Abstract
Objective To demonstrate use of the electronic health record (EHR) for health insurance surveillance and identify factors associated with lack of coverage.
Materials and Methods Using EHR data, we conducted a retrospective, longitudinal cohort study of adult patients ( n = 279 654) within a national network of community health centers during a 2-year period (2012–2013).
Results Factors associated with higher odds of being uninsured (vs Medicaid-insured) included: male gender, age >25 years, Hispanic ethnicity, income above the federal poverty level, and rural residence ( P < .01 for all). Among patients with no insurance at their initial visit ( n = 114 000), 50% remained uninsured for every subsequent visit.
Discussion During the 2 years prior to 2014, many patients utilizing community health centers were unable to maintain stable health insurance coverage.
Conclusion As patients gain access to health insurance under the Affordable Care Act, the EHR provides a novel approach to help track coverage and support vulnerable patients in gaining and maintaining coverage.
Keywords: electronic health records, health insurance, community health centers, health services accessibility, Patient Protection and Affordable Care Act
OBJECTIVE
Many low-income adults cannot afford commercial health insurance and have historically had difficulty obtaining public coverage. 1,2 For those able to gain coverage, health insurance retention is often challenging. 3 For example, patients report barriers to stable insurance coverage, including uncertainty about coverage status and current eligibility. 4,5 With new opportunities for coverage available under the Affordable Care Act (ACA), including Medicaid expansions and health insurance exchanges, 3,6–9 many Americans have new opportunities to obtain health insurance. Since even short gaps in coverage can negatively impact health, 10–12 stability of coverage will be critical to improving health outcomes. 13,14 Still, current insurance monitoring strategies are limited to self-reporting, which is subject to bias, or claims data, which excludes uninsured visits.
The electronic health record (EHR) revolutionized clinics’ capacity for monitoring and improving the health of their patients. Monitoring population health metrics is now the norm and the expectation for patient-centered medical facilities. 15,16 Among the pediatric population, the EHR has been used to conduct health insurance surveillance to promote enrollment and retention in the Children’s Health Insurance Program and other public programs. 17–22 As the ACA facilitates public coverage expansions for adults, patients at community health centers (CHCs)—many of whom have traditionally been uninsured—will likely have new insurance options. Thus, we selected the CHC setting to demonstrate the use of the EHR for insurance surveillance among a vulnerable population of patients. We aimed to (1) use the EHR to assess ‘baseline’ health insurance status among adult patients in a national network of safety net clinics during the two years prior to implementation of new ACA coverage options and (2) identify characteristics associated with a lack of coverage that could be used by clinics to identify patients most likely to benefit from health insurance outreach and support.
MATERIALS AND METHODS
We conducted a retrospective, longitudinal cohort study of adult patients receiving primary care at 122 CHCs across seven states during a two-year study period (January 1, 2012 to December 31, 2013). Participating CHCs were members of OCHIN, Inc.—originally called “Oregon Community Health Information Network” and renamed “OCHIN” as other states joined. OCHIN is a nonprofit organization that provides a fully hosted instance of Epic Systems® practice management system (PMS) and EHR to safety net clinics. 23,24 PMS and EHR data are managed centrally at OCHIN, including regular validation and cleaning. Data for these analyses were extracted at OCHIN.
Study population
Clinics were included if they had implemented OCHIN’s Epic Systems® PMS by the beginning of the study period. We included all living adult patients (aged 19–64 years) with at least one primary care office visit to an OCHIN clinic during the study period. We excluded patients who had unknown gender ( N = 13), or were pregnant ( N = 18 315) during the study period. A total of 279 654 patients met inclusion criteria. These patients had a combined total of 1 189 933 primary care office visits.
Variables
We obtained EHR data for each patient, including demographic characteristics routinely collected during registration and clinic information such as location and health center affiliation. Based on the Aday and Andersen behavioral model, 25 previous findings, 26,27 and available data, we selected the following covariates as potentially influencing insurance coverage and healthcare utilization: gender, age, race, ethnicity, language, income, and clinic location. We used the EHR to identify each patient’s insurance status for every visit during the study period. We measured utilization by calculating total number of visits per person throughout the study period.
