Abstract
Systematic analysis of STD programme data contributes to a national portrait of sexually transmitted disease (STD) prevention activities, including research and evaluation specifically designed to optimise programme efficiency and impact. We analysed the narrative of the 2009 annual progress reports of the US Comprehensive STD Prevention Systems cooperative agreement for 58 STD programmes, concentrating on programme characteristics and partnerships. Programmes described 516 unique partnerships with a median of seven organisations cited per STD programme. Non-profit organisations (including service providers) were most frequently cited. Higher gonorrhoea morbidity was associated with reporting more partnerships; budget problems were associated with reporting fewer. Challenges to engaging in partnerships included budget constraints, staff turnover and low interest. Data provide a source of information for judging progress in programme collaboration and for informing a sustained programme-focused research and evaluation agenda.
INTRODUCTION
The context for sexually transmitted disease (STD) control and prevention in the USA has shifted considerably in recent years, with economic and epidemiological trends and policy directions all playing significant roles. States in the USA operate STD prevention and control programmes in health departments under their own authority, with some states mediating operations through local health departments (cities or counties). The US Centers for Disease Control and Prevention (CDC) provide funding to STD programmes to assist with prevention and control activities in all 50 states. The proportion of total programme funding that comes from CDC varies by state, and CDC receives data on the outcomes of funded activities.
State governments across the country have been battling budget crises, resulting in cutbacks in state and local government spending.1 A 2008 survey of STD programmes revealed that 69% of STD programmes experienced budget cuts, resulting in reductions in STD programme workforce and services, reduced STD programme capacity, and closure of STD clinics.2 Meanwhile, some STD prevention and control activities, such as chlamydia screening for sexually active women aged 24 years and younger, may become available more widely.3,4 Such conditions may expand the already widening pool of clinicians who provide screening and testing, but who are not part of the public sector. The expanding role of community health centres in providing preventive and primary care services may also offer new opportunities to situate the provision of STD services within the context of primary care. Many state and city STD prevention programmes have sought opportunities to establish new partnerships and expand existing partnerships.5
The programme science framework helps public health practitioners address the challenges and opportunities inherent in periods of substantial change.6,7 This framework is premised upon directing efforts to bring science to programme and practice (eg, translational research),8 but also a reversal of the flow: directing efforts to bring programme to science.9,10 The intent of programme science is to take a systematic approach to optimising programme operations to produce maximal prevention impact (here, the incidence and prevalence of STD). An early step is to systematically evaluate the functions (nature, scope and scale) of a given programme. From such an appraisal, one can draw research or evaluation hypotheses to test and, if supported, feed back into programme operations.
Our present evaluation falls into the appraisal of functions category. It is focused on exploring the extent and nature of existing partnerships between CDC-funded STD programmes and external organisations, a need that has been noted for more than a decade.11
METHODS
Data source
Data for these analyses were drawn from the progress reports of sites funded under CDC’s Comprehensive STD Prevention Systems (CSPS) cooperative agreement. Specifically, we used the 2009 annual progress reports (APRs) submitted by CDC-funded health department STD programmes. The 58 APRs included in this analysis were submitted by the 50 state health departments, seven city health departments (Baltimore, Chicago, DC, Los Angeles, New York City, Philadelphia, San Francisco) and the Puerto Rico Department of Health.
STD programmes are asked to provide an overview of the year’s activities and updates on any changes that have occurred, followed by an overview of their STD epidemiology. The remainder of the report is dedicated to describing the status of programme activities. Typically, the original objective for each programme activity is stated, whether or not the objective was met is indicated, and barriers to meeting the objective are discussed. Information on partners and partner activities was not specific-ally required in the 2009 APR; therefore, the data for this analysis are not simply a function of reporting requirements.
Data abstraction and analyses
One of the study authors read the APR narratives and captured in NVivo8 (QSR International) any discussion of challenges and barriers to meeting objectives: for this analysis in particular, working with external partners. Data on partnerships with external organisations were abstracted and recorded in Excel (partnerships with other sectors within the health department containing the STD programme were excluded from this analysis).
