Abstract
Background
Although optimal bowel preparation is essential for high-quality screening colonoscopy, documentation of preparation quality, patient satisfaction and adherence is scarce.
Aim
The aim of this article is to compare low-volume (LV, 300 ml sodium picosulfate), intermediate-volume (IV, 2 l polyethylene glycol, PEG + ascorbic acid and sodium ascorbate), and high-volume (HV, 4 l PEG) purgatives.
Results
A total of 5000 individuals (50.5% women) were enrolled between March 2015 and July 2017 (LV:IV:HV = 3.61:1.54:1). Overall sex- and age-adjusted adenoma detection rate was 25.4% (LV 23.8%, IV 25.4%, HV 29.8%), median age was 59.6 years, and cleansing was successful in 96.8%. Success rates of bowel cleansing were highest with HV (97.6%), followed by LV (97.2%) and IV (95.3%) with OR 2.04 (CI 95% 1.20–3.45, p = 0.008) and OR 1.79 (CI 95% 1.27–2.50, p = 0.001), respectively, compared to IV. A total of 93.5% of the LV group would use the same purgative in the future, 73.2% of IV and 69.4% of HV. A total of 84.4% would prefer overnight preparation, 12.1% same-day preparation.
Conclusion
All purgatives investigated showed good bowel cleansing quality results, patient satisfaction and compliance. Improvement in patient information might lead to even higher participation rates in screening colonoscopy since one in five patients stated that bowel preparation worried him or her most prior to colonoscopy.
Keywords: Adenoma detection rate, bowel preparation, patient satisfaction, quality assurance, screening colonoscopy
Key summary
Success of bowel cleansing was highest with high-volume followed by low-volume and intermediate-volume purgatives.
Prior to colonoscopy, patients were worried most about the colonoscopy itself, followed by bowel preparation, and possible adverse events of sedation.
A total of 84.4% of patients would prefer overnight preparation, 12.1% same-day preparation.
Introduction
Adequate bowel cleansing is essential for high-quality screening colonoscopy to detect (pre)cancerous colorectal lesions.1,2 Optimal bowel preparation not only relies on a high-quality purgative but also on patient compliance in regard to consumption and dietary restrictions.3,4 In 2013 the European Society of Gastrointestinal Endoscopy (ESGE) published a guideline for bowel preparation before colonoscopy including dietary restrictions, and an overnight split-dose regimen (or same-day regimen in case of afternoon colonoscopy) for routine bowel preparation.5 The importance of bowel preparation quality was emphasized as it was defined as one of seven key quality parameters in colonoscopy in recent guidelines.6 Even though current guidelines recommend documentation of bowel cleansing quality in colonoscopy reports according to a validated scale,7 data from the Netherlands show that 38% of colonoscopy reports lack data on bowel preparation quality.8 Moreover, inadequate bowel preparation has been reported in up to 30% of all patients undergoing colonoscopy. Suboptimal bowel cleansing is not only associated with lower polyp detection rates,9,10 endoscopists tend to schedule surveillance colonoscopy earlier than the recommended intervals, which results in increased costs as well as increased risk of adverse events due to repeated procedures.10,11 Studies comparing effectiveness of and patient satisfaction and compliance with different bowel preparation regimens are scarce.10,12,13
Methods
Study aim
The aim of this study was to compare bowel cleansing quality, performance quality of screening colonoscopy, patient compliance, concerns and satisfaction of different bowel preparation regimens in one large, asymptomatic screening cohort.
As colonoscopy outcome we considered adenoma detection rate (ADR), defined as probability of detecting at least one adenoma during an examination; the same applies to advanced adenoma detection rate (AADR), polyp detection rate (PDR), proximal lesion detection rate (PDR, proximal to the sigmoid colon), serrated lesion detection rate (SLDR, including sessile and traditional serrated adenomas) and cecal intubation rate (CIR). An advanced adenoma was defined as adenoma ≥1 cm, high-grade dysplasia, or tubulovillous/villous histology.
The following purgatives were analyzed: Picoprep + Citrafleet as the low-volume group (LV, 300 ml sodium picosulfate), Moviprep as the intermediate-volume group (IV, 2 l polyethylene glycol, PEG + ascorbic acid and sodium ascorbate), and Kleanprep as the high-volume group (HV, 4 l PEG).
Study design
This is a prospective, phase IV, non-interventional, nonrandomized observational study of certified medical products.
Data collection
A total of 5000 patients, who underwent screening colonoscopy between March 2015 and July 2017, were enrolled in this study. All endoscopists participate in a nationwide quality assurance program for screening colonoscopy in Austria. Details on this project founded by the Austrian Society of Gastroenterology and Hepatology together with the Main Association of Austrian Insurance Institutions and the Austrian Cancer Aid were reported elsewhere.14,15 All included patients provided written informed consent for data analysis in the framework of scientific studies. The Austrian Data Protection Committee and the Ethics Committee of the Medical University of Vienna provided permission (Ethics Committee of the Medical University of Vienna, project number 1726/2014, ethical approval on November 4, 2014). The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
All participating endoscopists used the purgative they routinely apply within the framework of this study. There was no randomization or treatment-blinding of the endoscopist who assessed the cleansing quality. The choice of purgative was most likely based on remuneration of the insurance institution rather than particular patient characteristics since in each of the nine federal states in Austria different purgatives are refunded. Furthermore, to minimize possible differences in detection rates resulting from the performance quality of the endoscopists themselves, inclusion was limited to endoscopists with an ADR ≥20%. Screenees were included in the study on the day of screening colonoscopy. A questionnaire assessing expectations, compliance, and satisfaction with regards to the purgative used was filled out shortly before colonoscopy (Appendix 1).