Health insurance status was the primary dependent variable and was categorized as uninsured , Medicaid , commercial , or other (including worker’s compensation, motor vehicle accident insurance, and grant programs providing limited services such as breast and cervical cancer screening or contraceptive care). If a patient had more than one insurer, only the primary insurance was included in the analyses. Complex longitudinal coverage patterns were classified hierarchically using methods published previously. 19
Analyses
We described our patient population, evaluated the distribution of visit frequency during the study period, and examined longitudinal changes in health insurance. We analyzed the relationship between being uninsured (vs Medicaid or commercial insurance) and the covariates of interest using generalized estimating equation (GEE) logistic regression models to account for multiple visits nested within patients. A robust sandwich estimator was applied to account for possible misspecification of the correlation structure. All analyses were conducted using SAS software, Version 9.4 (SAS Institute Inc., Cary, NC, USA). This study was approved by the Institutional Review Board at our academic institution.
RESULTS
There were 279 654 adults in the study population who had at least one primary care office visit during the study period. Significant differences in insurance status ( P < .01) were seen for all demographic characteristics among this population ( Table 1 ).
Table 1:
Population characteristics, 2012–2013
| Covariate | Population % | Study population by insurance status at initial visit % | P | |||
|---|---|---|---|---|---|---|
| Uninsured | Medicaid | Commercial | Other a | |||
| N = 279 654 | N = 114 000 | N = 109 431 | N = 45 522 | N = 10 701 | ||
| Gender | <0.01 | |||||
| Male | 41.7 | 46.0 | 33.4 | 17.4 | 3.2 | |
| Female | 58.3 | 37.0 | 43.2 | 15.5 | 4.3 | |
| Age b (years) | <0.01 | |||||
| 19–25 | 17.6 | 37.1 | 42.8 | 14.6 | 5.5 | |
| 26–34 | 23.7 | 40.1 | 43.1 | 13.0 | 3.8 | |
| 35–44 | 22.9 | 43.2 | 38.1 | 15.6 | 3.0 | |
| 45–54 | 22.3 | 42.6 | 36.0 | 17.8 | 3.7 | |
| 55–63 | 13.5 | 39.5 | 34.2 | 22.9 | 3.4 | |
| Race/ethnicity | <0.01 | |||||
| White, Non-Hispanic | 55.2 | 34.8 | 38.8 | 20.9 | 5.5 | |
| Non-white, Non-Hispanic | 16.9 | 46.0 | 40.4 | 12.4 | 1.3 | |
| Hispanic/Latino | 26.3 | 50.2 | 39.1 | 8.8 | 1.9 | |
| Unknown | 1.6 | 38.4 | 36.4 | 19.1 | 6.1 | |
| Preferred language | <0.01 | |||||
| English | 77.6 | 36.9 | 40.1 | 18.6 | 4.4 | |
| Spanish | 18.3 | 57.8 | 33.7 | 7.2 | 1.4 | |
| Other | 2.7 | 33.9 | 59.6 | 5.6 | 1.0 | |
| Unknown | 1.5 | 47.9 | 17.7 | 25.4 | 9.0 | |
| Income | <0.01 | |||||
| >100% FPL | 29.0 | 46.2 | 22.9 | 27.2 | 3.7 | |
| At or below 100% FPL | 56.6 | 44.5 | 45.9 | 6.5 | 3.0 | |
| Missing | 14.4 | 15.0 | 44.4 | 33.3 | 7.3 | |
| Health center location c | <0.01 | |||||
| Rural | 4.6 | 37.3 | 21.9 | 36.9 | 4.0 | |
| Urban | 95.4 | 40.9 | 40.0 | 15.3 | 3.8 | |
FPL: federal poverty level
a For example: worker’s compensation, motor vehicle insurance, and grant programs providing limited services such as cervical cancer screening
b Age at initial visit during the study period
c Defined by 2010 census methodology based on geocoded clinic address
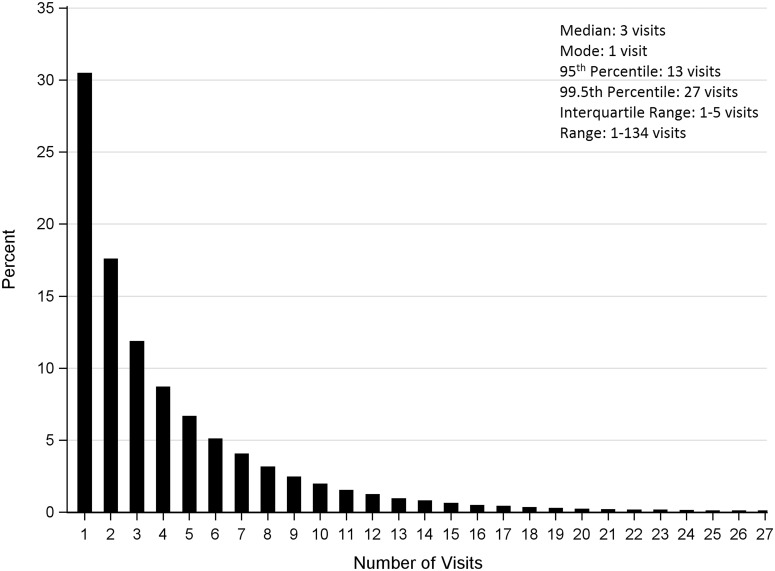
The cohort had a total of 1 189 933 clinic visits during the 2-year study period. Over half of patients had three or fewer visits (median: 3; interquartile range [IQR: 1–5]), with a range of 1–134 visits ( Figure 1 ).
