Abstract
Background
Telehealth programs are generally diverse in approaching patients, from traditional telephone calling and texting message and to the latest fourth-generation synchronous program. The predefined outcomes are also different, including hypertension control, lipid lowering, cardiovascular outcomes, and mortality. In previous studies, the telehealth program showed both positive and negative results, providing mixed and confusing clinical outcomes. A comprehensive and integrated approach is needed to determine which patients benefit from the program in order to improve clinical outcomes.
Objective
The CHA2DS2-VASc (congestive heart failure, hypertension, age >75 years [doubled], type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism [doubled], vascular disease, age of 65-75 years, and sex) score has been widely used for the prediction of stroke in patients with atrial fibrillation. This study investigated the CHA2DS2-VASc score to stratify patients with cardiovascular diseases receiving a fourth-generation synchronous telehealth program.
Methods
This was a retrospective cohort study. We recruited patients with cardiovascular disease who received the fourth-generation synchronous telehealth program at the National Taiwan University Hospital between October 2012 and June 2015. We enrolled 431 patients who had joined a telehealth program and compared them to 1549 control patients. Risk of cardiovascular hospitalization was estimated with Kaplan-Meier curves. The CHA2DS2-VASc score was used as the composite parameter to stratify the severity of patients’ conditions. The association between baseline characteristics and clinical outcomes was assessed via the Cox proportional hazard model.
Results
The mean follow-up duration was 886.1 (SD 531.0) days in patients receiving the fourth-generation synchronous telehealth program and 707.1 (SD 431.4) days in the control group (P<.001). The telehealth group had more comorbidities at baseline than the control group. Higher CHA2DS2-VASc scores (≥4) were associated with a lower estimated rate of remaining free from cardiovascular hospitalization (46.5% vs 54.8%, log-rank P=.003). Patients with CHA2DS2-VASc scores ≥4 receiving the telehealth program were less likely to be admitted for cardiovascular disease than patients not receiving the program. (61.5% vs 41.8%, log-rank P=.01). The telehealth program remained a significant prognostic factor after multivariable Cox analysis in patients with CHA2DS2-VASc scores ≥4 (hazard ratio=0.36 [CI 0.22-0.62], P<.001)
Conclusions
A higher CHA2DS2-VASc score was associated with a higher risk of cardiovascular admissions. Patients accepting the fourth-generation telehealth program with CHA2DS2-VASc scores ≥4 benefit most by remaining free from cardiovascular hospitalization.
Keywords: CHA2DS2-VASc score, fourth-generation synchronous telehealth program, hospitalization, cardiovascular disease
Introduction
Cardiovascular diseases remain the biggest health burden worldwide [1]. Telemedicine can be used to monitor disease and treat patients in real-time. Previous studies showed that patients with cardiovascular disease accepting telehealth medicine had better control of vascular risk factors such as hypertension, diabetes mellitus, and dyslipidemia [2]. Both Spyros et al and Sally et al reported that telemedicine was an important prognostic factor for reducing all-cause mortality in patients with congestive heart failure [3,4]. We have shown that the fourth-generation telehealth program—an internet-based, synchronized, disease-management program providing an immediate response—could lower mortality as compared to the control group [5]. However, Takahashi et al found that telemonitoring did not lead to fewer hospitalizations or emergency department visits [6]. A review article suggested that telemedicine should be carefully evaluated and applied to patients who benefit with improved clinical outcomes [7].
The European Society of Cardiology has published atrial fibrillation-management guidelines in 2016 to advocate using the CHA2DS2-VASc (congestive heart failure, hypertension, age >75 years [doubled], type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism [doubled], vascular disease, age of 65-75 years, and sex) score as a predictive scoring model for stroke in patients with atrial fibrillation [8]. In addition, the American Heart Association has already released similar recommendations for treatment of patients with atrial fibrillation in 2014 [9]. Based on the guidelines, patients with one or more stroke risk factors (ie, a CHA2DS2-VASc score ≥1 in men or ≥2 in women) are at a higher risk for future stroke events, which is a dosage effect. Oral anticoagulation is recommended or preferred for these patients with atrial fibrillation. Furthermore, Mitchell et al showed that CHA2DS2-VASc scores could predict the incidence of stroke or transient ischemic attack in a population of over 20,000 patients with acute coronary syndrome without atrial fibrillation [10]. This scoring system can also predict various categories of cardiovascular hospitalization events other than cerebrovascular accident events; the scores themselves were a composite of inflammatory risk factors [11]. However, no studies have thus far addressed the utility of CHA2DS2-VASc scores to stratify patients via a telehealth program.
Here, we aimed to investigate the relation between CHA2DS2-VASc scores and cardiovascular admission in patients receiving a fourth-generation telehealth program. In addition, we stratified patients by CHA2DS2-VASc score and examined the effect of the telehealth program on these scores and clinical outcomes.
Methods
Study Design
This was a single-center, clinical retrospective epidemiologic study that was approved by the Institutional Review Board of National Taiwan University Hospital, Taipei, Taiwan. All clinical managements of patients in the telehealth program were performed in accordance with relevant guidelines and regulations.
Patient Selection
The study was conducted from October 2012 to June 2015 at the Telehealth Center of the hospital by the Taiwan ELEctroHEALTH Study Group (TELEHEALTH Study Group). Patients older than 20 years diagnosed with chronic cardiovascular diseases and receiving the telehealth program at our telehealth center were enrolled as the study group. The telehealth-care program is a self-pay service in our hospital, which is not reimbursed by health insurance. Because the patients needed to pay for the service and receive long-term follow-up, we only included patients who were above 20 years old in this study. The decision of receiving the telehealth program depended on the patients or their caregivers. Chronic cardiovascular diseases included coronary artery disease, myocardial infarction, heart failure, peripheral artery disease, stroke, and hypertension. The control group included participants who visited our cardiovascular center during the same period but did not participate in the telehealth care program (received usual care only). The exclusion criteria in this study (for both telehealth group and control group) were age <20 years, absence of any one of the abovementioned chronic cardiovascular diseases, and no follow-up in our hospital.