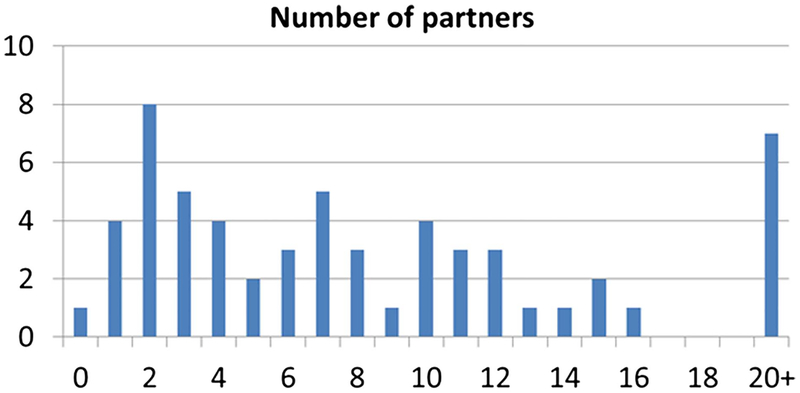
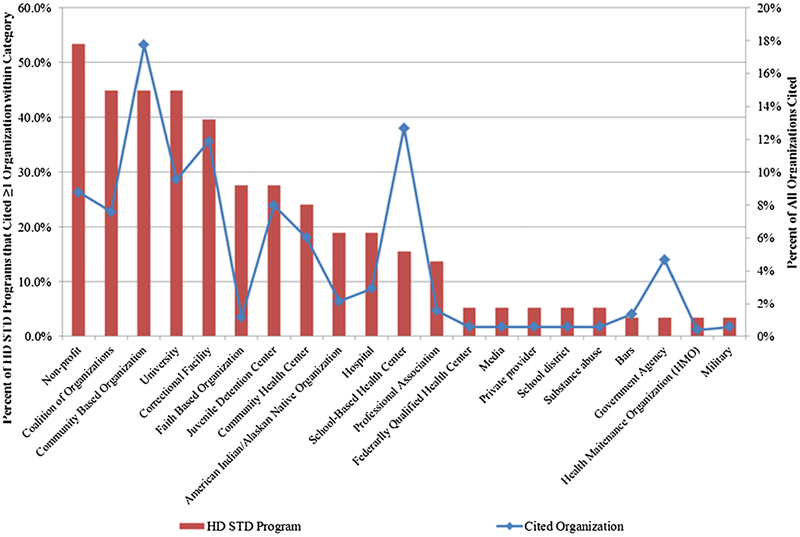
We assessed frequencies of all partnerships (figure 1) and frequencies of the types of external partner organisations cited in the APRs and the programme activities to which they typically contributed (figure 2). We paid particular attention to healthcare provision organisations because core goals of STD programmes include case detection and treatment. Then we calculated associations between characteristics of STD programmes and the number and types of partners with which they worked. We examined partners as a continuous variable and also as a dichotomous variable (median split at n=>8). The following variables were considered as potential correlates: area gonorrhoea morbidity, being a city (vs state) health department, overall funding levels as a proxy for programme size, receiving Syphilis Elimination Effort12 (SEE) funding (a marker for the STD programme serving a high-morbidity jurisdiction and receiving CDC support to establish partnerships) and reporting budget constraints in the APR. We also assessed whether working with one type of partner was associated with working with another, using the following four broad categories of organisation types: (1) non-profits/community-based/faith-based organisations, (2) correctional/juvenile detention/drug treatment facilities, (3) school-affiliated clinics and administrations and (4) healthcare providers (hospitals, community health centres, private providers). These associations involve comparisons of categorical and ordinal data, for which we used χ2 statistics, Fisher’s exact tests, t tests, ORs and Spearman correlations.
Figure 1.
Distribution of partnerships by reporting sexually transmitted disease (STD) programme. Note: Median=7. Health Department STD programmes reporting larger numbers of partners tended to report partnerships with specific agencies (eg, individual school-based health centres, correctional facilities).
Figure 2.
Per cent of Health Department sexually transmitted disease programmes (N=58) that cited at least one organisation within a specified category and the distribution of all organisations cited, as reported in 2009 annual progress reports.
RESULTS
External partners cited in the APRs: descriptive results
Figure 1 displays the range of partners cited by each STD programme. The 58 STD programmes described 516 partnerships (median=7 organisations per STD programme, range=0–37). There was substantial heterogeneity in how programmes construed partners; for example, some programmes reporting high number of partnerships did so because they reported partnerships with individual correctional facilities or school-based health centres (SBHCs). The bars on the histogram in figure 2 represent the proportion of STD programmes that reported collaborating with the category of partner, while the blue line represents the proportion of all partnerships that fell into each category. Of the 516 partnerships, 138 (27%) were accompanied by some form of evaluation measure. Most commonly, these measures described screening activities, such as the number of individuals screened.