Figure 1:
Distribution of OCHIN primary care clinic visits per person, 2012–2013 (total no. of visits = 1 189 933).
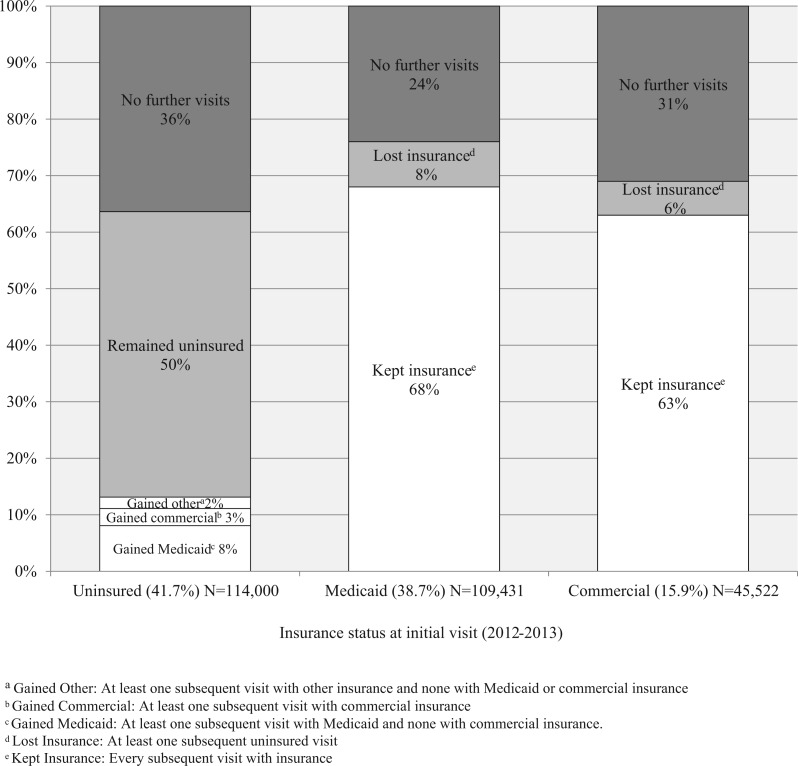
Of the 114 000 patients with no insurance at their first visit, 50% were uninsured at all subsequent visits during the study period, 13% gained insurance, and 36% had no further visits. Among patients with Medicaid or commercial insurance at their first visit, the majority remained insured at every subsequent visit, few lost insurance, and 24% and 31%, respectively, had no further visits ( Figure 2 ).
Figure 2.
Longitudinal assessment of insurance status over 2 years, 2012–2013. a Gained Other: At least one subsequent visit with other insurance and none with Medicaid or commercial insurance b Gained Commercial: At least one subsequent visit with commercial insurance c Gained Medicaid: At least one subsequent visit with Medicaid and none with commercial insurance d Lost Insurance: At least one subsequent uninsured visit e Kept Insurance: Every subsequent visit with insurance
In logistic GEE modeling of uninsured versus Medicaid-insured patients, females had lower odds of being uninsured than males (adjusted odds ratio [aOR]: 0.54, 95% confidence interval [CI], 0.53–0.55). Patients who identified as Hispanic and those who preferred Spanish language had higher odds of being uninsured than non-Hispanic whites (aOR: 1.67 [95% CI, 1.60–1.74]) and those who preferred English language (aOR: 2.59 [95% CI, 2.48–2.70]), respectively. Those who identified as non-white/non-Hispanic had slightly lower odds of being uninsured compared to non-Hispanic whites (aOR: 0.94 [95% CI, 0.91–0.97]). Patients living in rural areas had higher odds of being uninsured than those living in urban areas (aOR: 1.23 [95% CI, 1.15–1.33]). Adults living beneath the federal poverty level (FPL) had lower odds of being uninsured (aOR: 0.32 [95% CI, 0.31–0.32]) than those with >100% FPL.
