Abstract
Background
Endoscopic mucosal resection of large non-pedunculated colon polyps is challenging.
Objective
To determine if the time of day or daily endoscopic workload play a role in outcomes of endoscopic mucosal resection for large non-pedunculated colon polyps greater than 20 mm.
Methods
This is a retrospective study of patients who underwent endoscopic mucosal resection of large non-pedunculated colon polyps. The time of day and endoscopic workload were compared across the following outcomes: the rate of complete resection of the polyp, the rate of referral for surgery, and the rate of residual neoplasia on follow-up.
Results
One hundred and three endoscopic mucosal resection procedures were performed. There were no differences in the rates of complete resection (80.8% vs. 70.0%; P = 0.25), the need for surgery (27.4% vs. 33.3%; P = 0.55), and rate of residual neoplasia (24.5% vs. 50.0%; P = 0.07) when comparing the time of day. Colon polyps greater than 40 mm were less likely to be completely resected versus polyps sized 20–39 mm (56.8% vs. 91.9%; P < 0.001). In cases with no residual neoplasia on follow-up, the mean duration for the index procedure was 45.6 minutes versus 60.7 minutes when there was residual neoplasia (P < 0.01).
Conclusion
The time of day and endoscopic workload does not affect outcomes for endoscopic mucosal resection of large non-pedunculated colon polyps, but the size of large non-pedunculated colon polyps and resection times do.
Keywords: Endoscopic mucosal resection, colonoscopy, colon cancer
Key points
It is unknown if the time of day of colonoscopy with endoscopic resection of large sessile polyps or if daily endoscopic workload affects outcomes.
This study shows that the time of day and endoscopic workload does not affect clinically meaningful outcomes for endoscopic mucosal resection of large non-pedunculated polyps of the colon but the size of the polyp and resection times do.
Introduction
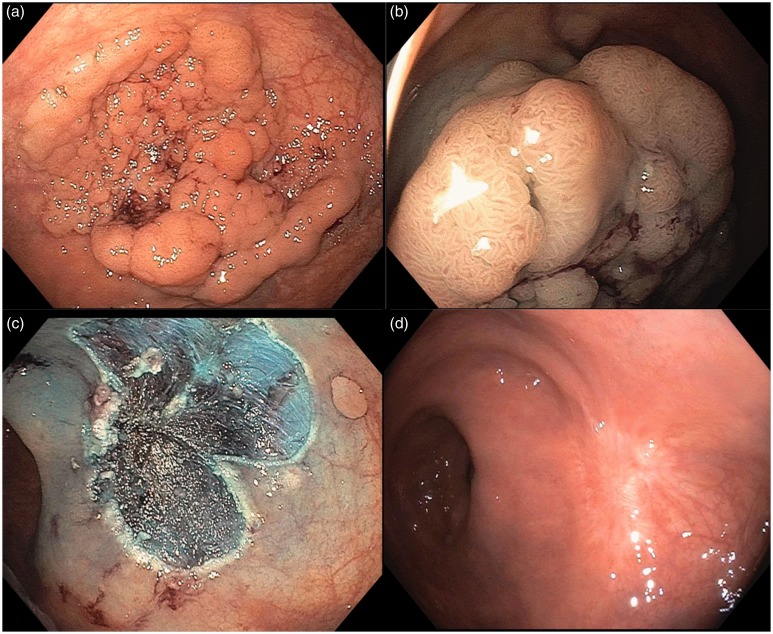
Colorectal adenocarcinoma is the second leading cause of cancer-related death in the United States.1 However, colonoscopy with polypectomy can decrease the incidence and mortality from colorectal cancer.2 In general, the removal of flat polyps up to 20 mm is often performed in the community setting without complications.3 However, the removal of large non-pedunculated colon polyps (LNPCPs) is often technically difficult and time consuming. LNPCPs are considered by many endoscopists the most challenging colorectal polyps for endoscopic resection.4 Polyps larger than 20 mm or those in challenging locations such as the ileocecal valve, appendicular orifice, near the dentate line or extending across an acute flexure are referred to as ‘complex colon polyps’.5,6 Such lesions are often referred to an expert endoscopist in a tertiary care center for removal by the endoscopic mucosal resection (EMR) technique.7 This technique typically involves using cap-fitted high definition colonoscopes, submucosal injection with a saline solution mixed with either methylene blue or indigo carmine, resection using snare polypectomy, avulsion or ablation of residual polypoid tissue at the resection margin and clip closure.8 Figure 1 shows an example of a colonoscopy with EMR in this study. Colon EMR has been shown to be both a safe and effective alternative to surgical resection for large or complex polyps.8–10 Modeling studies suggest that colon EMR may have lower morbidity and mortality than surgery for LNPCPs and provide significant cost savings to the health system when compared with surgery.9,11
Figure 1.
