Abstract
Newer understanding of volume loss as a critical component of facial aging and the integration of volume replacement into the surgical and nonsurgical therapeutic algorithm is arguably the most significant recent development in the field of facial rejuvenation. As all structural tissues play a role in the aging face, restoring youthful characteristics (or establishing them where they are congenitally absent) starts from the skeletal framework and builds progressively to the canvas of the face. The purpose of this article is to provide an introduction and brief summary of some of the current concepts concerning facial anatomy and the anatomy of facial aging, which serve as the basis for predictable and reproducible results with the use of injectable fillers. This article does not include the various types of fillers or techniques of filler injection, but covers how to decide where to use the filler and why, in different faces, as a result of the recognition and targeted correction of currently recognized specific anatomic deficiencies.
Keywords: Filler placement, anatomy of aging, facial volumization, facial analysis, facial fat compartments
Introduction
As noted by Pessa, “there are many arbitrary definitions of what constitutes a youthful face but the appearance of youth is not arbitrary; it is simply difficult to define” (Pessa et al., 2008). Facial morphology from infancy to old age is a complex, three-dimensional (3D) interplay of multiple structural tissue layers, and our understanding of this process is in a constant state of evolution and refinement. Current understanding of the facial aging process has historically been largely empirical, given that it has traditionally been based on the effectiveness of various treatments, both surgical and nonsurgical, aimed at rejuvenation but sometimes result in an odd or “done” appearance.
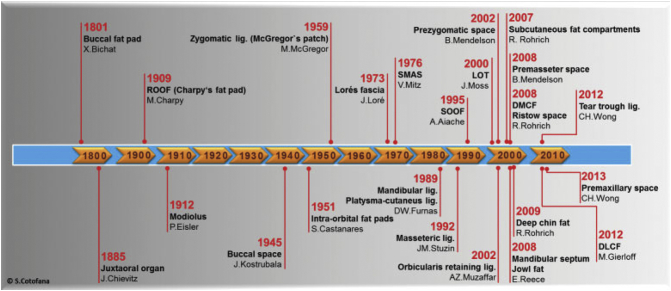
Although most of us would agree that this field is still in its infancy, a growing understanding of this complex process has informed and driven the change from an empiric approach to an anatomic one, in hopes of enabling improved and more natural-appearing results. Figure 1 was adapted from an article on facial aging by Cotofana et al. (2016) and provides an impressive illustration of how innovation and advances in technology, which have given us newer and faster ways to both gather and share information, are accelerating our understanding of facial anatomy (with more advances in the last few decades than in the last couple of centuries). This has led to a paradigm shift in the way we perceive and approach the changes that are observed in the aging face.
Fig. 1.
Timeline from 1800 to present, showing the date of the first description of important structures in the human face. DLCF, deep lateral cheek fat; DMCF, deep medial cheek fat; LOT, lateral orbital thickening; ROOF, retro-orbicularis oculi fat; SMAS, superficial musculoaponeurotic system; SOOF, suborbicularis oculi fat. Reproduced with permission from Cotofana et al. (2016).
At this time, facial aging research is defining the basic changes that occur in specific tissues, but it is how these changes affect what is observed in the aging face that remains to be defined (Rohrich and Pessa, 2012b). The answer to the question of whether we sink or we sag has become a yes to both. Newer understanding of volume loss as a critical component of facial aging and the integration of volume replacement into the surgical and nonsurgical therapeutic algorithm is arguably the most significant recent development in the field of facial rejuvenation. As all structural tissues play a role in the aging face, restoring youthful characteristics (or establishing them where they are congenitally absent) starts from the skeletal framework and builds progressively to the canvas of the face. Even with the aforementioned limitations in mind, with careful evaluation, some age-related changes or congenital deficiencies can now be addressed in a site-specific manner to achieve natural-looking results.
The purpose of this article is to provide an introduction and brief summary of some current concepts concerning facial anatomy and the anatomy of facial aging, which serve as the basis for predictable and reproducible results with the use of injectable fillers. This summary of current concepts is presented along with clinical examples of congenital absence or aging changes in each tissue layer to better illustrate the discussion. This article does not include various types of fillers or techniques of filler injection, but covers how to decide where to use the filler and why, in different faces, as a result of the recognition and targeted correction of currently recognized specific anatomic deficiencies.
The practical use of these concepts is illustrated using a number of clinical examples in women of different ages and ethnic backgrounds, along with a short description of where each face was treated and why, using both a layered anatomic (tissue structures) and regional approach (upper, mid, and lower face, shape, proportions). To examine a number of cases, as well as to compare and contrast different faces, these cases are presented in a composite format. This smaller format facilitates recognizing facial shapes and proportions and helps determine what is present or missing that may be moving faces away from ideal shapes and proportions.
Anatomy overview
Cumulative changes over time in all structural tissue layers of the face lead to a change in the morphology of the entire face in terms of shape, proportions, and topography. Changes in facial topography with aging sharpen the once smooth transition between anatomic units. In youth, the 3D surface contours of the face predominantly reflect light. Volume changes over time result in broken reflections with intervening shadows. This concept is critical to our understanding because seemingly subtle changes in light and shadow over time can have an enormous impact on our perception of a face in an almost indiscernible way. The rationale behind restoring 3D contours to the face as it ages, whether by lifting, tightening, or volume restoration, is easy to appreciate when looking at photographs that illustrate how aging takes us from 3D to 2D.
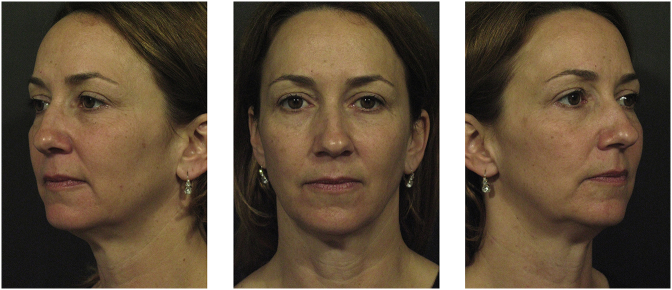
These changes can also be appreciated when looking at congenital asymmetry in a single individual. After neural tube development, the two sides of the body develop more like siblings than twins. The majority of individuals have a shorter, fuller side (usually the more attractive side in youth and the younger appearing side with age) and a longer, thinner side. The woman in Figure 2 appears more aged on her smaller right side compared with her fuller left side.
Fig. 2.
Less volumized side of the face in patient with mild asymmetry simulates the effects of volume loss in all layers with aging. Reproduced with permission from Fitzgerald and Vleggaar (2009).
Note that the less volumized side (right) of her face shows a clear delineation of her temple, lid, and cheek as separate entities, but the more volumized side (left) does not. One area appears to blend seamlessly with another, reflecting light uninterrupted by the shadows seen on the right. Less bony support and soft tissue in the upper face leads to a lower brow position, leading to lid lag laterally and an early hollowing A-frame deformity. There is less anterior and lateral cheek projection, a slightly deeper nasal sulcus, a longer upper lip, and an increased mental hollowing on the less volumized side, subtly affecting the perioral proportions in the lower third of her face. The convexity of the temple and the preauricular volume on the full side lends an overall oval shape to that side of her face that is lost due to the atrophy on the right. Finally, the volume loss on the initially smaller right side now contributes to a more pronounced ptosis and loss of jawline contour compared with the left side.
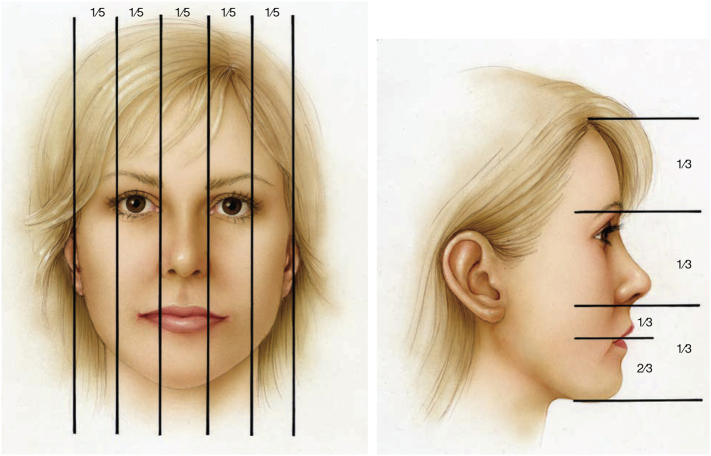
A comparison of each side with the ideal proportions of a youthful face (Fig. 3) depicts a width of five eyes across in vertical fifths, an equal volume in the upper, mid, and lower face when measured in horizontal thirds as well as the golden phi ratio of 1:1.6 in the perioral region of the lower third of the face. The fuller side of the face in Figure 2 is closer to these ideal proportions, providing a roadmap of where to revolumize the other side.
Fig. 3.
Facial proportions. (A) Vertical proportions are generally broken down into fifths based on the width of an eye. (B) Horizontal facial proportions are divided into thirds, measured from the hairline to the glabella, from the glabella to the subnasale, and from the subnasale to the menton. The lower third can be further broken down to the upper one-third, from the subnasale to the junction of the lips, and the lower two-thirds, from the junction of the lips to the menton. Reproduced with permission from Azizzadeh et al. (2007).
Lambros and Amos (2016) recently published an invaluable tool to visualize the facial aging process using 3D facial averaging. These are shown as static images in Figure 4 but can be viewed in animation online (http://links.lww.com/PRS/B922). Of note is the change in bony support in the superiomedial (under the medial brow) and inferiolateral orbit, as well under as the nose. Note the shadows that appear after flattening of the midface and lateral cheeks, the change in proportions in the lower third of the face, and the change from lip eversion in youth to inversion of the lips with aging.
Fig. 4.
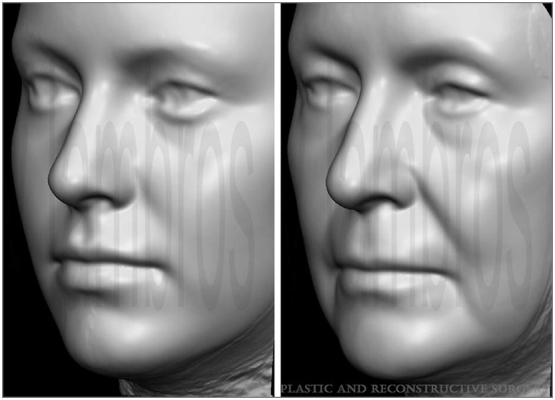
(Left) Average of facial surfaces of 116 female subjects, ages 20 to 30 years. (Right) Average of facial surfaces of 100 female subjects, ages 68 to 91 years (average, 76 years). Reproduced with permission from Lambros and Amos (2016). Three-dimensional facial averaging: Tool to understand facial aging. Image can be viewed animated online (http://links.lww.com/PRS/B922).