Bowel-preparation quality
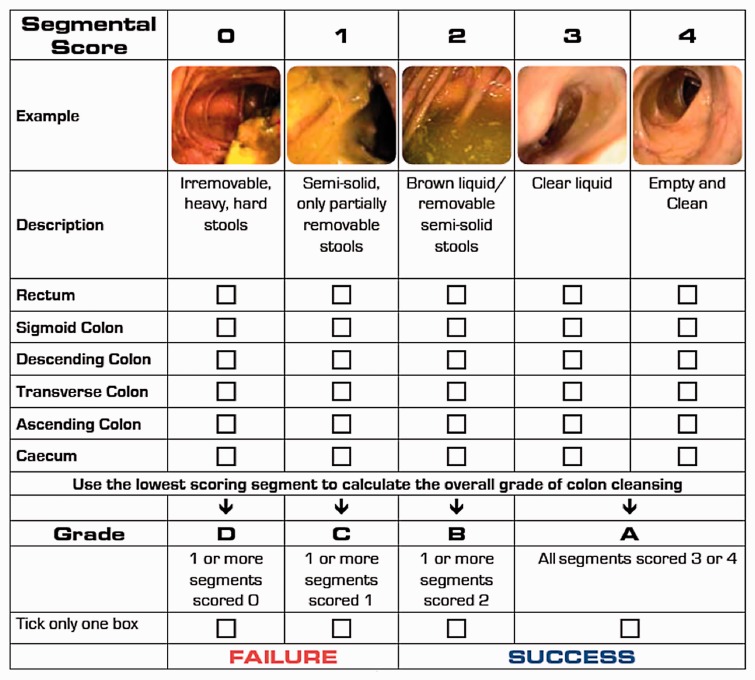
An assessment of the bowel preparation score according to the Harefield Cleansing Scale16 (Figure 1) was restricted to colonoscopies in which the cecum was reached (n = 4919) since only then can all colon segments be scored. In the framework of the present study, we used a modified Harefield Scale in which six colon segments were scored (rectum, sigmoid colon, descending colon, transverse colon, ascending colon, cecum). According to the current guidelines application of the purgative is recommended as a split-dose regimen.5,6 In case of a colonoscopy scheduled in the morning until noon, patients consume one-half dose of the purgative the evening before colonoscopy, and the other half in the early morning before colonoscopy (in this paper referred to as a two-day regimen). If the colonoscopy is scheduled after noon, patients consume one-half of the purgative in the early morning hours and the other half in the midmorning (same-day regimen). Success of bowel cleansing was defined as obtaining Harefield Scale grade A (all segments scored 3 (clear liquid) or 4 (empty and clean)) or grade B (one or more segments scored 2 (brown liquid/removable semi-solid stools)).
Figure 1.
Harefield Cleansing Scale (provided by Norgine Pharma).
Statistical analysis
Continuous variables are described by median and quartiles, and categorical variables by percentages. The association of successful bowel preparation with age, sex and purgative used was assessed by a logistic regression model. To evaluate the association of different lesion detection rates with age, sex and purgatives, we used a logistic model in which we included endoscopist-specific random intercepts as each endoscopist used the purgative that was applied in routine use also in the study. Where the association between an outcome and age appeared to be non-linear, age was modelled using restricted cubic splines. Two-sided p values less than 5% were considered statistically significant. For comparison of purgatives, we standardized and then averaged the predicted probabilities of the colonoscopy outcomes separately for each group of bowel purgatives and for each sex. Standardization was with respect to the pooled observed age distribution of the study cohort. Statistical analysis was conducted using R (version 3.4.0; Foundation for Statistical Computing, Vienna, Austria) with software packages rms (F. Harrell Jr, rms: Regression Modeling Strategies. R package version 5.1-1, 2017) and lme4 (Bates D, Maechler M, Bolker B, et al. Fitting linear mixed-effects models using lme4. J Stat Softw 2015; 67: 1-48).
Results
Baseline characteristics
Overall, 5000 screened individuals were included in this study (LV:IV:HV = 3.61:1.54:1). Median age (59.6 years) and gender distribution were similar in all groups. Baseline characteristics, grades and bowel cleansing success rates are summarized in Tables 1(a) and 2(a); rates according to sex in Tables 1(b) and 2(b).
Table 2.
