Abstract
Background
Yoga seems to exert its effect against arterial hypertension mainly through the associated breathing and meditation techniques, and less so through yoga postures. The goal of this trial was to compare the blood pressure–lowering effect of yoga interventions with and without yoga postures in patients with arterial hypertension.
Methods
75 patients taking medications for arterial hypertension (72% women, mean age 58.7 ± 9.5 years) were randomized into three groups: a yoga intervention group with yoga postures (25 patients, of whom 5 dropped out of the trial before its end), a yoga intervention group without yoga postures (25 patients, 3 dropouts), and a wait list control group (25 patients, one dropout). The interventions consisted of 90 minutes of yoga practice per week for twelve weeks. The data collectors, who were blinded to the intervention received, assessed the primary outcome measures “systolic 24-hour blood pressure” and “diastolic 24-hour blood pressure” before and after the intervention. In this report, we also present the findings on secondary outcome measures, including follow-up data.
Results
After the intervention, the systolic 24-hour blood pressure in the yoga intervention group without yoga postures was significantly lower than in the control group (group difference [?]= -3.8 mmHg; [95% confidence interval (CI): (-0.3; -7.4) p = 0.035]); it was also significantly lower than in the yoga intervention group with yoga postures (? = -3.2 mmHg; 95% CI: [-6.3; -0.8]; p = 0.045). Diastolic blood pressures did not differ significantly across groups. No serious adverse events were encountered in the course of the trial.
Conclusion
In accordance with the findings of earlier studies, we found that only yoga without yoga postures induced a short-term lowering of ambulatory systolic blood pressure. Yoga is safe and effective in patients taking medications for arterial hypertension and thus can be recommended as an additional treatment option for persons in this category.
The average blood pressure of the German population is decreasing, and a growing proportion of those with hypertension are receiving treatment. Nevertheless, arterial hypertension remains a serious health problem (1). Across the world, 9.4 million deaths each year are caused by excessively high blood pressure. The World Health Organization has pinpointed hypertension as one of the principal causes of premature morbidity and mortality in both developed and developing countries (2).
International medical guidelines recommend lifestyle changes for patients with arterial hypertension, e.g., physical activity and stress management (3). Yoga can comprise such a lifestyle-modifying intervention (4, 5). In western societies yoga is generally associated with specific body postures as well as breathing and/or meditation techniques (4, 6); various schools have developed with differing degrees of emphasis on the physical and mental aspects of yoga (6).
Three fourths of German residents who practice yoga state that they do so primarily for health reasons (7), and clinical studies have shown that the positive effects include a beneficial influence on physical and mental risk factors for hypertension (8, 9). However, no studies have yet been carried out in this country to ascertain the effect of yoga on hypertension, and the German guidelines do not take account of the existing evidence from other countries regarding yoga and related interventions (10). For example, a recent meta-analysis of studies on arterial hypertension and prehypertension performed in different countries (11) showed that yoga achieved significant reductions in systolic and diastolic blood pressure. In subgroup analyses, however, these effects were confirmed only for arterial hypertension. In studies that included both prehypertensive and hypertensive patients, the effects did not attain significance (mean difference: 0.9 mmHg systolic and 0.1 mmHg diastolic). Moreover, effects were demonstrated in studies that permitted individual antihypertensive co-medication, but not in those that excluded it (11). Finally, yoga was effective only in studies that included breathing and/or meditation techniques but no yoga postures. Studies that included yoga postures (alone or accompanied by breathing and meditation techniques) showed no significant effects (11). However, we are not aware of any studies in which the blood pressure–lowering effects of different yoga styles were compared directly. We therefore set out to investigate the efficacy of yoga interventions with and without yoga postures—as an accompaniment to antihypertensive medication—in lowering the 24-h blood pressure of patients with arterial hypertension. Our hypothesis was that the systolic and diastolic blood pressure would be lower following an intervention without yoga postures than in the absence of any specific intervention or after an intervention with yoga postures.
Methods
Study design
The study was carried out as a three-armed, single-center, randomized controlled trial between May 2016 and April 2017. Data acquisition ensued in blinded fashion. Study conduct adhered to the tenets of the Helsinki Declaration (12), and the report was written in conformance with the CONSORT 2010 Statement (13). Before the commencement of patient recruitment, approval was obtained from the ethics committee of the University of Duisburg–Essen (project number: 15–6726-BO) and the study was registered at ClinicalTrials.gov (registration number: NCT02727140).
Participants were recruited by means of appeals in the local press and via the e-mail distribution lists of local companies. Patients who came forward and fulfilled the inclusion criteria were recruited. They received detailed written and verbal information about the study before signing a consent form to indicate their agreement to participate.
Inclusion criteria
To be included in the study, patients had to be at least 18 years old with primary arterial hypertension (>140 mmHg systolic and/or >90 mm Hg diastolic blood pressure). Moreover, they had to be receiving antihypertensive medication from their primary care physician or specialist at the time of investigation. Furthermore, they had to agree to the following conditions:
No alteration of their antihypertensive medication in the next 7 months
Participation in at least 10 of the 12 yoga sessions in the study program
Additional unsupervised yoga sessions at home.
The reasons for exclusion included the following diseases and circumstances:
Secondary hypertension
Severe psychiatric comorbidities (major depression, dependency disorders, or psychosis)
Coronary heart disease, myocardial infarction, pulmonary embolism, or stroke in the previous 3 months
Heart failure of NYHA stage = I
Peripheral arterial occlusive disease of stage = 1
Renal failure of stage >2 with glomerular filtration rate (GFR) <60 mL/min/1.73 m²
Participation in any other clinical studies at the time of commencement of our trial or planned participation in such studies in the next 28 weeks
Pregnancy or breastfeeding.
Randomization
The patients were stratified by sex and divided by block randomization with randomly varying block sizes into the three following groups (ratio 1 : 1 : 1):
An intervention with yoga postures
An intervention without yoga postures
A wait list control group.
A biometrician who was not involved in patient recruitment or data acquisition used Random Allocation Software (14) to generate a password-protected randomization list to which only he had access. On the basis of this randomization list, opaque envelopes containing the study group allocation were numbered consecutively and sealed. Once a patient had signed the consent form and baseline data acquisition had been concluded, the study physician opened the envelope with the lowest remaining serial number and the patient was allocated to a group accordingly. The Cochrane Handbook for Systematic Reviews of Interventions describes this as a randomization method with a low risk of bias (15). At the end of the study, the biometrician checked the group allocations and found that all patients had been allocated correctly and according to the randomization list.
Interventions
Yoga
The two interventions were carried out by the same two yoga instructors. Each intervention comprised a 90-min session once each week for 12 weeks. In the intervention that included yoga postures, each session consisted of 45 min yoga postures and 45 min breathing, meditation, and relaxation techniques as well as short presentations and question-and-answer rounds. The yoga intervention without yoga postures consisted of only breathing, meditation, and relaxation techniques, short presentations, and question-and-answer rounds (eSupplement).
The study participants were encouraged to practice yoga and meditation every day at home, but no minimum duration was recommended. The exercises to be performed at home were explained in detail in the yoga sessions. Furthermore, the patients were given audio recordings of the yoga sessions and training manuals to support their unsupervised exercises. During the 12-week intervention period the participants noted in a diary how many minutes they spent on their exercises each day. At the end of the study (week 28), the patients were asked to state the average weekly duration of their exercises during the follow-up period.
Control group
The study participants allocated to the control group were put on a waiting list. They did not take part in any yoga interventions in the first 12 weeks of the study and were asked not to begin any yoga exercises or other new physical activities during this time. At the end of the 28th week of the study, the members of the control group were offered the opportunity to participate in an intervention corresponding to either of the other two study groups.
Outcome measures
The person who acquired the data was not involved in patient recruitment, group allocation, or the interventions and was blinded to group allocation for the whole duration of the study. Systolic and diastolic 24-h blood pressure were defined as primary outcome measures and were determined using an internationally accepted digital blood pressure monitor (Mobil-O-Graph PWA, I.E.M., Stolberg, Germany) (16). The systolic and diastolic blood pressure at week 28 were documented as secondary outcome measures. The first measurement, at week 1, took place within the week immediately preceding the beginning of the intervention and the second measurement, at week 12, was performed in the week after the end of the intervention. The blood pressure measurement started at the same time of day at all three documentation points. Incorrect measurements were automatically deleted by means of standardized algorithms in the software of the blood pressure monitor. The secondary outcome measures are described in full in the eSupplement.
All adverse events that occurred during the study period were recorded and classified according to the criteria of the U.S. Food and Drug Administration (17). Any participant who experienced an adverse event was asked to consult the study physician so that he/she could assess the severity of the event and take any necessary steps. At weeks 12 and 28 the participants were asked open questions to document any previously unmentioned adverse events. The patients were requested to report all adverse events that occurred during the study period, whether or not they had any possible connection with the study intervention.
