Abstract
Elevated blood pressure is the leading cause of death worldwide; however, treatment and control rates for hypertension are low. Here, we analyze the relationship between physician and nurse density and hypertension treatment rates worldwide.
Data on hypertension treatment rates were collected from the STEPwise approach to Surveillance country reports, individual studies resulting from a PubMed search for articles published between 1990 and 2010, and manual search of the reference lists of extracted studies. Data on health care worker density were obtained from the Global Atlas of the Health Workforce. We controlled for a variety of variables related to population characteristics and access to health care, data obtained from the World Bank, World Development Indicators, United Nations, and World Health Organization. We used clustering of standard errors at the country level.
Full data were available for 154 hypertension treatment rate values representing 68 countries between 1990–2010. Hypertension treatment rate ranged from 3.4% to 82.5%, with higher treatment rates associated with higher income classification. Physician and nurse/midwife generally increased with income classification. Total health care worker density was significantly associated with hypertension treatment rate in the unadjusted model (p < 0.001); however, only nurse density remained significant in the fully adjusted model (p = 0.050).
These analyses suggest that nurse density, not physician density, explains most of the relationship with hypertension treatment rate, and remains significant even after adjusting for other independent variables. These results have important implications for health policy, health system design, and program implementation.
Keywords: Hypertension, Human Resources for Health, LMICs, Treatment Rates, Nurse Density
Introduction
The burden of cardiovascular disease (CVD) continues to rise globally and its increase is not isolated to countries of particular income levels, geographical regions, or social conditions.1 Elevated blood pressure, a major risk factor for CVD,2,3 is the leading cause of death worldwide.4 Treatment for hypertension is well identified and effective.5 The challenge, however, is that treatment and control rates are low worldwide.6,7 Institutional and economic barriers to getting treatment to the individuals who need it are complex, and while some are shared across countries, others vary with institutional aspects of health care delivery and health insurance status across countries.8,9
One factor that may affect hypertension treatment rates is the density of the health care workforce—specifically physicians and nurses—within a country. Health care worker density has been shown to be favorably associated with vaccination rates10 and overall disability-adjusted life-years.11 In addition, the relationship between health care worker density and maternal, infant, and child mortality has been studied, with no clear consensus on the relationship between health care worker density and health outcomes. More recent studies indicate that health care worker density is associated with improved health outcomes,12–14 while other older studies have demonstrated either neutral15,16 or negative associations.17
While there has been more recent interest in investigating the relationship between health care worker density and non-communicable disease (NCD) (including CVD and hypertension) outcomes, there is no consensus regarding the direction or strength of the relationship. An analysis of the relationship between health care worker density (including physicians, nurses, and others) and CVD outcomes reported that a univariate analysis revealed that health care worker density is associated with better CVD outcomes, although a multivariable analysis yielded the opposite relationship.18 Another study reported no significant relationship between physician density and medical guideline adherence (including for CVD) in Germany.19
Current estimates of global health care worker shortages have largely not taken into account the human resource requirements for managing NCDs. In particular, the relationship between health care worker density and hypertension treatment rates is unknown. Recognizing this gap in the literature, and recognizing the growing importance of CVD, in this study we analyze the relationship between physician and nurse/midwife density and hypertension treatment rates, across countries of all World Bank income classifications.20
Methods
All data were extracted from publicly available databases and publicly accessible publications. Analytic methods will be made available to researchers upon formal request to the authors.
Choice of Variables
Our dependent variable was hypertension treatment rate, defined as the percentage of hypertensive individuals on treatment. Hypertension was defined as systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg or self-reported current use of BP-lowering medication. Hypertension treatment was defined as self-reported current use of antihypertensive medication.
We used three measures of health care worker density. First, an aggregate measure was derived by summing physician and nurse/midwife density per 1000 population. We also disaggregated physician and nurse densities. We limited our analysis to these cadres of health care workers since most hypertension management, treatment decisions, and prescription issuances are completed by physicians or nurses.21,22
To account for differences in population characteristics and access to health care across countries, we adjusted for the following country-level variables: gross domestic product (GDP) per capita, purchasing power parity (PPP; current international $), private health expenditure (% of GDP), land area, population, hospital beds, rural access to an improved water source (% of rural population with access), and disability-adjusted life year (DALY) estimates for 2004. PPP-adjusted GDP per capita was used as a measure of the general level of resources available in the country. Access to an improved water source (% of rural population with access) was also included as a measure of access to resources and poverty. Private health expenditure as percentage of GDP was included as a measure of private health expense burden. Land area likely impacts the geographic density of health care workers as well as the distance from patients to health care worker; therefore, it was included as it potentially influences treatment rates. Hospital beds per 1000 population was included as an indicator of health system resource availability. DALYs for infectious and parasitic diseases (per 100,000 population, age-standardized, 2004 estimates) were used to control for the potential impact of morbidity from communicable diseases.