Telehealth Care Program
The fourth-generation telehealth program at our center is a synchronized and integrated remote management program for chronic diseases. The internet-based platform was developed by the Graduate Institute of Biomedical Electronics and Bioinformatics, National Taiwan University, Taiwan. The details of this program have been reported previously [12]. Briefly, this telehealth program provides the following services: biometric data including single-lead electrocardiography, blood pressure, heart rate, and oximetry are transferred from patients to our telehealth center daily and on demand; nurse case managers telephone patients daily on demand for communication and health promotion; full-time nurse case managers and cardiologists are in charge of care 24 hours per day; and long-term medication and management are discussed with the patients’ primary care physician after acute events. This telehealth program bridges acute and home care and emphasizes on education, prevention, and early detection of clinical deterioration. The clinical information including CHA2DS2-VASc scores were relayed to the cardiology specialist who made the final judgment and suggestions regarding care.
Usual Care
Patients in the control group received the usual care provided by the primary care physicians at our cardiovascular center according to updated guidelines including, but not limited to, the American Heart Association’s guidelines for lifestyle modification and primary prevention to reduce cardiovascular risk, guidelines for the management of stable ischemic heart disease, and the American Diabetes Association’s guidelines for the management of diabetes. Patients made routine outpatient department visits (once every 3 months) to their primary care physicians. There was no contact between the telehealth center and patients receiving usual care.
Data Collection
All demographic and clinical data were obtained from the electronic database of the hospital. The CHA2DS2-VASc score was calculated retrospectively according to documentation of the electrical medical chart for congestive heart failure, hypertension, age >75 years (doubled), type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism (doubled), vascular disease, age of 65-75 years, and sex category. The calculation is not yet an automated process in our Web-based telehealth program. The diagnosis of a chronic disease was based on the electronic database. The discharge diagnosis was used if there was disagreement between outpatient and discharge diagnoses. The follow-up data were acquired from the electronic database of our hospital. The primary outcome of this study was hospitalization for cardiovascular events including acute coronary syndrome, peripheral artery disease, stroke, transient ischemic attack, congestive heart failure, atrial fibrillation, and sudden cardiac death. The end date of follow-up was the September 30, 2016.
Statistical Analysis
Normally distributed data were displayed as the mean (SD), and data were compared within the study group using the t test of variance. Nonnormally distributed continuous data were displayed as the median (interquartile range) and were compared in the study group using the Kruskal-Wallis analysis. The distribution of categorical variables was compared in the study group using the chi-squared test. There were no missing values in the basic variable collections in our cohort.
Kaplan-Meier curves were used to estimate survival rates of hospitalization for cardiovascular events, and a log-rank test was used to compare risks among the study groups. We further stratified the subjects according to the CHA2DS2-VASc scores of 0-3 and 4-8. To evaluate the independent effect of the telehealth program on the risks of hospitalization for cardiovascular events, we used a multivariable Cox proportional hazard model with adjustment for prespecified clinical characteristics including age >80 years, female gender, diabetes mellitus, hypertension, dyslipidemia, coronary artery disease, congestive heart failure, peripheral artery disease, ischemic stroke, atrial fibrillation, chronic kidney disease, and telehealth program. The assumption of proportional hazard was tested by the Schoenfeld partial residuals, in which the study group was the only explanatory continuous variable. The assumption of proportional hazard was not rejected. The Bonferroni correction was used to adjust for multiple (pairwise) comparisons in the study group when the overall test was statistically significant. Data were analyzed using Statistical Package for Social Science (version 22; IBM Corp, Armonk, NY). Statistical significance was set at two-sided P values <.05.
Results
Patient Demographics and Clinical Features
A total of 1980 patients (431 in the telehealth group and 1549 in the control group) were enrolled in this study (Figure 1). The baseline characteristics are reported in the Table 1. In the telehealth groups, the mean age was 70.3 (SD 14.9) years, and 66.1% (285/431) were men.
Figure 1.
Flow chart of enrolled patients. CV: cardiovascular; f/u: follow up.
Table 1.
Baseline characteristics.
| Characteristics | Telehealth care group (N=431) | Control group (N=1549) | P value | |
| Patient status | ||||
| Age (years), mean (SD) | 70.3 (14.9) | 64.2 (13.8) | <.001 | |
| Age > 80 years, n (%) | 85 (19.7) | 115 (7.4) | <.001 | |
| Female gender, n (%) | 146 (33.9) | 494 (31.9) | .45 | |
| Risk factors | ||||
| Diabetes mellitus, n (%) | 128 (29.7) | 369 (23.8) | .01 | |
| Hypertension, n (%) | 198 (45.9) | 642 (41.4) | .098 | |
| Hyperlipidemia, n (%) | 143 (33.2) | 484 (31.2) | .40 | |
| Atrial fibrillation, n (%) | 73 (16.9) | 152 (9.8) | <.001 | |
| CKDa, n (%) | 38 (8.8) | 116 (7.5) | .36 | |
| CADb, n (%) | 207 (48.0) | 907 (58.6) | <.001 | |
| CHFc, n (%) | 103 (23.9) | 166 (10.7) | <.001 | |
| Stroke, n (%) | 64 (14.8) | 128 (8.3) | <.001 | |
| PADd, n (%) | 14 (3.2) | 51 (3.3) | >.99 | |
| CHA2DS2-VASce score, mean (SD) | 2.7 (1.9) | 2.0 (1.6) | <.001 | |
| Medication | ||||
| Aspirin, n (%) | 184 (42.7%) | 788 (50.9%) | .003 | |
| Beta-blocker, n (%) | 150 (34.8%) | 321 (20.7%) | <.001 | |
| ACEI/ARBf, n (%) | 170 (39.4%) | 510 (32.3%) | .01 | |
| CCBg, n (%) | 44 (10.2%) | 390 (25.2%) | <.001 | |
| Statin, n (%) | 120 (27.8%) | 440 (28.4%) | .86 | |
| OHAh, n (%) | 78 (18.1%) | 229 (14.8%) | .098 | |
| Mean follow-up (days), mean (SD) | 701.7 (431.4) | 886.1 (530.9) | <.001 | |
aCKD: chronic kidney disease.
bCAD: coronary artery disease.
cCHF: congestive heart failure.
dPAD: peripheral artery disease.
eCHA2DS2-VASc: congestive heart failure, hypertension, age >75 years (doubled), type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism (doubled), vascular disease, age of 65-75 years, and sex.
fACEI/ARB: angiotensin-converting enzyme inhibitor/angiotensin II receptor blocker.
gCCB: calcium channel blocker.
hOHA: oral hypoglycemic agent.