Sample size calculation and statistical analysis
The necessary sample size was calculated a priori based on a meta-analysis according to which the systolic blood pressure was 14.13 mmHg lower following yoga interventions, corresponding to an effect size of d = 1.35 (11). On the basis of this effect, 17 patients per study group would be needed for a t-test with a two-sided significance level of a = 0.05. This would enable detection of a corresponding group difference with 80% power. To rule out the loss of power that would result from a drop-out rate of up to 30%, 75 patients (25 per group) were included in the study.
The outcome criteria were evaluated on the basis of the intention-to-treat principle: all randomized patients were included in analysis, regardless of whether the data were complete or whether the study protocol was followed correctly. Missing values, i.e., variables for which there were no data for a given patient at a particular measurement time, were multiply imputed by means of the Markov chain Monte Carlo procedure (18, 19). This resulted in a total of 50 complete data sets that each contained full data for all 75 patients and were combined for purposes of analysis.
All linear outcome measures (blood pressure, heart rate, questionnaire data) were evaluated by means of univariate analyses of covariance (ANCOVA). The outcome measure (dependent variable) was modeled as function of the following parameters:
Group allocation (independent variable)
Expectation of effect (covariate)
The respective baseline value (covariate).
This enabled determination of the overall effect estimates, the 95% confidence interval, and the p value. ANCOVA are recommended for evaluation of clinical studies because they control for possible baseline differences and ascertain group differences for all group comparisons and all measurement times. Moreover, they possess greater power than other statistical methods (20).
All analyses were carried out using Statistical Package for Social Sciences software (IBM SPSS Statistics for Windows, Version 22.0, Armonk, NY, USA: IBM Group). A p value <0.05 was interpreted as showing a significant difference.
Results
Patients
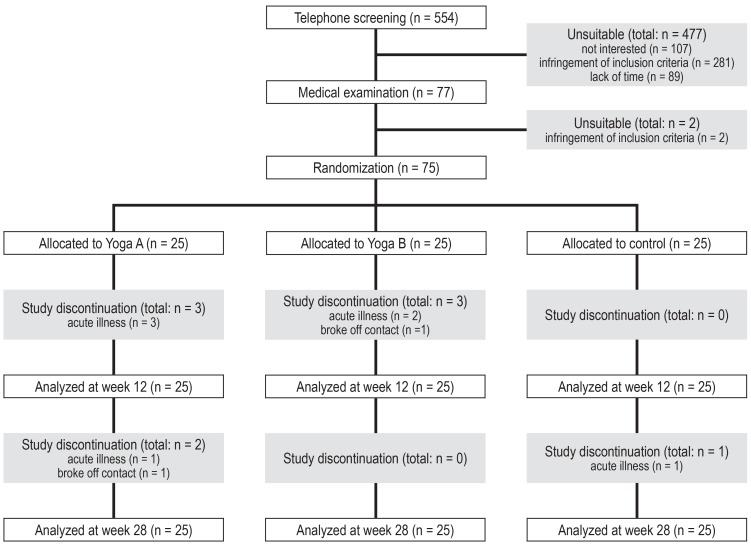
Seventy-five patients fulfilled all the inclusion criteria and were included in the study after providing written informed consent. They were assigned randomly to the yoga group with yoga postures (n = 25), the yoga group without yoga postures (n = 25), or the control group (n = 25). Five members of the group with yoga postures (20.0%), three of the group without yoga postures (12.0%), and one patient in the control group (4.0%) did not complete the study program (Figure 1; p = 0.22). Therefore, missing values were multiply imputed for six participants at week 12 and nine patients at week 28. At each of these time points missing blood pressure values had to be imputed for three further patients who felt uncomfortable with the measuring device and broke off the measurement early. The patients’ characteristics are shown in Table 1.
Figure 1.
Flow chart of study participation: Yoga A = yoga with yoga postures, Yoga B = yoga without yoga postures
eTable 1. Effects on blood pressure and heart rate in the yoga group with yoga postures (Yoga A), the yoga group without yoga postures (Yoga B), and the control group.
| Outcome measure | Group | Measurement time |
Group difference [95% CI] compared with control group (week 12) |
Group difference [95% CI] compared with Yoga B (week 12) |
Group difference [95% CI] compared with control group (week 28) |
Group difference [95% CI] compared with Yoga B (week 28) |
||
| Week 1 | Week 12 | Week 28 | ||||||
| 24-h SBP | Yoga A | 135.4 ± 11.6 | 136.9 ± 10.6 | 131.3 ± 8.4 | 0.2 [−4.2; 4.6]; p = 0.927 | 3.2 [0.8; 6.3]; p = 0.045 | −5.3 [−9.8; −0.8]; p = 0.022 | −4.6 [−9.0; −0.3]; p = 0.037 |
| Yoga B | 131.7 ± 11.3 | 130.9 ± 9.2 | 133.3 ± 11.9 | −3.8 [−7.4; −0.3]; p = 0.035 | – | −1.3 [−6.3; 3.7]; p = 0.602 | – | |
| Control | 133.3 ± 9.8 | 135.0 ± 8.0 | 134.81 ± 9.3 | – | – | – | – | |
| 24-h DBP | Yoga A | 82.5 ± 10.3 | 83.1 ± 10.3 | 80.9 ± 7.3 | −0.4 [−3.3; 2.6]; p = 0.081 | 1.7 [−0.6; 4.1]; p = 0.144 | −2.5 [−5.2; 0.2]; p = 0.065 | −1.2 [−3.3; 0.9]; p = 0.247 |
| Yoga B | 81.1 ± 10.9 | 80.0 ± 10.3 | 81.0 ± 9.1 | −2.0 [−4.3; 0.4]; p = 0.093 | – | −1.4 [−4.2; 1.3]; p = 0.295 | – | |
| Control | 81.1 ± 9.1 | 81.8 ± 8.1 | 81.9 ± 8.5 | – | – | – | – | |
| 24-h HR | Yoga A | 73.0 ± 12.4 | 74.0 ± 11.9 | 70.3 ± 11.4 | 1.0 [−2.1; 4.2]; p = 0.522 | 1.5 [−1.0; 3.9]; p = 0.242 | −3.0 [−7.2; 1.1]; p = 0.143 | −2.3 [−5.6; 1.1]; p = 0.184 |
| Yoga B | 73.5 ± 10.1 | 73.1 ± 8.1 | 73.3 ± 7.7 | 0.1 [−2.5; 2.6]; p = 0.950 | – | 0.3 [−3.2; 3.8]; p = 0.843 | – | |
| Control | 70.8 ± 7.6 | 70.4 ± 7.2 | 71.6 ± 7.4 | – | – | – | – | |
| Diurnal SBP | Yoga A | 137.1 ± 11.5 | 138.4 ± 10.0 | 133.3 ± 8.2 | −0.1 [−4.7; 4.4]; p = 0.943 | 3.3 [0.1; 6.5]; p = 0.042 | −5.6 [−10.4; −0.8]; p = 0.023 | −4.9 [−9.3; −0.5]; p = 0.030 |
| Yoga B | 133.4 ± 11.7 | 132.6 ± 9.0 | 135.5 ± 11.9 | −3.8 [−7.6; −0.1]; p = 0.045 | – | −1.1 [−6.3; 4.1]; p = 0.669 | – | |
| Control | 135.5 ± 9.3 | 137.2 ± 8.8 | 137.1 ± 9.5 | – | – | – | – | |
| Diurnal DBP | Yoga A | 84.2 ± 10.5 | 84.6 ± 9.8 | 82.4 ± 7.1 | −0.5 [−3.7; 2.7]; p = 0.751 | 1.6 [−0.7; 4.0]; p = 0.173 | −2.7 [−5.5; 0.2]; p = 0.065 | −1.6 [−3.7; 0.6]; p = 0.158 |
| Yoga B | 82.5 ± 11.3 | 81.3 ± 10.1 | 82.6 ± 9.2 | −2.1 [−4.5; 0.3]; p = 0.090 | – | −1.2 [−4.1; 1.8]; p = 0.429 | – | |
| Control | 82.7 ± 9.2 | 83.5 ± 8.7 | 83.4 ± 8.7 | – | – | – | – | |
| Diurnal HR | Yoga A | 74.2 ± 12.9 | 75.3 ± 12.6 | 71.3 ± 11.8 | 1.0 [−2.4; 4.5]; p = 0.544 | 1.9 [−0.6; 4.5]; p = 0.140 | −3.2 [−7.6; 1.1]; p = 0.144 | −2.3 [−5.9; 1.3]; p = 0.208 |
| Yoga B | 75.0 ± 10.1 | 74.1 ± 8.3 | 74.5 ± 8.0 | 0.0 [−2.6; 2.7]; p = 0.972 | – | 0.2 [−4.0; 3.5]; p = 0.894 | – | |
| Control | 72.2 ± 7.9 | 71.6 ± 7.4 | 72.9 ± 7.6 | – | – | – | – | |
| Nocturnal SBP | Yoga A | 122.4 ± 16.0 | 124.0 ± 15.2 | 120.8 ± 13.5 | 1.2 [−4.4; 7.7]; p = 0.585 | 3.3 [−3.5; 10.1]; p = 0.334 | −0.9 [−6.6; 4.8]; p = 0.749 | −1.1 [−6.0; 3.8]; p = 0.649 |
| Yoga B | 121.0 ± 11.8 | 117.8 ± 16.9 | 119.7 ± 13.3 | −3.2 [−9.6; 3.2]; p = 0.321 | – | −0.3 [−5.9; 5.3]; p = 0.911 | – | |
| Control | 120.0 ± 15.1 | 120.2 ± 7.7 | 120.3 ± 10.3 | – | – | – | – | |
| Nocturnal DBP | Yoga A | 71.5 ± 12.0 | 70.7 ± 11.5 | 70.0 ± 9.1 | −1.2 [−5.7; 3.3]; p = 0.594 | −0.1 [−4.7; 4.6]; p = 0.975 | 0.7 [−3.2; 4.7]; p = 0.722 | −0.8 [−4.3; 2.7]; p = 0.637 |
| Yoga B | 72.7 ± 9.3 | 71.1 ± 11.7 | 71.0 ± 7.9 | −0.4 [−4.9; 4.2]; p = 0.867 | – | −1.0 [−4.5; 2.6]; p = 0.588 | – | |
| Control | 71.2 ± 10.4 | 70.8 ± 7.1 | 70.7 ± 7.9 | – | – | – | – | |
| Nocturnal HR | Yoga A | 65.2 ± 10.7 | 64.3 ± 9.5 | 61.8 ± 8.9 | −2.2 [−6.0; 1.7]; p = 0.260 | −2.5 [−5.6; 0.6]; p = 0.118 | −4.0 [−7.7; −0.2]; p = 0.041 | −4.6 [−7.4; −1.7]; p = 0.002 |
| Yoga B | 63.1 ± 7.7 | 65.4 ± 7.9 | 65.9 ± 7.7 | −0.9 [−3.2; 4.9]; p = 0.672 | – | 1.2 [−2.2; 4.7]; p = 0.474 | – | |
| Control | 62.1 ± 6.3 | 61.8 ± 7.8 | 63.5 ± 6.5 | – | – | – | – | |
Effects expressed as mean ± standard deviation. Group differences were calculated within covariance models that controlled for baseline values.
