Abstract
Background
Self-management of health is important for improving health outcomes among primary care patients with chronic disease. Anxiety and depressive disorders are common and interfere with self-regulation, which is required for disease self-management. An insurance-reimbursable mindfulness intervention integrated within primary care may be effective for enhancing chronic disease self-management behaviors among primary care patients with anxiety, depression, trauma, and stress-related and adjustment disorders compared with the increasingly standard practice of referring patients to outside mindfulness resources.
Objective
Mindfulness Training for Primary Care (MTPC) is an 8-week, referral-based, insurance-reimbursable program integrated into safety-net health system patient-centered medical homes. We hypothesized that MTPC would be more effective for catalyzing chronic disease self-management action plan initiation within 2 weeks, versus a low-dose comparator (LDC) consisting of a 60-min mindfulness introduction, referral to community and digital resources, and addition to a 6-month waitlist for MTPC.
Participants
Primary care providers (PCPs) and mental health clinicians referred 465 patients over 12 months. All participants had a DSM-V diagnosis.
Design and Interventions
Participants (N = 136) were randomized in a 2:1 allocation to MTPC (n = 92) or LDC (n = 44) in a randomized controlled comparative effectiveness trial. MTPC incorporates mindfulness, self-compassion, and mindfulness-oriented behavior change skills and is delivered as insurance-reimbursable visits within primary care. Participants took part in a chronic disease self-management action planning protocol at week 7.
Main Measures
Level of self-reported action plan initiation on the action plan initiation survey by week 9.
Key Results
Participants randomized to MTPC, relative to LDC, had significantly higher adjusted odds of self-management action plan initiation in an intention-to-treat analysis (OR = 2.28; 95% CI = 1.02 to 5.06, p = 0.025).
Conclusions
An 8-week dose of mindfulness training is more effective than a low-dose mindfulness comparator in facilitating chronic disease self-management behavior change among primary care patients.
Electronic supplementary material
The online version of this article (10.1007/s11606-018-4739-5) contains supplementary material, which is available to authorized users.
KEY WORDS: primary care, mindfulness, self-management, health behavior, self-regulation, patient-centered
INTRODUCTION
Primary care treats the majority of patients with anxiety, depression, trauma, and stress,1–5 which are frequently comorbid with chronic physical illness (e.g., diabetes, arthritis).6–9 These mental illnesses often impair self-regulation skills,10 such as emotion regulation (e.g., impulse control), self-related processing (e.g., self-critical rumination, self-efficacy), and cognitive control (e.g., attention, executive function).11–15 Hence, mental illness combined with chronic physical illness predicts poor health outcomes,16 prompting integration of mental health treatment into patient-centered medical homes (PCMHs). Programs that enhance primary care patients’ self-regulation skills have been shown to improve health outcomes through enhancing chronic illness self-management.17–20 Self-management, a core focus within both the PCMH health care reform movement and the Chronic Care Model,18, 20–23 is commonly encouraged through a process of engaged goal setting using the SMART framework24 and accessible to a diversity of patient populations.25, 26
Mindfulness meditation may enhance self-regulation27–29 (e.g., attention, emotion regulation processes30, 31) by increasing cognitive resources28 (e.g., reappraisal, exposure) and modifying self-related processing32 (e.g., reduced rumination, enhanced body awareness). Mindfulness-based programs (MBPs)33, derived from mindfulness-based stress reduction (MBSR),34, 35 are evidence-based treatments that seem to harness self-regulatory mechanisms and could help people with self-regulation challenges catalyze behavior change related to managing chronic disease.36 Meta-analyses demonstrate moderate effects of 8-week MBPs on anxiety, depression, and quality of life during chronic disease.37, 38
Implementation of mindfulness training programs within primary care holds promise as a sustainable, large-scale model for enhancing chronic illness self-management, improving patient symptoms,39 and reducing health care service utilization.40–42 This study replicates a pilot study of Mindfulness Training for Primary Care (MTPC), an insurance-reimbursable MBP adapted for primary care PCMHs, which suggested MTPC might facilitate medical regimen adherence related to chronic disease self-management action plan initiation.43
To determine MTPC’s impact on catalyzing health behavior change, we compared health behavior self-management action plan initiation rates for primary care patients randomized to MTPC versus a low-dose comparator (LDC), consisting of 60-min introduction to mindfulness with referral to community and digital mindfulness resources.
METHODS
Study Design
This was a randomized controlled comparative effectiveness trial44, 45 evaluating the impact of 8-week MTPC versus LDC on action plan initiation within 2 weeks of setting a health behavior self-management SMART goal (primary outcome). Baseline, 8-week, and 24-week within-group and between-group intervention effects were assessed for health and self-regulation outcomes.
Participants
We recruited participants from 11 metro-north Boston primary care PCMHs via print and digital flyers, as well as referrals from primary and mental health care settings confirmed by a primary care provider. Individuals were eligible if ≥ 18 years old, had a DSM-V diagnosis, and received primary care within a participating PCMH site. Individuals were excluded if they presented with psychosis symptoms, thought disorder, active substance use disorder, cognitive impairment, severe mental illness, high risk for hospitalization, insurance coverage not including group psychotherapy, English reading proficiency below 7th grade (using REALM-SF Health Literacy Assessment46), or third trimester pregnancy. Participants were required to have an evaluation with a mental health clinician who completed a 9-item checklist to confirm eligibility and DSM-V diagnosis. A board-certified psychiatrist reviewed diagnosis and eligibility if unclear.
Informed Consent
Eligible individuals were invited to an informed consent group session which communicated they could continue receiving standard mental health treatment, including psychopharmacology and psychotherapy consistent with the IMPACT stepped care model47–50 regardless of their randomization status. There were 10 recruitment cycles, each with an average of 2 different date options for a consent session (total 20 group consent sessions), between January and October 2017.
60-min Mindfulness Introduction
After consenting, participants received a 60-min mindfulness introduction from a MTPC group leader before randomization. The session introduced basic mindfulness principles, brief guided mindfulness practices, inquiry,51 and review of mindfulness resources. After mindfulness introduction session, participants could decline continuation before randomization.
Randomization and Allocation
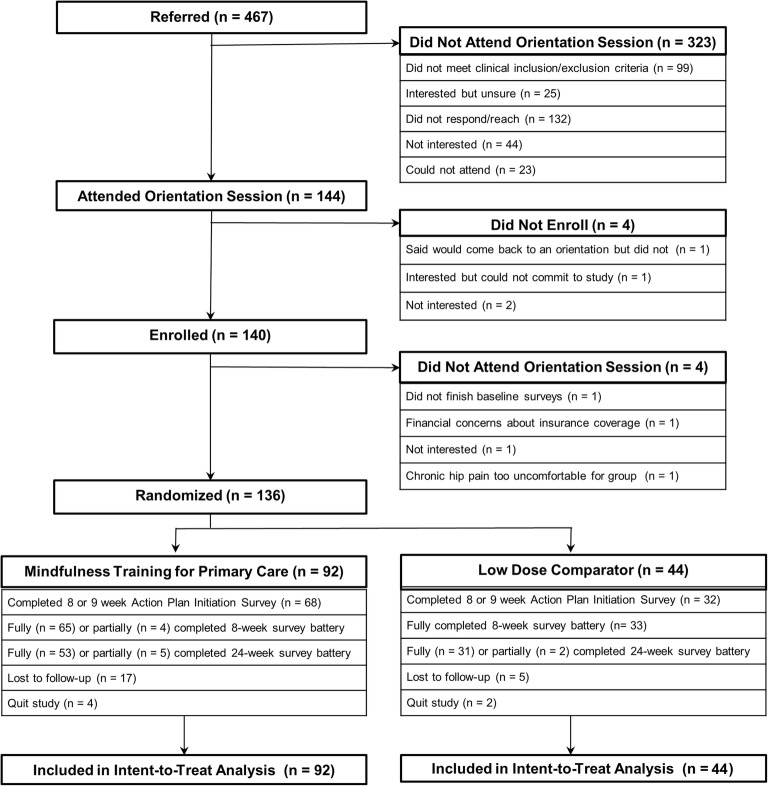
A blinded study staff member employed a computer-based forced block randomization algorithm in Stata with a 2:1 allocation ratio placing enrolled individuals who completed baseline surveys (N = 136) into MTPC (n = 92) or LDC (n = 44) arms (Fig. 1). The algorithm stratified across four PCMH regions offering MTPC and also by PCP mindfulness training level to prevent confounding by differences in PCP mindfulness expertise.