Endoscopic mucosal resection with no recurrence on follow-up examination. (a) Non-pedunculated colon polyp prior to resection. (b) The polyp after a submucosal injection of methylene blue solution. (c) Post-endoscopic resection of the polyp. (d) Follow-up examination 6 months later showing no residual polyp.
Given the complexity of EMR for LNPCPs, these procedures are often booked early in the morning to promote optimal conditions for the endoscopist. However, overbooked schedules or urgent cases with high-grade dysplasia often prompt cases to be scheduled later in the day to accommodate an earlier appointment, as it is uncertain how the time of day or endoscopic workload affects procedure outcomes. Endoscopist workload and fatigue in relation to the outcomes of endoscopic procedures has been measured for colonoscopy, endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound.12–14 Endoscopist fatigue has been measured in terms of the total number of endoscopic procedures, the total number of procedures weighted for the difficulty of those procedures, and the total number of relative value units (RVUs) performed prior to the procedure of interest.12 Other studies have assessed endoscopist fatigue by comparing outcomes for procedures performed in the morning versus the afternoon.13 Meanwhile, others have estimated fatigue using the procedure start time on a continuous scale.14 In the present study, our aim was to assess whether the time of day or daily endoscopic workload affected any of the clinically meaningful outcomes in colon EMR. Clinically meaningful outcomes with regard to colon EMR include the rates of complete resection during index colonoscopy, surgical management due to non-curative endoscopic resection, and residual neoplasia on surveillance.
Materials and methods
Study design, setting and patients
This is a retrospective cohort study of patients from four advanced endoscopists at an academic tertiary referral center who underwent colon EMR and who have appropriate follow-up. All four endoscopists, whose procedures are included in this review, had performed more than 100 colon EMR procedures prior to the beginning of the study period. This study was approved by the Zucker School of Medicine at Hofstra/Northwell Institutional Review Board on 14 June 2017. Written informed consent was not required from each patient, as per each institution’s institutional review board, as this was a retrospective study. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in prior approval by the institutional review board at each site.
Inclusion criteria for this study were sessile or flat polyps (Paris classification Is, 0–IIa, 0–IIb, 0–IIc), size greater than 20 mm, resection using the EMR technique, and patient age greater than 18 years. In this study, the technique used for colon EMR was saline lift with or without the cap assist technique. Exclusion criteria for this study included pedunculated polyps, size less than 20 mm, polyps that had prior attempts at resection, polyps resected not using the EMR technique and inadequate follow-up.
Data acquisition was conducted by reviewing all endoscopy reports from a prospectively maintained database. All procedures were performed by four endoscopists with formal training in advanced endoscopy, at North Shore University Hospital or Long Island Jewish Medical Centers between 1 October 2015 and 30 August 2017. Follow-up colonoscopy to survey the colon EMR site was performed 3–12 months after the index procedure when the colon polyp was removed. All surveillance colonoscopy reports were reviewed to assess for residual neoplasia. The primary outcomes measured were the rate of complete resection on initial colonoscopy, the rate of surgical management for non-curative endoscopic resection, and the rate of residual neoplasia on follow-up colonoscopy. These outcomes were compared to the time of day of the performed EMR and daily endoscopic workload as measured below.