CI = confidence interval, DBP = diastolic blood pressure, HR = heart rate, SBP = systolic blood pressure
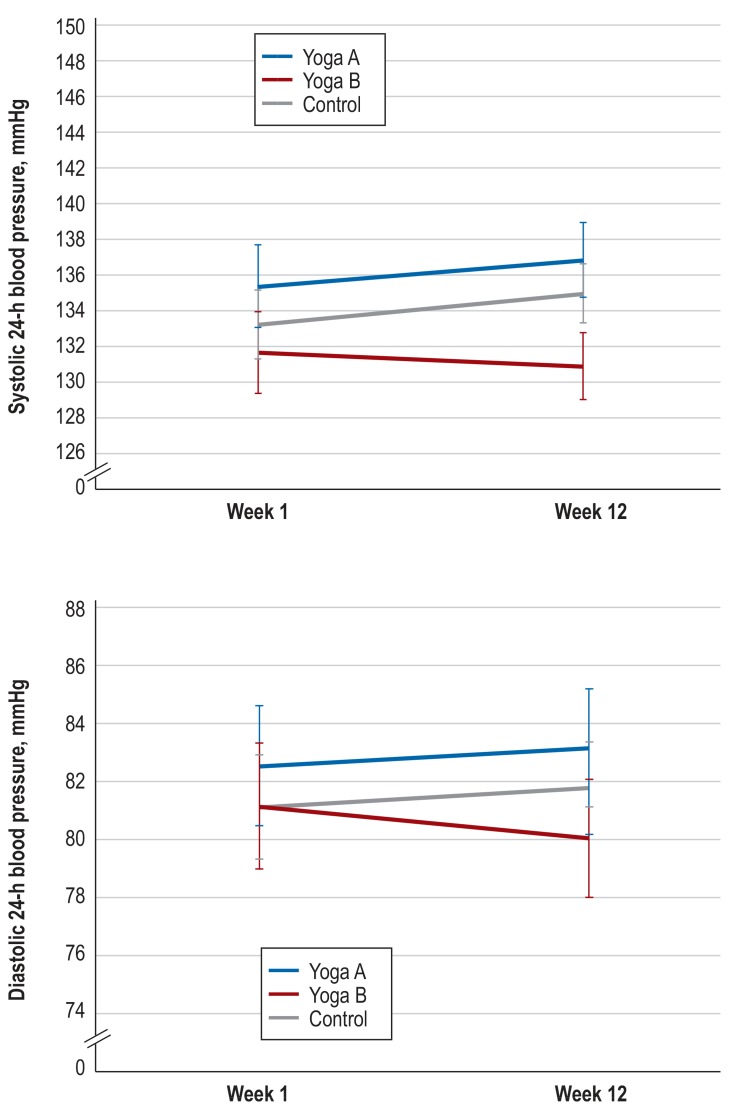
Ambulatory blood pressure measurement
At 12 weeks the systolic 24-h blood pressure (a primary outcome measure) was significantly lower in the group without yoga postures than in the group with yoga postures (p = 0.045; Figure 2; eTable 1) or the control group (p = 0.035). At 28 weeks the reverse was found: the systolic 24-h blood pressure in the group with yoga postures was significantly lower than in the control group (p = 0.022) and in the group without yoga postures (p = 0.037; eTable 1). At no time were there any intergroup differences with regard to diastolic 24-h blood pressure (Figure 2, eTable 1). Further results of the ambulatory measurement of blood pressure are given in the eSupplement.
Figure 2.
Effects on the primary outcome measure of 24-h blood pressure at week 1 and week 12 (mean ± standard deviation) in the intervention group with yoga postures (Yoga A), the intervention group without yoga postures (Yoga B), and the control group. Effects on the 24-h blood pressure at week 28 are shown in eTable 1.
Safety
No severe adverse events occurred during the study. Nine patients (36.0%) in the intervention group with yoga postures experienced a total of 15 minor adverse events, while in the group without yoga postures four patients (16.0%) reported five minor adverse events. In the control group, two patients (8.0%) had four minor adverse events (eSupplement).
Discussion
In this randomized controlled trial, a 12-week yoga intervention consisting purely of breathing and meditation techniques without any use of yoga postures lowered the joint primary outcome measure of 24-h systolic blood pressure by a greater amount than no treatment or an intervention with additional yoga postures. The other joint primary outcome measure, 24-h diastolic blood pressure, was not reduced. These results agree with the findings of a meta-analysis (11), although the effect sizes in our trial were smaller (-3.8 mmHg, 95% confidence interval [-7.5; -0.3] versus -14.1 mmHg, 95% confidence interval [-24.7; -3.6]). These differences from earlier studies are most likely attributable to differences in inclusion criteria, blood pressure recording methods (clinical versus ambulatory), and the country in which the study was carried out. In this last respect, yoga studies in India generally show larger effect sizes than studies performed in other countries (21).
Interestingly, though based only on secondary outcome measures, the pattern was reversed at week 28. In this final week of the study the group that had received the intervention with yoga postures exhibited greater reductions in ambulatory systolic blood pressure than the group without yoga postures.
In comparison with the untreated control group, 13 patients had to be treated with yoga to achieve substantial improvement in one patient.
A simultaneous increase in parasympathetic activity and decrease in sympathetic activity has been postulated as an important mechanism of action of therapeutic yoga (22). In this context, particularly yoga techniques of slow breathing and meditation may bring about a short-term reinforcement of parasympathetic activity (23– 25). In experimental studies where yoga relaxation techniques were supplemented with yoga postures, no further potentiation of parasympathetic activity ensued (23). Together with the findings of the meta-analysis (11), this led to breathing and meditation techniques, rather than yoga postures, being viewed as the principal mechanism of action of yoga in patients with arterial hypertension (26). While this hypothesis was certainly confirmed immediately after the end of the yoga interventions, the results of our trial indicate that longer-term positive effects on arterial hypertension can be achieved only with the integration of yoga postures. The adoption of yoga postures can be seen as a form of isometric training, while dynamic yoga sequences (e.g., the well-known sun salutation) add an element from aerobic training (27, 28). Both isometric and aerobic training can lower blood pressure (29– 31). These may then be the mechanisms responsible for the long-term effect of an intervention including yoga postures.
