4) the interaction of cynicism burnout × participatory atmosphere. To further assess the interaction, we probed the interaction using the simple slope analysis outlined by Aiken and West (1991), testing for the significance of burnout on mental health stigma at high (+1 standard deviation), mean, and low (−1 standard deviation) levels of participatory atmosphere. We also examined R2 and the change in R2 at each step in order to assess variance accounted for by each variable.
Results
Participants were predominantly white (80.7%), female (67%) and between 30 and 49 years old (64.9%). On average, they reported 95% of their caseloads were juvenile probationers (Table 1 displays descriptive statistics). Of note, females reported lower mental health stigma (t = 3.88, p < .001) compared to males; there were no other differences in mental health stigma across race, age, or management status (p’s > .05). Across the sample, the majority of JPOs reported mild to moderate levels of burnout (depersonalization/cynicism: M = 0.77, SD = 1.04; emotional exhaustion M = 1.23, SD = 1.17; personal accomplishment M = 3.09, SD = 0.96). Those in management positions reported less burnout-related cynicism (t = 2.23, p = .03) and greater participatory atmosphere (t = 5.45, p < .001) compared to those in non-management positions; there were no other differences across race, gender, or age (p’s > .05). Both burnout-related cynicism (r = 0.21, p < .01) and participatory atmosphere (r = −0.13, p = .05) were related to mental health stigma, and burnout-related cynicism was related to participatory atmosphere (r = −0.39, p < .01).
Table 1.
Demographics and study variables
| Variable | M (SD) or % (n) |
|---|---|
| Gender (% female) | 67% (156) |
| Age | |
| 20–29 | 17.5% (41) |
| 30–39 | 37.6% (88) |
| 40–49 | 26.9% (63) |
| 50–59 | 17.1% (40) |
| 60–69 | 0.9% (2) |
| Race | |
| Black/African American | 14.2% (33) |
| Hispanic | 2.1% (5) |
| Caucasian | 80.7% (188) |
| Native American | 1.7% (4) |
| Asian/Pacific Islander | 0 |
| Multiracial/American Indian/Other | 5.2% (12) |
| Other | 0.9% (2) |
| County type | |
| Rural | 29.8% (73) |
| Urban | 70.2% (172) |
| Management/supervisor position | 23.4% (55) |
| Caseload size | 39.67 (28.18) |
| Years in current position | 8 (6.7) |
| High-risk client on caseload (yes/no) | 59.9% |
| Participatory Atmosphere | 22.72 (6.31) |
| Mental health stigma | 4.63 (2.40) |
| Burnout | |
| Cynicism/depersonalization | 0.77 (1.04) |
| Emotional exhaustion | 1.23 ( 1.17) |
| Personal achievement | 3.09 (0.96) |
N = 226
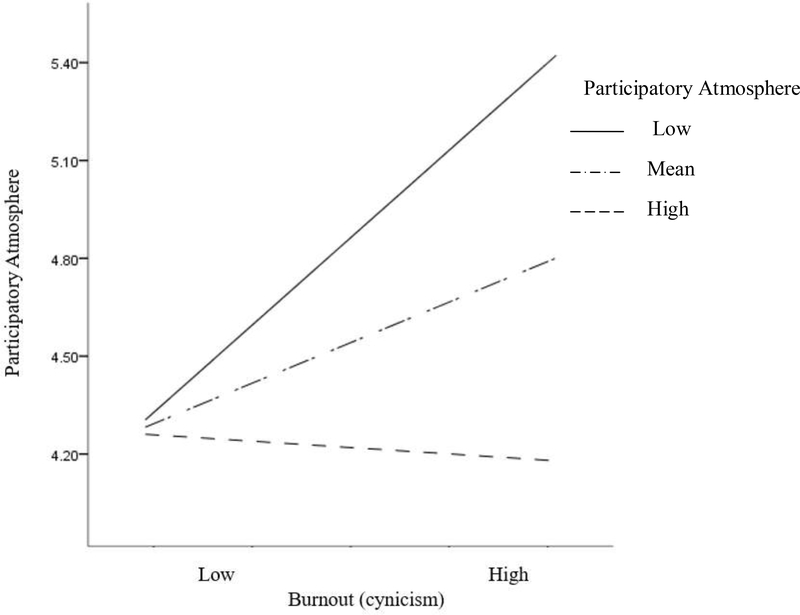
In the linear mixed model, neither burnout-related cynicism (β = 0.27, p = .11) nor participatory atmosphere (β = −0.05, p = .10) were independently related to mental health stigma; however, the interaction of burnout by participatory atmosphere on mental health stigma was significant (β = −0.05, p = .04). In other words, participatory atmosphere moderated the relationship between burnout-related cynicism and mental health stigma, such that burnout-related cynicism was only related to mental health stigma at low levels of participatory atmosphere (−1 standard deviation: β = 0.57, p = .001); at high levels of participatory atmosphere (+1 standard deviation: β = −0.02, p = .94), burnout was not related to mental health stigma. See Table 2 and Figure 1 for results.
