Abstract
Objective:
The cognitive indicators of preclinical behavioral variant Frontotemporal Dementia (bvFTD) have not been identified. To investigate these indicators, we compared cross-sectional performance on a range of cognitive measures in 12 carriers of pathogenic MAPT mutations not meeting diagnostic criteria for bvFTD (i.e. preclinical) versus 32 demographically-matched familial non-carriers (n=44). Studying preclinical carriers offers a rare glimpse into emergent disease, environmentally and genetically contextualized through comparison to familial controls.
Methods:
Evaluating personnel blinded to carrier status administered a standardized neuropsychological battery assessing attention, speed, executive function, language, memory, spatial ability, and social cognition. Results from mixed effect modeling were corrected for multiplicity of comparison by the False Discovery Rate method, and results were considered significant at p<0.05. To control for potential interfamilial variation arising from enrollment of six families, family was treated as a random effect, while carrier status, age, gender, and education were treated as fixed effects.
Results:
Group differences were detected in 17 of 31 cognitive scores and spanned all domains except spatial ability. As hypothesized, carriers performed worse on specific measures of executive function, and social cognition, but also on measures of attention, speed, semantic processing, and memory storage and retrieval.
Conclusions:
Most notably, group differences arose on measures of memory storage, challenging long-standing ideas about the absence of amnestic features on neuropsychological testing in early bvFTD. Current findings provide important and clinically relevant information about specific measures that may be sensitive to early bvFTD, and advance understanding of neurocognitive changes that occur early in the disease.
Keywords: Frontotemporal Dementia, MAPT Protein, Neurodegenerative Hereditary Disease, Cognition Disorders, Frontotemporal Lobar Degeneration, Tauopathy
Introduction
Behavioral variant Frontotemporal Dementia (bvFTD) is among several neurodegenerative disorders within the spectrum of Frontotemporal Degeneration (FTD) disorders. In bvFTD, progressive atrophy in regions of the frontal and temporal lobes gives rise to insidious changes in personality, behavior, and affect as well as specific aspects of cognition (Neary, Snowden, & Mann, 2005; Neary et al., 1998; Rascovsky, Hodges, et al., 2007; Snowden, Neary, & Mann, 2002). While the broader diagnostic criteria have evolved alongside advances in understanding of its etiology and heterogeneity, some symptoms have consistently been classified as core features of bvFTD, including socially inappropriate behaviors, apathy, and inertia (Neary et al., 1998; Rascovsky, Hodges, et al., 2007; Rascovsky et al., 2011; Snowden et al., 2002). The cognitive profile has traditionally been described as involving deficits in attention and executive function (i.e., judgment, abstraction, planning, and mental flexibility), and language to a lesser extent, with relative preservation of memory storage and spatial function(Neary et al., 1998). Changes in social cognition may accompany or precede executive dysfunction, corresponding to the early compromise of ventromedial structures prior to changes in the prefrontal dorsolateral cortex(Seeley et al., 2008).
Studying prodromal neurodegenerative disease requires an independent gold standard for the incipience of disease, such as a pathogenetic mutation. Among FTD cases, between 2–10 % may be accounted for by mutations in the microtubule-associated protein tau (MAPT) gene, which codes for production of tau: a protein crucial in microtubule stabilization, providing neuron polarity and signal transduction(Brandt, Hundelt, & Shahani, 2005), and located on chromosome 17(Lynch et al., 1994). MAPT mutations disrupt tau function, resulting in a tauopathy commonly expressed as the bvFTD phenotype (Boeve & Hutton, 2008; Brandt et al., 2005; Rohrer et al., 2015). Among MAPT carriers, age-of-onset and symptomatology vary genotypically, interfamilially, and even intrafamilially, though penetrance nonetheless approaches 100%(Boeve & Hutton, 2008; Goedert, Crowther, & Spillantini, 1998; Wittenberg et al., 2008). Heterogeneity is partly attributable to tau pathology, which varies by mutation in distribution, filamentous structure, and isoform conformation(Goedert et al., 1998; Spillantini, Bird, & Ghetti, 1998; Van Swieten et al., 1999; Wittenberg et al., 2008). Boeve and Hutton (2008) reported that the typical age of symptom onset amongst MAPT carriers varies between 25 – 65 years of age, with duration ranging from 3 – 10 years spanning onset to death(Boeve & Hutton, 2008).
FTD arising from MAPT mutations has been associated with symmetrical atrophy of the anteromedial temporal and orbitofrontal regions (Rohrer et al., 2010). Neuroimaging studies of presymptomatic carriers have found striatal dopaminergic abnormalities on Positron Emission Tomography, and hippocampal atrophy in carriers as compared with non-carriers(Miyoshi et al., 2010). Neuropsychological findings in MAPT carriers appear consistent with those reported in general bvFTD (Ferman et al., 2003; Hodges, 2001; Lynch et al., 1994; Rascovsky et al., 2011; Snowden et al., 2002; Wittenberg et al., 2008); thus studying MAPT carriers may elucidate disease progression in typical or “classic” bvFTD. This affords relatively greater generalizability to sporadic bvFTD than would be offered by studying carriers of other FTD-related mutations for which phenotypic expression is more diverse, such as the c9orf72 or Progranulin genes.
Though many studies have investigated the cognitive presentation of bvFTD at diagnosis or in the early stage of dementia, relatively little work has examined the cognitive prodrome of this disorder. Studies of tau mutation carriers report early executive dysfunction, particularly on measures of phonemic fluency (Alberici et al., 2004; Ferman et al., 2003; Jiskoot et al., 2016; Rohrer et al., 2015). Among early and presymptomatic N279K MAPT carriers, deficits were evident in word generation, motor speed and visual scanning, and divided attention and set shifting (Ferman et al., 2003). Boxer and Miller (2005) suggested tasks sensitive to impairment in executive functions such as set-shifting, abstraction, reasoning, self-monitoring, and adaptive incorporation of feedback may be suited for detecting deficits in bvFTD (Boxer & Miller, 2005; Hodges, 2001). In the present study, a standardized comprehensive cognitive battery spanning the domains of attention, speed, executive abilities, language, memory, spatial ability, and social cognition was administered to the Columbia University MAPT cohort: a group of preclinical MAPT mutation carriers not fully meeting bvFTD diagnostic criteria, as well as their demographically matched non-carrier relatives, analyzed as healthy controls. Juxtaposing preclinical carriers with non-carriers from a small number of families, grants the unique opportunity to investigate the earliest cognitive changes in incipient bvFTD while reducing covariation from environment or genetics that would otherwise arise from studying numerous families and unrelated controls. Social cognition and executive abilities were hypothesized to be among the earliest cognitive indicators of bvFTD.