Data sources
Data on hypertension treatment rates were collected from the World Health Organization (WHO) STEPwise approach to Surveillance (STEPS) country reports,23 individual studies resulting from a PubMed search for articles published between 1990 and 2010 using the key words “prevalence AND awareness AND treatment AND control AND (hypertension OR high blood pressure),” and a manual search of the reference lists from the extracted studies (full list of references available in the Appendix). A study was included if it contained information on country-specific hypertension treatment rate. The WHO STEPS data were obtained from surveys that follow a standardized framework for collecting, analyzing, and reporting data on NCD risk factors in WHO member countries.23
Data on health care worker density (physicians and nurses) were obtained from the WHO Global Atlas of the Health Workforce.24 Data for the other independent variables were obtained from the following sources: the World Development Indicators for gross domestic product (GDP) per person in international dollars at purchasing power parity (PPP$), private health expenditure as a percentage of GDP, land area, hospital beds per 1000 population, and access to an improved water source (% of rural population);25 the United Nations’ World Population Prospects: The 2010 Revision for population estimates;26 and the WHO database for DALYs for infectious and parasitic diseases (per 100,000 population, age-standardized).27
The dataset for our analysis was constructed by matching the country and year of our dependent and independent variables, within a +/− five-year window around the year of the hypertension treatment rate data. The DALYs data were obtained from the 2004 WHO estimates and thus did not conform to the +/− five-year criterion due to data availability limitation. World Bank income classification for each country was aligned with the year of hypertension treatment rate data for that country. In total, our dataset included 154 observations, representing 68 countries over the period 1990–2010.
Statistical Procedures
In order to compare data from the STEPS reports and individual studies collected from our PubMed search, we defined treatment of hypertension as self-reported current use of antihypertensive medication. To create our dependent variable, the rate of hypertension treatment, the number of people reporting hypertension treatment was divided by the total number of study participants with hypertension.
All regressions were estimated using a logistic-logarithmic functional form, similar to the analytic approach previously utilized to assess the relationship between health care worker density and vaccination coverage.10 The logistic form of the dependent variable reflects the boundedness of hypertension treatment rate between 0% and 100%, which in turn prevents predicted values from falling below 0% or exceeding 100%. The logarithmic form of the independent variables allows for the following interpretation of their estimated coefficients (β): a 1% increase in the independent variable corresponds to a β% change in the sum of the percentage increase in the level of the dependent variable and the percentage reduction in the shortfall from the upper bound of 100%.10,12 One exception to this is the “access to an improved water source” variable, for which a logit transformation was performed, as the variable is a proportion and is bounded by 0 and 1. All regressions used clustering of standard errors at the country level to control for possible correlation of error terms within countries.
We report the results of three regression analyses with hypertension treatment rate as the dependent variable, while controlling for GDP per capita, PPP (current international $), health expenditure, private (% of GDP), land area, population, hospital beds, access to an improved water source, rural (% of rural population with access), and DALYs estimates for 2004. In the first analysis, hypertension treatment rate was regressed against aggregate combined physician and nurse density. In the second analysis, separate models were used to regress hypertension treatment rate against physician and nurse densities, respectively. In the third analysis, hypertension treatment rate was regressed against disaggregate physician and nurse densities in a single model. We formally tested for interaction by World Bank income classification category. We also conducted sensitivity analyses by performing separate regressions for the studies between 1990–1999 and 2000–2010, as well as separate regressions for studies conducted in each of the World Bank income classification categories. Stata version 11.0 was used to perform the analyses.
Results
Hypertension treatment data were obtained from 28 WHO STEPS reports and 41 individual studies. Health care worker density and treatment data were available from 174 country and treatment data combinations, spanning 84 countries and all World Bank income classification categories. However, full data, including all independent variables, were available for 154 of these, representing 68 countries, over the period 1990–2010 (Table 1).
Table 1.