A larger proportion of STD programmes cited non-profits than any other partner, but this category was closely followed by coalitions, community-based organisations and universities. Least frequently cited were bars, other government agencies, health maintenance organisations and the military. Generally, the proportion of STD programmes citing a partner matched the proportion of times an organisation was cited (this is the metric on the right side of figure 2). There were some exceptions, the most obvious being SBHCs, which were approximately an eighth of all organisations cited, but which were only cited by 5% of STD programmes. This finding is due to the tendency of STD programmes that work with SBHC to report collaborating with a large number of different SBHCs. In contrast, faith-based organisations made up only around a twentieth of cited organisations, but these organisations were cited by over a quarter of STD programmes.
Six organisations were cited by multiple STD programmes. In particular, one major family planning organisation was cited by 18 STD programmes, mostly commonly as a provider of STD screening and treatment services. Ten STD programmes cited a non-profit organisation which hosts a website that facilitates patient-based partner notification. Six STD programmes indicated collaborating with one of two organisations with strategic planning, surveillance and infectious disease screening expertise. Other organisations were cited by no more than two programmes. Thus, the most commonly cited partners were directly involved in healthcare provision, including STD screening, case treatment and, in one partner, partner management.
A large proportion of STD programmes reported collaborating with at least one of the following types of organisations: non-profit organisations (53.4% of STD programmes), community-based organisations, coalitions and universities (all 44.8%, figure 2). The three most commonly cited types of organisations, overall, were community based organisations (17.5% of the 516 external organisations cited), school-based health clinics (12.7%) and correctional facilities (11.9%). These results principally reflect organisations that provide STD screening, the programme activity that most commonly involved external partners (74.1% of programme reported collaborating with at least one external partner on screening activities). Of the organisations involved in screening (318), the most common types of organisations were correctional/juvenile detention/drug treatment facilities (28.6%), non-profits/community-based/faith-based organisations (26.4%), and school-affiliated clinics and administrations (19.8%). Healthcare providers, including community health clinics, hospitals and private providers, comprised only 11.6% of the cited organisations involved in screening efforts.
Correlates of partnering with external organisations
We compared characteristics of STD programmes whether the STD programme cited eight or more partner organisations within their APR, a marker of a high level of partner engagement. First, higher gonorrhoea morbidity (measured in case reports per 100 000 population: range in 2008=6.0–258.6) in the programme catchment area was associated with citing more partners (OR=1.01, 95% CI 1.003 to 1.02). That is, the odds of reporting eight or more partners rose by 1% per unit rise in cases reported per 100 000 population. If number of partners is treated as a continuous variable, the conclusion remains the same (t=3.83, r=0.43, p<0.001). To look at types of partnerships specifically, we compared gonorrhoea morbidity in states reporting each of the four types of partnership: non-profits, schools, healthcare providers and corrections. Gonorrhoea morbidity was correlated with the number of school partners (r=0.45, p<0.001) and the number of healthcare provider partners (r=0.49, p<0.001), but not non-profits (r=0.03, p>0.80) or corrections partners (r=0.17, p=0.201). In a regression with gonorrhoea morbidity as the outcome variable and the four partner types and 2009 funding levels as covariates, funding was significantly related to morbidity (β=0.31, p=0.007), and healthcare partnerships remained significantly associated with morbidity (β=0.44, p=0.002), but schools dropped out (β=0.24, p=0.06).
Because it is possible that variance in numbers of partners named is due partly to heterogeneity in how programmes reported partners (eg, reporting a single administrative entity with two clinics as one partner or two), we also calculated associations between gonorrhoea morbidity and categorical variables describing whether the programme reported correctional partners, and so on (yes or no). As expected, significance levels for the two associations above dropped: for schools, t=1.58, p=0.12; and for healthcare providers, t=1.12, p=0.25. For corrections, however, t=2.42, p=0.019. Review of the data revealed the three programmes with the highest number of correctional partners had low gonorrhoea morbidity, reducing the size of the correlation. This effect was lost when corrections data were categorised at two levels.
A smaller proportion of programmes that cited budget problems cited eight or more external partners (29.6% vs 55.2%, p=0.05). A non-significantly larger proportion of SEE recipients reported collaborating with eight or more external organisations than non-SEE recipients (51.4% vs 28.6%, p=0.09). The number of external organisations cited did not differ significantly between STD programmes situated in city or state health departments. Regarding the correlates of working with healthcare provision organisations in particular, doing so was correlated with collaborating with non-profit/community-based/faith-based organisations (r=0.46, p<.001), schools (r=0.44, p<0.001) and correctional/juvenile detention/drug treatment facilities (r=0.36, p=0.006). No other variables were significantly associated with collaborating with a healthcare provision organisation.
