Abstract
Cellulite is a multifactorial condition that is present in 80% to 90% of postpubertal women and is one of the most intolerable esthetic imperfections. There are several theories on the pathophysiology of cellulite, and a number of different therapeutic regimens have been developed, from topical treatments to mechanical or energy-based devices. In this brief review, we summarize the scientific landscape to determine the clinical evidence with regard to the safety and efficacy of cellulite treatment options. Clinical protocols and the author’s experience using a combination of internal and external procedures are also discussed. Studies using laser and light modalities along with radiofrequency have shown improvements in cellulite and a good safety profile, but acoustic wave therapy, subcision, and the 1440-nm Nd:YAG minimally invasive laser have demonstrated the most beneficial results in cellulite reduction. Although there is paucity of scientific evidence for treatments that improve cellulite, future emerging options and their combination may pave the way to eradicate this primarily cosmetic esthetic concern.
Keywords: Cellulite, pathophysiology, adipocytes, radiofrequency, lasers
Introduction
Cellulite is a skin condition that affects up to 80% of postpubertal women (Luebberding et al., 2015). Cellulite is different from generalized obesity because with obesity, adipocytes undergo hypertrophy and hyperplasia; cellulite is characterized by large, metabolically stable adipocytes that are limited to lower body areas (e.g., pelvis, thighs, and abdomen; Quatresooz et al., 2006). Also known as edematous fibrosclerotic panniculopathy, cellulite was first described by Alquin and Pavot in 1920 and originally thought to be “interstitial edema associated with an increase in fat content.”
The phenotype of this condition is distinct, with the skin topography changing to a surface that resembles an orange peel. This is due to the herniation of subcutaneous fat lobules through the dermohypodermal junction, where fibrosis of the collagen septa leads to their shortening and ultimately their retraction, which causes the depressions that characterize cellulite. Although several factors are known to contribute to the development of cellulite (sex, genetics, lifestyle; Querleux, 2004, Querleux et al., 2002), the exact pathophysiology is not understood. The most prevalent models that have been proposed span from vascular/inflammatory to hormonal and/or structural causes.
Understanding the etiology of cellulite is key to developing targeted approaches, and a plethora of options is available to dermatologists to offer to their patients with cellulite. Topical agents, energy-based devices, subcision, injectable biologic medications, and more recently dermal fillers have all been used and studied in peer-reviewed publications for their safety and efficacy to treat cellulite (Table 1).
Table 1.
| Treatment type | Brand |
|---|---|
| Topical agents | Bliss, Clarins, Shisheido, Glytone |
| Radiofrequency devices | Venus Legacy (Venus Concept), Endymed PRO (Endymed), Velashape (Cynosure) |
| Laser/light devices | Cellulaze (Cynosure) |
| Acoustic wave therapy | Z-wave (Zimmer), Cellactor (Storz) |
| Subcision | Cellfina (Merz) |
| Injectable biologic treatments | EN3835 (Endo) |
| Fillers | Calcium hydroxyapatite (Radiesse), poly-l-lactic acid (Sculptra) |
Topical agents
Topical agents, combined with vigorous massage, were the earliest attempts to treat cellulite. As with all topical treatments, the main challenge of these therapies is for the active ingredients to reach their target in sufficient concentration to have a therapeutic effect. Methylxanthines (aminophylline, theophylline, and caffeine) and retinoids have been the most extensively evaluated ingredients used in topical formulations for cellulite.
Methylxanthines are hypothesized to improve cellulite by stimulating lipolysis and inhibiting the enzyme phosphodiesterase, which increases the concentration of cyclic adenosine monophosphate. Retinoids, on the other hand, are thought to reduce cellulite by increasing dermal thickness, increasing angiogenesis, synthesizing new connective tissue components, and increasing the number of active fibroblasts. For both agents, there have been several peer-reviewed publications with promising data, but the studies have been small with no long-term follow-up. Overall, certain formulations can improve collagen production and reduce skin laxity, but they are rarely effective on cellulite, which requires extensive fat, collagen, and connective tissue remodeling (Bertin et al., 2001, Green et al., 2015, Lupi et al., 2007, Pierard-Franchimont et al., 2000).