Many similar patterns were seen in logistic GEE modeling of no insurance coverage versus commercial insurance, with some exceptions. Those who identified as non-white/non-Hispanic had higher odds of being uninsured compared to non-Hispanic whites (aOR: 1.38 [95% CI, 1.32–1.46]), and patients living in rural areas had lower odds of being uninsured than their urban counterparts (aOR: 0.76 [95% CI, 0.70–0.83]).
Income was not included in the model for no insurance coverage versus commercial insurance because few patients had both commercial insurance and a household income beneath the FPL.
DISCUSSION
This study demonstrates a novel method for using the EHR to elucidate coverage patterns in an adult population of CHC patients. Now that millions of adults have new access to health insurance through opportunities provided by the ACA, primary care practices can implement these strategies to support their patients in obtaining and maintaining coverage. Though current clinic processes are reactive, with insurance status verification only at the time of an appointment, 18,20–22 we are developing health information technology tools to provide population-level health insurance surveillance and outreach through the EHR. 21 Ideally, these tools will improve the quality of EHR data and provide clinics with tools to support their patients in obtaining and maintaining insurance. Insurance surveillance methods could also be used by policy-makers and community leaders wishing to partner with primary care clinics to conduct health insurance outreach and better understand patterns of insurance among certain populations or regions. 18
The EHR also allowed us to identify characteristics associated with higher odds of a patient being uninsured at a clinic visit, including: rural residence, male gender, older age, and higher income. Hispanic and Spanish-speaking sub-groups had notably higher odds of an uninsured visit compared to their non-Hispanic and English-speaking counterparts. This confirms prior studies showing high rates of uninsurance among Hispanic populations. 28,29 Surprisingly, other minority groups—patients who identified as non-white/non-Hispanic, and those who preferred languages other than English and Spanish—had lower odds of having an uninsured clinic visit than being covered by Medicaid. One hypothesis is that these other minority groups are less likely to visit the clinic when uninsured. Another possible explanation is that some minority communities (but not all) have more dedicated outreach and community engagement to ensure that uninsured patients know about safety net clinics offering care for the uninsured. For example, a high level of healthcare engagement among Hispanic communities has been shown previously. 30 Patients from rural communities also had higher odds of being uninsured compared to Medicaid-insured, but much lower odds being uninsured compared to commercially insured. This type of information could aid clinics in focusing insurance outreach efforts on patients most at risk. For example, rural patient populations could be a target for outreach in the setting of ACA Medicaid expansions and/or exchange coverage options.
It is imperative that health centers routinely document patient demographics in the EHR, which may help identify subpopulations at higher risk of being uninsured. Demographic characteristics identified in this study and other social determinants of health (e.g., employment status, education history, etc.) have been associated with an individual’s ability to access healthcare services, to comprehend healthcare advice, and to improve overall health outcomes. 31,32 Expanding inclusion of social determinants of health in the EHR could be accomplished by developing new workflows to gather data, building new data fields into the EHR, and creating linkages to other existing data sources. 33,34
Surveillance of health insurance within the OCHIN network revealed a large population of adults who accessed clinic services when they had no health insurance coverage—similar to that reported previously. 7 Further, we found approximately half of initially uninsured adults remained uninsured at every subsequent visit, which shows that CHCs provide vital healthcare access that is often difficult for uninsured patients to find. 35–39 These findings also suggest that the uninsured likely had few options for gaining health insurance coverage prior to 2014. Our estimate of patients who remained uninsured over the 2-year study period is conservative, as the large segment of uninsured patients who did not return for a second visit are likely to have remained uninsured and may have had unmet healthcare needs as a result. It is known that uninsured patients visit clinics less frequently and experience barriers to accessing other types of care including prescription medications, diagnostic and screening tests, and specialty care. 11,40–46
Limitations
The method of insurance surveillance employed in our study requires multiple healthcare visits. Because patients are less likely to seek care when they have no insurance, 47 we expect that we underestimated the prevalence of uninsurance among the study population. We also acknowledge the potential for lack of documentation or misclassification of insurance status in the EHR, as different workflows and billing practices across health centers may result in inconsistent capture of coverage information, though validity of EHR data for identifying insurance status has been demonstrated previously. 17 We used missing data categories in our statistical analyses in order to minimize exclusions (e.g., Table 2 includes variables with a ‘missing’ category to denote a lack of available information), which may have limited our understanding of the true relationships between the study covariates and insurance outcomes. For example, some of the missing demographic categories were associated with higher or lower odds of being uninsured, a finding that is difficult to interpret. Imputation methods could have been considered to address this “missingness”; however, the use of such methods with EHR data has not yet been validated.