The main reason for the long-term group differences may, however, also lie in a discrepancy in treatment adherence following the end of the interventions: a higher proportion of patients in the group with yoga postures than in the group without yoga postures continued to practice the techniques they had been taught after study week 12. The group with yoga postures also practiced for a much longer time each week. It may be that yoga postures are easier to integrate into daily activities than yoga breathing and meditation techniques. When interpreting the findings in this way, however, it must be taken into account that the long-term group differences were greater in the intention-to-treat analysis than in the per-protocol analysis.
Limitations
Our study featured some limitations. First, the wait list group did not control for the expectations of the patients, the time taken up, or the attentiveness of the instructors. Moreover, the study participants were not blinded to the intervention they received. The participants were predominantly female and well educated, and thus tended to be more typical of yoga practitioners (7, 32) than of patients with hypertension. This reduced the generalizability of the findings. No effects of the interventions on diastolic blood pressure were detected, the overall reduction in systolic blood pressure was only slight, and only 8% of hypertension patients will benefit substantially from a yoga intervention.
Conclusion
Only yoga without yoga postures had an immediate effect on the 24-h systolic (but not diastolic) blood pressure; yoga with yoga postures had no such action. However, the inclusion of yoga postures seems necessary if the effects are to be maintained beyond the end of the intervention. Since we found yoga in patients with arterial hypertension to be effective and safe, yoga can be recommended as a complement to medication for reduction of systolic blood pressure in this group.
Supplementary Material
eSUPPLEMENT
Methods
Interventions
This trial compared the efficacy of two different yoga interventions, with or without yoga postures, in patients with arterial hypertension who were being treated with antihypertensive medication. While the interpretation of significant intergroup differences between two active interventions is unproblematic, nonsignificant results are open to potentially various and contradictory interpretations: they can be viewed as showing that the two interventions are similarly effective, ineffective, or even harmful (e1). To counter this possible ambiguity, the inclusion of an additional, inert study arm is generally recommended when comparing active interventions (e1). Accordingly, we included a third arm comprising an untreated control group in this trial.
Yoga
The two interventions were developed by an expert panel made up of seven certified and experienced yoga instructors representing various yoga traditions, based on earlier studies, classic yoga texts, and their own clinical experience. The committee members planned the interventions in such a way that they combined elements from various traditions and thus did not follow any particular “school” of yoga. The interventions were also adapted to the specific needs, potentials, and limitations of patients with arterial hypertension. The yoga instructors introduced all exercises gently at first, then increased their intensity in the course of the program. Aids (blocks, belts, or blankets) were used if necessary, and/or the exercises were modified for individual patients. Details of the two interventions can be found in eTables 2 and 3.
Outcome measures
The secondary outcome measures included 24-h heart rate and diurnal and nocturnal blood pressure, measured using a monitoring device. The parameters were categorized on the basis of the sleeping and waking times reported by the respective patients.
Further secondary outcome measures were defined a priori. They comprised:
The following questionnaires were used to survey these parameters, respectively:
Further variables were documented for evaluation in mediator analyses to investigate potential mechanisms of action of yoga in patients with arterial hypertension:
Because these variables did not serve to verify efficacy, they are not reported in this article.
Before randomization, the patients included in the study were assessed with regard to their expectations of the two interventions and of waiting for treatment in the control group. To this end, they stated their expectations on an 11-point Likert scale from 0 = ineffective to 10 = very effective. The later analysis considered only the expectation for the intervention to which the patient was then randomized.
Results
Adherence
During the first 12 weeks of the study the patients in the intervention group with yoga postures took part in 8.3 ± 3.3 (mean ± standard deviation) (68.3%) of the weekly yoga sessions and spent a further 105.2 ± 51.3 min doing their exercises at home. The participants in the intervention group without yoga postures visited 8.4 ± 3.3 (70.0%) of the sessions and spent 67.2 ± 54.3 min doing the exercises at home.
After the end of the interventions, from week 13 to week 28 of the study, 14 of the 20 patients from the group with yoga postures for whom this information was available (70%) continued to practice yoga, compared with 12 of 22 (54.5%) for the group without yoga postures. On average the participants from the group with yoga postures exercised 2.6 ± 1.6 times per week for a total of 55.8 ± 87.2 min, while those in the group without yoga postures performed their exercises times 2.2 ± 1.9 times per week for a total of 25.0 ± 38.8 min.
When only the participants who continued to practice yoga after the end of the interventions were included in analysis, those in the group with yoga postures did their exercises for 87.7 ± 96.2 min per week and those in the group without yoga postures for 50.0 ± 42.2 min per week.
Considering only those patients who continued the exercises after the end of the interventions, there was no difference between the groups with regard to systolic blood pressure (p = 0.439) or diastolic blood pressure (p = 0.452; eTable 4). There was also no significant difference between the groups in this respect when only those who had not continued practicing yoga were included (etable 5).
Antihypertensive medication
Most patients were treated with ACE inhibitors and AT1-receptor blockers (table). In the course of the study, 19 of the 23 patients in the intervention group with yoga postures for whom this information was available (82.6%) did not change their medication, three (13.0%) increased it, and one patient (4.3%) reduced his/her dose. In the intervention group without yoga postures, the medication intake remained the same in 19 of 24 patients (79.2%), increased in two (8.3%), and decreased in three patients (12.5%). In the control group, 21 of 23 patients (91.3%) did not change their medication, two (8.7%) increased it, and none decreased it. The distribution of patients in whom the medication intake remained the same, increased, or decreased did not differ significantly among the three study groups (chi-square test, p = 0.425).
Ambulatory blood pressure measurement
In week 1, an average of 73.3 ± 5.5 individual measurements were made per patient during the 24-h period of blood pressure monitoring. Of this total, an average of 60.4 ± 9.3 measurements were correct and could be used to calculate the 24-h blood pressure. The corresponding figures in weeks 12 and 28 were 73.7 ± 7.7 (57.6 ± 13.1 correct per patient) and 74.9 ± 4.8 (60.0 ± 11.9 correct), respectively.
The numbers of patients with normal blood pressure, prehypertension, and hypertension grade 1 or 2 (based on the 24-h monitoring) at weeks 1, 12, and 28 are shown in eTable 6. At week 12, four patients in the intervention group with yoga postures, six in the intervention group without yoga postures, and four in the control group switched to a lower blood pressure category (number needed to treat for the comparison yoga without yoga postures versus control group = 12.5). At week 28, nine patients in the group with yoga postures, four in the group without yoga postures, and six in the control group switched to a lower blood pressure category (number needed to treat for the comparison yoga with yoga postures versus control group = 12.5).
With regard to further ambulatory blood pressure measurements, all significant difference among the groups are reported in the following. The remaining group differences did not attain significance and are shown in detail in eTable 1. At 12 weeks the diurnal systolic blood pressure was significantly lower in the intervention group without yoga postures than in the control group (p = 0.045) and the yoga group with yoga postures (p = 0.042; eTable 1). At 28 weeks, in contrast, the diurnal systolic blood pressure in the yoga group with yoga postures was significantly lower than in the control group (p = 0.023) and the yoga group without yoga postures (p = 0.030; eTable 1). For heart rate measurements, significant intergroup differences were only observed at 28 weeks. At this time the nocturnal heart rate was significantly lower in the group with yoga postures than in either of the other groups (etable 1).
Questionnaires
Significant group differences were found in none of the outcome measures surveyed by means of questionnaires, with the sole exception of the SF-36 mental quality of life, which was significantly better among the participants in the group with yoga postures than in the group without yoga postures at week 28 (p = 0.028; eTable 7). No other differences among the groups were found at any time.
Safety
The adverse events registered in the intervention group with yoga postures were as follows:
The following adverse events occurred in the yoga group without yoga postures:
The adverse events recorded in the control group were:
None of the adverse events had a direct temporal relation with the respective study intervention. After careful assessment, none of the events was judged to be associated with the intervention.
Subjective stress
Anxiety and depression
Physical and mental quality of life.
The German 10-question version of the Perceived Stress Scale (e2)
The German version of the Hospital Anxiety and Depression Scale (e3)
The German version of the Short Form-36 Health Survey Questionnaire (SF-36) (e4).
Physical activity, surveyed by means of the Baecke Questionnaire (e5)
Nutritional habits, using the Five a Day Food Frequency Questionnaire (e6).