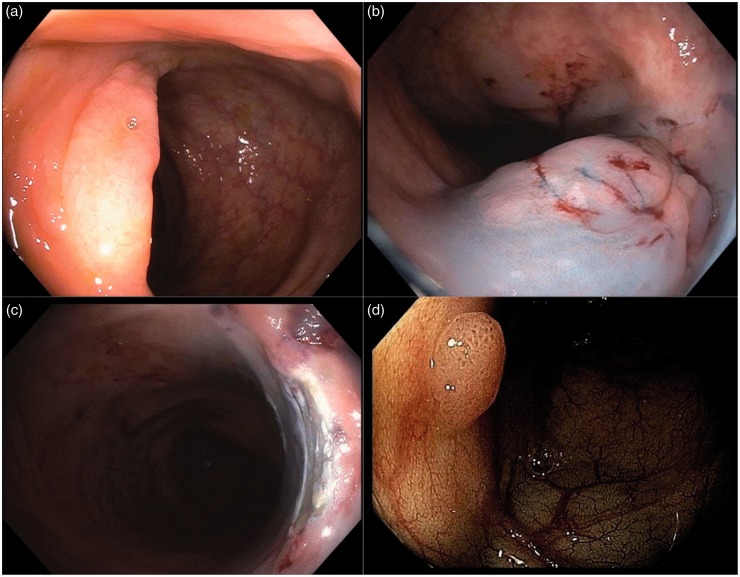
Primary outcome measures
The rate of complete resection on initial colonoscopy was defined as the percentage of complete resection of the target lesion during index colonoscopy. The rate of surgical management for non-curative endoscopic resection was defined as the overall rate of surgical colonic resection following colon EMR for any reason. This includes patients who required surgery due to invasive carcinoma, patients who required surgery for incompletely resected premalignant colonic polyps and patients with polyposis syndromes warranting surgery. The rate of residual neoplasia was defined as any residual polypoid tissue, found on surveillance colonoscopy at the polypectomy site, biopsy proved to be histologically identical to the original lesion. Figure 2 shows an example of this. If there was no residual polypoid tissue at the colon EMR site, the decision to biopsy the EMR site was left to the discretion of the endoscopist. If there was no residual polypoid tissue and no biopsy was performed, it was considered as absence of residual neoplasia.
Figure 2.
Endoscopic mucosal resection with recurrence on follow-up examination. (a) Non-pedunculated colon polyp prior to resection. (b) The polyp after a submucosal injection of methylene blue solution. (c) Post-endoscopic resection of the polyp. (d) Follow-up examination 6 months later showing residual polyp.
Time of procedure and measures of endoscopic workload
The start time for each colon EMR was recorded and used to compare morning (prior to 12:00 pm) versus afternoon (after 12:00 pm) procedures. Preprocedural endoscopic workload prior to the colon EMR procedure of interest was calculated using three different measures. These workload scores, also referred to as fatigue estimates, are specific metrics designed to measure endoscopist workload based on the number and complexity of the procedures performed prior to the colonoscopy with EMR of interest.12 The first of these metrics is called the raw endoscopic workload score. This score is calculated by adding the total number of endoscopic procedures completed before the colon EMR under consideration. All procedures are given a numeric value of one (e.g. oesophagogastroduodenoscopy (EGD) 1, colonoscopy 1, ERCP 1) (Table 1). The second of these metrics is called the consensus endoscopic workload score. In order to calculate this score, different endoscopic procedures are assigned different values based on their complexity (e.g. EGD 0.5, colonoscopy 1, ERCP 1.5) (Table 1). This score is calculated by adding the total value of all procedures performed prior to the colon EMR under consideration.15 The final of these metrics is called the RVU endoscopic workload score. This score is calculated by adding the RVU weights for all endoscopic procedures performed prior to the colon EMR under consideration (Table 1).16 In our endoscopist workload analysis, colon EMR procedures were considered more complex than colonoscopy with or without polypectomy, and were assigned a higher value in the consensus workload score (colon EMR 1.5, colonoscopy 1) as well as a higher RVU score.
Table 1.
Raw, consensus and RVU weights for endoscopic procedures.
| Endoscopic procedure | Raw weights | Consensus weightsa | RVU weightsb |
|---|---|---|---|
| Colonoscopy | 1 | 1 | 2.82–5.60 |
| EGD | 1 | 0.5 | 1.82–4.97 |
| Flexible sigmoidoscopy | 1 | 0.5 | 0.84–3.62 |
| EUS | 1 | 1.5 | 2.22–7.25 |
| ERCP | 1 | 1.5 | 5.95–8.94 |
| Luminal stent | 1 | 1.5 | 3.50–7.46 |
| Enteroscopy (push or single balloon) | 1 | 1.5 | 2.59–7.46 |
RVU: relative value unit; EGD: oesophagogastroduodenoscopy; EUS: endoscopic ultrasound; ERCP: endoscopic retrograde cholangiopancreatography.