Regional anatomy: The facial thirds
The traditional regional approach to assessing the face is to consider the upper, middle, and lower thirds (Fig. 3). Glasgold et al. (2008) have greatly increased our appreciation that a detailed examination of the shadow patterns that develop in all areas of the face with volumetric facial aging will lead to a better understanding of how to apply volumetric techniques to create a natural-appearing result. The authors feel that the clues to a youthful and attractive appearance lie in the twin concepts of facial shape and shadows. Although every face is unique, the shadows that develop as we age are consistent. Not everyone develops every shadow, but the typical shadows of aging are universal. Glasgold et al. note the ease with which an artist can depict an aging face with a few shadow strokes, which makes this concept easy to grasp.
In the upper face, the upper eyelid, brow, temple, and forehead develop shadowing in the temple and upper orbit. A deep shadow of the temple sets off the lateral orbital rim and zygomatic arch. The eccentric shadow of the medial upper orbit leads to the A-frame changes of the upper eyelid. In the midface, the lower eyelid, cheek, and perioral area cast shadows in the inferior orbital rim that visually separate the eye from the cheek. The anterior cheek develops a midface hollow, which creates a parallel shadow to the nasolabial fold. The precanine fossa deepens into the nasolabial fold, and the buccal hollow shadow adds to the skeletal appearance of the zygoma.
The lower face (i.e., marionette, prejowl, and jawline) has two distinct components: the jawline and the perioral region. The labiomental hollow creates a U-shaped shadow that separates the lower lip from the chin, and the labiomental fold creates a distinct shadow that typifies the frown. The prejowl sulcus is the shadow in front of the jowl, and it is not uncommon to find shadowing in the lateral mandible behind the jowl.
The skin of the face has consistent attachment points to the underlying structures through the facial retaining ligaments, and as the volume of the face deflates, these attachment points will define most of the shadows that develop with age (Glasgold, 2015). These changes are well illustrated in the smaller side of the face in Figure 2, as well as the animated version of Figure 4.
Structural anatomy: Facial layers and functionality
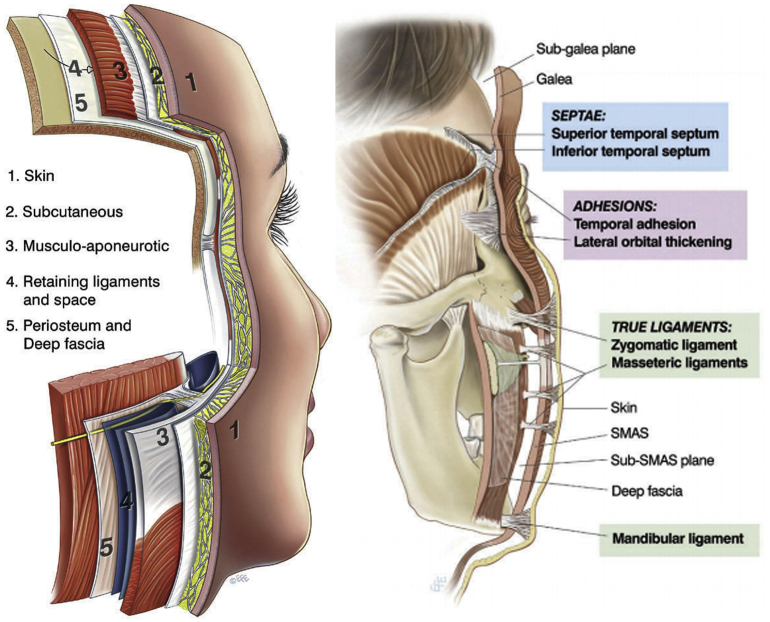
Mendelson and Wong (2013) suggest that, in addition to the traditional assessment of facial thirds, a more global understanding is facilitated by distinguishing between the different functional regions of the face and by considering the anatomy in terms of a layered construct. Their view is that the face can be divided into the highly mobile anterior face, which is functionally adapted for facial expressions, and the fixed lateral face, which overlies masticatory structures.
Mendelson and Wong (2013) conceptualize the soft tissues of the face as arranged concentrically into five basic layers that are bound together by a system of facial retaining ligaments, as first hypothesized by Stuzin et al. (1992). These facial layers and the vertical line of the retaining ligaments (layer 4), which separate the anterior and lateral face, are illustrated in Figure 5. The retaining ligaments of the face are responsible for binding the soft-tissue layers of the face to the underlying facial skeleton, from the dermis to the periosteum where bone is available, or otherwise to the deep fascia of the underlying structures, such as the parotid gland and the muscles of mastication.
Fig. 5.
(A) The face is constructed of five basic layers. This five-layered construct is most evident in the scalp but exists in the rest of the face, with significant modification and compaction for functional adaptation. Layer 4 is the most significantly modified layer, with alternating facial soft tissue spaces and retaining ligaments. (B) To secure the superficial fascia to the facial skeleton, a system of retaining ligaments binds the dermis to the skeleton, and the components of this system pass through all layers. There are three morphological forms of retaining ligaments of the face. SMAS, superficial musculoaponeurotic system. Reproduced with permission from Mendelson and Wong (2013).
Additionally, Mendelson and Wong’s extensive work supports that a large part of the sub–superficial musculoaponeurotic system (SMAS) layer 4 consists of soft tissue spaces that have defined boundaries that are strategically reinforced by retaining ligaments. Conceptually, these spaces are gliding planes that function to facilitate mobility of the superficial fascia (layers 1-3) over the deep fascia, as well as movement of the orbital part of the superficial fascia independent of the perioral part, and vice versa. Several soft-tissue spaces in the upper and lower face have now been described. As the roof of each space is the least supported part, it is more prone to developing laxity with aging compared with the ligament-reinforced boundaries. The authors feel that this differential laxity accounts for most of the characteristic changes that are observed in the aging face (Mendelson and Jacobson, 2008, Mendelson and Wong, 2013, Moss et al., 2000, Muzaffar et al., 2002, Wong et al., 2012).
Preprocedural facial assessment
No single algorithm addresses an aging face. As Pessa noted, although anatomy is consistent among most individuals, nuances of the anatomic structures makes each individual unique, and consequentially the onset and outcome of aging varies (Pessa and Rohrich, 2012). As discussed, at this time, facial aging research defines basic changes that occur in specific tissues, but how these changes affect what is observed in the aging face remains to be defined. Observing structural tissue changes that affect the face in front of us at a particular point in time may allow us to recognize how some of these changes affect the shape, proportions, topography, and frames of that face and help us choose which area to treat.
When assessing the face, it is useful to consider what causes that face to deviate from the ideal proportions shown in Figure 3, which shows an ovalized upside-down-egg shape, an anterior convexity, an oval frame, youthful proportions of five eyes across, and three relatively equal thirds of the face. For instance, is masseteric hypertrophy squaring off the face? Is volume loss in the temples and lateral cheek fat altering the facial shape? Is the loss of anterior/lateral cheek projection making a young face appear wider? What you choose to address depends on the extent of the changes observed in each structural layer or region and the parity of these changes between the layers or regions. If there is just a little change in all layers, almost any interventional approach will work. Others need focused attention to one structural tissue layer (i.e., replace lost fat in HIV or congenital lipoatrophy, enhance bony support in congenital craniofacial hypoplasia, or tighten or trim an elastotic overlying skin envelope; Fig. 6).
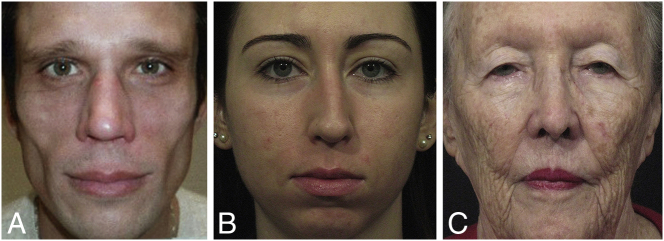
Fig. 6.
Individual variations in the onset and outcome of aging are commonplace. Many individuals age with relative parity in all structural tissue layers, but some are mostly a one tissue issue. (A) Young man with good bone structure and good skin, but extreme loss of fat. (B) Young woman with good skin and soft tissue volume, but congenital lack of craniofacial support. (C) Elderly woman who has good bone structure and ample soft tissue, but very elastotic skin. Photographs courtesy of Rebecca Fitzgerald, MD.
Determine whether regionally “one of these things is not like the other.” If there is a regional disparity between the thirds of the face, try to blend them all back to a more similar place. An obvious congenital issue is a suboptimal chin, which affects the perception of the jawline, lips, and facial frame. Common disparities in facial rejuvenation may arise from the preferential treatment of the midface or lips without regard to atrophic temples and perioral bone loss. Restoring volume in the temples and chin has a large effect on the facial shape. Finally, treating an isolated problem without regard for how it affects the entire face at any age may lead to an odd appearance. This is most commonly seen with over-aggressive filling of the tear trough, where too much product placed too high gives an unnatural contour, or in the upper lip with no surrounding support.
A recent extensive review of research on facial beauty determined that four characteristics emerge as the most statistically significant determinants of attractiveness: youthfulness, sexual dimorphism, averageness (prototypicality), and symmetry (Bashour, 2006). This information has some important clinical correlations. For instance, averageness requires harmony of all regions of the face, young or old. Sexual dimorphism requires recognition of sex differences. Men often have a stronger forehead and straighter brow, a cheek apex that is lower and more medial, and a stronger chin and jawline than females. Conversely, women’s faces have a higher, more lateral cheek apex and a more tapered lower face than men.
Note that this review included symmetry. The contribution of symmetry to beauty is often maligned by showing an original photograph along with pictures made using the two right and two left sides of that face, often showing a bizarre-looking thin face and fat face. However, if the original face is truly symmetric, then all three photographs would be identical. In one author’s experience (RF), augmenting the volume around the temple, brow, orbit, and zygomatic arch just enough to restore more symmetrical light reflection from both sides can make a surprisingly positive difference in our perception of that face.
Aging of the face, of course, affects much more than esthetics. The face (in particular the upper face) conveys a wide range of expressions, representing a critical nonverbal form of communication that is fundamental to all social interactions (Kirkpatrick et al., 1996). Changes commonly seen with aging may communicate an unintended message of anger, sadness, or fatigue. In fact, “I don’t mind getting older, I just don’t want to look mad, sad, or tired” is one of the most common presenting complaints from patients.
Finally, it is prudent to let the patient know prior to any intervention that their baseline tissue quality will ultimately determine the final outcome of the intervention. An individual with very depleted fat volume (e.g., HIV, congenital lipoatrophy, endurance exercise) will be more challenging to revolumize and will require frequent touch-ups to sustain that volume. An older patient with advanced bony remodeling, fat loss, and elastotic skin may be treated successfully with fillers; however, the procedure may require a lot of product and surgical interventions (e.g., lift), and fat augmentation may be a better option for that individual.
