Abstract
Gene electrotransfer (GET) enhances delivery of DNA vaccines by increasing both gene expression and immune responses. Our lab has developed the multi-electrode array (MEA) for DNA delivery to skin. The MEA was used at constant pulse duration (150 ms) and frequency (6.67 Hz). In this study, delivery parameters including applied voltage (5–45 V), amount of plasmid (100–300 μg), and number of treatments (2−3) were evaluated for delivery of a DNA vaccine. Mice were intradermally injected with plasmid expressing Bacillus anthracis protective antigen with or without GET and αPA serum titers measured. Within this experiment no significant differences were noted in antibody levels from varying dose or treatment number. However, significant differences were measured from applied voltages of 25 and 35 V. These voltages generated antibody levels between 20,000 and 25,000. Serum from animals vaccinated with these conditions also resulted in toxin neutralization in 40–60% of animals. Visual damage was noted at MEA conditions of 40 V. No damage was noted either visually or histologically from conditions of 35 V or below. These results reflect the importance of establishing appropriate electrical parameters and the potential for the MEA in noninvasive DNA vaccination against B. anthracis.
Keywords: Gene electrotransfer, DNA vaccination, Electroporation, Anthrax, Bacillus anthracis
1. Introduction
DNA vaccines are becoming an increasingly used tool for the development of novel vaccines. Advantages of DNA vaccines over recombinant protein and viral vaccines include: ease of production and storage, as well as biological stability. Original DNA vaccine studies were conducted against HIV [1] and HBV [2] using direct injection of DNA. While these studies demonstrated the ability of DNA vaccines to induce an immune response, results were low. Techniques for increasing DNA delivery have been evaluated to enhance gene expression. One of these methods is GET.
GET enhances entry of molecules into the cell through the application of electrical pulses. It has been shown to augment both gene expression and immune responses. GET delivered DNA vaccines have been shown to induce immune responses against a variety of infectious agents including but not limited to: Human Immunodeficiency virus (HIV) [3–6], Hepatitis B virus (HBV) [3,7,8], Influenza [9–13], Bacillus anthracis [14,15]. Most GET mediated DNA vaccines have been injected into the muscle. While muscle is a desirable target for obtaining long term expression [16], the pain associated with needle penetration is undesirable for vaccine technologies. This limitation can be overcome by delivering to the skin. The skin is an advantageous vaccine delivery target because it provides a large and superficial surface as well as having natural antigen presenting properties. Our lab developed a GET delivery device specifically for non-invasive GET delivery to the skin known as the MEA [17].
The MEA is a 4 × 4 (16) electrode array with 2 mm spacing between electrodes. Our previous publications have demonstrated that the MEA can enhance gene expression [18,19] and stimulate humoral immunity in vivo [20]. The MEA has been shown to cause minimal to no tissue damage in a human-like guinea pig skin model [19].
The organism selected for evaluation of the MEA in DNA vaccine was B. anthracis. B. anthracis is a gram positive spore forming rod-shaped bacterium. The Centers for Disease Control and Prevention classify B. anthracis as a category A agent because “it can be easily disseminated or transmitted from person to person, causes a high mortality rate and public health impact, may cause panic and social disruption, and requires special action for public health preparedness.” The current available vaccine, Biothrax®, is an aluminum adjuvant bacterial cell free filtrate protein vaccine delivered intramuscularly in a 5 regimen dose over the course of 18 months. Following this series, annual boosters are recommended [21]. Side effects have been noted in approximately one-third of vaccinated individuals including: injection site swelling, redness, and tenderness [22,23]. The primary component of this vaccine is a toxin associated protein called PA [24]. PA is involved in the formation of two toxins: edema and lethal toxin [25]. Lethal toxin, the more damaging of the two, causes a disruption in the Mitogen-activated protein kinase kinase pathway leading to cell death [26]. Research has demonstrated that some antibodies formed against PA can prevent toxin formation which is a critical component of vaccine development [27,28]. For this reason most research conducted for the formulation of novel B. anthracis vaccines has utilized PA as a target.
The goal of this study was to identify appropriate and critical delivery parameters using the MEA for the induction of humoral immunity against B. anthracis.
2. Materials and methods
2.1. Animals and injections
All animal studies were conducted with approval from the Institutional Animal and Care Use Committee. 6–8 week old female Balb/c mice were injected either intradermally at two sites on the left flank, or intramuscularly at one site with 50 μl of plasmid. Experimental mice were boosted either once or twice 14 days after the previous treatment (Day 14, Day 28). Mice were bled by tail vein at various time-points. All animals were anesthetized with 2–3% isoflurane + O2 for treatments. These experiments were performed at Eastern Virginia Medical School and Old Dominion University.