Table 2:
Factors associated with being uninsured compared to being insured by Medicaid or commercial insurance
| Factors | Comparison group = Medicaid | Comparison group = commercial insurance | ||||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) of being uninsured | P | aOR a (95% CI) of being uninsured | P | OR (95% CI) of being uninsured | P | aOR a (95% CI) of being uninsured | P | |
| Gender | ||||||||
| Male | 1.00 | − | 1.00 | − | 1.00 | − | 1.00 | − |
| Female | 0.60 (0.59–0.61) | <0.01 | 0.54 (0.53–0.55) | <0.01 | 0.97 (0.94–1.01) | 0.14 | 0.95 (0.92–0.98) | <0.01 |
| Age (years) | ||||||||
| 19–25 | 1.00 | − | 1.00 | − | 1.00 | − | 1.00 | − |
| 26–34 | 1.07 (1.04–1.10) | <0.01 | 0.98 (0.95–1.01) | 0.13 | 1.24 (1.18–1.29) | <0.01 | 1.16 (1.12–1.21) | <0.01 |
| 35–44 | 1.26 (1.22–1.29) | <0.01 | 1.09 (1.06–1.13) | <0.01 | 1.08 (1.04–1.13) | <0.01 | 0.98 (0.94–1.02) | 0.25 |
| 45–54 | 1.27 (1.23–1.31) | <0.01 | 1.23 (1.19–1.27) | <0.01 | 1.00 (0.95–1.06) | 0.90 | 0.98 (0.93–1.03) | 0.42 |
| 55–64 | 1.29 (1.24–1.33) | <0.01 | 1.29 (1.24–1.33) | <0.01 | 0.80 (0.77–0.84) | <0.01 | 0.83 (0.79–0.87) | <0.01 |
| Race/ethnicity | ||||||||
| White, non-Hispanic | 1.00 | − | 1.00 | − | 1.00 | − | 1.00 | − |
| Hispanic | 3.10 (3.02–3.18) | <0.01 | 1.67 (1.60–1.74) | <0.01 | 2.18 (2.08–2.29) | <0.01 | 1.13 (1.07–1.19) | <0.01 |
| Non-white/non-Hispanic | 0.83 (0.80–0.86) | <0.01 | 0.94 (0.91–0.97) | <0.01 | 1.52 (1.44–1.60) | <0.01 | 1.38 (1.32–1.46) | <0.01 |
| Missing | 1.16 (1.07–1.26) | <0.01 | 1.28 (1.18–1.39) | <0.01 | 1.05 (0.96–1.14) | 0.33 | 1.05 (0.96–1.15) | 0.27 |
| Language | ||||||||
| English | 1.00 | − | 1.00 | − | 1.00 | − | 1.00 | − |
| Spanish | 3.92 (3.82–4.03) | <0.01 | 2.59 (2.48–2.70) | <0.01 | 2.80 (2.66–2.96) | <0.01 | 2.56 (2.40–2.73) | <0.01 |
| Other | 0.54 (0.51–0.57) | <0.01 | 0.56 (0.53–0.60) | <0.01 | 1.99 (1.78–2.22) | <0.01 | 1.74 (1.56–1.94) | <0.01 |
| Unknown | 2.40 (2.19–2.63) | <0.01 | 2.29 (2.08–2.52) | <0.01 | 0.71 (0.66–0.77) | <0.01 | 0.70 (0.64–0.76) | <0.01 |
| Income | ||||||||
| >100% FPL | 1.00 | − | 1.00 | − | N/A | N/A | N/A | N/A |
| At or below 100% FPL | 0.32 (0.31–0.33) | <0.01 | 0.32 (0.31–0.32) | <0.01 | N/A | N/A | N/A | N/A |
| Missing | 0.12 (0.12–0.13) | <0.01 | 0.13 (0.13–0.14) | <0.01 | N/A | N/A | N/A | N/A |
| Health center location | ||||||||
| Urban | 1.00 | − | 1.00 | − | 1.00 | − | 1.00 | − |
| Rural | 1.13 (1.06–1.22) | <0.01 | 1.23 (1.15–1.33) | <0.01 | 0.65 (0.59–0.71) | <0.01 | 0.76 (0.70–0.83) | <0.01 |
N/A = Not applicable; aOR = adjusted odd ratio; CI = confidence interval; FPL = Federal poverty level
a Multivariable generalized estimating equation models with robust sandwich estimators adjusted for covariates and exchangeable correlation structure where visits were clustered within subjects and health center was included as a fixed covariate
CONCLUSIONS
Primary care clinics have a timely and unique opportunity to utilize the EHR for health insurance surveillance and outreach, which will likely lead to improvements in patient health. In addition to using EHR data for surveillance, EHR-based tools can be developed to assist with outreach. Such health information technologies have been developed previously and their use has been demonstrated in the pediatric population. 20–22 Through data linkages, these tools can provide up-to-date insurance status information via the EHR to allow clinics to assist their patients with insurance enrollment or renewal.
SUPPORT
This work was financially supported by The National Cancer Institute of the National Institutes of Health, grant number (1 R01 CA181452 01), the Patient-Centered Outcomes Research Institute (PFA Cycle I), and the Oregon Health & Science University Department of Family Medicine.
CONFLICT OF INTEREST