Materials and Methods
Experimental Design
44 participants were drawn from the Columbia University MAPT cohort, a group of 59 subjects from six families carrying distinct MAPT mutations, enrolled in a longitudinal observational multi-site research study conducted in the United States and Ireland. Recruitment efforts targeted multiple generations of at-risk branches in families in which at least one person was confirmed to carry a MAPT mutation. Over half of the 59 enrolled subjects descend from a single extended kindred carrying an exon 10 +14 C>T MAPT mutation. In fact, this is the family in which FTLD was first linked to chromosome 17 (Lynch et al., 1994). In 1994, Lynch and colleagues reported on the parent generation of the offspring recruited herein; early symptoms included behavioral and personality changes, followed by executive dysfunction, hyperphagia, and Parkinsonism (Lynch et al., 1994). Members were enrolled from this Exon 10 + 14 C>T family, as well as other families carrying different MAPT mutations including: Exon 10 + 15 (IVS10+15 A>C), Exon 10 + 16 (IVS10+16 C>T), V337M, P301L, and R406W, all of which have been established as pathogenic (Ghetti et al., 2015). All subjects gave written informed consent prior to study participation. All study sites received institutional ethical board approval prior to beginning study procedures.
Genetic and Clinical Assessment
All enrolled subjects contributed a blood sample from which DNA was isolated, and tested for carrier status in a research laboratory. Out of 59 enrolled subjects, genomic DNA testing identified 12 (8 females, and 4 males) as mutation positive: four each of V337M and Exon 10 +14 mutations, two of an Exon 10 + 15, one of an Exon 10 + 16, and one of a P301L mutation. No carriers were enrolled from the R406W family. Evaluating study personnel were blinded to carrier status at evaluation. All subjects underwent a neurological examination and afterward were assigned a Global Clinical Dementia Rating (CDR) score by the evaluating neurologist (Hughes, Berg, Danziger, Coben, & Martin, 1982). Recruitment efforts were extensive and targeted entire at-risk sibships, but we rarely succeeded in enrolling all siblings in a particular sibship. More often than not, a few family members from an at-risk sibship were unwilling to participate in the study. Given that only 12 of 59 enrolled subjects were found to be mutation positive, we speculate that more carriers exist within the families in this cohort, who were unwilling to participate in research perhaps due to anxiety of knowing they were at-risk for inheriting a devastating neurodegenerative illness.
Subjects
Following a neurological examination, six of twelve carriers received CDR=0, indicating no symptoms, and the remaining six were deemed CDR=0.5, indicating questionable symptoms. 32 familial non-carriers matched in a group fashion to individual carriers by sex, age (up to ten years younger or older than matched carrier), years of education (up to four years fewer or more than matched carrier), and Global CDR score (all controls are CDR=0) were analyzed as controls, to ensure that the distribution of main demographics were comparable between carriers and non-carriers. 15 enrolled non-carriers not matching to at least one carrier on all these criteria were excluded from the analysis. Due to the demographic distribution of the sample, some carriers matched to more non-carriers than others.
Cognitive Testing
Certified personnel administered a comprehensive standardized neuropsychological assessment comprising of the National Alzheimer’s Coordinating Center’s (NACC) Uniform Data Set (UDS 2.0)(Weintraub et al., 2009) and FTLD Module Version 2.0 (Beekly et al., 2012), as well as additional select tests including the Selective Reminding Test (SRT) (Buschke, 1973), Frontal Assessment Battery (FAB)(Dubois, Slachevsky, Litvan, & Pillon, 2000), Delis-Kaplan Executive Function System (D-KEFS) Twenty Questions(Delis, Kaplan, & Kramer, 2001), and Design Fluency Graphic Pattern Generation (Design Fluency)(Glosser & Goodglass, 1990). The NACC UDS 2.0 was administered first and included: the Mini Mental State Examination (MMSE), Logical Memory IA and IIA, Digit Span Forward and Backward, Category Fluency, Trail Making Test (TMTA and TMTB), WAIS-R Digit Symbol, and the Boston Naming Test. Next, subjects completed the NACC FTLD Module 2.0, which included the Benson Complex Figure Copy and Delay, Phonemic Fluency (C, F, and L), Word Reading Test Regular and Irregular Words, Semantic Word-Picture Matching Test, Semantic Associates Test, Northwestern Anagram Test (NAT) Short Form, Sentence Repetition Test, Noun and Verb Naming Subtests, and Sentence Reading Test. Also administered in the FTLD Module 2.0 were the Social Norms Questionnaire (SNQ), the examiner-completed Social Behavior Observer Checklist (SBOC), and three informant-completed questionnaires: the Behavioral Inhibition Scale (BIS), Interpersonal Reactivity Index (IRI), and the Revised Self-Monitoring Scale (RSMS).Informants were subject-elected, usually family members, spouses, or close friends, and a small minority of subjects elected informants who were also enrolled in the study as controls (except in one case, where a control’s informant was found to be a carrier, but closer examination of the informant’s reports found no reason to suspect validity).Lastly, after completion of the NACC UDS 2.0 and FTLD Module 2.0, the aforementioned additional select tests were administered: the Selective Reminding Test, Frontal Assessment Battery, D-KEFS Twenty Questions, and Design Fluency. The traditional multiple choice recognition component of the Selective Reminding Test was replaced with a more rigorous yes/no recognition measure, to more sensitively assess this preclinical sample. The SRT recognition measure used herein is a locally developed experimental measure modeled on the components of other list learning tests, in which a list of words is recited one at a time, including targets, semantically related, and unrelated words (all matched for a variety of linguistic features including work length, frequency, number of syllables, etc.), and the subject must indicate which words were on the original target list. A discriminability index ranging from 0 to 1 is computed by subtracting the sum of omissions and commissions from one, and dividing this number by 36 (the total number of words presented), with a maximum score of one. Higher scores indicate better recognition.