Table 2.
Hierarchical regression predicting mental health stigma
| b | β | SE | p | R2 change | |
|---|---|---|---|---|---|
| Step 1 | .07 | ||||
| Gender | −1.16 | −0.21 | .33 | .001 | |
| Management | 0.54 | 0.10 | .36 | .16 | |
| High-risk | 0.37 | 0.08 | .34 | .28 | |
| Step 2 | .04 | ||||
| Burnout (cynicism) | 0.49 | 0.17 | .16 | .01 | |
| Step 3 | .01 | ||||
| Participatory atmosphere | −0.05 | −0.12 | .03 | .09 | |
| Step 4 | .02 | ||||
| Gender | −1.22 | −0.21 | .33 | .001 | |
| Management | 0.74 | 0.10 | .36 | .04 | |
| High-risk | 0.37 | 0.08 | .34 | .51 | |
| Burnout (cynicism) | 0.25 | 0.11 | .17 | .14 | |
| Participatory atmosphere | −0.05 | −0.12 | .03 | .09 | |
| Burnout × Participatory atmosphere | −0.05 | −0.14 | .03 | .04 |
N = 226. Gender (0 = male, 1 = female). High-risk (0 = no high risk clients, 1 = high-risk clients on caseload). Management (0 = non-management position, 1 = management position or supervisory role). Gender, management, and high-risk only shown in the first and last steps to save space. Overall model R = .38.
Figure 1.
Moderation of Participatory Atmosphere on Burnout and Mental Health Stigma. Participatory atmosphere significantly moderated burnout-related cynicism and mental health stigma (interaction: β = −0.14, p = .04). At low levels (−1SD) of participatory atmosphere higher burnout was significantly related to greater mental health stigma (β = 0.57, p = .001). At mean and high (+1SD) levels of participatory atmosphere, burnout was not significantly related to mental health stigma (mean: β = .25, p = .14; +1 SD: β = −0.02, p = .94).
Discussion
The current study sought to examine whether burnout and participatory atmosphere were related to mental health stigma among JPOs. Results showed that participatory atmosphere moderated the relationship between cynicism/depersonalization related to burnout and mental health stigma, such that greater participatory atmosphere buffered – or mitigated – negative effects of burnout-related cynicism on mental health stigma. Although the effect size is small, this is one of few studies examining mental health stigma among JPOs, and the first study to examine effects of burnout-related cynicism and workplace atmosphere on mental health stigma. Findings highlight directions for future research on mental health stigma among JPOs and offer implications for organization-level interventions to reduce burnout and stigma.
As hypothesized, participatory atmosphere moderated the relationship between burnout – specifically depersonalization/cynicism – and mental health stigma. Burnout-related cynicism was only related to mental health stigma when JPOs perceived less participatory atmosphere. When JPOs perceived a high level of opportunities for participation in decision-making in the workplace, burnout-related cynicism was not related to mental health stigma. In other words, participatory atmosphere had a protective effect on negative effects of burnout-related cynicism on mental health stigma. The current findings are consistent with research with other professional groups, such as criminal justice and health care providers. For instance, a study of law enforcement professionals found participatory atmosphere – and other aspects of organizational climate – can ameliorate job stress and the negative effects of job stress on performance (Slate et al., 2003). The current study is the first to examine moderating effects of participatory atmosphere on associations between cynicism related to burnout and job performance-related outcomes among JPOs, thus expanding on existing literature. Additionally, these findings among JPOs are similar to literature on mental health stigma among other mental health service providers. Studies of nurses (Ford et al., 2009) and substance use service providers (Kulesza et al., 2017) have both found that a more supportive workplace environment is related to lower mental health stigma and lower negative attitudes toward clients.