Energy-based devices
Energy-based devices that harness power from various sources such as lasers, light, radiofrequency (RF), and acoustic waves have been extensively tested for the treatment of localized adiposities and/or skin laxity.
Radiofrequency
RF devices deliver thermal energy to the dermal/subcutaneous plane via electrode(s). By elevating the tissue temperature at the target area, collagen denaturation, remodeling and neocollagenesis is stimulated, but lipolysis is also triggered. Depending on the electrode or generator configuration, RF devices come in various iterations, starting with the first generation (e.g., unipolar, monopolar, and bipolar) to the latest generation (e.g., multipolar, multigenerator, and temperature-controlled) devices. Some RF devices also integrate other energies in their technological design, such as infrared light, vacuum suction, and pulsed-electromagnetic fields (Sadick, 2007, Sadick and Rothaus, 2016a, Sadick and Rothaus, 2016b, Sadick and Sorhaindo, 2005, Sadick et al., 2014).
The latest generation of RF devices have been studied and shown to be effective in clinical trials to reduce the appearance of cellulite (Luebberding et al., 2015, Romero et al., 2008, Sadick, 2009, Sadick and Magro, 2007, Sadick and Mulholland, 2004, Wanitphakdeedecha et al., 2017). Specifically, Velasmooth and Velashape systems (Syneron Medical, Israel) that combine infrared light, bipolar RF, and mechanical manipulation of the skin with suction and massage have been shown to reduce cellulite.
In a study by Sadick and Magro (2007) where 16 subjects with cellulite were treated twice weekly for 6 weeks with the VelaSmooth system, there was a 71.87% decrease in thigh circumference and 25% improvement of cellulite in > 50% of subjects at the end of the study. In another study, where 35 female subjects with cellulite were received eight to 16 treatments twice weekly with the VelaSmooth device, 70% of patients showed a reduction in thigh circumference after 4 weeks of treatment, and 100% of patients showed some level of improvement in skin texture and cellulite (Sadick and Mulholland, 2004). Researchers have hypothesized that this is achieved due to increased circulation, stimulation of the adipocyte metabolism, and mechanical stretching of the fibrous cords.
Other devices that have been approved by the U.S. Food and Drug Administration (FDA) for the noninvasive treatment of cellulite include Exilis Elite (BTL Aesthetics, United Kingdom), which is a monopolar RF device; Venus Legacy (Venus Concept, Ontario, Canada), which is a multipolar RF device with pulsed magnetic fields; Endymed Body Shaper (Endymed), a multigenerator RF device, and ThermiRF (Thermi Aesthetics, Hayward, CA), a novel temperature-controlled RF device with internal probes (Fig. 1).
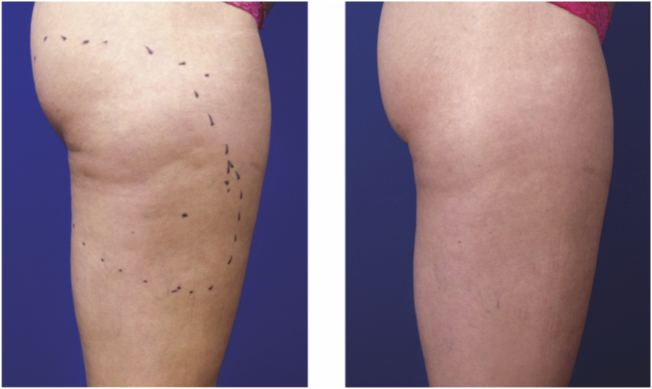
Fig. 1.
Before (left) and after (right) seven treatments in the outer thigh with Venus Legacy (Venus concept, Toronto, Ontario, Canada).