Country-years and number of observations by country income classification. Numbers in parentheses represent the number of studies from that country in that particular year.
| High Income (n = 65) | ||
| Country | # of Studies | Years of Treatment Data |
| Australia | 1 | 1994 |
| Belgium | 1 | 1992 |
| Canada | 5 | 1992, 1995, 2002, 2009(2) |
| Czech Republic | 1 | 2008 |
| Denmark | 3 | 1992, 1998, 2004 |
| Finland | 4 | 1992(3), 2005 |
| France | 2 | 1998, 2006 |
| Germany | 6 | 1992, 1995(3), 2001(2) |
| Greece | 6 | 1997, 1998, 2001(2), 2002, 2004 |
| Italy | 2 | 1994(2) |
| Japan | 1 | 1995 |
| Korea, Rep. | 2 | 2001(2) |
| Kuwait | 1 | 2008 |
| Netherlands | 3 | 2003, 2004(2) |
| New Zealand | 1 | 1994 |
| Portugal | 2 | 2003(2) |
| Saudi Arabia | 1 | 2005 |
| Spain | 3 | 1990, 1996, 2004 |
| Sweden | 3 | 1994, 1996 |
| Switzerland | 1 | 1993 |
| United Kingdom | 8 | 1995, 1998(2), 2003(4), 2006, |
| United States of America | 7 | 1990, 1994, 2000(2), 2003, 2004, 2005 |
| United Arab Emirates | 1 | 2009 |
| Upper Middle Income (n = 26) | ||
| Country | # of Studies | Years of Treatment Data |
| Argentina | 1 | 2009 |
| Barbados | 1 | 1996 |
| Botswana | 1 | 2007 |
| Brazil | 1 | 2009 |
| Chile | 3 | 2004(2) |
| China | 1 | 2010 |
| Colombia | 1 | 2009 |
| Czech Republic | 3 | 2001(3) |
| Gabon | 1 | 2003 |
| Iran, Islamic Rep. | 1 | 2009 |
| Korea, Rep. | 1 | 2000 |
| Lebanon | 1 | 2008 |
| Malaysia | 4 | 1996(2), 2004 |
| Mexico | 3 | 1993, 2000, 2002 |
| Romania | 1 | 2005 |
| St. Lucia | 1 | 1996 |
| Turkey | 1 | 2009 |
| Lower Middle Income (n = 30) | ||
| Country | # of Studies | Years of Treatment Data |
| China | 8 | 1999, 2001(4), 2002(2), 2009 |
| Egypt, Arab Rep. | 1 | 2005 |
| Fiji | 1 | 2002 |
| Iran, Islamic Rep. | 1 | 2005 |
| Iraq | 2 | 2003, 2006 |
| Maldives | 1 | 2004 |
| Mongolia | 1 | 2009 |
| Russian Federation | 2 | 2005(2) |
| Thailand | 2 | 2003, 2004 |
| Tunisia | 1 | 2001 |
| Turkey | 4 | 1995, 1999, 2003(2) |
| Venezuela, RB | 1 | 1996 |
| India | 3 | 2007(2), 2009 |
| Pakistan | 1 | 2009 |
| Micronesia | 1 | 2002 |
| Low Income (n = 33) | ||
| Country | # of Studies | Years of Treatment Data |
| Bangladesh | 1 | 2009 |
| Benin | 1 | 2007 |
| Cambodia | 1 | 2010 |
| Cameroon | 1 | 2004 |
| China | 3 | 1993, 1994, 1998 |
| Egypt, Arab Rep. | 1 | 1991 |
| Eritrea | 1 | 2004 |
| Ghana | 5 | 2001, 2002, 2004(3) |
| India | 6 | 1999, 2000, 2002(2), 2004, 2005 |
| Lao PDR | 1 | 2008 |
| Madagascar | 1 | 2005 |
| Malawi | 1 | 2009 |
| Mauritania | 1 | 2007 |
| Mongolia | 1 | 2006 |
| Mozambique | 1 | 2005 |
| Nepal | 2 | 2003, 2005 |
| Nigeria | 1 | 2003 |
| Sierra Leone | 1 | 2009 |
| Solomon Islands | 1 | 2006 |
| Vietnam | 1 | 2008 |
| Zambia | 1 | 2008 |
Hypertension treatment rate ranged from 3.4% to 82.5% (Table 2). Mean hypertension treatment rate was 34.5% overall, with higher mean treatment rates observed as income classification increased from low- to high-income. Physician and nurse density varied widely, but generally increased as income classification increased.