Statistical Analyses
Group performance across 31 representative measures was analyzed with mixed-effects models, with carrier status, age, gender, and education treated as fixed effects, and family treated as a random effect, to control for potential intrafamilial variation (see Table 2). Measures of constructs already captured in other tests, such as the Logical Memory Task were excluded to minimize multiplicity bias. Because published normative data were unavailable for some measures, analyses were conducted using raw scores; however, all models included adjustment for age, gender, and education. The multiple comparison correction controlling false discovery rate method was chosen for its power (Benjamini & Hochberg, 1995).False discovery rate (FDR) controlling procedures are designed to control the expected proportion of rejecting null hypotheses that are false, and they provide less stringent control of Type I errors compared to familywise error rate (FWER) controlling procedures, which control the probability of at least one Type I error. Thus, FDR-controlling procedures have greater power. Most outcomes with significant differences showed greater than medium effect size difference. Thus, over correcting has a higher chance of losing signal for our data, and so we chose to apply FDR controlling procedures. Results were considered significant at p <0.05.Statistical analyses were conducted using SAS software, Version 9.4 of the SAS System. Copyright © [2017] SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
Table 2:
Findings from individual mixed-effect models of group differences between carriers and non-carriers
| Controls (n=32) | All Carriers (n=12) | Correct ed pvalue | CDR=0 Carriers | CDR=0.5 Carriers | |
|---|---|---|---|---|---|
| Mean (±SD) | Mean (±SD) | Mean (±SD) | Mean (±SD) | ||
| Attention & Processing | |||||
| Digit Span | 15.72 (2.77) | 16.25 (4.16) | 0.6948 | 17.83 (3.82) | 14.67 (4.18) |
| WAIS-Digit Symbol^ | 60.22 (13.01) | 53.00 (15.08) | 0.1347 | 62.50 (12.65) | 43.50 (11.11) |
| Trail Making Part A (TMTA)^ | 24.66 (6.71) | 36.08 (24.30) | 0.0203 | 22.00 (5.83) | 50.17 (28.10) |
| Executive Abilities | |||||
| Trail Making Part B (TMTB)^* | 58.37 (22.41) | 86.33 (61.58) | 0.0203 | 54.17 (18.05) | 118.50 (74.38) |
| Frontal Assessment Battery | 16.69 (1.47) | 15.17 (3.16) | 0.0126 | 16.83 (1.17) | 13.50 (3.73) |
| Design Fluency Total Correct# | 17.13 (2.04) | 13.82 (7.61) | 0.0096 | 18.67 (1.51) | 8.00 (8.03) |
| Design Fluency Perseveration Distance*# | 7.10 (3.71) | 3.70 (4.60) | 0.0465 | 3.70 (4.60) | 3.70 (5.14) |
| Design Fluency time*# | 291.77 (136.95) | 310.90 (206.72) | 0.9216 | 261.60 (155.94) | 360.20 (256.43) |
| D-KEFS Twenty Questions Initial Abstraction* | 11.40 (2.71) | 10.17 (3.33) | 0.1263 | 12.00 (1.79) | 8.33 (3.61) |
| Language | |||||
| Boston Naming Test (BNT)^ | 27.44 (1.79) | 20.75 (8.62) | 0.0001 | 27.50 (1.38) | 14.00 (7.24) |
| Category Fluency Animals^ | 20.09 (4.60) | 16.17 (8.11) | 0.0203 | 22.50 (2.74) | 9.83 (6.40) |
| Phonemic Fluency (CFL) ^* | 44.41 (9.31) | 40.08 (13.24) | 0.1263 | 45.83 (9.13) | 34.33 (14.92) |
| Semantic Associates Test | 15.97 (0.18) | 15.17 (1.34) | 0.0009 | 15.83 (0.41) | 14.50 (1.64) |
| Sentence Reading Test | 4.94 (0.25) | 4.83 (0.39) | 0.2060 | 5.00 (0.00) | 4.67 (0.52) |
| Sentence Repetition Test | 4.41 (0.76) | 4.42 (0.67) | 0.8620 | 4.67 (0.52) | 4.17 (0.75) |
| Northwestern Anagram Test | 9.38 (1.29) | 8.83 (1.53) | 0.1268 | 9.50 (0.55) | 8.17 (1.94) |
| Word Reading Test | 29.19 (0.93) | 28.50 (2.20) | 0.1855 | 29.00 (1.67) | 28.00 (2.68) |
| Nouns and Verbs Naming Test | 0.99 (0.02) | 1.00 (0.14) | 0.9501 | 1.00 (0.00) | 0.99 (0.20) |
| Semantic Word-Picture Matching | 20.00 (0.00) | 19.58 (1.00) | 0.0203 | 20.00 (0.00) | 19.17 (1.33) |
| Memory | |||||
| Selective Reminding Test (SRT) Discriminability Index | 0.98 (0.04) | 0.87 (0.19) | 0.0126 | 0.99 (0.03) | 0.75 (0.21) |
| Selective Reminding Test (SRT) Immediate Recall^ | 56.00 (6.82) | 43.50 (19.13) | 0.0126 | 60.67 (5.72) | 26.33 (8.07) |
| Selective Reminding Test (SRT) Delayed Recall^ | 9.47 (1.72) | 6.50 (4.80) | 0.0197 | 10.67 (1.51) | 2.33 (2.58) |
| Benson Complex Figure Copy Delay^ | 12.59 (2.58) | 11.00 (5.20) | 0.0224 | 14.67 (2.34) | 7.33 (4.68) |
| Spatial Abilities | |||||
| Benson Complex Figure Copy^ | 16.19 (1.28) | 15.83 (1.34) | 0.3150 | 16.17 (1.17) | 15.50 (1.52) |
| Social Cognition | |||||
| Social Behavior Observer Checklist*# | 4.10 (4.93) | 3.60 (4.14) | 0.7992 | 2.33 (3.39) | 5.50 (4.93) |
| Social Norms Questionnaire^ | 20.13 (1.34) | 18.75 (1.82) | 0.0465 | 18.83 (2.48) | 18.67 (1.03) |
| Behavioral Inhibition Scale^* | 18.27 (4.04) | 17.50 (3.87) | 0.9475 | 17.50 (4.09) | 17.50 (4.04) |
| Interpersonal Reactivity Index – Empathic Concern (IRI-EC)^* | 27.90 (5.24) | 25.58 (5.81) | 0.4261 | 28.67 (6.47) | 22.50 (3.08) |
| Interpersonal Reactivity Index – Perspective Taking (IRI-PT)^* | 25.20 (5.96) | 17.92 (7.17) | 0.0162 | 21.67 (8.45) | 14.17 (2.79) |
| Revised Self-Monitoring Scale ^* | 47.50 (9.43) | 38.00 (16.70) | 0.0403 | 48.17 (16.57) | 27.83 (9.52) |
| Mini Mental State Examination^ | 29.63 (0.71) | 28.50 (1.93) | 0.0277 | 29.33 (1.21) | 27.67 (2.25) |
Note:
normative/adjusted data available
some controls missing specific test scores
some carriers missing specific test scores
The same mixed-effect regression was conducted with normalized scores as outcomes with and without controlling for age, gender and education. A web-based normative calculator for the NACC UDS 2.0 was used to compute z-scores of measures for which normative data was available(Shirk et al., 2011; Weintraub et al., 2009). Results were similar to the primary model and are therefore not presented. To allow qualitative comparison of group performance to clinical norms, Table 3 presents group averages of scores individually adjusted to normative data, where available (see Table 3).