Surprisingly, neither the emotional exhaustion nor personal accomplishment subscales of the burnout inventory were related to mental health stigma. One reason could be that cynicism and detachment from juvenile probationers in particular might contribute to more negative attitudes about probationers being served and in turn greater stigma.
Given the increasing responsibility of JPOs to connect clients to services, as well as the added strain that probationer mental health issues have on probation officers, a better understanding of stigma – as well as mental health knowledge and training needs – is warranted. JPOs in the current sample endorsed higher levels of mental health stigma than that reported by police officers in a previous study (Wester et al., 2010), further highlighting the need for additional research on mental health stigma among JPOs. Importantly, mental health stigma and knowledge among probation officers may influence probation officers’ decisions about risk assessment, case management, and general probationer-officer interactions (Eno Louden, Skeem, Camp, & Christensen, 2008; Eno Louden & Skeem, 2013; Wasserman et al., 2008). There have been some recent efforts to provide mental health training to probation officers. For example, one recent study sought to implement a mandatory statewide mental health training program for probation officers; the program curriculum consisted of information regarding mental health issues, such as severe mental illness symptoms, as well as training in responding to mental health crises and determining the need for mental health referrals (Tomar et al., 2017). The study found no differences in ratings of mental health stigma pre and post training, suggesting that training to increase mental health knowledge alone may not be sufficient to reduce mental health stigma. These findings parallel evidence from research with mental health service providers that educational and training programs alone are not successful for decreasing stigma and negative attitudes among service providers (Ford et al., 2009).
Research from related fields including mental health and child welfare suggest that workforce interventions that focus on improving organizational climate can positively influence attitudes toward clients, while simultaneously improving outcomes related to burnout, including staff turnover and attitudes. Research by Glisson and colleagues (2002, 2008) suggest that improving the organizational climate in social service systems is as important to improving service outcomes as the delivery of evidence-based practices. The Availability, Responsiveness, and Continuity (ARC) model is a rigorously evaluated organizational intervention that has demonstrated success in improving organizational culture, climate, and morale; reducing staff turnover; and improving service outcomes (Glisson et al., 2010). ARC has demonstrated success in improving the organizational social context of child mental health clinics and child welfare agencies; in randomized controlled trials, youth receiving services from the clinics that demonstrated the strongest climates in response to the ARC intervention showed the strongest clinical improvements (Glisson et al., 2010; Glisson, Dukes, & Green, 2006). More recently, the R3 supervisor implementation strategy was developed to improve the organizational culture of a child welfare workforce through provision of evidence-based supervision (Saldana, Chamberlain, & Chapman, 2016). Through promotion of the use of targeted positive reinforcement, caseworkers demonstrated improved attitudes toward casework and clients, and in turn, youth and families demonstrated improved outcomes (Saldana, Chamberlain, & Chapman, 2017). Similar to the role of JPOs as “gateway providers” for youth’s mental health needs, child welfare caseworkers serve in a primary role of referrer to, and monitoring of compliance with, mental health and related services. The R3 intervention actively facilitates supportive casework to increase client cooperation and participation with treatment goals. Future research might consider the applicability of similar interventions in the Juvenile Justice social service system.
One challenge in implementing social service models in juvenile probation organizations is JPOs have competing roles of law enforcement and rehabilitation. JPOs may be hesitant to adopt evidence-based practices that are not seen to align with the organizational culture of the juvenile justice system (Young, Moline, Farrell, & Bierie, 2006). Thus, it is particularly important to address an organizational culture that is supportive of JPOs emphasizing equally mental health and criminal justice needs. This can, in part, be accomplished through the establishment of stakeholder “buy-in,” as outlined in the Office of Juvenile Justice and Delinquency Prevention (OJJDP) Implementation Guide (https://www.ojjdp.gov/mpg-iguides/) for adopting evidence-based practice within juvenile justice settings. Indeed, there has been success in implementing social service models in juvenile justice settings (Glisson et al., 2006; Taxman, Henderson, Young, & Farrell, 2014). Intervention strategies that target the social climate – including participatory atmosphere – are particularly effective in increasing organizational readiness to adopt new practices and policies and should be considered in implementation (Taxman et al., 2014).