Figure 1.
Consort Diagram.
Interventions
Intervention: Mindfulness Training for Primary Care
MTPC incorporates elements from MBSR and mindfulness-based cognitive therapy52 (MBCT) with evidence-based elements from other mindfulness-oriented behavior change approaches.43, 52–55 MTPC is also designed to be trauma-informed.56–59 MTPC offers 8 weekly 2-h sessions, a 7-h all-day session, and 30–45 min of recommended daily home practice with guided recordings. Sessions cover awareness of body sensations and breathing, autopilot, and stress responses, relating to discomfort, integration of core practices from MBCT and mindful self-compassion,53 and novel components related to health behavior, communication, chronic illness self-management,60 values clarification,61 and mindful orientation towards action planning.62 Weekly session curricula were designed to be adaptable to different primary care treatment contexts, allowing mental health and primary care providers to adapt session format to meet criteria for insurance billing as group psychotherapy or group medical visit, respectively.43
MTPC groups were co-led by two of 13 trained providers, including 12 licensed mental health clinicians (e.g., psychology, social-work, psychiatry) and one primary care provider, who all completed 35 h of 8-week MBSR plus practicum and 40 h of MTPC specific training.43 MTPC curriculum adherence was tracked through weekly supervision and session-specific fidelity checklists.63 Adherence to curriculum was rated as 0-1-2 (absent-partial-complete), with a mean of 1.91 (SD = 0.31) over 10 MTPC cycles (80 total sessions). Sessions were audio-recorded, and 10% were reviewed by trained observers for adherence and competency, preventing drift.64–66
Low-Dose Comparator
Participants randomized to LDC were encouraged to practice mindfulness skills learned during 60-min introductions and use digital67 and community resources43 while continuing standard mental health care described earlier. Participants were guaranteed an 8-week MBP spot 6 months later contingent on survey completion.
Participant Outreach
Participants in both arms received engagement calls (~ 10 min) every other week for 8 weeks to provide attention-matched study staff support (e.g., logistics, mindfulness practice encouragement), minimize attrition,68 and facilitate survey completion.69 Participants unresponsive to a survey were contacted by phone, e-mail, and/or text message up to five times within the 14-day completion window.70
Measures
We collected and managed data using REDCap data capture tools.71 Participants completed baseline surveys for sociodemographic and meditation experience variables (Table 1).
Table 1.
Baseline Demographic and Clinical Characteristics of Participants by Study Arm
| Variable | MTPC (n = 92) | Comparator (n = 44) | Total (n = 136) |
|---|---|---|---|
| Female, N (%) | 63 (68.5) | 26 (59.1) | 89 (65.4) |
| Age (years), mean (SD) | 40.6 (12.7) | 40.3 (12.2) | 40.5 (12.5) |
| Race, N (%) | |||
| White | 73 (79.3) | 32 (72.3) | 105 (77.2) |
| Black | 3 (3.3) | 4 (9.1) | 7 (5.1) |
| Other | 16 (17.3) | 8 (18.2) | 24 (17.6) |
| Ethnicity Hispanic, N (%) | 17 (18.5) | 4 (9.1) | 21 (15.4) |
| English as second language, N (%) | 19 (20.1) | 5 (11.4) | 24 (17.7) |
| Annual income < $20,000, N (%) | 31 (33.7) | 9 (20.5) | 40 (29.4) |
| Marital status, N (%)+ | |||
| Single | 44 (48.4) | 23 (54.8) | 67 (49.3) |
| Married/cohabitating | 32 (35.1) | 17 (40.5) | 49 (36.0) |
| Divorced | 13 (14.2) | 2 (4.8) | 15 (11.0) |
| Education (years), mean (SD) | 16.6 (3.1) | 15.5 (4.1) | 16.2 (3.4) |
| Insurance, N (%) | |||
| Medicaid or Medicare | 12 (13.0) | 8 (18.2) | 20 (14.7) |
| Subsidized | 39 (42.4) | 12 (27.3) | 51 (37.5) |
| Private | 39 (42.4) | 22 (50.0) | 61 (44.9) |
| Other | 2 (2.2) | 2 (4.6) | 4 (2.9) |
| Have practiced meditation before, N (%) | 56 (60.1) | 22 (50.0) | 78 (57.3) |
| Baseline meditation practice, mean min/day (SD) | 6.8 (10.5) | 4.1 (6.5) | 5.9 (9.4) |
| DSM-V diagnosis, N (%) | |||
| Single DSM-V diagnosis | 59 (64.1) | 30 (68.2) | 89 (65.4) |
| 2+ DSM-V diagnoses | 33 (35.9) | 14 (31.8) | 47 (34.6) |
| Primary DSM-V diagnosis, N (%) | |||
| Major depressive disorder* | 27 (29.3) | 10 (22.7) | 37 (27.2) |
| Generalized anxiety disorder (300.02) | 16 (17.4) | 7 (15.9) | 23 (16.9) |
| Anxiety NOS (300) | 14 (15.2) | 6 (13.6) | 20 (14.7) |
| Adjustment disorder** | 11 (12.0) | 10 (22.7) | 21 (15.4) |
| Other depressive disorder^ | 9 (9.8) | 6 (13.6) | 15 (11.0) |
| Other*** | 15 (16.3) | 5 (11.4) | 20 (14.7) |
| Any PTSD diagnosis, N (%) | 11 (12.0) | 1 (2.3) | 12 (8.8) |
| Any depression diagnosis, N (%) | 48 (52.2) | 19 (43.2) | 67 (49.3) |
+Not shown: widowed (MTPC n = 1; LDC n = 1)
*Includes DSM-V codes: major depressive disorder (MDD), single (296.20), MDD, recurrent (296.31–296.35)
**Includes adjustment disorder, with depressed mood (309.0); adjustment disorder, with anxiety (309.24); adjustment disorder, with mixed anxiety and depressed mood (309.28)
^Includes depression NOS (311), persistent depressive disorder/dysthymia (300.4)
***Includes post-traumatic stress disorder (PTSD) (309.81), mood disorder NOS (296.89), somatic disorder (300.82), attention-deficit disorders (314.01), psychological factors affecting medical (316), panic disorder with or without agoraphobia (300.01/300.21), social anxiety disorder (300.23), obsessive compulsive disorder (300.3)
T test and χ2 test conducted; there were no significant differences between groups. DSM-V, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; PROMIS, Patient-Reported Outcomes Measures
Primary Outcome
During study week 7, participants created a short-term action plan focused on behavior change related to self-management of chronic disease and/or health maintenance using video and written materials outlining the well-established SMART goal framework.25, 62 Participants then reported their level of action plan initiation in the action plan initiation (API) survey,72 from 1 (not at all) to 7 (completely) at weeks 8 and 9, a 2-week time window consistent with previously published studies.26, 72, 73 Evidence of plan initiation was defined as API score ≥ 5. Primary outcome was the highest score on either API survey by the end of week 9.