Adapted from Lurix et al.15 Used with permission from Elsevier.
For each endoscopic procedure current procedural terminology codes were recorded and the corresponding RVU weight as specified by the Centers of Medicare and Medicaid were calculated.
Procedural complexity and workload was assessed by evaluating procedure duration for the colon EMR of interest. In cases in which two lesions were removed by the EMR technique during a single colonoscopy, the overall procedure time was averaged across both lesions. Procedure duration was then compared against the colon EMR outcomes of interest. Additional data on patient and polyp characteristics were tabulated for all procedures included in this retrospective review.
Statistical analyses
Summary statistics were generated to describe patient and polyp characteristics for each endoscopist individually (Supplementary Table 1) and overall (Supplementary Table 2). Student’s t-test was used to assess differences in patient age and polyp size (when considered as a continuous variable) between morning and afternoon cases. The chi square test was used to assess differences in polyp location and polyp size (when considered as a dichotomous variable, 20–39 mm vs. >40 mm). The same analyses were performed across time of day quartiles for the raw, consensus and RVU workload scores.
For the primary analysis, the predictors (exposures) were the time of day (morning vs. afternoon), the three measures of endoscopic workload (raw, consensus and RVU workload scores) and procedure duration. In order to calculate the three different measures of endoscopic workload, all the procedures performed prior to the colon EMR under investigation were recorded and assigned a specified value and or weight used to calculate the raw, consensus and RVU workload scores.
To assess the effect of preprocedural endoscopic workload on colon EMR outcomes, the dataset was divided into quartiles using SPSS statistical software. The first quartile represented the colon EMR procedures with the lowest workload estimates while the fourth quartile represented colon EMR procedures with the highest workload estimates. The associations between time of day as well as endoscopic workload and the outcomes of interest were evaluated using logistic regression.
In order to assess the impact of each individual endoscopist on the colon EMR outcomes of interest and to assess their association with endoscopic workload, binary logistic regression using a stepwise approach was performed. First, the effect of each individual endoscopist was assessed as a predictor in relation to the outcomes of interest using logistic regression (step 1). Next, logistic regression analysis was performed assessing the effect of workload on the colon EMR outcomes of interest when controlling for differences between the individual endoscopists (step 2). To assess the effect of the procedure-related endoscopic workload on colon EMR outcomes, the procedure duration was assessed and compared against the colon EMR outcomes of interest using t-tests.
In secondary analysis, the size and location of the colon polyp were considered the predictors (exposures). Colon EMR outcomes were compared with regard to colon polyps sized 20–39 mm versus greater than 40 mm and right-sided colon lesions versus left-sided lesions. Logistic regression analysis was used in these calculations. All analyses were performed using IBM SPSS statistics version 25 (IBM SPSS statistics, Pittsburgh, PA, USA).
Results
Patient and lesion characteristics
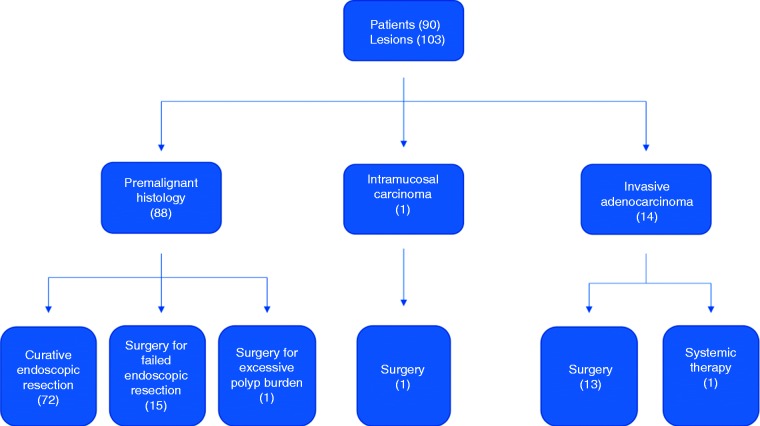
In total, 90 patients underwent colonoscopy with EMR to remove a total of 103 LNPCPs. In 85 cases, a single EMR procedure was performed during colonoscopy. Meanwhile, in nine cases two different lesions were resected by the EMR technique during the same colonoscopy. Figure 3 contains a flow chart that summarizes the follow-up for the patients included in this study. Overall, the median age of patients undergoing colon EMR was 64 years. The mean size of colon polyps being treated using the EMR technique was 35.3 mm. There were more right than left-sided colon polyps (59.2% vs. 40.8%) (Supplementary Table 2). The characteristics of the patients and the colon lesions treated are summarized for each endoscopist in Supplementary Table 1.