Limitations
Despite the novelty of findings, there are some limitations. First, the study is cross-sectional, and thus, results are subject to common method bias. Second, all JPOs were from Indiana, and although they were taken from a diverse range of counties, including rural and urban, it is possible that these findings might not translate to other states or organizations. Third, across the sample there were no county-level differences in participatory atmosphere, burnout, and mental health stigma. Further, effects of participatory atmosphere on associations between burnout and mental health stigma were similar across counties. More heterogeneous samples – such as organizations across states – are needed in order to identify and determine if there are organization-level differences. Fourth, the cross-sectional nature of the study did not allow us to test for causation. For example, it could be that mental health stigma influences burnout. Fifth, there are likely a multitude of factors that influence mental health stigma that we did not measure, such as JPOs’ mental health knowledge or training. We also did not examine the racial/ethnic composition of JPO caseloads, which may influence mental health stigma, as there is evidence that juvenile offender race influences JPO decision-making and case management (Leiber & Mack, 2003). Lastly, further research is needed to determine how mental health stigma in turn influences JPOs’ actual interactions with probationers and decision-making in case management.
Conclusion
This was one of the first studies to examine mental health stigma among JPOs; findings highlight the important role of burnout-related cynicism/depersonalization and participatory atmosphere in mental health stigma. Findings that greater participatory atmosphere in the workplace mitigated effects of burnout-related cynicism/depersonalization on mental health stigma offers important implications for organizational efforts to reduce mental health stigma among JPOs as well as improve workplace atmosphere. Additional research mental health stigma burnout-related cynicism/depersonalization among JPO’s is crucial given that stigma and negative attitudes towards probationers may negatively influence JPOs’ relationships with probationers and even their decisions regarding case management.
References
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage. [Google Scholar]
- Demerouti E, Bakker AB, Nachreiner F, & Schaufeli WB (2001). The job demands resources model of burnout. Journal of Applied Psychology, 86, 499–512. doi: 10.1037/0021-9010.86.3.499 [DOI] [PubMed] [Google Scholar]
- Eno Louden J, & Skeem JL. (2013). How do probation officers assess and manage recidivism and violence risk for probationers with mental disorder? An experimental investigation. Law and Human Behavior, 37, 22–34. doi: 10.1037/h0093991 [DOI] [PubMed] [Google Scholar]
- Eno Louden JE, Skeem JL, Camp J, & Christensen E (2008). Supervising probationers with mental disorder: How do agencies respond to violations? Criminal Justice and Behavior, 35, 832–847. doi: 10.1177/0093854808319042 [DOI] [Google Scholar]
- Fazel S, Doll H, & Långström N (2008). Mental disorders among adolescents in juvenile detention and correctional facilities: A systematic review and meta regression analysis of 25 surveys. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 1010–1019. doi: 10.1097/CHI.ObO13e31817eecf3 [DOI] [PubMed] [Google Scholar]
- Ford R, Bammer G, & Becker N (2008). The determinants of nurses’ therapeutic attitude to patients who use illicit drugs and implications for workforce development. Journal of Clinical Nursing, 17, 2452–2462. doi: 10.1111/j.1365-2702.2007.02266.x [DOI] [PubMed] [Google Scholar]
- Ford R, Bammer G, & Becker N (2009). Improving nurses’ therapeutic attitude to patients who use illicit drugs: Workplace drug and alcohol education is not enough. International Journal of Nursing Practice, 15, 112–118. doi: 10.1111/j.1440-172X.2009.01732.x [DOI] [PubMed] [Google Scholar]
- Gayman MD, & Bradley MS (2013). Organizational climate, work stress, and depressive symptoms among probation and parole officers. Criminal Justice Studies: A Critical Journal of Crime, Law and Society, 26, 326–346. doi: 10.1080/1478601X.2012.742436 [DOI] [Google Scholar]