2.2. Plasmids
The plasmids used for these experiments were pSecTagPA and pCMVER/PA at various concentrations for B. anthracis studies. The plasmid backbones are commercially available from Invitrogen and are constructed to generate secreted forms (pSecTagPA) and membrane bound forms (pCMVER/PA) of PA. Both PA plasmids were constructed [29] and generously donated by Dr. Ulrike K Hahn (University of Hohenheim, Stuttgart, Germany). pSecTagPA and pCMVER/PA were used together in all experiments, mixed at a 1:1 ratio, with a final concentration of 2 mg/ml and noted here as pPA [30]. Reporter assays were done using pGwizLuc (Aldevron, Fargo, ND) also at 2 mg/ml.
2.3. Delivery by GET with the MEA
The MEA was used at applied voltages ranging from 5 to 45 V (25–45 V) but always maintained at a constant pulse duration (t_p) of 150 ms and frequency (f) = 6.67 Hz. Eight pulses were applied to each of 9 squares with a constant 2 mm gap. The eight pulses were applied 4 at a time in perpendicular directions as described in Heller et al.[17] for a total of 72 pulses (p). Electrodes were circular, gold plated and flat at the end with a 0.2 mm in diameter. The Four Plate Electrode (4PE) consists of four plates aligned in a 6 mm square. The 4PE was used at 60 V and a t_p = 150 ms and f = 6.67 Hz based on previous results [31]. The four needle electrode is used intramuscularly in the gastrocnemius.
2.4. In vivo bioluminescent imaging
The Caliper life sciences IVIS Spectrum was used for live animal bioluminescent imaging. Animals were injected i.p. with 15 mg/ml luciferin. 20 min post-luciferin injection the animals were imaged and relative light units measured. All luciferase data are represented as average total flux (photons/s) per injection site.
2.5. Histology
Skin samples were taken from mice 48 h after treatment and fixed in formalin for histological analysis. Mouse skin 6–8 mm in diameter, was collected and snap frozen in OCT on dry ice. Skin sections were sectioned to 7 μm on a cryostat at −22°C and placed on slides. Hematoxylin & Eosin staining was performed to assess inflammation and damage.
2.6. Indirect ELISA for the determination of antibodies
Briefly, antigen was coated with 100 μl of PA at 0.1 mg/ml and incubated overnight at 4°C. Plates were blocked with 5% skim milk buffer for 2 h at 37°C. Samples were diluted in blocking buffer and incubated for 1 h at 37°C. HRP conjugated Secondary antibodies (Santa Cruz) were diluted in blocking buffer to working concentration and added for 30 to 60 min in the dark. Research and Development (R&D) Systems substrate reagent (DY999) was added for 10 min and stopped with 2 NH2SO4. Plates were read at 450 nm and results represented as Anti-PA Serum titers, reciprocal (1/x) of the highest serum dilution above background (where x = 1:final dilution).
2.7. TNA
J774A.1 murine macrophages (ATCC) were cultured in DMEM media supplemented with 5% FBS, 10 mM HEPES buffer, and Pen-Strep. 50,000 cells/well were plated in 96 well cell culture plates. The following day, serum was diluted starting at 1:50 in media and incubated for 1 h with 100 ng/ml protective antigen. Lethal Factor was added to the Serum/PA mix at a final concentration of 80 ng/ml. Media was removed from the cells and the serum/PA/LF mix was added to the macrophages for 4 h at 37°C and 5% CO2. All plates contained a titration curve to confirm that the concentration of toxin used was sufficient to cause 95% cell death. Following the 4 hour incubation an MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay was performed to determine cell viability.
2.8. Statistical analysis
For reporter experiments, luciferase is expressed as average total flux. Antibody titers are reflected as average serum titers. In all experiments, error is reflected as standard deviation. ANOVA was performed to compare groups within experiments to determine significance, where p < 0.05.