Managing expectations will decrease frustration for both the patient and the practitioner. Conversely, as a general rule, fuller and younger faces bring in their own volume; therefore, these are more easily reshaped with a conservative amount of filler, making this a good place to start for the novice injector.
Current concepts in anatomy of aging
Skin (layer 1)
Skin appearance (e.g., elasticity, absence of wrinkles, smooth texture, and clarity and evenness of color) is a primary indicator of age. A major feature of aged skin is fragmentation of the dermal collagen matrix, which occurs mostly due to extrinsic aging from long-wave ultraviolet light. Fibroblasts cannot attach to fragmented collagen, preventing stretching, which is critical for the normal, balanced production of collagen and collagen-degrading enzymes. This imbalance advances the aging process in a self-perpetuating, never-ending deleterious cycle.
There is some evidence that cross-linked hyaluronic acid (HA) may substitute for fragmented collagen in restoring extracellular matrix required for normal activity of fibroblasts (Landau and Fagien, 2015). Anecdotal skin improvement has also been observed in patients treated with fat augmentation or poly-l-lactic acid (PLLA). Within the scope of this paper, suffice it to say that healthy skin can accommodate for mild-to-moderate volume loss, sometimes even “camouflaging” the progression of aging changes in other tissue layers for a time. In these patients a conservative amount of filler will usually make a nice difference. However, the opposite is true in an elastotic outer skin envelope, which means that fillers alone may not be able to deliver the desired result unless paired with a (surgical or nonsurgical) skin tightening procedure.
Fat (layer 2)
Only a decade ago, Rohrich and Pessa (2007) published their landmark discovery that facial fat exists in discrete compartments rather than in a homogeneous sheet over the face. Their initial studies used dye sequestration in cadaveric dissections, and subsequent studies used radiopaque dye and 3D imaging to identify both superficial and deep compartments. This refined our understanding of these structures as targets for facial rejuvenation (Pessa and Rohrich, 2012, Rohrich and Pessa, 2009, Rohrich and Pessa, 2012a, Rohrich et al., 2009).
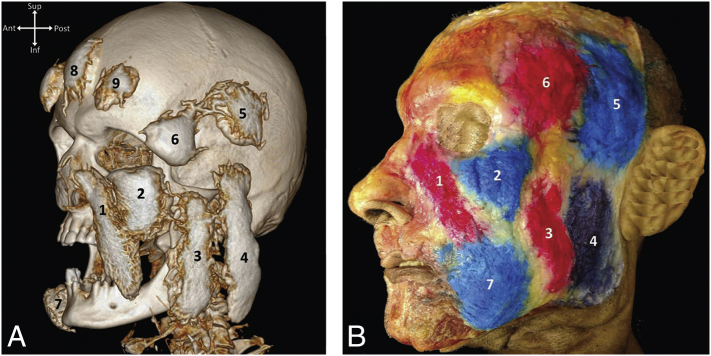
An early dye sequestration study by Rohrich et al. (2008) showed that inflation of the deep medial cheek fat (DMCF) with saline in a cadaveric specimen eliminated V deformity, reduced the size of the nasolabial fold, and diminished the appearance of the tear trough. The subsequent study by Gierloff et al. (2012a) using radiopaque dye and 3D imaging confirmed that the deep fat of the midface was comprised of medial and lateral suborbicularis oculi fat compartments (SOOF) and refined the initial dye study by showing that the deep mid-cheek compartment exists in discreet medial (DMCF) and lateral (deep lateral cheek fat [DLCF]) compartments as well. The researchers also identified a discrete midfacial compartment they termed the “buccal extension of the buccal fat,” which they feel serves to support the compartments superior to it. Schematics of the superficial and deep fat compartments of the face from Gierloff’s study are shown in Figure 7 and can be reviewed repeatedly throughout this section for orientation.
Fig. 7.
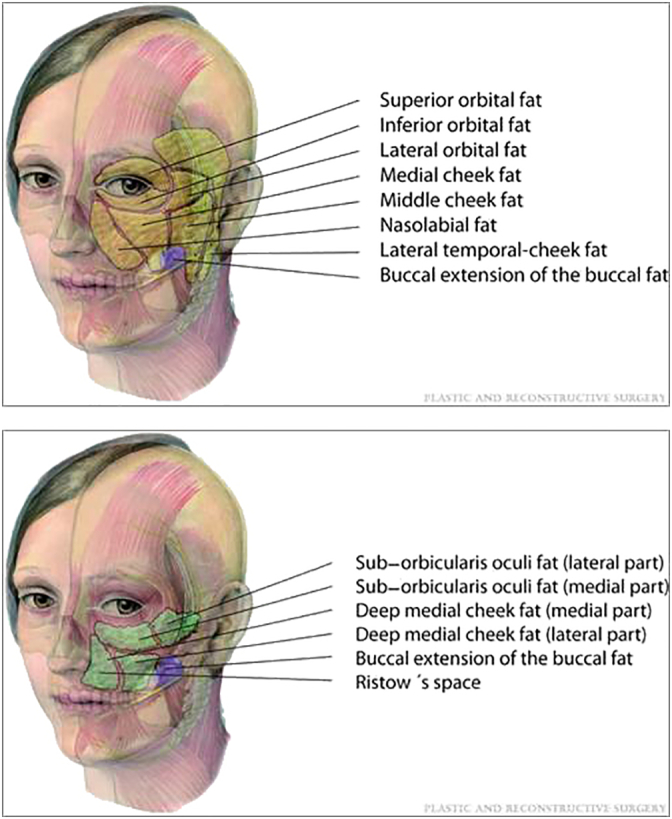
Schematic of the superficial and deep fat compartments. The superficial layer is composed of the nasolabial, medial cheek, middle cheek, and lateral temporal cheek compartments, as well as the three orbital compartments. The deep layer is composed of the suborbicularis oculi fat (medial SOOF and lateral SOOF) and the deep medial cheek fat (medial DMFC and lateral DLCF). A deep compartment termed Ristow’s space is located posterior to the most medial aspect of the deep medial cheek fat and lateral to the pyriform aperture. Reproduced with permission from Gierloff et al., 2012a, Gierloff et al., 2012b.
The latest study of superficial compartments by Schenck et al. (2018) is in agreement with the previous studies (Fig. 8). This study also provides evidence that these compartments behave differently when injected with soft-tissue fillers. An injection of volumizing material leads to an inferior displacement of the superficial nasolabial, middle cheek, and jowl compartments. An injection into the medial cheek, lateral cheek, and superficial temporal compartments leads to an increase in volume without inferior displacement.(i.e., an increase in local projection). Further research indicates that regional metabolic differences may exist between these compartments that contribute to the morphologic changes in the aging face (Wan et al., 2014).
Fig. 8.
(A) Three-dimensional reconstruction of a contrast enhanced computed tomography (CT) scan. The superficial (subcutaneous) facial fat compartments have been injected with radiopaque dye. (B) Cadaveric dissection of the left side of a face after the same fat compartments have been injected with colored dye. Note that in this latter specimen, the tear trough, lateral orbital thickening, and area of the zygomatic arch did not stain. The dye did not migrate inferior to the nasolabial sulcus or medial to the labiomandibular sulcus. The superficial (subcutaneous) facial fat compartments shown are (1) superficial nasolabial, (2) medial cheek, (3) middle cheek, (4) lateral cheek, (5) superficial superior temporal, (6) superficial inferior temporal, and (7) jowl. The superficial central (8) and superficial lateral (9) forehead compartments are visualized in the CT image. Reproduced with permission from Schenck et al. (2018).
Clinical observation suggests that these compartments may age variably, both between individuals and between compartments in one individual (Rohrich and Pessa, 2007). Focused localized injection of fat and/or soft-tissue filler into discrete compartments can have a dramatic effect on facial volume and reshaping of the soft tissues of the face into an anatomically more youthful position (Fitzgerald and Rubin, 2014). We discuss a few examples to illustrate.
Forehead
Figure 8A illustrates the superficial facial fat compartments, including the central and lateral forehead fat compartments. Volumizing these compartments will recontour the convexity of the forehead (Figs. 8B and C), and can add height and convexity to the forehead (Fig. 9).
Fig. 9.

The upper third of the patient’s face is somewhat smaller and flatter than the lower two thirds, which looks more proportional and convex after treatment of the upper forehead at the hairline (using hyaluronic acid [HA]) with a 25-gauge cannula in the subgaleal space). The temples were also treated (HA placed on the bone with a 25-gauge needle). A very slight enhancement of the midface convexity was achieved by injecting HA into the prezygomatic space (25-gauge cannula), pyriform space (26-gauge needle after aspiration), and submentalis and labiomandibular fat compartments. On closer observation, the patient may have benefited from treatment in the superficial middle fat compartment (appreciated in the three quarter view) and the superficial lateral cheek compartment adjacent to the earlobe. Photographs courtesy of Rebecca Fitzgerald, MD.
Brow
Replenishing the deep fat of the retro-orbicularis oculi fat pads that sit underneath the brows can result in anterior projection of the brow region (Fitzgerald, 2013). This results in the youthful feature of a parallel brow, lid sulcus, and lash line (Fig. 10).
Fig. 10.
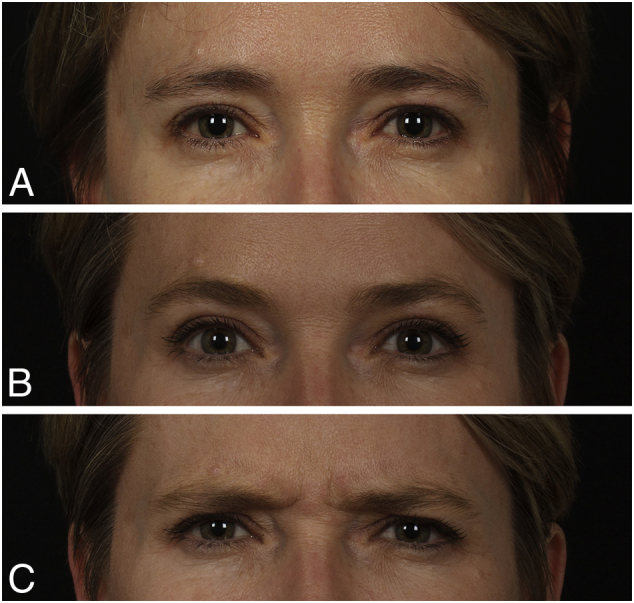
(A) Patient (age 40s) was treated along her lateral upper lid and brow and her temples. (B) The after picture shows an anterior projection of the brows and lid after placement of product in the retro-orbicularis oculi fat (using hyaluronic acid and 25-gauge cannula), which gives the eye the youthful feature of a parallel brow, lid sulcus, and lash line. (C) Patient is shown frowning to demonstrate that this effect is not from a neuromodulator. Reproduced with permission from Azizzadeh et al. (2018).