Recently, the Venus Legacy devices were used to evaluate their efficacy to treat abdominal cellulite in 25 healthy adult women who underwent eight weekly treatments. A reduction in subcutaneous thickness in the axial and sagittal plane of the abdomen was observed at 1 week after treatment initiation, and assessments by a blinded investigator at 1, 4, and 12 weeks after the final treatment demonstrated a significant improvement in cellulite appearance. No adverse effects were reported, and the treatment was well tolerated (Wanitphakdeedecha et al., 2017).
Laser and light
Laser and light devices, depending on their wavelength, emit energy to the dermis/subcutaneous plane; by heating the local tissue they can stimulate collagen remodeling and increase microcirculation, which can improve the appearance of cellulite. The impact of these devices is not very substantial in terms of adipolysis or even disruption of the fibrous septa that characterize cellulite, but they can improve the appearance of the skin and smooth the surface.
The main laser technology that has been proven effective to treat cellulite is a minimally invasive side-firing fiber 1440-nm Nd:YAG laser (DiBernardo et al., 2013, DiBernardo et al., 2016, Sasaki, 2013). This technology provides a highly targeted means of delivering laser energy into the targeted anatomical structures that underlie the cellulite as the thermal-sensing cannula is integrated with the laser delivery system to provide a safe and even distribution of energy to the treatment site. Only one treatment is required, and aside from the clinical improvement of cellulite, there is high subject satisfaction and minimal adverse events (Fig. 2).
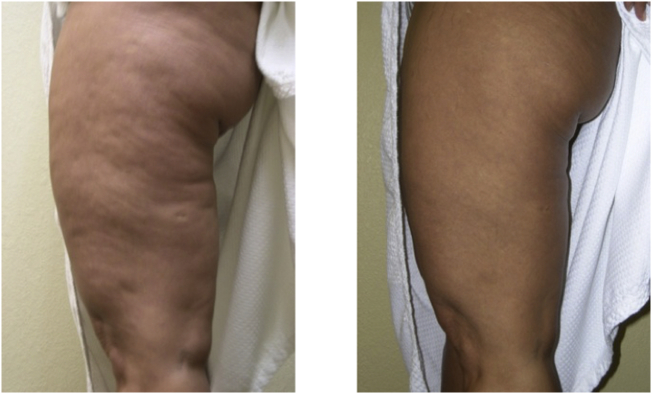
Fig. 2.
Before (left) and after (right) one treatment in the buttocks with 1440 nm Cellulaze (photograph courtesy of Cynosure).
In a multicenter clinical trial, where 57 patients underwent a three-step cellulite treatment with a 1440-nm Nd:YAG laser with a side-firing fiber and temperature-sensing cannula, the average improvement score was 1.7 for dimples and 1.1 for contour irregularities at the 6-month follow-up examination. The average satisfaction score was 5.6 for the physician and 5.3 for the patient on a 6-point scale. Treatment was well tolerated by patients (DiBernardo et al., 2016).
Acoustic wave therapy
Acoustic wave therapy (AWT) is another energy-based therapy, whereby pressure waves are transmitted to the subcutaneous tissue and promote lipolysis, improve local blood flow, enable lymphatic drainage, and stimulate the production of new collagen. Two types of acoustic waves have been used to treat cellulite: focused shock waves (ESWT) and radial shock waves. The main devices that have been used for cellulite include Cellactor (Storz, Switzerald) and Z-wave (Zimmer, Irvine, CA; Angehrn et al., 2007, Knobloch and Kraemer, 2015, Nassar et al., 2015, Russe-Wilflingseder et al., 2013). On average, AWT requires seven treatment sessions, does not require topical anesthesia, and results in only minor pain (Fig. 3; Schlaudraff et al., 2014).
