ABSTRACT
Maladaptive patterns of attention to emotional stimuli are a common feature of posttraumatic stress disorder (PTSD), with growing evidence supporting sustained attention to threatening stimuli across trauma samples. However, it remains unclear how different PTSD symptom clusters are associated with attentional bias patterns, particularly in urban civilian settings with high rates of trauma exposure and PTSD. The present study examined associations among these variables in 70 traumatized primarily African American women. PTSD was measured using the Clinician Administered PTSD Scale, and eye tracking was used to measure patterns of attention as participants engaged in an attention bias (dot probe) task to emotional faces; average initial fixation (1 s) and dwell duration (overall time spent looking at emotional face versus neutral face across the 5 s task) were used to assess attention bias patterns toward emotional faces. Women with PTSD showed significantly longer dwell duration toward angry faces than women without PTSD (F = 5.16, p < .05). Bivariate correlation analyses with the PTSD symptom clusters showed a significant association between average initial fixation toward angry faces and higher levels of avoidance symptoms (r = 0.29, p < .05) as well as sustained attention to angry faces and higher levels of re-experiencing symptoms (r = 0.24, p < .05). Using separate linear regression models based on initial significant correlations, we found that PTSD avoidance symptoms were significantly related to average initial fixation toward angry faces (R2∆ = 0.09, p < .05) and PTSD re-experiencing symptoms were significantly related to dwell duration toward angry faces (R2∆ = 0.06, p < .05). These findings contribute to evidence that PTSD is related to both initial vigilance and sustained attention to threat and that certain symptom clusters may either drive or be more impacted by attentional biases, highlighting the benefits of addressing attentional biases within treatment.
KEYWORDS: Attention bias, eye tracking, trauma, PTSD, urban population
HIGHLIGHTS
•Biased attention patterns are related to PTSD symptoms in a civilian urban population of women.• PTSD diagnosis is associated with sustained attention toward threat.• Avoidance symptoms are related to initial biased attention toward angry faces, while re-experiencing symptoms are related to sustained attention toward angry faces.
Abstract
Los patrones desaptativos de atención a estímulos emocionales son una característica común del trastorno de estrés postraumático (TEPT), con evidencias crecientes que respaldan el rol de la atención sostenida hacia estímulos amenazadores a través de muestras de traumas. Sin embargo, aún permanece poco claro cómo diferentes conglomerados de síntomas de TEPT se asocian con los patrones de sesgo atencional, especialmente en entornos civiles urbanos con altas tasas de exposición al trauma y TEPT. El presente estudio examinó las asociaciones entre estas variables en 70 mujeres traumatizadas principalmente afroamericanas. El TEPT se midió utilizando la Escala de TEPT Administrada por el Medico, y el seguimiento ocular se usó para medir los patrones de atención cuando los participantes se involucraron en una tarea de sesgo atencional (sonda de puntos) a las caras emocionales; la fijación inicial promedio (1 segundo) y la duración de permanencia (tiempo total dedicado a mirar la cara emocional en contraste a la cara neutral en la tarea de 5 segundos) se utilizaron para evaluar los patrones de sesgo de atención hacia las caras emocionales. Las mujeres con TEPT mostraron una duración de permanencia de la mirada significativamente más prolongada hacia las caras enojadas que las mujeres sin TEPT (F = 5.16, p <.05). Los análisis de correlación bivariada con los conglomerados de síntomas de TEPT mostraron una asociación significativa entre la fijación inicial promedio hacia las caras enojadas y los niveles más altos de síntomas de evitación (r = 0.29, p <.05), así como la atención sostenida a las caras enojadas y niveles más altos los síntomas de re-experimentación (r = 0.24, p <.05). Usando modelos de regresión lineal separados basados en correlaciones significativas iniciales, encontramos que los síntomas de evitación de TEPT se relacionaron significativamente con la fijación inicial promedio hacia caras de enojo (R2∆=0.09, p<0.05) y los síntomas de re-experimentación de TEPT se relacionaron significativamente con la duración de permanencia hacia caras enojadas (R2∆=0.06, p<0.05). Estos hallazgos contribuyen a la evidencia de que el TEPT está relacionado con la vigilancia inicial y la atención sostenida a la amenaza y que ciertos conglomerados de síntomas pueden impulsar o verse más afectados por los sesgos atencionales, destacando los beneficios de abordar los sesgos atencionales dentro del tratamiento.