Table 2.
Summary statistics of published hypertension treatment rate and health care worker density data (per 1000 population) by country income classification.
| High-Income (n = 65) | ||||
| Variable | Mean | Std. Dev. | Min | Max |
| Treatment Rate | 38.9 | 18.3 | 11.1 | 82.5 |
| Aggregate Physician and Nurse Density | 11.46 | 3.01 | 3.50 | 18.41 |
| Physician Density | 3.03 | 0.92 | 1.37 | 4.91 |
| Nurse Density | 8.43 | 3.01 | 1.93 | 14.41 |
| Upper-Middle-Income (n = 26) | ||||
| Variable | Mean | Std. Dev. | Min | Max |
| Treatment Rate | 35.2 | 20.2 | 10.7 | 79.5 |
| Aggregate Physician and Nurse Density | 4.69 | 3.29 | 1.72 | 12.41 |
| Physician Density | 1.86 | 1.36 | 0.29 | 6.42 |
| Nurse Density | 2.83 | 2.59 | 0.48 | 8.94 |
| Lower-Middle-Income (n = 30) | ||||
| Variable | Mean | Std. Dev. | Min | Max |
| Treatment Rate | 30.9 | 16.2 | 3.4 | 69.5 |
| Aggregate Physician and Nurse Density | 3.56 | 2.80 | 1.16 | 12.79 |
| Physician Density | 1.36 | 0.98 | 0.30 | 4.26 |
| Nurse Density | 2.20 | 1.93 | 0.38 | 8.53 |
| Low-Income (n = 33) | ||||
| Variable | Mean | Std. Dev. | Min | Max |
| Treatment Rate | 28.5 | 16.6 | 5.7 | 74.2 |
| Aggregate Physician and Nurse Density | 1.58 | 1.32 | 0.19 | 6.26 |
| Physician Density | 0.53 | 0.67 | 0.02 | 2.76 |
| Nurse Density | 1.04 | 0.73 | 0.17 | 3.50 |
| Overall (n = 154) | ||||
| Variable | Mean | Std. Dev. | Min | Max |
| Treatment Rate | 34.5 | 18.2 | 3.4 | 82.5 |
| Aggregate Physician and Nurse Density | 6.66 | 5.03 | 0.19 | 18.41 |
| Physician Density | 1.97 | 1.39 | 0.02 | 6.42 |
| Nurse Density | 4.69 | 4.04 | 0.17 | 14.41 |
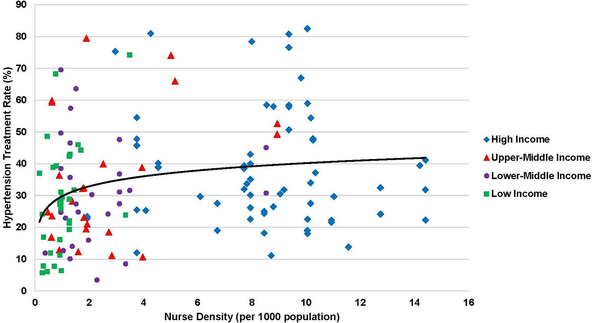
As total health care worker density (physician and nurse) increased, hypertension treatment rates generally tended to increase as well, although there was notable variation in the scatterplot (Supplemental Figure, Online Supplement). Total health care worker density was significantly associated with hypertension treatment rate in the unadjusted model, and nearly significant at the 0.05 level in the fully adjusted model (Table 3). In the separate regressions, both physician and nurse density were significantly associated with hypertension treatment rate in the unadjusted model; however, only nurse density remained significant in the fully adjusted model (Table 3, Figure). In the disaggregated model, only nurse density was significantly associated with hypertension treatment rate, in both the adjusted and unadjusted models. Taken together, these analyses suggest that nurse density, not physician density, explains most of the relationship between health care worker density and hypertension treatment rate. This relationship remains significant even after adjusting for all of the other independent variables listed above. Full multivariable regression results for all four models are presented in the Supplemental Table, Online Supplement.
Table 3.