Temple
Atrophy of the temporal fat pad and superior preauricular fat areas posterior to the hairline can result in a peanut-shaped face, which can be restored to an oval shape with volume augmentation (Fig. 11).
Fig. 11.
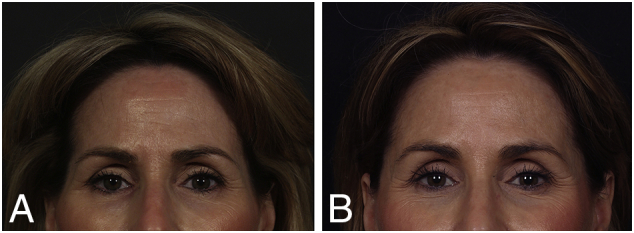
(A) Patient lost temporal fat and superior preauricular fat area posterior to the hairline. Note that this affects the shape of her face, which is no longer 5-eyes across in the upper third. (B) This is restored with volume augmentation in this area. Reproduced with permission from Fitzgerald and Rubin (2014).
Lateral cheek fat
Figure 12 shows a patient with loss of lateral cheek fat, resulting in a concave lateral cheek appearance and visibility of the tragus in anterior view. After volumization in this area, the tragus is no longer visible, and the facial shape is improved.
Fig. 12.

(A) Patient has some shadowing in her temples; however, the striking loss of lateral cheek fat is what gives the lateral area of her midface a concave appearance. (B) Treatment in this area restores an oval facial frame. The tragus is visible in an anterior view in a patient without lateral cheek fat and is less visible when this area is full. This defect is not uncommon in thin patients after face lifting. Hyaluronic acid was used with a 25-gauge cannula. Reproduced with permission from Azizzadeh et al. (2018).
Deep midfacial fat
As previously noted, SOOF and the deep cheek fat exist in both the medial and lateral compartments. Computed tomography (CT) imaging of deep midfacial fat pads with clinical correlation is illustrated in Figure 13. This image does not show the DLCF, which is shown in Figure 14 in a cadaveric specimen, and lies just medial to the zygomatic major muscle, inferior to the SOOF. Note that this compartment lies directly on the bone.
Fig 13.
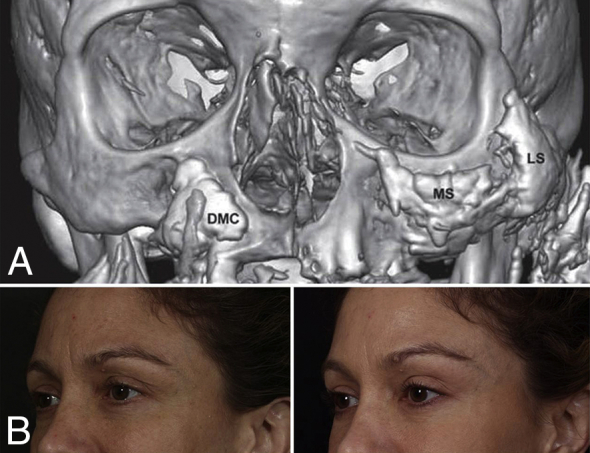
(A) Deep midfacial fat compartments. The deep medial cheek fat is composed of a medial part and a lateral part (not shown). The medial part extends medially almost to the lateral incisor tooth. Augmentation of the deep medial cheek fat will consequently elevate and efface the nasolabial fold. The suborbicularis oculi fat is composed of a medial part and lateral part. With aging, inferior migration of these compartments occurs, as well as an inferior volume shift within the compartments, as seen on this computed tomography (CT) image. Reproduced from Gierloff et al., 2012a, Gierloff et al., 2012b. (B) Before and after hyaluronic acid filler was placed in the fat compartments shown in the CT image using a 25 gauge cannula. Improvement can be seen on the right side of the face in the three-quarter view. The patient was also treated along the lateral upper lid and brow as well as the temples, similar to the patient in Figure 10; however, neuromodulater was also used in the glabella and crow’s feet. Note the increased improvement when both filler and neuromodulater are used together. Reproduced with permission from Fitzgerald and Rubin (2014).
Fig. 14.
View of the right and left infraorbital region of layer 4 (deep to the OOM) in a female (A) and male (B) fresh-frozen specimen. (A) The PZ and lateral part of the deep cheek fat (DLCF) are circled. The hash symbol indicates the zygomaticus major muscle with its broadly based fibrous origin. This long attachment represents the lateral-inferior boundary of the DLCF. The facial vein is marked by the arrows and represents the medial-inferior boundary of the DLCF. The OOM is flipped toward the nose to expose the BB where this muscle attaches on the orbital rim. (B) Dye has been injected into the prezygomatic space (red and blue) and the lateral part of the DMCF (DLCF, green). The injection was performed with constant contact to the bone during application in all three locations. The red and blue areas correspond to the medial (MS) and lateral SOOF (LS). The hash symbol indicates zygomaticus major muscle with its broadly based fibrous origin; BB, bare bone area after sharp removal of the OOM from its attachment on the orbital rim. The asterisk marks the levator labii superioris alaeque nasi muscle. The arrows point to the facial vein. BB, Bare bone; DLCF, deep lateral cheek fat; DMCF, deep medial cheek fat; LS, lateral suborbicularis oculi fat; MS, medial suborbicularis oculi fat; OOM, orbicularis oculi muscle; PZ, prezygomatic space; SOOF, suborbicularis oculi fat. Reproduced with permission from Cotofana et al. (2015).
Figure 15 illustrates the clinical appearance of both the presence and absence of deep midface fat. The first woman is a patient with congenital lipoatrophy and extreme loss of superficial fat but has intact medial and lateral SOOF and deep cheek fat, resulting in a convex midface. The loss of this deep midfacial fat in the other woman reveals the ligamentous attachments around the orbit. As noted previously, the skin of the face has consistent attachment points to the underlying structures through the facial retaining ligaments, and when the volume of the face deflates, these attachment points will define most of the shadows that develop with age. Note that the tear trough and nasojugal fold are more visible on this patient’s less volumized right side.
Fig. 15.
Clinical correlation of superficial and deep midfacial facial fat compartments. (A) In the first face pictured, deep midfacial fat is visible clinically. There is no visible undereye hollowing or nasolabial fold, and there is a convex contour to the midface. However, due to a congenital lipodystrophy, there is a striking lack of superficial fat. This is most obvious in the lateral temporal cheek compartment and upper periorbital area. However, on closer observation, the lack of superficial fat in the midface results in a good deal of shadowing in the lower lateral cheeks. When this face with ample deep midfacial fat is compared to the second face (B), the endurance exercise patient has only slight loss of the superficial fat, with only a small amount of shadowing in the temples and lateral cheeks, but a loss of fat in the deep midfacial compartments, which leads to a lack of midfacial projection and a very visible lid-cheek junction. Both patients are slightly asymmetric with the smaller side on their right. There is increased visibility of the zygomatic muscle on the smaller side of the first patient, and shape difference in the cheeks of the second patient with more deep midfacial fat on the left side, especially in the area of the lat SOOF and DLCF. Photographs courtesy of Rebecca Fitzgerald, MD.
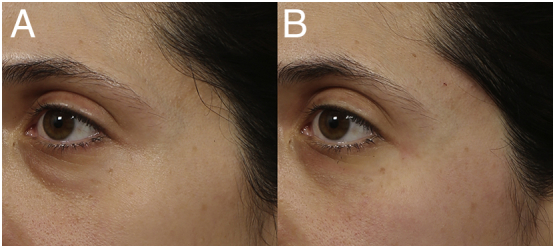
The replacement of deep midfacial fat in the older patient pictured in Figure 16 camouflages the mild orbital fat herniation that was left visible by its absence. Note the slight difference in the clinical appearance/shadow patterns of the differing volume in these four deep midfacial fat compartments on the more (her left) and less (her right) volumized sides of her face.
Fig. 16.

(A) Before and (B) after camouflage of the nasojugal folds following volume augmentation of the four deep midfacial fat compartments (medial and lateral SOOF using hyaluronic acid and a 25-gauge cannula, and the deep medial cheek fat [DMCF] and deep lateral cheek fat [DLCF] using calcium hydroxylapatite and a 25-gauge cannula) is possible in this patient because she has strong midfacial bone structure, her orbital fat herniation does not exceed the volume loss in her deep midfacial fat, and her skin has good elasticity. On close observation, the difference in the volume of the DMCF and DLCF can be discerned between the larger (left) and smaller (right) sides of the face in the before picture. Photographs courtesy of Rebecca Fitzgerald, MD.
Lips
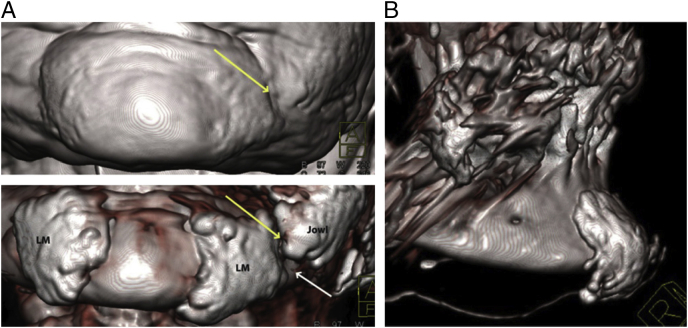
Performing lip augmentation without addressing the surrounding structures, both skeletal and soft tissue, may result in unnatural appearing duck lips. Note in Figure 17 how the fat deep to the orbicularis oris muscle helps serve to evert the upper and lower lip margins and blend the vermillion lip in with the cutaneous portion of the lip. Filler placed directly in the vermillion border in a patient without surrounding soft tissue support may do just the opposite, disconnecting the vermillion from the cutaneous lip (Fig. 18). Soft tissue support inferior to this area is equally important. Imaging studies of superficial labiomandibular fat compartments by Gierloff et al. (2012b); Fig. 19) demonstrated that increased volume in this region resulted in less of a marionette fold (albeit in a small sample size), making this compartment an important target when treating these folds.
Fig. 17.