3. Results and discussion
3.1. Luciferase gene expression from intradermal GET with the MEA in Balb/c mice
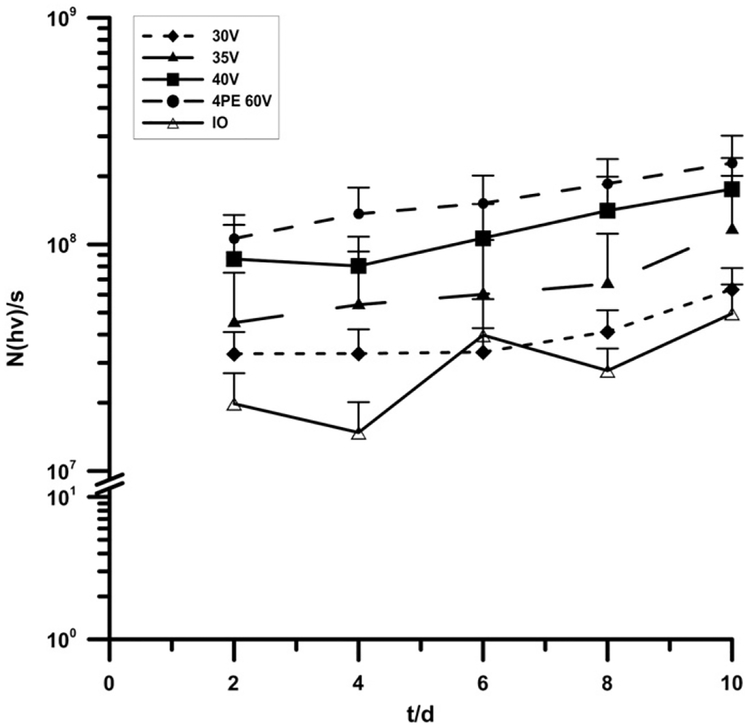
In order to assess the ability of the MEA to enhance gene expression in a mouse model, Balb/c mice were injected with 50 μl of GwizLuc (2 mg/ml) plasmid intradermally on the left flank. Sites received GET with various voltages using the MEA or 60 V with a non-invasive 4PE both with a t_p = 150 ms. A control group of IO was included as a negative control. While delivery using the 4PE resulted in higher expression, luciferase expression was also increased following delivery with the MEA compared to IO. Here Fig. 1 shows a voltage dependent trend, higher voltages resulted in increased luciferase expression. While not significant, all MEA conditions were found to be greater than IO and demonstrated similar expression patterns as the 4PE animals over time. It should be noted that in previously published work luciferase gene expression was significantly increased using the MEA in other animal models [17–19]. This result further strengthened our hypothesis of needing to evaluate electrical parameters for induction of immunity in the mouse model. In addition, visual tissue damage was noted in animals treated with the MEA at 40 V further indicating that lower voltage conditions may be necessary.
Fig. 1.
Luciferase gene expression from intradermal electrically mediated delivery with the MEA in Balb/c mice. Mice were intradermally injected with 50 μl of GwizLuc plasmid. Negative control group (IO) did not receive GET. Positive control group (4PE) was immediately electroporated with the 4PE at 60 V and t_p = 150 ms. Experimental groups were immediately electroporated at 30 V, 35 V, or 40 V for t_p = 150 ms and 72p. Results are expressed as average total flux = N(hv)/s. n = 8. Error is represented as std dev.
3.2. Humoral immune response, as represented by total IgG production, from intradermal GET with the MEA against B. anthracis toxin protein PA
The ability of the MEA to enhance humoral immunity in a mouse model was tested by comparing the production of total IgG antibodies to other GET devices (4PE and an intramuscular four needle electrode). Both alternative GET devices have been previously optimized for gene expression. GET parameters for each electrode were: MEA 30–40 V with constant t_p = 150 ms, 4PE 60 V 150 ms, and muscle four needle 50 V 20 ms. Mice were injected as described, two sites on the left flank with 50 μl per site (2 mg/ml) for skin GET animals and 50 μl of pPA in one site in the gastrocnemius for muscle GET samples.