Secondary Outcomes
Secondary outcomes were assessed at baseline and 8 and 24 weeks.
Health Outcomes
Anxiety and depression were assessed using Patient-Reported Outcomes Measurement Information System (PROMIS) Anxiety Short Form 8a (Cronbach’s α = 0.92)74, 75 and PROMIS Depression Short Form 8a (α = 0.97).76, 77 Both were scored from 1 (never) to 5 (always).76T scores were generated using PROMIS scoring conversion tables.78
Stress was assessed by the 10-item Perceived Stress Scale (PSS),79 with items scored from 0 (never) to 4 (very often) (α = 0.83).80
Self-regulation Outcomes
Emotional regulation challenges were assessed by the 36-item Difficulties in Emotion Regulation Scale (DERS),81 with items scored from 1 (almost never) to 5 (almost always). Higher scores indicated greater levels of difficulty with emotion regulation (α = 0.94).82
Interoceptive awareness was assessed by the 32-item Multidimensional Assessment of Interoceptive Awareness (MAIA),83 with items scored from 0 (never) to 5 (always). Higher scores indicated higher levels of positive awareness (α = 0.69–0.83).84
Mindfulness was assessed by the 39-item Five-Facet Mindfulness Questionnaire (FFMQ),85, 86 with items scored from 1 (never or very rarely true) to 5 (very often or always true) (α = 0.75–0.92).86
Self-compassion was assessed by the 12-item Self-Compassion Scale Short Form (SCS-SF),87 with items scored from 1 (almost never) to 5 (almost always). Higher scores indicated higher experience of self-compassion (α = 0.87).87
The 6-item Self-Efficacy for Chronic Disease (SECD-6) scale60 measured participant confidence in the ability to do activities related to managing their chronic disease from 1 (not at all confident) to 10 (totally confident) (α = 0.90).88
The 5-item Perceived Control Questionnaire (PCQ)89, 90 asked participants to rate their sense of control over chronic disease from 1 (none) to 7 (total) (α = 0.74).89
Home Practice and Resource Use
Participants recorded 18 daily practice/resource variables weekly until week 8 using either hand-delivered scantron (MTPC) or link to REDCap (LDC), including formal practice (e.g., body scan), informal practice (e.g., breathing space), and use of mindfulness resources (e.g., guided recordings) (Table 4).
Table 4.
Weekly Mindfulness Practice and Resource Use (Weeks 2–8) by Study Arm
| Practice | MTPC | LDC | t | p | ||
|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | |||
| Formal practice (mean min/week) | 78 | 190.9 (121.5) | 36 | 53.0 (79.4) | 6.2 | < 0.001* |
| Informal practice (mean count/week) | 78 | 15.4 (11.5) | 36 | 6.2 (8.2) | 4.3 | < 0.001* |
| Formal (mean min/week) | ||||||
| Body scan | 78 | 87.6 (60.0) | 36 | 18.4 (46.9) | 6.1 | < 0.001* |
| Mindful sitting | 77 | 38.4 (34.8) | 36 | 13.5 (21.8) | 3.9 | < 0.001* |
| Mindful movement | 77 | 40.5 (46.1) | 36 | 16.1 (26.2) | 3.0 | < 0.005* |
| Kindness/compassion | 76 | 26.0 (30.8) | 36 | 5.1 (9.8) | 4.0 | < 0.001* |
| Informal (mean count/week) | ||||||
| Gratitude | 77 | 2.3 (2.4) | 36 | 1.0 (2.0) | 2.8 | < 0.01* |
| Mindful eating | 78 | 2.1 (1.9) | 36 | 0.9 (1.7) | 3.4 | < 0.005* |
| Body awareness | 78 | 3.8 (2.3) | 36 | 1.7 (2.4) | 4.5 | < 0.001* |
| Informal kindness | 77 | 2.2 (2.5) | 36 | 0.5 (1.2) | 3.8 | < 0.001* |
| Mindful walking | 78 | 1.8 (1.8) | 36 | 0.96 (1.7) | 2.4 | < 0.05* |
| Breathing space | 78 | 1.8 (2.1) | 36 | 0.7 (1.6) | 2.9 | < 0.01* |
| Self-compassion break | 78 | 1.4 (1.8) | 36 | 0.4 (0.9) | 3.2 | < 0.01* |
| Resource use (mean count/week) | ||||||
| Mindfulness/wellness centers | 80 | 0.42 (0.5) | 36 | 0.1 (0.26) | 3.4 | < 0.001* |
| Online recordings | 80 | 1.3 (1.8) | 36 | 0.4 (0.77) | 3.1 | < 0.005* |
| Mobile apps | 80 | 0.9 (1.6) | 36 | 0.7 (1.3) | 0.7 | 0.50 |
| MTPC recordings | 80 | 2.8 (2.2) | 36 | 0.1 (0.3) | 7.5 | < 0.001* |
| Mindfulness books/articles | 80 | 1.2 (1.7) | 36 | 0.6 (1.1) | 1.9 | 0.059 |
| Spiritual centers | 80 | 0.3 (1.0) | 36 | 0.3 (0.97) | − 0.1 | 0.96 |
| Yoga centers | 80 | 0.3 (1.0) | 36 | 0.1 (0.28) | 1.2 | 0.22 |
*Significant after Hochberg FDR procedure, family-wise p < 0.05
Adverse Events
We collected adverse event reports (AERs) during engagement phone calls, week 8, and week 24, using a combination of checklist and open-ended questions. Research staff documented any AERs occurring during group sessions. We categorized AERs as serious or non-serious. An independent reviewer monitored AERs quarterly.
Statistical Analysis
To evaluate randomization, we compared sociodemographic and baseline variables using t test, Fisher’s exact, or χ2 test.
To evaluate comparative effectiveness of MTPC versus LDC on action plan initiation, we used unadjusted bivariate logistic regression (logit) in a cross-sectional analysis to assess between-group changes in frequency of initiation. In intent-to-treat (ITT) analysis, we defined non-initiator status as participants who never endorsed greater than 4 or who did not complete the API survey at all by week 9. We powered the study based on expected differences in action plan initiation between study arms. Assuming α = 0.05, a sample of 136 participants randomized 2:1 would have 80% power to detect a 20% difference in API rates between arms. We used adjusted multivariable logistic regression models to determine other API predictors, in addition to study arm, using covariates where p < 0.05 in bivariate analyses.
To evaluate health and self-regulation outcomes, we conducted a difference-in-differences, ITT, repeated measures analysis using linear mixed effects models91 (mixed) to evaluate time × treatment interaction from baseline to 8 weeks and from baseline to 24 weeks. Mixed effects models accounted for clustering of multiple observations within participants and handled missing data with maximum likelihood estimation. We computed contrasts of predictive margins92 to test for significant within-group changes and difference-in-differences (between-group) estimates over time and to ease interpretation of results. Between-group and within-group effect size (Cohen’s d) was computed based on the predictive margins generated from the mixed models.