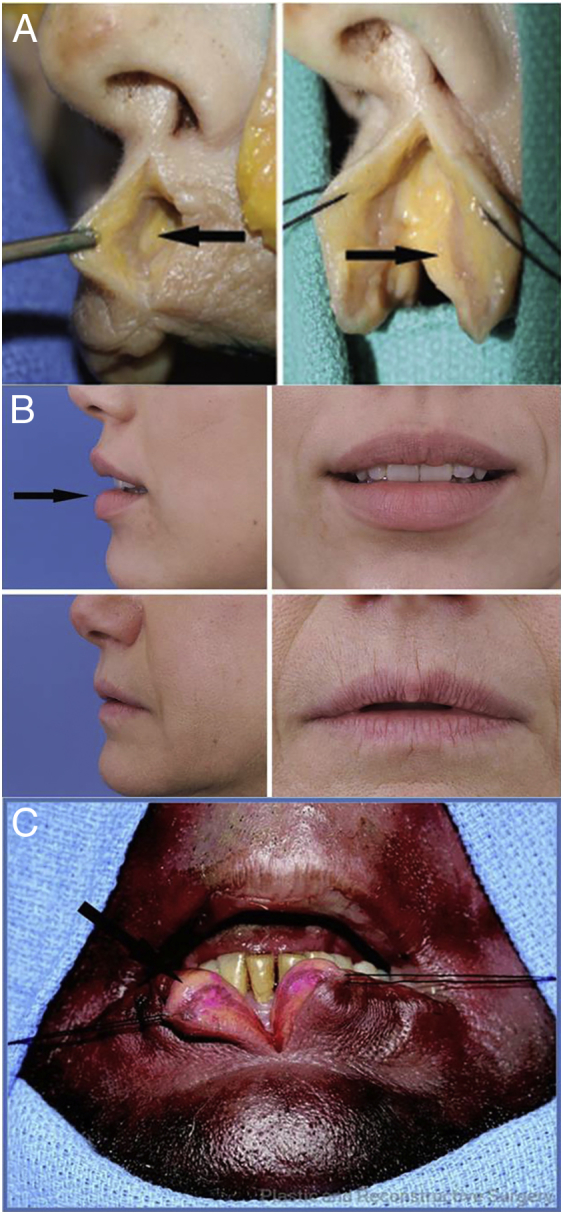
Just as there is suborbicularis fat around the eye, there is suborbicularis fat in the perioral region. Histologic examination confirms the macroscopic finding that the orbicularis insertion defines the wet-dry border of the lip. (A) Vertical sectioning of the upper lip reveals fat deep to the orbicularis oris muscle (arrow) and superficial to the buccal mucosa. (B) The clinical impression from this research is that the volume of deep lip fat contributes significantly to the appearance of the youthful lip. (C) Vertical sectioning of the lower lip shows deep submuscular fat (arrow). Of particular note, this specimen’s lower lip, which contained an ample amount of submuscular fat, showed anterior projection and eversion similar to that seen in a much younger individual. Reproduced with permission from Rohrich et al., 2008, Rohrich et al., 2009.
Fig. 18.

(A; top and bottom) After a previous injection, the patient’s lips appeared unnatural. (B; (top and bottom) Removing suboptimally placed filler in the vermillion border and body of the lip (with hyaluronidase) followed by placement of filler (using hyaluronic acid and a 25-gauge cannula) in a submuscular location in the mucosal and cutaneous portion of the patient’s upper and lower lip, as well as in the lateral and anterior chin, provide more support for the lips and a more natural-appearing result. Reproduced with permission from Fitzgerald and Rubin (2014).
Fig. 19.
(A) Volume-rendered three-dimensional spiral computed tomography (CT) image of the lower face, demonstrating the surface of the skin (above) and anterior part of the mandible with the labiomandibular fat compartments (LM) and the left inferior jowl fat (below). The yellow arrows indicate the position of the labiomandibular fold. The white arrow indicates the position of the mandibular retaining ligament. (B) Volume-rendered three-dimensional spiral CT image of the chin, demonstrating the submentalis fat. Note that this compartment does not lie immediately adjacent to the mentolabial sulcus. With permission from Gierloff et al., 2012a, Gierloff et al., 2012b.
Finally, overfilling directly in the vermillion border may blunt the definition of this border in younger and older patients with or without surrounding support. Figure 18 shows how dissolving the filler in the vermillion border, followed by judicious filling of the suborbicular oris fat in the upper and lower lips and in the labiomental fat compartments results in more natural appearing lips. This patient was also treated around the pyriform aperture.
Facial muscles (layer 3)
The mimetic muscles of the face are located in the superficial fascia of the anterior face, made up of the skin, fat, and the SMAS. The question of whether facial mimetic muscles age histologically or physiologically in response to the aging process or secondary to the changes that occur with the aging of neighboring structures is not yet clear. What is currently clear is that clinically, these mimetic muscles appear to tighten in the face and neck with age and that this can be mitigated with chemodenervation. Additionally, the relatively fixed lateral face overlies the masticatory structures, including the temporalis and masseter muscles. Hypertrophy in these muscles is not uncommon, may greatly affect facial shape, and is readily treated with neuromodulaters.
Ligaments and facial spaces (layer 4)
Layer 4 contains the facial ligaments that attach the superficial fascia (layers 1-3) to the underlying skeleton and the soft tissue spaces, which allows the superficial fascia to glide over the deep fascia or periosteum (layer 5; Fig. 5). As previously noted, the skin of the face has consistent attachment points to the underlying structures through the facial retaining ligaments, and as the volume of the face deflates, these attachment points will define most of the shadows that develop with age (Glasgold, 2015). The most relevant ligaments in the midface are the orbital retaining ligament, malar septum (zygomaticocutaneous ligament), and the McGregors patch (zygomatic ligament). Relevant lower face ligaments include the parotid masseteric ligaments and the platysma attachments to the mandibular ligament (Mendelson and Wong, 2013).
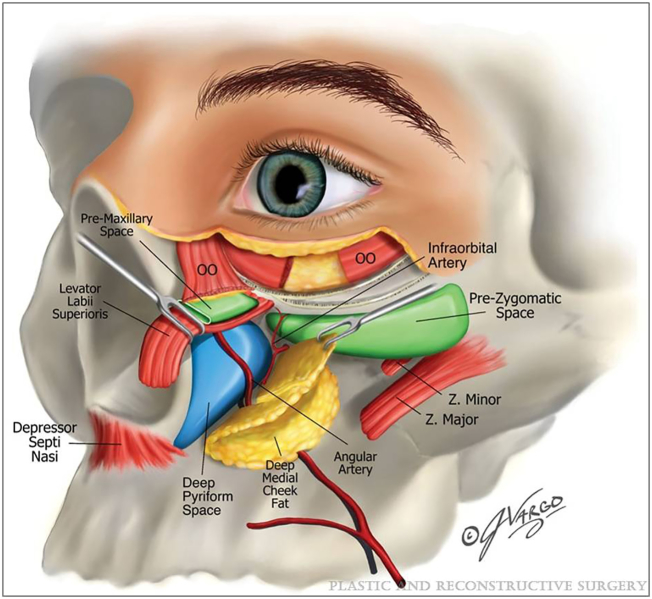
The discovery of the prezygomatic and premaxillary space and their anatomical implications for rhytidectomies and midface cheek lifts are now well documented (Mendelson and Jacobson, 2008, Moss et al., 2000, Muzaffar et al., 2002, Wong et al., 2012). The utility of these spaces for injection-based procedures has only recently been described (Surek et al., 2015a). Herein, we discuss injection-based procedures in the prezygomatic space (PZS) and pyriform space, which are illustrated in the schematic in Figure 20.
Fig. 20.
Schematic illustration of the prezygomatic space (PZS), deep pyriform space, and important adjacent structures. Reproduced with permission from Surek et al. (2016).
The PZS, which is pictured in Figure 20, is a triangular space over the body of the zygoma that is bounded superiorly by the orbicularis retaining ligament and inferiorly by the zygomatic ligaments. The floor of the PZS is covered by a layer of preperiosteal (PP) fat. The orbital part of the orbicularis oculi forms the roof of the space. Recent research has delineated the difference between the PP fat and the SOOF. The PP fat is deep to the PZS. Encapsulating the PZS is a uniform fibrous lining that begins superficially at the posterior capsule of the orbicularis oculi muscle, traverses inferiorly within the zygomatico-cutaneous ligaments, and ascends over the PP fat to coalesce with the arcus marginalis-orbitomalar ligament junction and forms the prezygomatic capsule. The SOOF lies superficial to the PP fat, deep to the orbicularis oculi muscle, and maintains a loose areolar consistency (Surek et al., 2015a).
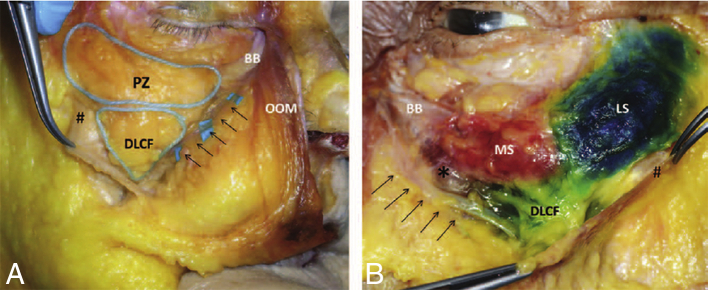
Cadaveric dissections of the PZS are illustrated in Figures 21A and B, and the clinical correlation is illustrated in Figure 22. As previously noted, a buccal extension of the buccal fat compartment was identified in the Gierloff study (Gierloff et al., 2012a, Gierloff et al., 2012b; Fig. 7), which the authors felt serves to support the compartments superior to it. However, even though injection of filler into this central lobe of the buccal fat may improve volume deficiency and support in that region of the face, one must avoid injecting into the inferior lobe of the buccal fat because this may lead to more prominent jowling of the cheeks and an undesired aesthetic result through a cavernous connection (referred to as the buccal recess; Fig. 21B).
Fig. 21.
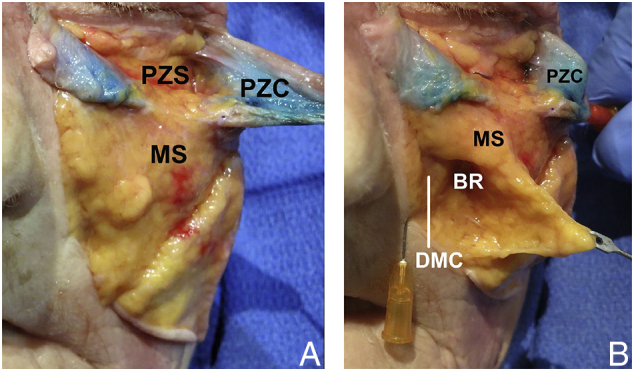
(A) Layered dissection of the midface in an elderly male fresh cadaver after percutaneous injection of red dyed hyaluronic acid in the left hemiface. The orbicularis retaining ligament together with the periosteum of the orbital rim and orbital septum forms the arcus marginalis. In this dissection, the arcus marginalis was released to unveil the prezygomatic space. The superficial medial cheek fat is labeled for orientation. The prezygomatic capsule (PZC) is dyed with methylene blue. (B) The superficial medial cheek fat has been retracted to reveal the deep medial cheek fat and cavernous connection in the buccal recess. Reproduced with permission from Surek et al 2016.
Fig. 22.