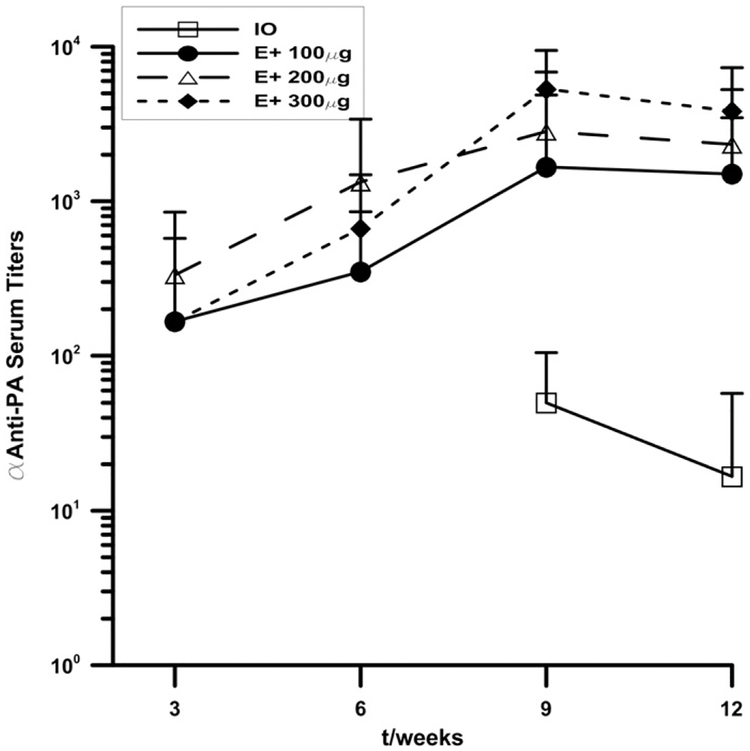
Here Fig. 2, shows that at early time points skin IO animals had slightly higher antibody titers than muscle IO groups. Though these groups were not statistically different, the trend shows slightly higher levels of antibodies. However, over time those animals that received GET, regardless of delivery tissue, rapidly increased above IO groups. Intradermal MEA groups generally increased at a steady rate over time whereas muscle GET animals peaked by week 9 and began to drop off slightly by week 12. Additionally, when comparing MEA delivered groups to 4PE delivered groups there is also a notable difference in antibody production. Despite the increased luciferase gene expression, as shown in Fig. 1 using the 4PE, MEA delivered groups produced approximately a five-fold-increase in antibody production compared to the 4PE.
Fig. 2.
Humoral immune response to PA from intradermal electrically mediated delivery with the MEA. Mice were injected with 50 μl of pPA plasmid into either the muscle (gastrocnemius) or intradermal in the left flank at two sites. Negative control groups included both muscle injection only (MIO) and skin injection only (skin IO). Electroporated groups were immediate electroporated with either the four needle muscle electrode at 60 V and t_p = 20 ms (muscle injection), the 4PE at 60 V and t_p = 150 ms (skin injection), or the MEA at 35 V and t_p = 150 ms (skin injection). Serum was collected at three week intervals and indirect ELISA used to measure αPA IgG. Results are expressed as average αPA serum titers. n = 5 and error is represented as std dev.
3.3. Evaluation of delivery parameters for DNA vaccination with the MEA against B. anthracis
Three parameters were investigated to determine the appropriate delivery conditions for MEA DNA vaccination against B. anthracis. The first was the plasmid dose injected during each treatment. The second was the number of treatments each animal was given; either a prime boost protocol (Days 0 and 14) or a prime plus two boost protocol (Days 0, 14 and 28). The final parameter was the effect of voltage. Absolute voltages from 25 to 45 V were tested to determine the effect on humoral immune induction.
3.3.1. Effect of plasmid dose on MEA mediated DNA vaccination against B. anthracis
Differing amounts of plasmid were injected to compare its effect on immune induction. Plasmid was injected at 100 μg (1 site with 50 μl at 2 mg/ml), 200 μg (two sites with 50 μl at 2 mg/ml), or 300 μg (three sites with 50 μl at 2 mg/ml) of DNA intradermally. GET conditions of 45 V and 150 ms were used for delivery at all three plasmid amounts. IO control was injected with 200 μg of plasmid. Serum was collected and antibody levels measured. Here Fig. 3 shows there were very little differences in antibody production observed. All conditions were, on average, increased above IO at all-time points. IO samples did not have detectable levels of antibodies at week 3 or 6. Anti-PA antibodies were not detectable until week 9 for this set of experiments. However, at early time points 200 μg + GET seemed to be slightly increased over 100 μg + GET and 300 μg + GET. By week 9, 300 μg had surpassed 200 μg + GET and maintained at week 12. The results obtained from this set of experiments did not generate significant differences between groups. However, the largest differences between groups occurred between weeks 3–6. Over this time 200 μg + GET represented the highest antibody response. For this reason, it was decided to continue further experimentation with a dose of 200 μg. Additionally, due to visual tissue damage seen from 40 and 45 V, these conditions were not used in further experiments.