In the control group, the mean age was 64.2 (SD 13.8) years, and 68.11% were men (1055/1549). The telehealth group had more patients with congestive heart failure (103/431, 23.9% vs 166/1549, 10.7%), stroke (64/431, 14.8% vs 128/1549, 8.3%), diabetes mellitus (128/431, 29.7% vs 369/1549, 23.8%), and atrial fibrillation (73/431, 16.9% vs 152/1549, 9.8%) than the control group; all these variables were significantly different between the two groups. The CHA2DS2-VASc score was significantly higher in the telehealth group than in the control group (2.7 [SD 1.9] vs 2.0 [SD 1.6], P<.001). The mean follow-up time was 701.7 (SD 431.4) days for the telehealth group and 886.1 (SD 530.9) days for the control group (P<.001).
Prognosis of Patients Stratified by CHA 2DS2-VASc Score
We stratified all patients (telehealth and control group) into higher (4-8 points) and lower (0-3 points) score groups according to their CHA2DS2-VASc score. A total of 414 patients were included in the higher score group and 1566 were included in the lower score group. The Kaplan-Meier curve showed significant differences in the factor remaining free of hospitalization for a cardiovascular event between the two groups. The overall estimated survival rate was 46.5% in the higher CHA2DS2-VASc score group and 54.8% in the lower CHA2DS2-VASc score group (log-rank test P=.003; Figure 2).
Figure 2.
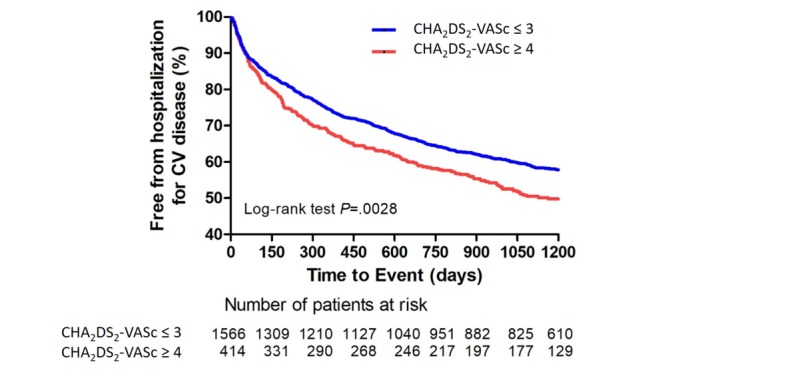
Kaplan-Meier curve of cardiovascular hospitalization according to CHA2DS2-VASc scores. The overall estimated rate of cardiovascular hospitalization was 54.8% and 46.5% in patients with CHA2DS2-VASc score ≤3 and ≥4, respectively (log-rank test P=.003). The dotted lines represented the error bars of 95% CI in both figures. CV: cardiovascular; CHA2DS2-VASc: congestive heart failure, hypertension, age >75 years (doubled), type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism (doubled), vascular disease, age of 65-75 years, and sex.
Impact of Telehealth Program on Patients with Different CHA 2DS 2-VASc Scores
The lower CHA2DS2-VASc score group included 299 subjects in the telehealth group and 1267 subjects in the usual care group. The estimated survival rate of patients remaining free from cardiovascular hospitalization was 61.4% for the telehealth program and 54.3% in the control group. The Kaplan-Meier curve showed similar survival rates in both groups without significant differences (log-rank P=.57; Figure 3). The higher CHA2DS2-VASc score group included 132 subjects in the telehealth group and 282 in the usual care group. The estimated survival rate in patients remaining free from cardiovascular hospitalization was 61.5% and 41.8% in patients in the telehealth program and those in the control group, respectively. Patients accepting the telehealth program had better survival, with significant differences observed in the Kaplan-Meier curve between the two groups (log-rank P=.01; Figure 3).
Figure 3.
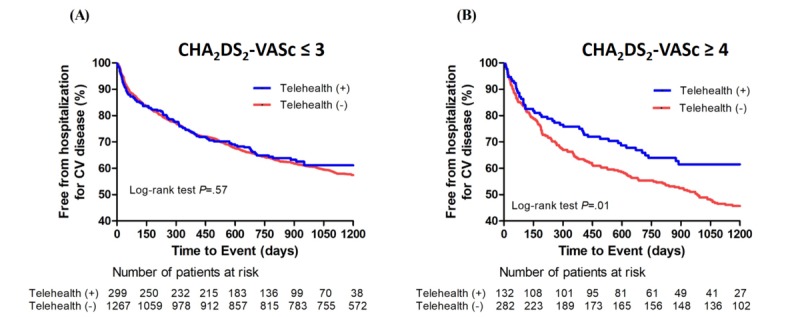
(A) Kaplan-Meier curve of cardiovascular hospitalization and the fourth generation synchronous telehealth program in patients with CHA2DS2-VASc score ≤3. The overall estimated survival rate of remaining free from cardiovascular hospitalization was 61.1% in patients accepting the fourth-generation telehealth program, and 54.3% in patients not accepting the program (log-rank test P=.57). (B) CHA2DS2-VASc score ≥4. The overall estimated survival rate of remaining free from cardiovascular hospitalization was 61.5% in patients accepting the fourth-generation telehealth program and 41.8% in patients not accepting the program (log-rank test P=.01). CV: cardiovascular; CHA2DS2-VASc: congestive heart failure, hypertension, age >75 years (doubled), type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism (doubled), vascular disease, age of 65-75 years, and sex.