PALABRAS CLAVES: Sesgo atencional, seguimiento ocular, trauma, TEPT, población urbana
Abstract
情绪刺激的注意的适应不良模式是创伤后应激障碍(PTSD)的共同特征,越来越多的证据支持创伤样本对威胁刺激的持续注意。然而,目前尚不清楚不同PTSD症状簇与注意偏向模式的关系,特别是在创伤暴露率和PTSD发生率高的城市居民环境中。本研究调查了70名创伤暴露(主要为)非裔美国女性中的这些变量之间的关联。使用《临床医师使用的PTSD量表》测量PTSD,被试对情绪面孔进行注意力偏向(点探测)任务时,使用眼睛跟踪来测量注意模式;平均初始固定(1秒)和停留持续时间(在5秒任务中观察情绪面部相对中性面部所花费的总时间)被用于评估对情绪面孔的注意偏差模式。患有创伤后应激障碍的女性对生气面孔的停留时间显著长于没有创伤后应激障碍的女性(F = 5.16,p <.05)。与创伤后应激障碍症状簇的双变量相关分析显示,对愤怒面孔平均初始固定眼动与较高水平的回避症状(r = 0.29,p <.05)显著相关,并且持续关注愤怒面孔和更高水平的再体验症状(r = 0.24,p <.05)。基于初步显著相关性的单独线性回归模型,我们发现PTSD回避症状与对愤怒面部的平均初始固定显著相关(R2Δ= 0.09,p <0.05)并且PTSD再体验症状与对愤怒面孔眼动持续停留时间显著相关(R2Δ= 0.06,p <0.05)。这些发现有助于证明创伤后应激障碍与初始警惕和对威胁的持续关注有关,并且某些症状簇可能会引起注意偏向或者受到注意偏差的影响更多,这突出了解决治疗中注意偏差的好处。
关键词: 注意偏差, 眼动追踪, 创伤, PTSD, 城市人口
1. Introduction
The long-lasting negative effects of chronic interpersonal trauma exposure on adult mental health outcomes, like posttraumatic stress disorder (PTSD), are well documented (Bailey, Moran, & Pederson, 2007; Boney-McCoy & Finkelhor, 1995; Kendall-Tackett, Williams, & Finkelhor, 1993). PTSD is characterized by four main clusters of symptoms: re-experiencing symptoms, avoidance behaviours, negative cognitions and mood (including emotional numbing/anhedonia symptoms), and hypervigilance (APA, 2013). Thus the variability in symptom presentation and resulting functional impairment across individuals with PTSD is high. It has become increasingly important to delineate broader mechanisms that may be permanently altered as a result of trauma exposure, as clarifying these mechanisms will broaden our understanding of the pathways through which trauma may increase risk for PTSD. One important factor to consider is maladaptive attentional patterns (Fani, Bradley-Davino, Ressler, & McClure-Tone, 2011; Pine et al., 2005).
Evidence suggests that trauma-exposed adults with PTSD demonstrate biases in attention (Bryant & Harvey, 1997; Vasterling & Brailey, 2005). These biased attention patterns may be a result of maladaptive emotional processing that develops following trauma exposure. More precisely, some individuals develop maladaptive conditioned fear expressions (i.e. fear load) that reflect impairment in the extinction of fear (often measured with fear-potentiated startle methodologies, see review by Norrholm and Jovanovic, 2018) and may lead them to perceive benign stimuli (e.g. visual cues that vaguely resemble the original trauma stimulus) as threatening (Fani, Tone, et al., 2012; Foa & Kozak, 1986; Norrholm et al., 2015; Zalta, 2015). This altered fear load may lead them to respond with hypervigilance to their surroundings and help to initiate or maintain other symptoms of PTSD, including intrusive memories and avoidance behaviours (Ehlers & Clark, 2000). The interplay between trauma exposure, PTSD symptoms, and attention bias patterns may help to further illuminate the ways in which attention bias may initiate or maintain PTSD and could aid in efforts to identify valuable treatment targets.
Across PTSD studies of attention bias using behavioural tasks, the results are mixed. The majority of studies examining PTSD and biased attention support attention bias towards threat in adults (Bar-Haim et al., 2007; Bryant & Harvey, 1997; Dalgleish et al., 2003; Elsesser, Sartory, & Tackenberg, 2005; Fani, Tone, et al., 2012; Latack, Moyer, Simon, & Davila, 2017) and children/adolescents (Dalgleish, Moradi, Taghavi, Neshat-Doost, & Yule, 2001). However, there is some evidence that avoidance of threat during attention bias tasks may also relate to PTSD (Sipos, Bar‐Haim, Abend, Adler, & Bliese, 2014) or PTSD symptoms (Bar-Haim et al., 2010) in adults.
Compared to behavioural methods, which rely on motor response to characterize attention patterns, eye tracking offers a more direct way to examine attention bias, permitting examination of both attentional facilitation and sustained attention patterns. Studies in civilian and veteran samples have found evidence that PTSD (or higher levels of PTSD symptoms) is associated with initial and sustained attention for threatening cues (Armstrong, Bilsky, Zhao, & Olatunji, 2013; Kimble, Fleming, Bandy, Kim, & Zambetti, 2010; Thomas, Goegan, Newman, Arndt, & Sears, 2013). A recent meta-analysis including 11 eye tracking studies of PTSD found support for sustained attention to threat among individuals with PTSD compared to those without PTSD (Lazarov et al., 2018).
Despite growing evidence to support sustained attention to threat in PTSD, it remains unclear how attention bias to threat is related to the specific symptom clusters of PTSD. Additionally, to our knowledge there is one population at particularly high risk for chronic trauma exposure and PTSD that is vastly underrepresented in this literature: minority individuals living in low income, inner-city environments, who show PTSD rates of 46% (Gillespie et al., 2009). The high rates of trauma exposure and PTSD in this population make it particularly necessary to examine cognitive mechanisms of risk and resilience for trauma-related psychopathology. Additionally, because females are at greater risk for the development of PTSD (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Olff et al., 2007), we felt it was particularly important to examine attentional bias patterns among women in this population.
The goal of present investigation was to extend attention bias research to African American women living in an urban setting, with a focus on clarifying how PTSD symptoms differentially relate to initial and sustained attention bias using an eye tracking technology approach. In this study, we used an eye tracking paradigm to measure gaze bias to emotional face stimuli (happy, angry, and neutral expressions of Caucasian and African American males and females). We investigated (1) initial visual fixation to emotional stimuli within the first 1000 ms of the trial to identify initial hypervigilance or avoidance of emotional stimuli and (2) dwell duration to emotional stimuli, which enabled us to assess patterns of sustained vigilance or avoidance over the full 5000 ms of the trial. We examined attention bias toward angry versus neutral face patterns across PTSD diagnosis as well as differential associations with PTSD symptom clusters (re-experiencing, avoidance, numbing/anhedonia,1 and hypervigilance). Based on prior research (see Lazarov et al., 2018), we hypothesized that women with PTSD would show greater sustained attention to threat compared with women without PTSD. No a priori hypotheses were made regarding PTSD symptom clusters since all previous studies examined overall symptoms.
