Abstract
A phytobezoar is a bezoar or trapped mass in the gastrointestinal system that consists of indigestible plant material such as fibers, skins and seeds. A persimmon phytobezoar (considered to be harder than other types of phytobezoars) is formed after frequent consumption of persimmons. The complication of gastrointestinal tract obstruction from bezoars was found to exist in the intestines but was rarely reported in the gastric tract because of its flexible volume. Here we present a 57-year-old man with persimmon phytobezoars, which ultimately led to gastric outlet obstruction.
Keywords: persimmon phytobezoar, gastric outlet obstruction, surgery
Introduction
Persimmon, a tropical fruit rich in fleshy fiber, is commonly grown and consumed in certain countries [1]. The surface of persimmon contains high concentrations of persimmon tannin. Reaction between persimmon tannin and stomach polymerizes fibers and other vegetable substances and produces a persimmon phytobezoar in which cellulose, hemicelluloses and various proteins are accumulated [2]. The most common risk factors for phytobezoar formation are previous gastric surgery, poor mastication, overindulgence of food with high fiber content, diabetes mellitus complicated by gastroparesis and coexisting diseases with delayed gastric emptying [3]. Depending on the location and size, clinical manifestations of gastrointestinal bezoars can vary, such as abdominal pain, bloody or tarry stool, abdominal fullness, anemia—or even upper GI bleeding—or signs of intestinal obstruction due to large intestinal bezoars [4,5]. Gastric bezoars may frequently cause intestinal obstruction and are occasionally associated with gastric ulcer. However, it is rare presentation of gastric obstruction result from flexible gastric volume. Here we report an unusual case of gastric outlet obstruction caused by multiple giant persimmon phytobezoars.
Case presentation
A 57-year-old man with intermittent mild abdominal pain, abdominal mass and frequent vomiting was admitted to the emergency room of the Mayang Traditional Medical Hospital. The site with intermittent mild pain was located in the left upper quadrant. In addition, a left upper quadrant abdominal mass was palpable half a year before the admission. The patient also claimed that he felt the mass increase gradually. All of these symptoms did not catch enough attention for the patient to seek medical treatment. Three days before admission, the patient started vomiting immediately after a normal or semiliquid diet, but the symptom of vomiting could be relieved while lying in the left lateral position.
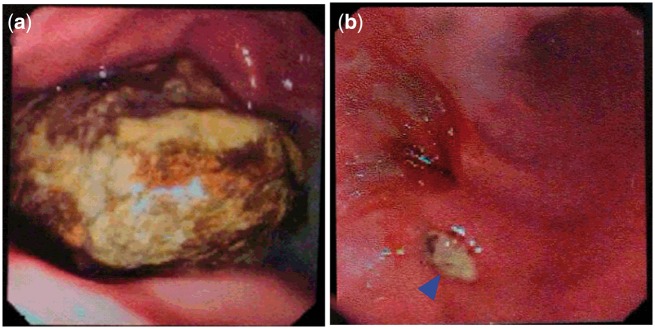
Upon physical examination, the patient was emaciated with a low body mass index (16.2). Slight distension and moderate tenderness were noted in the upper abdomen. A giant mass was present in upper quadrant abdominal, and the mass was firm, mobile and elliptical. Esophagogastroduodenoscopy (EGD) revealed multiple yellow, tough, round bezoars with irregular surfaces in the stomach (the largest being 8 × 5 × 5 cm), and several ulcers up to 3 cm in diameter were found. Moreover, the endoscope could not enter the duodenum after several attempts due to pylorus obstruction from phytobezoars (Figure 1). Except for a positive diagnosis of Helicobacter pylori , other laboratory test results were all normal.
Figure 1.
Esophagogastroduodenoscopy (EGD) findings. (a) A persimmon phytobezoar obstructed the pylorus and endoscope could not enter into the duodenum; (b) Several ulcers (blue arrow) up to 3 cm in diameter were found
During an interview about his dietary habits, the patient reported that he had consumed five or more persimmons per week during the last three months. The following day, the patient underwent emergency gastrostomy with removal of three large persimmon phytobezoars. We confirmed gastric outlet obstruction during the operation and cleared it. The largest phytobezoar could not be removed as a whole piece (Figure 2). Postoperatively, the patient recovered well and was started on total enteral nutrition. H pylori eradication was performed after the patient was discharged.
Figure 2.