Headache (n = 3)
Shoulder pain (n = 1)
Knee pain (n = 1)
Tendinitis (n = 1)
Meniscus rupture (n = 1)
Knee injury from bicycle accident (n = 1)
Prolapsed intervertebral disc (n = 1)
Influenza (n = 2)
Parodontitis (n = 1)
Hypertensive emergency (n = 1)
Mental problems (n = 1)
Breast operation (n = 1)
Influenza (n = 1)
Parodontitis (n = 1)
Tinnitus (n = 1)
Autoimmune disease (n = 1)
Knee pain (n = 1)
Headache (n = 1)
Neck pain (n = 1)
Sleep disturbances (n = 1)
Kidney disease (n = 1)
Table. Sociodemographic and clinical characteristics at the start of the study.
|
Yoga A (n = 25) |
Yoga B (n = 25) |
Control (n = 25) |
|
| Sociodemographic characteristics | |||
| Age, years*1 | 59.4 ± 9.1 | 56.5 ± 10.6 | 57.0 ± 8.7 |
| Sex | |||
| Female*2 | 18 (72.0%) | 18 (72.0%) | 18 (72.0%) |
| Male*2 | 7 (28.0%) | 7 (28.0%) | 7 (28.0%) |
| Height, cm*1 | 171.3 ± 8.9 | 169.6 ± 8.2 | 168.0 ± 8.0 |
| Weight, kg*1 | 85.4 ± 15.2 | 87.9 ± 27.9 | 80.5 ± 13.5 |
| Marital status*2 | |||
| Married/stable partnership | 4 (16.0%) | 4 (16.0%) | 7 (28.0%) |
| Single | 21 (84.0%) | 21 (84.0%) | 17 (72.0%) |
| Education*3 | |||
| Year 9 lower secondary school certificate (Hauptschulabschluss) |
5 (20.0%) | 3 (12.0%) | 8 (32.0%) |
| Year 10 intermediate secondary school certificate (Realschulabschluss) |
14 (56.0%) | 10 (40.0%) | 7 (28.0%) |
| University entrance qualification | 2 (8.0%) | 4 (16.0%) | 5 (20.0%) |
| University/technical university degree | 4 (16.0%) | 8 (32.0%) | 4 (16.0%) |
| Occupation*2 | |||
| Employed full-time | 2 (8.0%) | 5 (20.0%) | 8 (32.0%) |
| Employed part-time | 8 (32.0%) | 9 (36.0%) | 4 (16.0%) |
| Unemployed | 15 (60.0%) | 11 (44.0%) | 13 (52.0%) |
| Blood pressure, mmHg*1 | |||
| Systolic/24 h | 135.4 ± 11.6 | 131.7 ± 11.3 | 133.3 ± 9.8 |
| Diastolic/24 h | 82.5 ± 10.3 | 81.1 ± 10.9 | 81.1 ± 9.1 |
| Systolic, diurnal | 137.1 ± 11.5 | 133.4 ± 11.7 | 135.5 ± 9.3 |
| Diastolic, diurnal | 84.2 ± 10.5 | 82.5 ± 11.3 | 82.7 ± 9.2 |
| Systolic, nocturnal | 122.4 ± 16.0 | 121.0 ± 11.8 | 120.0 ± 15.1 |
| Diastolic, nocturnal | 71.5 ± 12.0 | 72.7 ± 9.3 | 71.2 ± 10.4 |
| Heart rate, beats/min*1 | |||
| 24 h | 73.0 ± 12.4 | 73.5 ± 10.1 | 70.8 ± 7.6 |
| Diurnal | 74.2 ± 12.9 | 75.0 ± 10.1 | 72.2 ± 7.9 |
| Nocturnal | 65.2 ± 10.7 | 63.1 ± 7.7 | 62.1 ± 6.3 |
| Expectation of effect | 7.3 ± 1.7 | 6.1 ± 2.1 | 3.9 ± 2.3 |
| Antihypertensive medication*2 | |||
| ACE inhibitors/AT1-receptor blockers | 21 (84.0%) | 23 (92.0%) | 23 (92.0%) |
| Diuretics | 10 (40.0%) | 9 (36.0%) | 10 (40.0%) |
| Beta blockers | 13 (52.0%) | 8 (32.0%) | 6 (24.0%) |
| Calcium channel blockers | 9 (36.0%) | 8 (32.0%) | 9 (36.0%) |
| Alpha blockers | 2 (8.0%) | 1 (4.0%) | 5 (20.0%) |
*1 Mean ± standard deviation; *2 n (% of n); *3 Data on education were missing for one patient
Key Messages.
Only yoga interventions that do not include any yoga postures seem to lower the ambulatory blood pressure of patients with arterial hypertension as measured immediately after the end of the intervention.
Further research is necessary before a specific yoga style can conclusively be recommended to patients with arterial hypertension.
eTable 2. Exercises from the intervention with yoga postures.
| Sessions 1 to 4 | Sessions 5 to 8 | Sessions 9 to 12 | |||||
| Introduction | 15 min | 3 min | Greeting and brief period of contemplation | 3 min | Greeting and brief period of contemplation | 3 min | Greeting and brief period of contemplation |
| 12 min | Philosophical/ theoretical topic | 12 min | Philosophical/ theoretical topic | 12 min | Philosophical/ theoretical topic | ||
| Yoga postures | 45 min | 10 min | Light mobilization exercises and work on sitting upright | 8 min | Light mobilization exercises and work on sitting upright | 6 min | Light mobilization exercises and work on sitting upright |
| 4 min | Vyaghrasana (tiger pose) | 2 min | Vyaghrasana (tiger pose) | 2 min | Vyaghrasana (tiger pose) | ||
| 6 min | Mountain flow | 4 min | Mountain flow | 3 min | Mountain flow | ||
| 8 min | Half sun salutation | 4 min | Half sun salutation | 4 min | Half sun salutation | ||
| 8 min | Virabhadrasana 1 (warrior pose 1) with twist variation | 5 min | Virabhadrasana 1 (warrior pose 1) with twist variation | ||||
| 5 min | Virabhadrasana 2 (dynamic warrior pose 2) | 3 min | Virabhadrasana 2 (dynamic warrior pose 2) | ||||
| 8 min | Virabhadrasana 2 (warrior pose 2) with transition to Parsvakonasana (extended side angle pose) | ||||||
| 4 min | Paschimottanasana (seated forward bend) | 3 min | Paschimottanasana (seated forward bend) | 3 min | Paschimottanasana (seated forward bend) | ||
| 8 min | Setu Bandha Sarvangasana (dynamic/static bridge pose) with intervening Apanasana (knees to chest pose) | 6 min | Setu Bandha Sarvangasana (dynamic/static bridge pose) with intervening Apanasana (knees to chest pose) | 6 min | Setu Bandha Sarvangasana (dynamic/static bridge pose) with intervening Apanasana (knees to chest pose) | ||
| 5 min | Supta Parivartana‧sana (twist-stretch pose) | 5 min | Supta Parivartana‧sana (twist-stretch pose) | 5 min | Supta Parivartanasana (twist-stretch pose) | ||
| Breathing and meditation exercises | 10–15 min | 4 min | Perception exercise in supine position | 3 min | Perception exercise in supine position | 2 min | Perception exercise in supine position |
| 4 min | Deeper breathing and completion of breathing with feet flat on floor | 4 min | Deeper breathing and completion of breathing with feet flat on floor | 2 min | Deeper breathing and completion of breathing with feet flat on floor | ||
| 2 min | Setu Bandha Sarvangasana (dynamic/static bridge pose) with intervening Apanasana (knees to chest pose) | 1 min | Setu Bandha Sarvangasana (dynamic/static bridge pose) with intervening Apanasana (knees to chest pose) | 1 min | Setu Bandha Sarvangasana (dynamic/static bridge pose) with intervening Apanasana (knees to chest pose) | ||
| 6 min | “Light” Nadi Shodhana (alternate nostril breathing) | 7 min | Nadi Shodhana (alternate nostril breathing) | ||||
| 1–2 min | Meditation—observe stillness | 3 min | Meditation—observe stillness | ||||
| Conclusion | 15–20 min | 10 min | Supervised deep relaxation | 10 min | Supervised deep relaxation | 10 min | Supervised deep relaxation |
| 5 min | Discussion of home exercise program | ||||||
| 5 min | Final group discussion and farewell | 5 min | Final group discussion and farewell | 5 min | Final group discussion and farewell |
eTable 3. Exercises from the intervention without yoga postures.