Predictors of Cardiovascular Hospitalization for Patients With CHA2DS2-VASc Scores ≥4
Univariate analysis revealed a significant association between hospitalization for cardiovascular events and the following variables in patients with CHA2DS2-VASc scores ≥ 4 (Table 2): chronic kidney disease (hazard ratio [HR]=1.87 [CI 1.32-2.63], P<.001), telehealth program (HR=0.66 [CI 0.48-0.91], P=.01), and angiotensin receptor blocker (HR=0.70 [CI: 0.52-0.94], P=.006). However, only chronic kidney disease (HR=1.65 [CI 1.13-2.40], P=.01) and the telehealth program (HR=0.36 [CI 0.22-0.62], P<.001) remained significant in multivariable Cox regression. On the other hand, the variable peripheral artery disease was insignificant in univariable analysis (HR=0.97 [CI 0.74-1.29], P=.86) but became significant (HR=1.92 [CI 1.24-2.98], P =.003) after multivariable Cox regression (Table 2).
Table 2.
Univariate and multivariable Cox analyses: Predictors of hospitalization for cardiovascular events in patients with CHA2DS2-VASc scores ≥4 (N=414).
| Variables | Univariate analysis | Multivariable analysis | ||
| Hazard ratio (95% CI) | P value | Hazard ratio (95% CI) | P value | |
| Age >80 years | 0.85 (0.65-1.12) | .26 | 0.93 (0.69-1.23) | .59 |
| Female gender | 0.86 (0.66-1.14) | .30 | 0.97 (0.73-1.30) | .85 |
| Diabetes mellitus | 0.99 (0.75-1.30) | .93 | 0.85 (0.60-1.22) | .39 |
| Hypertension | 1.05 (0.73-1.50) | .81 | 1.35 (0.91-2.02) | .14 |
| Dyslipidemia | 1.07 (0.82-1.41) | .62 | 0.94 (0.69-1.30) | .72 |
| Coronary artery disease | 1.30 (0.98-1.73) | .07 | 1.22 (0.88-1.68) | .23 |
| Congestive heart failure | 1.24 (0.93-1.66) | .14 | 1.31 (0.96-1.80) | .09 |
| Peripheral artery disease | 0.97 (0.74-1.29) | .86 | 1.92 (1.24-2.98) | .003 |
| Ischemic stroke | 0.76 (0.40-1.32) | .39 | 0.84 (0.44-1.61) | .60 |
| Atrial fibrillation | 1.03 (0.73-1.46) | .86 | 1.13 (0.78-1.64) | .51 |
| Chronic kidney disease | 1.87 (1.32-2.63) | <.001 | 1.65 (1.13-2.40) | .01 |
| Telehealth program | 0.66 (0.48-0.91) | .01 | 0.36 (0.22-0.62) | <.001 |
| Antiplatelet | 1.03 (0.78-1.35) | .86 | 1.03 (0.75-1.41) | .86 |
| Angiotensin converting enzyme inhibitor | 0.99 (0.54-1.83) | .99 | 0.96 (0.50-1.82) | .89 |
| Angiotensin II receptor blocker | 0.70 (0.52-0.94) | .02 | 0.80 (0.56-1.17) | .25 |
| Calcium channel blocker | 0.76 (0.55-1.05) | .098 | 0.75 (0.53-1.06) | .10 |
| Beta-blocker | 1.02 (0.74-1.40) | .92 | 1.06 (0.75-1.49) | .76 |
| Statin | 0.93 (0.69-1.27) | .65 | 1.08 (0.74-1.57) | .69 |
| Oral hypoglycemic agent | 0.75 (0.55-1.04) | .08 | 1.00 (0.65-1.53) | .99 |
| Insulin | 0.80 (0.44-1.47) | .47 | 0.97 (0.51-1.84) | .92 |
Interaction Between the Telehealth Program and the CHA2DS2-VASc Score
Figure 4 shows the Kaplan-Meier curve of cardiovascular hospitalization among patients with different CHA2DS2-VASc scores (≥4 and ≤3) who did and did not receive the fourth-generation synchronous telehealth program. In the usual care group, the overall estimated survival rate of patients who were not hospitalized for cardiovascular complications was 41.8% in group D and 54.3% in group B (Figure 4). In the telehealth group, the overall estimated survival rate of subjects remaining free from cardiovascular hospitalization was 61.5% in group C and 61.1% in group A (log-rank P=.0006) After a pairwise multiple comparison-adjustment procedure for Kaplan-Meier survival curve with Bonferroni correction, the estimated survival rate of group C remained significantly higher than that for group D and was similar to that of groups A and B (group A vs group C, log-rank P=.97; group B vs group C, log-rank P=.59; group C vs group D, log-rank P=.01; Figure 4).
Figure 4.
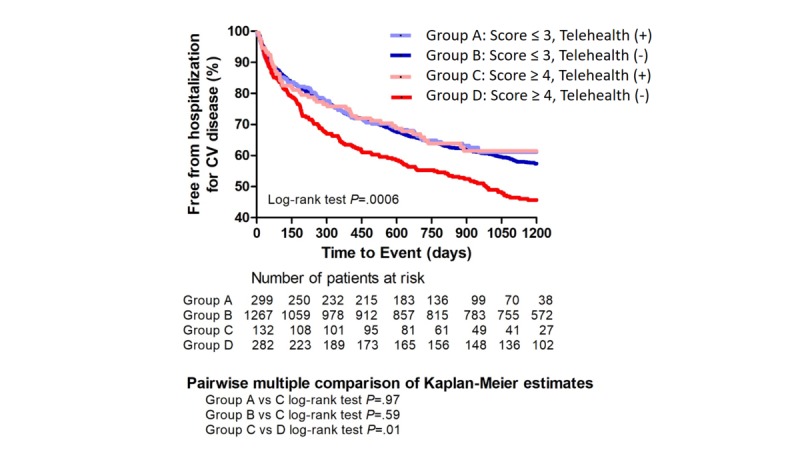
Kaplan-Meier curve of cardiovascular hospitalization in patients with different CHA2DS2-VASc scores (≥4 and ≤3) with/without the fourth-generation synchronous telehealth program. In the usual care group, the overall estimated survival rate of free from cardiovascular hospitalization was 41.8% in group D and 54.3% in group B. In the telehealth group, the overall estimated survival rate while remaining free of cardiovascular hospitalization was 61.5% in group C and 61.1 % in group A (log-rank test P=.0006). After pairwise multiple comparison adjustment procedure for Kaplan-Meier survival curve with Bonferroni correction, the estimated survival rate of group C remained significantly higher than that of group D. It was similar in groups A and B (Group A vs C: log-rank test P=.97; Group B vs C: log-rank test P=.59; Group C vs D: log-rank test P=.01). CV: cardiovascular; CHA2DS2-VASc: congestive heart failure, hypertension, age >75 years (doubled), type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism (doubled), vascular disease, age of 65-75 years, and sex.