Fig. 3.
Effect of plasmid dose on MEA mediated DNA vaccination against B. anthracis. Mice were injected with 50 μl of pPA plasmid on the left flank. Mice were injected at one, two, or three sites. Negative control injection only group (IO) received injection at two sites. Experimental groups were electroporated with the MEA at 45 V and t_p = 150 ms. Serum was collected at three week intervals and indirect ELISA used to measure anti-PA IgG. Results are expressed as average αPA serum titers (n = 5) and error is represented as std dev.
3.3.2. Effect of number of treatments on MEA mediated DNA vaccination against B. anthracis
Animals were injected with 50 μl of pPA plasmid at two sites on the left flank and GET was performed at 35 V. Two protocols were evaluated for this set of experiments to evaluate either a prime-boost or prime plus two boosts protocol. The prime-boost protocol was performed and GET was applied at Days 0 and 14, while the prime plus two boosts protocol was administered on Days 0, 14, and 28. Serum was collected at various time points and antibodies were measured and plotted over time. Similar to the results from the plasmid dosing experiments, there were no significant differences seen between either of these two conditions. However, the results did reveal that at early time-points there may be some benefit to an additional treatment. Here Fig. 4 shows that over time, the prime boost protocol achieved the same levels of antibody titers as the prime plus two boost protocol. This suggests that additional benefits from a third treatment would not be gained for prolonged immunity and would only be beneficial for short term immune responses. It should be noted that the results of this experiment only reflect multiple treatments at two week time intervals between treatments.
Fig. 4.
Effect of number of treatments on MEA mediated DNA vaccination against B. anthracis. Mice were injected with 50 μl of pPA plasmid at two sites on the left flank. Two schedules were performed with either a prime and boost (Days 0 and 14) or a prime plus two boost protocol (Days 0, 14 and 28). Negative control injection only groups were used for both prime boost (IO 2Tx) and prime plus two boost (IO 3Tx). Experimental groups were immediately electroporated for each treatment with the MEA at 35 V and t_p = 150 ms. Serum was collected at three week intervals and indirect ELISA used to measure αPA IgG. Results are expressed as average αPA serum titers (n = 5) and error is represented as std dev.
3.3.3. Effect of voltage on MEA mediated DNA vaccination against B. anthracis
The final parameter for analysis was the effect of voltage with the MEA on antibody production. Mice were injected at two sites on the left flank with 50 μl of pPA. Experimental animals underwent GET with MEA at voltages ranging from 25 to 35 V. The max voltage was limited to 35 V due to visual tissue damage seen at both 45 and 40 V in earlier studies. Here Fig. 5 shows that at week 3, 25 V generated the highest response. By week 9, significant increases of both 25 and 35 V were seen as compared to IO and 25 V was significantly greater than all other lower voltages. 15 V also showed high antibody levels but was not significant due to high standard deviation. At week 12 significant increases were again seen as compared to IO for both 25 and 35 V. Based on these results the voltage parameter generated the only significant differences between groups.
Fig. 5.
Effect of applied voltage on MEA mediated DNA vaccination against B. anthracis. Mice were injected with 50 μl of pPA plasmid at two sites on the left flank at Days 0 and 14. Negative control injection only groups (IO) did not receive GET. Experimental groups were electroporated with the MEA at 5 V, 15 V, 25 V, and 35 V at t_p = 150 ms. Serum was collected at three week intervals and indirect ELISA used to measure αPA IgG. Results are expressed as average αPA serum titers (n = 10) and error is represented as std dev. Significance was evaluated by ANOVA and differences (p < 0.05) were seen for 25 and 35 V groups at weeks 9 and 12 as compared to IO.
These results compare favorably to muscle GET studies. Two studies, one in mice [15] and one in non-human primates [14], have been conducted specifically evaluating the use of GET to deliver a B. anthracis vaccine. Our results are similar to the mouse study demonstrating serum titers of approximately 25,000 and peaking at similar time points between weeks 6 and 9. While our study required additional DNA, the use of the non-invasive MEA provides a positive advancement. The NHP study was conducted with penetrating needle electrodes into the muscle and demonstrated a high development of protective immune responses [14]. While it would be difficult to compare our results to these, we feel that their data corroborate the claim that GET could be an effective delivery method for DNA vaccination against B. anthracis. Utilizing a minimally invasive approach and reducing the potential discomfort associated with needle electrodes may potentially make this treatment more tolerable.