| Sessions 1 to 4 | Sessions 5 to 8 | Sessions 9 to 12 | |||||
| Introduction | 15 min | 3 min | Greeting and brief period of contemplation | 3 min | Greeting and brief period of contemplation | 3 min | Greeting and brief period of contemplation |
| 12 min | Philosophical/ theoretical topic | 12 min | Philosophical/ theoretical topic | 12 min | Philosophical/ theoretical topic | ||
|
Breathing and meditation exercises |
58–60 min | 4 min | Light mobilization exercises and work on sitting upright | 4 min | Light mobilization exercises and work on sitting upright | 4 min | Light mobilization exercises and work on sitting upright |
| 5 min | Perception exercise in supine position | 4 min | Perception exercise in supine position | 4 min | Perception exercise in supine position | ||
| 5 min | Deeper breathing with feet flat on floor | 4 min | Deeper breathing with feet flat on floor | 4 min | Deeper breathing with feet flat on floor | ||
| 5 min | Completion of breathing with feet flat on floor | 4 min | Completion of breathing with feet flat on floor | 3 min | Completion of breathing with feet flat on floor | ||
| 4 min | Setu Bandha Sarvangasana (dynamic bridge pose) with inter- vening Apana- sana (knees to chest pose) | 4 min | Setu Bandha Sarvangasana (dynamic bridge pose) with inter- vening Apana- sana (knees to chest pose) | 4 min | Setu Bandha Sarvangasana (dynamic bridge pose) with inter- vening Apana- sana (knees to chest pose) | ||
| 6 min | Work on sitting upright | 3 min | Work on sitting upright | 2 min | Work on sitting upright | ||
| 4 min | Gradual guidance towards full yoga breathing | 4 min | Gradual guidance towards full yoga breathing | 4 min | Gradual guidance towards full yoga breathing | ||
| 11 min | Ujjayi (victorious breathing) | 7 min | Ujjayi (victorious breathing) | 5 min | Ujjayi (victorious breathing) | ||
| 2 min | Meditation | 4 min | Meditation | 5 min | Meditation | ||
| 3 min | Relaxation with appreciation of the effect in supine position | 3 min | Relaxation with appreciation of the effect in supine position | 3 min | Relaxation with appreciation of the effect in supine position | ||
| 5 min | Supta Parivarta- nasana (twist- stretch pose) | 4 min | Supta Parivarta- nasana (twist- stretch pose) | 4 min | Supta Parivarta- nasana (twist- stretch pose) | ||
| 2 min | Again, observe, deepen, and complete breathing | 3 min | Again, observe, deepen, and complete breathing | 3 min | Again, observe, deepen, and complete breathing | ||
| 9 min | “Light” Nadi Shodhana (alter- nate nostril breathing) „light“ | 10 min | Nadi Shodhana (alternate nostril breathing) | ||||
| 2 min | Meditation | 3 min | Meditation— observe silence | 5 min | Meditation— observe silence | ||
| Conclusion | 15–18 min | 8 min | Supervised deep relaxation | 10 min | Supervised deep relaxation | 10 min | Supervised deep relaxation |
| 5 min | Discussion of home exercise program | ||||||
| 5 min | Final group discussion and farewell | 5 min | Final group discussion and farewell | 5 min | Final group discussion and farewell | ||
eTable 4. Effects on systolic and diastolic 24-h blood pressure in the yoga group with yoga postures (Yoga A; n = 14) and the yoga group without yoga postures (Yoga B; n = 12).
| Outcome measure | Group | Measurement time |
Group difference [95% CI] week 28 |
|
| Week 1 | Week 28 | |||
| 24-h SBP | Yoga A | 138.3 ± 10.6 | 132.4 ± 8.3 | −2.8 [−10.0; 4.5]; p = 0.439 |
| Yoga B | 132.3 ± 13.0 | 131.7 ± 11.3 | – | |
| 24-h DBP | Yoga A | 81.6 ± 8.2 | 79.8 ± 5.3 | −1.1 [−4.2; 1.9]; p = 0.452 |
| Yoga B | 80.7 ± 9.3 | 79.3 ± 6.7 | – | |
Effects expressed as mean ± standard deviation. Only patients who continued to practice yoga after week 12 were included in this analysis. Group differences were calculated within covariance models that controlled for baseline values.
CI = confidence interval, DBP = diastolic blood pressure, SBP = systolic blood pressure
eTable 5. Effects on systolic and diastolic 24-h blood pressure in the yoga group with yoga postures (Yoga A; n = 11) and the yoga group without yoga postures (Yoga B; n = 13).
| Outcome measure | Group | Measurement time |
Group difference [95% CI] week 28 |
|
| Week 1 | Week 28 | |||
| 24-h SBP | Yoga A | 131.7 ± 12.3 | 130.0 ± 8.6 | −5.3 [−10.9; 0.3]; p = 0.060 |
| Yoga B | 131.1 ± 10.1 | 134.9 ± 12.7 | – | |
| 24-h DBP | Yoga A | 83.6 ± 12.8 | 82.4 ± 9.3 | −1.3 [−4.4; 1.99]; p = 0.409 |
| Yoga B | 83.1 ± 11.7 | 82.7 ± 9.3 | – | |
Effects expressed as mean ± standard deviation. Only patients who did not continue to practice yoga after week 12 were included in this analysis. Group differences were calculated within covariance models that controlled for baseline values.
CI = confidence interval, DBP = diastolic blood pressure, SBP = systolic blood pressure
eTable 6. Distribution of the blood pressure categories in the three study groups.
| Group | Normal | Prehypertension | Hypertension grade 1 | Hypertension grade 2 |
| Yoga A | ||||
| Week 1 | 3 | 1 | 9 | 12 |
| Week 12 | 0 | 4 | 7 | 14 |
| Week 28 | 0 | 4 | 16 | 5 |
| Yoga B | ||||
| Week 1 | 2 | 6 | 7 | 10 |
| Week 12 | 1 | 4 | 15 | 5 |
| Week 28 | 1 | 5 | 8 | 11 |
| Control | ||||
| Week 1 | 2 | 3 | 9 | 11 |
| Week 12 | 0 | 4 | 8 | 13 |
| Week 28 | 0 | 4 | 13 | 8 |
Numbers of patients with normal blood pressure (<120 mmHg systolic and <80 mmHg diastolic),
prehypertension (120–129 mmHg systolic and <80 mmHg diastolic),
hypertension grade 1 (130–139 mmHg systolic or 80–89 mmHg diastolic), and
hypertension grade 2 (>140 mmHg systolic or >80 mmHg diastolic) in the intervention group with yoga
postures (Yoga A), the intervention group without yoga postures (Yoga B), and the control group at weeks 1, 12, and 28
eTable 7. Effects on psychometric variables in the yoga group with yoga postures (Yoga A), the yoga group without yoga postures (Yoga B), and the control group.
| Outcome measure | Group | Measurement time |
Group difference [95% CI] compared with control group (week 12) |
Group difference [95% CI] compared with Yoga B (week 12) |
Group difference [95% CI] compared with control group (week 28) |
Group difference [95% CI] compared with Yoga B (week 28) |
||
| Week 1 | Week 12 | Week 28 | ||||||
| Stress | Yoga A | 20.3 ± 8.0 | 20.2 ± 10.0 | 17.7 ± 8.2 | −1.7 [−60; 2.6]; p = 0.423 | −1.7 [−5.5; 2.1]; p = 0.373 | −1.2 [−4.7; 2.2]; p = 0.483 | −3.3 [−6.6; 0.1]; p = 0.057 |
| Yoga B | 24.0 ± 9.8 | 25.3 ± 9.7 | 24.5 ± 9.8 | −1.0 [−5.0; 3.0]; p = 0.617 | – | 2.9 [−1.2; 7.1]; p = 0.155 | – | |
| Control | 19.2 ± 7.6 | 21.2 ± 8.9 | 19.0 ± 7.7 | – | – | – | – | |
| Anxiety | Yoga A | 12.4 ± 2.2 | 12.1 ± 2.0 | 12.1 ± 2.0 | −0.6 [−1.5; 0.3]; p = 0.187 | 0.5 [−0.5; 1.5]; p = 0.330 | −0.5 [−1.6; 0.7]; p = 0.416 | 0.5 [−0.6; 1.6]; p = 0.349 |
| Yoga B | 12.2 ± 2.6 | 11.4 ± 2.8 | 11.5 ± 2.9 | −0.8 [−2.0; 0.3]; p = 0.147 | – | −0.5 [−1.6; 0.6]; p = 0.353 | – | |
| Control | 12.0 ± 1.9 | 12.0 ± 2.1 | 12.0 ± 2.0 | – | – | – | – | |
| Depression | Yoga A | 9.8 ± 1.8 | 10.0 ± 1.5 | 10.0 ± 1.4 | −0.4 [−1.4; 0.6]; p = 0.397 | 0.3 [−0.5; 1.2]; p = 0.428 | −0.4 [−1.5; 0.6]; p = 0.414 | −0.1 [1.0; 0.8]; p = 0.802 |
| Yoga B | 10.1 ± 1.7 | 9.7 ± 1.5 | 10.2 ± 1.8 | −0.7 [−1.6; 0.3]; p = 0.147 | – | 0.0 [−1.1; 1.0]; p = 0.948 | – | |
| Control | 9.6 ± 1.4 | 10.1 ± 1.5 | 10.1 ± 1.7 | – | – | – | – | |
| Physical QoL | Yoga A | 50.4 ± 5.7 | 47.9 ± 9.4 | 48.5 ± 7.9 | −1.1 [−6.6; 4.3]; p = 0.677 | −1.1 [−6.0; −3.9]; p = 0.669 | 1.7 [−3.5; 6.9]; p = 0.509 | 2.9 [−7.8; 2.0]; p = 0.242 |
| Yoga B | 46.4 ± 10.1 | 46.9 ± 8.4 | 48.1 ± 10.8 | 0.1 [−3.6; 3.8]; p = 0.961 | – | 2.0 [−2.5; 6.6]; p = 0.375 | – | |
| Control | 48.9 ± 10.3 | 48.5 ± 10.3 | 46.4 ± 9.8 | – | – | – | – | |
| Yoga A | 53.1 ± 6.6 | 52.3 ± 7.6 | 53.3 ± 6.2 | 1.7 [−3.2; 6.5]; p = 0.492 | 2.4 [−1.6; 6.3]; p = 0.237 | −0.9 [−5.5; 3.8]; p = 0.704 | 4.5 [0.5; 8.4]; p = 0.028 | |
| Yoga B | 50.0 ± 11.1 | 47.5 ± 11.0 | 47.1 ± 10.2 | −0.4 [−5.5; 4.7]; p = 0.874 | – | −4.3 [−9.8; 1. 2]; p = 0.124 | – | |
| Control | 50.6 ± 10.6 | 48.7 ± 10.2 | 51.0 ± 8.3 | – | – | – | – | |
Effects expressed as mean ± standard deviation. Group differences were calculated within covariance models that controlled for baseline values. The following questionnaires were used to survey the outcome measures:
stress: Perceived Stress Scale (e2), anxiety and depression: Hospital Anxiety and Depression Scale (e3), physical and mental QoL: Short Form-36 Health Survey Questionnaire (e4)
CI = confidence interval; QoL = quality of life
Acknowledgments
Acknowledgments
This study was supported by the German Occupational Union for Yoga Teachers (Berufsverband der Yogalehrenden in Deutschland, BDY). The sponsor had no influence on the planning or conduct of the study, on the acquisition, management, analysis, or interpretation of the data, on the writing, revision, or approval of the manuscript, or on the decision to submit the manuscript for publication. We are particularly grateful to Peter Greve, Dr. Bettina Knothe, Nicole Verheyden, Frank Loddo, Eva Grandao, Janine Nagel, and Dr. Matthias Deparade for the development of the yoga interventions and to Eva Grandao and Janine Nagel for implementing the yoga interventions.