Table 3:
Group performance data derived from normalized scores
| Controls (n=32) | All Carriers (n=12) | CDR=0 Carriers (n=6) | CDR=0.5 Carriers (n=6) | |
|---|---|---|---|---|
| Mean (±SD) | Mean (±SD) | Mean (±SD) | Mean (±SD) | |
| Attention & Processing | ||||
| WAIS-Digit Symbol | 0.28 (1.05) | −0.28 (0.95) | 0.09 (0.91) | −0.65 (0.91) |
| Trail Making Part A (TMTA) | −0.37 (0.55) | −1.09 (1.41) | −0.48 (0.44) | −1.69 (1.82) |
| Executive Abilities | ||||
| Trail Making Part B (TMTB)* | −0.35 (0.59) | −0.89 (1.01) | −0.56 (0.30) | −1.23 (1.37) |
| Language | ||||
| Boston Naming Test (BNT) | −0.60 (0.64) | −2.81 (2.67) | −0.73 (0.71) | −4.88 (2.20) |
| Category Fluency Animals | −0.61 (0.82) | −1.32 (1.27) | −0.35 (0.54) | −2.28 (1.01) |
| Phonemic Fluency (CFL)* | 46.44 (8.85) | 42.25 (12.06) | 47.00 (9.36) | 37.50 (13.35) |
| Memory | ||||
| Selective Reminding Test (SRT) – Immediate Recall T Score | 47.75 (10.28) | 32.47 (19.87) | 50.42 (4.34) | 14.52 (8.73) |
| Selective Reminding Test (SRT) – Delayed Recall T Score | 50.18 (7.98) | 37.62 (18.22) | 53.26 (6.16) | 21.98 (10.26) |
| Benson Complex Figure Copy Delay | 0.02 (1.07) | −0.56 (2.06) | 0.90 (1.02) | −2.01 (1.80) |
| Spatial Abilities | ||||
| Benson Complex Figure Copy | 0.61 (1.16) | 0.31 (1.20) | 0.59 (1.05) | 0.03 (1.37) |
| Social Cognition | ||||
| Social Norms Questionnaire (SNQ) | −0.20 (0.96) | −1.18 (1.30) | −1.12 (1.77) | −1.24 (0.74) |
| Behavioral Inhibition Scale (BIS)* | −0.46 (1.06) | −0.66 (1.02) | −0.66 (1.08) | −0.66 (1.06) |
| Interpersonal Reactivity Index – Empathic Concern (IRI-EC)* | 0.00 (1.07) | −0.45 (1.12) | 0.17 (1.30) | −1.07 (0.39) |
| Interpersonal Reactivity Index – Perspective Taking (IRI-PT)* | 0.18 (1.02) | −1.06 (1.27) | −0.40 (1.42) | −1.72 (0.70) |
| Revised Self-Monitoring Scale* | −1.57 (1.10) | −2.67 (1.94) | −1.49 (1.93) | −3.86 (1.11) |
| Mini Mental State Examination^ | 0.64 (0.75) | −0.25 (1.45) | 0.25 (1.13) | −0.75 (1.66) |
Note: Unless indicated otherwise, individual data points were adjusted by normative data, using a web-based calculator(Shirk et al., 2011).
some controls missing specific test scores
some carriers missing specific test scores
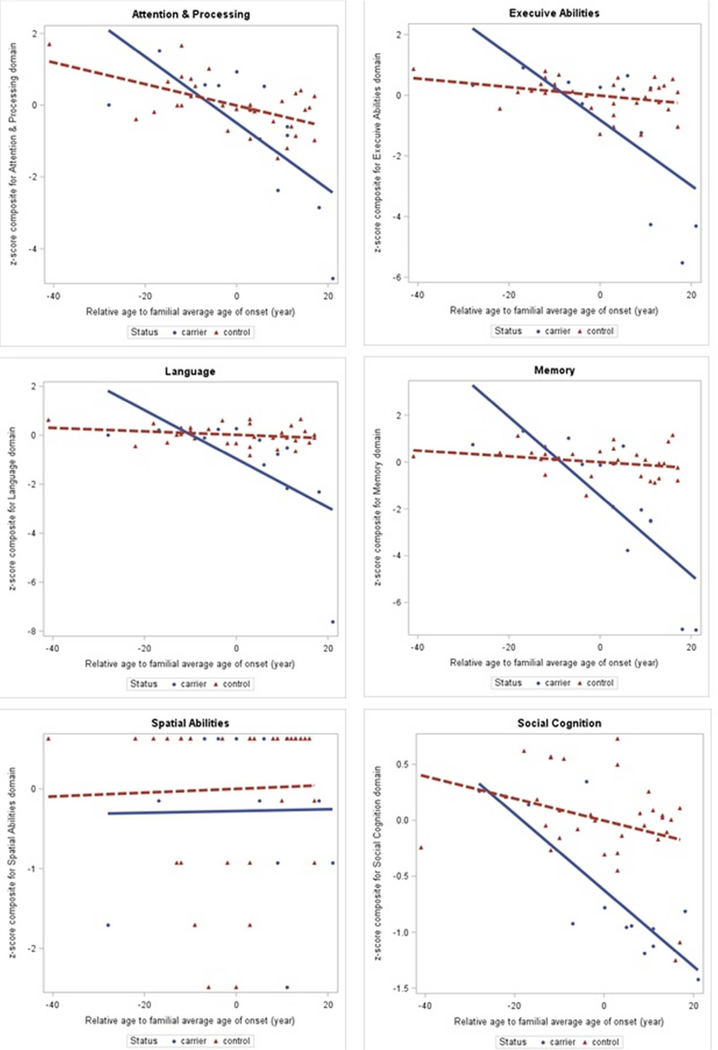
To explore the broader dimensions of cognitive changes in early disease, we performed a separate exploratory analysis, in which we calculated composite scores for each cognitive domain by averaging group performance on the individual measures within that domain, based on scores that were normalized within group against the 32 controls. Additional mixed effect models were fitted to include the interaction between mutation carrier status and subject age relative to the average familial age-of-onset, while controlling for gender and education as fixed effects, and family as a random effect. Average familial age-of-onset for each family excluded carriers enrolled in the present study, and was referenced from prior publications if available, or otherwise from subject report. The average familial age-of-onset was reported as 45 for the Exon 10 + 14 family (Lynch et al., 1994), 45 for the Exon 10 + 15 family (McCarthy et al., 2015), 49 for the Exon 10 + 16 family according to family reports, 48 for the V337M family according to family reports, 49 for the P301L family (Bird et al., 1999), and 69 according to family reports for the R406W family from which no carriers were enrolled. Characterizing carriers by their expected age-of-onset has been informative in other studies of preclinical genetic FTD (Rohrer et al., 2015). However, anecdotal reports from the families enrolled in our cohort suggest that age-of-onset can vary considerably, both intrafamilially and interfamilially, thus we applied this approach exploratorily as a secondary analysis to grouping carriers by CDR scores. Multiplicity adjustments were performed using the False Discovery Rate (FDR) method, which was selected for its power and suitability to our analysis. Findings from this analysis are reported in Table 4, and displayed in the scatterplots in Figure 1.