(b) Age-adjusted lesion detection rates separately for men and women per purgative of all colonoscopies where the cecum was reached (n = 4914, 100%).
| ADR % |
AADR % |
PDR % |
PLDR % |
SLDR % |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | |
| LV | 31.5 | 16.5 | 9.3 | 5.3 | 58.9 | 45.2 | 16.9 | 6.9 | 2.0 | 1.6 |
| HV | 34.2 | 25.2 | 15.3 | 9.7 | 65.5 | 52.2 | 16.0 | 13.0 | 2.7 | 2.0 |
| IV | 30.6 | 20.2 | 9.4 | 5.4 | 59.6 | 51.6 | 19.8 | 13.2 | 2.7 | 2.8 |
AADR: advanced adenoma detection rate; ADR: adenoma detection rate; HV: high volume; IV: intermediate volume; LV: low volume; PDR: polyp detection rate; PLDR: proximal lesion detection rate; SLDR: serrated lesion detection rate.
Table 1.
(a) Distribution of grades (A–D) according to the Harefield Cleansing Scale, overall and per purgative, and sex and age distribution of the study cohort and per grade of all colonoscopies where the cecum was reached (n = 4914, 100%).
| Total | Grade A | Grade B | Grade C | Grade D | |
|---|---|---|---|---|---|
| Total, N (%) | 4914 (100) | 3810 (77.5) | 946 (19.3) | 135 (2.7) | 23 (0.5) |
| LV, N (%) | 2875 (58.5) | 2356 (82.0) | 439 (15.2) | 70 (2.4) | 10 (0.4) |
| HV, N (%) | 794 (16.2) | 540 (68.0) | 235 (29.6) | 13 (1.6) | 6 (0.8) |
| IV, N (%) | 1245 (25.3) | 914 (73.4) | 272 (21.9) | 52 (4.2) | 7 (0.5) |
| Men, N (%) | 2431 (49.5) | 1874 (77.0) | 473 (19.5) | 72 (3.0) | 12 (0.5) |
| Women, N (%) | 2483 (50.5) | 1936 (78.0) | 473 (19.0) | 63 (2.6) | 11 (0.4) |
| Age, median (IQR) | 59.6 (53.8–67.2) | 59.7 (54.0–67.0) | 59.1 (53.4–67.5) | 59.4 (53.1–69.9) | 63.8 (56.0–67.2) |
HV: high volume; IQR: interquartile range; IV: intermediate volume; LV: low volume.
Grade A%: Percentage of patients scored grade A according to the Harefield Cleansing Scale (all segments scored segmental score 3 (clear liquid) or 4 (empty and clean)).
Grade B%: Percentage of patients scored grade B according to the Harefield Cleansing Scale (one or more segments scored segmental score 2 (brown liquid/removable semi-solid stools)).
Grade C%: Percentage of patients scored grade C according to the Harefield Cleansing Scale (one or more segments scored segmental score 1 (semi-solid, only partially removable stools)).
Grade D%: Percentage of patients scored grade D according to the Harefield Cleansing Scale (one or more segments scored segmental score 0 (irremovable, heavy, hard stools)).
Table 2.
(a) Overall sex- und age-adjusted lesion detection rates per purgative and age-adjusted lesion detection rates for men and women of all colonoscopies where the cecum was reached (n = 4914, 100%).
| ADR % | AADR % | PDR % | PLDR % | SLDR % | |
|---|---|---|---|---|---|
| Total | 25.2 | 8.1 | 54.0 | 13.7 | 2.1 |
| LV | 23.8 | 7.3 | 51.9 | 11.2 | 1.8 |
| HV | 29.8 | 12.5 | 59.0 | 21.9 | 2.4 |
| IV | 25.4 | 7.4 | 55.6 | 15.8 | 2.7 |
| Men | 31.7 | 10.3 | 60.2 | 17.8 | 2.3 |
| Women | 18.8 | 6.0 | 47.9 | 9.6 | 1.9 |
CIRs
Overall sex- and age-adjusted CIR was 98.3%. CIR was highest with HV (99.4%), followed by LV (98.5%) and IV (97.5%) (HV compared to IV odds ratio (OR) was 1.96, confidence interval (CI) 95% 1.02–3.85, p = 0.044). There was no difference between CIR in different age groups or between men and women.
Bowel preparation quality
Overall and per purgative grades according to the Harefield Cleansing Scale and sex and age distributions overall and per grade are summarized in Table 1(a); age-adjusted success probabilities for each purgative and separately for men and women are shown in Table 1(b). Overall sex- and age-adjusted success rate of bowel cleansing was 96.8%. Comparing the purgatives, sex- and age-adjusted successful bowel cleansing rate was highest with HV (97.6%), followed by LV (97.2%) and IV (95.3%) with OR 2.04 (CI 95% 1.20–3.45, p = 0.008) and OR 1.79 (CI 95% 1.27–2.50, p = 0.001), respectively, compared to IV; there was no significant difference between HV and LV (OR 1.15 CI 95% 0.69–1.90, p = 0.6). Segment score 3 or 4 in the cecum and ascending colon was reached in 84.1% with LV, 76.1% with IV and 71.0% with HV; in the cecum, ascending colon and transverse colon in 83.0%, 75.4% and 69.5%, respectively.