2. Methods
2.1. Procedure
Participants were drawn from an ongoing study of risk factors for the development of PTSD in a low socioeconomic status, primarily African American, urban population. Participants were recruited from waiting rooms in the gynaecology and primary care medical (non-psychiatric) clinics at Grady Memorial Hospital, a publicly funded hospital in Atlanta, Georgia. We did not narrow our recruitment to specific selection criteria; people in the waiting rooms were approached at random and informed about the study. To be eligible for participation, subjects had to be at least 18 years old, not actively psychotic, and able to give informed consent. If willing to participate, individuals signed the informed consent approved by the Emory Institutional Review Board and the Research Oversight Committee of Grady Memorial Hospital, and an initial interview was administered with questionnaires regarding trauma history and psychological variables was conducted. Trained research assistants administered this interview (approximately 45–75 minutes depending on trauma history) in the waiting rooms of Grady Memorial Hospital. All participants were compensated for their time. Participants were scheduled for further participation if they were eligible for other ongoing studies being conducted at the time in the Grady Trauma Project (GTP) laboratory. A subset of participants completed the behavioural task with eye tracking methods during follow-up visits at the GTP laboratory located on Grady Hospital campus. Participants included in the present study were recruited for the behavioural task when they came to complete a clinical interview to assess PTSD and other psychiatric symptoms as part of other ongoing research in the laboratory. Only individuals with complete data from the PTSD clinical interview and eye tracking task were included in the present analyses. The task took approximately 15 minutes. No prior studies from this larger project have analysed any eye tracking data presented in the current study.
2.2. Participants
The sample consisted of 70 females, age 20–59 (mean = 40.10, SD = 10.35). The subjects were primarily African American (95.7%) or mixed race (4.3%). The majority of participants were unemployed (68.6%) and 79.4% had a household monthly income of US$1999 or less. Education level of participants was as follows: 17.1% had less than a 12th grade education, 32.9% completed high school, 22.9% completed at least some college or technical school, and 21.4% graduated from college or technical school. All participants in the study met criteria for at least one DSM-IV-TR criterion A traumatic event. The average number of lifetime trauma types experienced by participants across the whole sample was greater than six, demonstrating the magnitude of trauma exposure in this population
2.3. Measures
The Traumatic Events Inventory (TEI) is a 14-item measure of lifetime history of traumatic events and details frequency and type of trauma(s) experienced; consistent with prior research (Gillespie et al., 2009), total level of trauma exposure was measured by a sum score reflecting the total number of different types of trauma (e.g. car accident, sexual assault, and natural disaster) to which a participant had been exposed in their lifetime. For this study, the TEI was used to measure overall trauma load for events witnessed or experienced (i.e. TEI total score). See Table 1 for a list of percentages of types of traumas witnessed or experienced by participants.
Table 1.
Descriptive details for variables of interest.
| Mean (SD); range | |
|---|---|
| TEI Total Score | 6.07 (3.34); 1–16 |
| CAPS Re-experiencing | 4.26 (4.38); 0–17 |
| CAPS Avoidance | 2.88 (2.12); 0–8 |
| CAPS Anhedonia/Numbing | 2.82 (2.63); 0–10 |
| CAPS Hyperarousal | 6.89 (4.07); 0–16 |
| Happy initial fixation difference score (ms) | −0.01 (0.20); −1.06–0.57 |
| Angry initial fixation difference score (ms) | 0.05 (0.29); −0.58–1.33 |
| Happy dwell duration difference score (ms) | 0.05 (0.22); −0.88–0.58 |
| Angry dwell duration difference score (ms) | 0.05 (0.17) −0.35–0.55 |
| % (N) | |
| PTSD Diagnosis (CAPS) | 47.1 (33) |
| Trauma Type | % Exposed |
| Natural Disaster | 32.9 |
| Experienced Serious Accident or Injury | 58.6 |
| Experienced Sudden Life-threatening Illness | 27.5 |
| Witnessed Close Friend/Family Member Murdered | 15.7 |
| Attacked with a Weapon by Significant Other | 27.1 |
| Attacked without a Weapon by Significant Other | 54.3 |
| Attacked with a Weapon by Others (not romantic partner) | 28.6 |
| Attacked without a Weapon by Others (not romantic partner) | 34.3 |
| Witnessed Family Member Attacked with a Weapon | 28.6 |
| Witnessed Non-family Member Attacked with a Weapon | 37.1 |
| Witnessed Family Member Attacked without a Weapon | 45.7 |
| Witnessed Non-family Member Attacked without a Weapon | 35.7 |
| Witnessed Violence between Caregivers | 42.9 |
| Experienced Physical Abuse | 25.7 |
| Experienced Emotional Abuse | 37.7 |
| Experienced Sexual Abuse prior to age 13 | 32.9 |
| Experienced Sexual Abuse (age 13–17; with physical force) | 25.7 |
| Experienced Sexual Assault (age 18+; with physical force) | 24.6 |
N = 70; TEI = Traumatic Events Inventory; CAPS = Clinical Administered PTSD Scale
2.3.1. Clinician-administered PTSD scale (CAPS)
The CAPS is an interviewer-administered psychometrically validated diagnostic instrument measuring current PTSD (Blake et al., 1990). Interrater reliability (IRR) within this sample has been examined previously and showed good IRR for current diagnosis of PTSD (k = 0.83; Powers et al., 2017). The CAPS was used to determine presence/absence of a PTSD diagnosis based on DSM criteria, as well as yielded continuous scores of symptom severity across the PTSD symptom clusters. Both CAPS for DSM-IV (CAPS-IV) and DSM-5 (CAPS-5) were used in the present study due to switching when CAPS-5 was released; 7% (n = 5) received the CAPS for DSM-IV. Based on evidence of the importance of separating avoidance and numbing symptoms (Kashdan, Elhai, & Frueh, 2006) and in order to be able to combine continuous data across CAPS-IV and CAPS-5, we constructed the following clusters: re-experiencing (five symptoms), avoidance (two symptoms), numbing/anhedonia (three symptoms), and hyperarousal (five symptoms).2 In the overall sample, 47% (n = 33) met criteria for PTSD.