The authors have no conflicts to disclose.
CONTRIBUTIONS
All authors contributed substantially to this manuscript in accordance with ICMJE standards.
TRIAL REGISTRATION
This study was registered as part of NCT02355262 at www.clinicaltrials.gov .
REFERENCES
- 1. Stuber J, Bradley E . Barriers to medicaid enrollment: who is at risk? Am J Public Health. 2003. ; 95 ( 2 ): 292 – 298 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stuber J, Maloy K, Rosenbaum S . Beyond stigma: what barriers actually affect the decisions of low-income families to enroll in Medicaid? Center for Health Services Research and Policy . Washington, DC: : The George Washington University; ; 2000. . [Google Scholar]
- 3. Sommers BD, Musco T, Finegold K, et al. . Health reform and changes in health insurance coverage in 2014 . New Engl J Med. 2014. ; 371 ( 9 ): 867 – 874 . [DOI] [PubMed] [Google Scholar]
- 4. Devoe JE, Baez A, Angier H, et al. . Insurance + access not equal to health care: typology of barriers to health care access for low-income families . Ann Fam Med. 2007. ; 5 ( 6 ): 511 – 518 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. DeVoe JE, Ray M, Graham A . Public health insurance in Oregon: underenrollment of eligible children and parental confusion about children's enrollment status . Am J Public Health. 2011. ; 101 ( 5 ): 891 – 898 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Reed M, Huang J, Graetz I, et al. . Outpatient electronic health records and the clinical care and outcomes of patients with diabetes mellitus . Ann Int Med. 2012. ; 157 ( 7 ): 482 – 489 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hawkins D, Groves D . The future role of community health centers in a changing health care landscape . J Ambulatory Care Manag. 2011. ; 34 ( 1 ): 90 – 99 . [DOI] [PubMed] [Google Scholar]
- 8. Shin P, Sharac J, Rosenbaum S, et al. . Community health centers: a 2013 profile and prospects as ACA implementation proceeds. http://kff.org/medicaid/issue-brief/community-health-centers-a-2013-profile-and-prospects-as-aca-implementation-proceeds . Published March 17, 2015. Accessed April 21, 2015 . [Google Scholar]
- 9. Sommers BD, Buchmueller T, Decker SL, et al. . The affordable care act has led to significant gains in health insurance and access to care for young adults . Health Aff. 2013. ; 32 ( 1 ): 165 – 174 . [DOI] [PubMed] [Google Scholar]
- 10. Gold R, DeVoe JE, Shah A, et al. . Insurance continuity and receipt of diabetes preventive care in a network of federally qualified health centers . Med Care. 2009. ; 47 ( 4 ): 431 – 439 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cowburn S, Carlson M, Lapidus J, et al. . Insurance continuity and human papillomavirus vaccine uptake in Oregon and California federally qualified health centers . Am J Public Health. 2014. ; 104 ( 9 ): e71 – e79 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. DeVoe JE, Graham A, Krois L, et al. . “Mind the gap” in children's health insurance coverage: Does the length of a child's coverage gap matter? Ambulatory Pediatrics. 2008. ; 8 ( 2 ): 129 – 134 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Aiken KD, Freed GL, Davis MM . When insurance status is not static: Insurance transitions of low-income children and implications for health and health care . Ambulatory Pediatrics. 2004. ; 4 ( 3 ): 237 – 243 . [DOI] [PubMed] [Google Scholar]
- 14. Gold R, DeVoe JE, McIntire PJ, et al. . Receipt of diabetes preventive care among safety net patients associated with differing levels of insurance coverage . J Am Board Fam Med. 2012. ; 25 ( 1 ): 42 – 49 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Center for Medicaid and Medicare Services . 2014 clinical quality measures. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/2014_ClinicalQualityMeasures.html . Updated July, 2014 . [Google Scholar]