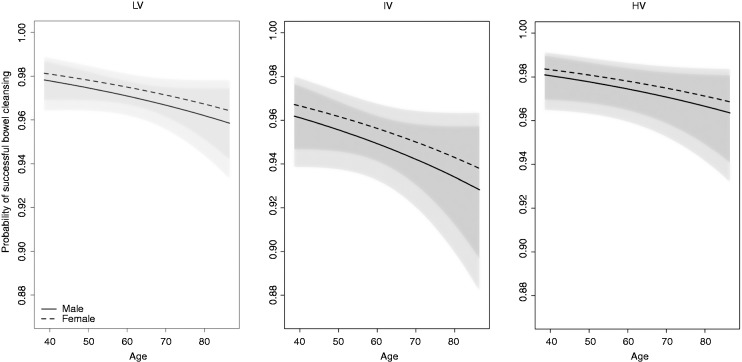
There was a slight decrease in bowel cleansing quality with increasing age (Figure 2); however, the effect of age was not statistically significant.
Figure 2.
Probability for successful bowel cleansing according to age per purgative for men (solid lines) and women (dashed lines) with corresponding 95% confidence interval (shaded area). HV: high volume; IV: intermediate volume; LV: low volume.
Performance quality measures
An analysis of performance quality measures was restricted to colonoscopies in which the cecum was reached (n = 4919). Sex- and age-adjusted lesion detection rates are summarized in Table 2(a); additionally, Table 2(b) shows age-adjusted detection rates separately for men and women. Sex- and age-adjusted overall ADR was 25.4%, 32.1% for men and 18.9% for women. Mixed-effects logistic regression models showed that HV was significantly superior to LV with regard to AADR (OR 2.11, CI 95% 1.10–4.02, p = 0.024) and ADR (OR 1.69, CI 95% 1.03–2.78, p = 0.037). HV was also significantly superior to IV in AADR (OR 1.96, CI 95% 1.02–3.70, p = 0.042) and CIR (OR 1.96, CI 95% 1.02–3.85, p = 0.044); there was no significant difference in other lesion detection rates between the investigated groups.
Patient questionnaire
For the assessment of the patient questionnaire, all 5000 questionnaires were evaluated.
Concerns prior to colonoscopy
Before colonoscopy the majority of patients were worried the most about the colonoscopy itself (55.3%), followed by bowel preparation (19.6%) and sedation (12.9%); 0.5% answered colonoscopy and sedation, 0.7% colonoscopy and bowel preparation, 0.04% sedation and bowel preparation, 11.2% N/A.
Prior to colonoscopy patients informed themselves mostly about possible adverse events of colonoscopy (3.7% of patients informed themselves well, 15.7% barely and 9.8% not at all (0.9% N/A)); followed by concerns about possible adverse events of sedation (59.7% well, 20.2% barely, 18.9% not at all, 1.3% N/A). Less than half of patients informed themselves about possible adverse events of a purgative (41.1% well, 24.2% barely, 32.0% not at all, 2.7% N/A).
The compliance regarding dietary restrictions was high; only 1.6% stated that they did not follow the dietary restrictions.
Experience with the purgative
The majority of patients described the taste of the purgative as more pleasant than expected. In the LV group 19.6% described the taste as neutral, 76.7% as better and 2.9% as worse than expected; in the IV group 24.4%, 49.1% and 24.1% and in the HV group 25.9%, 42.8% and 29.7%, respectively. However, a logistic regression model adjusted for age, sex, bowel purgative and taste showed that there was no significant association between the taste of bowel purgative and success of bowel cleansing.
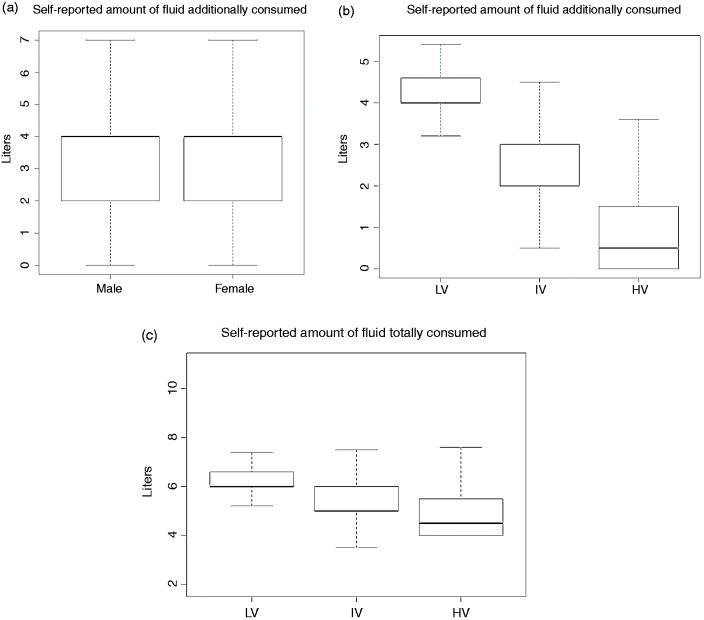
A total of 88.6% of patients indicated that they consumed the entire amount of the purgative of both portions. The compliance was high, regardless of the purgative’s volume (89.3% of LV, 87.7% of IV, 87.4% of HV). The logistic regression model adjusted for age, sex and purgative used showed no significant difference in success of bowel cleansing between patients who did not drink the entire amounts of bowel purgative and those who did. There was also no difference between women and men in the amount of fluid additionally drunk (Figure 3(a) and (b)). Figure 3(c) shows that notably the self-reported amount of fluid totally consumed was highest with LV, followed by IV and HV.