(A) Patient with a shallow orbit, retrusive anterior maxilla, and inferior orbital rim. When the cornea has more anterior projection than the bony infraorbital rim, it is referred to as a negative vector, and a deep tear trough (TT) is often seen in these patients. The amount of filler required to correct the deep TT directly in these patients often results in an unnatural undereye contour and a Tyndall effect. A more natural-appearing correction can be achieved by providing volume support in the prezygomatic space and the pyriform aperature, as well as in the deep midfacial fat prior to treating the TT. (B) Patient after volumizing the prezygomatic space (hyaluronic acid administered with a 25 gauge cannula), which volumizes the inferiolateral rim and minimizes the amount of filler needed to fill the TT (which has not yet been filled). Photographs courtesy of Rebecca Fitzgerald, MD.
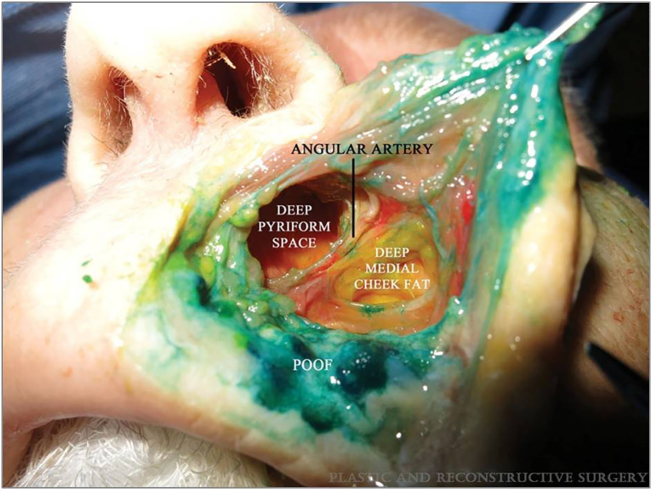
Finally, Surek et al. (2016) dissected 12 hemifacial fresh cadaver specimens to define the anatomical boundaries and clinical implications of the area termed Ristow’s space in the early studies by both Rohrich et al. (2008) and Gierloff et al. (2012a). The study revealed a deep midface cavity cradled by the pyriform aperture and a deep medial cheek compartment they renamed the deep pyriform space (Fig. 20). Pneumatization of this space traversed cephalic to the level of the tear trough ligament in a plane deep to the premaxillary space. The authors note that bony recession of the maxilla with age predisposes this space for use as a potential area of deep volumization to support overlying cheek fat and draping lip elevators, and it may prove to be a vital target area for restructuring the aging anterior midface. This will be addressed further in the section on bone. The position of the angular artery in the roof of the space allows safe injection on the bone without concern for vascular injury (Fig. 23).
Fig. 23.
Deep pyriform space is cradled medially by the pyriform aperture and depressor septi nasi. The angular artery courses between the space and deep medial cheek fat compartment. Note that the artery is not directly on the periosteum, but rather superficial and lateral within the roof of the space. Postorbicularis oris fat is stained green. Reproduced with permission from Surek et al. (2016).
Periosteum and deep fascia (layer 5)
The deep fascia (deepest soft tissue layer of the face) is formed by the periosteum and overlies the bone. Over the lateral face, where the muscles of mastication (temporalis and masseter) overlie the bone, the deep fascia is instead the fascial covering of the muscles, the deep temporal fascia above the zygomatic arch, and masseteric fascia below the arch.
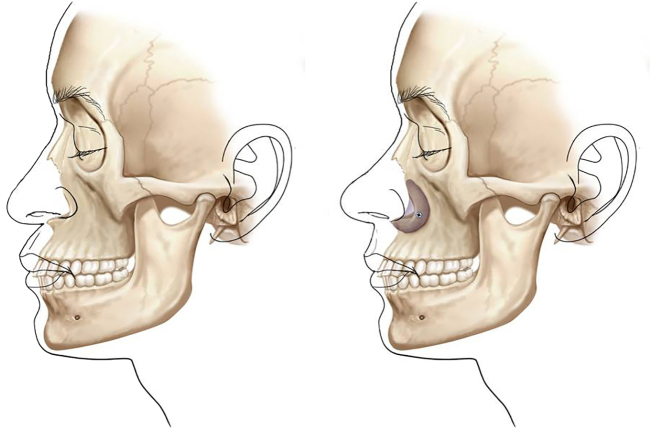
Bone
The main concept can be summarized by stating that morphologic changes in bony structures affect soft-tissue position. The presence and maintenance of bone volume and contour is necessary to preserve soft-tissue relationships. Aging, bony trauma, and congenital bony abnormalities can all result in soft tissue distortion. Improvements in imaging technology have enabled a better understanding of facial skeletal aging than previously possible. Shaw and Kahn (2007) used 3D renderings of CT findings in 60 male and 60 female individuals, studied in three different age groups, and provided evidence that aging of the facial skeleton includes selective remodeling at specific sites, including a change in the size and contour of the orbit; a decrease in the glabellar, pyriform, and maxillary angles; and an increase in the size of the pyriform aperature.
Mendelson and Wong (2012) summarized the findings of this and other nonlongitudinal studies in an excellent comprehensive review and illustrated the statistically significant findings in a schematic (Fig. 24). The size of the arrow in the schematic correlates with the amount of resorption. Note that these changes can be appreciated by comparing the asymmetric sides of the face in Figure 2 and in the still (and even more so in the animated) composite images of Figure 4.
Fig. 24.
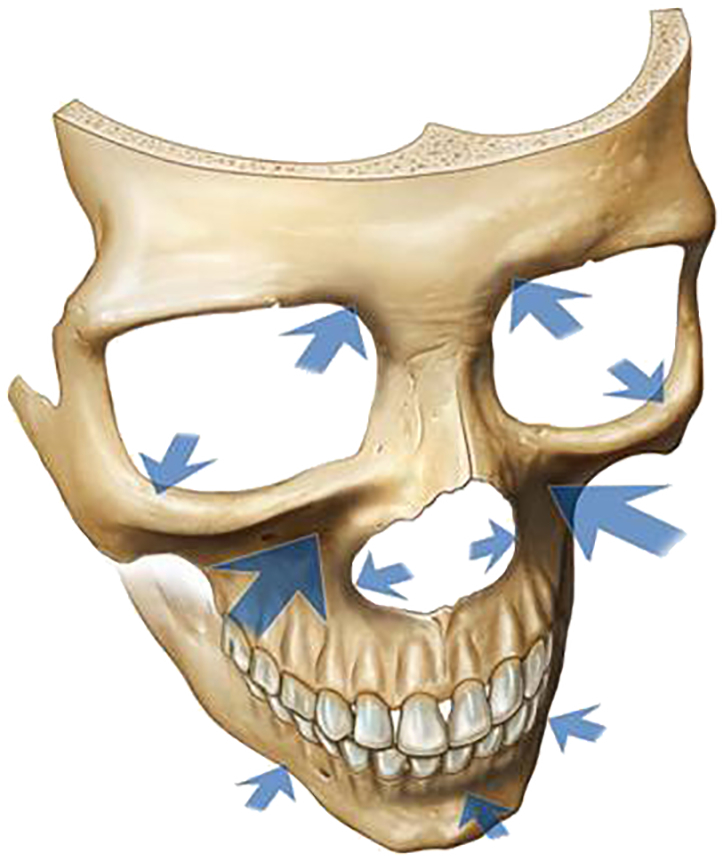
In this schematic, arrows indicate the areas of the craniofacial skeleton that are susceptible to resorption with aging. The size of the arrow correlates with the amount of resorption. Reproduced with permission from Mendelson and Wong (2012).
A recent longitudinal study was conducted by Karunanayake et al. (2017). Their electronic medical record system was reviewed since its inception in 2001 for patients for whom two CT scans of the midface were obtained at least 9 years apart. The CT scans were converted into 3D craniofacial models for each patient, using the initial and follow-up CT scan data. Seven patients with a mean age of 61 years and CT scans on average 10.3 years apart were included. Bone remodeling in the same individual, over a period of 10 years, was characterized by resorption at the pyriform aperture(100%) anterior wall of the maxilla; (100%), and superocentral (71%), superomedial (57%), and inferolateral (57%) aspects of the orbital rims.
Finally, in a recent study by Avelar et al. (2018), 241 skulls from the Forensic Anthropology Department at the Institute of Forensic Medicine in Brazil were evaluated according to sex and age group (< 20, 20-50, and > 50 years). The authors emphasized the importance of a better understanding of the contribution of craniofacial support in achieving natural appearing results.
Stuzin (2007) noted that a youthful face seems to represent a point in time when a particular set of skeletal proportions are ideal for their soft-tissue envelope. Enlargement of the pyriform aperture and orbital aperture may effectively decrease the bony surface area available to support the overlying soft-tissue envelope, leading to some of the observed soft-tissue changes noted with age. These changes share some similarity with the soft-tissue draping seen in an infant face (Pessa et al., 1999).
The schematic in Figure 25 illustrates the impact of adequate pyriform support on the convexity of the midface and is best seen in a profile view. The first figure shows the lack of pyriform and anterior maxillary support resulting in midface concavity and an acute nasolabial angle. Note how this lack of support causes the philtrum to fall further back and gives the impression of an overly prominent upper lip. This problem can be worsened with the addition of filler into the body and vermillion border of the upper lip (Fig. 18). The second picture in this schematic illustrates how pyriform augmentation creates a convex profile and opens the nasolabial angle, resulting in a normal-appearing upper lip. A clinical example with no prior treatment is shown in Figure 26.
Fig. 25.
Relationship of the lip and nose affect overall facial balance. This schematic depicts the position of the lip in relation to the amount of pyriform support. Reproduced with permission from Yaremchuk 2007.
Fig. 26.

Clinical correlation of placement of product (here using poly-l-lactic acid/2 sessions) in the preperiosteal pyriform space, which pushes the base of the nose anteriorly and serves to evert the upper lip and increase the prominence of the cupid’s bow and philtral columns without direct augmentation of the lip. Product was also placed in the chin in the area of labiomandibular fat and deep submentalis fat, which serves to evert the lower lip. It is not uncommon to see the width of the lip shorten slightly with these injections. No product was used in the lips. Photographs courtesy of Rebecca Fitzgerald MD.
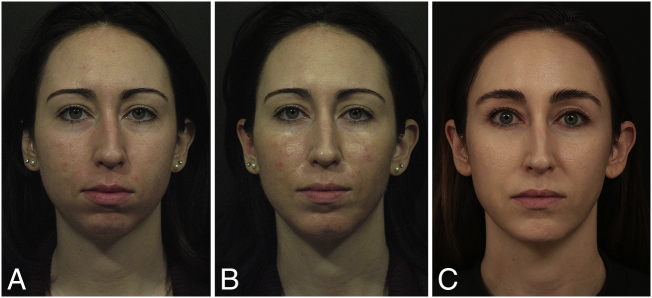
Recall that the aforementioned longitudinal study on craniofacial aging discussed above showed that 100% of the patients studied (albeit a small sample size) showed bony remodeling in this area over a 10-year period. Also recall that the authors of the study delineating the pyriform space noted that bony recession of the maxilla with age predisposes this space for use as a potential area of deep volumization to support the overlying cheek fat and draping lip elevators and may prove to be a vital target area for restructuring the aging anterior midface. The presence and maintenance of bone volume and contour are necessary to provide and preserve ideal soft-tissue relationships. The result of addressing this one structural tissue is seen in young patients with congenital skeletal hypoplasia (Fig. 27). This was the biggest deficit in this patient, and addressing that one tissue issue served to bring this face closer to its ideal shape and proportions.