- 16. Ryan A, Tompkins C . Efficiency and value in healthcare: linking cost and quality measures. National Quality Forum. www.qualityforum.org . Published November, 2014 . [Google Scholar]
- 17. Heintzman J, Marino M, Hoopes M, et al. . Supporting health insurance expansion: Do electronic health records have valid insurance verification and enrollment data? J Am Med Inform Assoc. 2015. ; 22 ( 4 ): 909 – 913 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Angier H, Likumahuwa S, Finnegan S, et al. . Using geographic information systems to identify communities in need of health insurance outreach within the OCHIN practice-based research network . J Am Board Fam Med. 2014. ; 27 ( 6 ): 804 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hatch B, Angier H, Marino M, et al. . Using electronic health records for children's health insurance surveillance . Pediatrics. 2013. ; 132 ( 6 ): e1584 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Devoe J, Angier H, Burdick T, et al. . Health information technology: an untapped resource to help keep patients insured . Ann Fam Med. 2014. ; 12 ( 6 ): 568 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. DeVoe JE, Angier H, Likumahuwa S, et al. . Use of qualitative methods and user-centered design to develop customized health information technology tools within federally qualified health centers to keep children insured . J Ambulatory Care Manag. 2014. ; 37 ( 2 ): 148 – 154 . [DOI] [PubMed] [Google Scholar]
- 22. Likumahuwa S, Angier H, Sumic A, et al. . IMPACCT kids' care: a real-world example of stakeholder involvement in comparative effectiveness research . J Comparative Effectiveness Res . 2015. ; 4 ( 4 ): 351 – 357 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. DeVoe JE, Gold R, Spofford M, et al. . Developing a network of community health centers with a common electronic health record: description of the safety net west practice-based research network (SNW-PBRN) . J Am Board Fam Med. 2011. ; 24 ( 5 ): 597 – 604 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. DeVoe JE, Sears A . The OCHIN community information network: bringing together community health centers, information technology, and data to support a patient-centered medical village . J Am Board Fam Med. 2013. ; 26 ( 3 ): 271 – 278 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Aday LA, Andersen R . A framework for the study of access to medical care . Health Services Res. 1974. ; 9 ( 3 ): 208 – 220 . [PMC free article] [PubMed] [Google Scholar]
- 26. Decker SL, Kostova D, Kenney GM, et al. . Health status, risk factors, and medical conditions among persons enrolled in Medicaid vs uninsured low-income adults potentially eligible for Medicaid under the affordable care act . JAMA. 2013. ; 309 ( 24 ): 2579 – 2586 . [DOI] [PubMed] [Google Scholar]
- 27. Decker SL, Kenney GM, Long SK . Characteristics of uninsured low-income adults in states expanding vs not expanding medicaid . JAMA Intern Med. 2014. ; 174 ( 6 ): 988 – 989 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kaiser Commission on Medicaid and the Uninsured . Health coverage for the Hispanic population today and under the Affordable Care Act. http://kaiserfamilyfoundation.files.wordpress.com/2013/04/84321 . Published April, 2013 . [Google Scholar]
- 29. Doty MM . Hispanic patients' double burden: lack of health insurance and limited English. The Commonwealth Fund. http://www.commonwealthfund.org/publications/fund-reports/2003/feb/hispanic-patients-double-burden–lack-of-health-insurance-and-limited-english. Published February, 2003 . [Google Scholar]
- 30. Franzini L, Ribble JC, Keddie AM . Understanding the Hispanic health paradox . Ethnicity Dis. 2001. ; 11 ( 3 ): 496 . [PubMed] [Google Scholar]