Data sharing
After the conclusion of further analyses on the data used for this study, the authors will be willing to share the data with other researchers for scientific purposes. Interested parties should contact Dr. Holger Cramer.
Translated from the original German by David Roseveare
Footnotes
Conflict of interest statement
Dr. Cramer received support for this study from the BDY. The remaining authors declare that no conflict of interest exists.
References
- 1.Neuhauser H, Diederichs C, Boeing H, et al. Hypertension in Germany—data from seven population-based epidemiological studies (1994-2012) Dtsch Arztebl Int. 2016;113:809–815. doi: 10.3238/arztebl.2016.0809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation. Global Status Report on noncommunicable diseases. www.apps.who.int/iris/bitstream/10665/148114/1/ 9789241564854_eng.pdf?ua=1 (last accessed on 11 April 2018) [Google Scholar]
- 3.Woolf KJ, Bisognano JD. Nondrug interventions for treatment of hypertension. J Clin Hypertens (Greenwich) 2011;13:829–835. doi: 10.1111/j.1751-7176.2011.00524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feuerstein G. The yoga tradition. Prescott: Hohm Press; 1998 [Google Scholar]
- 5.Iyengar BKS. Light on yoga. New York: Schocken Books; 1966 [Google Scholar]
- 6.De Michelis E. Großbritannien: Continuum International Publishing Group. London: 2005. A history of modern yoga: Patanjali and western esotericism. [Google Scholar]
- 7.Cramer H. Yoga in Deutschland - Ergebnisse einer national repräsentativen Umfrage. Forsch Komplementmed. 2015;22:304–310. doi: 10.1159/000439468. [DOI] [PubMed] [Google Scholar]
- 8.Cramer H, Thoms MS, Anheyer D, Lauche R, Dobos G. Yoga in women with abdominal obesity—a randomized controlled trial. Dtsch Arztebl Int. 2016;113:645–652. doi: 10.3238/arztebl.2016.0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klatte R, Pabst S, Beelmann A, Rosendahl J. The efficacy of body-oriented yoga in mental disorders—a systematic review and meta-analysis. Dtsch Arztebl Int. 2016;113:195–202. doi: 10.3238/arztebl.2016.0195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lund S, Angelow A, Baum E, et al. Hausärztliche Risikoberatung zur kardiovaskulären Prävention - S3-Leitlinie. www.awmf.org/uploads/tx_szleitlinien/053-024l_Hausaerztliche_Risikoberat_kardiovask_Prae_vention_2017-11_1.pdf(last accessed on 11 April 2018) [Google Scholar]
- 11.Cramer H, Haller H, Lauche R, Steckhan N, Michalsen A, Dobos G. A systematic review and meta-analysis of yoga for hypertension. Am J Hypertens. 2014;27:1146–1151. doi: 10.1093/ajh/hpu078. [DOI] [PubMed] [Google Scholar]
- 12.World Medical Association. WMA Declaration of Helsinki - ethical principles for medical research involving human subjects. www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (last accessed on 11 April 2018) [Google Scholar]
- 13.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152:726–732. doi: 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 14.Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol. 2004;4 doi: 10.1186/1471-2288-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions, John Wiley & Sons Ltd. West Sussex, UK, 2008 [Google Scholar]
- 16.Westhoff TH, Straub-Hohenbleicher H, Schmidt S, Tolle M, Zidek W, van der Giet M. Convenience of ambulatory blood pressure monitoring: comparison of different devices. Blood Press Monit. 2005;10:239–242. doi: 10.1097/01.mbp.0000172711.82287.7f. [DOI] [PubMed] [Google Scholar]
- 17.U.S. Food & Drug Association. Code of Federal Regulations,Title 21, Volume 5, Chapter I, Part 312. www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=312.32 (last accessed on 11 April 2018) [Google Scholar]
- 18.Rubin DB. New York: 1987. Multiple imputation for nonresponse in surveys, John Wiley & Sons. [Google Scholar]
- 19.Schafer JL. Analysis of incomplete multivariate data. Chapman and Hall. New York. 1997 [Google Scholar]
- 20.Vickers AJ, Altman DG. Statistics notes: analysing controlled trials with baseline and follow up measurements. BMJ. 2001;323:1123–1124. doi: 10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cramer H, Lauche R, Langhorst J, Dobos G. Are Indian yoga trials more likely to be positive than those from other countries? A systematic review of randomized controlled trials. Contemp Clin Trials. 2015;41:269–272. doi: 10.1016/j.cct.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 22.Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. 2012;78:571–579. doi: 10.1016/j.mehy.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 23.Markil N, Whitehurst M, Jacobs PL, Zoeller RF. Yoga Nidra relaxation increases heart rate variability and is unaffected by a prior bout of Hatha yoga. J Altern Complement Med. 2012;18:953–958. doi: 10.1089/acm.2011.0331. [DOI] [PubMed] [Google Scholar]
- 24.Mourya M, Mahajan AS, Singh NP, Jain AK. Effect of slow- and fast-breathing exercises on autonomic functions in patients with essential hypertension. J Altern Complement Med. 2009;15:711–717. doi: 10.1089/acm.2008.0609. [DOI] [PubMed] [Google Scholar]
- 25.Telles S, Raghavendra BR, Naveen KV, Manjunath NK, Kumar S, Subramanya P. Changes in autonomic variables following two meditative states described in yoga texts. J Altern Complement Med. 2013;19:35–42. doi: 10.1089/acm.2011.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cramer H. The efficacy and safety of yoga in managing hypertension. Exp Clin Endocrinol Diabetes. 2016;124:65–70. doi: 10.1055/s-0035-1565062. [DOI] [PubMed] [Google Scholar]
- 27.Coulter D. London UK: 2002. Anatomy of hatha yoga: a manual for students, teachers and practitioners, Deep Books. [Google Scholar]
- 28.Mody BS. Acute effects of Surya Namaskar on the cardiovascular & metabolic system. J Bodyw Mov Ther. 2011;15:343–347. doi: 10.1016/j.jbmt.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Millar PJ, Paashuis A, McCartney N. Isometric handgrip effects on hypertension. Current Hypertension Reviews. 2009;5:54–60. [Google Scholar]
- 30.Brook RD, Appel LJ, Rubenfire M, et al. Beyond medications and diet: Alternative approaches to lowering blood pressure. Hypertension. 2013;61:1360–1383. doi: 10.1161/HYP.0b013e318293645f. [DOI] [PubMed] [Google Scholar]
- 31.Fagard RH, Cornelissen VA. Effect of exercise on blood pressure control in hypertensive patients. Eur J Cardiovasc Prev Rehabil. 2007;14:12–17. doi: 10.1097/HJR.0b013e3280128bbb. [DOI] [PubMed] [Google Scholar]
- 32.Cramer H, Ward L, Steel A, Lauche R, Dobos G, Zhang Y. Prevalence, patterns, and predictors of yoga use: results of a US. nationally representative survey. Am J Prev Med. 2016;50:230–235. doi: 10.1016/j.amepre.2015.07.037. [DOI] [PubMed] [Google Scholar]
- E1.Streiner DL. The lesser of 2 evils: the ethics of placebo-controlled trials. Can J Psychiatry. 2008;53:430–432. doi: 10.1177/070674370805300705. [DOI] [PubMed] [Google Scholar]
- E2.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- E3.Zigmond A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- E4.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36) I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- E5.Wagner P, Singer R. Ein Fragebogen zur Erfassung der habituellen körperlichen Aktivität verschiedener Bevölkerungsgruppen. Sportwissenschaft. 2003;33:383–397. [Google Scholar]
- E6.Thompson FE, Kipnis V, Subar AF, et al. Evaluation of 2 brief instruments and a food-frequency questionnaire to estimate daily number of servings of fruit and vegetables. Am J Clin Nutr. 2000;71:1503–1510. doi: 10.1093/ajcn/71.6.1503. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eSUPPLEMENT
Methods
Interventions
This trial compared the efficacy of two different yoga interventions, with or without yoga postures, in patients with arterial hypertension who were being treated with antihypertensive medication. While the interpretation of significant intergroup differences between two active interventions is unproblematic, nonsignificant results are open to potentially various and contradictory interpretations: they can be viewed as showing that the two interventions are similarly effective, ineffective, or even harmful (e1). To counter this possible ambiguity, the inclusion of an additional, inert study arm is generally recommended when comparing active interventions (e1). Accordingly, we included a third arm comprising an untreated control group in this trial.