2.3.2. Measure of attention bias using eye tracking
The emotional stimuli task was a modified dot probe task (Mogg & Bradley, 1999) which included 80 trials where a pair of face photographs (both of the same actor) was presented for 5000 ms.3 The task stimuli included photographs of African American and Caucasian men and women. After the offset of the face pair, an asterisk was presented in the location that one of the faces had occupied. To help maintain continued participant engagement, participants were asked to determine as quickly as possible, with a forced-choice button press response, whether the asterisk appeared on the left- or right-hand side of the screen. Face pairs included either one face displaying an emotional expression (either threatening or happy) and the other a neutral expression or two neutral faces. The task consisted of 80 trials (32 positive-neutral face pairs, 32 neutral-threat face pairs, and 16 neutral-neutral face pairs) presented in random order. The probe appeared on the left or right side of the screen an equal number of times. During half of the neutral-neutral trials, the probe appeared on the left; during the other half, it appeared on the right.4
2.3.2.1. Eye tracking
All participants placed their head on a chin rest, directly in front of the computer monitor. Pictures were displayed on the screen in front of them. All pictures were black and white. The eye tracking procedure began with a calibration/validation sequence during which participants had to follow a dot presented randomly at nine different locations on the screen with their eyes. The accuracy of the calibration was checked between each trial and the participant was recalibrated if the system noted an error. Once the calibration was completed, the emotional stimuli task began. Line of visual gaze was assessed using a remote optics eye tracking system Model R6 from Applied Science Laboratories (Bedford, MA). Direction of gaze, measured with x and y coordinates, was sampled every 16.7 ms (60 Hz), producing 299 gaze location measurements for each 5000 ms trial. Eye movements that were stable for more than 100 ms within 1° of visual angle were classified as a fixation. An individual dwell was defined as the time during which a contiguous series of 1 or more fixations remains within an Area of Interest (AOI), regardless of how many individual fixations this action comprises. Average initial fixation toward angry versus neutral faces (difference score) within the first 1000 ms of each trial was used as the measure of initial fixation in the present study. Average dwell duration over full 5000 ms of each trial was used as the measures of sustained gaze bias in the present study. Difference scores were calculated for emotional face (happy or angry) compared to neutral face in terms of average dwell duration for each face type per trial (see Table 1 for descriptive statistics). See Figure 1 for an illustration of how visual gaze is tracked.
Figure 1.
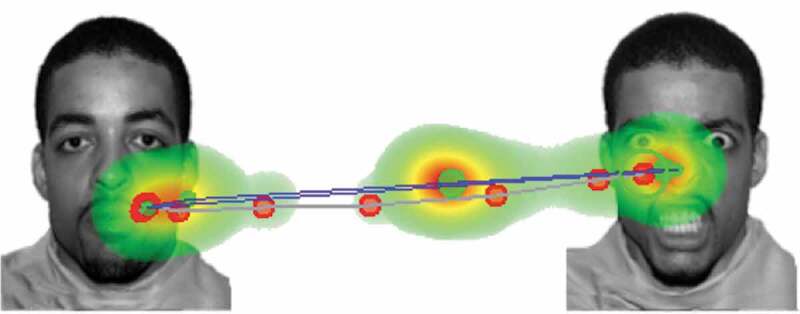
Example of emotional images from dot probe with visual gaze pattern, as captured by eye tracking device, superimposed.
2.4. Data analysis
All statistical analyses were conducted using SPSS Version 24.0 (Armonk, NY: IBM Corp.), with alpha level of 0.05. Descriptive statistics for all variables of interest are presented in Table 1. Analysis of variance (ANOVA) tests were run to examine the association between PTSD diagnosis and (1) initial fixation toward angry faces and (2) dwell duration toward angry faces. Additionally, bivariate correlations between PTSD symptom clusters and attention bias were run to determine what variables may be included in a follow-up regression analyses; p < .05 was used in order to determine inclusion of variables for follow-up analyses.5 Then, based on correlational results, hierarchical linear regression models were conducted to assess the unique variance of attentional bias variables that PTSD symptoms accounted for above and beyond trauma exposure.
3. Results
3.1. PTSD diagnosis
ANOVA results showed that women with PTSD showed significantly greater dwell duration to angry faces than women without PTSD (F = 5.164, p = .026); mean differences across PTSD diagnosis were not significantly different for initial fixation to angry faces (F = 0.41, p = .53). See Table 2 for mean differences across groups for both measures of attention bias. Mean differences across groups for initial fixation and dwell duration difference scores to happy versus neutral emotional stimuli are included in Supplemental Table 2.
Table 2.