Table 4:
Exploratory group comparison of cohort by age relative to familial average age-of-onset
| Domain Cognitive Test | Controls (n=32) | Carriers (n=12) | p-values for interaction term in mixed models | |||||
|---|---|---|---|---|---|---|---|---|
| Composite scores | Subscores | |||||||
| Mean | SD | Mean | SD | Raw p | FDR corrected | Raw p | FDR corrected | |
| Attention & Processing | 0.00 | 0.73 | −0.69 | 1.84 | 0.0037 | 0.0056 | ||
| Digit Span | 0.00 | 1.00 | 0.19 | 1.50 | 0.2354 | 0.3040 | ||
| WAIS-Digit Symbol | 0.00 | 1.00 | −0.56 | 1.16 | 0.2005 | 0.2703 | ||
| Trail Making Part A(TMTA) | 0.00 | 1.00 | −1.70 | 3.62 | 0.0020 | 0.0077 | ||
| Executive Abilities | 0.00 | 0.58 | −1.04 | 2.28 | 0.0003 | 0.0009 | ||
| Trail Making Part B (TMTB)* | 0.00 | 1.00 | −1.25 | 2.75 | 0.0017 | 0.0074 | ||
| Frontal Assessment Battery | 0.00 | 1.00 | −1.04 | 2.15 | 0.0511 | 0.1065 | ||
| Design Fluency Total Correct# | 0.00 | 1.00 | −1.62 | 3.72 | 0.0007 | 0.0041 | ||
| Design Fluency Perseveration Distance*# | 0.00 | 1.00 | −0.92 | 1.24 | 0.1734 | 0.2560 | ||
| Design Fluency time*# | 0.00 | 1.00 | −0.14 | 1.51 | 0.6491 | 0.6939 | ||
| D-KEFS 20 Questions Total Weighted Achievement* | 0.00 | 1.00 | −0.45 | 1.23 | 0.0542 | 0.1065 | ||
| Language | 0.02 | 0.40 | −1.17 | 2.22 | 0.0005 | 0.0009 | ||
| Boston Naming Test (BNT) | 0.00 | 1.00 | −3.73 | 4.81 | <.0001 | <.0001 | ||
| Category Fluency Animals | 0.00 | 1.00 | −0.85 | 1.76 | 0.0045 | 0.0138 | ||
| Phonemic Fluency (CFL) * | 0.00 | 1.00 | −0.46 | 1.42 | 0.1263 | 0.2061 | ||
| Semantic Associates Test | 0.00 | 1.00 | −4.54 | 7.56 | 0.0026 | 0.0090 | ||
| Sentence Reading Test | 0.00 | 1.00 | −0.42 | 1.58 | 0.1933 | 0.2703 | ||
| Sentence Repetition Test | 0.00 | 1.00 | 0.01 | 0.88 | 0.5737 | 0.6351 | ||
| Northwestern Anagram Test | 0.00 | 1.00 | −0.42 | 1.19 | 0.0419 | 0.0999 | ||
| Word Reading Test | 0.00 | 1.00 | −0.74 | 2.36 | 0.1231 | 0.2061 | ||
| Nouns and Verbs Naming Test | 0.00 | 1.00 | 0.04 | 5.88 | 0.5541 | 0.6351 | ||
| Semantic Word-Picture Matching | 0.21 | 0.00 | −0.56 | 1.85 | 0.0008 | 0.0041 | ||
| Memory | 0.00 | 0.70 | −1.79 | 2.99 | <.0001 | <.0001 | ||
| Selective Reminding Test (SRT) Discriminability Index | 0.00 | 1.00 | −2.99 | 5.13 | <.0001 | 0.0007 | ||
| Selective Reminding Test (SRT) Immediate Recall | 0.00 | 1.00 | −1.72 | 2.78 | <.0001 | <.0001 | ||
| Selective Reminding Test (SRT) Delayed Recall | 0.00 | 1.00 | −1.83 | 2.81 | <.0001 | <.0001 | ||
| Benson Complex Figure Copy Delay | 0.00 | 1.00 | −0.62 | 2.02 | 0.0205 | 0.0531 | ||
| Spatial Abilities | 0.00 | 1.00 | −0.28 | 1.04 | 0.9957 | 0.9957 | ||
| Benson Complex Figure Copy | 0.00 | 1.00 | −0.28 | 1.04 | 0.9957 | 0.9957 | ||
| Social Cognition | 0.00 | 0.43 | −0.70 | 0.60 | 0.0123 | 0.0147 | ||
| Social Behavior Observer Checklist*# | 0.00 | 1.00 | −0.10 | 0.84 | 0.4472 | 0.5332 | ||
| Social Norms Questionnaire | 0.00 | 1.00 | −0.19 | 0.96 | 0.3309 | 0.4103 | ||
| Behavioral Inhibition Scale* | 0.00 | 1.00 | −1.03 | 1.36 | 0.7948 | 0.8213 | ||
| Interpersonal Reactivity Index - Empathic Concern (IRI-EC)* | 0.00 | 1.00 | −0.44 | 1.11 | 0.0550 | 0.1065 | ||
| Interpersonal Reactivity Index - Perspective Taking (IRI-PT)* | 0.00 | 1.00 | −1.22 | 1.20 | 0.0979 | 0.1785 | ||
| Revised Self-Monitoring Scale * | 0.00 | 1.00 | −1.01 | 1.77 | 0.0145 | 0.0409 | ||
| Mini Mental State Examination | 0.00 | 1.00 | −1.59 | 2.73 | 0.1598 | 0.2477 | ||
some controls missing specific test scores
some carriers missing specific test scores
Figure 1:
Scatterplots of domain composite z-scores in sample, relative to familial average age-of-onset
Results
In the primary analysis, we found that over half the variables (17 out of 31) demonstrated significant associations with mutation status. Non-carriers outperformed carriers on the Mini Mental State Examination, and also on specific measures of memory (Selective Reminding Test Discriminability Index, Immediate and Delayed Recall, and Benson Delay), executive function (Frontal Assessment Battery, Trail Making Test B, Design Fluency total correct and perseveration distance), language (Boston Naming Test, Animal Fluency, Semantic Associates Test, and Semantic Word-Picture Matching Test), social cognition (Social Norms Questionnaire, Interpersonal Reactivity Index Perspective-taking subscore, and Revised Self Monitoring Scale), and attention and processing speed (Trail Making Test A) (See Table 2). No group differences arose in the Benson Complex Figure Copy, the sole variable selected to represent spatial ability. CDR=0 carriers were the youngest subgroup studied, and perhaps for that reason, outperformed both CDR=0.5 carriers and non-carriers on many tests, though the limited sample size is insufficient for statistical analyses of this trend.
Results from the second, exploratory analysis, in which we generated composite scores for domains and considered subject age relative to average familial age-of-onset similarly found 11 of 31 measures showed significant differences between carriers and non-carriers, when corrected for multiplicity by the FDR method. Group differences were observed in composite scores of all domains, excluding spatial ability.
Discussion
The present study compared multi-domain cognitive performance in preclinical MAPT mutation carriers not yet meeting bvFTD diagnostic criteria, versus familial non-carrier controls who were stringently matched to carriers by age, sex, and education. Age-of-onset was not estimated in the primary analysis; rather, we blindly and comprehensively assessed carriers ranging from the second to sixth decades of life, to investigate how early differences are detectable. CDR=0.5 carriers meeting some but not all diagnostic criteria were assessed, to capture a spectrum ranging from pre- to early-symptomatic but subthreshold of bvFTD diagnostic criteria. Mixed effect modeling adjusted for multiplicity found group differences in 17 of 31 selected variables spanning the domains of memory, executive function, processing speed, language, and social cognition (see Table 2). In a second, exploratory analysis, 11 variables further showed significant group differences when mixed effect modeling accounted for subject age relative to familial average age-of-onset, and composite scores generated for cognitive domains showed group differences in all domains but spatial ability, for which a composite score was not calculable. These findings substantiate prior research suggesting differences are discernable in preclinical bvFTD, and extend previous studies by evaluating a comprehensive battery of tests and identifying those that detect mutation-related differences.