Given the significant increase in humoral immunity, the question remained whether a protective immune response is generated using this delivery method. Therefore, a toxin neutralization assay was performed to determine whether PA toxin formation could be inhibited by serum from MEA delivered pPA DNA vaccination at 25 and/or 35 V. For this study, serum was collected at four weeks after the second treatment and neutralization measured at a single serum dilution (1:50) for all samples. For those samples, 60% (3/5) of mice could neutralize toxin formation using the MEA at 35 V and 40% (2/5) at 25 V. IO and GET with backbone plasmid did not demonstrate any neutralizing activity. This further demonstrates that the critical factor, when utilizing the MEA is the voltage. These results are similar to work conducted with the gene gun against B. anthracis [29,30]. In that study, toxin neutralization was quite low and in several cases non-existent; however, several of these animals were protected in a lethal challenge assay. Future work developing a MEA mediated DNA vaccine would need to include these types of challenge experiments to confirm these effects.
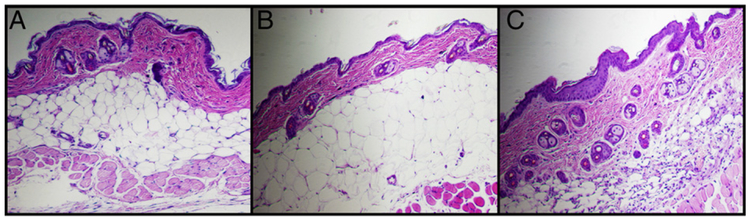
3.4. Effect of GET with the MEA on the skin
Histology was performed to evaluate skin tissue for damage at 35 V. Control animals of no treatment and IO (pPA) were included for comparison. Here Fig. 6A, no treatment, shows the appearance of normal mouse skin. When comparing IO and GET treated samples, no gross visual difference in swelling or skin damage can be seen. Here Fig. 6C GET (pPA + GET) samples shows a large influx of cellular infiltrate as well as a thickening of the epidermis as compared to the results shown in Fig. 6B in IO. Increases in cellular infiltrate may represent protective effects that are not represented by measurement of antibody responses and neutralizing activity.
Fig. 6.
Effect to the skin from electroporation with the MEA. Mice were injected with 50 μl of pPA plasmid. Negative control groups included untreated skin (A) and injection only (B). Electroporated samples (C) were performed using the MEA at 35 V and t_p = 150 ms. Images are representative of groups at 100× magnification.
4. Conclusions
In this study we have evaluated the appropriate parameters necessary for inducing humoral immunity from a MEA delivered DNA vaccine against B. anthracis. We evaluated the necessary dosage and GET conditions for the development of antibody responses and toxin neutralizing activity. Our results showed no significant differences in antibody levels from altering amount of plasmid or number of treatments; however, significant increases were noted with the MEA at particular GET voltages (25 and 35 V) as compared to IO. The results were similar to those obtained from muscle GET samples without needing to penetrate the skin during GET administration. Histological assessment of the skin showed no damage from treatment as compared to IO, but did show an increase in infiltrate which may provide additional immunity not demonstrated by antibody responses. Additionally, we demonstrated the importance of considering the desired outcome for the evaluation of electrode design. This was expressly shown where high gene expression (4PE or MEA at 40 V) did not correlate to high antibody levels. Given this information, the MEA should be considered a possible alternative to invasive GET devices when used with appropriate conditions. Future applications with the MEA should also evaluate the presence of a cellular immune response.
Acknowledgments
This research was supported in part by the Frank Reidy Research Center for Bioelectrics at Old Dominion University and the Center for Molecular Delivery at the University of South Florida. We would also like to acknowledge support from the Defense Advanced Research Projects Agency grant number HR0011–08-1–0087. The authors also wish to thank Dr. Mark Jaroszeski (University of South Florida) for construction of the MEA.
Abbreviations:
- GET
Gene electrotransfer
- MEA
Multi electrode array
- PA
Protective antigen
- ELISA
Enzyme linked immunosorbent assay
- TNA
Toxin neutralization assay
- IO
Injection alone of plasmid DNA
Footnotes
Conflict of interest
With respect to conflict of interest, Dr. R. Heller is an inventor on patents which cover the technology that was used in the work reported in this manuscript. In addition, Dr. R. Heller owns stock in Inovio Pharmaceutical Corp.