MTPC practice diaries were scanned and scored using Remark.93 Average weekly practice was calculated by summing daily minutes/counts of all weekly diaries and dividing by the number of diaries completed. Missing diaries were recorded but not included in averages. We used t tests to compare MTPC with LDC.
Multiple Comparisons Testing
The Benjamini-Hochberg false discovery rate (FDR) procedure,94 which accounts for multiple comparisons, was implemented according to Cao et al.95 in which a cutoff p value is determined for a family of similar variables and analyses (family-wise error rate = 0.05).96, 97 Statistical significance was determined for the following analysis families: within- and between-group health (family size n = 3) and self-regulation (n = 6) outcomes at both time points, formal practices (n = 4), informal practices (n = 7), and resource use (n = 7).
Adverse events were analyzed using descriptive statistics and χ2 test.
To prevent bias during analysis, an external statistical consultant (T.C.) oversaw the analysis plan and conduct and reviewed Stata MP 14.298 results and syntax. This study had a NIH-approved data safety monitoring plan with an independent monitor and was approved by the Cambridge Health Alliance (CHA) Institutional Review Board.
RESULTS
Participant Flow and Characteristics
Over 12 months, providers (n = 142) referred 465 patients, 140 of whom attended an orientation and provided informed consent (Fig. 1). Randomized participants (N = 136) were 65% female, 40.5 years old (SD = 12.5) on average, and 23% identified as non-white or mixed race. Participants most commonly had a type of anxiety disorder (36.0%) or depressive disorder (37.5%). Baseline characteristics, diagnoses, and scores on outcomes were similar between intervention and LDC arms (Table 1).
Completion Rates
All randomized participants completed baseline surveys (n = 92 [MTPC], n = 44 [LDC]). Survey completion rates were similar across study arms: API survey by 9 weeks: MTPC = 74%, LDC = 75% (p = 0.89); 8-week surveys: MTPC = 75%, LDC = 75% (p = 1.0); 24-week surveys: MTPC = 63%, LDC = 75% (p = 0.17). Individuals with private insurance were overrepresented among completers of 8-week (51% vs. 27%, p = 0.01) and API surveys (51.5% vs. 25.7%, p = 0.008) versus non-completers.
Attendance
Participants in the MTPC arm (n = 92) attended an average of 6.3 of 9 (SD = 2.7) sessions: 74% (n = 68) attended ≥ 6 sessions and 59% (n = 54) attended the all-day session. PTSD diagnosis was overrepresented among participants who attended ≥ 6 sessions (15% vs. 3%, p = 0.016).
Action Plan Initiation
Of all randomized participants, 75% (n = 101) made an action plan goal and reported level of initiation by week 9. The action plans related to mindfulness or self-care (45%), physical activity (31%), diet (8%), or other aspects impacting health or capacity for self-management of health condition (18%). There were no significant differences in action plan category between arms.
MTPC participants reported a higher rate of action plan initiation (API) compared with LDC (57.6% [n = 53] vs. 31.8% [n = 14], OR = 2.91, p = 0.006). Baseline variables such as education and diagnosis were individually associated with API (Supplementary Fig. 1); however, the association between MTPC and API remained significant when holding these variables constant (Table 2).
Table 2.
Multivariate Analysis of Predictors of Action Plan Initiation (N = 136)
| Odds ratio | 95% CI | Z | p | |
|---|---|---|---|---|
| MTPC arm | 2.28 | 1.02–5.06 | 2.24 | 0.025* |
| Education (years) | 1.17 | 1.03–1.33 | 2.47 | 0.013* |
| Any PTSD Dx | 11.00 | 1.35–89.48 | 2.24 | 0.025* |
*Significance defined by p < 0.05
Multicollinearity was assessed using variance inflation factor (VIF) and was not found among variables
Of participants who responded to the API survey (n = 101), MTPC remained associated with higher API rates (77.9% [n = 53 of 68] vs. 42.4% [n = 14 of 33], OR = 4.8, p = 0.001).
Dose of formal or informal practice was not significantly different for individuals with API versus non-initiators, but online mindfulness recording use was (n = 116, OR = 1.39 [1.03–1.88], p = 0.029). Other practice and resource variables were not significantly associated with API.
Health and Self-regulation Outcomes Analysis
MTPC was more effective than LDC for improving emotion regulation, interoceptive awareness, self-compassion, and mindfulness between baseline and 8 weeks and between baseline and 24 weeks (Table 3). There were no significant between-group changes in the scores for health outcomes at either time point.
Table 3.
Mixed Effects Intention-to-Treat Analysis (N = 136)
| Outcome | Arm | Baseline mean score (SD) | 8-week vs. baseline | 24-week vs. baseline | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Week 8 mean score (SD) | d (within-group) | Difference-in-differences MTPC vs. LDC | Week 24 mean score (SD) | d (within-group) | Difference-in-differences MTPC vs. LDC | |||||
| Β (SE) | d | Β (SE) | d | |||||||
| PROMIS-Anx | MTPC | 63.9 (6.9) | 58.5 (6.6) | − 0.80 (p < 0.001*) | − 2.44 (1.58) | − 0.36 | 58.1 (6.4) | − 0.87 (p < 0.001*) | − 2.02 (1.63) | − 0.30 |
| LDC | 61.9 (6.6) | 58.9 (6.9) | − 0.45 (p = 0.02*) | p = 0.12 | 58.0 (6.7) | − 0.59 (p = 0.004*) | p = 0.22 | |||
| PROMIS-Dep | MTPC | 59.2 (8.6) | 53.9 (7.9) | − 0.59 (p < 0.001*) | − 2.94 (1.68) | − 0.34 | 54.4 (7.3) | − 0.59 (p < 0.001*) | 0.20 (1.4) | 0.02 |
| LDC | 58.0 (8.6) | 55.6 (8.0) | − 0.29 (p = 0.08) | p = 0.08 | 52.9 (7.8) | − 0.62 (p < 0.001*) | p = 0.91 | |||
| PSS | MTPC | 25.0 (6.7) | 19.9 (6.3) | − 0.77 (p < 0.001*) | − 1.69 (1.28) | − 0.25 | 19.7 (6.0) | − 0.81 (p < 0.001*) | − 1.15 (1.32) | − 0.17 |
| LDC | 24.3 (6.6) | 20.9 (6.3) | − 0.53 (p = 0.001*) | p = 0.19 | 20.2 (6.1) | − 0.64 (p < 0.001*) | p = 0.39 | |||
| SECD | MTPC | 6.1 (1.9) | 6.7 (1.6) | 0.30 (p = 0.001*) | 0.34 (0.34) | 0.15 | 6.7 (1.5) | 0.30 (p = 0.002*) | 0.40 (0.35) | 0.21 |
| LDC | 6.2 (2.0) | 6.5 (1.7) | 0.16 (p = 0.32) | p = 0.31 | 6.4 (1.7) | 0.11 (p = 0.39) | p = 0.25 | |||
| FFMQ | MTPC | 115.8 (18.2) | 132.0 (16.9) | 0.92 (p < 0.001*) | 12.46 (3.49) | 0.57 | 135.2 (16.0) | 1.11 (p < 0.001*) | 8.95 (3.53) | 0.41 |
| LDC | 115.6 (24.5) | 119.4 (26.4) | 0.15 (p = 0.19) | p < 0.001* | 126.0 (25.6) | 0.42 (p < 0.001*) | p = 0.01* | |||
| SCS-SF | MTPC | 2.6 (0.67) | 3.1 (0.65) | 0.85 (p < 0.001*) | 0.29 (0.13) | 0.41 | 3.2 (0.62) | 0.98 (p < 0.001*) | 0.25 (0.13) | 0.36 |
| LDC | 2.6 (0.73) | 2.8 (0.69) | 0.52 (p = 0.01^) | p = 0.03* | 3.0 (0.67) | 0.52 (p < 0.001*) | p = 0.06 | |||
| PCQ | MTPC | 23.5 (4.4) | 25.3 (4.2) | 0.41 (p = 0.001*) | 1.04 (0.92) | 0.22 | 24.3 (4.0) | 0.19 (p = 0.14) | − 0.76 (0.95) | − 0.19 |