- Glisson C (2002). The organizational context of children’s mental health services. Clinical Child and Family Psychology Review, 5, 233–253. doi: 10.1023/A:1020972906177 [DOI] [PubMed] [Google Scholar]
- Glisson C (2010). Organizational climate and service outcomes in child welfare settings In Webb MB, Dowd K, Harden BJ, Landsverk J, & Testa M (Eds.), Child welfare and child well-being: New perspectives from the national survey of child and adolescent well-being (pp. 380–408). New York, NY: Oxford University Press. [Google Scholar]
- Glisson C, Dukes D, & Green P (2006). The effects of the ARC organizational intervention on caseworker turnover, climate, and culture in children’s service systems. Child Abuse and Neglect, 30, 855–880. doi: 10.1016/j.chiabu.2005.12.010 [DOI] [PubMed] [Google Scholar]
- Glisson C, Schoenwald SK, Hemmelgarn A, Green P, Dukes D, Armstrong K, & Chapman JE (2010). Randomized trial of MST and ARC in a two-level evidence-based treatment implementation strategy. Journal of Consulting and Clinical Psychology, 78, 537–550. PMCID: PMC3951378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glisson C, Schoenwald SK, Kelleher K, Landsverk J, Hoagwood KE, Mayberg S, & Green P (2008). Therapist turnover and new program sustainability in mental health clinics as a function of organizational culture, climate, and service structure.Administration & and Policy in Mental Health & Mental Health Services Research, 35, 124–133. [DOI] [PubMed] [Google Scholar]
- Goodman M, & Thompson L (2011, April 13). Indiana’s new risk assessment tools: What you should know. Indiana Court Times. Retrieved from http://indianacourts.us/ [Google Scholar]
- Holloway ED, Brown JR, Suman PD, & Aalsma MC (2013). A qualitative examination of juvenile probation officers as gateway providers to mental health care. Criminal Justice Policy Review, 24, 370–392. doi: 10.1177/0887403412436603 [DOI] [Google Scholar]
- Holmqvist R, & Jeanneau M (2006). Burnout and psychiatric staff’s feelings towards patients. Psychiatry Research, 145, 207–213. doi: 10.1016/j.psychres.2004.08.012 [DOI] [PubMed] [Google Scholar]
- Komiya N, Good GE, & Sherrod NB (2000). Emotional openness as a predictor of college students’ attitudes toward seeking psychological help. Journal of Counseling Psychology, 47, 138–143. doi: 10.1037/0022-0167.47.1.138 [DOI] [Google Scholar]
- Kulesza M, Hunter SB, Shearer AL, & Booth M (2017). Relationship between provider stigma and predictors of staff turnover among addiction treatment providers. Alcoholism Treatment Quarterly, 35, 63–70. doi: 10.1080/07347324.2016.1256716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee WJ, Joo HJ, & Johnson W (2009). The effect of participatory management on internal stress, overall job satisfaction, and turnover intention among federal probation officers. Federal Probation, 73, 33. [Google Scholar]
- Leiber MJ, & Mack KY (2003). The individual and joint effects of race, gender, and family status on juvenile justice decision-making. Journal of Research in Crime and Delinquency, 40, 34–70. doi: 10.1177/0022427802239253 [DOI] [Google Scholar]
- Link BG, & Phelan JC (2001). Conceptualizing stigma. Annual Review of Sociology, 27, 363–385. doi: 10.1146/annurev.soc.27.1.363 [DOI] [Google Scholar]
- Maslach C, Jackson SE, & Leiter MP (1996). Maslach Burnout Inventory: Manual (3rd ed.). Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Maslach C, Schaufeli WB, & Leiter MP (2001). Job burnout. Annual Review of Psychology, 52, 397–422. doi: 10.1146/annurev.psych.52.1.397 [DOI] [PubMed] [Google Scholar]
- Morse G, Salyers MP, Rollins AL, Monroe-DeVita M, & Pfahler C (2012). Burnout in mental health services: A review of the problem and its remediation. Administration and Policy in Mental Health and Mental Health Services Research, 39, 341–352. doi: 10.1007/s10488-011-0352-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saldana L, Chamberlain P, & Chapman JE (2017). Creating system change: A state-initiated rollout of the R3 supervisor-targeted practice change model. Presented at the Society for Implementation Research Collaborative Seattle, Washington September. [Google Scholar]