Challenges to collaborating with external partners
Eleven STD programmes described difficulties in establishing and maintaining relationships with external partners. Several STD programmes described how budget constraints limited their partners’ ability to engage in collaborative projects and the ensuing staff turnover disrupted established relationships and collaborative activities. Other STD programmes noted that a lack of interest in collaboration among potential partners hindered collaborative activities. Several STD programmes noted specific barriers to collaborating with correctional facilities. Acquiring data in a timely manner from external partners was another common challenge.
DISCUSSION
The health department STD programmes reporting progress data in 2009 revealed an extensive range of external partners, including such diverse partners as health centres, school districts and faith-based organisations.
The juxtaposition of the proportion of STD programmes working with a given partner and the number of partners with which they are working may inform future programme action. For example, a few STD programmes are working with a relatively large number of SBHCs. These institutions are of natural interest for STD prevention because (1) adolescents have high rates of some STDs and (2) SBHCs reach a population typically at or near the beginning of sexual activity. Collaboration in this area matches the clinical and epidemiological expertise in STD programmes with partners that have access to important populations from the perspective of prevention in high-morbidity populations. Programmes with success may assist others, and CDC can facilitate the partnering across jurisdictions, as well as local evaluation, if needed.
CDC would also expect to provide a national portrait in more detail than we do in this paper, including for other commonly-cited partnership types. The data are also instructive with respect to where action is needed on increasing partnerships. For example, if STD programmes can help meet their goals through collaborating with community health centres, then one would like the proportion of programmes reporting collaboration with community health centres to rise from the 25% to 30% shown in figure 2.
The relationships between morbidity and partnerships bear examination. Although higher gonorrhoea morbidity was related to reporting more collaborative partners, a smaller proportion of STD programmes that noted budget challenges reported more partners. The second finding is somewhat counter-intuitive, as one might expect a programme experiencing budget shortfalls to explore efficiencies through partnerships. Although STD programmes receiving SEE funds, which by definition serve populations with high syphilis morbidity, were somewhat more likely to report eight or more partnerships, the SEE federal programme offered additional resources to direct toward partnerships and encouraged such engagement. Close to 20% of all HD STD programmes noted some challenge pertaining to collaborating with external organisations. The establishment and maintenance of partnerships thus appears to require STD programme staff time and perseverance. If the value of current partnerships were indexed in terms of morbidity reduction or other indicators, results would inform the value of investment in collaborative endeavours.
As noted in the results, STD programmes reporting on partners likely construed the variable differently. That is, variance in reported numbers of partners has a ‘true’ component (different numbers of partners) and an error component (different approaches to reporting numbers). Although we were able to analyse data from two perspectives, continuous data and categories of partners (yes or no for each type of partner), we could only choose between allowing both components to vary and reducing both. In similar fashion, heterogeneity in partner organisations affects comparisons in figures 1 and 2: a national organisation may be widely cited by programmes and influential, yet, when counting partners, they would appear as a single organisation. Therefore, the range of estimates should be interpreted with care. Finally, the nature of the data restricted our ability to characterise the quality of the partnerships or their impact on programmatic outcomes (ie, reduction in STD morbidity).
Regarding implications for programmes and programme science, the analysis of CSPS reporting data may serve prevention in two ways. First, to the extent there are clear a priori plans, processes or existing data that will be used to guide action, CDC and states can specify objectives for funding recipients and provide technical assistance to assist those needing help to meet objectives. For example, the US federal funding is aligned with HIV and AIDS morbidity for HIV and AIDS case numbers (r=0.84 and 0.88) and rates (r=0.42 and 0.35).13 The exchanges between CDC and the field inform the fit of action to plans, fidelity to interventions and changes needed to fit local conditions.