Logistic-logarithmic regression results.
| Model | Unadjusted (n = 154) | Adjusted (n = 154) | ||
|---|---|---|---|---|
| β (CI) | p-value | β (CI) | p-value | |
| Total density (aggregate physician and nurse density) | 0.27 (0.13, 0.41) | < 0.001 | 0.33 (−0.10, 0.76) | 0.133 |
| Physician density (disaggregate) | 0.03 (−0.15, 0.20) | 0.740 | −0.07 (−0.41, 0.27) | 0.678 |
| Nurse (disaggregate) | 0.22 (0.04, 0.42) | 0.020 | 0.30 (0.00, 0.60) | 0.050 |
| Physician density (separate regression) |
0.18 (0.06, 0.30) | 0.004 | −0.03 (−0.36, 0.30) | 0.849 |
| Nurse Density (separate regression) |
0.25 (0.12, 0.38) | < 0.001 | 0.29 (−0.01, 0.58) | 0.055 |
Figure.
Relationship between nurse density and hypertension treatment rates worldwide, with countries of different income classification indicated. Solid curve is derived from the fully adjusted model.
Sensitivity analyses for year of publication suggested that studies conducted between 2000 and 2010, as compared to those conducted between 1990 and 1999, yielded results consistent with the overall results presented above, although it is difficult to arrive at a definitive conclusion due to small numbers. Similarly, low- and lower-middle-income countries appeared to have nurse density-hypertension treatment rate relationships that were consistent with the overall results, but the small numbers in the stratified analyses restrict any definitive conclusion (Supplemental Table, Online Supplement).
Discussion
In our worldwide econometric analysis of the relationship between hypertension treatment rates and health care worker density, we report that hypertension treatment rates vary widely, health care worker density rates also vary widely, and health care worker density was significantly associated with hypertension treatment. Notably, our approach of aggregating and disaggregating physicians and nurses allowed us to highlight that nurse density, not physician density, appears to explain most of the relationship between health care worker density and hypertension treatment rate. The relationship between nurse density and hypertension treatment rate remained statistically significant after adjusting for several potential confounder variables.
The relationship between health care worker density and NCDs has not been well studied, and examples from the literature are limited.28 In fact, to the best of our knowledge, this is the first report examining the relationship between health care worker density and hypertension treatment rates using worldwide data. Given the health workforce shortage worldwide, this is an important first step in the ultimate goal of aligning disease burden with human resources for health.
One notable finding from our study is that nurse density, not physician density, was more strongly associated with hypertension treatment rate. This is striking because, in many parts of the world, only physicians and clinicians, not nurses, are authorized to prescribe anti-hypertensive medications.29 The nurse’s role in hypertension care, in contrast, has generally been limited to enhancing self-management strategies by educating and counseling the patient about medication adherence and lifestyle modification.30,31 It is possible, however, that even in countries or regions that do not allow nurses to treat hypertension directly, the availability of nurses to work with physicians may enable physicians to shift other responsibilities, which may allow them to focus more time and effort on hypertension management, thus contributing to higher hypertension treatment rates. It is also possible that the presence of other cadres of health worker, such as pharmacists, could be confounding the observed results. Unfortunately, data regarding pharmacist density were not as routinely available as physician or nurse density. Therefore, this potential hypothesis was not able to be tested.
The relationship between health care worker density and health outcomes has been characterized by conflicting results in previous literature. An inherent challenge is that, while health care worker density may have favorable impacts on health care delivery measures, health outcomes per se may be affected by many other factors beyond care delivery alone. For instance, control of hypertension is also impacted by drug supply,29,32 medication adherence,33 lifestyle factors,34 and a variety of socio-economic factors.35 Hence, in this study, we limited our analysis to hypertension treatment rates (care delivery measure) rather than hypertension control rates (health outcome measure).
Given the inclusion of NCDs in the Sustainable Development Goals,36 health care worker requirements need to also take into account human resources for health needed to manage hypertension and other NCDs. Health care workers are a critical component of the health care delivery process that can promote population health, and the supply of health professionals worldwide has been highlighted as a significant problem.37 In addition, other cadres of health worker, such as community health workers, can also positively impact outcomes for hypertension and other NCDs.38,39 On balance, our results support the strategy of task redistribution to meet the human resource challenge of management of NCDs including hypertension. Task redistribution, in which specific tasks are “reorganized and dispersed” among health care workers with different duration of training and different qualifications, can allow for more efficient use of available human resources for health.40,41 Non-physicians have been effective in hypertension management in LMICs.42–46 Given the growing global need for hypertension and NCD management, dissemination and evaluation of task redistribution strategies is urgently required.