- Saldana L, Chamberlain P, & Chapman JE (2016). A supervisor-targeted implementation approach to promote system change: The R3 Model. Administration and Policy in Mental Health and Mental Health Services Research. Advance online publication: doi: 10.1007/s10488-016-0730-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons C, Cochran JK, & Blount WR (1997). The effects of job-related stress and job satisfaction on probation officers’ inclinations to quit. American Journal of Criminal Justice, 21, 213–229. doi: 10.1007/BF02887450 [DOI] [Google Scholar]
- Slate RN, & Johnson WW (2013). Stressors experienced by state and federal probation officers In Miller MK & Bornstein BH (Eds.), Stress, trauma, and wellbeing in the legal system (pp. 197–215). New York, NY: Oxford University Press. [Google Scholar]
- Slate RN, Johnson WW, & Wells T (2000). Probation officer stress: Is there an organizational solution? Federal Probation, 64, 56–59. [Google Scholar]
- Slate RN, & Vogel RE (1997). Participative management and correctional personnel: A study of the perceived atmosphere for participation in correctional decision making and its impact on employee stress and thoughts about quitting. Journal of Criminal Justice, 25, 397–408. doi: 10.1016/S0047-2352(97)00023-8 [DOI] [Google Scholar]
- Stiffman A, Pescosolido B, Cabassa L (2004). Building a model to understand youth service access: The gateway provider model. Mental Health Services Research, 6, 189–198. doi: 10.1023/B:MHSR.0000044745.09952.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomar N, Ghezzi MA, Brinkley-Rubinstein L, Wilson AB, Van Deinse TB, Burgin S, & Cuddeback GS (2017). Statewide mental health training for probation officers: Improving knowledge and decreasing stigma. Health & Justice, 5, 11. doi: 10.1186/s40352-017-0057-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Boekel LC, Brouwers EP, Van Weeghel J, & Garretsen HF (2013). Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug and Alcohol Dependence, 131, 23–35. doi: 10.1016/j.drugalcdep.2013.02.018 [DOI] [PubMed] [Google Scholar]
- van der Kluit MJ, & Goossens PJ (2011). Factors influencing attitudes of nurses in general health care toward patients with comorbid mental illness: An integrative literature review. Issues in Mental Health Nursing, 32, 519–527. doi: 10.3109/01612840.2011.571360 [DOI] [PubMed] [Google Scholar]
- Vilardaga R, Luoma JB, Hayes SC, Pistorello J, Levin ME, Hildebrandt MJ, ... & Bond F. (2011). Burnout among the addiction counseling workforce: The differential roles of mindfulness and values-based processes and work-site factors. Journal of Substance Abuse Treatment, 40, 323–335. doi: 10.1016/j.jsat.2010.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent GM, Grisso T, Terry A, & Banks S (2008). Sex and race differences in mental health symptoms in juvenile justice: The MAYSI-2 national meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 282–290. doi: 10.1097/CHI.0b013e318160d516 [DOI] [PubMed] [Google Scholar]
- Wasserman GA, McReynolds LS, Whited AL, Keating JM, Musabegovic H, & Huo Y (2008). Juvenile probation officers’ mental health decision making. Administration and Policy in Mental Health and Mental Health Services Research, 35, 410–422. doi: 10.1007/s10488-008-0183-x [DOI] [PubMed] [Google Scholar]
- Wester SR, Arndt D, Sedivy SK, & Arndt L (2010). Male police officers and stigma associated with counseling: The role of anticipated risks, anticipated benefits and gender role conflict. Psychology of Men & Masculinity, 11, 286–302. doi: 10.1037/a0019108 [DOI] [Google Scholar]
- White LM, Aalsma MC, Holloway ED, Adams EL, & Salyers MP (2015). Job-related burnout among juvenile probation officers: Implications for mental health stigma and competency. Psychological Services, 12, 291–302. doi: 10.1037/ser0000031 [DOI] [PubMed] [Google Scholar]
- Young D, Moline K, Farrell J, & Bierie D (2006). Best implementation practices: Disseminating new assessment technologies in a juvenile justice agency. Crime & Delinquency, 52, 135–158. doi: 10.1177/0011128705281752 [DOI] [Google Scholar]
- Taxman FS, Henderson C, Young D, & Farrell J (2014). The impact of training interventions on organizational readiness to support innovations in juvenile justice offices. Administration and Policy in Mental Health, 41, 177–188. doi: 1007/s10488-0120445-5 [DOI] [PMC free article] [PubMed] [Google Scholar]