In the domain of social cognition, which was hypothesized to comprise some of the earliest cognitive indicators of bvFTD, specific measures that captured group differences included the Social Norms Questionnaire, the Interpersonal Reactivity Index Perspective-Taking Subscore, and the Revised Self-Monitoring Scale Total Score. The Social Norms Questionnaire gauges crystallized knowledge of social norms by having the subject rate whether specific behaviors (e.g. eating pasta with fingers, or cutting ahead of others waiting in a line) are socially acceptable(Beekly et al., 2012). In the Interpersonal Reactivity Index Perspective-Taking Subscore and the Revised Self Monitoring Scale Total Score, informants respectively rate the subject’s perception of others’ autonomous perspectives (e.g. if the subject sees there are multiple sides to topics or issues), and the subject’s ability to modulate behavior in response to social information (e.g. can the subject correctly read others’ emotions)(Davis, 1980; Lennox & Wolfe, 1984). As may be expected of a pre-clinical sample, no group differences arose in the Social Behavior Observer Checklist, an instrument rated by the examiner based on behaviors observed during interview (e.g., insensitivity, inappropriate familiarity, stimulus bound behavior). Notably, both groups performed comparably on the Behavioral Inhibition Scale and Interpersonal Reactivity Index Empathic Concern index— informant-completed measures which assess subjects’ affective response to interpersonal scenarios—suggesting that affective behavior and empathic concern may not be reliable early indicators of bvFTD (Carver & White, 1994; Davis, 1980). In contrast, previous studies have demonstrated that symptomatic bvFTD patients show impairment in both the Empathic Concern and Perspective Taking subscores of the Interpersonal Reactivity Index (Lough et al., 2006), and so it may be that these social cognitive changes become more detectable with disease progression, or perhaps that more sensitive measures are needed to detect very subtle and early changes in this limited sample. In the secondary analysis in which age relative to familial average age-of-onset was considered, only the Revised Self Monitoring Scale total score showed group differences, suggesting that this test may be sensitive to subtle preclinical changes in incipient disease.
Executive functioning was another domain hypothesized to show early differences in carriers versus noncarriers. Indeed performance on measures tapping effective mental set-shifting and cognitive flexibility, including the Trail Making Test B, Frontal Assessment Battery, and Design Fluency (total score and perseverative distance), differed between groups. Total time taken to complete Design Fluency did not differ across groups, suggesting that faster performance is not necessarily better. Individuals who complete the task quickly may do so accurately, or at the expense of repeating designs. Total score and the distance between perseverations, appear to offer more reliable information regarding the integrity of cognitive flexibility than time to completion. Relatively deficient performance on the Trail Making Test B among carriers was also evident, and may in part reflect deficits in attention and/or processing speed, given the difference observed on the Trail Making Test A across the two groups as well. Although attentional differences were not seen on other measures such as digit span, decreased relatively slower Trails A performance may reflect momentary inattention or speed variability that could potentially influence other aspects of cognitive performance even when attention appears to be grossly intact per examiner observation. Finally, it is worth pointing out that the D-KEFS Twenty Questions task, another measure of executive function placing demands on abstract thinking and efficient problem solving, did not differ between groups. In the secondary exploratory analysis, group differences were only detected in the Trail Making Test B, and Design fluency total score, providing further support for these measures’ ability to distinguish preclinical subjects. These findings may be useful in projecting the evolution of executive dysfunction, perhaps from more basic to more complex abilities, over the course of bvFTD.
Within language profiles, group differences emerged only on measures of semantic knowledge including word picture matching, confrontation naming, semantic association, and category fluency, a pattern which was also observed in the secondary exploratory analysis accounting for subject age relative to familial average age-ofonset. Though previous studies of bvFTD have reported changes in verbal fluency, no consistent trend has emerged: most studies found changes in phonemic fluency only, or in both phonemic and category fluency(Alberici et al., 2004; Ferman et al., 2003; Jiskoot et al., 2016; Rohrer et al., 2015). In our cohort, the carriers’ verbal fluency profiles, characterised by relatively impaired semantic fluency with intact phonemic fluency, unexpectedly paralleled a dichotomy traditionally associated with Alzheimer’s disease (AD) and the semantic variant of FTD(Rascovsky, Salmon, Hansen, Thal, & Galasko, 2007). Historically, this “fluency split” is used in part to differentiate AD from bvFTD, consistent with a report by Rascovsky and colleagues’ (2007) showing distinct fluency patterns in autopsy-confirmed bvFTD versus AD patients, with the former having worse phonemic than category fluency, and the latter exhibiting the converse pattern, or comparably impaired fluencies(Rascovsky, Salmon, et al., 2007). In Rascovsky et al., (2007), patients with the semantic variant of FTD showed a similar fluency profile to those with AD, as would be expected based on the disproportionate compromise to temporal lobe regions responsible for supporting semantic networks in both of these illnesses(Rascovsky, Salmon, et al., 2007). It thus appears our cohort manifests elements of impairment historically associated with the semantic variant of FTD. Longitudinal evaluation will elucidate whether the fluency profile evolves with disease progression, and eventually conforms to the profile traditionally associated with bvFTD, the phenotype previously observed in this cohort. Further investigation should also be carried out to explore whether specific mutational variants are associated with particular profiles of fluency impairment. Finally, neuroimaging should be undertaken in conjunction to correlate dichotomous fluency impairment with structural or functional deficits in the regions which support these functions.
Perhaps most notable in the current findings is that group differences arose in all measures of memory assessed in the primary analysis, and 3 of 4 measures in the secondary analysis. The group difference in the SRT Discriminability Index, a recognition memory measure hypothesized to measure information storage rather than retrieval, is intriguing given that this component of memory relies largely on integrity of the hippocampus, a structure not traditionally considered vulnerable to early bvFTD (Beyer et al., 2013; Deweer et al., 1995; Manns, Hopkins, & Squire, 2003). Indeed, episodic memory, and memory storage in particular, has typically been described as being spared in bvFTD (Hodges, 2001). Although Hornberger and colleagues (2010) described memory storage deficits in bvFTD (Hornberger, Piguet, Graham, Nestor, & Hodges, 2010), and memory impairment can be an early symptom in a minority of pathologically verified bvFTD cases, (Hornberger et al., 2010; Neary et al., 1998), these memory deficits may be secondary to deficits in attention, executive function, and/or behavior in the context of symptomatic disease. Indeed, when impaired memory performance does occur in bvFTD, it is generally attributed to impaired retrieval strategies (Hodges, 2001) or theorized to reflect regulatory deficits in attention and effective implementation of learning and retrieval strategies, rather than a primary amnestic syndrome (Neary et al., 1998).