Indeed, the WHO Global Strategy for human resources for health indicates that the supply of health care workers needs to match health needs and priorities, including the increasing burden of NCDs.47 Given that hypertension and other NCDs are chronic conditions that require longitudinal care, repeated contact with the health system, and interaction between patients and health workers, it is critical that governments, health systems, and health facilities account for NCD-related health workforce requirements in their planning and implementation processes.48 The most recent health workforce requirements calculated by the WHO do in fact include NCDs such as hypertension, but the empirical basis for these requirements related to NCDs is weak. Our study therefore helps to fill that empirical gap, and we anticipate that our results will further inform the policy, planning, and health system development tasks of the global health community.
One limitation of our study is that, by utilizing a single regression analysis across the entire pooled dataset, we assumed that the relationship between health care worker density and hypertension treatment rate was the same across countries and over time. The sensitivity analyses we conducted were aimed at evaluating whether there were differences by date of study or income category classification, but the resulting smaller sample sizes did not allow for a definitive conclusion. Thus, while it is possible that this assumption may not hold across all health care worker density-treatment dyads, we feel that our contribution is an important first step to incorporate hypertension and other NCDs into health care worker requirements worldwide. Similarly, it is possible that high- vs. low-quality studies could yield different results. While this was beyond the scope of this paper, future research in this area can consider including quality grading in the selection of study data. Second, we acknowledge that, by focusing only on hypertension treatment rates, we do not take into consideration all of the other tasks that health care workers perform (e.g. vaccinations, antenatal care, care for other disease entities). The WHO has recently advocated for the use of a more integrated “index” of services required to meet the Sustainable Development Goals, and future efforts will benefit from that type of approach. Third, health workforce density is only one component that contributes to overall health care worker performance; other important components include accessibility, acceptability, and quality of care.49 In addition, nurse density may reflect better access to health care in general, thus the interpretation of our results requires some caution. Fourth, we were not able to use pharmacist density data, as the data were not as routinely available as physician or nurse density. Given the importance of pharmacists in the dispensing of hypertension medications in many parts of the world, future research in this area should include pharmacist density as the data become more routinely available. Fifth, our analytic model aggregated all variables to the country level; therefore, individual-level variables impacting hypertension treatment rates (e.g. individual socio-economic status, access to care) were not evaluated. Relatedly, we pursued an analytic approach analogous to one previously utilized to assess the relationship between health care worker density and vaccination coverage.10 We recognize that this is not the only way to analyze this relationship, and alternative models and approaches can be adopted.
Perspectives
Our results support the strategy of task redistribution to meet the human resource challenge of management of NCDs including hypertension. Given the growing global need for hypertension and NCD management, our results have important implications for health policy, health system design, and program implementation. Future research assessing dissemination and evaluation of task redistribution strategies is urgently required. Investigating the relationship between health worker performance and other health outcomes will also be critical.
Conclusions
In this worldwide econometric analysis, we found that health care worker density was significantly associated with hypertension treatment. Notably, we found that that nurse density, not physician density, appeared to explain most of the relationship with hypertension treatment rate, after adjusting for several potential confounder variables. Our study contributes to the literature on cross-country analyses of health care worker density and treatment outcomes. Given the growing burden of CVD, hypertension, and other NCDs, these results have important implications for health policy, health system design, and program implementation. Future research assessing the relationship between health care worker performance and other health outcomes will also be critical.
Supplementary Material
Novelty and Significance.
What is New?
Health worker density was significantly associated with hypertension treatment rate
Our approach of aggregating and disaggregating physicians and nurses allowed us to highlight that nurse density, not physician density, appears to explain more of the relationship with hypertension treatment rate
What is Relevant?
To the best of our knowledge, this is the first report examining the relationship between health worker density and hypertension treatment rates using worldwide data
Summary
Our results support the strategy of task redistribution to meet the human resource challenge of management of non-communicable diseases including hypertension.
Future research assessing the relationship between health worker performance and other health outcomes will also be critical.
Acknowledgments:
The authors would like to thank Julia Dickhaus, Claire Kofler, and Briana Cortez for editorial assistance, and Carl DeFranco for research assistance.