Mean differences across initial fixation and dwell duration toward angry faces and PTSD diagnosis based on Analysis of Variance results.
| PTSD- n = 37 |
PTSD+ n = 33 |
|
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Angry initial fixation difference score (ms) | 0.03 (0.24) | 0.07 (0.34) |
| Angry dwell difference score (ms) | 0.01 (0.16) | 0.10 (0.16)* |
*Reflects mean differences significant at p < .05 in between-group analysis
3.2. Correlation and regression results with PTSD symptom clusters
Bivariate correlation analyses showed significant positive correlations between mean initial fixation toward angry faces and avoidance symptoms (r = 0.29, p = .016), as well as mean dwell duration toward angry faces and re-experiencing symptoms (r = 0.24, p = .043). No other symptom clusters were significantly associated with mean initial fixation or mean dwell duration toward angry faces (see Table 3). As shown in Table 4, hierarchical linear regression models showed that PTSD avoidance symptoms significantly predicted average initial fixation to angry faces above and beyond overall trauma exposure (R2∆ = 0.08, p = .019). PTSD re-experiencing symptoms also significantly predicted average dwell duration for angry faces, above and beyond overall trauma exposure (R2∆ = 0.06, p = .044). Total trauma load was not significantly associated with dwell duration toward angry faces in the first step of either model (see Table 4).
Table 3.
Bivariate correlations between trauma load and current PTSD symptom clusters with difference scores for mean initial fixation and dwell duration of viewing angry faces compared to neutral faces.
| Angry Initial Fixation Diff | Angry Dwell Diff | |
|---|---|---|
| TEI Total Score | 0.04 | 0.04 |
| CAPS Re-experiencing | 0.23 | 0.24* |
| CAPS Avoidance | 0.29* | 0.23 |
| CAPS Anhedonia/Numbing | 0.13 | 0.05 |
| CAPS Hyperarousal | 0.22 | 0.12 |
N = 70; *p < .05; TEI = Traumatic Events Inventory; CAPS = Clinician Administered PTSD Scale
Table 4.
Hierarchical linear regression predicting mean initial fixation and dwell duration difference scores for angry faces by trauma load and PTSD symptoms.
| Predicting Attention Bias toward Angry Faces vs Neutral Faces | Stand β | T | R | R2change | Fchange | pchange |
|---|---|---|---|---|---|---|
| Initial Fixation Difference Score | ||||||
| Step 1 | 0.07 | 0.004 | 0.29 | 0.59 | ||
| TEI Total Score | 0.07 | 0.54 | ||||
| Step 2 | 0.29 | 0.08 | 5.83 | 0.019* | ||
| TEI Total Score | −0.03 | −0.23 | ||||
| CAPS Avoidance | 0.30 | 2.42* | ||||
| Dwell Duration Difference Score | ||||||
| Step 1 | 0.04 | 0.002 | 0.13 | 0.71 | ||
| TEI Total Score | 0.29 | 2.49* | ||||
| Step 2 | 0.25 | 0.06 | 4.20 | 0.043* | ||
| TEI Total Score | −0.05 | −0.37 | ||||
| CAPS Re-experiencing | 0.26 | 2.05* |
N = 70; *p < .05; TEI = Traumatic Events Inventory; CAPS = Clinician Administered PTSD Scale
4. Discussion
In the present study, we used eye tracking methods to examine associations among trauma exposure, PTSD symptoms, and indices of attention bias, namely, initial fixation and overall dwell duration to angry versus neutral emotional stimuli. In line with our hypothesis and previous research, we found that PTSD diagnosis was associated with greater sustained attention to threatening emotional stimuli among women in our study. We did not find a mean difference by PTSD diagnosis for average initial fixation to angry versus neutral emotional stimuli. When associations were examined based on individual symptom clusters of PTSD, we found differential associations based on attention bias indices: PTSD avoidance symptom severity was associated with greater initial fixation to angry expressions than neutral expressions and re-experiencing symptom severity was associated with longer dwell duration to angry expressions than neutral expressions.
Previous studies have shown a fairly consistent pattern of sustained attention to threatening stimuli in individuals with PTSD (see Lazarov et al., 2018, for a meta-analytic review); this includes our own research indicating attention biases toward threat-related stimuli (angry faces; Fani, Tone, et al., 2012). In this sample of chronically traumatized African American women utilizing services in an urban hospital, we found further support for that pattern, observing significantly greater dwell duration toward angry emotional stimuli compared to neutral stimuli. However, it has previously been unclear whether certain symptom clusters may be particularly related to sustained attention bias. In this study, PTSD re-experiencing symptom cluster severity was related to an overall attention bias toward negative emotional stimuli, such that over the full course of the five second trial, individuals with higher re-experiencing symptoms were spending more time looking at angry faces regardless of how many times they may have fixated on either angry or neutral faces. Interestingly, higher levels of PTSD avoidance symptoms were associated with greater average initial fixation to angry emotional stimuli versus neutral emotional stimuli.
These findings were somewhat surprising considering the expected role of hypervigilance in maintaining attention toward threat and its relation to heightened activation of the amygdala to emotional stimuli (Stevens et al., 2013). However, previous research by our lab in this population has shown evidence that attention bias toward threat is related to exaggerated fear expression (Fani, Jovanovic, et al., 2012) and, in turn, re-experiencing PTSD symptoms in particular are associated with exaggerated fear response (Norrholm et al., 2015, 2011). Additionally, re-experiencing symptoms are associated with hippocampal function in traumatized women and appear to play a role in memory encoding activation in the hippocampus and amygdala (Stevens et al., 2018), and therefore may be critical in maintaining attention to threat. Re-experiencing symptoms (in addition to hyperarousal symptoms) may also represent particular difficulty with emotional undermodulation, or failure of prefrontal inhibition of limbic regions in the face of trauma reminders (or negative emotional cues) (Lanius et al., 2010). Importantly, research by Fani, Jovanovic, et al. (2012) in African American women with high trauma exposure showed that women with PTSD showed increased activation of the dorsolateral prefrontal cortex (dlPFC) in relation to threat cues, suggesting potential efforts by these women to overcompensate for emotional disruption caused by threatening facial expressions and disturbing trauma memories that might be evoked by the emotional stimuli. It is possible that the greater severity of intrusive symptoms might feed the vigilant attention bias patterns that we observed. It is also possible that difficulty disengaging with threatening stimuli feeds additional re-experiencing symptoms (or even greater awareness of their presence). Cross-sectional data makes it impossible for us to determine the direction of the relationship in the observed patterns.