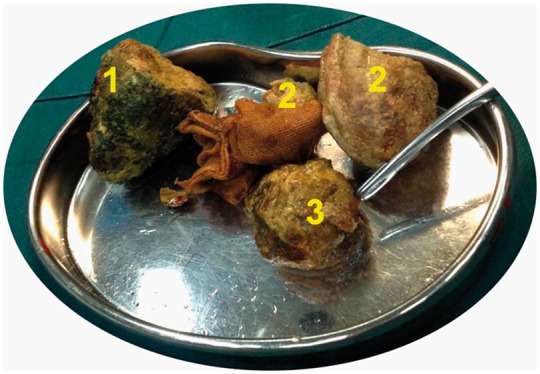
All persimmon phytobezoars of the patient were removed
Discussion
Bezoar, an indigestible conglomeration trapped in the gastrointestinal tract, is a relatively rare disease entity with a variable incidence among studies [6]. Bezoars are mainly classified into four types according to their material make-up: phytobezoars, trichobezoars, pharmacobezoars and lactobezoars. Persimmon phytobezoars, a type of phytobezoar, are often formed after frequent and excessive consumption of persimmons [7]. Compared with other phytobezoars, persimmon phytobezoars are more difficult to dissolve or break up into small pieces owing to their tough consistency [8]. Previous reports have suggested that the spectra obtained from the surface and the inner parts of a persimmon phytobezoar are quite similar to that of persimmon juice [1]. The phytobezoars form as a complication of delayed gastric emptying. Predisposing risk factors include partial gastrectomy, vagotomy and pyloroplasty, peptic ulcer disease, chronic gastritis, Crohn’s disease and carcinoma of the gastrointestinal tract. The patient in our report harbored high risk factors including H pylori infection and chronic erosive gastritis.
The clinical manifestations of persimmon phytobezoars are similar to other phytobezoars and hinge on the localization and size of the phytobezoars. The most frequent symptoms of phytobezoars in the stomach are dyspepsia, abdominal pain and vomiting or nausea. However, symptoms such as upper gastrointestinal bleeding, intestinal obstruction and gastric outlet obstruction are rather uncommon [9]. It is obvious that our patient had existing gastric outlet obstruction with the symptom of emesis immediately after intake of non-liquid food; the obstruction was certified by EGD and the surgical procedure. Interestingly, symptoms of obstruction in the patient could be relieved when lying in the left lateral position. The possible reason was that the left lateral position could ease the pressure of persimmon phytobezoars to the pylorus so that some gastric contents could be emptied.
Current feasible treatment methods for gastric phytobezoars include dissolution of the bezoar by Coca-Cola (or chemical drugs) and endoscopic surgery. It has been indicated that persimmon phytobezoars were often resistant to chemical dissolution. Due to its specific challenge, endoscopic removal is often difficult and incomplete. Moreover, it has been reported that a case of intestinal obstruction was caused by a phytobezoar after chemical dissolution for a large gastric phytobezoar [10]. Combining the patient’s special food history with EGD presentation, the diagnosis of gastric outlet obstruction is apparent. Emergency surgery was then carried out because gastric outlet obstruction would result in serious complications such as malnutrition, water-electrolyte imbalance and acid-base imbalance without urgent treatment, [11]. The phytobezoars were then completely removed by laparotomy. While it is apparent from the previous reports that nonsurgical treatment is safe and effective for phytobezoars, surgery— which can avoid the development of serious complications—should be considered for multiple giant phytobezoars with gastric outlet obstruction.
Conflict of interest statement: none declared.
References
- 1. Iwamuro M, Okada H, Matsueda K et al. Review of the diagnosis and management of gastrointestinal bezoars. World J Gastrointest Endosc 2015;7:336–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ertugrul G, Coskun M, Sevinc M et al. A rare cause of gastrointestinal phytobezoars: diospyros lotus. World J Emerg Surg 2012;7:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee J. Bezoars and foreign bodies of the stomach. Gastrointest Endosc Clin N Am 1996; 6:605–19. [PubMed] [Google Scholar]
- 4. Cheng Y, Song W. Efficacy of FOLFOXIRI versus XELOXIRI plus bevacizumab in the treatment of metastatic colorectal cancer. Int J Clin Exp Med 2015; 8:18713–20. [PMC free article] [PubMed] [Google Scholar]
- 5. Kurguzov OP. Bezoars as a cause for acute small intestinal obstruction. Khirurgiia (Mosk) 2004;(12):18–21(in Russian). [PubMed] [Google Scholar]
- 6. Uchida K. Letter: Coca-Cola can dissolve gastric phytobezoars. Aliment Pharmacol Ther 2013;37:842–3. [DOI] [PubMed] [Google Scholar]
- 7. Krausz MM, Moriel EZ, Ayalon A et al. Surgical aspects of gastrointestinal persimmon phytobezoar treatment. Am J Surg 1986;152:526–30. [DOI] [PubMed] [Google Scholar]
- 8. Iwamuro M, Urata H, Furutani M et al. Ultrastructural analysis of a gastric persimmon phytobezoar. Clin Res Hepatol Gastroenterol 2014;38:e85–7. [DOI] [PubMed] [Google Scholar]
- 9. Kaplan O, Klausner JM, Lelcuk S et al. Persimmon bezoars as a cause of intestinal obstruction: pitfalls in their surgical management. Br J Surg 1985;72:242–3. [DOI] [PubMed] [Google Scholar]
- 10. Ha SS, Lee HS, Jung MK et al. Acute intestinal obstruction caused by a persimmon phytobezoar after dissolution therapy with Coca-Cola. Korean J Int Med 2007;22:300–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mohammed AA, Benmousa A, Almeghaiseeb I et al. Gastric outlet obstruction. Hepatogastroenterology 2007;54:2415–20. [PubMed] [Google Scholar]