Such an explanation is unlikely to account for group differences in recognition memory seen in the present cohort, however, in whom auditory attention and behavior were relatively intact. This memory difference detected in our prodromal cohort may eventually become entangled with or overtaken by a primarily behavioral presentation as symptoms progress. Alternatively, it may also be that the cognitive profile of bvFTD evolves throughout the disease course, and that amnestic symptoms are present early on but not so much later. Whether these group differences in memory measures persist and how they evolve, as our carriers pass into the threshold of diagnosable disease and progression will be the topic of anticipated examination in longitudinal evaluation slated for 24 and 48 months following the baseline assessment analyzed here.
Noteworthy though, is that the observed weakness in memory need not necessarily equate to functional impairment – that is, carriers could perform more poorly than non-carriers in memory measures, but still rank within clinically normative standards, and thus the observed relative reduction may only be detectable across longitudinal evaluation, or, by our study design, when carriers are juxtaposed to matched controls. Our study design enables detection of subclinical, but nonetheless important changes in early bvFTD, which are easily overlooked in studies designed to investigate clinical deficits and impairment.Nevertheless, from a clinical standpoint, current findings highlight the point that early deficits in memory storage need not imply the presence of an Alzheimer’s based amnestic mild cognitive impairment, and underscore the importance of comprehensive clinical assessment across a range of cognitive domains.
Overall, the present study identified specific measures, which captured differences between pre- and earlysymptomatic MAPT carriers, and matched controls. Our cohort could benefit from additional carriers, but nevertheless, our blinded comprehensive assessment and usage of stringently matched familial controls optimizes detection of differences in a rare and valuable cohort with incipient bvFTD. Though the SRT recognition measure used in this study is an experimental measure not yet validated externally, it utilizes yes/no identification of target words amongst a list of linguistically matched items, and is thereby designed to be more rigorous than its traditional counterpart. Nonetheless, and as expected, performance of the control group at 98% discriminability suggests that cognitively healthy individuals are able to decipher between new and old words with very high accuracy. Group differences identified in this cohort replicate some but not all findings from prior studies, as is to be expected across studies of varying size, composition and symptomatology. Some tests consistently emerge as capturing differences, including the Trail Making Tests A & B, the Category fluency test, and the Boston Naming Test, suggesting that these may pose utility in detecting incipient bvFTD. Our findings affirm the specific tests and broader cognitive domains that undergo changes in preclinical bvFTD. Furthermore and importantly, some unexpected results arise in our findings, which challenge certain longstanding conceptualizations of bvFTD. Future research can extend this work by comprehensively assessing larger samples of preclinical carriers, to elucidate whether cognitive decline in bvFTD progresses differently by factors including specific mutation, gender and education, or symptomatic stage.
Table 1:
Sample demographic characteristics by group
| Controls (n=32) | All Carriers (n=12) | CDR=0 Carriers (n=6) | CDR=0.5 Carriers (n=6) | |||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Females | 22 | 68.75 | 8 | 66.67 | 4 | 66.67 | 4 | 66.67 |
| Males | 10 | 31.25 | 4 | 33.33 | 2 | 33.33 | 2 | 33.33 |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Age (years) | 45.75 | 12.04 | 48.75 | 13.55 | 38.83 | 11.82 | 58.67 | 5.32 |
| Education (years) | 15.03 | 2.31 | 15.25 | 2.14 | 15.33 | 2.07 | 15.17 | 2.40 |
Acknowledgements
We thank all our participants, without whom this work would not have been possible. Data presented herein was collected at the Irving Institute for Clinical and Translational Research, a resource supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1 TR000040, formerly the National Center for Research Resources, Grant Number UL1 RR024156. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The NACC database is funded by NIA/NIH Grant U01 AG016976. Statistical analyses were supported by the National Institute on Aging through grant 5K01AG051348-02. No authors have potential conflicts of interest to disclose.
Funding
This study was supported by the Association for Frontotemporal Degeneration and the National Institute of Neurological Disorders and Stroke (NINDS) at the National Institute of Health (NIH) (5R01NS076837-03).
References
- Alberici A, Gobbo C, Panzacchi A, Nicosia F, Ghidoni R, Benussi L, . . . Binetti G. (2004). Frontotemporal dementia: impact of P301L tau mutation on a healthy carrier. J Neurol Neurosurg Psychiatry, 75(11), 1607–1610. doi: 10.1136/jnnp.2003.021295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beekly D, Monsell S, Besser L, Robichaud E, Knopman D, & Kukull W (2012). The NACC FTLD Module Data. Dementia and Geriatric Cognitive Disorders, 33, 109–110. [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the royal statistical society. Series B (Methodological), 289–300. [Google Scholar]
- Beyer MK, Bronnick KS, Hwang KS, Bergsland N, Tysnes OB, Larsen JP, . . . Apostolova LG (2013). Verbal memory is associated with structural hippocampal changes in newly diagnosed Parkinson’s disease. J Neurol Neurosurg Psychiatry, 84(1), 23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird TD, Nochlin D, Poorkaj P, Cherrier M, Kaye J, Payami H, . . . Schellenberg GD. (1999). A clinical pathological comparison of three families with frontotemporal dementia and identical mutations in the tau gene (P301L). Brain, 122 (Pt 4), 741–756. [DOI] [PubMed] [Google Scholar]
- Boeve BF, & Hutton M (2008). Refining frontotemporal dementia with parkinsonism linked to chromosome 17: introducing FTDP-17 (MAPT) and FTDP-17 (PGRN). Archives of Neurology, 65(4), 460–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boxer AL, & Miller BL (2005). Clinical features of frontotemporal dementia. Alzheimer Dis Assoc Disord, 19 Suppl 1, S3–6. [DOI] [PubMed] [Google Scholar]
- Brandt R, Hundelt M, & Shahani N (2005). Tau alteration and neuronal degeneration in tauopathies: mechanisms and models. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease, 1739(2), 331–354. [DOI] [PubMed] [Google Scholar]
- Buschke H (1973). Selective reminding for analysis of memory and learning. Journal of Verbal Learning and Verbal Behavior, 12(5), 543–550. [Google Scholar]