The relationship between avoidance and initial attention toward threatening stimuli was unexpected for two reasons. First, intuitively it seems plausible that avoidance behaviours might carry over into attentional patterns and that other symptoms may drive the attention bias effect. Second, some previous research has found evidence of attention bias away from threatening stimuli among individuals with PTSD (Sipos et al., 2014). It is possible that an inability to disengage initial attention from threatening stimuli leads to heightened emotional response and facilitates avoidance behaviours, making it difficult for these individuals to engage with the world around them. This behavioural avoidance, in turn, could influence their ability to work, to engage socially, and to maintain positive relationships (Pineles et al., 2007). Distress associated with this attention bias toward threat and trauma reminders may contribute to the long-term development of the full range of avoidance behaviours seen in PTSD, such as thought suppression, substance use, and avoidance of trauma cues in the environment. Specifically, people may engage in such behaviours in an effort to reduce this bias-linked distress, and those avoidance behaviours may then contribute to the maintenance of the disorder limiting normative habituation to trauma reminders (Feeny, Zoellner, Fitzgibbons, & Foa, 2000; Shipherd and Beck, 2005). Alternatively, recent evidence suggests that patterns of attentional avoidance of threat prior to trauma exposure may lead to greater risk for PTSD (Beevers et al., 2011). It is thus possible that pre-trauma attentional avoidance fuels avoidance behaviour which then leads to changes in an individual’s attention bias patterns (increased hypervigilance) with the development of PTSD. Because our data are cross-sectional, it is unclear whether the attention bias or the avoidance behaviour came first. However, it would be useful to assess for changes in attention bias during the course of trauma-focused treatment to see if reductions in attention bias toward threat improve functional outcomes such as social engagement and relationship satisfaction or vice versa.
Several study limitations must be noted, some of which are relevant to our population. First, as mentioned above, given the cross-sectional nature of this study and the use of retrospective reports, we cannot make assertions about causality or time of onset for PTSD symptoms and attention bias. Prospective, longitudinal studies are required to examine the specific roles that trauma and PTSD symptoms may play in the development of attentional difficulties. Our sample size was also relatively small to detect significant effects across symptoms and replication of these findings in a larger sample is warranted. We did not adjust for multiple testing in our analyses and therefore it is possible that some of our findings are spurious. Additionally, because our measure of dwell duration (overall 5000 ms of trial) included data used for our other attention bias measure (initial fixation in first 1000 ms), these measures of attention bias are not fully orthogonal; however, a dwell reflects the overall time spent on an AOI (as long as at least one fixation occurs) regardless of how many different fixations, while the initial fixation measure reflects the average number of fixations on the AOI within the first second of the trial; thus we feel that the measures are providing us with distinct information. Fearful faces were not included in the stimulus set of this task and would be beneficial to include in future studies to evaluate attention bias responses to potential indirect threats as well as direct threats. Due to the specificity of our sample, it is possible that the findings observed here may be most generalizable to populations with similarly high rates of trauma and comparable demographic characteristics. Finally, it is also critical to acknowledge that this was an all-female sample and therefore it is possible that different outcomes would be observed in men. In fact, there is some evidence that men and women recognize and process emotional stimuli differently (Collignon et al., 2010; McRae, Ochsner, Mauss, Gabrieli, & Gross, 2008); however, little remains known about the nature of sex differences in attention bias patterns for individuals with PTSD.
Overall, we found evidence that women with PTSD showed greater sustained attention to threatening (angry faces) emotional stimuli compared with women without PTSD, suggesting a hypervigilance toward threatening stimuli. Importantly, we examined differences across symptom clusters and found differential associations suggesting that certain symptoms may be driving the association found between PTSD and attention bias indices, namely avoidance symptoms for initial fixation and re-experiencing symptoms for dwell duration toward angry faces. Abnormal patterns of attention to emotional face cues, regardless of type and direction of bias, may be a biological marker of risk for trauma-related sequelae. These data indicate the need for continued research using both behavioural and physiological methods on the role of attentional biases in PTSD, as such work may lead to a better understanding of the treatment implications of attention bias in relation to certain PTSD symptom clusters.
Supplementary Material
Acknowledgments
We would like to thank Allen W. Graham, Angelo Brown, Rebecca Hinrichs, and the entire Grady Trauma Project team for this assistance in data collection and management for this project.
Notes
Some of the subjects in this study were administered DSM-IV PTSD measures prior to the release of DSM-5 materials and updated criteria and therefore negative cognitions (PTSD symptoms added in DSM-5) were not included in analyses of PTSD symptom clusters.
CAPS-IV frequency and intensity scores were combined and divided by 2 to match the new single severity score for CAPS-5.
5000 ms was chosen based on prior eye tracking studies conducted with similar stimuli and behavioural tasks.