Figure 3.
Flowchart of patients included in this study.
Endoscopic workload analysis
The four endoscopists in the study performed a median of two (range 0–10) endoscopic procedures prior to performing the colon EMR of interest. The majority of the colonoscopy with EMR procedures were performed in the morning (70.9%) versus the afternoon (29.1%). There were no differences in the rates of complete resection (80.8% vs. 70.0%; P = 0.25), the need for surgery due to non-curative resection (27.4% vs. 33.3%; P = 0.55) and the rate of residual neoplasia (24.5% vs. 50.0%; P = 0.07) when comparing morning and afternoon colon EMRs. Endoscopic workload, estimated using the raw, consensus and RVU scores, did not have any effect on these outcome measures when comparing across quartiles (Table 2).
Table 2.
Association between endoscopic workload and colon EMR outcome measures.
| Workload measure | Complete resection | P value | Surgery | P value | Residual neoplasia | P value |
|---|---|---|---|---|---|---|
| Start time | ||||||
| Morning | 80.8 | 0.25 | 27.4 | 0.55 | 24.5 | 0.07 |
| Afternoon | 70.0 | 33.3 | 50.0 | |||
| Raw fatigue score | ||||||
| Quartile 1 | 80.8 (21/26) | 0.66 | 34.6 (9/26) | 0.54 | 23.5 (4/17) | 0.52 |
| Quartile 2 | 73.8 (31/42) | 21.4 (9/42) | 30.3 (10/33) | |||
| Quartile 3 | 87.5 (14/16) | 37.5 (6/16) | 50.0 (5/10) | |||
| Quartile 4 | 73.7 (14/19) | 31.6 (6/19) | 25.0 (3/12) | |||
| Consensus fatigue score | ||||||
| Quartile 1 | 80.8 (21/26) | 0.88 | 34.6 (9/26) | 0.52 | 23.5 (4/17) | 0.73 |
| Quartile 2 | 74.1 (20/27) | 22.2 (6/27) | 28.6 (6/21) | |||
| Quartile 3 | 80.8 (21/26) | 23.1 (6/26) | 40.0 (8/20) | |||
| Quartile 4 | 75.0 (18/24) | 37.5 (9/24) | 28.6 (4/14) | |||
| RVU fatigue score | ||||||
| Quartile 1 | 80.8 (21/26) | 0.86 | 34.6 (9/26) | 0.60 | 23.5 (4/17) | 0.83 |
| Quartile 2 | 69.6 (16/23) | 21.7 (5/23) | 38.9 (7/18) | |||
| Quartile 3 | 82.8 (24/29) | 24.1 (7/29) | 31.8 (7/22) | |||
| Quartile 4 | 76.0 (19/25) | 36.0 (9/25) | 26.7 (4/15) | |||
EMR: endoscopic mucosal resection; RVU: relative value unit.
In assessing differences between individual endoscopists across the colon EMR outcomes of interest there were significant differences in terms of the rate of complete resection (range 60.9–100%; P = 0.01) and the rate of residual neoplasia on follow-up (range 0–42.9%; P < 0.01). There was no difference in terms of the rate of referral for surgical resection (range 22.2–47.8%; P = 0.18). To evaluate whether these differences had any influence with regard to the relationship between endoscopic workload and the colon EMR outcomes of interest when controlling for the effect of the endoscopist, binary linear regression analysis was performed in a stepwise fashion and demonstrated no significant effect.
The procedure duration did not influence rates of complete resection (P = 0.27) or the rate of referral for surgery (P = 0.98). However, there was a significant relationship between procedure duration and the rates of residual neoplasia on follow-up. In cases with no residual neoplasia on surveillance colonoscopy, the mean duration for the index colon EMR procedure was 45.6 minutes versus 60.7 minutes for colon EMR cases in which there was residual neoplasia on follow-up (P < 0.01).