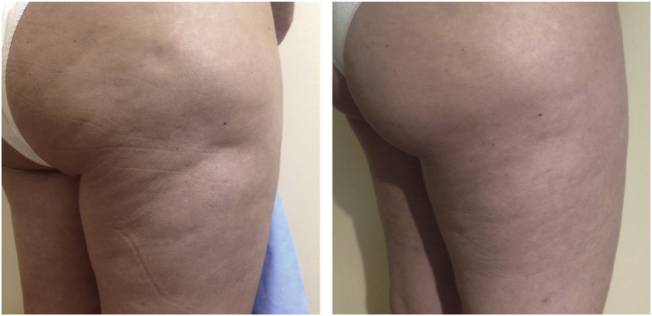
Fig. 3.
Before (left) and after (right) six treatments in the buttocks with Z-wave (photograph courtesy of Zimmer).
A study by Nassar et al. (2015) evaluated the efficacy of ESWT in 15 individuals, and eight sessions during 4 weeks were carried out. The authors concluded that ESWT was efficient in the improvement of body contour (i.e., reduction of circumference and fat layer) as well as in the appearance of cellulite 3 months after treatment. Hexsel et al. (2017) also recently evaluated the efficiency of ESWT in the treatment of cellulite in 30 women who received 12 sessions over 6 weeks. The treatment reduced cellulite severity from baseline up to 12 weeks after the last treatment session (subjects with severe cellulite: 60%-38%), and the average thickness of the subcutaneous fat tissue decreased (28.3 ± 6.5 mm to 26.7 ± 6.1 mm; p < .001). The treatment also improved patients’ quality of life, and no serious adverse events were reported (Hexsel et al., 2017).
Subcision
Manual subcision has also been evaluated for the treatment of cellulite. During this procedure, the areas are numbed with a topical anesthetic agent (vasoconstrictor with lidocaine), a needle (18 G) is inserted under the skin, and a fanning technique is used to release the fibrous cords of cellulite. Although efficacious, the main drawbacks of this treatment are the side effects, including edema, discomfort, pain, and bruising (Hexcel and Mazzuco, 2000).
Recently, a novel tissue stabilized-guided subsicion (TS-GS) system (Cellfina System; Merz North America, Inc., Raleigh, NC) was developed and FDA approved for the improvement of cellulite in the buttocks and thigh areas of adult women. The benefits of Cellfina over traditional manual subscision with a needle are its precise control of treatment depth and area of tissue (fibrous septae) and a unique vacuum-assisted design. Cellfina has been shown in multicenter clinical studies to improve cellulite with results lasting > 3 years (Kaminer et al., 2017).
In the latest clinical study, 45 subjects were followed for an extended period of up to 3 years after receiving a single treatment using the TS-GS system. The results of this trial supported an FDA clearance of the device for the long-term reduction in the appearance of cellulite following TS-GS (Kaminer et al., 2017).
Injectable treatments for cellulite
Among minimally invasive procedures for cellulite, active biologic agents and dermal fillers have been used to treat cellulite, with promising results.
Collagenase Clostridium histolyticum
Collagenase enzymes isolated and purified from the fermentation of Clostridium histolyticum are used in clinical trials for the treatment of cellulite. Collagenase I (AUX-I, Clostridial class I collagenase) and Collagenase II (AUX-II; Clostridial class II collagenase) are not immunologically cross-reactive and have different specificities; mixed in a 1:1 ratio, they become synergistic and provide a very broad hydrolyzing reactivity toward collagen (Yang and Bennett, 2015). Thus, they can hydrolyze the triple-helical region of collagen and have the potential to be effective in lysing subdermal collagen, such as those observed in the dermal septa (underlying cause of cellulite).
In phase 2b trials, a collagenase mixture, EN3835 (Endo pharmaceuticals, Malvern, PA), has been shown to be well tolerated by all dose groups, and most adverse events were mild to moderate and primarily limited to the local injection area. A phase 3 multicenter, randomized, double-blind, placebo-controlled study is currently underway to evaluate the safety and efficacy of this agent in reducing the appearance of cellulite (Callaghan et al., 2017).