Yoga
The two interventions were developed by an expert panel made up of seven certified and experienced yoga instructors representing various yoga traditions, based on earlier studies, classic yoga texts, and their own clinical experience. The committee members planned the interventions in such a way that they combined elements from various traditions and thus did not follow any particular “school” of yoga. The interventions were also adapted to the specific needs, potentials, and limitations of patients with arterial hypertension. The yoga instructors introduced all exercises gently at first, then increased their intensity in the course of the program. Aids (blocks, belts, or blankets) were used if necessary, and/or the exercises were modified for individual patients. Details of the two interventions can be found in eTables 2 and 3.
Outcome measures
The secondary outcome measures included 24-h heart rate and diurnal and nocturnal blood pressure, measured using a monitoring device. The parameters were categorized on the basis of the sleeping and waking times reported by the respective patients.
Further secondary outcome measures were defined a priori. They comprised:
The following questionnaires were used to survey these parameters, respectively:
Further variables were documented for evaluation in mediator analyses to investigate potential mechanisms of action of yoga in patients with arterial hypertension:
Because these variables did not serve to verify efficacy, they are not reported in this article.
Before randomization, the patients included in the study were assessed with regard to their expectations of the two interventions and of waiting for treatment in the control group. To this end, they stated their expectations on an 11-point Likert scale from 0 = ineffective to 10 = very effective. The later analysis considered only the expectation for the intervention to which the patient was then randomized.
Results
Adherence
During the first 12 weeks of the study the patients in the intervention group with yoga postures took part in 8.3 ± 3.3 (mean ± standard deviation) (68.3%) of the weekly yoga sessions and spent a further 105.2 ± 51.3 min doing their exercises at home. The participants in the intervention group without yoga postures visited 8.4 ± 3.3 (70.0%) of the sessions and spent 67.2 ± 54.3 min doing the exercises at home.
After the end of the interventions, from week 13 to week 28 of the study, 14 of the 20 patients from the group with yoga postures for whom this information was available (70%) continued to practice yoga, compared with 12 of 22 (54.5%) for the group without yoga postures. On average the participants from the group with yoga postures exercised 2.6 ± 1.6 times per week for a total of 55.8 ± 87.2 min, while those in the group without yoga postures performed their exercises times 2.2 ± 1.9 times per week for a total of 25.0 ± 38.8 min.
When only the participants who continued to practice yoga after the end of the interventions were included in analysis, those in the group with yoga postures did their exercises for 87.7 ± 96.2 min per week and those in the group without yoga postures for 50.0 ± 42.2 min per week.
Considering only those patients who continued the exercises after the end of the interventions, there was no difference between the groups with regard to systolic blood pressure (p = 0.439) or diastolic blood pressure (p = 0.452; eTable 4). There was also no significant difference between the groups in this respect when only those who had not continued practicing yoga were included (etable 5).
Antihypertensive medication
Most patients were treated with ACE inhibitors and AT1-receptor blockers (table). In the course of the study, 19 of the 23 patients in the intervention group with yoga postures for whom this information was available (82.6%) did not change their medication, three (13.0%) increased it, and one patient (4.3%) reduced his/her dose. In the intervention group without yoga postures, the medication intake remained the same in 19 of 24 patients (79.2%), increased in two (8.3%), and decreased in three patients (12.5%). In the control group, 21 of 23 patients (91.3%) did not change their medication, two (8.7%) increased it, and none decreased it. The distribution of patients in whom the medication intake remained the same, increased, or decreased did not differ significantly among the three study groups (chi-square test, p = 0.425).
Ambulatory blood pressure measurement
In week 1, an average of 73.3 ± 5.5 individual measurements were made per patient during the 24-h period of blood pressure monitoring. Of this total, an average of 60.4 ± 9.3 measurements were correct and could be used to calculate the 24-h blood pressure. The corresponding figures in weeks 12 and 28 were 73.7 ± 7.7 (57.6 ± 13.1 correct per patient) and 74.9 ± 4.8 (60.0 ± 11.9 correct), respectively.
The numbers of patients with normal blood pressure, prehypertension, and hypertension grade 1 or 2 (based on the 24-h monitoring) at weeks 1, 12, and 28 are shown in eTable 6. At week 12, four patients in the intervention group with yoga postures, six in the intervention group without yoga postures, and four in the control group switched to a lower blood pressure category (number needed to treat for the comparison yoga without yoga postures versus control group = 12.5). At week 28, nine patients in the group with yoga postures, four in the group without yoga postures, and six in the control group switched to a lower blood pressure category (number needed to treat for the comparison yoga with yoga postures versus control group = 12.5).
With regard to further ambulatory blood pressure measurements, all significant difference among the groups are reported in the following. The remaining group differences did not attain significance and are shown in detail in eTable 1. At 12 weeks the diurnal systolic blood pressure was significantly lower in the intervention group without yoga postures than in the control group (p = 0.045) and the yoga group with yoga postures (p = 0.042; eTable 1). At 28 weeks, in contrast, the diurnal systolic blood pressure in the yoga group with yoga postures was significantly lower than in the control group (p = 0.023) and the yoga group without yoga postures (p = 0.030; eTable 1). For heart rate measurements, significant intergroup differences were only observed at 28 weeks. At this time the nocturnal heart rate was significantly lower in the group with yoga postures than in either of the other groups (etable 1).
Questionnaires
Significant group differences were found in none of the outcome measures surveyed by means of questionnaires, with the sole exception of the SF-36 mental quality of life, which was significantly better among the participants in the group with yoga postures than in the group without yoga postures at week 28 (p = 0.028; eTable 7). No other differences among the groups were found at any time.
Safety
The adverse events registered in the intervention group with yoga postures were as follows:
The following adverse events occurred in the yoga group without yoga postures:
The adverse events recorded in the control group were:
None of the adverse events had a direct temporal relation with the respective study intervention. After careful assessment, none of the events was judged to be associated with the intervention.
Subjective stress
Anxiety and depression
Physical and mental quality of life.
The German 10-question version of the Perceived Stress Scale (e2)
The German version of the Hospital Anxiety and Depression Scale (e3)
The German version of the Short Form-36 Health Survey Questionnaire (SF-36) (e4).
Physical activity, surveyed by means of the Baecke Questionnaire (e5)
Nutritional habits, using the Five a Day Food Frequency Questionnaire (e6).
Headache (n = 3)
Shoulder pain (n = 1)
Knee pain (n = 1)
Tendinitis (n = 1)
Meniscus rupture (n = 1)
Knee injury from bicycle accident (n = 1)
Prolapsed intervertebral disc (n = 1)
Influenza (n = 2)
Parodontitis (n = 1)
Hypertensive emergency (n = 1)
Mental problems (n = 1)
Breast operation (n = 1)
Influenza (n = 1)
Parodontitis (n = 1)
Tinnitus (n = 1)
Autoimmune disease (n = 1)
Knee pain (n = 1)
Headache (n = 1)
Neck pain (n = 1)
Sleep disturbances (n = 1)
Kidney disease (n = 1)