Polyp characteristics analysis
Colon polyps greater than 40 mm were less likely to be completely resected during the initial procedure as compared with polyps sized 20–39 mm (56.8% vs. 91.9%; P < 0.001). The rate of surgical treatment was greater for lesions greater than 40 mm than those sized 20–39 mm (48.6% vs. 18.0%; P = 0.002). The rate of invasive carcinoma in lesions greater than 40 mm did not differ significantly from lesions sized 20–39 mm (16.2% vs. 11.5%; P = 0.53). There was no difference in the rate of residual neoplasia for colon polyps greater than 40 mm versus lesions sized 20–39 mm (28.0 vs. 33.3; P = 0.71) (Table 3).
Table 3.
Polyp size and correlation to outcomes.
| Size of polyp | 20–39 mm (61) | >40 mm (37) | P value |
|---|---|---|---|
| Rate of invasive carcinoma | 11.5% | 16.2% | 0.53 |
| Rate of complete resection on index EMR | 91.9% | 56.8% | <0.001 |
| Rate of surgery | 18.0% | 48.6% | 0.002 |
| Curative endoscopic resection of premalignant lesions | 94.2% | 58.1% | <0.001 |
| Residual neoplasia | 28.0% | 33.3% | 0.71 |
EMR: endoscopic mucosal resection.
Complete resection during initial colon EMR was 78.6% for left-sided lesions as compared with 77.0% for right-sided lesions (P = 0.82). There was no difference in the rate of surgical management for right and left-sided lesions (26.2% vs. 33.3%; P = 0.44). The rate of residual neoplasia did not differ between right and left-sided lesions (37.8% vs. 18.5%; P = 0.09).
Discussion
In this study we found no significant difference in the rates of complete resection, the need for surgery, and residual neoplasia between colon EMR procedures performed in the morning compared with those performed in the afternoon.
In assessing the effect of endoscopic workload on procedural outcomes in colon EMR, neither the total number of procedures, with or without consideration of procedure complexity, adversely affected the clinical outcomes of interest. These findings are significant because heretofore, neither the time of day nor measures of endoscopic workload have been assessed as factors that may affect clinical outcomes in colon EMR.
The rate of complete resection in our series (77.7%) is comparable to that in a previously published study when controlling for the size of colon polyps (69.7%).8 The rate of residual neoplasia in our study (30.6%) is similar to that found in a large multicenter Australian study of EMR for large colon polyps (20.4%).17 Within the literature on colon EMR there is heterogeneity in the reported rates of residual neoplasia (4.4–20.4%).8,17–19 This heterogeneity may reflect the size of the polyps included in the studies and the rates of follow-up. One study with a particularly low rate of residual neoplasia included patients with polyps less than 20 mm as well polyps greater than 20 mm in reporting their rates of residual neoplasia.8 By virtue of only including polyps greater than 20 mm, it can be expected that the rate of residual neoplasia may be greater in our series. Furthermore, many previous studies reporting on this measure had varying degrees of follow-up making it difficult to assess the true rate of residual neoplasia. In our study, we excluded cases with inadequate follow-up and therefore our results may more accurately reflect the true rates of residual neoplasia.
Very large polyps (>40 mm in size) had significantly lower rates of complete endoscopic resection on initial colon EMR than polyps sized 20–39 mm. Very large polyps were more likely to be treated surgically than those sized 20–39 mm. This is consistent with previously published series.8,10,19,20 A recent retrospective review of a large Australian series showed that size as part of a more comprehensive scoring system – known as the size, morphology, site, access (SMSA) – influenced rates of complete resection and adenoma recurrence.20 In the SMSA scoring system more points are attributed to more complex lesions; however, larger size plays a relatively disproportionate role relative to morphology, site and access. All the lesions included in this study would be scored as SMSA3 or SMSA4 lesions. Furthermore, all lesions in this review greater than 40 mm would be classified as SMSA4 lesions, which were shown to have lower rates of complete resection relative to SMSA3 or SMSA2 lesions.20
Procedure duration did not have any effect on the rate of complete resection or referral for surgical resection; however, it did have a significant effect on the rates of residual neoplasia. The direct relationship between procedure duration and the rate of residual neoplasia on follow-up suggests that increased procedure length of index colon EMR is associated with an increased rate of residual neoplasia on follow-up colonoscopy. Longer procedure duration may be indicative of a more complex procedure and might therefore explain the relationship between increased duration of the index procedure and higher rates of residual neoplasia on follow-up.