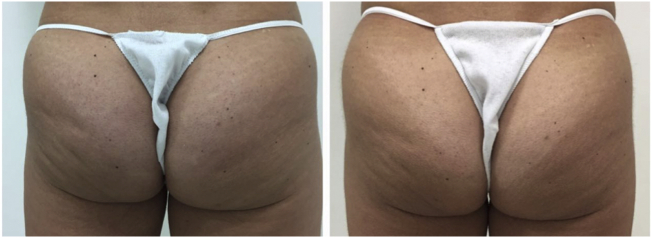
Dermal fillers
Another up-to-date option to treat cellulite is the new generation dermal fillers injections, such as calcium hydroxyapatite (CaHa) and poly-l-lactic acid microspheres (Fig. 4). These fillers have been used extensively to treat scars and can also be applied to smoothen the cellulite-induced skin irregularities. A recent study evaluated the effects of microfocused ultrasound with visualization (Ultherapy) in combination with diluted calcium hydroxylapatite (CaHA; Radiesse) on cellulite appearance in 20 women. The results showed statistically significant improvements compared with baseline for each item on the cellulite severity scale (p < .001) with a 4.5-point improvement in mean overall score (p < .001) after a single microfocused ultrasound with visualization/CaHA treatment. Both procedures were well tolerated, and subject satisfaction was high (Casabona and Pereira, 2017).
Fig. 4.
Before (left) and after (right) five treatments in the buttocks with poly-l-lactic acid (one vial; photograph courtesy of Arruda Dermatology).
Conclusions
Despite multiple therapeutic approaches that attempt to treat cellulite, no procedures have been proven successful long term. Topical agents, injectable treatments, and energy-based devices can ameliorate the appearance of cellulite, sometimes to a satisfactory degree, but never eradicate cellulite because this involves extensive tissue remodeling.
In the author’s opinion, a combination approach where internal and external approaches are used strategically and in a staged manner to yield synergistic results has the best clinical outcome. For example, injections with CaHa followed by five weekly treatments with an RF device can result in improvements of severe cellulite around 3 months after the final treatment. Other examples of combining strategies can be six sessions of weekly acoustic wave therapy, followed by a one-side firing of an 1440 nm laser.
More large-scale studies, particularly with respect to combination approaches, need to be conducted to evaluate the long-term results of therapies for cellulite in terms of safety, efficacy, and patient satisfaction.
References
- Angehrn F., Kuhn C., Voss A. Can cellulite be treated with low-energy extracorporeal shock wave therapy? Clin Interv Aging. 2007;2(4):623–630. doi: 10.2147/cia.s1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertin C., Zunino H., Pittet J.C., Beau P., Pineau P., Massonneau M. A double-blind evaluation of the activity of an anti-cellulite product containing retinol, caffeine, and ruscogenine by a combination of several non-invasive methods. J Cosmet Sci. 2001;52(4):199–210. [PubMed] [Google Scholar]
- Callaghan D.J.R., Robinson D.M., Kaminer M.S. Cellulite: A review of pathogenesis-directed therapy. Semin Cutan Med Surg. 2017;36(4):179–184. doi: 10.12788/j.sder.2017.031. [DOI] [PubMed] [Google Scholar]
- Casabona G., Pereira G. Microfocused ultrasound with visualization and calcium hydroxylapatite for improving skin laxity and cellulite appearance. Plast Reconstr Surg Glob Open. 2017;5(7) doi: 10.1097/GOX.0000000000001388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiBernardo B., Sasaki G., Katz B.E., Hunstad J.P., Petti C., Burns A.J. A multicenter study for a single, three-step laser treatment for cellulite using a 1440-nm Nd:YAG laser, a novel side-firing fiber, and a temperature-sensing cannula. Aesthet Surg J. 2013;33(4):576–584. doi: 10.1177/1090820X13480858. [DOI] [PubMed] [Google Scholar]