Reaction time data with ≥ 75% accuracy was available for 77% of participants (n = 54), with descriptive details included in Supplemental Table 1. Eye tracking outcome variables did not differ significantly between participants with and without reaction time data (p > .05). Reasons for missing or inaccurate reaction time data included overwritten data due to participants with duplicate SIDs completing the task (i.e. the woman’s child returned and participated in eye tracking with same SID which resulted in overriding of reaction time data; n = 5) and participants mistakenly using the number key pad to respond instead of the numbers at the top of the keyboard which resulted in no recorded reaction time data but did not affect eye tracking data (n = 11).
Correlations between age and attention bias outcome variable was also assessed but were not significant and therefore age was not included in remaining analysis.
Disclosure statement
No potential conflict of interest was reported by the authors.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additionally, the contents of this report do not represent the views of the Department of Veterans Affairs or the USA Government.
Supplemental data
Supplemental data for this article can be accessed here.
References
- American Psychiatric Association (2013). DSM 5. Washington D.C.: Author. [Google Scholar]
- Armstrong T., Bilsky S. A., Zhao M., & Olatunji B. (2013). Dwelling on potential threat cues: An eye movement marker for combat-related PTSD. Depression and Anxiety, 30(5), 497–9. [DOI] [PubMed] [Google Scholar]
- Bailey H. N., Moran G., & Pederson D. R. (2007). Childhood maltreatment, complex trauma symptoms, and unresolved attachment in an at-risk sample of adolescent mothers. Attachment & Human Development, 9(2), 139–161. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y., Holoshitz Y., Eldar S., Frenkel T. I., Muller D., Charney D. S., … Wald I. (2010). Life-threatening danger and suppression of attention bias to threat. American Journal of Psychiatry, 167(6), 694–698. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y., Lamy D., Pergamin L., Bakermans-Kranenburg M. J., & Van Ijzendoorn M. H. (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin, 133(1), 1. [DOI] [PubMed] [Google Scholar]
- Beevers C. G., Marti C. N., Lee H. J., Stote D. L., Ferrell R. E., Hariri A. R., & Telch M. J. (2011). Associations between serotonin transporter gene promoter region (5-HTTLPR) polymorphism and gaze bias for emotional information. Journal of Abnormal Psychology, 120(1), 187. [DOI] [PubMed] [Google Scholar]
- Blake D. D., Weathers F., Nagy L. M., Kaloupek D. G., Klauminzer G., Charney D. S, & Keane T. M (1990). A clinician rating scale for assessing current and lifetime PTSD: The Caps-1. The Behavior Therapist, 13, 187–188. [Google Scholar]
- Boney-McCoy S., & Finkelhor D. (1995). Prior victimization: A risk factor for child sexual abuse and for PTSD-related symptomatology among sexually abused youth. Child Abuse & Neglect, 19(12), 1401–1421. [DOI] [PubMed] [Google Scholar]
- Bryant R. A., & Harvey A. G. (1997). Attentional bias in posttraumatic stress disorder. Journal of Traumatic Stress, 10(4), 635–644. [DOI] [PubMed] [Google Scholar]
- Collignon O., Girard S., Gosselin F., Saint-Amour D., Lepore F., & Lassonde M. (2010). Women process multisensory emotion expressions more efficiently than men. Neuropsychologia, 48(1), 220–225. [DOI] [PubMed] [Google Scholar]
- Dalgleish T., Moradi A. R., Taghavi M. R., Neshat-Doost H. T., & Yule W. (2001). An experimental investigation of hypervigilance for threat in children and adolescents with post-traumatic stress disorder. Psychological Medicine, 31(3), 541–547. [DOI] [PubMed] [Google Scholar]
- Dalgleish T., Taghavi R., Neshat-Doost H., Moradi A., Canterbury R., & Yule W. (2003). Patterns of processing bias for emotional information across clinical disorders: A comparison of attention, memory, and prospective cognition in children and adolescents with depression, generalized anxiety, and posttraumatic stress disorder. Journal of Clinical Child and Adolescent Psychology, 32(1), 10–21. [DOI] [PubMed] [Google Scholar]
- Ehlers A., & Clark D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. [DOI] [PubMed] [Google Scholar]
- Elsesser K., Sartory G., & Tackenberg A. (2005). Initial symptoms and reactions to trauma‐related stimuli and the development of posttraumatic stress disorder. Depression and Anxiety, 21(2), 61–70. [DOI] [PubMed] [Google Scholar]
- Fani N., Bradley-Davino B., Ressler K. J., & McClure-Tone E. B. (2011). Attention bias in adult survivors of childhood maltreatment with and without posttraumatic stress disorder. Cognitive Therapy and Research, 35(1), 57–67. [Google Scholar]
- Fani N., Jovanovic T., Ely T. D., Bradley B., Gutman D., Tone E. B., & Ressler K. J. (2012). Neural correlates of attention bias to threat in post-traumatic stress disorder. Biological Psychology, 90(2), 134–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fani N., Tone E. B., Phifer J., Norrholm S. D., Bradley B., Ressler K. J., … Jovanovic T. (2012). Attention bias toward threat is associated with exaggerated fear expression and impaired extinction in PTSD. Psychological Medicine, 42(03), 533–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeny N. C., Zoellner L. A., Fitzgibbons L. A., & Foa E. B. (2000). Exploring the roles of emotional numbing, depression, and dissociation in PTSD. Journal of Traumatic Stress, 13(3), 489–498. [DOI] [PubMed] [Google Scholar]
- Foa E. B., & Kozak M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20. [PubMed] [Google Scholar]