The strengths of this study include assessment exclusively of LNPCPs, and a series of over 100 cases with long-term follow-up ranging from 3 months to 2 years. All patients included in this study had follow-up colonoscopy, went for surgery or were treated for metastatic disease. Polyp or tumor histology was available for all patients included in this review. In addition, all four endoscopists included in this study had sufficient experience with colon EMR prior to the study period. A learning curve study for colon EMR found that 100 colon EMR procedures were necessary before the operator achieved a plateau phase in terms of clinically meaningful outcomes.21 Finally, including four endoscopists, with a distribution of cases done by each endoscopist, protects against skew in our dataset and makes the data more generalizable to everyday practice.
This study is limited by its nature as a retrospective observational study. Review of the data did not allow assessment of whether any prior biopsy of the lesion had been performed. Extensive biopsy can lead to scarring and fibrosis which complicates subsequent colon EMR. It has been shown that previous intervention is an independent risk factor for failed endoscopic therapy (odds ratio 3.75, 95% confidence interval 1.77–7.97).17 However, this study reports on a ‘real-life’ practice of four endoscopists and thus controlling for this, if possible, would affect the applicability of this study to everyday practice. This study did exclude polyps that had prior attempts at removal, as this would create significant fibrosis that would make a polyp more challenging to remove. Finally, not surprisingly, there were differences between individual endoscopists in terms of the outcomes of interest, and thus aggregating colon EMR cases from four different endoscopists is another limitation. However, to account for this, stepwise logistic regression analysis controlling for the effect of the individual endoscopist demonstrated that despite these differences, endoscopic workload did not have an effect on the colon EMR outcomes evaluated in this study.
The findings of this study contribute to data on the time of day and the effect of endoscopic workload on endoscopic outcome measures. In a large community setting, neither the time of day nor endoscopist workload affected adenoma detection rates during screening or surveillance colonoscopy.12 In another study, it was found that neither biliary cannulation success, ERCP completion rates nor serious adverse events differed between ERCP done in the morning versus the afternoon.13 However, another study assessing the time of day on the sensitivity and diagnostic accuracy of fine needle aspiration during endoscopic ultrasound for solid pancreatic lesions found that later start times had an adverse effect.14
Supplemental Material
Supplemental material for Effect of time of day and daily endoscopic workload on outcomes of endoscopic mucosal resection for large sessile colon polyps by Yonatan J Hillman, Bari S Hillman, Divyesh V Sejpal, Calvin Lee, Larry S Miller, Petros C Benias and Arvind J Trindade in United European Gastroenterology Journal
Author contribution
Conception and design AJT, YJH. Analysis and interpretation of the data AJT, YJH, BSH, PCB, CL, DVS and LSM. Drafting of the article AJT, YJH, BSH, PCB, CL, DVS and LSM. Critical revision of the article for important intellectual content AJT, YJH, BSH, PCB, CL, DVS and LSM. Final approval of the article AJT, YJH, BSH, PCB, CL, DVS and LSM.
Declaration of conflicting interests
DVS is a consultant for Boston Scientific and Olympus America. AJT is a consultant for Pentax Medical. PCB is a consultant for Medtronic and Apollo. YJH, BSH, CL and LSM have no conflicts of interest to report.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethics approval
Institutional review board approval was obtained. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a prior approval by the institutions’ human research committees.
Informed consent
Not required, as this was a retrospective study.