| LDC | 23.0 (4.4) | 23.8 (4.3) | 0.19 (p = 0.29) | p = 0.26 | 24.6 (4.2) | 0.38 (p = 0.38) | p = 0.42 | |||
| DERS | MTPC | 76.1 (23.0) | 60.2 (21.8) | − 0.71 (p < 0.001*) | − 13.42 (4.28) | − 0.58 | 58.5 (20.4) | − 0.80 (p < 0.001*) | − 7.73 (4.45) | − 0.34 |
| LDC | 72.2 (23.2) | 68.8 (21.8) | − 0.15 (p = 0.48) | p < 0.00* | 61.4 (21.7) | − 0.48 (p = 0.006*) | p = 0.08 | |||
| MAIA | MTPC | 2.4 (0.73) | 3.1 (0.64) | 1.00 (p < 0.001*) | 0.55 (0.13) | 0.75 | 3.1 (0.63) | 1.00 (p < 0.001*) | 0.55 (0.14) | 0.71 |
| LDC | 2.5 (0.73) | 2.6 (0.69) | 0.14 (p = 0.42) | p < 0.001* | 2.6 (0.67) | 0.28 (p = 0.14) | p = 0.001* | |||
*Significant after Hochberg FDR procedure, family-wise p < 0.05
^Significant before Hochberg FDR procedure
PROMIS-Anx, anxiety; PROMIS-Dep, depression; PSS, perceived stress; SECD, self-efficacy; FFMQ, mindfulness; SCS-SF, self-compassion; PCQ, perceived control; DERS, emotion regulation difficulty; MAIA, interoceptive awareness
Baseline: n = 92 (MTPC), n = 44 (LDC); week 8: n = 65 (MTPC), n = 33 (LDC); week 24: n = 53 (MTPC), n = 31 (LDC)
Large within-group effect sizes (d > 0.8)99 for MTPC were observed for anxiety, mindfulness, self-compassion, and interoceptive awareness at both 8 and 24 weeks, and for emotion regulation at 24 weeks. Moderate-to-large within-group effect sizes (0.5 < d < 0.79) were observed within MTPC for depression and stress at 8 and 24 weeks and within LDC arm for self-compassion and stress at 8 and 24 weeks, in addition to anxiety and depression at 24 weeks.
Mindfulness Practice and Community Resources
Most participants recorded practice and resource use: 85% (n = 78) of MTPC and 82% (n = 36) of LDC completed a weekly practice/resource diary (Table 4).
Adverse Events
During the study, there were 18 AERs completed (14 [MTPC] vs. 4 [LDC], p = 0.32). Of these, 14 were non-serious and two were related to the protocol. Of the two related to the protocol, one MTPC participant experienced a flashback during the day of silent practice, calmed himself, finished the session, and received consultation from group leaders. Another MTPC participant felt anxious during an open awareness practice, consulted with a group leader, and continued participating. There were no serious adverse events in the LDC arm.
Of the 4 serious events, one participant was diagnosed with cancer. Three individuals had psychiatric hospitalizations related to worsening of their underlying conditions (hypomanic episode, increased PTSD symptoms, suicidal ideation), but all took place > 2 months after completing MTPC.
DISCUSSION
Findings demonstrated MTPC was more effective in catalyzing health behavior action plan initiation (API) than LDC. API survey response rates (~ 75% in both arms) within 2 weeks of goal setting were similar to previous action planning studies.26, 73
MTPC was more effective for improving emotion regulation, interoceptive awareness, self-compassion, and mindfulness at 8 weeks compared with LDC. These improvements in self-regulation mechanisms may contribute to the effectiveness of mindfulness meditation.32 Follow-up studies in an adequately powered sample are needed to answer whether improvements in self-regulation mechanisms mediate the impact of mindfulness training on self-management behavior change in primary care patients.29
Trauma is associated with impairment of self-regulation.100, 101 A trauma-sensitive approach102, 103 is increasingly recognized as essential for providing MBPs safely in clinical settings.56, 58, 104, 105 PTSD diagnosis was non-significantly more common among MTPC (p = 0.1), and unexpectedly, PTSD was a strong predictor of API, which supports the trauma-informed106 nature of MTPC.
By combining access to standard mental health (psychopharmacology and psychotherapy) and mindfulness resources with biweekly encouragement calls from staff, LDC participants received a gradual 6-month self-led training in mindfulness. While this LDC program may not be as effective at catalyzing behavior change or as immediately impactful on mental health as MTPC, the positive changes in LDC at 24 weeks suggest a program offering access to high-quality mental health treatment in conjunction with ongoing encouragement calls for mindfulness practice with digital and community resources, and the potential to join an intensive mindfulness group in the future may moderately reduce stress, depression, and anxiety. The modest positive impact of the LDC program on mental health outcomes at 24 weeks warrants future study of low-dose mindfulness interventions combined with standard mental health care.
This study had several limitations. The use of an enhanced standard care comparator rather than a purely passive or well-defined active control led to variability in the level of mental health care that the LDC received, limiting conclusions about secondary health outcomes. A comparison with MBCT or cognitive-behavioral therapy, which are commonly integrated into clinical settings for depression, might elucidate how MTPC compares with other MBPs and well-defined non-mindfulness interventions in its impact on chronic disease self-management behavior change and mental health. Finally, the API protocol relies on self-report assessment of API. Future studies will compare self-reported behavior changes with experience sampling and ecological activity tracking to objectively verify API and health behavior change.
This study demonstrates that fully integrating MTPC into the health care system as an insurance-reimbursable, referral-based treatment is effective in facilitating health behavior change for primary care patients with a variety of chronic health conditions. MTPC’s unique combination of whole-person orientation107 with a focus on self-regulation and self-management skills within a group-based format makes it a promising treatment that may be associated with less stigma compared with traditional mental health treatment.108–110
MTPC facilitates self-management of chronic diseases and represents a compelling model for dissemination within primary care patient-centered medical homes.
Electronic Supplementary Material
(PNG 122 kb)
Funding Information
This study was made possible through grant funding provided by a cooperative agreement supported by the NIH Common Fund Science of Behavior Change Initiative and the National Center for Complementary and Integrative Health: “Mindfulness Influences on Self-Regulation: Mental and Physical Health Implications” (UH2AT009145) (PI: Loucks, Project PI: Schuman-Olivier). Additional funding was provided by the Arthur Vining Davis Foundations (PI: Schuman-Olivier), the Arnold P. Gold Foundation (PI: Schuman-Olivier), as well as with funding from Cambridge Health Alliance.
Data Availability
The authors will make all data available upon request.