- 31. Galea S, Tracy M, Hoggatt KJ, et al. . Estimated deaths attributable to social factors in the United States . Am J Public Health. 2011. ; 101 ( 8 ): 1456 – 1465 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sorlie PD, Backlund E, Keller JB . US mortality by economic, demographic, and social characteristics: The national longitudinal mortality study . Am J Public Health. 1995. ; 85 ( 7 ): 949 – 956 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. IOM (Institute of Medicine) . Integrating Research And Practice: Health Systems Leaders Working Toward High Value Care . 2015. . [PubMed] [Google Scholar]
- 34. Bazemore AW, Cottrell EK, Gold R, et al. . “Community vital signs”: Incorporating geocoded social determinants into electronic records to promote patient and population health . J Am Med Inform Assoc. pii:ocv088, doi: 10.1093/jamia/ocv088 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Angier H, Hoopes M, Gold R, et al. . An early look at rates of uninsured safety net clinic visits after the Affordable Care Act . Ann Fam Med. 2015. ; 13 ( 1 ): 10 – 16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bruen BK, Ku L, Lu X, et al. . No evidence that primary care physicians offer less care to Medicaid, community health center, or uninsured patients . Health Aff. 2013. ; 32 ( 9 ): 1624 – 1630 . [DOI] [PubMed] [Google Scholar]
- 37. Berk ML, Schur CL . Access to care: How much difference does Medicaid make? Health Aff. 1998. ; 17 ( 3 ): 169 – 180 . [DOI] [PubMed] [Google Scholar]
- 38. Devoe JE, Tillotson CJ, Wallace LS, et al. . The effects of health insurance and a usual source of care on a child's receipt of health care . J Pediatric Health Care. 2012. ; 26 ( 5 ): e25 – e35 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Eisert SL, Durfee MJ, Welsh A, et al. . Changes in insurance status and access to care in an integrated safety net healthcare system . J Commun Health. 2009. ; 34 ( 2 ): 122 – 128 . [DOI] [PubMed] [Google Scholar]
- 40. Baicker K, Finkelstein A . Effects of Medicaid on clinical outcomes . New Engl J Med. 2013. ; 369 ( 6 ): 583 . [DOI] [PubMed] [Google Scholar]
- 41. Cowburn S, Carlson MJ, Lapidus JA, et al. . The association between insurance status and cervical cancer screening in community health centers: exploring the potential of electronic health records for population-level surveillance, 2008-2010 . Prevent Chronic Dis. 2013. ; 10 : E173 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Freeman JD, Kadiyala S, Bell JF, et al. . The causal effect of health insurance on utilization and outcomes in adults: a systematic review of US studies . Med Care. 2008. ; 46 ( 10 ): 1023 – 1032 . [DOI] [PubMed] [Google Scholar]
- 43. Gold R, DeVoe JE, McIntire PJ, et al. . Receipt of diabetes preventive care among safety net patients associated with differing levels of insurance coverage . J Am Board Fam Med. 2012. ; 25 ( 1 ): 42 – 49 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. DeVoe JE, Fryer GE, Phillips R, et al. . Receipt of preventive care among adults: insurance status and usual source of care . Am J Public Health. 2003. ; 93 ( 5 ): 786 – 791 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hadley J . Insurance coverage, medical care use, and short-term health changes following an unintentional injury or the onset of a chronic condition . JAMA. 2007. ; 297 ( 10 ): 1073 – 1084 . [DOI] [PubMed] [Google Scholar]
- 46. Katz MH . Health insurance is not health care . JAMA Intern Med. 2014. ; 174 ( 6 ): 859 – 860 . [DOI] [PubMed] [Google Scholar]
- 47. Freeman JD, Kadiyala S, Bell JF, et al. . The causal effect of health insurance on utilization and outcomes in adults: a systematic review of US studies . Med Care. 2008. ; 46 ( 10 ): 1023 – 1032 . [DOI] [PubMed] [Google Scholar]