- Carver CS, & White TL (1994). Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS Scales. Journal of Personality and Social Psychology, 67(2), 319. [Google Scholar]
- Davis MH (1980). Interpersonal reactivity index: Edwin Mellen Press. [Google Scholar]
- Delis DC, Kaplan E, & Kramer JH (2001). Delis-Kaplan executive function system (D-KEFS): Psychological Corporation. [Google Scholar]
- Deweer B, Lehericy S, Pillon B, Baulac M, Chiras J, Marsault C, . . . Dubois B (1995). Memory disorders in probable Alzheimer’s disease: the role of hippocampal atrophy as shown with MRI. Journal of Neurology, Neurosurgery & Psychiatry, 58(5), 590–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubois B, Slachevsky A, Litvan I, & Pillon B (2000). The FAB A frontal assessment battery at bedside. Neurology, 55(11), 1621–1626. [DOI] [PubMed] [Google Scholar]
- Ferman TJ, McRae C, Arvanitakis Z, Tsuboi Y, Vo A, & Wszolek ZK (2003). Early and presymptomatic neuropsychological dysfunction in the PPND family with the N279K tau mutation. Parkinsonism & related disorders, 9(5), 265–270. [DOI] [PubMed] [Google Scholar]
- Ghetti B, Oblak AL, Boeve BF, Johnson KA, Dickerson BC, & Goedert M (2015). Invited review: Frontotemporal dementia caused by microtubule-associated protein tau gene (MAPT) mutations: a chameleon for neuropathology and neuroimaging. Neuropathol Appl Neurobiol, 41(1), 24–46. doi: 10.1111/nan.12213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glosser G, & Goodglass H (1990). Disorders in executive control functions among aphasic and other braindamaged patients. Journal of Clinical and experimental Neuropsychology, 12(4), 485–501. [DOI] [PubMed] [Google Scholar]
- Goedert M, Crowther RA, & Spillantini MG (1998). Tau mutations cause frontotemporal dementias. Neuron, 21(5), 955–958. [DOI] [PubMed] [Google Scholar]
- Hodges JR (2001). Frontotemporal dementia (Pick’s disease): clinical features and assessment. Neurology, 56(suppl 4), S6–S10. [DOI] [PubMed] [Google Scholar]
- Hornberger M, Piguet O, Graham A, Nestor P, & Hodges J (2010). How preserved is episodic memory in behavioral variant frontotemporal dementia? Neurology, 74(6), 472–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes CP, Berg L, Danziger WL, Coben LA, & Martin R (1982). A new clinical scale for the staging of dementia. The British journal of psychiatry, 140(6), 566–572. [DOI] [PubMed] [Google Scholar]
- Jiskoot LC, Dopper EG, den Heijer T, Timman R, van Minkelen R, van Swieten JC, & Papma JM (2016). Presymptomatic cognitive decline in familial frontotemporal dementia: A longitudinal study. Neurology, 87(4), 384–391. [DOI] [PubMed] [Google Scholar]
- Lennox RD, & Wolfe RN (1984). Revision of the self-monitoring scale. [DOI] [PubMed]
- Lough S, Kipps CM, Treise C, Watson P, Blair JR, & Hodges JR. (2006). Social reasoning, emotion and empathy in frontotemporal dementia. Neuropsychologia, 44(6), 950–958. [DOI] [PubMed] [Google Scholar]
- Lynch T, Sano M, Marder K, Bell K, Foster N, Defending R, . . . Fahn S (1994). Clinical characteristics of a family with chromosome 17‐linked disinhibition‐dementia‐parkinsonismamyotrophy complex. Neurology, 44(10), 1878–1878. [DOI] [PubMed] [Google Scholar]
- Manns JR, Hopkins RO, & Squire LR (2003). Semantic memory and the human hippocampus. Neuron, 38(1), 127–133. [DOI] [PubMed] [Google Scholar]
- McCarthy A, Lonergan R, Olszewska DA, O’Dowd S, Cummins G, Magennis B, . . . Lynch T. (2015). Closing the tau loop: the missing tau mutation. Brain, 138(Pt 10), 3100–3109. doi: 10.1093/brain/awv234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyoshi M, Shinotoh H, Wszolek ZK, Strongosky AJ, Shimada H, Arakawa R, . . . Fukushi K. (2010). In vivo detection of neuropathologic changes in presymptomatic MAPT mutation carriers: a PET and MRI study. Parkinsonism & related disorders, 16(6), 404–408. [DOI] [PubMed] [Google Scholar]
- Neary D, Snowden J, & Mann D (2005). Frontotemporal dementia. The Lancet Neurology, 4(11), 771–780. [DOI] [PubMed] [Google Scholar]
- Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S. a., . . . Albert M. (1998). Frontotemporal lobar degeneration: A consensus on clinical diagnostic criteria. Neurology, 51(6), 15461554. [DOI] [PubMed] [Google Scholar]
- Rascovsky K, Hodges JR, Kipps CM, Johnson JK, Seeley WW, Mendez MF, . . . Salmon DP. (2007). Diagnostic criteria for the behavioral variant of frontotemporal dementia (bvFTD): current limitations and future directions. Alzheimer Disease & Associated Disorders, 21(4), S14–S18. [DOI] [PubMed] [Google Scholar]
- Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, . . . Onyike CU. (2011). Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain, 134(9), 2456–2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rascovsky K, Salmon DP, Hansen LA, Thal LJ, & Galasko D (2007). Disparate letter and semantic category fluency deficits in autopsy-confirmed frontotemporal dementia and Alzheimer’s disease. Neuropsychology, 21(1), 20. [DOI] [PubMed] [Google Scholar]
- Rohrer JD, Nicholas JM, Cash DM, van Swieten J, Dopper E, Jiskoot L, . . . Clegg S. (2015). Presymptomatic cognitive and neuroanatomical changes in genetic frontotemporal dementia in the Genetic Frontotemporal dementia Initiative (GENFI) study: a cross-sectional analysis. The Lancet Neurology, 14(3), 253–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeley WW, Crawford R, Rascovsky K, Kramer JH, Weiner M, Miller BL, & Gorno-Tempini ML (2008). Frontal paralimbic network atrophy in very mild behavioral variant frontotemporal dementia. Archives of Neurology, 65(2), 249–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirk SD, Mitchell MB, Shaughnessy LW, Sherman JC, Locascio JJ, Weintraub S, & Atri A (2011). A web-based normative calculator for the uniform data set (UDS) neuropsychological test battery. Alzheimer’s research & therapy, 3(6), 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snowden JS, Neary D, & Mann DM (2002). Frontotemporal dementia. The British journal of psychiatry, 180(2), 140–143. [DOI] [PubMed] [Google Scholar]
- Spillantini MG, Bird TD, & Ghetti B (1998). Frontotemporal dementia and Parkinsonism linked to chromosome 17: a new group of tauopathies. Brain pathology, 8(2), 387–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Swieten J, Stevens M, Rosso S, Rizzu P, Joosse M, De Koning I, . . . Niermeijer M. (1999). Phenotypic variation in hereditary frontotemporal dementia with tau mutations. Annals of neurology, 46(4), 617–626. [DOI] [PubMed] [Google Scholar]
- Weintraub S, Salmon D, Mercaldo N, Ferris S, Graff-Radford NR, Chui H, . . . Galasko D. (2009). The Alzheimer’s disease centers’ uniform data set (UDS): The neuropsychological test battery. Alzheimer disease and associated disorders, 23(2), 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittenberg D, Possin KL, Rascovsky K, Rankin KP, Miller BL, & Kramer JH (2008). The early neuropsychological and behavioral characteristics of frontotemporal dementia. Neuropsychology review, 18(1), 91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]