Another route is to allow for fewer specifications in some areas and to analyse the variation in reports to generate research and evaluation questions that are intrinsically relevant to programme activities—because programme data are a fundamental source. This is especially relevant if programmes have the flexibility to write broadly about their construal of the STD ecology in their jurisdictions. For example, programmes began outlining internet partner services (IPS) protocols in 2010, with minimal instructions on what to report to CDC. Rather than fitting the reports to a predefined model of how IPS ‘should’ be done, the variation in protocols can be used with efficacy data to guide research and evaluation and thus inform recommendations. In the best-case scenario, documents such as the CSPS applications and progress reports can become one of the principal mechanisms enabling the feedback loops required for programme science—the grist for research and evaluation questions that are inherently relevant to optimising programme impact because they are drawn from current programme data and tested specifically for programme use. Results would be returned to the field for scale-up; this is ‘getting research into policy.’10
CONCLUSIONS
Routine and comprehensive assessments of STD prevention are vital to guide a priori planning and to identify new challenges and opportunities from the field. In this paper, we have identi-fied a routinely collected and detail-rich source of data for these purposes, but we note that we have focused on one area (partnerships) of many, and that a truly holistic effort will encompass more topics, the relationships among those topics and other infections. Moreover, we intend to develop tools for assessing partnerships and service provision patterns that are more suitable for state and local use, in contrast to our national portrait here. Finally, the essential public health assessment function14 we discuss is delinked from performance evaluation. The point of programme collaboration is not to adjudicate levels of success among partners. Instead, national, state and local prevention programmes must succeed with each other—the avenue to national prevention success. The principles of programme science aid this endeavour.
Footnotes
Publisher's Disclaimer: Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention.
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement Data are drawn from data provided to the Division of STD Prevention by state and other jurisdictions in the USA. Data may be requested from the Division of STD Prevention and will be made available subject to constraints and requirements of confidential reporting agreements.
A preliminary version of this paper was presented at the 2012 National (US) STD Prevention Conference, Minneapolis, Minnesota, USA.
REFERENCES
- 1.Golden MR, Kerndt PR. Improving clinical operations: Can we and should we save our STD clinics? Sex Transm Dis 2010;37:264–5. [DOI] [PubMed] [Google Scholar]
- 2.Wong W Fact sheet: STD programme capacity and preparedness in the United States: results of a National Survey. Washington, DC: National Coalition of STD Directors, 2009. [Google Scholar]
- 3.United States Preventive Services Task Force. Screening for chlamydial infection: U.S. preventive services task force recommendation. Ann Intern Med 2007;147:128–34. [DOI] [PubMed] [Google Scholar]
- 4.Meyers DS, Halvorson H, Luckhaupt S. U.S. preventive services task force. screening for chlamydial infection: an evidence update for the U.S. preventive services task force. Ann Intern Med 2007;147:135–42. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Programme collaboration and service integration: enhancing the prevention and control of HIV/AIDS, viral hepatitis, sexually transmitted diseases, and tuberculosis in the United States. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2009. [Google Scholar]
- 6.Aral SO, Blanchard JF. The programme science initiative: improving the planning, implementation and evaluation of HIV/STI prevention programmemes. Sex Transm Infect 2012;88:157–9. [DOI] [PubMed] [Google Scholar]
- 7.Blanchard JF, Aral SO. Programme science: an initiative to improve the planning, implementation and evaluation of HIV/sexually transmitted infection prevention programmemes. Sex Transm Infect 2011;87:1–3. [DOI] [PubMed] [Google Scholar]
- 8.Woolf SH. The meaning of translational research and why it matters. JAMA 2008;299:211–13. [DOI] [PubMed] [Google Scholar]
- 9.Westfall JM, Mold J, Fagnan L. Practice-based research—“blue highways” on the NIH roadmap. JAMA 2007;297:403–6. [DOI] [PubMed] [Google Scholar]
- 10.Parkhurst J, Weller I, Kemp J. Getting research into policy, or out of practice, in HIV? Lancet 2010;375:1414–15. [DOI] [PubMed] [Google Scholar]
- 11.Gunn RA, Rolfs RT, Greenspan JR, et al. The changing paradigm of sexually transmitted disease control in the era of managed health care. JAMA 1998;279:680–4. [DOI] [PubMed] [Google Scholar]
- 12.Syphilis Elimination Effort (SEE). www.cdc.gov/stopsyphlis (accessed 22 Jun 2012).
- 13.Mansergh G, Valdiserri RO, Yakovchenko V, et al. Aligning resources to fight HIV/AIDS in the United States: funding to states through the U.S. Department of Health and Human Services. J Acquir Immune Defic Syndr 2012;59:516–22. [DOI] [PubMed] [Google Scholar]
- 14.Institute of Medicine. The future of public health. Washington, DC: National Academy Press, 1988. [Google Scholar]