Fig. 27.
(A) Patient is shown before and (B) immediately after the first treatment, and (C) again 6 years later, maintained with annual treatments. Calcium hydroxylapatite administered with a 25-gauge cannula was used in the midface, and hyaluronic acid in the chin. All treatments were done with a 25-gauge cannula. A small chin implant was placed by a surgeon after the first treatment, but did not give the volume the patient desired. Since that time, hyaluronic acid was used after sterile scrub using care to avoid contact with the capsule of the implant. Change in the facial shape and perioral ratio is visible with this treatment. Photographs courtesy of Rebecca Fitzgerald, MD.
Clinical examples
The practical use of these concepts in injectable treatment of the face is illustrated in a number of patients of different ages, ethnic backgrounds, and with different issues (Fig. 28). To consider a number of examples, and to more easily compare and contrast different faces, these cases are presented in a “composite” format. This smaller format also facilitates the recognition of facial shapes and proportions, the harmony or disharmony of the three thirds of the face, and determination of what is present or missing that may be moving the face away from ideal shapes and proportions (Fig. 3). The patient photographs are lined up vertically for easy comparison of the morphology of these faces, both before and after treatment. The faces were analyzed by looking at the tissue structures independently (one tissue issue vs. multiple tissue issues), facial shape and proportions (oval face, phi ratio in lower third of face), harmony of the three thirds of the face, and topography (concavity vs. convexity).
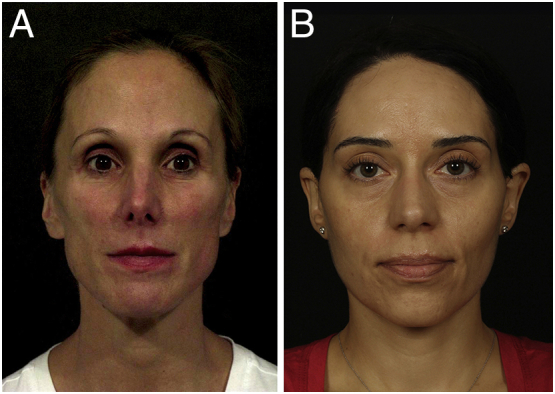
Fig. 28.
Practical use of these concepts in injectable treatment of the face can be illustrated using a number of patients of different ages and ethnic backgrounds. To examine a number of cases, as well as to compare and contrast different faces, these cases are presented in a “composite” format. This smaller format makes it easier to recognize facial shape and proportions and harmony or disharmony of the three thirds of the face, as well as to determine what is present or missing that may be moving the face away from the ideal shape and proportions illustrated in Figure 3. The photographs are lined up vertically to enable an easy comparison of the morphology of these faces both before and after treatment. In all cases, the facial shape is more ovalized and convex in the after pictures. Photographs courtesy of Rebecca Fitzgerald MD.
Patient A (age in the early 50s) had previously been treated in the tear troughs. The undereye filler is too high, too superficial, and excessive. In addition to the Tyndall effect, the irregular topography created by this placement gives the face an odd look. This is probably the most common novice placement error. The volume loss in the temples is skeletonizing and affects the facial frame. In the lower face, there is a U-shaped hollow around the chin. The HA in the tear trough was dissolved, and the patient was initially treated in the superficial temporolateral cheek compartments and the superficial medial and middle fat pads with PLLA. The patient was also treated in the four deep fat pads of the midface with HA improvement.
Months later, the treating physician (R.F.) eventually recognized that the flattening of the anterior convexity of the face was consistent with bony remodeling, and she was treated along the inferior lateral orbital rim, the supraperiosteal midface (pyriform, anterior maxilla, zygoma), and lower face (anterior mandible) (using PLLA), which restored some convexity to her midface and improved her outcome. A small amount of filler was also placed in her oral commissures.
Patient B (age in the mid 40s) had some regional disparity with the upper third of her face, which was a bit smaller than the lower two thirds. There is also mild flattening of the mid face. The patient was treated with HA in her temples, middle forehead fat compartments, and PZS. HA was also used around the pyriform fossa. Note the improvement in the shape, topography, and regional harmony of her face.
Patient C (age in the mid 50s) had one main tissue issue that needed craniofacial augmentation. The biggest issue was the flatness of her midface, followed by the hollowing in her temples and a U-shaped hollow in her chin. Her midface was addressed with filler (PLLA) over the entire zygoma, anterior maxilla, and pyriform aperature bilaterally. Note how these midface arcs and convexities improve the shadow patterns and seem to make her face look smaller (i.e., less wide).
Patient D (age in the mid 30s) primarily had a one tissue issue in the bone. However, it was only in the bone of the lateral mid-third and lower third of her face, which gave her face an odd-looking regional disparity. The congenital lack of craniofacial support in the lateral zygoma, the mandible, and chin in this patient made her forehead look too large for her face, an illusion that disappears with correction of the aforementioned areas (here done with HA). In addition it gives the impression of early jowling, often seen in young patients with a suboptimal chin. This is, of course, normal jowl fat with inadequate bony support, but it can also exacerbate what is seen in older patients as they lose bone in this area.
Patient E (age in the late 20s) had a facial shape that was addressed with treatment of both the upper and lower thirds of her face. Neuromodulator in the hypertrophic masseters served to ovalize and feminize her lower face. Filler in the temples brought the face closer to the ideal 5-eyes across (Fig. 3). Temple filler also served to harmonize the upper third with the lower two thirds of her face. A small amount of filler in the chin was added to harmonize this area with her large cheekbones.
Patient F (age in the mid 40s) has good skin and minimal fat loss, but poor craniofacial support. This is initially obscured by her masseteric hypertrophy. However, on closer observation, the soft tissue of her temples has more lateral projection than her cheekbones (opposite of patient E), and her brow and midface are flattened. Neuromodulater was used in the masseters and glabella, and HA was used in the lateral brows and over the lateral inferior orbital rim. PLLA was used over the anterior and lateral maxilla and zygomatic arch and in the pyriform aperature. This combination served to ovalize her facial frame and her anterior face.
Patient G (age in the early 40s) had enough fat loss to make her zygoma quite visible. She was treated with HA in the temple and two sessions of PLLA in the superficial lateral and middle cheek compartments. The patient did not want to remove any filler in her lips or around her eyes (performed elsewhere prior to first visit); therefore, PLLA (two sessions) was also used in the pyriform fossa to minimize the upper lip projection, and HA was used in the deep fat pads of the lower lip and in the labiomandibular fat compartments to blend in the lower lip with the chin. Upon further review in the preparation of this manuscript, the patient may have benefited from a small amount of HA filler in her medial SOOF.
Patient H (age in the early 40s) is an endurance exercise patient with both superficial and deep-fat compartment volume loss and suboptimal anterior maxillary craniofacial support. The global oval facial frame was addressed with treatment in the superficial temporal lateral fat compartments (one session of PLLA). The suboptimal bony support in the midface left the patient with a negative vector (i.e., shallow orbits and retrusive orbital rim where the cornea has more projection than the orbital rim, much like the patient in Fig. 22), and a deep tear trough and nasojugal fold with visible infraorbital fat.
Direct treatment of this area requires a lot of product and often results in a Tyndall effect such as in Patient A. Therefore, she was first treated with three sessions of PLLA over the anterior maxilla and in the pyriform space, as well as in the DMCF and DLCF, to minimize the amount of HA filler needed under her eyes. The patient was also treated with HA in the PZS prior to treatment of the tear through with HA. The patient had much improvement, but still has a slight Tyndall effect from the amount of HA needed to treat her tear trough.
Conclusions
Systematic assessment and site-specific nonsurgical rejuvenation of the face with fillers may lead to increased safety, accuracy, and technique reproducibility in this commonly performed procedure. Although out of the scope of this article, several publications referenced herein offer excellent detailed descriptions of techniques (often accompanied by anatomical dissections) used to access some of these areas safely, effectively, and reproducibly (Fitzgerald and Vleggaar, 2011, Pessa and Rohrich, 2012, Lamb and Surek, 2018, Scheuer III et al., 2017, Sieber et al., 2016, Surek et al., 2015b, Wang et al., 2017).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijwd.2018.08.011.
Appendix A. Supplementary data
Supplementary material 1
Supplementary material 2
Supplementary material 3
Supplementary material 4
Supplementary material 5
Supplementary material 6
Supplementary material 7
Supplementary material 8
Supplementary material 9
Supplementary material 10
Supplementary material 11
Supplementary material 12.
Supplementary material 13.
Supplementary material 14.
Supplementary material 15.
Supplementary material 16.
Supplementary material 17
Supplementary material 18.
Supplementary material 19.
Supplementary material 20
Supplementary material 21.
Supplementary material 22.
Supplementary material 23.
Supplementary material 24
Supplementary material 25
Supplementary material 26.