References
- 1.Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology 2008; 134: 1570–1595. [DOI] [PubMed] [Google Scholar]
- 2.Zauber AG, Winawer SJ, Obrien MJ, et al. Colonoscopic polypectomy and long term prevention of colorectal-cancer deaths. N Engl J Med 2012; 366: 687–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rex D, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc 2015; 81: 31–53. [DOI] [PubMed] [Google Scholar]
- 4.Overhiser AJ, Rex DK. Work and resources needed for endoscopic resection of large sessile colorectal polyps. Clin Gastroenterol Hepatol 2007; 5: 1076–1079. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez-Yague A, Kaltlenbach T, Raju G, et al. Advanced endoscopic resection of colorectal lesions. Gastroenterol Clin N Am 2013; 42: 459–477. [DOI] [PubMed] [Google Scholar]
- 6.Rutter M, Nickerson C, Rees C, et al. Risk factors for adverse events related to polypectomy in the English Bowel Cancer Screening Programme. Endoscopy 2014; 46: 90–97. [DOI] [PubMed] [Google Scholar]
- 7.Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection: European Society of Gastrointestinal Endoscopy Clinical Guideline. Endoscopy 2017; 49: 270–297. [DOI] [PubMed] [Google Scholar]
- 8.Raju G, Lum PJ, Ross W, et al. Outcome of EMR as an alternative to surgery in patients with complex colon polyps. Gastrointest Endosc 2016; 84: 315–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahlenstiel G, Hourigan LF, Brown G, et al. Actual endoscopic versus predicted surgical mortality for treatment of advanced mucosal neoplasia of the colon. Gastrointest Endosc 2014; 80: 668–676. [DOI] [PubMed] [Google Scholar]
- 10.Hassan C, Repici, SharmaP, et al. Efficacy and safety of endoscopic resection of large colorectal polyps: a systematic review and meta-analysis. Gut 2016; 65: 806–820. [DOI] [PubMed] [Google Scholar]
- 11.Jayanna M, Burgess NG, Singh R, et al. Cost Analysis of endoscopic mucosal resection vs surgery for large laterally spreading colorectal lesions. Clin Gastroenterol Hepatol 2016; 14: 271–278. [DOI] [PubMed] [Google Scholar]
- 12.Lee A, Jensen CD, Marks AR, et al. Endoscopist fatigue estimates and colonoscopic adenoma detection in a large community-based setting. Gastrointest Endosc 2017; 85: 601–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mehta PP, Sanaka MR, Mullen KD, et al. Effect of the time of day on the success and adverse events of ERCP. Gastrointest Endosc 2011; 74: 303–308. [DOI] [PubMed] [Google Scholar]
- 14.Korenblit J, Tholey DM, Tolin J, et al. Effect of the time of day and queue position in the endoscopic schedule on the performance characteristics of endoscopic ultrasound-guided fine-needle aspiration for diagnosing pancreatic malignancies. Endosc Ultrasound 2016; 5: 78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lurix E, Hernandez AV, Thoma M, et al. Adenoma detection rate is not influenced by full day blocks, time or modified queue position. Gastrointest Endosc 2012; 75: 827–834. [DOI] [PubMed] [Google Scholar]
- 16.American College of Gastroenterology. 2016 Medicare Physician Final Fee Schedule Reimbursement and RVU Changes. American College of Gastroenterology website. www.gi.org/wp-content/uploads/2016/01/Medicare-2016-RVU-breakdown-Nov-20152.pdf. Published November, 2015. Accessed December, 2016.
- 17.Moss A, Bourke MJ, Williams SJ, et al. Endoscopic mucosal resection and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology 2011; 140: 1909–1918. [DOI] [PubMed] [Google Scholar]
- 18.Ferrara T, Luigiano C, Ghersi S, et al. Efficacy, safety and outcomes of ‘inject and cut’ endoscopic mucosal resection of large sessile and flat colorectal polyps. Digestion 2010; 82: 213–220. [DOI] [PubMed] [Google Scholar]
- 19.Lee TJ, Rees CJ, Nickerson C, et al. Management of complex colonic polyps in the English Bowel Cancer Screening Programme. Br J Surg 2013; 100: 1633–1639. [DOI] [PubMed] [Google Scholar]
- 20.Sidhu M, Tate DJ, Desomer L, et al. The size, morphology, site, and access score predicts critical outcomes of endoscopic mucosal resection in the colon. Endoscopy 2018; 50: 684–692. [DOI] [PubMed] [Google Scholar]
- 21.Bhurwal A, Bartel MJ, Heckman M, et al. Endoscopic mucosal resection: learning curve for large nonpolypoid colorectal neoplasia. Gastrointest Endosc 2016; 84: 959–968. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for Effect of time of day and daily endoscopic workload on outcomes of endoscopic mucosal resection for large sessile colon polyps by Yonatan J Hillman, Bari S Hillman, Divyesh V Sejpal, Calvin Lee, Larry S Miller, Petros C Benias and Arvind J Trindade in United European Gastroenterology Journal