Compliance with Ethical Standards
This study had a NIH-approved data safety monitoring plan with an independent monitor and was approved by the Cambridge Health Alliance (CHA) Institutional Review Board and procedures followed all provisions of the Declaration of Helsinki.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Olfson M, Kroenke K, Wang S, Blanco C. Trends in office-based mental health care provided by psychiatrists and primary care physicians. J Clin Psychiatry. 2014;75(3):247–253. doi: 10.4088/JCP.13m08834. [DOI] [PubMed] [Google Scholar]
- 2.Miranda J, Cooper LA. Disparities in care for depression among primary care patients. J Gen Intern Med. 2004;19(2):120–126. doi: 10.1111/j.1525-1497.2004.30272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lesser I, Rosales A, Zisook S, et al. Depression outcomes of Spanish- and english-speaking Hispanic outpatients in STAR*D. Psychiatr Serv. 2008;59(11):1273–1284. doi: 10.1176/ps.2008.59.11.1273. [DOI] [PubMed] [Google Scholar]
- 4.Nadeem E, Lange JM, Miranda J. Mental health care preferences among low-income and minority women. Arch Womens Ment Health. 2008;11(2):93–102. doi: 10.1007/s00737-008-0002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Culpepper L, et al. Treating depression and anxiety in primary care. Prim Care Companion J Clin Psychiatry. 2008;10(2):145–152. [DOI] [PMC free article] [PubMed]
- 6.Fava M, Rankin MA, Wright EC, et al. Anxiety disorders in major depression. Compr Psychiatry. 2000;41(2):97–102. doi: 10.1016/S0010-440X(00)90140-8. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, DuPont RL, Berglund P, Wittchen HU. Impairment in pure and comorbid generalized anxiety disorder and major depression at 12 months in two national surveys. Am J Psychiatry. 1999;156(12):1915–1923. doi: 10.1176/ajp.156.12.1915. [DOI] [PubMed] [Google Scholar]
- 8.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 9.Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Prev Chronic Dis. 2005;2(1):A14. [PMC free article] [PubMed] [Google Scholar]
- 10.Baumeister RF, Gailliot M, DeWall CN, Oaten M. Self-regulation and personality: how interventions increase regulatory success, and how depletion moderates the effects of traits on behavior. J Pers. 2006;74(6):1773–1801. doi: 10.1111/j.1467-6494.2006.00428.x. [DOI] [PubMed] [Google Scholar]
- 11.Paulus MP, Stein MB. Interoception in anxiety and depression. Brain Struct Funct. 2010;214(5–6):451–463. doi: 10.1007/s00429-010-0258-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Raedt R, Koster EH, Joormann J. Attentional control in depression: A translational affective neuroscience approach. Cogn Affect Behav Neurosci. 2010;10(1):1–7. doi: 10.3758/CABN.10.1.1. [DOI] [PubMed] [Google Scholar]
- 13.Demeyer I, De Lissnyder E, Koster EH, De Raedt R. Rumination mediates the relationship between impaired cognitive control for emotional information and depressive symptoms: A prospective study in remitted depressed adults. Behav Res Ther. 2012;50(5):292–297. doi: 10.1016/j.brat.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. 2007;164(10):1476–1488. doi: 10.1176/appi.ajp.2007.07030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bishop SJ. Trait anxiety and impoverished prefrontal control of attention. Nat Neurosci. 2009;12(1):92–98. doi: 10.1038/nn.2242. [DOI] [PubMed] [Google Scholar]
- 16.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 17.Swendeman D, Ingram BL, Rotheram-Borus MJ. Common elements in self-management of HIV and other chronic illnesses: an integrative framework. AIDS Care. 2009;21(10):1321–1334. doi: 10.1080/09540120902803158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health. 2014;104(8):e25–31. doi: 10.2105/AJPH.2014.302041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 21.Antonucci J. A new approach group visits: helping high-need patients make behavioral change. Fam Pract Manag. 2008;15(4):A6–8. [PubMed] [Google Scholar]
- 22.Kanaan S. Promoting Effective Self-Management Approaches to Improve Chronic Disease Care: Lessons Learned. 2008; http://www.chcf.org/publications/2008/04/promoting-effective-selfmanagement-approaches-to-improve-chronic-disease-care-lessons-learned. Accessed July 27, 2017, 2017.
- 23.Pearson M. Patient Self-Management Support Programs: An Evaluation. Santa Monica, CA: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services; 2007. [Google Scholar]
- 24.Assurance NCfQ. Goals to Care. 2015; https://www.ncqa.org/wp-content/uploads/2018/07/20180531_Report_Goals_to_Care_Spotlight_.pdf. Accessed June 8th, 2018.
- 25.Davis TC, Seligman HK, Dewalt DA, et al. Diabetes Implementation of a Self-management Program in Resource Poor and Rural Community Clinics. J Prim Care Community Health. 2012;3(4):239–242. doi: 10.1177/2150131911435673. [DOI] [PubMed] [Google Scholar]
- 26.Handley M, MacGregor K, Schillinger D, Sharifi C, Wong S, Bodenheimer T. Using action plans to help primary care patients adopt healthy behaviors: a descriptive study. J Am Board Fam Med. 2006;19(3):224–231. doi: 10.3122/jabfm.19.3.224. [DOI] [PubMed] [Google Scholar]
- 27.Tang YY, Leve LD. A translational neuroscience perspective on mindfulness meditation as a prevention strategy. Transl Behav Med. 2016;6(1):63–72. doi: 10.1007/s13142-015-0360-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang YY, Holzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16(4):213–225. doi: 10.1038/nrn3916. [DOI] [PubMed] [Google Scholar]
- 29.Loucks EB, Schuman-Olivier Z, Britton WB, et al. Mindfulness and Cardiovascular Disease Risk: State of the Evidence, Plausible Mechanisms, and Theoretical Framework. Curr Cardiol Rep. 2015;17(12):112. doi: 10.1007/s11886-015-0668-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guendelman S, Medeiros S, Rampes H. Mindfulness and Emotion Regulation: Insights from Neurobiological, Psychological, and Clinical Studies. Front Psychol. 2017;8:220. doi: 10.3389/fpsyg.2017.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Farb NA, Anderson AK, Segal ZV. The mindful brain and emotion regulation in mood disorders. Can J Psychiatry. 2012;57(2):70–77. doi: 10.1177/070674371205700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- 33.Crane RS, Brewer J, Feldman C, et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med. 2017;47(6):990–999. doi: 10.1017/S0033291716003317. [DOI] [PubMed] [Google Scholar]
- 34.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. 2. New York: Bantam Books; 2013. [Google Scholar]
- 35.Carmody J, Baer RA. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. J Clin Psychol. 2009;65(6):627–638. doi: 10.1002/jclp.20555. [DOI] [PubMed] [Google Scholar]
- 36.Benzo RP. Mindfulness and motivational interviewing: two candidate methods for promoting self-management. Chron Respir Dis. 2013;10(3):175–182. doi: 10.1177/1479972313497372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Demarzo MM, Montero-Marin J, Cuijpers P, et al. The Efficacy of Mindfulness-Based Interventions in Primary Care: A Meta-Analytic Review. Ann Fam Med. 2015;13(6):573–582. doi: 10.1370/afm.1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sundquist J, Palmer K, Johansson LM, Sundquist K. The effect of mindfulness group therapy on a broad range of psychiatric symptoms: A randomised controlled trial in primary health care. Eur Psychiatry. 2017;43:19–27. doi: 10.1016/j.eurpsy.2017.01.328. [DOI] [PubMed] [Google Scholar]
- 40.Roth B, Stanley TW. Mindfulness-based stress reduction and healthcare utilization in the inner city: preliminary findings. Altern Ther Health Med. 2002;8(1):60–62. [PubMed] [Google Scholar]