Discussion
Principal Findings
This is the first study to apply CHA2DS2-VASc scores to stratify patients receiving the fourth-generation synchronous telehealth program and determine who benefits most from the program. Our study showed that the fourth-generation synchronous telehealth program provided better outcomes with reduced cardiovascular hospitalization than usual care in patients with higher CHA2DS2-VASc scores (≥4 points).
Overview
Telehealth care has been shown to reduce hospitalizations in patients with chronic conditions such as asthma, chronic obstructive pulmonary disease, and heart failure [13-16]. We previously reported better cost effectiveness and clinical outcomes with the use of a fourth-generation synchronous telehealth program in patients with chronic cardiovascular diseases [12]. In that study, patients who received and those who did not receive telehealth programs were matched for sex, age, and Charlson score, which is a method of predicting mortality by classifying or weighting comorbid conditions [17]. However, some studies failed to show better clinical outcomes in patients receiving telehealth program [6,7]. Although the types of subjects enrolled were diverse, research on telehealth programs in chronic diseases management has shown mixed results. Development of an objective stratification system for patients and identification of which group of patients benefit from the telehealth program are needed.
The CHA2DS2-VASc score is a validated clinical tool predicting stroke occurrence in patients with atrial fibrillation [8,9]. Previous studies have shown that the CHA2DS2-VASc score enables a substantially comprehensive risk evaluation and improves physicians’ ability to identify genuinely low-risk patients who have atrial fibrillation. It is not surprising that the components of these risk scores are associated with adverse outcomes because the majority of variables reflect the presence of heart disease or heart disease risk factors independent of atrial fibrillation. These grave outcomes are highlighted in studies that have examined CHA2DS2-VASc scores in patients without atrial fibrillation. These studies have noted a significant risk of major adverse cardiovascular events with increasing scores [18-20]. Comprehensive care for a patient with higher scores is extremely important because they have a greater risk and worse outcomes of congestive heart failure, acute coronary syndrome, and even mortality [18-20]. In this study, we did not match both groups by the Charlson score: Several components of CHA2DS2-VASc and Charlson scores were repetitive. Since patients with higher CHA2DS2-VASc scores exhibited a higher prevalence of cardiovascular diseases, the CHA2DS2-VASc score may be a better parameter than the Charlson score to select potential candidates for telehealth care.
In patients with nonvalvular atrial fibrillation, the CHADS2 score was significantly associated with the risk of a future stroke event. This new scoring system can identify patients with lower CHADS2 scores (≤1) who remain at high risk for stroke. However, Eva et al reported that the demarcation may be minimal for patients with CHA2DS2-VASc scores ≤3 [21]. We apply this result to our patients in two groups, with higher (≥4) and lower (≤3) CHA2DS2-VASc scores. In this study, the two groups had a significant difference in survival of subjects remaining free from cardiovascular hospitalization overall. More importantly, we found that this demarcation can stratify whether patients receive benefits after accepting the telehealth program.
In the usual care group, we found that a higher CHA2DS2-VASc score (≥4) is significantly associated with a higher risk of cardiovascular admission compared to a lower score (≤3) (Multimedia Appendix 1). However, the cardiovascular admissions were similar for patients with CHA2DS2-VASc scores ≥4 and those with scores ≤3 in the telehealth group (Multimedia Appendix 1). This suggested that telehealth care could diminish the CHA2DS2-VASc score-associated cardiovascular admission. In the patient group with CHA2DS2-VASc scores ≤3, the overall estimated survival rate of subjects remaining free from cardiovascular hospitalization was similar irrespective of whether patients accepted the fourth-generation telehealth program (Figure 3). However, patients with scores ≥4 who accepted the telehealth program had significantly better outcome than those who did not accept the program (Figure 3B). After multiple comparison adjustments by Bonferroni methods, patients with scores ≥4 accepting telehealth were found to have similar clinical outcomes as patients with scores ≤3, regardless of whether they accepted the telehealth program; their outcomes were significantly better than those of patients with scores ≥4 not accepting the telehealth program (Figure 4). This implied that patients with scores ≥4 benefit most from telehealth monitoring and the need for cardiovascular hospitalization is reduced. These results showed that the CHA2DS2-VASc score might be a good indicator to select patients for the telehealth program.
The telehealth program has changed over time. We used the fourth-generation telehealth program, which is a synchronous and integrated remote-management program for chronic disease. This new system takes the initiative to offer an interactive environment and in-time responsiveness for patients who encountered acute illness or deterioration in condition. Compared to usual care, more accurate diagnoses and decisions can be made through quick communication after accepting the telehealth program. In our previous report, there were significantly fewer emergency department visits, hospitalizations, hospitalization days, and intensive care unit admissions per month in the telehealth group compared to the control group [12]. Thus, this new intervention program may be helpful in improving patient outcomes.
Apart from the telehealth program, we found that chronic kidney disease and peripheral artery disease were the two remaining prognostic factors for cardiovascular admission in patients with CHAS2DS2-VASc scores ≥ 4 after multivariable Cox regression. Studies on patients with chronic kidney disease accepting telehealth are rare [22,23]. We reported that among patients receiving the telehealth program, renal function status remains a predictor for first hospitalization—this is identical to our study [24]. On the other hand, patients with peripheral artery disease accepting the telehealth program are rarer despite their higher mortality rate [25]. According to previous studies, the mortality of symptomatic and asymptomatic patients was 19% and 24%, respectively, at 5 years [26]. Furthermore, patients with peripheral artery disease share similar risk factors as patients with coronary artery disease, carotid artery stenosis, and congestive heart failure as compared to the general population [27-29]. Early identification of peripheral artery disease with optimized and comprehensive treatment is mandatory to improve clinical outcomes; the telehealth program may have a role in this process. There have been studies addressing the issue of telehealth applications in patients with peripheral artery disease with wounds or gangrene, but these studies focused on wound infection control rather than general patient care [30,31]. Larger clinical trials applying telehealth care to patients with peripheral artery disease may be needed to improve clinical outcomes.