Figure 3.
Self-reported amount of fluid (a) additionally consumed by male and female patients, (b) additionally consumed in the LV, IV, and HV group, (c) totally consumed by purgative. HV: high volume; IV: intermediate volume; LV: low volume.
The following qualities would prevent the interviewed screenees from consuming the entire amount of the purgative: 37.6% bad taste, 34.1% large volume, 10.1% bad smell, 1.6% off-putting color (5.2% combined answered, 11.4% N/A).
Future preference
A total of 93.7% of patients of the LV group would use the same purgative again if they had to undergo another colonoscopy, compared with 73.3% of the IV and 68.5% of the HV group.
Among respondents, 31.5% prefer the two-day regimen preparation, compared with 51.5% the single-day regimen the day before colonoscopy (17.0% N/A).
If patients preferred a different purgative, they would favor: 28.1% better taste, 19.5% less volume, 1.0% others (better effect, better smell), 2.1% combined, 49.3% N/A.
Discussion
The present study is the largest study so far analyzing performance quality measures, bowel-preparation quality, and patient experience of routinely used purgatives in one large asymptomatic screening colonoscopy cohort. The investigated cohort of 5000 screenees was well matched in sex and age. Bowel-preparation quality, one of seven key quality parameters defined in the recent ESGE guidelines,6 is associated with ADR and CIR and affects the definition of surveillance intervals.5,17 All purgatives met the target standard of ≥90% rate of adequate bowel preparation. Success rates were significantly higher with HV and LV than with IV; there was no significant difference between HV and LV. This is reflected in the CIR: CIR was excellent in all groups (>98%); highest CIR was achieved with HV, followed by LV and IV (99.4%, 98.5%, 97.5%). Regarding lesion detection rates, all investigated groups met the required ADR standards of ≥20% according to guidelines at the time the study was initiated.18 The more recent quality improvement initiative, requiring an ADR ≥25%, was published during data recruitment.6 This standard was met with HV and IV purgatives, but failed with LV (23.9%). However, lesion detection rates depend on endoscopists’ skills and equipment rather than bowel cleansing quality.15,19,20 An analysis of each bowel segment separately showed that segmental scores of 3 or 4 were least often reached in the right-sided colon with HV, even though HV scored the highest success rates. This discrepancy arises from the definition of success rates according to the Harefield Scale, which requires at least two segments at the same time to have a segmental score of 2 (or better). When analyzing each bowel segment separately, it is unapparent if certain segmental scores were reached in multiple segments at the same time.
Another defined key quality measure is patients’ experience during colonoscopy.6 Interestingly, the present study showed that prior to colonoscopy, only 55.4% of patients worry most about the colonoscopy itself; every fifth patient worries most about possible inconvenience of the purgative and 12.9% about sedation. Therefore, in the future the assessment of patients’ experience should focus on the whole colonoscopy experience, which begins with bowel preparation; especially since despite continuous improvement of performance quality, adherence to screening colonoscopy is rather low. The results of the present study strongly contribute to this important issue. Existing data are scarce and the results of previous studies are controversial. Moreover, most studies included only a small number of patients,12,21–24 and outcomes were often considerably biased because of inhomogeneous patient groups with dissimilar colonoscopy indications or exclusion of large patient groups, i.e. severe constipation or severe heart failure.23,24 Two studies compared 4 l PEG and 2 l sodium picosulfate, one in a split-dose regimen the day before colonoscopy (n = 194)12 and one in a two-day split-dose regimen (n = 173).23 The recommended time interval of no more than five hours between bowel preparation and colonoscopy25 was considered in neither study. The first study showed higher success rates with sodium picosulfate; however, neither showed a difference in preparation quality in the right-sided colon. Sodium picosulfate was superior in convenience, completeness of protocol, side effects and willingness to reuse the same purgative. This might be explained by the large volume consumption at once in the one-day preparation regimen. The amount of fluid intake in the two-day regimen was rather high with 5.2 l in the PEG and 4.3 l in the sodium picosulfate group.23 The present study showed that 52% of the HV group would prefer two-day preparation, while 61% of the LV group would prefer single-dose, split preparation the day before colonoscopy; in the IV group there was no difference. In other studies one-third of patients would prefer two-day and two-thirds preferred same-day preparation in an LV regimen.26 In the present study patient satisfaction and compliance regarding consumption was best with LV purgatives, but the difference was marginal. Notably, patients in the LV group consumed the largest volume of additional fluid and also the largest volume in total. The amount of fluid additionally consumed is estimated and self-reported by the patients. The declared quantities are extraordinary high. However, since the questionnaire was analyzed in an anonymized fashion and was not discussed with the patient, these high amounts of fluid could result as a consequence of misinterpretation by the patient in the questionnaire.