- 41.Kurdyak P, Newman A, Segal Z. Impact of mindfulness-based cognitive therapy on health care utilization: a population-based controlled comparison. J Psychosom Res. 2014;77(2):85–89. doi: 10.1016/j.jpsychores.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 42.McCubbin T, Dimidjian S, Kempe K, Glassey MS, Ross C, Beck A. Mindfulness-based stress reduction in an integrated care delivery system: one-year impacts on patient-centered outcomes and health care utilization. Perm J. 2014;18(4):4–9. doi: 10.7812/TPP/14-014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gawande R, Pine E, Griswold T, Creedon T, Vallejo Z, Rosenbaum E, Lozada A, Schuman-Olivier Z. Integrating Insurance-Reimbursable Mindfulness Training for Primary Care Patients in a Safety-Net Community Health System: A Pilot Randomized Controlled Comparative Effectiveness Trial. Mindfulness. 2019. Under Review. [DOI] [PMC free article] [PubMed]
- 44.Fiore LD, Lavori PW. Integrating Randomized Comparative Effectiveness Research with Patient Care. N Engl J Med. 2016;374(22):2152–2158. doi: 10.1056/NEJMra1510057. [DOI] [PubMed] [Google Scholar]
- 45.Chalkidou K, Tunis S, Whicher D, Fowler R, Zwarenstein M. The role for pragmatic randomized controlled trials (pRCTs) in comparative effectiveness research. Clin Trials. 2012;9(4):436–446. doi: 10.1177/1740774512450097. [DOI] [PubMed] [Google Scholar]
- 46.Arozullah AM, Yarnold PR, Bennett CL, et al. Development and validation of a short-form, rapid estimate of adult literacy in medicine. Med Care. 2007;45(11):1026–1033. doi: 10.1097/MLR.0b013e3180616c1b. [DOI] [PubMed] [Google Scholar]
- 47.Unutzer J, Park M. Strategies to improve the management of depression in primary care. Prim Care. 2012;39(2):415–431. doi: 10.1016/j.pop.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 49.Hegel MT, Imming J, Cyr-Provost M, Noel PH, Arean PA, Unutzer J. Role of behavioral health professionals in a collaborative stepped care treatment model for depression in primary care: Project IMPACT. Fam Syst Health. 2002;20(3):265–277. doi: 10.1037/h0089475. [DOI] [Google Scholar]
- 50.Lin EH, VonKorff M, Russo J, et al. Can depression treatment in primary care reduce disability? A stepped care approach. Arch Fam Med. 2000;9(10):1052–1058. doi: 10.1001/archfami.9.10.1052. [DOI] [PubMed] [Google Scholar]
- 51.Crane RS, Stanley S, Rooney M, Bartley T, Cooper L, Mardula J. Disciplined Improvisation: Characteristics of Inquiry in Mindfulness-Based Teaching. Mindfulness (N Y). 2015;6(5):1104–1114. doi: 10.1007/s12671-014-0361-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615–623. doi: 10.1037/0022-006X.68.4.615. [DOI] [PubMed] [Google Scholar]
- 53.Neff KD, Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013;69(1):28–44. doi: 10.1002/jclp.21923. [DOI] [PubMed] [Google Scholar]
- 54.Brewer JA, Mallik S, Babuscio TA, et al. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug Alcohol Depend. 2011;119(1–2):72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Garland EL, Schwarz NM, Kelly A, Whitt A, Howard MO. Mindfulness-Oriented Recovery Enhancement for Alcohol Dependence: Therapeutic Mechanisms and Intervention Acceptability. J Soc Work Pract Addict. 2012;12(3):242–263. doi: 10.1080/1533256X.2012.702638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Amaro H, Spear S, Vallejo Z, Conron K, Black DS. Feasibility, acceptability, and preliminary outcomes of a mindfulness-based relapse prevention intervention for culturally-diverse, low-income women in substance use disorder treatment. Subst Use Misuse. 2014;49(5):547–559. doi: 10.3109/10826084.2013.852587. [DOI] [PubMed] [Google Scholar]
- 57.Pollack S, Pedulla T, Siegel R. Sitting Together: Essential Skills for Mindfulness-Based Psychotherapy. New York: Guilford Publications; 2014. [Google Scholar]
- 58.Lindahl JR, Fisher NE, Cooper DJ, Rosen RK, Britton WB. The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLoS One. 2017;12(5):e0176239. doi: 10.1371/journal.pone.0176239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Elliott DE, Bjelajac P, Fallot RD, Markoff LS, Reed BG. Trauma-informed or trauma-denied: Principles and implementation of trauma-informed services for women. J Community Psychiatry. 2005;33(4):461–477. [Google Scholar]
- 60.Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4(6):256–262. [PubMed] [Google Scholar]
- 61.Miller WR, C’de Baca J, Matthews DB, Wilbourne PL. Personal Values Card Sort 2001. Accessed September 27th, 2017, 2017.
- 62.Lazarus A. Reality check: Is your behavior aligned with organizational goals? Physician Exec. 2004;30(5):50–52. [PubMed] [Google Scholar]
- 63.Chawla N, Collin S, Bowen S, et al. The mindfulness-based relapse prevention adherence and competence scale: development, interrater reliability, and validity. Psychother Res. 2010;20(4):388–397. doi: 10.1080/10503300903544257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Breitenstein SM, Gross D, Garvey CA, Hill C, Fogg L, Resnick B. Implementation fidelity in community-based interventions. Res Nurs Health. 2010;33(2):164–173. doi: 10.1002/nur.20373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hildebrand M, Host HH, Binder EF, et al. Measuring Treatment Fidelity in a Rehabilitation Intervention Study. Am J Phys Med Rehabil. 2014;91(8):715–724. doi: 10.1097/PHM.0b013e31824ad462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Waller G. Evidence-based treatment and therapist drift. Behav Res Ther. 2009;47(2):119–127. doi: 10.1016/j.brat.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 67.Plaza I, Demarzo MM, Herrera-Mercadal P, Garcia-Campayo J. Mindfulness-based mobile applications: literature review and analysis of current features. JMIR mHealth uHealth. 2013;1(2):e24. doi: 10.2196/mhealth.2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kinser PA, Robins JL. Control group design: enhancing rigor in research of mind-body therapies for depression. Evid Based Complement Alternat Med. 2013;2013:140467. doi: 10.1155/2013/140467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Richards J, Wiese C, Katon W, et al. Surveying adolescents enrolled in a regional health care delivery organization: mail and phone follow-up--what works at what cost? J Am Board Fam Med. 2010;23(4):534–541. doi: 10.3122/jabfm.2010.04.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kleschinsky JH, Bosworth LB, Nelson SE, Walsh EK, Shaffer HJ. Persistence pays off: follow-up methods for difficult-to-track longitudinal samples. J Stud Alcohol Drugs. 2009;70(5):751–761. doi: 10.15288/jsad.2009.70.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Guck TP. Attributions regarding unmet treatment goals after interdisciplinary chronic pain rehabilitation. The Clinical Journal of Pain. 2008;24(5):415–420. doi: 10.1097/AJP.0b013e3181671a1c. [DOI] [PubMed] [Google Scholar]
- 73.DeWalt DA, Davis TC, Wallace AS, et al. Goal setting in diabetes self-management: taking the baby steps to success. Patient Educ Couns. 2009;77(2):218–223. doi: 10.1016/j.pec.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Deyo RA, Katrina R, Buckley DI, et al. Performance of a Patient Reported Outcomes Measurement Information System (PROMIS) Short Form in Older Adults with Chronic Musculoskeletal Pain. Pain Med. 2016;17(2):314–324. doi: 10.1093/pm/pnv046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18(7):873–880. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Schalet BD, Cook KF, Choi SW, Cella D. Establishing a common metric for self-reported anxiety: linking the MASQ, PANAS, and GAD-7 to PROMIS Anxiety. J Anxiety Disord. 2014;28(1):88–96. doi: 10.1016/j.janxdis.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vilagut G, Forero CG, Adroher ND, et al. Testing the PROMIS(R) Depression measures for monitoring depression in a clinical sample outside the US. J Psychiatr Res. 2015;68:140–150. doi: 10.1016/j.jpsychires.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 78.Cella D, Gershon R, Bass M, Rothrock N. Assessment Center. https://www.assessmentcenter.net/. Accessed May 2018, 2018.