Limitations
This study has several limitations. First, the study was not randomized, which resulted in heterogeneity of the patient population, disease severity, and patient selection. Patients with the capacity to self-monitor and be enrolled in a program for home remote monitoring are potentially more likely to receive medical assistance when experiencing clinical changes or a clinical decline. The patient-selection process should be recognized as a limitation. Second, the presence of numerous confounding factors in our cohort might have influenced the result, including the missing events. We tried to perform multivariable Cox regression analysis to minimize the possible confounding effect of other clinical factors. Third, there might be some statistical limitations and considerations of statistical testing/modeling. For example, peripheral artery disease was not significantly associated with hospitalization for cardiovascular events in the univariate Cox regression but became significant in the multivariable Cox model in patients with CHA2DS2-VASc scores ≥4 (Table 2). This might be due to some reverse confounding or overfitting. On the other hand, the survival analysis stratified by CHA2DS2-VASc scores (≤3 vs >4) may induce type I error inflation (Figure 3). However, the result would be significant even if Bonferroni correction was done in patients with CHA2DS2-VASc scores ≥4. This indicates that type I error inflation may not be a serious problem in this study. Fourth, the clinical outcomes were derived from the electronic billing and medical records of our hospital, and the patients who received care outside our hospital were not recorded. Resources that were used but not billed may have also been overlooked when extracting data from our billing system.
Conclusions
Patients with higher CHA2DS2-VASc scores had higher risks of cardiovascular admissions, but the fourth-generation telehealth program could diminish the outcome difference associated with scores. Patients with CHA2DS2-VASc scores ≥4 benefited the most from the fourth-generation telehealth program and remained free of cardiovascular hospitalization.
Acknowledgments
We thank Kuo-Liong Chien for his consultation in the statistical analysis during data analysis. This research was supported by the Joint Research Center for AI Technology and All Vista Healthcare under Ministry of Science and Technology of Taiwan (MOST 107-2634-F-002-018) and Center for Artificial Intelligence & Advanced Robotics, and National Taiwan University Hospital (106-A136, 107-EDN11, 108-N4406).
Abbreviations
- ACEI
angiotensin converting enzyme inhibitor
- ARB
angiotensin II receptor blocker
- CAD
coronary artery disease
- CCB
calcium channel blocker
- CHA2DS2-VASc
congestive heart failure, hypertension, age >75 years (doubled), type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism (doubled), vascular disease, age of 65-75 years, and sex
- CHF
congestive heart failure
- CKD
chronic kidney disease
- HR
hazard ratio
- OHA
oral hypoglycemic agent
- PAD
peripheral artery disease
(A) Kaplan-Mayer curve of cardiovascular hospitalization with CHA2DS2-VASc score in patients who did not accept the fourth-generation synchronous telehealth program. The overall estimated survival rate of cardiovascular hospitalization was 41.8% in patients with CHA2DS2-VASc score ≥4 and 54.3% in patients with a score ≤3 (log-rank test P=.0001). (B) Patients using the fourth-generation synchronous telehealth program. The overall estimated survival rate of cardiovascular hospitalization was 61.5% in patients with CHA2DS2-VASc score ≥4 and 61.1% in patients with the score ≤3 (log-rank test P=.97). CV: cardiovascular; CHA2DS2-VASc: congestive heart failure, hypertension, age > 75 years (doubled), type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism (doubled), vascular disease, age of 65-75 years, and sex.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, Alla F, Alvis-Guzman N, Amrock S, Ansari H, Ärnlöv J, Asayesh H, Atey TM, Avila-Burgos L, Awasthi A, Banerjee A, Barac A, Bärnighausen T, Barregard L, Bedi N, Belay Ketema E, Bennett D, Berhe G, Bhutta Z, Bitew S, Carapetis J, Carrero JJ, Malta DC, Castañeda-Orjuela CA, Castillo-Rivas J, Catalá-López F, Choi J, Christensen H, Cirillo M, Cooper L, Criqui M, Cundiff D, Damasceno A, Dandona L, Dandona R, Davletov K, Dharmaratne S, Dorairaj P, Dubey M, Ehrenkranz R, El Sayed Zaki M, Faraon EJA, Esteghamati A, Farid T, Farvid M, Feigin V, Ding EL, Fowkes G, Gebrehiwot T, Gillum R, Gold A, Gona P, Gupta R, Habtewold TD, Hafezi-Nejad N, Hailu T, Hailu GB, Hankey G, Hassen HY, Abate KH, Havmoeller R, Hay SI, Horino M, Hotez PJ, Jacobsen K, James S, Javanbakht M, Jeemon P, John D, Jonas J, Kalkonde Y, Karimkhani C, Kasaeian A, Khader Y, Khan A, Khang Y, Khera S, Khoja AT, Khubchandani J, Kim D, Kolte D, Kosen S, Krohn KJ, Kumar GA, Kwan GF, Lal DK, Larsson A, Linn S, Lopez A, Lotufo PA, El Razek HMA, Malekzadeh R, Mazidi M, Meier T, Meles KG, Mensah G, Meretoja A, Mezgebe H, Miller T, Mirrakhimov E, Mohammed S, Moran AE, Musa KI, Narula J, Neal B, Ngalesoni F, Nguyen G, Obermeyer CM, Owolabi M, Patton G, Pedro J, Qato D, Qorbani M, Rahimi K, Rai RK, Rawaf S, Ribeiro A, Safiri S, Salomon JA, Santos I, Santric Milicevic M, Sartorius B, Schutte A, Sepanlou S, Shaikh MA, Shin M, Shishehbor M, Shore H, Silva DAS, Sobngwi E, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadele Atnafu N, Tesfay F, Thakur JS, Thrift A, Topor-Madry R, Truelsen T, Tyrovolas S, Ukwaja KN, Uthman O, Vasankari T, Vlassov V, Vollset SE, Wakayo T, Watkins D, Weintraub R, Werdecker A, Westerman R, Wiysonge CS, Wolfe C, Workicho A, Xu G, Yano Y, Yip P, Yonemoto N, Younis M, Yu C, Vos T, Naghavi M, Murray C. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol. 2017 Jul 04;70(1):1–25. doi: 10.1016/j.jacc.2017.04.052. https://linkinghub.elsevier.com/retrieve/pii/S0735-1097(17)37244-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vernooij J, Kaasjager H, van der Graaf Y, Wierdsma J, Grandjean H, Hovens M, de Wit GA, Visseren FSG, SMARTStudy Group Internet based vascular risk factor management for patients with clinically manifest vascular disease: randomised controlled trial. BMJ. 2012 Jun 12;344:e3750. doi: 10.1136/bmj.e3750. http://europepmc.org/abstract/MED/22692651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kitsiou S, Paré G, Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure: an overview of systematic reviews. J Med Internet Res. 2015 Mar 12;17(3):e63. doi: 10.2196/jmir.4174. http://www.jmir.org/2015/3/e63/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inglis S, Clark R, McAlister F, Stewart S, Cleland J. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: Abridged Cochrane Review. Eur J Heart Fail. 2011 Sep;13(9):1028–40. doi: 10.1093/eurjhf/hfr039. doi: 10.1093/eurjhf/hfr039. [DOI] [PubMed] [Google Scholar]
- 5.Hung C, Yu J, Lin Y, Chen Y, Huang C, Lee J, Chuang P, Ho Y, Chen M. Mortality Benefit of a Fourth-Generation Synchronous Telehealth Program for the Management of Chronic Cardiovascular Disease: A Longitudinal Study. J Med Internet Res. 2016 May 13;18(5):e102. doi: 10.2196/jmir.5718. http://www.jmir.org/2016/5/e102/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takahashi PY, Pecina JL, Upatising B, Chaudhry R, Shah ND, Van Houten Holly, Cha S, Croghan I, Naessens JM, Hanson GJ. A randomized controlled trial of telemonitoring in older adults with multiple health issues to prevent hospitalizations and emergency department visits. Arch Intern Med. 2012 May 28;172(10):773–9. doi: 10.1001/archinternmed.2012.256. http://europepmc.org/abstract/MED/22507696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wootton R. Twenty years of telemedicine in chronic disease management--an evidence synthesis. J Telemed Telecare. 2012 Jun;18(4):211–20. doi: 10.1258/jtt.2012.120219. http://europepmc.org/abstract/MED/22674020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener H, Heidbuchel H, Hendriks J, Hindricks G, Manolis A, Oldgren J, Popescu B, Schotten U, Van Putte Bart, Vardas P, ESC Scientific Document Group 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016 Dec 07;37(38):2893–2962. doi: 10.1093/eurheartj/ehw210. [DOI] [PubMed] [Google Scholar]
- 9.January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW, ACC/AHA Task Force Members 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014 Dec 02;130(23):2071–104. doi: 10.1161/CIR.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell LB, Southern DA, Galbraith D, Ghali WA, Knudtson M, Wilton SB, APPROACH investigators Prediction of stroke or TIA in patients without atrial fibrillation using CHADS2 and CHA2DS2-VASc scores. Heart. 2014 Oct;100(19):1524–30. doi: 10.1136/heartjnl-2013-305303. [DOI] [PubMed] [Google Scholar]
- 11.Mazzone C, Cioffi G, Carriere C, Barbati G, Faganello G, Russo G, Cherubini A, Sinagra G, Zeriali N, Di Lenarda A. Predictive role of CHADS-VASc score for cardiovascular events and death in patients with arterial hypertension and stable sinus rhythm. Eur J Prev Cardiol. 2017 Dec;24(15):1584–1593. doi: 10.1177/2047487317726068. [DOI] [PubMed] [Google Scholar]
- 12.Ho Y, Yu J, Lin Y, Chen Y, Huang C, Hsu T, Chuang P, Hung C, Chen M. Assessment of the cost-effectiveness and clinical outcomes of a fourth-generation synchronous telehealth program for the management of chronic cardiovascular disease. J Med Internet Res. 2014 Jun 10;16(6):e145. doi: 10.2196/jmir.3346. http://www.jmir.org/2014/6/e145/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McLean S, Chandler D, Nurmatov U, Liu J, Pagliari C, Car J, Sheikh A. Telehealthcare for asthma. Cochrane Database Syst Rev. 2010 Oct 06;(10):CD007717. doi: 10.1002/14651858.CD007717.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLean S, Nurmatov U, Liu J, Pagliari C, Car J, Sheikh A. Telehealthcare for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011 Jul 06;(7):CD007718. doi: 10.1002/14651858.CD007718.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clark R, Inglis S, McAlister F, Cleland J, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ. 2007 May 05;334(7600):942. doi: 10.1136/bmj.39156.536968.55. http://europepmc.org/abstract/MED/17426062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clarke M, Shah A, Sharma U. Systematic review of studies on telemonitoring of patients with congestive heart failure: a meta-analysis. J Telemed Telecare. 2011;17(1):7–14. doi: 10.1258/jtt.2010.100113. [DOI] [PubMed] [Google Scholar]
- 17.Charlson M, Pompei P, Ales K, MacKenzie C. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Crandall M, Horne B, Day J, Anderson J, Muhlestein J, Crandall B, Weiss J, Osborne J, Lappé DL, Bunch T. Atrial fibrillation significantly increases total mortality and stroke risk beyond that conveyed by the CHADS2 risk factors. Pacing Clin Electrophysiol. 2009 Aug;32(8):981–6. doi: 10.1111/j.1540-8159.2009.02427.x. [DOI] [PubMed] [Google Scholar]