In a prior study, compliance regarding consumption of the full amount of the product and adjuvant fluids was 78.9% in case of a two-day and only 70.4% in case of a same-day preparation regimen with LV purgatives.22 Independent predictors of poor bowel preparation with LV were same-day preparation, discomfort during preparation, constipation and obesity. A recent meta-analysis of 14 trials showed that generally willingness to repeat, completion of bowel preparation fluid and side effects did not differ within two-day and same-day regimens; both regimens were comparable in terms of bowel cleanliness, CIR and ADR.27 However, the meta-analysis did not differentiate between HV, IV and LV purgatives.
Studies comparing 2 l PEG and sodium picosulfate showed no differences in overall lesion detection rates21,22,24 and preparation quality according to the Boston Bowel Preparation Scale.22,24 In one study PEG was superior in adequate preparation quality (Harefield Score A or B) as well as detection rates of adenomas, polyps, and flat adenomas in the right-sided colon. However, the difference in detection rate might result from the inhomogeneous patient cohort since there was no differentiation between diagnostic, surveillance and screening colonoscopies.21 An asymptomatic screening cohort like in the present study is more eligible to assess the impact of bowel preparation quality on lesion detection rates. Moreover, although colonoscopy was performed in the afternoon, sodium picosulfate was administered in a split-dose regimen the day of the procedure, while PEG was administered in a two-day regimen.
A strength of the present study was the large, homogenous study cohort. In addition the study design was non-interventional, which avoids potential bias in patient management of a non-routinely used purgative. However, limitations of the study also arise from the non-interventional design, which did not allow randomization of the purgatives and may also have led to residual confounding of the effects of purgatives and the skills of the endoscopists. The choice of a particular purgative most likely depended on remuneration of insurance institutions rather than distinct patient characteristics since remuneration varies among federal states. Consequently, there was a large variation in treatment group sizes, and Picoprep and Citrafleet needed to be grouped as one LV group, resulting in a four-times ratio between HV and LV. Moreover, even though endoscopists were comparable in terms of training and endoscopic skills (all included endoscopists participate in a nationwide quality control program), lesion detection rates obtained from this study might represent the endoscopists’ skills rather than bowel-preparation quality.28 To minimize a possible bias resulting from performance quality of participating endoscopists, inclusion was limited to endoscopists with an ADR ≥ 20%. Furthermore, we have adjusted all comparisons of lesion detection rates between purgatives for endoscopists and sex and age of the patients, but we cannot exclude the possibility of case-mix effects beyond those attributes.
In summary, all purgatives investigated in the present study showed good bowel-cleansing quality results and patient satisfaction, and compliance was high. More than 90% would use the same purgative again if they had another colonoscopy. The primary quality measure in colonoscopy, ADR, was higher with HV than LV. LV purgatives had higher approval for same-day preparation, while with HV patient comfort was higher when the volume was split overnight. Notably, every fifth patient stated that bowel preparation is the factor that worries him or her most before colonoscopy. Therefore, although the quality of bowel preparation is satisfactory, optimization in taste and volume intake would lead to even higher participation rates in screening colonoscopy.
Table 1.
(b) Overall sex- and age-adjusted success rates of bowel cleansing, age-adjusted success rates for men and women and median age per purgative and sex of all colonoscopies where the cecum was reached (n = 4914, 100%).
| Men |
Women |
|||||||
|---|---|---|---|---|---|---|---|---|
| Purgative | Median age (IQR) | Sex- and-age- adjusted success rate in % | N (%) | Age-adjusted success rate in % | Median age (IQR) | N (%) | Age-adjusted success rate in % | Median age (IQR) |
| LV | 60.6 (54.4–68.1) | 97.2 | 1412 (49.1) | 96.0 | 60.8 (54.4–68.5) | 1463 (50.9) | 97.2 | 60.6 (54.5–67.7) |
| HV | 58.2 (53.1–65.3) | 97.6 | 405 (51.0) | 98.2 | 58.4 (52.9–65.4) | 389 (49.0) | 97.2 | 58.0 (53.3–65.0) |
| IV | 57.8 (53.1–65.7) | 95.2 | 614 (49.3) | 95.4 | 57.0 (52.6–65.0) | 631 (50.7) | 95.1 | 58.6 (53.6–66.1) |
HV: high volume; IQR: interquartile range; IV: intermediate volume; LV: low volume.
Success: grade A (all segments scored segmental score 3 (clear liquid) or 4 (empty and clean)) or grade B (one or more segment scored segmental score 2 (brown liquid/removable semi-solid stools)) according to the Harefield Cleansing Scale (Figure 1). Success (%) is defined as percentage of men and women respectively scored as “success” according to the Harefield Cleaning Scale.