- 79.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 80.Cole SR. Assessment of differential item functioning in the Perceived Stress Scale-10. J Epidemiol Community Health. 1999;53(5):319–320. doi: 10.1136/jech.53.5.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gratz KL, Roemer L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess. 2004;26(1):41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- 82.Hallion LS, Steinman SA, Tolin DF, Diefenbach GJ. Psychometric Properties of the Difficulties in Emotion Regulation Scale (DERS) and Its Short Forms in Adults With Emotional Disorders. Front Psychol. 2018;9:539. doi: 10.3389/fpsyg.2018.00539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bornemann B, Herbert BM, Mehling WE, Singer T. Differential changes in self-reported aspects of interoceptive awareness through 3 months of contemplative training. Front Psychol. 2014;5:1504. doi: 10.3389/fpsyg.2014.01504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mehling WE, Price C, Daubenmier JJ, Acree M, Bartmess E, Stewart A. The Multidimensional Assessment of Interoceptive Awareness (MAIA) PLoS One. 2012;7(11):e48230. doi: 10.1371/journal.pone.0048230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Baer RA, Smith GT, Lykins E, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- 86.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 87.Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin Psychol Psychother. 2011;18(3):250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- 88.Ritter PL, Lorig K. The English and Spanish Self-Efficacy to Manage Chronic Disease Scale measures were validated using multiple studies. J Clin Epidemiol. 2014;67(11):1265–1273. doi: 10.1016/j.jclinepi.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 89.Jerant A, Moore M, Lorig K, Franks P. Perceived control moderated the self-efficacy-enhancing effects of a chronic illness self-management intervention. Chronic Illn. 2008;4(3):173–182. doi: 10.1177/1742395308089057. [DOI] [PubMed] [Google Scholar]
- 90.Armitage CCM. Distinguishing perceptions of control from self-efficacy: predicting consumption of a low-fat diet using the theory of planned behavior. J Appl Soc Psychol. 1999;29:72–90. doi: 10.1111/j.1559-1816.1999.tb01375.x. [DOI] [Google Scholar]
- 91.Rabe-Hesketh SSA. Multilevel and Longitudinal Modeling Using Stata. 3. College Station, TX: Stata Press; 2012. [Google Scholar]
- 92.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata Journal. 2012;12(2):308. doi: 10.1177/1536867X1201200209. [DOI] [Google Scholar]
- 93.Gravic I. Remark Optical Mark Recognition Software. 2018; https://remarksoftware.com/products/office-omr/. Accessed June 7, 2018, 2018.
- 94.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J R Stat Soc Ser B. 1995;57:289–300. [Google Scholar]
- 95.Cao J, Zhang S. Multiple comparison procedures. JAMA. 2014;312(5):543–544. doi: 10.1001/jama.2014.9440. [DOI] [PubMed] [Google Scholar]
- 96.Glickman ME, Rao SR, Schultz MR. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol. 2014;67(8):850–857. doi: 10.1016/j.jclinepi.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 97.Wahbeh H, Goodrich E, Goy E, Oken BS. Mechanistic Pathways of Mindfulness Meditation in Combat Veterans With Posttraumatic Stress Disorder. J Clin Psychol. 2016;72(4):365–383. doi: 10.1002/jclp.22255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Stata Statistical Software: Release 14. [computer program]. College Station, TX: StataCorp LP: StataCorp; 2015.
- 99.Leppink J, O’Sullivan P, Winston K. Effect size - large, medium, and small. Perspect Med Educ. 2016;5(6):347–349. doi: 10.1007/s40037-016-0308-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lackner CL, Santesso DL, Dywan J, O’Leary DD, Wade TJ, Segalowitz SJ. Adverse childhood experiences are associated with self-regulation and the magnitude of the error-related negativity difference. Biol Psychol. 2018;132:244–251. doi: 10.1016/j.biopsycho.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 101.van der Kolk BA, Fisler RE. Childhood abuse and neglect and loss of self-regulation. Bull Menninger Clin. 1994;58(2):145–168. [PubMed] [Google Scholar]
- 102.Emerson DSR, Chaudry S, Turner J. Trauma-Sensitive Yoga: Principles, Practice, and Research. Int J Yoga Therapy. 2009;19.
- 103.Treleaven DA. Trauma-Sensitive Mindfulness: Practices for Safe and Transformative Healing. New York: W.W. Norton & Company; 2018. [Google Scholar]
- 104.Dutton MA, Bermudez D, Matas A, Majid H, Myers NL. Mindfulness-Based Stress Reduction for Low-Income, Predominantly African American Women With PTSD and a History of Intimate Partner Violence. Cogn Behav Pract. 2013;20(1):23–32. doi: 10.1016/j.cbpra.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Vujanovic AA, Youngwirth NE, Johnson KA, Zvolensky MJ. Mindfulness-based acceptance and posttraumatic stress symptoms among trauma-exposed adults without axis I psychopathology. J Anxiety Disord. 2009;23(2):297–303. doi: 10.1016/j.janxdis.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.SAMHSA. Trauma-Informed Approach and Trauma-Specific Interventions. 2018; https://www.samhsa.gov/nctic/trauma-interventions. Accessed June 8, 2018, 2018.
- 107.Ferrante JM, Balasubramanian BA, Hudson SV, Crabtree BF. Principles of the patient-centered medical home and preventive services delivery. Ann Fam Med. 2010;8(2):108–116. doi: 10.1370/afm.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Corrigan PW, Druss BG, Perlick DA. The Impact of Mental Illness Stigma on Seeking and Participating in Mental Health Care. Psychol Sci Public Interest. 2014;15(2):37–70. doi: 10.1177/1529100614531398. [DOI] [PubMed] [Google Scholar]
- 109.Yang X, Mak WWS. The Differential Moderating Roles of Self-Compassion and Mindfulness in Self-Stigma and Well-Being Among People Living with Mental Illness or HIV. Mindfulness. 2017;8(3):595–602. doi: 10.1007/s12671-016-0635-4. [DOI] [Google Scholar]
- 110.Burnett-Zeigler IE, Satyshur MD, Hong S, Yang A, J TM, Wisner KL. Mindfulness based stress reduction adapted for depressed disadvantaged women in an urban Federally Qualified Health Center. Complement Ther Clin Pract. 2016;25:59–67. doi: 10.1016/j.ctcp.2016.08.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PNG 122 kb)
Data Availability Statement
The authors will make all data available upon request.