- Gillespie C., Bradley B., Mercer K., Smith A., Conneely K., Gapen M., & Ressler K. (2009). Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry, 31, 505–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan T. B., Elhai J. D., & Frueh B. C. (2006). Anhedonia and emotional numbing in combat veterans with PTSD. Behaviour Research and Therapy, 44(3), 457–467. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett K. A., Williams L. M., & Finkelhor D. (1993). Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychological Bulletin, 113(1), 164. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Sonnega A., Bromet E., Hughes M., & Nelson C. B. (1995). Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry, 52(12), 1048–1060. [DOI] [PubMed] [Google Scholar]
- Kimble M. O., Fleming K., Bandy C., Kim J., & Zambetti A. (2010). Eye tracking and visual attention to threating stimuli in veterans of the Iraq war. Journal of Anxiety Disorders, 24(3), 293–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanius R. A., Vermetten E., Loewenstein R. J., Brand B., Schmahl C., Bremner J. D., & Spiegel D. (2010). Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. American Journal of Psychiatry, 167(6), 640–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latack J. A., Moyer A., Simon V. A., & Davila J. (2017). Attentional bias for sexual threat among sexual victimization survivors: A meta-analytic review. Trauma. Violence, & Abuse, 18(2), 172–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarov A., Suarez-Jimenez, B., Tamman, A., Falzon, L., Zhu, X., Edmondson, D. E., & Neria, Y. (2018). Attention to threat in posttraumatic stress disorder as indexed by eye-tracking indices: A systematic review. Psychological Medicine, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRae K., Ochsner K. N., Mauss I. B., Gabrieli J. J. D., & Gross J. J. (2008). Gender differences in emotion regulation: An fMRI study of cognitive reappraisal. Group Processes & Intergroup Relations, 11(2), 143–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogg K., & Bradley B. P. (1999). Some methodological issues in assessing attentional biases for threatening faces in anxiety: A replication study using a modified version of the probe detection task. Behaviour Research and Therapy, 37(6), 595–604. [DOI] [PubMed] [Google Scholar]
- Norrholm S. D., Glover E. M., Stevens J. S., Fani N., Galatzer-Levy I. R., Bradley B., … Jovanovic T. (2015). Fear load: The psychophysiological over-expression of fear as an intermediate phenotype associated with trauma reactions. International Journal of Psychophysiology, 98(2), 270–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norrholm S. D., & Jovanovic T. (2018). Fear processing, psychophysiology, and PTSD. Harvard Review of Psychiatry, 26(3), 129–141. [DOI] [PubMed] [Google Scholar]
- Norrholm S. D., Jovanovic T., Olin I. W., Sands L. A., Bradley B., & Ressler K. J. (2011). Fear extinction in traumatized civilians with posttraumatic stress disorder: Relation to symptom severity. Biological Psychiatry, 69(6), 556–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M., Langeland W., Draijer N., & Gersons B. P (2007). Gender differences in posttraumatic stress disorder. Psychological Bulletin, 133(2), 183. [DOI] [PubMed] [Google Scholar]
- Pine D. S., Mogg K., Bradley B. P., Montgomery L., Monk C. S., McClure E., … Kaufman J. (2005). Attention bias to threat in maltreated children: Implications for vulnerability to stress-related psychopathology. American Journal of Psychiatry, 162(2), 291–296. [DOI] [PubMed] [Google Scholar]
- Pineles S. L., Shipherd J. C., Welch L. P., & Yovel I (2007). The role of attentional biases in PTSD: Is it interference or facilitation?. Behaviour Research and Therapy, 45(8), 1903-1913. [DOI] [PubMed] [Google Scholar]
- Powers A., Fani N., Carter S., Cross D., Cloitre M., & Bradley B (2017). Differential predictors of DSM-5 PTSD and ICD-11 complex PTSD among African American women. European Journal of Psychotraumatology, 8(1), 1338914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shipherd J. C., & Beck J. G (2005). The role of thought suppression in posttraumatic stress disorder. Behavior Therapy, 36(3), 277–287. [Google Scholar]
- Sipos M. L., Bar‐Haim Y., Abend R., Adler A. B., & Bliese P. D. (2014). Postdeployment threat‐related attention bias interacts with combat exposure to account for PTSD and anxiety symptoms in soldiers. Depression and Anxiety, 31(2), 124–129. [DOI] [PubMed] [Google Scholar]
- Stevens J. S., Jovanovic T., Fani N., Ely T. D., Glover E. M., Bradley B., & Ressler K. J. (2013). Disrupted amygdala-prefrontal functional connectivity in civilian women with posttraumatic stress disorder. Journal of Psychiatric Research, 47(10), 1469–1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens J. S., Reddy R., Kim Y. J., van Rooij S. J., Ely T. D., Hamann S., … Jovanovic T. (2018). Episodic memory after trauma exposure: Medial temporal lobe function is positively related to re-experiencing and inversely related to negative affect symptoms. NeuroImage: Clinical, 17, 650–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas C. L., Goegan L. D., Newman K. R., Arndt J. E., & Sears C. R. (2013). Attention to threat images in individuals with clinical and subthreshold symptoms of post-traumatic stress disorder. Journal of Anxiety Disorders, 27(5), 447–455. [DOI] [PubMed] [Google Scholar]
- Vasterling J. J., & Brailey K. (2005). Neuropsychological findings in adults with PTSD. In J. J. Vasterling & C. R. Brewin (Eds.), Neuropsychology of PTSD: Biological, Cognitive, and Clinical Perspectives (pp. 178–207). New York, NY: Guilford Press. [Google Scholar]
- Zalta A. K. (2015). Psychological mechanisms of effective cognitive–behavioral treatments for PTSD. Current Psychiatry Reports, 17(4), 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