Supplementary material 27
References
- Avelar L.E., Cazerta C.E., Ave M.N., Shitara D.I. Dynamic changes of facial supporting cornerstones (pillars): Considerations in aesthetic approach. J Drugs Dermatol. 2018;17(4):466–470. [PubMed] [Google Scholar]
- Azizzadeh B., Murphy M., Johnson C. Elsevier; 2007. Master techniques in facial rejuvenation. [Google Scholar]
- Azizzadeh B., Murphy M., Johnson C., Massry G., Fitzgerald R. Elsevier; London: 2018. Master techniques in facial rejuvenation. [Google Scholar]
- Bashour M. History and current concepts in the analysis of facial attractiveness. Plast Reconstr Surg. 2006;118:741–756. doi: 10.1097/01.prs.0000233051.61512.65. [DOI] [PubMed] [Google Scholar]
- Cotofana S., Schenck T.L., Trevidic P. Midface: clinical anatomy and regional approaches with injectable fillers. Plast Reconstr Surg. 2015;136.5S:219S–234S. doi: 10.1097/PRS.0000000000001837. [DOI] [PubMed] [Google Scholar]
- Cotofana S., Fratila A., Schenck T., Redka-Swoboda W., Zilinsky I., Pavicic T. The anatomy of the aging face: A review. Facial Plast Surg. 2016;32:253–260. doi: 10.1055/s-0036-1582234. [DOI] [PubMed] [Google Scholar]
- Fitzgerald R. Contemporary concepts in brow and eyelid aging. Clin Plast Surg. 2013;40:21–42. doi: 10.1016/j.cps.2012.08.005. [DOI] [PubMed] [Google Scholar]
- Fitzgerald R., Rubin A. Filler placement and the fat compartments. Dermatol Clin. 2014;32:37–50. doi: 10.1016/j.det.2013.09.007. [DOI] [PubMed] [Google Scholar]
- Fitzgerald R., Vleggar D. Using Poly-L-lactic acid (PLLA) to mimic volume in multiple tissue layers. J Drugs Dermatol. 2009;8:s5–s14. [PubMed] [Google Scholar]
- Fitzgerald R., Vleggaar D. Facial volume restoration of the aging face with poly-l-lactic acid. Dermatol Ther. 2011;24:2–27. doi: 10.1111/j.1529-8019.2010.01375.x. [DOI] [PubMed] [Google Scholar]
- Gierloff M., Stöhring C., Buder T., Gassling V., Acil Y., Wiltfang J. Aging changes of the midfacial fat compartments: A computed tomographic study. Plast Reconstr Surg. 2012;129(1):263–273. doi: 10.1097/PRS.0b013e3182362b96. [DOI] [PubMed] [Google Scholar]
- Gierloff M., Stöhring C., Buder T., Wiltfang J. The subcutaneous fat compartments in relation to aesthetically important facial folds and rhytides. J Plast Reconstr Aesthet Surg. 2012;65(10):1292–1297. doi: 10.1016/j.bjps.2012.04.047. [DOI] [PubMed] [Google Scholar]
- Glasgold M. Introduction to volumetric facial rejuvenation. Facial Plast Surg. 2015;31:10–14. doi: 10.1055/s-0035-1544251. [DOI] [PubMed] [Google Scholar]
- Glasgold M.J., Glasgold R.A., Lam S.M. Volume restoration and facial aesthetics. Facial Plast Surg Clin North Am. 2008;16(4):435–442. doi: 10.1016/j.fsc.2008.05.004. [DOI] [PubMed] [Google Scholar]
- Karunanayake M., To F., Efanov J. Analysis of craniofacial remodeling in the aging midface using reconstructed three-dimensional models in paired individuals. Plast Reconstr Surg. 2017;140:448e. doi: 10.1097/PRS.0000000000003590. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick S.W., Bell F.E., Johnson C., Perkins J., Sullivan L.A. Interpretation of facial expressions of emotion: The influence of eyebrows. Genet Soc Gen Psychol Monogr. 1996;122:405. [PubMed] [Google Scholar]
- Lamb J.P., Surek C. Thieme; New York, NY: 2018. Facial volumization: An anatomic approach. [Google Scholar]
- Lambros V., Amos G. Three-dimensional facial averaging: A tool for understanding facial aging. Plast Reconstr Surg. 2016;138:980e. doi: 10.1097/PRS.0000000000002752. [DOI] [PubMed] [Google Scholar]
- Landau M., Fagien S. Science of hyaluronic acid beyond filling: Fibroblasts and their response to the extracellular matrix. Plast Reconstr Surg. 2015;136:188S. doi: 10.1097/PRS.0000000000001823. [DOI] [PubMed] [Google Scholar]
- Mendelson B., Wong C. Aesthetic surgery of the face. Elsevier; London: 2013. Anatomy of the aging face. [Google Scholar]
- Mendelson B., Wong C.H. Changes in the facial skeleton with aging: Implications and clinical applications in facial rejuvenation. Aesthet Plast Surg. 2012;36:753–760. doi: 10.1007/s00266-012-9904-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendelson B.C., Jacobson S.R. Surgical anatomy of the midcheek: Facial layers, spaces, and the midcheek segments. Clin Plast Surg. 2008;35(3):395–404. doi: 10.1016/j.cps.2008.02.003. [DOI] [PubMed] [Google Scholar]
- Moss C.J., Mendelson B.C., Taylor G.I. Surgical anatomy of the ligamentous attachments in the temple and periorbital regions. Plast Reconstr Surg. 2000;105:1475–1490. discussion 1491. [PubMed] [Google Scholar]
- Muzaffar A.R., Mendelson B.C., Adams W.P., Jr. Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus. Plast Reconstr Surg. 2002;110(3):873–884. doi: 10.1097/00006534-200209010-00025. [DOI] [PubMed] [Google Scholar]
- Pessa J.E., Rohrich R.J. Quality Medical Publishing, Inc; St Louis, MO: 2012. Facial topography. In: Clinical anatomy of the face. [Google Scholar]
- Pessa J.E., Slice D.E., Hanz K.R., Broadbent T.H., Jr., Rohrich R.J. Aging and the shape of the mandible. Plast Reconstr Surg. 2008;121(1):196–200. doi: 10.1097/01.prs.0000293864.94138.ae. [DOI] [PubMed] [Google Scholar]
- Pessa J.E., Zadoo V.P., Yuan C., Ayedelotte J.D., Cuellar F.J., Cochran C.S. Concertina effect and facial aging: Nonlinear aspects of youthfulness and skeletal remodeling, and why, perhaps, infants have jowls. Plast Reconstr Surg. 1999;103:635–644. doi: 10.1097/00006534-199902000-00042. [DOI] [PubMed] [Google Scholar]
- Rohrich R., Pessa J. Discussion: Aging changes of the midfacial fat compartments: A computed tomographic study. Plast Reconstr Surg. 2012;129(1):274–275. doi: 10.1097/PRS.0b013e3182362be2. [DOI] [PubMed] [Google Scholar]
- Rohrich R., Pessa J. Discussion: Aging of the facial skeleton: Aesthetic implications and rejuvenation strategies. Plast Reconstr Surg. 2012;129(1):274–275. doi: 10.1097/PRS.0b013e3181fad698. [DOI] [PubMed] [Google Scholar]
- Rohrich R.J., Arbique G.M., Wong C., Brown S., Pessa J.E. The anatomy of suborbicularis fat: Implications for periorbital rejuvenation. Plast Reconstr Surg. 2009;124(3):946–951. doi: 10.1097/PRS.0b013e3181b17b76. [DOI] [PubMed] [Google Scholar]
- Rohrich R.J., Pessa J.E. The fat compartments of the face: Anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119(7):2219–2227. doi: 10.1097/01.prs.0000265403.66886.54. [DOI] [PubMed] [Google Scholar]
- Rohrich R.J., Pessa J.E. The anatomy and clinical implications of perioral submuscular fat. Plast Reconstr Surg. 2009;124(1):266–271. doi: 10.1097/PRS.0b013e3181811e2e. [DOI] [PubMed] [Google Scholar]
- Rohrich R.J., Pessa J.E., Ristow B. The youthful cheek and the deep medial fat compartment. Plast Reconstr Surg. 2008;121(6):2107–2112. doi: 10.1097/PRS.0b013e31817123c6. [DOI] [PubMed] [Google Scholar]
- Schenck T., Koban K., Schlattau A. The functional anatomy of the superficial fat compartments of the face: A detailed imaging study. Plast Reconstr Surg. 2018;141:1351. doi: 10.1097/PRS.0000000000004364. [DOI] [PubMed] [Google Scholar]
- Scheuer J.F., III, Sieber D.A., Pezeshk R.A., Campbell C.F., Gassman A.A., Rohrich R.J. Anatomy of the facial danger zones: Maximizing safety during soft-tissue filler. Plast Reconstr Surg. 2017;139(1):50e–8. doi: 10.1097/PRS.0000000000002913. [DOI] [PubMed] [Google Scholar]
- Shaw R.B., Jr., Kahn D.M. Aging of the midface bony elements: A three-dimensional computed tomographic study. Plast Reconstr Surg. 2007;119:675–681. doi: 10.1097/01.prs.0000246596.79795.a8. discussion 682–3. [DOI] [PubMed] [Google Scholar]
- Sieber D.A., Scheuer J.F., III, Villanueva N.L., Pezeshk R.A., Rohrich R.J. Review of 3-dimensional facial anatomy: Injecting fillers and neuromodulators. Plast Reconstr Surg Glob Open. 2016;4 doi: 10.1097/GOX.0000000000001166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuzin J.M. Restoring facial shape in face lifting: The role of skeletal support in facial analysis and midface soft tissue repositioning. Plast Reconstr Surg. 2007;119:362–376. doi: 10.1097/01.prs.0000251092.82860.25. discussion 377–8. [DOI] [PubMed] [Google Scholar]
- Stuzin J.M., Baker T.J., Gordon H.L. The relationship of the superficial and deep facial fascias: Relevance to rhytidectomy and aging. Plast Reconstr Surg. 1992;89(3):441–449. [PubMed] [Google Scholar]
- Surek C., Beut J., Stephens R., Jelks G., Lamb J. Pertinent anatomy and analysis for midface volumizing procedures. Plast Reconstr Surg. 2015;818e:135. doi: 10.1097/PRS.0000000000001226. [DOI] [PubMed] [Google Scholar]
- Surek C., Beut J., Stephens R., Lamb J., Jelks G. Volumizing viaducts of the midface: Defining the beut techniques. Aesthet Surg J. 2015;35(2):121–134. doi: 10.1093/asj/sju073. [DOI] [PubMed] [Google Scholar]
- Surek C.K., Vargo J., Lamb J. Deep pyriform space: Anatomical clarifications and clinical implications. Plast Reconstr Surg. 2016;138(1):59–64. doi: 10.1097/PRS.0000000000002262. [DOI] [PubMed] [Google Scholar]
- Wan D., Amirlak B., Giessler P. The differing adipocyte morphologies of deep versus superficial midfacial fat compartments: A cadaveric study. Plast Reconstr Surg. 2014;133:615e. doi: 10.1097/PRS.0000000000000100. [DOI] [PubMed] [Google Scholar]
- Wang W., Xie Y., Huang R.L., Zhou J., Tanja H., Zhao P. Facial contouring by targeted restoration of facial fat compartment volume: The midface. Plast Reconstr Surg. 2017;139:563–572. doi: 10.1097/PRS.0000000000003160. [DOI] [PubMed] [Google Scholar]
- Wong C., Hsieh M., Mendelson B. The tear trough ligament: Anatomical basis for the tear trough deformity. Plast Reconstr Surg. 2012;129:1392–1402. doi: 10.1097/PRS.0b013e31824ecd77. [DOI] [PubMed] [Google Scholar]
- Yaremchuk M. Saunders Elsevier; Philadelphia: 2007. Atlas of Facial Implants. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1
Supplementary material 2
Supplementary material 3
Supplementary material 4
Supplementary material 5
Supplementary material 6
Supplementary material 7
Supplementary material 8
Supplementary material 9
Supplementary material 10
Supplementary material 11
Supplementary material 17
Supplementary material 20
Supplementary material 24
Supplementary material 25
Supplementary material 27