- 19.Svendsen J, Nielsen J, Darkner S, Jensen G, Mortensen L, Andersen HR, DANPACE Investigators CHADS2 and CHA2DS2-VASc score to assess risk of stroke and death in patients paced for sick sinus syndrome. Heart. 2013 Jun;99(12):843–8. doi: 10.1136/heartjnl-2013-303695. http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=23539553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ntaios G, Lip G, Makaritsis K, Papavasileiou V, Vemmou A, Koroboki E, Savvari P, Manios E, Milionis H, Vemmos K. CHADS₂, CHA₂S₂DS₂-VASc, and long-term stroke outcome in patients without atrial fibrillation. Neurology. 2013 Mar 12;80(11):1009–17. doi: 10.1212/WNL.0b013e318287281b. [DOI] [PubMed] [Google Scholar]
- 21.Pueo E, Campos B, Anguita M, Worner F. Does CHA₂DS₂-VASc score select patients who will benefit most from anticoagulation? Rev Esp Cardiol (Engl Ed) 2014 May;67(5):417–8. doi: 10.1016/j.rec.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Ishani A, Christopher J, Palmer D, Otterness S, Clothier B, Nugent S, Nelson D, Rosenberg ME, Center for Innovative Kidney Care Telehealth by an Interprofessional Team in Patients With CKD: A Randomized Controlled Trial. Am J Kidney Dis. 2016 Jul;68(1):41–9. doi: 10.1053/j.ajkd.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 23.Ong S, Jassal S, Miller J, Porter E, Cafazzo J, Seto E, Thorpe K, Logan A. Integrating a Smartphone-Based Self-Management System into Usual Care of Advanced CKD. Clin J Am Soc Nephrol. 2016 Dec 06;11(6):1054–62. doi: 10.2215/CJN.10681015. http://cjasn.asnjournals.org/cgi/pmidlookup?view=long&pmid=27173169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hung C, Lee J, Chen Y, Huang C, Wu V, Wu H, Chuang P, Ho Y. Effect of Contract Compliance Rate to a Fourth-Generation Telehealth Program on the Risk of Hospitalization in Patients With Chronic Kidney Disease: Retrospective Cohort Study. J Med Internet Res. 2018 Jan 24;20(1):e23. doi: 10.2196/jmir.8914. http://www.jmir.org/2018/1/e23/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davins Riu M, Borràs Pérez X, Artigas Raventós V, Palomera Fanegas E, Serra Prat M, Alós Villacrosa J. Use of Telehealth as a New Model for Following Intermittent Claudication and Promoting Patient Expertise. Telemed J E Health. 2018 Oct;24(10):773–781. doi: 10.1089/tmj.2017.0226. [DOI] [PubMed] [Google Scholar]
- 26.Diehm C, Allenberg J, Pittrow D, Mahn M, Tepohl G, Haberl R, Darius H, Burghaus I, Trampisch HJ, German Epidemiological Trial on Ankle Brachial Index Study Group Mortality and vascular morbidity in older adults with asymptomatic versus symptomatic peripheral artery disease. Circulation. 2009 Nov 24;120(21):2053–61. doi: 10.1161/CIRCULATIONAHA.109.865600. [DOI] [PubMed] [Google Scholar]
- 27.Sukhija R, Yalamanchili K, Aronow W. Prevalence of left main coronary artery disease, of three- or four-vessel coronary artery disease, and of obstructive coronary artery disease in patients with and without peripheral arterial disease undergoing coronary angiography for suspected coronary artery disease. Am J Cardiol. 2003 Aug 01;92(3):304–5. doi: 10.1016/s0002-9149(03)00632-5. [DOI] [PubMed] [Google Scholar]
- 28.Ness J, Aronow W, Newkirk E, McDanel D. Prevalence of symptomatic peripheral arterial disease, modifiable risk factors, and appropriate use of drugs in the treatment of peripheral arterial disease in older persons seen in a university general medicine clinic. J Gerontol A Biol Sci Med Sci. 2005 Feb;60(2):255–7. doi: 10.1093/gerona/60.2.255. [DOI] [PubMed] [Google Scholar]
- 29.Wu C, Lee J, Chiang F, Yang C, Huang S, Hwang J, Lin J, Tseng C, Chen J, Tsai C. Plasma levels of tumor necrosis factor-α and interleukin-6 are associated with diastolic heart failure through downregulation of sarcoplasmic reticulum Ca2+ ATPase. Crit Care Med. 2011 May;39(5):984–92. doi: 10.1097/CCM.0b013e31820a91b9. [DOI] [PubMed] [Google Scholar]
- 30.van Netten JJ, Clark D, Lazzarini P, Janda M, Reed L. The validity and reliability of remote diabetic foot ulcer assessment using mobile phone images. Sci Rep. 2017 Aug 25;7(1):9480. doi: 10.1038/s41598-017-09828-4. doi: 10.1038/s41598-017-09828-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith-Strøm H, Igland J, Østbye T, Tell G, Hausken M, Graue M, Skeie S, Cooper J, Iversen M. The Effect of Telemedicine Follow-up Care on Diabetes-Related Foot Ulcers: A Cluster-Randomized Controlled Noninferiority Trial. Diabetes Care. 2018 Dec;41(1):96–103. doi: 10.2337/dc17-1025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Kaplan-Mayer curve of cardiovascular hospitalization with CHA2DS2-VASc score in patients who did not accept the fourth-generation synchronous telehealth program. The overall estimated survival rate of cardiovascular hospitalization was 41.8% in patients with CHA2DS2-VASc score ≥4 and 54.3% in patients with a score ≤3 (log-rank test P=.0001). (B) Patients using the fourth-generation synchronous telehealth program. The overall estimated survival rate of cardiovascular hospitalization was 61.5% in patients with CHA2DS2-VASc score ≥4 and 61.1% in patients with the score ≤3 (log-rank test P=.97). CV: cardiovascular; CHA2DS2-VASc: congestive heart failure, hypertension, age > 75 years (doubled), type 2 diabetes mellitus, previous stroke, transient ischemic attack or thromboembolism (doubled), vascular disease, age of 65-75 years, and sex.