Sources of Funding: Research reported in this publication was supported by the Fogarty International Center of the National Institutes of Health under Award Number 1R01HL125487. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict(s) of Interest/Disclosure(s): None
References
- 1.Naghavi M, Abajobir AA, Abbafati C, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet.390(10100):1151–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913. [DOI] [PubMed] [Google Scholar]
- 3.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383(9932):1899–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gakidou E, Afshin A, Abajobir AA, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet.390(10100):1345–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. 2018;71(19):e127–e248. [DOI] [PubMed] [Google Scholar]
- 6.Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA : the journal of the American Medical Association. 2013;310(9):959–968. [DOI] [PubMed] [Google Scholar]
- 7.Mills KT, Bundy JD, Kelly TN, et al. <span hwp:id=“article-title-1” class=“article-title”>Global Disparities of Hypertension Prevalence and Control<span hwp:id=“article-title-35” class=“sub-article-title”>Clinical Perspective. A Systematic Analysis of Population-Based Studies From 90 Countries. 2016;134(6):441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maimaris W, Paty J, Perel P, et al. The influence of health systems on hypertension awareness, treatment, and control: a systematic literature review. PLoS Med. 2013;10(7):e1001490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khatib R, Schwalm JD, Yusuf S, et al. Patient and healthcare provider barriers to hypertension awareness, treatment and follow up: a systematic review and meta-analysis of qualitative and quantitative studies. PLoS One. 2014;9(1):e84238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anand S, Barnighausen T. Health workers and vaccination coverage in developing countries: an econometric analysis. Lancet. 2007;369(9569):1277–1285. [DOI] [PubMed] [Google Scholar]
- 11.Castillo-Laborde C Human resources for health and burden of disease: an econometric approach. Hum Resour Health. 2011;9:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anand S, Barnighausen T. Human resources and health outcomes: cross-country econometric study. Lancet. 2004;364(9445):1603–1609. [DOI] [PubMed] [Google Scholar]
- 13.Robinson J, Wharrad H. Invisible nursing: exploring health outcomes at a global level. Relationships between infant and under-5 mortality rates and the distribution of health professionals, GNP per capita, and female literacy. Journal of advanced nursing. 2000;32(1):28–40. [DOI] [PubMed] [Google Scholar]
- 14.Robinson JJ, Wharrad H. The relationship between attendance at birth and maternal mortality rates: an exploration of United Nations’ data sets including the ratios of physicians and nurses to population, GNP per capita and female literacy. Journal of advanced nursing. 2001;34(4):445–455. [DOI] [PubMed] [Google Scholar]
- 15.Kim K, Moody PM. More resources better health? A cross-national perspective. Social science & medicine (1982). 1992;34(8):837–842. [DOI] [PubMed] [Google Scholar]
- 16.Hertz E, Hebert JR, Landon J. Social and environmental factors and life expectancy, infant mortality, and maternal mortality rates: results of a cross-national comparison. Social science & medicine (1982). 1994;39(1):105–114. [DOI] [PubMed] [Google Scholar]
- 17.Cochrane AL, St Leger AS, Moore F. Health service ‘input’ and mortality ‘output’ in developed countries. Journal of epidemiology and community health. 1978;32(3):200–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu Y, Dalal K, Stollenwerk B. The association between health system development and the burden of cardiovascular disease: an analysis of WHO country profiles. PLoS One. 2013;8(4):e61718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jurges H, Pohl V. Medical guidelines, physician density, and quality of care: evidence from German SHARE data. The European journal of health economics : HEPAC : health economics in prevention and care. 2012;13(5):635–649. [DOI] [PubMed] [Google Scholar]
- 20.The World Bank. [online]. Countries and lending groups: country-classifications 2013. http://data.worldbank.org/about/. Accessed September 30, 2015.
- 21.Carter BL, Bosworth HB, Green BB. The Hypertension Team: The Role of the Pharmacist, Nurse and Teamwork in Hypertension Therapy. Journal of Clinical Hypertension (Greenwich, Conn). 2012;14(1):51–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clark CE, Smith LF, Taylor RS, Campbell JL. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ (Clinical research ed). 2010;341:c3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chronic diseases and health promotion. 2016; www.who.int/chp/steps/reports/en. Accessed February 23, 2016.
- 24.WHO Global Health Workforce Statistics. 2016; www.who.int/hrh/statistics/hwfstats. Accessed February 23, 2016.
- 25.Data: Indicators. 2016; http://data.worldbank.org/indicator. Accessed February 23, 2016.
- 26.World Population Prospects. 2016; esa.un.org/unpd/wpp. Accessed February 23, 2016.
- 27.Health statistics and information systems. 2016; www.who.int/healthinfo/global_burden_disease/estimates/en/index2.html. Accessed February 23, 2016.