Appendix 1
| PATIENT QUESTIONNAIRE |
|---|
| What concerns you most? (1 answer possible) ○ Possible inconvenience of the colonoscopy ○ Possible inconvenience of the sedation ○ Possible inconvenience of the purgative |
| I informed myself of the possible risks/adverse events of a colonoscopy ○ It applies ○ It barely applies ○ It is not the case |
| I informed myself of the possible risks/adverse events of a sedation (twilight sleep) ○ It applies ○ It barely ○ It is not the case |
| I informed myself of the possible risks/adverse events of a purgative ○ It applies ○ It barely applies ○ It is not the case |
| This is my first colonoscopy ○ yes ○ no |
| I consumed the first portion of the purgative ○ on ______ from (time) _____ until (time) _____ ○ I additionally consumed the amount of _____ liters ○ I consumed the entire amount of the purgative □ _yes □ _no |
| I consumed the second portion of the purgative ○ on ______ from (time) _____ until (time) _____ ○ I additionally consumed the amount of _____ liters ○ I consumed the entire amount of the purgative □ yes □ no |
| I adhered to the nutritional recommendations (no whole grain products, no muesli, no salads, no berries/grapes, no tomatoes/pickles/bell peppers, no onions, no corn, etc.) ○ The day of the colonoscopy ○ The day before colonoscopy ○ Two days before colonoscopy ○ Three days before colonoscopy ○ Four days before colonoscopy ○ Five days before colonoscopy ○ I did not adhere to the nutritional recommendations |
| I ate the following products ______ Last _____ days before the examination |
| I would prefer to consume the purgative the following way ○ Half of the purgative the day before, half the day of colonoscopy ○ The total amount of the purgative on the day of colonoscopy |
| I experienced the taste as ○ Neutral ○ Better than expected ○ Worse than expected |
| Overall I experienced the purgative as ○ Neutral ○ Better than expected ○ Worse than expected |
| What would discourage you most to consume the entire volume of the purgative? ○ Bad taste ○ Too large volume of liquid intake ○ Bad smell ○ Inconvenient color |
| What would be the maximum volume of purgative you would consume ○ 0.5 liter ○ 1 liter ○ 2 liter ○ 3 liter ○ 4 liter ○ >4 liter |
| If I had the choice I would for the next colonoscopy ○ use this purgative again ○ use a different purgative |
| If you would prefer another purgative, what qualities would you prefer ○ better taste ○ less volume to drink ○ others ____ |
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This work was supported by Norgine Pharma GmbH.
Ethics approval
The Austrian Data Protection Committee and the Ethics Committee of the Medical University of Vienna provided permission (Ethics Committee of the Medical University of Vienna, project number 1726/2014, ethical approval on November 4, 2014). The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Informed consent
All included patients provided written, informed consent for data analysis in the framework of scientific studies.
References
- 1.Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc 2003; 58: 76–79. [DOI] [PubMed] [Google Scholar]
- 2.Froehlich F, Wietlisbach V, Gonvers JJ, et al. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: The European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc 2005; 61: 378–384. [DOI] [PubMed] [Google Scholar]
- 3.Wu KL, Rayner CK, Chuah SK, et al. Impact of low-residue diet on bowel preparation for colonoscopy. Dis Colon Rectum 2011; 54: 107–112. [DOI] [PubMed] [Google Scholar]
- 4.Aoun E, Abdul-Baki H, Azar C, et al. A randomized single-blind trial of split-dose PEG-electrolyte solution without dietary restriction compared with whole dose PEG-electrolyte solution with dietary restriction for colonoscopy preparation. Gastrointest Endosc 2005; 62: 213–218. [DOI] [PubMed] [Google Scholar]
- 5.Hassan C, Bretthauer M, Kaminski MF, et al. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2013; 45: 142–150. [DOI] [PubMed] [Google Scholar]
- 6.Kaminski MF, Thomas-Gibson S, Bugajski M, et al. Performance measures for lower gastrointestinal endoscopy: A European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. United European Gastroenterol J 2017; 5: 309–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lieberman D, Nadel M, Smith RA, et al. Standardized colonoscopy reporting and data system: Report of the Quality Assurance Task Group of the National Colorectal Cancer Roundtable. Gastrointest Endosc 2007; 65: 757–766. [DOI] [PubMed] [Google Scholar]
- 8.de Jonge V, Sint Nicolaas J, Cahen DL, et al. Quality evaluation of colonoscopy reporting and colonoscopy performance in daily clinical practice. Gastrointest Endosc 2012; 75: 98–106. [DOI] [PubMed] [Google Scholar]