- DiBernardo B.E., Sasaki G.H., Katz B.E., Hunstad J.P., Petti C., Burns A.J. A multicenter study for cellulite treatment using a 1440-nm Nd:YAG wavelength laser with side-firing fiber. Aesthet Surg J. 2016;36(3):335–343. doi: 10.1093/asj/sjv203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J.B., Cohen J.L., Kaufman J., Metelitsa A.I., Kaminer M.S. Therapeutic approaches to cellulite. Semin Cutan Med Surg. 2015;34(3):140–143. doi: 10.12788/j.sder.2015.0169. [DOI] [PubMed] [Google Scholar]
- Kaminer M.S., Coleman W.P., III, Weiss R.A., Robinson D.M., Grossman J. A multicenter pivotal study to evaluate tissue stabilized-guided subcision using the Cellfina device for the treatment of cellulite with 3-year follow-up. Dermatol Surg. 2017;43(10):1240–1248. doi: 10.1097/DSS.0000000000001218. [DOI] [PubMed] [Google Scholar]
- Knobloch K., Kraemer R. Extracorporeal shock wave therapy (ESWT) for the treatment of cellulite--A current metaanalysis. Int J Surg. 2015;24(Pt B):210–217. doi: 10.1016/j.ijsu.2015.07.644. [DOI] [PubMed] [Google Scholar]
- Luebberding S., Krueger N., Sadick N.S. Cellulite: An evidence-based review. Am J Clin Dermatol. 2015;16(4):243–256. doi: 10.1007/s40257-015-0129-5. [DOI] [PubMed] [Google Scholar]
- Lupi O., Semenovitch I.J., Treu C., Bottino D., Bouskela E. Evaluation of the effects of caffeine in the microcirculation and edema on thighs and buttocks using the orthogonal polarization spectral imaging and clinical parameters. J Cosmet Dermatol. 2007;6(2):102–107. doi: 10.1111/j.1473-2165.2007.00304.x. [DOI] [PubMed] [Google Scholar]
- Nassar A.H., Dorizas A.S., Shafai A., Sadick N.S. A randomized, controlled clinical study to investigate the safety and efficacy of acoustic wave therapy in body contouring. Dermatol Surg. 2015;41(3):366–370. doi: 10.1097/DSS.0000000000000290. [DOI] [PubMed] [Google Scholar]
- Pierard-Franchimont C., Pierard G.E., Henry F., Vroome V., Cauwenbergh G. A randomized, placebo-controlled trial of topical retinol in the treatment of cellulite. Am J Clin Dermatol. 2000;1(6):369–374. doi: 10.2165/00128071-200001060-00005. [DOI] [PubMed] [Google Scholar]
- Quatresooz P., Xhauflaire-Uhoda E., Pierard-Franchimont C., Pierard G.E. Cellulite histopathology and related mechanobiology. Int J Cosmet Sci. 2006;28(3):207–210. doi: 10.1111/j.1467-2494.2006.00331.x. [DOI] [PubMed] [Google Scholar]
- Querleux B. Magnetic resonance imaging and spectroscopy of skin and subcutis. J Cosmet Dermatol. 2004;3(3):156–161. doi: 10.1111/j.1473-2130.2004.00118.x. [DOI] [PubMed] [Google Scholar]
- Querleux B., Cornillon C., Jolivet O., Bittoun J. Anatomy and physiology of subcutaneous adipose tissue by in vivo magnetic resonance imaging and spectroscopy: relationships with sex and presence of cellulite. Skin Res Technol. 2002;8(2):118–124. doi: 10.1034/j.1600-0846.2002.00331.x. [DOI] [PubMed] [Google Scholar]
- Romero C., Caballero N., Herrero M., Ruiz R., Sadick N.S., Trelles M.A. Effects of cellulite treatment with RF, IR light, mechanical massage and suction treating one buttock with the contralateral as a control. J Cosmet Laser Ther. 2008;10(4):193–201. doi: 10.1080/14764170802524403. [DOI] [PubMed] [Google Scholar]