References
- [1].Wang B, Ugen KE, Srikantan V, Agadjanyan MG, Dang K, Refaeli Y, Sato AI, Boyer J, Williams WV, Weiner DB, Gene inoculation generates immune responses against human immunodeficiency virus type 1, Proc. Natl. Acad. Sci. U. S. A 90 (1993) 4156–4160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Liu S, Tan D, Li C, Specific cellular and humoral immune responses induced by intramuscular injection of DNA vaccine containing HBV HBsAg gene in mice, Hunan Yi Ke Da Xue Xue Bao (Bull. Hunan Med. Univ.), 24 (1999) 313–315. [PubMed] [Google Scholar]
- [3].Widera G, Austin M, Rabussay D, Goldbeck C, Barnett SW, Chen M, Leung L, Otten GR, Thudium K, Selby MJ, Ulmer JB, Increased DNA vaccine delivery and immunogenicity by electroporation in vivo, J. Immunol 164 (2000) 4635–4640. [DOI] [PubMed] [Google Scholar]
- [4].Otten G, Schaefer M, Doe B, Liu H, Srivastava I, zur Megede J, O’Hagan D, Donnelly J,Widera G, Rabussay D, Lewis MG, Barnett S, Ulmer JB, Enhancement of DNA vaccine potency in rhesus macaques by electroporation, Vaccine 22 (2004) 2489–2493. [DOI] [PubMed] [Google Scholar]
- [5].Otten GR, Schaefer M, Doe B, Liu H, Megede JZ, Donnelly J, Rabussay D, Barnett S, Ulmer JB, Potent immunogenicity of an HIV-1 gag-pol fusion DNA vaccine delivered by in vivo electroporation, Vaccine 24 (2006) 4503–4509. [DOI] [PubMed] [Google Scholar]
- [6].Luckay A, Sidhu MK, Kjeken R, Megati S, Chong SY, Roopchand V, Garcia-Hand D,Abdullah R, Braun R, Montefiori DC, Rosati M, Felber BK, Pavlakis GN, Mathiesen I, Israel ZR, Eldridge JH, Egan MA, Effect of plasmid DNA vaccine design and in vivo electroporation on the resulting vaccine-specific immune responses in rhesus macaques, J. Virol 81 (2007) 5257–5269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Drabick JJ, Glasspool-Malone J, King A, Malone RW, Cutaneous transfection and immune responses to intradermal nucleic acid vaccination are significantly enhanced by in vivo electropermeabilization, Mol. Ther 3 (2001) 249–255. [DOI] [PubMed] [Google Scholar]
- [8].Babiuk S, Baca-Estrada ME, Foldvari M, Storms M, Rabussay D, Widera G, Babiuk LA, Electroporation improves the efficacy of DNA vaccines in large animals, Vaccine 20 (2002) 3399–3408. [DOI] [PubMed] [Google Scholar]
- [9].Kadowaki S, Chen Z, Asanuma H, Aizawa C, Kurata T, Tamura S, Protection against influenza virus infection in mice immunized by administration of hemagglutinin-expressing DNAs with electroporation, Vaccine 18 (2000) 2779–2788. [DOI] [PubMed] [Google Scholar]
- [10].Laddy DJ, Yan J, Khan AS, Andersen H, Cohn A, Greenhouse J, Lewis M,Manischewitz J, King LR, Golding H, Draghia-Akli R, Weiner DB, Electroporation of synthetic DNA antigens offers protection in nonhuman primates challenged with highly pathogenic avian influenza virus, J. Virol 83 (2009) 4624–4630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Zheng L, Wang F, Yang Z, Chen J, Chang H, Chen Z, A single immunization with HA DNA vaccine by electroporation induces early protection against H5N1 avian influenza virus challenge in mice, BMC Infect. Dis 9 (2009) 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chen Z, Kadowaki S, Hagiwara Y, Yoshikawa T, Matsuo K, Kurata T, Tamura S, Cross-protection against a lethal influenza virus infection by DNA vaccine to neuraminidase, Vaccine 18 (2000) 3214–3222. [DOI] [PubMed] [Google Scholar]
- [13].Bachy M, Boudet F, Bureau M, Girerd-Chambaz Y, Wils P, Scherman D, Meric C, Electric pulses increase the immunogenicity of an influenza DNA vaccine injected intramuscularly in the mouse, Vaccine 19 (2001) 1688–1693. [DOI] [PubMed] [Google Scholar]
- [14].Livingston BD, Little SF, Luxembourg A, Ellefsen B, Hannaman D, Comparative performance of a licensed anthrax vaccine versus electroporation based delivery of a PA encoding DNA vaccine in rhesus macaques, Vaccine 28 (2010) 1056–1061. [DOI] [PubMed] [Google Scholar]