- 9.Ben-Horin S, Bar-Meir S, Avidan B. The impact of colon cleanliness assessment on endoscopists’ recommendations for follow-up colonoscopy. Am J Gastroenterol 2007; 102: 2680–2685. [DOI] [PubMed] [Google Scholar]
- 10.Enestvedt BK, Fennerty MB, Eisen GM. Randomised clinical trial: MiraLAX vs. Golytely—A controlled study of efficacy and patient tolerability in bowel preparation for colonoscopy. Aliment Pharmacol Ther 2011; 33: 33–40. [DOI] [PubMed] [Google Scholar]
- 11.Shieh FK, Gunaratnam N, Mohamud SO, et al. MiraLAX-Gatorade bowel prep versus GoLytely before screening colonoscopy: An endoscopic database study in a community hospital. J Clin Gastroenterol 2012; 46: e96–e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim YS, Hong CW, Kim BC, et al. Randomized clinical trial comparing reduced-volume oral picosulfate and a prepackaged low-residue diet with 4-liter PEG solution for bowel preparation. Dis Colon Rectum 2014; 57: 522–528. [DOI] [PubMed] [Google Scholar]
- 13.Kwon JE, Lee JW, Im JP, et al. Comparable efficacy of a 1-L PEG and ascorbic acid solution administered with bisacodyl versus a 2-L PEG and ascorbic acid solution for colonoscopy preparation: A prospective, randomized and investigator-blinded trial. PloS One 2016; 11: e0162051–e0162051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferlitsch M, Reinhart K, Pramhas S, et al. Sex-specific prevalence of adenomas, advanced adenomas, and colorectal cancer in individuals undergoing screening colonoscopy. JAMA 2011; 306: 1352–1358. [DOI] [PubMed] [Google Scholar]
- 15.Waldmann E, Britto-Arias M, Gessl I, et al. Endoscopists with low adenoma detection rates benefit from high-definition endoscopy. Surg Endosc 2015; 29: 466–473. [DOI] [PubMed] [Google Scholar]
- 16.Halphen M, Heresbach D, Gruss HJ, et al. Validation of the Harefield Cleansing Scale: A tool for the evaluation of bowel cleansing quality in both research and clinical practice. Gastrointest Endosc 2013; 78: 121–131. [DOI] [PubMed] [Google Scholar]
- 17.Hassan C, Quintero E, Dumonceau JM, et al. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2013; 45: 842–851. [DOI] [PubMed] [Google Scholar]
- 18.Jover R, Herráiz M, Alarcón O, et al. Clinical practice guidelines: Quality of colonoscopy in colorectal cancer screening. Endoscopy 2012; 44: 444–451. [DOI] [PubMed] [Google Scholar]
- 19.Bretagne JF, Hamonic S, Piette C, et al. Interendoscopist variability in proximal colon polyp detection is twice higher for serrated polyps than adenomas. World J Gastroenterol 2016; 22: 8549–8557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brenner H, Chang-Claude J, Seiler CM, et al. Interval cancers after negative colonoscopy: Population-based case-control study. Gut 2012; 61: 1576–1582. [DOI] [PubMed] [Google Scholar]
- 21.Pohl J, Halphen M, Kloess HR, et al. Impact of the quality of bowel cleansing on the efficacy of colonic cancer screening: A prospective, randomized, blinded study. PloS One 2015; 10: e0126067–e0126067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manes G, Amato A, Arena M, et al. Efficacy and acceptability of sodium picosulphate/magnesium citrate vs low-volume polyethylene glycol plus ascorbic acid for colon cleansing: A randomized controlled trial. Colorectal Dis 2013; 15: 1145–1153. [DOI] [PubMed] [Google Scholar]
- 23.Munsterman ID, Cleeren E, van der Ploeg T, et al. ‘Pico-Bello-Klean study’: Effectiveness and patient tolerability of bowel preparation agents sodium picosulphate-magnesium citrate and polyethylene glycol before colonoscopy. A single-blinded randomized trial. Eur J Gastroenterol Hepatol 2015; 27: 29–38. [DOI] [PubMed] [Google Scholar]
- 24.Jeon SR, Kim HG, Lee JS, et al. Randomized controlled trial of low-volume bowel preparation agents for colonic bowel preparation: 2-L polyethylene glycol with ascorbic acid versus sodium picosulfate with magnesium citrate. Int J Colorectal Dis 2015; 30: 251–258. [DOI] [PubMed] [Google Scholar]
- 25.Bucci C, Rotondano G, Hassan C, et al. Optimal bowel cleansing for colonoscopy: Split the dose! A series of meta-analyses of controlled studies. Gastrointest Endosc 2014; 80: 566–576.e2. [DOI] [PubMed] [Google Scholar]
- 26.Longcroft-Wheaton G, Bhandari P. Same-day bowel cleansing regimen is superior to a split-dose regimen over 2 days for afternoon colonoscopy: Results from a large prospective series. J Clin Gastroenterol 2012; 46: 57–61. [DOI] [PubMed] [Google Scholar]
- 27.Cheng YL, Huang KW, Liao WC, et al. Same-day versus split-dose bowel preparation before colonoscopy: A meta-analysis. J Clin Gastroenterol 2018; 52: 392–400. [DOI] [PubMed] [Google Scholar]
- 28.Waldmann E, Gessl I, Sallinger D, et al. Trends in quality of screening colonoscopy in Austria. Endoscopy 2016; 48: 1102–1109. [DOI] [PubMed] [Google Scholar]