- Russe-Wilflingseder K., Russe E., Vester J.C., Haller G., Novak P., Krotz A. Placebo controlled, prospectively randomized, double-blinded study for the investigation of the effectiveness and safety of the acoustic wave therapy (AWT((R))) for cellulite treatment. J Cosmet Laser Ther. 2013;15(3):155–162. doi: 10.3109/14764172.2012.759235. [DOI] [PubMed] [Google Scholar]
- Sadick N. Bipolar radiofrequency for facial rejuvenation. Facial Plast Surg Clin North Am. 2007;15(2):161–167. doi: 10.1016/j.fsc.2007.01.004. v. [DOI] [PubMed] [Google Scholar]
- Sadick N.S. Overview of ultrasound-assisted liposuction, and body contouring with cellulite reduction. Semin Cutan Med Surg. 2009;28(4):250–256. doi: 10.1016/j.sder.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Sadick N., Magro C. A study evaluating the safety and efficacy of the VelaSmooth system in the treatment of cellulite. J Cosmet Laser Ther. 2007;9(1):15–20. doi: 10.1080/14764170601134461. [DOI] [PubMed] [Google Scholar]
- Sadick N.S., Mulholland R.S. A prospective clinical study to evaluate the efficacy and safety of cellulite treatment using the combination of optical and RF energies for subcutaneous tissue heating. J Cosmet Laser Ther. 2004;6(4):187–190. doi: 10.1080/14764170410003039. [DOI] [PubMed] [Google Scholar]
- Sadick N., Rothaus K.O. Minimally invasive radiofrequency devices. Clin Plast Surg. 2016;43(3):567–575. doi: 10.1016/j.cps.2016.03.015. [DOI] [PubMed] [Google Scholar]
- Sadick N., Rothaus K.O. Aesthetic applications of radiofrequency devices. Clin Plast Surg. 2016;43(3):557–565. doi: 10.1016/j.cps.2016.03.014. [DOI] [PubMed] [Google Scholar]
- Sadick N., Sorhaindo L. The radiofrequency frontier: a review of radiofrequency and combined radiofrequency pulsed-light technology in aesthetic medicine. Facial Plast Surg. 2005;21(2):131–138. doi: 10.1055/s-2005-872414. [DOI] [PubMed] [Google Scholar]
- Sadick N.S., Nassar A.H., Dorizas A.S., Alexiades-Armenakas M. Bipolar and multipolar radiofrequency. Dermatol Surg. 2014;40(Suppl. 12):S174–S179. doi: 10.1097/DSS.0000000000000201. [DOI] [PubMed] [Google Scholar]
- Sasaki G.H. Single treatment of grades II and III cellulite using a minimally invasive 1,440-nm pulsed Nd:YAG laser and side-firing fiber: an institutional review board-approved study with a 24-month follow-up period. Aesthet Plast Surg. 2013;37(6):1073–1089. doi: 10.1007/s00266-013-0219-9. [DOI] [PubMed] [Google Scholar]
- Schlaudraff K.U., Kiessling M.C., Csaszar N.B., Schmitz C. Predictability of the individual clinical outcome of extracorporeal shock wave therapy for cellulite. Clin Cosmet Investig Dermatol. 2014;7:171–183. doi: 10.2147/CCID.S59851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanitphakdeedecha R., Sathaworawong A., Manuskiatti W., Sadick N.S. Efficacy of multipolar radiofrequency with pulsed magnetic field therapy for the treatment of abdominal cellulite. J Cosmet Laser Ther. 2017;19(4):205–209. doi: 10.1080/14764172.2017.1279332. [DOI] [PubMed] [Google Scholar]
- Yang K.K., Bennett N. The history of collagenase Clostridium histolyticum. Sex Med Rev. 2015;3(4):289–297. doi: 10.1002/smrj.54. [DOI] [PubMed] [Google Scholar]