- [15].Luxembourg A, Hannaman D, Nolan E, Ellefsen B, Nakamura G, Chau L, Tellez O, Little S, Bernard R, Potentiation of an anthrax DNA vaccine with electro-poration, Vaccine 26 (2008) 5216–5222. [DOI] [PubMed] [Google Scholar]
- [16].McMahon JM, Wells DJ, Electroporation for gene transfer to skeletal muscles: current status, BioDrugs 18 (2004) 155–165. [DOI] [PubMed] [Google Scholar]
- [17].Heller R, Cruz Y, Heller LC, Gilbert RA, Jaroszeski MJ, Electrically mediated delivery of plasmid DNA to the skin, using a multielectrode array, Hum. Gene Ther 21 (2010) 357–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Guo S, Donate A, Basu G, Lundberg C, Heller L, Heller R, Electro-gene transfer to skin using a noninvasive multielectrode array, J. Control. Release 151 (2011) 256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ferraro B, Heller LC, Cruz YL, Guo S, Donate A, Heller R, Evaluation of delivery conditions for cutaneous plasmid electrotransfer using a multielectrode array, Gene Ther 18 (2011) 496–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Donate A, Coppola D, Cruz Y, Heller R, Evaluation of a novel non-penetrating electrode for use in DNA vaccination, PLoS One 6 (2011) e19181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Puziss M, Wright GG, Studies on immunity in anthrax. IV. Factors influencing elaboration of the protective antigen of Bacillus anthracis in chemically defined media, J. Bacteriol 68 (1954) 474–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Wasserman GM, Grabenstein JD, Pittman PR, Rubertone MV, Gibbs PP, Wang LZ, Golder LG, Analysis of adverse events after anthrax immunization in US Army medical personnel, J. Occup. Environ. Med 45 (2003) 222–233. [DOI] [PubMed] [Google Scholar]
- [23].Wright JG, Quinn CP, Shadomy S, Messonnier N, Use of anthrax vaccine in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009, MMWR. Recomm. Rep.: Morb. Mortal Wkly Rep. Recomm. Rep. / CDC 59 (2010) 1–30. [PubMed] [Google Scholar]
- [24].Wright GG, Green TW, Kanode RG Jr., Studies on immunity in anthrax. V. Immunizing activity of alum-precipitated protective antigen, J. Immunol 73 (1954) 387–391. [PubMed] [Google Scholar]
- [25].Duesbery NS, Vande Woude GF, Anthrax lethal factor causes proteolytic inactivation of mitogen-activated protein kinase kinase, J. Appl. Microbiol 87 (1999) 289–293. [DOI] [PubMed] [Google Scholar]
- [26].Duesbery NS, Webb CP, Leppla SH, Gordon VM, Klimpel KR, Copeland TD, Ahn NG, Oskarsson MK, Fukasawa K, Paull KD, Vande Woude GF, Proteolytic inactivation of MAP-kinase–kinase by anthrax lethal factor, Science 280 (1998) 734–737. [DOI] [PubMed] [Google Scholar]
- [27].Ivins BE, Ezzell JW Jr., Jemski J, Hedlund KW, Ristroph JD, Leppla SH, Immunization studies with attenuated strains of Bacillus anthracis, Infect. Immun 52 (1986) 454–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Leppla SH, Robbins JB, Schneerson R, Shiloach J, Development of an improved vaccine for anthrax, J. Clin. Invest 110 (2002) 141–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Hahn UK, Alex M, Czerny CP, Bohm R, Beyer W, Protection of mice against challenge with Bacillus anthracis STI spores after DNA vaccination, Int. J. Med. Microbiol 294 (2004) 35–44. [DOI] [PubMed] [Google Scholar]
- [30].Hahn UK, Boehm R, Beyer W, DNA vaccination against anthrax in mice-combination of anti-spore and anti-toxin components, Vaccine 24 (2006) 4569–4571. [DOI] [PubMed] [Google Scholar]
- [31].Heller LC, Jaroszeski MJ, Coppola D, McCray AN, Hickey J, Heller R, Optimization of cutaneous electrically mediated plasmid DNA delivery using novel electrode, Gene Ther 14 (2007) 275–280. [DOI] [PMC free article] [PubMed] [Google Scholar]