- 28.Scheffler R, Cometto G, Tulenko K, et al. Health workforce requirements for universal health coverage and the Sustainable Development Goals – Background paper N.1 to the WHO Global Strategy on Human Resources for Health: Workforce 2030. Geneva: 2016. [Google Scholar]
- 29.Joshi R, Alim M, Kengne AP, et al. Task shifting for non-communicable disease management in low and middle income countries--a systematic review. PLoS One. 2014;9(8):e103754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bengtson A, Drevenhorn E. The nurse’s role and skills in hypertension care: a review. Clinical nurse specialist CNS. 2003;17(5):260–268. [DOI] [PubMed] [Google Scholar]
- 31.Sol BG, van der Bijl JJ, Banga JD, Visseren FL. Vascular risk management through nurse-led self-management programs. Journal of vascular nursing : official publication of the Society for Peripheral Vascular Nursing. 2005;23(1):20–24. [DOI] [PubMed] [Google Scholar]
- 32.Kishore SP, Vedanthan R, Fuster V. Promoting global cardiovascular health ensuring access to essential cardiovascular medicines in low- and middle-income countries. J Am Coll Cardiol. 2011;57(20):1980–1987. [DOI] [PubMed] [Google Scholar]
- 33.Elliott WJ. What factors contribute to the inadequate control of elevated blood pressure? Journal of clinical hypertension (Greenwich, Conn). 2008;10(1 Suppl 1):20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Opie LH, Seedat YK. Hypertension in sub-Saharan African populations. Circulation. 2005;112(23):3562–3568. [DOI] [PubMed] [Google Scholar]
- 35.Niessen LW, Mohan D, Akuoku JK, et al. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet. 2018;391(10134):2036–2046. [DOI] [PubMed] [Google Scholar]
- 36.Sustainable Development Goals. http://www.un.org/sustainabledevelopment/sustainable-development-goals/. Accessed January 25, 2017.
- 37.Crisp N, Chen L. Global supply of health professionals. The New England journal of medicine. 2014;370(23):2247–2248. [DOI] [PubMed] [Google Scholar]
- 38.Abdel-All M, Putica B, Praveen D, Abimbola S, Joshi R. Effectiveness of community health worker training programmes for cardiovascular disease management in low-income and middle-income countries: a systematic review. BMJ open. 2017;7(11):e015529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alaofe H, Asaolu I, Ehiri J, et al. Community Health Workers in Diabetes Prevention and Management in Developing Countries. Annals of global health. 2017;83(3–4):661–675. [DOI] [PubMed] [Google Scholar]
- 40.Task shifting: Rational redistribution of tasks among health workforce teams. Geneva: World Health Organization; 2008. [Google Scholar]
- 41.Human Resources for Health: Overcoming the Crisis. Cambridge, MA: Joint Learning Initiative; 2004. [Google Scholar]
- 42.Coleman R, Gill G, Wilkinson D. Noncommunicable disease management in resource-poor settings: a primary care model from rural South Africa. Bulletin of the World Health Organization. 1998;76(6):633–640. [PMC free article] [PubMed] [Google Scholar]
- 43.Kumar A, Kamano JH, Too K, et al. Effect of Nurse-Based Management of Hypertension in Rural Western Kenya. American College of Cardiology Scientific Sessions; 2016; Chicago, USA. [Google Scholar]
- 44.Adeyemo A, Tayo BO, Luke A, Ogedegbe O, Durazo-Arvizu R, Cooper RS. The Nigerian antihypertensive adherence trial. Journal of hypertension. 2013;31(1):201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kengne AP, Awah PK, Fezeu LL, Sobngwi E, Mbanya J-C. Primary Health Care for Hypertension by Nurses in Rural and Urban Sub-Saharan Africa. The Journal of Clinical Hypertension. 2009;11(10):564–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jafar TH, Silva A, Naheed A, et al. Control of blood pressure and risk attenuation: a public health intervention in rural Bangladesh, Pakistan, and Sri Lanka: feasibility trial results. Journal of hypertension. 2016;34(9):1872–1881. [DOI] [PubMed] [Google Scholar]
- 47.Global strategy on human resources for health: workforce 2030. Geneva: World Health Organization;2016. [Google Scholar]
- 48.Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. The Lancet. 2016;388(10060):2665–2712. [DOI] [PubMed] [Google Scholar]
- 49.Campbell J, Dussault G, Buchan J, et al. A universal truth: no health without a workforce. Geneva: Global Health Workforce Alliance and World Health Organization;2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.